Abstract
Introduction
The COVID-19 pandemic has been challenging for healthcare systems in the United States and globally. Understanding how the COVID-19 pandemic has impacted emergency departments (EDs) and patient outcomes in a large integrated healthcare system may help prepare for future pandemics. Our primary objective was to evaluate if there were changes to ED boarding and in-hospital mortality before and during the COVID-19 pandemic.
Methods
This was a retrospective cohort study of all patients ages 18 and over who presented to one of 17 EDs (11 hospital-based; 6 freestanding) within our healthcare system. The study timeframe was March 1, 2019- February 29, 2020 (pre-pandemic) vs. March 1, 2020-August 31, 2021 (during the pandemic). Categorical variables are described using frequencies and percentages, and p-values were obtained from Pearson chi-squared or Fisher's exact tests where appropriate. In addition, multiple regression analysis was used to compare ED boarding and in-hospital mortality pre-pandemic vs. during the pandemic.
Results
A total of 1,374,790 patient encounters were included in this study. In-hospital mortality increased by 16% during the COVID-19 Pandemic AOR 1.16(1.09–1.23, p < 0.0001). Boarding increased by 22% during the COVID-19 pandemic AOR 1.22(1.20–1.23), p < 0.0001). More patients were admitted during the COVID-19 pandemic than prior to the pandemic (26.02% v 24.97%, p < 0.0001). Initial acuity level for patients presenting to the ED increased for both high acuity (13.95% v 13.18%, p < 0.0001) and moderate acuity (60.98% v 59.95%, p < 0.0001) during the COVID-19 pandemic.
Conclusion
The COVID-19 pandemic led to increased ED boarding and in-hospital mortality.
Keywords: Boarding, COVID-19, Emergency department, Mortality
1. Introduction
The COVID-19 pandemic has been challenging for healthcare systems in the United States and globally, with COVID-19 claiming over one million lives in the United States since March 2020 [1]. Initial studies that analyzed the impact COVID-19 had on the emergency department (ED) during the first several months of the pandemic showed decreased patient volumes and hospital admission [[2], [3], [4], [5], [6], [7], [8], [9], [10]]. However, these studies focused on the initial phases of the pandemic, with only one study using patient data as late as September 2020. Since prior studies only evaluated the initial phase of the COVID-19 pandemic, understanding the long-term impact on ED boarding and patient mortality has yet to be studied.
Studies before the COVID-19 pandemic showed ED boarding and increased ED length of stay correlated with increased hospital length of stay and in-hospital mortality [[11], [12], [13]]. Early in the COVID-19 pandemic, research showed patients had longer lengths of stay despite decreased ED volumes [14]. However, this study did not report any overall patient outcomes. Our study aims to bridge the literature gap from the COVID-19 pandemic's initial phase with more current data.
The primary objective of this study was to determine if the COVID-19 pandemic impacted ED boarding compared to the year prior to the COVID-19 pandemic. The secondary objective of this study was to determine if there was a difference in all cause in-hospital mortality pre-pandemic and during the COVID-19 pandemic.
2. Methods
2.1. Study design
This was a retrospective cohort study of all patients who presented to one of 17 EDs (11 hospital-based; 6 freestanding) within a large integrated healthcare system. The study timeframe was March 1, 2019--February 29, 2020 (pre-pandemic) vs. March 1, 2020--August 31, 2021 (during the COVID-19 pandemic). This study was approved by the Institutional Review Board.
2.2. Setting
The population studied included all patients ages 18 and over who presented to an ED within the healthcare system. Our healthcare system EDs are a mix of academic, community, critical access, and freestanding.
2.3. Selection of participants
Participants were eligible if they were seen at one of 17 emergency departments within our healthcare system. Patients were excluded if they had missing data.
2.4. Data collection
Study data were abstracted from the electronic medical record (EPIC®, Verona, WA.) via an automated query performed by one data analyst for the healthcare system. The data analyst was blinded to the study hypothesis. Data collected included patient demographic information, ED setting (freestanding, community, academic), emergency severity index score (ESI), COVID-19 test result, ED length of stay (LOS) (defined as the time of patient arrival in the ED until the patient departed the ED), ED disposition (admitted versus discharged), ED boarding, intensive care unit (ICU) admission, hospital (LOS), and in-hospital mortality. A patient was determined to be boarding if they remained in the ED for >60 min from when their disposition was changed to admitted.
