Abstract
Suicide is among the most devastating problems facing clinicians, who currently have limited tools to predict and prevent suicidal behavior. Here we report on real-time, continuous smartphone and sensor data collected before, during, and after a suicide attempt made by a patient during a psychiatric inpatient hospitalization. We observed elevated and persistent sympathetic nervous system arousal and suicidal thinking leading up to the suicide attempt. This case provides the highest resolution data to date on the psychological, psychophysiological, and behavioral markers of imminent suicidal behavior and highlights new directions for prediction and prevention efforts.
Keywords: suicide, suicidal ideation, inpatient, wearables
Suicide is a leading cause of death1 and rates of psychiatric inpatient unit admissions due to suicidal thoughts and behaviors (STBs) have increased over the past decade.2 Suicidal behaviors on inpatient units are a relatively common and devastating clinical phenomenon.3 Unfortunately, clinicians have limited tools to predict which inpatients are at highest risk for suicide, and when risk is highest.4 Current standards of risk assessment on inpatient units rely on in-person observation by staff members and patients’ self-reported levels of risk.2 These strategies are resource-intensive and fail to capture many instances of risk. One study found that 78% of patients who died by suicide on an inpatient unit denied suicidal ideation in their last verbal communications with providers before killing themselves.5
A crucial step in building an understanding of suicide is more carefully observing the natural unfolding of suicidal behavior.6 Digital phenotyping, defined as “the moment-by-moment quantification of the individual-level phenotype in situ using data from personal digital devices,”7 provides an opportunity to study suicidal behavior as it unfolds in real-time.8 We present a report of a patient who attempted suicide on an inpatient unit while participating in an intensive longitudinal monitoring study. This report focuses on description of the clinical phenomenon rather than any a priori hypotheses. This report is the first to document the fine-grained psychological, psychophysiological, and behavioral characteristics associated with suicidal behavior captured in real-time.
Methods
Study Protocol
This patient was participating in a real-time monitoring study aiming to identify psychological and physiological predictors of suicidal behavior.9 All study procedures were approved by the primary Institutional Review Board for Massachusetts General Hospital, Partners Healthcare IRB (IRB# 2015P000598, “Real-time assessment of suicidal thoughts among psychiatric inpatients”). We focus on a case report in the current paper as the patient described here was the only patient in the overall study with a self-reported and medically documented suicide attempt.
As part of the parent study, six surveys per day (randomly within pre-defined windows) were sent to her smartphone and the patient was monitored passively with a wrist-worn biosensor.10 Current suicidal thoughts were measured with three items that assessed: (a) current desire to die by suicide, (b) current intention to die by suicide, and (c) current ability to resist the urge to die by suicide. All items were rated on a 0 (none) to 9 (very much) scale. The three items were summed (with ability to resist the urge to die by suicide reverse coded) to create a suicidal thought sum score (0 to 27). These items are based on the Beck Scale for Suicide Ideation 11, have been used other real-time studies of suicidal thinking 12,13, and have shown predictive validity for suicide behavior.9 Fifteen momentary affective states were measured with self-report items rated on a 1 (very low) to 10 (very high) scale. These states were taken from the Positive and Negative Affect Schedule14 and include other cognitive-affective states associated with risk for suicide.15 The 15 states assessed were: fatigued, desperate, hopeless, abandoned, self-hate, rage, anxious, lonely, guilty, humiliated, upset, ashamed, nervous, afraid, burdensome. More details on the psychometrics of these items in the overall study have been published.16 We used all the smartphone surveys the patient completed for descriptive statistics and visualizations.
For the duration of the inpatient stay, the patient wore a research-grade wrist-worn behavioral and psychophysiological monitor (Empatica E4). The E4 has been analytically validated against laboratory devices.17,18 In the parent study, patients were asked to wear two monitors (one on each wrist). Patients were asked to wear two monitors to examine asymmetry in sympathetic nervous system activation across the two halves of the body.19 Due to technical issues with the available monitors, this patient wore one monitor on her right wrist for the duration of the study. She wore one monitor on study days 0 to 3, and a second monitor (due to a memory problem with the first) on days 4 to 5.
