Abstract
Background
The rates of mental health disorders such as anxiety and depression are at an all-time high especially since the onset of COVID-19, and the need for readily available digital health care solutions has never been greater. Wearable devices have increasingly incorporated sensors that were previously reserved for hospital settings. The availability of wearable device features that address anxiety and depression is still in its infancy, but consumers will soon have the potential to self-monitor moods and behaviors using everyday commercially-available devices.
Objective
This study aims to explore the features of wearable devices that can be used for monitoring anxiety and depression.
Methods
Six bibliographic databases, including MEDLINE, EMBASE, PsycINFO, IEEE Xplore, ACM Digital Library, and Google Scholar were used as search engines for this review. Two independent reviewers performed study selection and data extraction, while two other reviewers justified the cross-checking of extracted data. A narrative approach for synthesizing the data was utilized.
Results
From 2408 initial results, 58 studies were assessed and highlighted according to our inclusion criteria. Wrist-worn devices were identified in the bulk of our studies (n = 42 or 71%). For the identification of anxiety and depression, we reported 26 methods for assessing mood, with the State-Trait Anxiety Inventory being the joint most common along with the Diagnostic and Statistical Manual of Mental Disorders (n = 8 or 14%). Finally, n = 26 or 46% of studies highlighted the smartphone as a wearable device host device.
Conclusion
The emergence of affordable, consumer-grade biosensors offers the potential for new approaches to support mental health therapies for illnesses such as anxiety and depression. We believe that purposefully-designed wearable devices that combine the expertise of technologists and clinical experts can play a key role in self-care monitoring and diagnosis.
Keywords: Anxiety, Depression, Mental health, Wearable devices, Digital mental health, Self-care
1. Introduction
1.1. Background
Globally, “common mental illnesses” such as anxiety and depression are widespread. The lifetime prevalence of depression varies by culture and is as much as 20% in countries such as the United States [1,2]. Not only do depression and anxiety have a significant economic impact on society [3], but they also significantly impact individuals in terms of lost years due to ill health. Disability-adjusted life years for mental illness are comparable to those for cardiovascular and circulatory illnesses. The proportion of Years Lived with Disability for mental health problems is significant, at 32.4% globally [4]. Not only is depression a major risk factor for suicide [5], those affected tend to have a shorter lifespan due to health issues correlated to their mental status [6]. The global figures for anxiety are also unfavorable, with 3.76% of the world population reported to have suffered from an anxiety disorder; the figures have remained unchanged since 1990 [7].
Recent studies have looked at self-care mobile applications (apps) [8], considered a vital tool for giving patients the feeling of autonomy for self-regulating their health needs. However, few reviews exist on the technical solutions linked to mobile apps. In this study, we focus on a large class of such solutions, namely on publicly available wearable devices and their tools to monitor, detect, diagnose, or manage mental health [9]. Wearable devices, such as smart watches and wrist bands, have given rise to wearable devices becoming influential technologies. They affect our decisions and behaviors in much the same way that mobile apps have in the domain of mental health [10], albeit in comparison, wearable devices are still in their infancy. Integrating sensors into wearable devices has enhanced their monitoring capabilities to a level that was previously reserved to hospital settings. While wearable device technologies have long been used in health interventions in clinical settings with promising results [11], the ease and accessibility of consumer-level devices containing such integrated sensors, be it in clothes or other accessories, could further democratize their use and might provide health benefits to users suffering from anxiety and depression. At the same time, that democratization is raising questions about the appropriate limits of data use in the provision of care through wearables [12].
1.2. Research problem and aim
With a growing emphasis on alleviating the onerous symptoms of mental health disorders—particularly those that have been exacerbated by the global response to COVID-19—the necessity for a review that can enlighten individuals looking for easily available mental health-focused wearable devices has never been greater. As this field is fast evolving, wearable devices require the same quality reviews previously published on app features [13], both to enable consumers to make informed decisions and the research community to identify gaps and opportunities. The authors aim to explore features of publicly available WD technologies within the domain of anxiety and depression. Many studies have been conducted about WDs but to the best of our knowledge this is the first scoping review (overview of the available research evidence) looking at WDs and their use with anxiety and depression. We hope to provide researchers with some extra insight of this emerging field. Our review assesses information and could form a pre-cursor for a future systematic review.
2. Methods
This scoping review was carried out to satisfy the study's goals of exploring features of wearable devices for anxiety and depression. The PRISMA Extension for Scoping Reviews (PRISMA-ScR) [14] was utilized as a guiding approach to construct a complete scoping review.
2.1. Search strategy
2.1.1. Search sources
Searches for this study were executed in the following bibliographic databases: MEDLINE, EMBASE, PsycINFO, IEEE Xplore, ACM Digital Library, and Google Scholar.
Bibliographic collection took place from July 10th to July 12th, 2021. Because Google Scholar typically returns several hundred items sorted by relevance to the search topic, only the first 100 hits were scanned. The reference lists of the included studies and reviews were also screened to look for other publications relevant to the review. Additionally, relevant papers that cited the included studies were located by using Google Scholar's "cited by" tool (forward reference list checking).
2.1.2. Search terms
For the present study, two sets of keywords were designed to search databases. We considered the subject terms included in the databases to complete our search queries. We combined four keywords describing the relevant population (anxiety, depression, depressed, and anxious) with each relevant intervention (wearable*, smart*). For example, the following search term was applied in Google Scholar: (“Wearable*” OR “smart*” OR “Wearable device*”) AND (“anxiety*” OR “depression” OR “depressive*” OR “depression*” OR “anxious*”).
2.2. Study eligibility criteria
Studies were chosen based on the criteria in Table 1 . Only peer-reviewed articles, conference proceedings (not abstracts), and reports were considered. In addition, only studies published in English and during the last ten years were included in this study. Dissertations, theses, conference abstracts (not proceedings), proposals, and editorials were not accepted.
Table 1.