2.5. Statistical analyses
Categorical variables were described using frequencies and percentages. P-values were obtained from Pearson chi-squared or Fisher's exact tests for categorical variables. Multiple logistic regression analysis was used to compare boarding and in-hospital mortality pre-pandemic vs. during the pandemic. In addition, a subgroup analysis comparing COVID-19 and non-COVID-19 patients during the COVID-19 pandemic study period was performed to evaluate potential differences between patients with COVID-19 and those without COVID-19.
3. Results
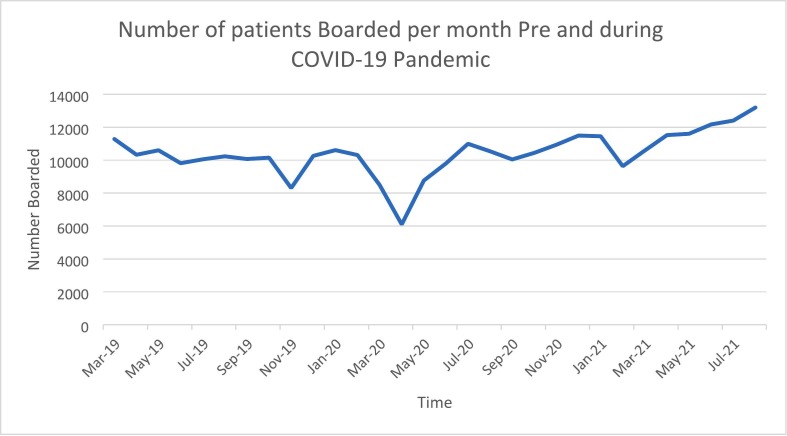
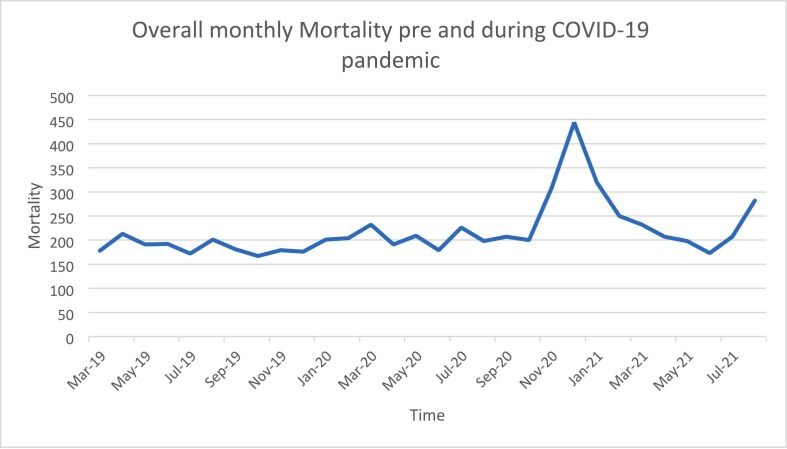
A total of 1,557,513 patient encounters occurred during the study timeframe. Of those encounters, 1,374,790 had complete data sets and were included in our study. Demographic data, ESI score, COVID-19 test results, ED LOS, ED disposition, ED boarding, ICU admission, hospital LOS, and in-patient mortality are reported in Table 1 . Boarding increased by 22% during the COVID-19 pandemic, (95% CI 1.22(1.20–1.23)). In-hospital mortality increased by 16% during the COVID-19 pandemic, (95%CI 1.16(1.09–1.23)). More patients were admitted during the pandemic than before the COVID-19 pandemic (26.02% v 24.97%, p < 0.001). Initial triage ESI score for patients who presented to the ED increased in both high acuity (13.95% v 13.18%, p < 0.0001) and moderate acuity groups (60.98% v 59.95%, p < 0.001) during the COVID-19 pandemic. We found that patients were 88% more likely to board at a hospital-based ED compared to a freestanding ED (95%CI: 1.88 (1.85–1.97)). In addition, we found that patients seen at a hospital-based ED were 229% more likely to die compared to those seen at a freestanding ED (95%CI 2.29 (1.77–2.94)). Boarding and mortality trends pre and post pandemic are shown in Fig. 1, Fig. 2 .