We created features from the movement (via 3-axis accelerometer) and electrodermal activity sensors (measured in microsiemens). We focused on the movement sensor because of prior research has found an association between agitation, which includes increased motor function, and suicidal thoughts and behaviors.20 Additionally, numerous algorithms have been developed for accurately processing and classifying movement data.21 We also focused on the electrodermal activity sensors because sympathetic autonomic activity is broadly associated with psychological distress and high arousal.22 Prior research using laboratory based electrodermal activity sensors have found an association between electrodermal activity and suicidal thoughts and behaviors.23
We specifically focused on biosensor data during morning hours (6am - noon) each day because time of day can impact physiology,24 disruptions in circadian processes have been associated with suicidal behavior,25 and the patient’s suicide attempt occurred during the morning hours. All biosensor results presented in the current report were consistent when using only data during the morning and all data from the day. Results with biosensor data from the entire day are available in the supplemental materials. From the electrodermal activity sensors we created the following features: average skin conductance level, average skin conductance response peaks amplitude, and time-varying EDA index of sympathetic control (TVSymp). TVSymp is created by using the mean spectral amplitudes in the frequency band associated with sympathetic tone of the EDA.26 This allows some extraction of the components of EDA (i.e., sympathetic arousal) most likely associated with psychological stress. We ran a classification algorithm on the accelerometer data to classify activity into light, moderate, and vigorous.21 For each day during the morning hours, we computed the time spent at each of these three different activity levels. The patient did not wear the monitor on the morning of study day 0 and therefore we began analyses on study day 1. We visualized these different features of physiology and activity for each day.
Case Description
The patient was a woman in her 50s diagnosed with borderline personality disorder, significant somatization, and unspecified depressive disorder. She was admitted to the hospital following a suicide attempt. The goal of the admission was mood stabilization and reduction of suicidal thoughts. The patient was in the hospital for a total of ten days. She provided informed consent for the study on their fourth day of hospitalization and then was in the study for seven days.
At the start of treatment, the patient reported to staff that she thought about suicide all the time and had a suicide plan. During her stay, the team attempted to assist her with managing her suicidal thoughts and urges. The patient made a suicide attempt on the morning of her ninth day of treatment (study day 5) via cutting her arm with a piece of glass. We verified the suicide attempt through patient self-report at the time of discharge and chart review – including matching dates/times of the attempt. In the discharge survey, the patient specifically endorsed the item, “Did you make a suicide attempt (that is, purposefully hurt yourself with at least some intent to die)?” and endorsed doing things to prepare to kill herself during hospitalization. The author team determined this qualified as suicidal behavior rather than non-suicidal self-injury because the patient reported intent to die in both the momentary and end of study surveys and engaged in self-injurious behavior.27 A nurse was called following the attempt and a surgical team sutured the wound. The patient later reported to staff that the attempt occurred due to her impulsivity.
Although the patient continued to have suicidal thoughts, her mood was functionally stabilized during her stay. After the self-inflicted laceration, the multidisciplinary team felt that further hospitalization would increase her regression, would not reduce acute risk, and would likely provoke more impulsive self-injurious behaviors. Medications were adjusted to address this, and a safety plan was developed. The patient’s medication treatment is shown in Figure 1. While risperidone and gabapentin were administered a day before the attempt, these medications were added in an attempt to address the patient’s increasing distress. The increased suicidal thinking in the context of these medications is more likely an epiphenomenon than caused by the medications. She was referred to a partial hospital program for ongoing support after discharge.
Figure 1.