Inclusion and exclusion criteria.
| Criteria | Specified criteria |
|---|---|
| Inclusion | • Any wearable technology or approaches used for anxiety and depression for any purpose such as: screening, diagnosis, treatment, monitoring, tracking, etc. |
| • Publicly available, consumer-grade devices (e.g., wrist band, glasses, clothes etc.) | |
| • Studies published between 2010 and 2021 | |
| • Peer-reviewed articles, theses, conference proceedings, and reports | |
| • English articles | |
| Exclusion | • Proposed new devices not currently on the market |
| • Sensors or tracking devices infused inside a person's body | |
| • Wearable devices that need professional or hospital settings | |
| • Reviews, conference abstracts, dissertations, proposals, editorials, commentaries |
Only studies that addressed publicly available wearable devices used for anxiety and depression purposes that did not require a hospital setting were included.
2.3. Study selection
The studies for this review were chosen in two stages. Two reviewers independently reviewed the titles and abstracts of all retrieved papers in the first stage. In the second phase, the same reviewers read the complete texts of the papers included in the first step separately. If there were any disputes between the two reviewers, these were settled by consulting a third reviewer, both during the first and second steps of the selection process.
2.4. Data extraction and data synthesis
The included studies were screened in two phases by four reviewers. As indicated in Multi-media Appendix B, two reviewers created the data extraction form. Two additional reviewers independently undertook the data extraction procedure, and any differences were addressed by the third reviewer. The first reviewers synthesized relevant extracted study data from the Microsoft Excel data extraction sheet. To synthesize the collected data from the included research, the narrative technique was used. Narrative research is a broad term encompassing a variety of approaches that rely on people's written or spoken words, as well as their visual representations [14].
3. Results
3.1. Search results
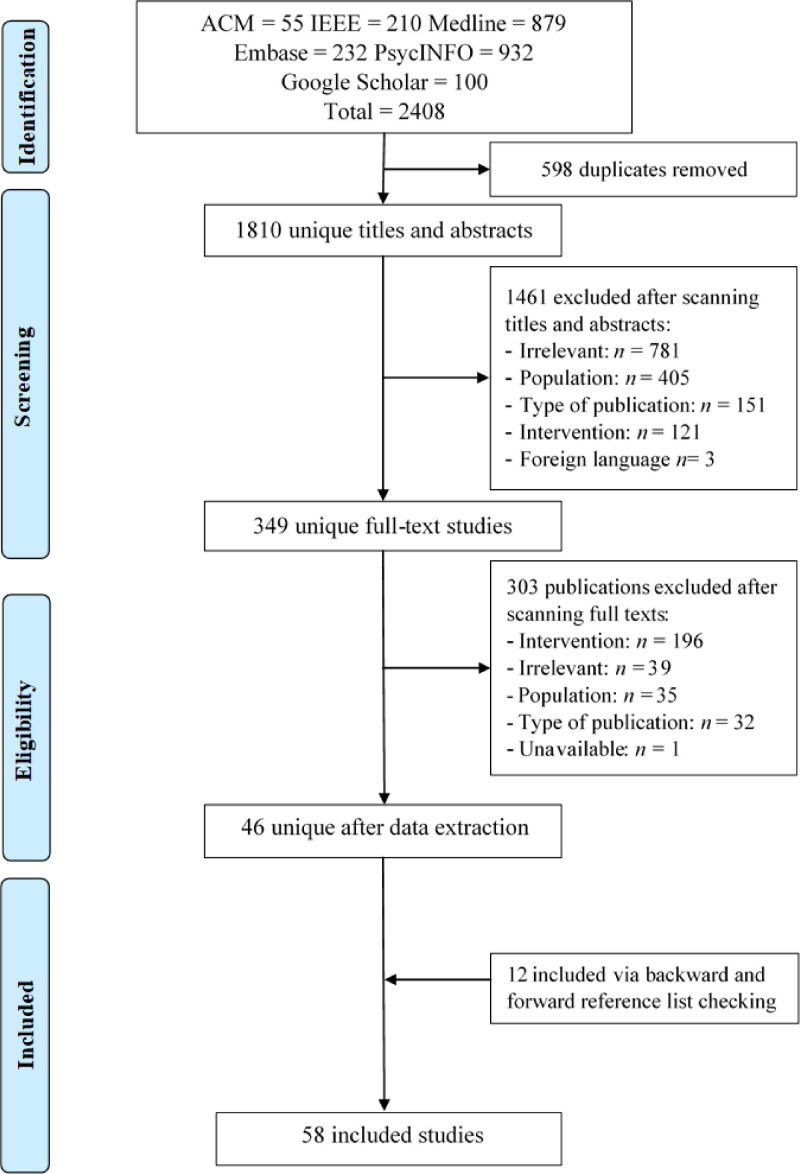
The search of six bibliographic databases yielded 2408 citations. As shown in Fig. 1 , 598 duplicates were excluded, leaving 1810 unique titles and abstracts. Of those, 1461 citations were further excluded after screening their titles and abstracts. Of the remaining 349 references, 303 publications were excluded during the full text screening. Finally, 46 unique individual studies were identified. Backward reference list checking and forward reference list checking yielded 12 new studies. The synthesis includes a total of 58 articles.
Fig. 1.
Flowchart of the study selection process.
3.2. General description of included studies
As presented in Table 2 , most published studies were journal articles (71%), and less than one-third were conference articles (29%). Although studies were published in more than 17 countries, about 23.7% of the included studies were published in the USA. More than half of the studies were published between 2016 and 2021 (51%).
Table 2.