Table 1.
Characteristics of participants pre and During C0VID-19 pandemic, N = 1,374,790.
| Variable | Overall (N = 1,374,790) |
COVID (N = 780,329) |
Pre-C0VID (N = 594,461) |
p-value |
|---|---|---|---|---|
| Age | 46.21(24.024) | 46.94(23.48) | 45.24(24.69) | <0.0001 |
| Gender |
<0.0001 |
|||
| Female | 773,130(56.24) | 434,832(55.72) | 338,298(56.91) | |
| Male | 601,660(43.76) | 345,497(44.28) | 256,163(43.09) | |
| Race |
<0.0001 |
|||
| Black | 462,405(33.63) | 263,822(33.81) | 198,583(33.41) | |
| White | 825,589(60.05) | 467,893(59.96) | 357,696(60.17) | |
| Other | 86,796(6.31) | 48,614(6.23) | 38,182(6.42) | |
| Ethnicity |
0.0136 |
|||
| Hispanic | 56,012(4.07) | 31,509(4.04) | 24,503(4.12) | |
| Not Hispanic | 1,318,778(95.93) | 748,820(95.96) | 569,958(95.88) | |
| Payor |
<0.0001 |
|||
| Medicaid | 488,179 (35.51) | 275,731(35.34) | 212,448(35.74) | |
| Medicare | 362,346 (26.36) | 206,912(26.52) | 155,434(26.15) | |
| Private | 524,265 (38.13) | 297,686(38.15) | 226,579(38.12) | |
| ESI Level |
<0.0001 |
|||
| High | 197,780(14.39) | 115,251(14.77) | 82,529(13.88) | |
| Mod | 837,452(60.91) | 477,906(61.24) | 359,546(60.48) | |
| low | 339,558(24.70) | 187,172(23.99) | 152,386(25.63) | |
| Mortality |
<0.0001 |
|||
| No | 1,368,272(99.53) | 776,066(99.45) | 592,206(99.62) | |
| Yes | 6518(0.47) | 4263(0.55) | 2255(0.38) | |
| ED LOS (mins) | 165.0(95.0–257.0) | 169.0(96.0–265.0) | 160.0(94.0–248.0) | <0.0001 |
| Hospital LOS (Days) | 3.95(2.18–6.73) | 3.98(2.19–6.85) | 3.90(2.17–6.45) | <0.0001 |
| ICU |
<0.0001 |
|||
| No | 1,314,030(95.58) | 745,373(95.52) | 568,657(95.66) | |
| Yes | 60,760(4.42) | 34,956(4.48) | 25,804(4.34) | |
| COVID-19 diagnosis |
<0.0001 |
|||
| No | 1,352,851(98.40) | 758,395(97.19) | 594,456(100.00) | |
| Yes | 21,939(1.60) | 21,934(2.81) | 5(0.00) | |
| Boarded | ||||
| No | 1,062,581(77.29) | 590,135(75.63) | 472,446(79.47) | <0.0001 |
| yes | 312,209(22.710 | 190,194(24.37) | 122,015(20.53) | |
| Admission |
<0.0001 |
|||
| No | 1,123,515(81.72) | 631,162(80.88) | 492,353(82.82) | |
| Yes | 251,275(18.28) | 149,167(19.12) | 102,108(17.18) | |
| Department group |
0.9692 |
|||
| FSED | 228,180(16.60) | 129,523(16.60) | 98,657(16.60) | |
| HBED | 1,146,610(83.40) | 650,806(83.40) | 495,804(83.40) | |
| Department Type |
<0.0001 |
|||
| Academic | 775,169(56.38) | 437,881(56.11) | 337,288(56.74) | |
| Community | 599,621(43.62) | 342,448(43.89) | 257,173(43.26) |
Statistics presented as mean (SD), or Median (Q1 – Q3), or n (%).