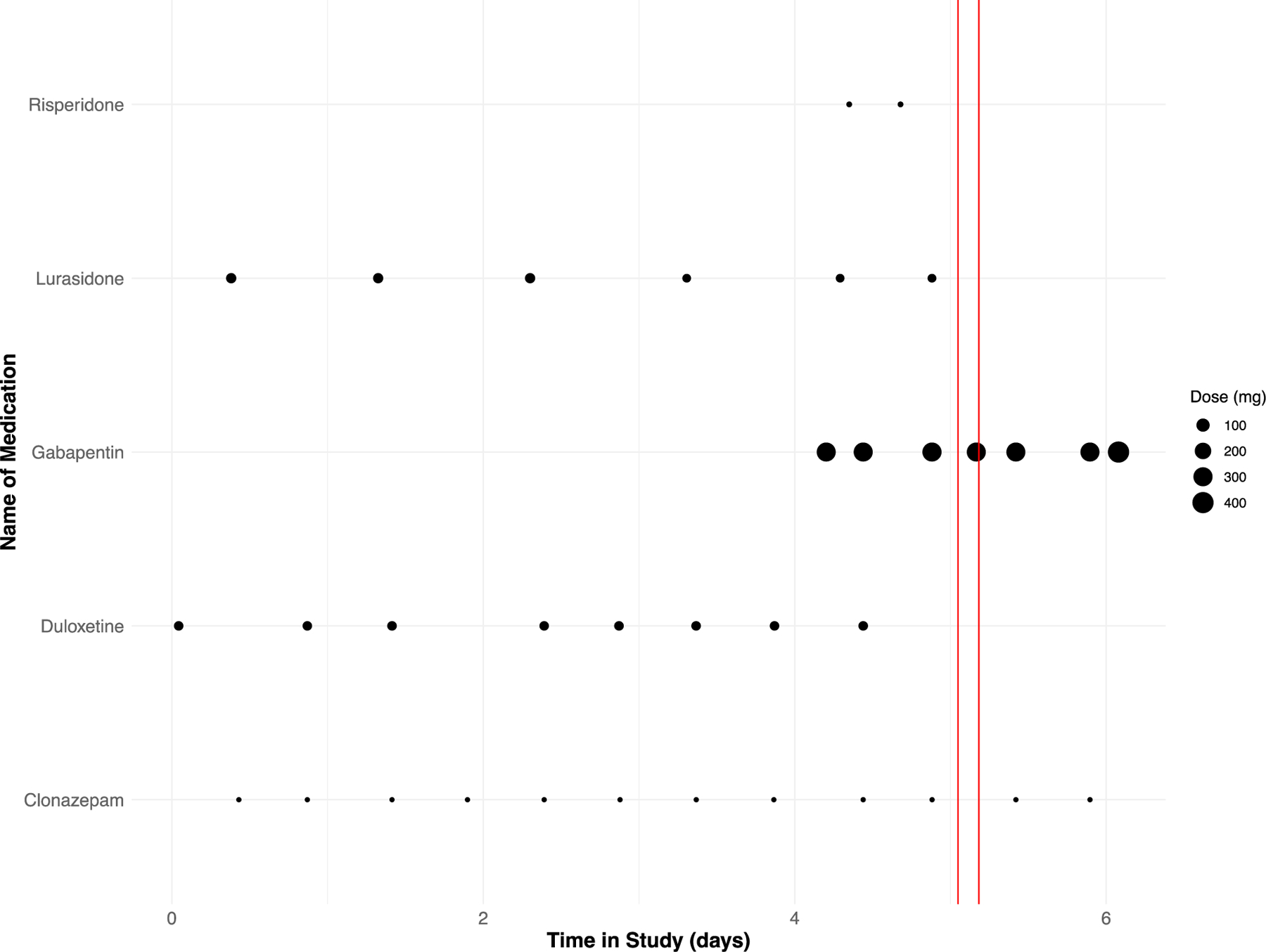
Psychotropic medications administered over time. Note: The two red lines indicate the estimated window of the suicide attempt.