General characteristics of included studies.
| Characteristics | Number of studies | Studies (see Appendix A) |
|---|---|---|
| Year of publication | 2021: 9 | S14, S15, S30, S32, S36, S39, S42, S45, S47 |
| 2020: 9 | S12, S19, S25, S26, S29, S34, S38, S49, S57 | |
| 2019: 8 | S1, S11, S17, S21, S41, S43, S48, S58 | |
| 2018: 8 | S8, S24, S28, S31, S37, S40, S52, S54 | |
| 2017: 11 | S2, S4, S6, S9, S10, S22, S35, S50, S51, S55, S56 | |
| 2016: 4 | S16, S18, S23, S46 | |
| 2015: 5 | S3, S5, S27, S44, S53 | |
| 2014: 1 | S7 | |
| 2012: 1 | S20 | |
| 2011: 1 | S33 | |
| 2010: 1 | S13 | |
| Country | USA: 24 | S1, S3, S9, S13, S14, S18, S22, S26, S27, S28, S29, S31, S32, S34, S35, S36, S37, S40, S41, S47, S48, S50, S52, S54 |
| UK: 6 | S2, S10, S42, S43, S51, S58 | |
| Germany: 4 | S15, S16, S23, S45 | |
| Japan: 4 | S6, S25, S38, S53 | |
| Canada:2 | S4, S24 | |
| China: 3 | S12, S55, S56 | |
| Australia:2 | S11, S57 | |
| Korea: 2 | S17, S49 | |
| Austria: 2 | S7, S8, | |
| Ireland: 2 | S30, S46 | |
| Brazil: 1 | S19 | |
| Finland: 1 | S39 | |
| Norway:1 | S5 | |
| Italy:1 | S21 | |
| Netherland: 1 | S44 | |
| Switzerland: 1 | S33 | |
| Mexico: 1 | S20 | |
| Type of publication | Journal article: 41 | S1, S2, S4, S5, S6, S7, S8, S9, S11, S12, S13, S14, S15, S17, S18, S19, S20, S21, S24, S25, S26, S27, S28, S29, S30, S32, S33, S34, S36, S39, S41, S42, S43, S44, S45, S46, S49, S51, S54, S57, S58 |
| Conference:17 | S3, S10, S16, S22, S23, S31, S35, S37, S38, S40, S47, S48, S50, S52, S53, S55, S56 | |
| Wearable Device Type | Smart band: 19 | S2, S11, S18, S19, S25, S26, S27, S28, S31, S34, S35, S38, S42, S43, S48, S50, S51, S52, S57 |
| Smart watch: 17 | S4, S8, S12, S15, S16, S17, S22, S23, S26, S30, S32, S36, S37, S49, S55, S56, S58 | |
| Actigraphy: 8 | S5, S6, S7, S9, S13, S20, S33, S44 | |
| Smart glass: 4 | S8, S9, S21, S45 | |
| Smart Belt:3 | S40, S41, S54 | |
| Smart shirt:2 | S1, S10 | |
| Smart necklace: 2 | S14, S47 | |
| smart clip: 2 | S24, S29 | |
| Smart Ring: 1 | S39 | |
| Human Performance electrodes Device: 1 | S3 | |
| Skin conductance biofeedback device:1 | S46 | |
| Wearable near-infrared spectroscopy (NIRS): 1 | S53 | |
| Placement of wearable device | Wrist: 42 | S1, S2, S4, S5, S7, S9, S11, S12, S13, S15, S16, S17, S18, S19, S20, S22, S23, S25, S26, S27, S28, S30, S31, S32, S33, S34, S35, S36, S37, S38, S42, S43, S44, S48, S49, S50, S51, S52, S55, S56, S57, S58 |
| Waist: 5 | S6, S28, S40, S41, S54 | |
| Head: 5 | S8, S9, S21, S45, S53 | |
| Chest:2 | S3, S26 | |
| Suit: 2 | S1, S10 | |
| Neck: 2 | S14, S47 | |
| Finger: 2 | S39, S46 | |
| Anywhere: 2 | S24, S29 | |
| Mood assessed methods | State-Trait Anxiety Inventory: 8 | S12, S21, S23, S26, S48, S51, S55, S56 |
| Diagnostic and Statistical Manual of Mental Disorders (DSM): 8 | S3, S7, S8, S20, S32, S40, S41, S54 | |
| Hamilton Depression Rating Scale (HAM-D): 6 | S6, S7, S9, S25, S33, S34 | |
| Patient Health Questionnaire (PHQ): 6 | S30, S36, S42, S49, S52, S58 | |
| Online interview or survey: 5 | S1, S11, S15, S24, S27 | |
| Montgomery-Asberg depression rating scale (MADRS): 4 | ||
| Depression, Anxiety and Stress Scale (DASS):3 | S20, S25, S44, S57 | |
| NA: 3 | S16, S18, S39 | |
| Ecological Momentary Assessment (EMA): 2 | S10, S22, S47 | |
| Gamification: 2 | S17, S49 | |
| Profile of Mood States (POMS): 2 | S19, S46 | |
| Generalised Anxiety Disorder questionnaire (GAD): 2 | S28, S53 | |
| Beck's Depression Inventory (BDI): 2 | S30, S43 | |
| Center for Epidemiologic Studies Depression scale (CES-D): 1 | S4, S21, | |
| Depression and Anxiety Mood Scale (DAMS): 1 | S14 | |
| Activities of daily living (ADL): 1 | S38 | |
| Clinical Global Impression (CGI): 1 | S2 | |
| Heart Rate Variability (HRV): 1 | S57 | |
| Mood & Anxiety Symptoms Questionnaire (MASQ): 1 | S50 | |
| Positive and Negative Syndrome Scale (PANSS): 1 | S29 | |
| Positive and Negative Affect Schedule (PANAS): 1 | S5 | |
| moderate-to-vigorous physical activity (MVPA):1 | S35 | |
| Quick Inventory of Depressive Symptomatology (QIDS): 1 | S28 | |
| Social Interaction Anxiety Scale (SIAS):1 | S31 | |
| Symptomatic Organic Mental Disorder Assessment Scale (SOMAS):1 | S37 | |
| The UWIST Mood Adjective Checklist: 1 | S5 | |
| S46 | ||
| Mental disorder | Depression: 27 | S2, S4, S5, S6, S7, S8, S9, S13, S14, S17, S20, S24, S25, S30, S31, S32, S33, S34, S35, S36, S42, S44, S49, S52, S53, S57, S58 |
| Anxiety: 15 | S1, S10, S11, S15, S22, S23, S26, S37, S45, S46, S47, S48, S51, S55, S56 | |
| Depression & Anxiety: 16 | S3, S12, S16, S18, S19, S21, S27, S28, S29, S38, S39, S40, S41, S43, S50, S54 |
3.3. Features of wearable devices
A smart band was utilized in 32% of the studies, and a smartwatch in 29% of the studies. The actigraphy brand is the most commonly available commercial brand used by 15% of the studies. Only 7% of the studies utilized smart glasses. Smart belts, smart necklaces, and smart clips were only used by 3% of the studies. Other uncommon devices were described only once, such as a smart ring, human performance electrodes device, skin conductance biofeedback device, and a wearable near-infrared spectroscopy (NIRS).