Fig. 1.
Monthly boarding in the emergency department pre and during the COVID pandemic.
Fig. 2.
Monthly mortality pre and during the COVID-19 pandemic.
A subgroup analysis compared patients diagnosed with COVID-19 to patients without COVID-19. This subgroup contained 780,329 patient encounters and we controlled for age, ESI, race, sex, insurance, ICU admission, ED boarding, COVID-19 diagnosis and whether patients were seen at a freestanding or hospital-based ED. Demographic data for this subgroup is reported in Table 2 . Patients diagnosed with COVID-19 had lower initial ESI triage score for both high acuity (26.86% v 14.42%, p < 0.0001) and moderate acuity (67.19% v 61.07%, p < 0.001). Patients diagnosed with COVID-19 had a longer ED length of stay (95%CI 11.77 (9.41–14.12)) and were more likely to be boarded in the ED (95%CI 1.68 (1.63–1.73)). Patients diagnosed with COVID-19 were more likely to be admitted to the hospital (95%CI 2.81 (2.73–2.91)), more likely to be admitted to the ICU (95%CI 2.29 (2.19–2.39)), and had a longer hospital length of stay (95%CI 2.32 (2.19–2.45)). Patients diagnosed with COVID-19 had a significantly increased likelihood of in-hospital mortality compared to non-COVID-19 patients (95%CI 3.30 (3.03–3.59)).
Table 2.
Demographic and other Characteristics of participants During C0VID-19 pandemic, N = 780,329.
| Variable | Overall | COVID-19 N = 21,934 |
Non-COVID-19 N = 758,395 |
p-value |
|---|---|---|---|---|
| Age | 46.94(23.48) | 56.51(20.15) | 46.67(23.51) | <0.0001 |
| Gender |
<0.0001 |
|||
| Female | 434,832 (55.72) | 11,855(54.05) | 422,977(55.77) | |
| Male | 345,497 (44.28) | 10,079(45.95) | 335,418(44.23) | |
| Race |
<0.0001 |
|||
| Black | 263,822 (33.81) | 7181(32.74) | 256,641(33.84) | |
| White | 467,893 (59.96) | 13,214(60.24) | 454,679(59.95) | |
| Other | 48,614 (6.23) | 1539(7.02) | 47,075(6.21) | |
| Ethnicity |
<0.0001 |
|||
| Hispanic | 31,509 (4.04) | 966(4.40) | 30,543(4.03) | |
| Not Hispanic | 748,820 (95.96) | 20,968(95.60) | 727,852(95.97) | |
| Payor |
<0.0001 |
|||
| Medicaid | 275,731 (35.34) | 4717(21.51) | 271,014(35.74) | |
| Medicare | 206,912 (26.52) | 7690(35.06) | 199,222(26.27) | |
| Private | 297,686 (38.15) | 9527(43.43) | 288,159(38.00) | |
| ESI Level |
<0.0001 |
|||
| High | 115,251 (14.77) | 5892(26.86) | 109,359(14.42) | |
| Mod | 477,906 (61.24) | 14,737(67.19) | 463,169(61.07) | |
| low | 187,172 (23.99) | 1305(5.95) | 185,867(24.51) | |
| Mortality |
<0.0001 |
|||
| No | 776,066(99.45) | 21,104(96.22) | 754,962(99.55) | |
| Yes | 4263(0.55) | 830(3.78) | 3433(0.45) | |
| ED LOS(minutes) | 169.0(96.0–265.0) | 233.0(165.0–321.0) | 167.0(94.0–263.0) | <0.0001 |
| Hospital LOS (days) | 3.98(2.19–6.85) | 5.40(3.37–9.8) | 3.90(2.15–6.64) | <0.0001 |
| ICU |
<0.0001 |
|||
| No | 745,373 (95.52) | 18,850(85.94) | 726,523(95.80) | |
| Yes | 34,956 (4.48) | 3084(14.06) | 31,872(4.20) | |
| Boarded |
<0.0001 |
|||
| No | 590,135 (75.63) | 11,851(54.03) | 578,284(76.25) | |
| yes | 190,194 (24.37) | 10,083(45.97) | 180,111(23.75) | |
| ADMISSION |
<0.0001 |
|||
| No | 631,162 (80.88) | 11,568(52.74) | 619,594(81.70) | |
| Yes | 149,167 (19.12) | 10,366(47.26) | 138,801(18.30) | |
| Department Group |
<0.0001 |
|||
| FSED | 129,523 (16.60) | 2286(10.42) | 127,237(16.78) | |
| HBED | 650,806 (83.40) | 19,648(89.58) | 631,158(83.22) | |
| Department Type |
<0.0001 |
|||
| Academic | 437,881 (56.11) | 13,435(61.25) | 424,446(55.97) | |
| Community | 342,448 (43.89) | 8499(38.75) | 333,949(44.03) |
Statistics presented as mean (SD), or Median (Q1 – Q3), or n (%).