Results
Real-Time Suicidal Thoughts and Affect
The patient completed 24 (66% compliance) smartphone-based self-report surveys during hospitalization. Observation of the patient’s smartphone-based self-report data reveals several notable findings. First, the patient reported a sustained period of maximum severity of suicidal thoughts (27 out of 27) in the 2-day period (4 surveys at maximum severity) leading up to her suicide attempt (Figure 2, Panel A). In the larger study of 83 inpatients,9 only 1.31% of the 1,374 smartphone-based self-reports were at the maximum severity of suicidal thoughts. Second, the patient reported similar sustained increases in some of the negative affective states. For example, increases in desperation, burdensomeness, and hopelessness, each lasted at least 24 hours (Figure 2, Panel B).
Figure 2.
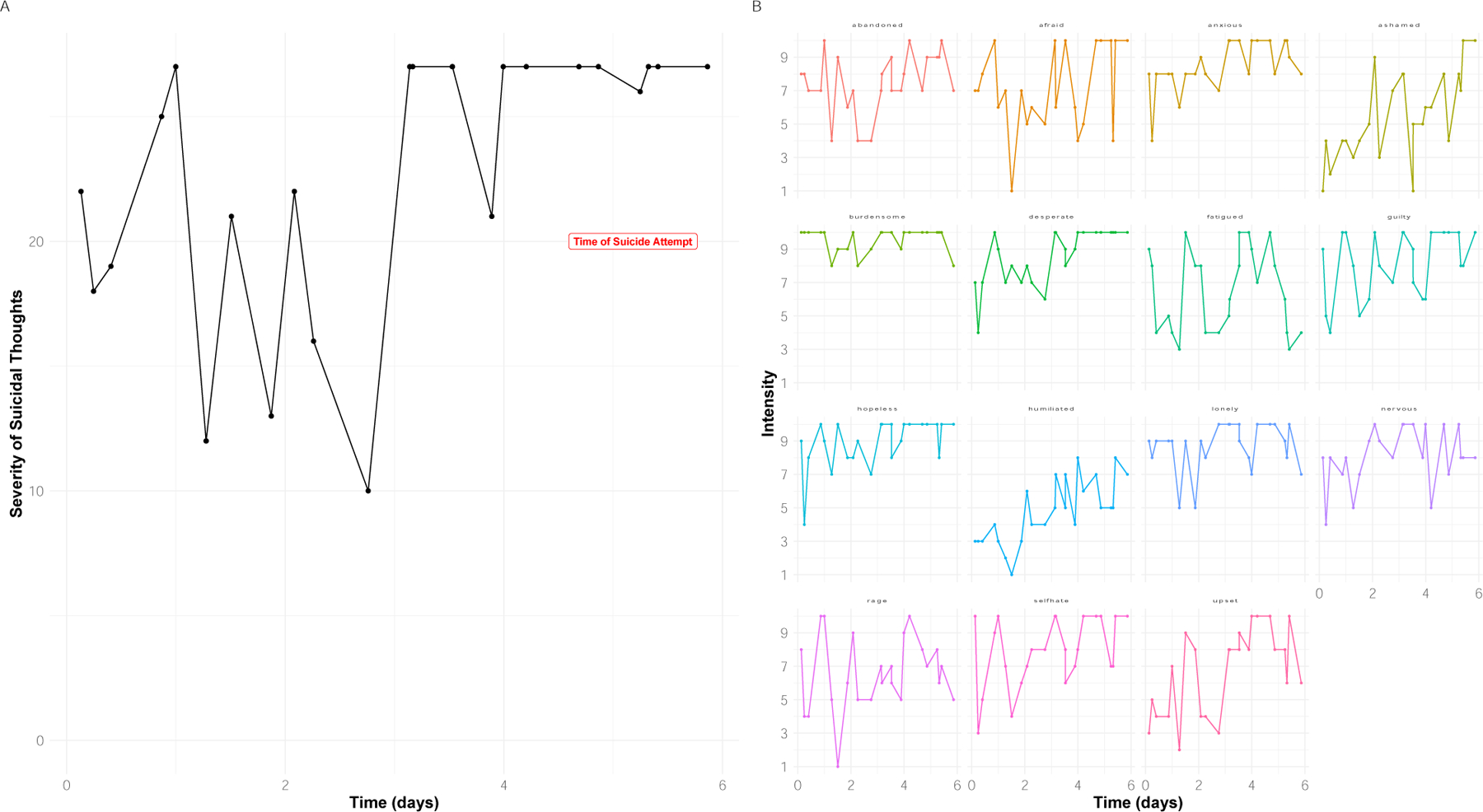
Suicidal thoughts and affective states over time. Time is coded continuously from when the patient enrolled in the study.