The included studies show a clear dominance of wrist-worn devices (71%) over devices worn across the rest of the body or attire: waist (n = 5), head (n = 5), chest (n = 2), suit (n = 2), neck (n = 2), finger (n = 2), or elsewhere (n = 2) together make up the remaining 20%. Note that numbers do not add up since four references (S1, S9, S26, S29) describe the use of multiple devices.
Table 2 also presents the 26-moods assessment methods discussed by included studies for identification of anxiety and depression. The most common methods were State-Trait Anxiety Inventory (14%) and Diagnostic and Statistical Manual of Mental Disorders (14%). The mental health illness most targeted by wearable devices in the included studies is depression (47%), whereas anxiety was only assessed in 25% of studies. More than a quarter (27%) of the included studies assessed both mental illnesses.
3.4. Technical device operation details and evaluation
Among the 58 studies, Table 3 highlights that Fitbit (16%) is the most common wearable device technology brand producer, followed by Actiwatch and Empatica (12%). Five different host devices were identified that were used as a gateway for collected data storage or further processing. Amongst them, smartphones (45%) are the most frequent devices, followed by computers (10%), and online websites (3%), whereas 34% did not use any host terminal. The most used operating systems in wearable devices are Android (5%) and iOS (5%). Other studies supported both of these OSes (17%), though the majority of studies (72%) did not specify the compatible operating system, leading us to speculate that they may be compatible with both systems, as Android and iOS together represent more than 99% market share as of this writing [15]. The most prevalent data transfer mode between wearable and host devices was Bluetooth (22%), followed by internet technology (19%) in the form of WiFi or cellular data. Few devices made use of removable media (9%) such as memory cards, whereas a single (n = 1) study used wired connections.
Table 3.
Technical device operation details.
| Characteristics | Number of studies | Study ID |
|---|---|---|
| Device Technology brands | Fitbit: 9 | S1,S4,S11,S24,S27,S31,S38,S42,S43 |
| ActiWatch: 7 | S5,S7,S13,S15,S17,S20,S33 | |
| Empatica: 7 | S18,S26,S34,S35,S47,S48,S50 | |
| Apple watch:3 | S11,S30,S58 | |
| Proposed watches using ARM Cortex:3 | S12,S22,S23 | |
| Acti Graph:2 | S28,S32 | |
| 3-space sensor:2 | S40,S41 | |
| Estera Corporation:1 | S6 | |
| Microsoft band:2 | S37,S52 | |
| Re-Timer and Actiware:2 | S8,S9 | |
| Others:22 | ||
| N/A:3 | S3, S6,S14,S16,S19,S21,S25,S29, | |
| S36,S39,S44,S45,S46,S49,S51,S53-S55,S57 | ||
| S2,S10,S56 | ||
| Host device | Smartphone: 26 | S1,S3,S11,S16,S19,S21,S25-S31,S34-S39,S43,S45,S46,S49,S51,S52,S56,S58 |
| Computer: 6 | S7,S12,S13,S23,S33,S47 | |
| Online database: 2 | S4, S24 | |
| Stored locally in the flash memory: 1 | S50 | |
| N/A: 20 | S2,S5-S6,S8-S10,S14,S15,S17,S20,S22,S32,S40-S42,S44,S48,S53-S55,S57 | |
| Operating systems compatible with | Android: 3 | S35, S36, S44 |
| iOS: 3 | S31,S40,S59 | |
| Android and iOS: 10 | S3,S16,S19,S27,S31,S36,S52,S49, S55,S56 | |
| N/A: 42 | S2,S4-S15,S17,S18,S20-S26,S28, S29,S32,S33,S37,S38,S40,S41,S42, S44-S48,S50,S51,S53,S54,S57 | |
| Mode of Data transfer | Bluetooth: 14 | S3,S18,S19,S23,S25,S27,S28,S36, S43,S46,S47, S49,S51,S52 |
| Internet (WiFi, Mobile data; optionally combined with cloud storage): 11 | S4,S16,S24,S31,S34,S35,S37,S39, S45,S47,S58 | |
| Removable media: 5 | S7,S10,S13,S26,S33 | |
| Wired:1 | S53 | |
| N/A: 27 | S1,S2,S5,S6,S8,S9,S11,S12,S14, S15,S17,S20,S21,S29,S30,S32,S38,S40-S42,S44,S48,S50,S54,S55-S57 | |
| Effectiveness measure | Statistical methods/measures: 40 | S1,S2,S4,S5,S10,S12,S13,S14,S17,S18, S20,S21,S23,S25,S26,S28,S29,S32-S36,S38,S40-S42,S44-S46,S48,S49,S51,S52,S54-S58 |
| Pre-post testing: 2 | S6,S53 | |
| User Interviews:1 | S16 | |
| Technology Acceptance Model: 1 | S19 | |
| N/A: 14 | S3,S8,S9,S11,S15,S22,S24,S27,S30, S37,S39,S43,S47,S50 | |
| Number of Participants | 0–49: 29 | S3,S4,S6,S7-S10,S14,S16-S20,S24,S27,S28,S35-S37,S44,S45,S48-S51,S53,S56-S58 |
| 50–99:20 | S5,S12,S13,S21-S23,S25,S26,S30,S32-S34,S38-S41,S46,S52,S54,S55 | |
| 100–300:6 | S1,S2,S11,S15,S29,S31 | |
| above 300:2 | S42,S43 | |
| closed laboratory setting:1 | S47 | |
| Study experimentation duration | <=1 day: 4 | S5,S33,S46,S51 |
| <=1 week:8 | S2,S25,S31-S32,S44,S52,S53,S57 | |
| <=1 month:15 | S3,S6,S7,S13,S17,S19,S27-S29,S36-S39,S49,S50 | |
| <=1 year:15 | S1,S4,S8,S9,S11,S14,S18,S20,S24, S30,S34,S35,S41,S54,S58 | |
| Above 1 year:3 | S15,S42,S43 | |
| N/A:13 | S10,S12,S16,S21-S23,S26,S40,S45,S47,S48,S55,S56 |
Studies performed experiments on these wearable devices using small sets of participants mostly below age 50 (50%) and were carried out for months (26%).