4. Discussion
This study aimed to quantify the impact the COVID-19 pandemic had on ED boarding and in-hospital mortality. We found an overall 22% increase in patients boarding in the EDs within a large integrated healthcare system. Concurrently, in-hospital mortality for patients increased by 16% during the COVID-19 pandemic. Prior studies have shown that an increase in ED boarding directly correlates to patient morbidity and mortality [[11], [12], [13],15]. Based on the previous literature, there is a potential correlation between increased ED boarding and in-hospital mortality. The increase in mortality could have also been secondary to an increase in deaths attributed to COVID-19. However, future studies evaluating this correlation would be warranted.
We also found an increase in high (ESI level 1 or 2) and moderate (ESI level 3) acuity level patients who presented to the ED. These findings are supported by a previous study which showed that early in the pandemic, an increase for high and moderate acuity presentations with a concomitant decrease for low acuity presentations [8].
Our results showed an overall increase in patients admitted to the hospital during the COVID -19 pandemic compared to pre-COVID-19. Early in the COVID-19 pandemic, studies revealed an initial decrease in patient volume and hospital admissions [2,4,[7], [8], [9]]. However, our study time frame included both the initial lockdown and post-lockdown period of the pandemic in our region. These results highlight a more comprehensive view of the impact that the COVID-19 pandemic had on hospital admission rates.
Our subgroup analysis of COVID-19 patients vs. non-COVID-19 patients showed that COVID-19 patients were more likely to die in the hospital, have a longer ED and hospital length of stay, and were more likely to be boarded in the ED. In addition, COVID-19 patients were more likely to be admitted to the hospital and the ICU than patients without COVID-19. These results show that COVID-19 patients were more likely to impact key ED and hospital metrics. These results can further help the medical community understand how and where a pandemic can impact a healthcare system.
This study has several limitations, including those inherent to all retrospective studies. First, this study is limited because, since the study's timeframe, additional variants of COVID-19 have occurred. Also, because the study includes the first 18 months of the pandemic, the impact of the pandemic post-lockdown may be more significant than we identified. Our healthcare system saw the same decreased volume and admissions trend during that time. Second, this study evaluated patients in a large integrated regional healthcare system which may limit its generalizability. However, this system covers urban and rural areas and includes academic, community, and critical access ED settings. As a result, the system serves a diverse patient population. Finally, we did not include the cause of death, as this was outside the project's scope. Future studies should be considered evaluating the cause of inpatient death during the pandemic.
5. Conclusion
During the COVID-19 pandemic, ED boarding and in-patient mortality increased. The COVID-19 pandemic also increased moderate, and high acuity patient encounters with an increased percentage of patients admitted to the hospital. In addition, COVID-19-positive patients were more likely to be boarded and admitted, had longer ED and hospital LOS, and had an increased likelihood of ICU admission and in-hospital mortality.
Prior presentations
Society for Academic Emergency Medicine 2022; Cleveland Clinic Akron General Post Graduate Research Day 2022.
CRediT authorship contribution statement
Gregory Griffin: Writing – original draft, Methodology, Investigation, Conceptualization. Jessica Krizo: Writing – review & editing, Project administration, Methodology. Caroline Mangira: Writing – original draft, Software, Methodology, Formal analysis, Data curation. Erin L. Simon: Writing – review & editing, Supervision, Project administration, Methodology, Investigation, Data curation, Conceptualization.