(A) Suicidal thoughts measured via smartphone surveys;
(B) Affective states measured via smartphone surveys.
Psychophysiology
Psychophysiological data also revealed several notable findings in sympathetic nervous system activation building up to the attempt (Figure 3). In the 4 days preceding the suicide attempt, the activity and EDA measures aggregated over morning were increasing. On day 4, the day prior to the attempt, all EDA measures were elevated, and the patient showed more time at light and moderate activity. On that day, the patient reported to staff feeling irritated, an inability to sit still, and difficulty sleeping leading up to the suicide attempt.
Figure 3.

Physiology and activity data streams over time. Note: the attempt occurred on day 5.
(A) Time at different activity levels (Light, Moderate and Vigorous) aggregated over morning hours (6am - noon) computed from accelerometer data;
(B) Average Electrodermal Activity (EDA) Skin Conductance Level (SCL) during morning hours;
(C) Number of EDA peaks during morning hours;
(D) Average EDA Skin Conductance Response (SCR) peaks amplitude during morning hours;
(E) Time-varying EDA index of sympathetic control (TVSymp) computed during morning hours by using the mean spectral amplitudes in the frequency band associated with sympathetic tone of the EDA.
Note: The red box indicates the day of the suicide attempt.
Discussion
This case report presents for the first time the psychological, psychophysiological, and behavioral features characterizing a suicide attempt as it unfolded in real-time. There are three main findings from this case report. First, digital phenotyping is a feasible approach for collecting data to better understand suicidal behavior. Second, we observed elevated suicidal thinking in the two days leading up to the suicide attempt. Third, passively observed physiological data also revealed a pattern of increased physical activity and sympathetic arousal in the days leading up to the attempt. We expand upon each of these points below.
While in the throes of suicidal thinking, the patient engaged with digital technologies and provided valuable data on their experiences. A common concern is that intensive engagement required of digital phenotyping could be too burdensome for patients. Contrary to this belief, this patient receiving intensive psychiatric hospital care completed the majority of smartphone surveys and wore the wearable device for the majority of her hospitalization. The smartphone surveys compliance of this patient (66%) was actually higher than the average compliance (52%) in the overall study.9 The relatively high levels of engagement resulted in high-resolution data at a low clinical burden that has the potential to inform clinical decision-making.