Various methods were used to measure the effectiveness of wearable devices for assessments of anxiety and depression. Among those, statistical methods (69%) were most used. Such methods mainly constitute tests such as Pearson's and Spearman correlation coefficient, p-value, F1 score, accuracy, and the ANOVA test, along with many others. Pre-/post testing (3%), user interviews and a Technology Acceptance Model were also used by single studies.
4. Discussion
4.1. Principal findings
Considering that the Fitbit (released in 2009) and the Apple Watch (released in 2015) were seminal products that paved the way for early wearable devices, it is hardly surprising that most of the devices used by the studies are wrist-worn. We believe that their resemblance to wrist watches lends legibility to such devices and allows users to check them frequently and discretely. Furthermore, most of the recent studies (e.g., 5 years) report the use of connected devices, for example connected via WiFi or Bluetooth to a host smartphone. Among the many likely reasons for this trend are (a) a decline in price for mobile online data, (b) ever more energy-efficient local connectivity technology, such as Bluetooth Low Energy, (c) the opportunity to “outsource” more complex tasks to considerably more powerful host devices, thereby extending battery life on the wearable device, (d) the convenience of being able to explore one's data on bigger screens or across device boundaries (“cloud storage”), and (e) the pervasiveness of mobile devices. However, whereas a modern lifestyle seems to drive the development of technology that supports personal fitness (e.g., Fitbit and the many apps that track one's personal fitness status, including vitals such as heart rate or body temperature), most devices used in studies are purpose-shifted, that is, they are used outside of their original purpose for the benefit of mental health applications. We believe that the effectiveness of such purpose-shifted devices deserves more scrutiny, possibly in the form of a separate, systematic review, although another possible explanation is that regular exercise may be associated with some improvement in mental well-being. [16,17].
We see the main potential of wearable devices being their ability to track or infer habits, such as work-rest balances and exercise levels, from various biosensors, potentially allowing medical experts (or software expert systems) to infer the user's mood or therapeutical progress. It is particularly useful that relevant data can be gathered from more data points during the day than with traditional hospital visits. This may, soon, prove itself to be the enabling technology behind mental health-targeting software becoming increasingly augmented by additional biosensors. Consequently, purposefully wearable devices that target mental health issues designed in collaboration between technologists and clinical experts could add substantial (self-)diagnostic and therapeutic value.
However, we must note that most of the studies are either woefully short (n = 27, less than a month) or underpopulated (n = 29, less than 50 participants). Only two of the studies (S42, S43) recruited a population of over 300 participants and lasted more than a year. In the context of mental health disorders, it is important to note that improvement often comes gradually and requires expert intervention for several months (e.g., cognitive behavioral therapy (CBT) to treat anxiety typically involves a meeting with a therapist for 1 h per week for 3—4 months, according to the UK's National Health Service [18]. Further, for some mental health disorders, the positive effects of CBT may require years of follow-up treatment to be maintained [19].
4.2. Strengths
The review has been reported according to the PRISMA Extension for Scoping Reviews; therefore, it can be considered a review of good quality. Furthermore, this study is the first review in the literature that has focused on wearable devices targeting anxiety and depression. Thus, this study could assist readers with making decisions about the best wearable devices to use in the current market, and could highlight gaps to the research community and to technology hardware and software developers (e.g., the need for larger and longer systematic studies).
The most popular databases in both the healthcare and information technology fields were searched to retrieve as many relevant studies as possible. The authors searched Google Scholar and conducted backward and forward reference list checking to identify gray literature, reducing the risk of publication bias. All studies included in this review were from peer-reviewed journals.
4.3. Limitations
Some limitations are that only English studies were included, and that only studies published between 2010 and 2021 were included, by the time the study had gone through the review process and published no doubt in this fast paced and rapidly changing field it is not farfetched to expect yearly updates for this review. Due to practical restrictions (e.g., accessing Web of Science and Scopus), we may have overlooked some pertinent research papers. In addition, the databases were searched using only the terms "wearable*, smart*" for this study. We only included studies that utilized commercial wearable devices that require no clinical setting. Therefore, other kinds of wearable devices, such as EEG and ECG, were excluded. Finally, this is a scoping review that does not critically assess the quality of the included studies. Although the different wearable device technologies were examined, the review falls short of reporting the effectiveness measure values, and therefore does not assess performance. The latter goes beyond the scope of a scoping review and would be more suited to a full systematic review article. We hope a systematic review shall follow.