Declaration of Competing Interest
The authors have no conflicts of interest.
References
- 1.NVSS - Provisional Death Counts for COVID-19 - Executive Summary https://www.cdc.gov/nchs/Covid19/mortality-overview.htm Published April 23, 2021. Accessed August 25, 2021.
- 2.Nourazari S., Davis S.R., Granovsky R., et al. Decreased hospital admissions through emergency departments during the COVID-19 pandemic. Am J Emerg Med. 2021;42:203–210. doi: 10.1016/j.ajem.2020.11.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cohen B.A., Wessling E.G., Serina P.T., et al. Emergency department operations in a large health system during COVID-19. Am J Emerg Med. 2021;41:241–243. doi: 10.1016/j.ajem.2020.05.097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gormeli Kurt N., Gunes C. How has Covid-19 pandemic affected crowded emergency services? Int J Clin Pract. 2020;74(12) doi: 10.1111/ijcp.13624. [DOI] [PubMed] [Google Scholar]
- 5.Reschen M.E., Bowen J., Novak A., et al. impact of the COVID-19 pandemic on emergency department attendances and acute medical admissions. BMC Emerg Med. 2021;21(1):143. doi: 10.1186/s12873-021-00529-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Barten D.G., Latten G.H.P., van Osch F.H.M. Reduced emergency department utilization during the early Phase of the COVID-19 pandemic: Viral fear or lockdown effect? Disaster Med Public Health Prep. 2020:1–4. doi: 10.1017/dmp.2020.303. Published online August 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rennert-May E., Leal J., Thanh N.X., et al. The impact of COVID-19 on hospital admissions and emergency department visits: A population-based study. PLoS One. 2021;16(6) doi: 10.1371/journal.pone.0252441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Alharthi S., Al-Moteri M., Plummer V., Al Thobiaty A. The impact of COVID-19 on the service of emergency department. Healthcare. 2021;9(10):1295. doi: 10.3390/healthcare9101295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Boserup B., McKenney M., Elkbuli A. The impact of the COVID-19 pandemic on emergency department visits and patient safety in the United States. Am J Emerg Med. 2020;38(9):1732–1736. doi: 10.1016/j.ajem.2020.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Birkmeyer J.D., Barnato A., Birkmeyer N., Bessler R., Skinner J. The impact Of The COVID-19 pandemic on hospital admissions in the United States. Health Aff (Millwood) 2020;39(11):2010–2017. doi: 10.1377/hlthaff.2020.00980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Singer A.J., Thode H.C., Viccellio P., Pines J.M. The association between length of emergency department boarding and mortality. Acad Emerg Med Off J Soc Acad Emerg Med. 2011;18(12):1324–1329. doi: 10.1111/j.1553-2712.2011.01236.x. [DOI] [PubMed] [Google Scholar]
- 12.Bernstein S.L., Aronsky D., Duseja R., et al. The effect of emergency department crowding on clinically oriented outcomes. Acad Emerg Med. 2009;16(1):1–10. doi: 10.1111/j.1553-2712.2008.00295.x. [DOI] [PubMed] [Google Scholar]
- 13.Carter E.J., Pouch S.M., Larson E.L. The relationship between emergency department crowding and patient outcomes: A systematic review. J Nurs Scholarsh. 2014;46(2):106–115. doi: 10.1111/jnu.12055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lucero A., Sokol K., Hyun J., et al. Worsening of emergency department length of stay during the COVID-19 pandemic. J Am Coll Emerg Physicians Open. 2021;2(3) doi: 10.1002/emp2.12489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chalfin D.B., Trzeciak S., Likourezos A., Baumann B.M., Dellinger R.P. Group for the DE study. Impact of delayed transfer of critically ill patients from the emergency department to the intensive care unit*. Crit Care Med. 2007;35(6):1477–1483. doi: 10.1097/01.CCM.0000266585.74905.5A. [DOI] [PubMed] [Google Scholar]