The precise relationship between suicidal thinking and behavior is relatively unknown because of the historically long follow-up periods between assessment periods.4 The closest research has come so far are follow-back methods where following a suicide attempt, participants recall what their thoughts and emotions looked like prior to the behavior28 or short-term prediction over a few days or weeks.9,29 This research suggests that variability in suicidal thinking may be a warning sign prior to suicidal behavior.9 In the current case, we zoomed in on this relationship at an extremely granular timescale. The findings suggest that whereas between-day variability may be indicative of overall risk, within-day persistence may be indicative of imminent risk. This builds on prior work showing that thinking about suicide for extended periods of time (e.g., 5 hours per day) is a risk factor suicidal behavior among people with suicidal ideation.30 This case demonstrates how digital phenotyping allows us to examine the timescales in which suicide risk unfolds as well as when risk of suicidal behavior may be elevated. Digital phenotyping can thus help study people more closely at the individual level.31
Suicidal behavior is a dynamic and complex process that unfolds quickly over short timeframes of minutes and hours.8 Historically, psychiatry and psychology have relied on static measurements to understand this dynamic process. Digital phenotyping provides dynamic multivariate data at high resolution to understand this process. In the current case report, passive data types showed increased activity and arousal leading up to the suicide attempt. The EDA findings from the current case report also align with recent work predicting suicidal thinking with EDA captured via wearable devices.32 All these factors map onto existing risk factors for suicidal behavior.20 Digital phenotyping, however, allows for these factors to be captured at relatively low burden and cost. The current report provides preliminary validity for using digital phenotyping to study suicidal behavior.
This case has several notable limitations. First, the results reflect only one patient having only one suicide attempt captured. Many more such cases are needed before general statements can be made. Second, this attempt was of relatively low lethality and therefore the phenotype captured here may not generalize to more lethal attempts. Additionally, the phenotype of a suicide attempt does not necessarily generalize to suicide death.4 Fourth, this case highlights the challenge of distinguishing suicide attempts from non-suicidal self-injury 27,33 with low-lethality self-injury. Fifth, the wearable data showed trends at the daily level, but precise temporal prediction of suicidal thinking and attempts will require significantly larger sets of data, covering many real-world suicide attempts, before an algorithm could be trained to reliably perform prediction. Finally, the psychological and behavioral processes associated with suicidal behavior in the context of a psychiatric inpatient unit may not generalize to suicidal behavior in everyday life.
Future studies could expand upon this case report. Given the relatively low base-rate of suicidal behavior, digital phenotyping consortia could be formed to capture a large number of cases of suicidal behavior. A greater number of cases will allow for tests of generality and heterogeneity in real-time suicide risk. Ultimately, a more precise understanding of suicidal behavior from digital phenotyping could be leveraged to develop just-in time adaptive interventions for suicidal behavior.34,35 This case illustrates how digital phenotyping has the potential to transform how we understand, predict, and ultimately prevent suicide.
Supplementary Material
Funding:
This research was supported by the Chet and Will Griswold Suicide Prevention Fund. Ms Wang and Mr Coppersmith are supported by the National Science Foundation Graduate Research Fellowship under grant No. DGE-1745303. Mr. Coppersmith is also supported by the National Institute of Mental Health under Grant F31MH130055. Ms. Wang is also supported by the National Institute of Mental Health under Grant F31MH125495. Dr. Bentley is supported by the National Institute of Mental Health under Grant K23MH120436.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Declaration of Interest statement:
Dr. Picard receives royalties on patents for her AI-related and wearables inventions owned by MIT and is a co-founder and shareholder of Empatica, Inc., where she serves as Chairman of the Board and consults part-time as Chief Scientist. She is also a shareholder at Smart Eye AB, which acquired Affectiva, a company she co-founded. At MIT, her lab’s research receives funding from a consortium of over fifty companies listed at https://www.media.mit.edu/posts/member-companies/. She receives speaker fees through Stern Strategy. Dr. Huffman receives salary support from Elsevier outside the submitted work. Dr. Nock receives publication royalties from Macmillan, Pearson, and UpToDate. He has been a paid consultant in the past year for Microsoft Corporation, the Veterans Health Administration, and for a legal case regarding a death by suicide. He holds stock options in Cerebral Inc and is an unpaid scientific advisor for Empatica, Koko, and TalkLife.