4.4. Practical and research implications
The emergence of wearable devices and their integration with smart devices such as mobile phones, paired with the ease and style in which wearable devices can be worn in the form of wrist bands and watches, highlights that wearable devices have gained wide acceptance. What makes them appealing to mental health applications is that they can be equipped with a multitude of biosensors that measure vitals and bio-signals casually and at the user's leisure. As a result, it has never been easier to gather data on patients’ habits, moods, etc. Given today's increasing popularity of purpose shifted wearable devices to counteract anxiety and depression (e.g., exercise trackers), it is likely that a boom of purposefully designed wearable devices in mental health is imminent. This assessment is supported by the acceptance and success of wearable devices in general health care in the last decade (e.g., heart rate monitors, body temperature scanners, respiratory monitors, blood sugar monitors, etc.). Especially in the domain of self-care, wearable devices paired with smart devices could allow users access to early-onset diagnostic tools to monitor habits and mood, recommend unsupervised therapy, or instigate referrals to therapeutic experts. This review outlined the significance of such devices in anxiety and depression. Just as mobile apps for mental health have become more prominent in the past decade, purpose shifted wearable devices can be predicted to make tremendous leaps in the coming years. In particular, the setting of wearable devices in an Internet-of-Things (IoT) environment seems to open limitless possibilities, combining data gathered from wearable device sensors with other patient and personal data in real-time.
However, every new technology must undergo careful evaluation and scrutiny. Rigorous, systematic studies involving larger populations over longer time periods are direly needed. A future review should be conducted to include device and the parameters for judging accuracy, not only from the viewpoint of professional experts, but also that of those who agree to be assessed, including those who may be mildly affected, but also those with severe mental illness. Other research directions include general questions of privacy and data sovereignty that arise from the use of cloud-based storage of data or in the context of myriads of interconnected devices which are also connected to the datacenters of hospitals, private companies, and governments. There are related questions concerning the scope of an individual's consent to use their data, and potential liability where data is misused. Not only is the method of obtaining proper informed consent important, but also whether consent should be obtained at multiple stages of a study. That consent process may also be multi-layered, involving several entities. On liability, there are risks with misdiagnoses, harmful recommendations, or recommendations that do not adhere to the requisite standard of care.
These questions are becoming ever more pertinent with the integration of artificial intelligence into wearable technologies. The potential legal implications are significant, with vast data now being incorporated into making wearable devices viable diagnostic and monitoring tools on a larger scale. Unintended consequences may arise from data security breaches or the reidentification of previously de-identified data.
Further, the status of wearables as being either ‘medical’ or ‘therapeutic’ and their risk classification will have implications for their permitted use and how the associated mental health data should be managed. Ultimately, there will be questions about the appropriate balance between allowing the necessary flow of information to ensure that the devices are useful, and the flow of data that goes beyond what is needed. The most rewarding and exciting research will require a multidisciplinary endeavor of engineers, medical practitioners, policy makers and legal experts.
5. Conclusion
This is the first review scoping the landscape of using wearable devices as ingredients to alleviate mental health symptoms, in particular: anxiety and depression. Despite most wearable devices being purpose-shifted from fitness monitoring or other smart functions, the emergence of affordable, consumer-grade biosensors offers the potential for new approaches to support mental health therapies. Their main potential is their ability to track users’ habits and vitals at many measurement points at the leisure of the user. Such data could either fuel software expert systems, supporting early (self-)diagnosis or supporting full, expert-guided treatment. Two main research directions as of this writing are: (a) a focus on purposefully designed wearable devices that combine the expertise of technologists and clinical experts and (b) longer and better populated systematic studies scrutinizing the benefits of wearable devices, both as data gathering and recommendation devices in the context of anxiety and depression.
Funding
N/A.
Ethical approval
Not applicable within the manuscript.
Guarantor
Not applicable within the manuscript.
Contributor ship
Mahmood and Sarah performed the searches, Hashem and Sara performed the data extraction. Arfan drafted the initial manuscript, Alaa and Mowafa guided and supervised the process. All other authors contributed to the final manuscript write up.
Declaration of Competing Interests
The authors have no competing interests to declare.
Acknowledgements
We acknowledge the help of Samantha Cayo (MLIS), affiliated with the Health Sciences Library at Weill Cornell Medicine-Qatar, in editing the manuscript.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.cmpbup.2023.100095.
Appendix. Supplementary materials
References
- 1.Hasin D.S., et al. Epidemiology of adult DSM-5 major depressive disorder and its specifiers in the United States. JAMA Psychiatry. 2018;75(4):336–346. doi: 10.1001/jamapsychiatry.2017.4602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kessler R.C., Bromet E.J. The epidemiology of depression across cultures. Annu. Rev. Public Health. 2013;34:119–138. doi: 10.1146/annurev-publhealth-031912-114409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Konnopka A., König H. Economic burden of anxiety disorders: a systematic review and meta-analysis. Pharmacoeconomics. 2020;38(1):25–37. doi: 10.1007/s40273-019-00849-7. [DOI] [PubMed] [Google Scholar]
- 4.Vigo D., Thornicroft G., Atun R. Estimating the true global burden of mental illness. Lancet Psychiatry. 2016;3(2):171–178. doi: 10.1016/S2215-0366(15)00505-2. [DOI] [PubMed] [Google Scholar]
- 5.Hawton K., et al. Risk factors for suicide in individuals with depression: a systematic review. J. Affect. Disord. 2013;147(1–3):17–28. doi: 10.1016/j.jad.2013.01.004. [DOI] [PubMed] [Google Scholar]
- 6.Plana-Ripoll O., et al. A comprehensive analysis of mortality-related health metrics associated with mental disorders: a nationwide, register-based cohort study. Lancet. 2019;394(10211):1827–1835. doi: 10.1016/S0140-6736(19)32316-5. [DOI] [PubMed] [Google Scholar]
- 7.Elflein, J. "Share of the population worldwide who suffered from anxiety disorders from 1990 to 2017". 2019 [cited 2020 30/12/2020]; Available from: https://www.statista.com/statistics/1035153/percentage-of-people-with-anxiety-worldwide/.
- 8.Azhar F.A.B., Dhillon J.S. in 2016 3rd International Conference on Computer and Information Sciences (ICCOINS) IEEE; 2016. A systematic review of factors influencing the effective use of mHealth apps for self-care. [Google Scholar]
- 9.Elgendi M., Menon C. Assessing anxiety disorders using wearable devices: challenges and future directions. Brain Sci. 2019;9(3):50. doi: 10.3390/brainsci9030050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ahmed A., et al. A review of mobile chatbot apps for anxiety and depression and their self-care features. Comput. Methods Prog. Biomed. Update. 2021 [Google Scholar]
- 11.Jakicic J.M., et al. Effect of wearable technology combined with a lifestyle intervention on long-term weight loss: the IDEA randomized clinical trial. JAMA. 2016;316(11):1161–1171. doi: 10.1001/jama.2016.12858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Solaiman B. Addressing access with artificial intelligence: overcoming the limitations of deep learning to broaden remote care today. U. Mem. L. Rev. 2020;51:1103. [Google Scholar]
- 13.Abd-Alrazaq A.A., et al. An overview of the features of chatbots in mental health: a scoping review. Int. J. Med. Inform. 2019;132 doi: 10.1016/j.ijmedinf.2019.103978. [DOI] [PubMed] [Google Scholar]
- 14.Tricco A.C., et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann. Intern. Med. 2018;169(7):467–473. doi: 10.7326/M18-0850. [DOI] [PubMed] [Google Scholar]
- 15.statista, "Mobile operating systems' market share worldwide from January 2012 to June 2021". 2021. [cited 2020 30/12/2020]; Available from: https://www.statista.com/statistics/272698/global-market-share-held-by-mobile-operating-systems-since-2009/.
- 16.Chekroud S.R., et al. Association between physical exercise and mental health in 1· 2 million individuals in the USA between 2011 and 2015: a cross-sectional study. Lancet Psychiatry. 2018;5(9):739–746. doi: 10.1016/S2215-0366(18)30227-X. [DOI] [PubMed] [Google Scholar]
- 17.Pascoe M., et al. Physical activity and exercise in youth mental health promotion: a scoping review. BMJ Open Sport Exercise Med. 2020;6(1) doi: 10.1136/bmjsem-2019-000677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Service, N.H. "Treatment - generalised anxiety disorder in adults". 2021 [cited 2021]; Available from: https://www.nhs.uk/mental-health/conditions/generalised-anxiety-disorder/treatment/.
- 19.Zhang Z., et al. The effect of CBT and its modifications for relapse prevention in major depressive disorder: a systematic review and meta-analysis. BMC Psychiatry. 2018;18(1):1–14. doi: 10.1186/s12888-018-1610-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Further reading
- 1.Tiwari A., et al. 2019 41st Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC) IEEE; 2019. A comparative study of stress and anxiety estimation in ecological settings using a smart-shirt and a smart-bracelet. [DOI] [PubMed] [Google Scholar]
- 2.O'Brien J., et al. A study of wrist-worn activity measurement as a potential real-world biomarker for late-life depression. Psychol. Med. 2017;47(1):93–102. doi: 10.1017/S0033291716002166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cruz L., et al. Proceedings of the 14th International Conference on Mobile and Ubiquitous Multimedia. 2015. A wearable and mobile intervention delivery system for individuals with panic disorder. [Google Scholar]
- 4.Chum J., et al. Acceptability of the fitbit in behavioural activation therapy for depression: a qualitative study. Evid. Based Ment. Health. 2017;20(4):128–133. doi: 10.1136/eb-2017-102763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Krane-Gartiser K., et al. Actigraphically assessed activity in unipolar depression: a comparison of inpatients with and without motor retardation. J. Clin. Psychiatry. 2015;76(9):0. doi: 10.4088/JCP.14m09106. [DOI] [PubMed] [Google Scholar]
- 6.Nishida M., et al. Actigraphy in patients with major depressive disorder undergoing repetitive transcranial magnetic stimulation: an open label pilot study. J. ECT. 2017;33(1):36–42. doi: 10.1097/YCT.0000000000000352. [DOI] [PubMed] [Google Scholar]
- 7.Winkler D., et al. Actigraphy in patients with treatment-resistant depression undergoing electroconvulsive therapy. J. Psychiatr. Res. 2014;57:96–100. doi: 10.1016/j.jpsychires.2014.06.006. [DOI] [PubMed] [Google Scholar]
- 8.Swanson L.M., et al. An open-label pilot study of a home wearable light therapy device for postpartum depression. Arch. Womens Ment. Health. 2018;21(5):583–586. doi: 10.1007/s00737-018-0836-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Swanson L., et al. 1105 An open-label pilot study of a wearable home morning light therapy for postpartum depression. Sleep. 2017;40(suppl_1):A412. [Google Scholar]
- 10.Cosma G., et al. in 2017 International Conference on Internet of Things for the Global Community (IoTGC) IEEE; 2017. Analysis of multimodal data obtained from users of smart textiles designed for mental wellbeing. [Google Scholar]
- 11.Ryan J., Edney S., Maher C. Anxious or empowered? A cross-sectional study exploring how wearable activity trackers make their owners feel. BMC Psychol. 2019;7(1):1–8. doi: 10.1186/s40359-019-0315-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jin J., et al. Vol. 8. IEEE Access; 2020. pp. 89258–89268. (Attention-block Deep Learning Based Features Fusion in Wearable Social Sensor For Mental Wellbeing Evaluations). [Google Scholar]