References
- 1.Fazel S, Runeson B. Suicide. New England Journal of Medicine 2020;382(3):266–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kleiman EM, Nock MK. New directions for improving the prediction, prevention, and treatment of suicidal thoughts and behaviors among hospital patients. General Hospital Psychiatry 2020;63:1–4. [DOI] [PubMed] [Google Scholar]
- 3.Bowers L, Banda T, Nijman H. Suicide Inside: A Systematic Review of Inpatient Suicides. The Journal of Nervous and Mental Disease 2010;198(5):315–28. [DOI] [PubMed] [Google Scholar]
- 4.Franklin JC, Ribeiro JD, Fox KR, et al. Risk factors for suicidal thoughts and behaviors: A meta-analysis of 50 years of research. Psychological Bulletin 2017;143(2):187–232. [DOI] [PubMed] [Google Scholar]
- 5.Busch KA, Fawcett J, Jacobs DG. Clinical correlates of inpatient suicide. J Clin Psychiatry 2003;64(1):14–9. [DOI] [PubMed] [Google Scholar]
- 6.Millner AJ, Robinaugh DJ, Nock MK. Advancing the Understanding of Suicide: The Need for Formal Theory and Rigorous Descriptive Research. Trends in Cognitive Sciences 2020;24(9):704–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Onnela J-P, Rauch SL. Harnessing Smartphone-Based Digital Phenotyping to Enhance Behavioral and Mental Health. Neuropsychopharmacology 2016;41(7):1691–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kleiman EM, Nock MK. Real-time assessment of suicidal thoughts and behaviors. Current Opinion in Psychology 2018;22:33–7. [DOI] [PubMed] [Google Scholar]
- 9.Wang SB, Coppersmith DDL, Kleiman EM, et al. A Pilot Study Using Frequent Inpatient Assessments of Suicidal Thinking to Predict Short-Term Postdischarge Suicidal Behavior. JAMA Network Open 2021;4(3):e210591–e210591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Torous J, Kiang MV, Lorme J, Onnela J-P. New Tools for New Research in Psychiatry: A Scalable and Customizable Platform to Empower Data Driven Smartphone Research. JMIR Ment Health 2016;3(2):e16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Beck AT, Kovacs M, Weissman A. Assessment of suicidal intention: The Scale for Suicide Ideation. Journal of Consulting and Clinical Psychology 1979;47(2):343–52. [DOI] [PubMed] [Google Scholar]
- 12.Kleiman EM, Turner BJ, Fedor S, Beale EE, Huffman JC, Nock MK. Examination of real-time fluctuations in suicidal ideation and its risk factors: Results from two ecological momentary assessment studies. Journal of Abnormal Psychology 2017;126(6):726–38. [DOI] [PubMed] [Google Scholar]
- 13.Coppersmith DDL, Fortgang RG, Kleiman EM, et al. Effect of frequent assessment of suicidal thinking on its incidence and severity: high-resolution real-time monitoring study. Br J Psychiatry 2022;220(1):41–3. [DOI] [PubMed] [Google Scholar]
- 14.Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: the PANAS scales. J Pers Soc Psychol 1988;54(6):1063–70. [DOI] [PubMed] [Google Scholar]
- 15.Van Orden KA, Witte TK, Cukrowicz KC, Braithwaite S, Selby EA, Joiner TE. The Interpersonal Theory of Suicide. Psychol Rev 2010;117(2):575–600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bentley KH, Coppersmith DL, Kleiman EM, et al. Do Patterns and Types of Negative Affect During Hospitalization Predict Short-Term Post-Discharge Suicidal Thoughts and Behaviors? Affec Sci 2021;2(4):484–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.McCarthy C, Pradhan N, Redpath C, Adler A. Validation of the Empatica E4 wristband In: 2016 IEEE EMBS International Student Conference (ISC). 2016. p. 1–4. [Google Scholar]
- 18.Schuurmans AAT, de Looff P, Nijhof KS, et al. Validity of the Empatica E4 Wristband to Measure Heart Rate Variability (HRV) Parameters: a Comparison to Electrocardiography (ECG). J Med Syst 2020;44(11):190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Picard RW, Fedor S, Ayzenberg Y. Multiple Arousal Theory and Daily-Life Electrodermal Activity Asymmetry. Emotion Review 2016;8(1):62–75. [Google Scholar]
- 20.Rogers ML, Ringer FB, Joiner TE. A meta-analytic review of the association between agitation and suicide attempts. Clinical Psychology Review 2016;48:1–6. [DOI] [PubMed] [Google Scholar]
- 21.Migueles JH, Cadenas-Sanchez C, Rowlands AV, et al. Comparability of accelerometer signal aggregation metrics across placements and dominant wrist cut points for the assessment of physical activity in adults. Sci Rep 2019;9(1):18235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kilpatrick DG. Differential Responsiveness of Two Electrodermal Indices to Psychological Stress and Performance of a Complex Cognitive Task. Psychophysiology 1972;9(2):218–26. [DOI] [PubMed] [Google Scholar]
- 23.Sarchiapone M, Gramaglia C, Iosue M, et al. The association between electrodermal activity (EDA), depression and suicidal behaviour: A systematic review and narrative synthesis. BMC Psychiatry 2018;18(1):22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hot P, Naveteur J, Leconte P, Sequeira H. Diurnal variations of tonic electrodermal activity. Int J Psychophysiol 1999;33(3):223–30. [DOI] [PubMed] [Google Scholar]
- 25.Perlis ML, Grandner MA, Chakravorty S, Bernert RA, Brown GK, Thase ME. Suicide and sleep: Is it a bad thing to be awake when reason sleeps? Sleep Med Rev 2016;29:101–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Posada-Quintero HF, Florian JP, Orjuela-Cañón ÁD, Chon KH. Highly sensitive index of sympathetic activity based on time-frequency spectral analysis of electrodermal activity. American Journal of Physiology-Regulatory, Integrative and Comparative Physiology 2016;311(3):R582–91. [DOI] [PubMed] [Google Scholar]
- 27.Nock MK. Self-injury. Annu Rev Clin Psychol 2010;6:339–63. [DOI] [PubMed] [Google Scholar]
- 28.Bagge CL, Littlefield AK, Glenn CR. Trajectories of Affective Response as Warning Signs for Suicide Attempts: An Examination of the 48 Hours Prior to a Recent Suicide Attempt. Clinical Psychological Science 2017;5(2):259–71. [Google Scholar]
- 29.Ribeiro JD, Huang X, Fox KR, Walsh CG, Linthicum KP. Predicting Imminent Suicidal Thoughts and Nonfatal Attempts: The Role of Complexity. Clinical Psychological Science 2019;7(5):941–57. [Google Scholar]
- 30.Nock MK, Millner AJ, Joiner TE, et al. Risk Factors for the Transition from Suicide Ideation to Suicide Attempt: Results from the Army Study to Assess Risk and Resilience in Servicemembers (Army STARRS). J Abnorm Psychol 2018;127(2):139–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sewall CJR, Wright AGC. Personalizing Suicidology. Crisis 2021;42(6):405–10. [DOI] [PubMed] [Google Scholar]
- 32.Kleiman EM, Bentley KH, Maimone JS, et al. Can passive measurement of physiological distress help better predict suicidal thinking? Transl Psychiatry 2021;11(1):1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Millner AJ, Lee MD, Nock MK. Single-Item Measurement of Suicidal Behaviors: Validity and Consequences of Misclassification. PLOS ONE 2015;10(10):e0141606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Nahum-Shani I, Smith SN, Spring BJ, et al. Just-in-Time Adaptive Interventions (JITAIs) in Mobile Health: Key Components and Design Principles for Ongoing Health Behavior Support. Ann Behav Med 2018;52(6):446–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Coppersmith DDL, Dempsey W, Kleiman EM, Bentley KH, Murphy SA, Nock MK. Just-in-Time Adaptive Interventions for Suicide Prevention: Promise, Challenges, and Future Directions. Psychiatry 2022;0(0):1–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