- 13.McCall C., McCall W.V. Comparison of actigraphy with polysomnography and sleep logs in depressed insomniacs. J. Sleep Res. 2012;21(1):122–127. doi: 10.1111/j.1365-2869.2011.00917.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mishra R., et al. Decrease in mobility during the COVID-19 pandemic and its association with increase in depression among older adults: a longitudinal remote mobility monitoring using a wearable sensor. Sensors. 2021;21(9):3090. doi: 10.3390/s21093090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jacobson N.C., et al. Deep learning paired with wearable passive sensing data predicts deterioration in anxiety disorder symptoms across 17–18 years. J. Affect. Disord. 2021;282:104–111. doi: 10.1016/j.jad.2020.12.086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chow P., et al. Proceedings of the 2016 ACM International Joint Conference on Pervasive and Ubiquitous Computing: Adjunct. 2016. DEMONS: an integrated framework for examining associations between physiology and self-reported affect tied to depressive symptoms. [Google Scholar]
- 17.Kim H., et al. Depression prediction by using ecological momentary assessment, actiwatch data, and machine learning: observational study on older adults living alone. JMIR Mhealth Uhealth. 2019;7(10):e14149. doi: 10.2196/14149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Winslow B.D., et al. Development and clinical evaluation of an mHealth application for stress management. Front. Psychiatry. 2016;7:130. doi: 10.3389/fpsyt.2016.00130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dias L.P.S., et al. Development and testing of iAware model for ubiquitous care of patients with symptoms of stress, anxiety and depression. Comput. Methods Programs Biomed. 2020;187 doi: 10.1016/j.cmpb.2019.105113. [DOI] [PubMed] [Google Scholar]
- 20.Rothschild-Fuentes B., et al. Effects of mirtazapine on the sleep wake rhythm of geriatric patients with major depression: an exploratory study with actigraphy. Pharmacopsychiatry. 2013;46(02):59–62. doi: 10.1055/s-0032-1323655. [DOI] [PubMed] [Google Scholar]
- 21.Balconi M., Fronda G., Crivelli D. Effects of technology-mediated mindfulness practice on stress: psychophysiological and self-report measures. Stress. 2019;22(2):200–209. doi: 10.1080/10253890.2018.1531845. [DOI] [PubMed] [Google Scholar]
- 22.Costa J., et al. EmotionCheck: a wearable device to regulate anxiety through false heart rate feedback. GetMobile: Mobile Comput. Commun. 2017;21(2):22–25. doi: 10.1145/3131214.3131222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Costa J., et al. in Proceedings of the 2016 ACM International Joint Conference on Pervasive and Ubiquitous Computing. 2016. EmotionCheck: leveraging bodily signals and false feedback to regulate our emotions. [Google Scholar]
- 24.Tazawa Y., et al. Evaluating depression with multimodal wristband-type wearable device: screening and assessing patient severity utilizing machine-learning. Heliyon. 2020;6(2):e03274. doi: 10.1016/j.heliyon.2020.e03274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yadav Megha, et al. Exploring individual differences of public speaking anxiety in real-life and virtual presentations. IEEE Trans. Affect. Comput. 2020;13(3):1168–1182. [Google Scholar]
- 26.Naslund J.A., et al. Feasibility of popular m-health technologies for activity tracking among individuals with serious mental illness. Telemed. e-Health. 2015;21(3):213–216. doi: 10.1089/tmj.2014.0105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cushing C.C., et al. Individual differences in negative affectivity and physical activity in adolescents: an ecological momentary assessment study. J. Child Fam. Stud. 2018;27(9):2772–2779. [Google Scholar]
- 28.Smith E.N., et al. Integrating wearables in stress management interventions: promising evidence from a randomized trial. Int. J. Stress Manag. 2020;27(2):172. [Google Scholar]
- 29.Nadal C., et al. Integration of a smartwatch within an internet-delivered intervention for depression: protocol for a feasibility randomized controlled trial on acceptance. Contemp. Clin. Trials. 2021;103 doi: 10.1016/j.cct.2021.106323. [DOI] [PubMed] [Google Scholar]
- 30.Lu J., et al. Joint modeling of heterogeneous sensing data for depression assessment via multi-task learning. Proc. ACM Interact., Mob., Wearable Ubiquitous Technol. 2018;2(1):1–21. [Google Scholar]
- 31.Rojo-Wissar D.M., et al. Maternal bonding predicts actigraphy-measured sleep parameters in depressed and non-depressed adults. J. Nerv. Ment. Dis. 2020;208(1):33. doi: 10.1097/NMD.0000000000001071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Razavi N., et al. Measuring motor activity in major depression: the association between the Hamilton depression rating scale and actigraphy. Psychiatry Res. 2011;190(2–3):212–216. doi: 10.1016/j.psychres.2011.05.028. [DOI] [PubMed] [Google Scholar]
- 33.Pedrelli P., et al. Monitoring changes in depression severity using wearable and mobile sensors. Front. Psychiatry. 2020;11:1413. doi: 10.3389/fpsyt.2020.584711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ghandeharioun Asma, et al. 2017 Seventh International Conference on Affective Computing and Intelligent Interaction (ACII) Vol. 54. IEEE; 2017. Objective assessment of depressive symptoms with machine learning and wearable sensors data. [Google Scholar]
- 35.Shah R.V., et al. Personalized machine learning of depressed mood using wearables. Transl. Psychiatry. 2021;11(1):1–18. doi: 10.1038/s41398-021-01445-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Boukhechba M., et al. in 2018 IEEE EMBS International Conference on Biomedical & Health Informatics (BHI) IEEE; 2018. Physiological changes over the course of cognitive bias modification for social anxiety. [Google Scholar]
- 37.Fukuda Shuichi, et al. 2020 IEEE International Conference on Pervasive Computing and Communications Workshops (PerCom Workshops) Vol. 57. IEEE; 2020. Predicting depression and anxiety mood by wrist-worn sleep sensor. [Google Scholar]
- 38.Moshe I., et al. Predicting symptoms of depression and anxiety using smartphone and wearable data. Front. Psychiatry. 2021;12 doi: 10.3389/fpsyt.2021.625247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.McGinnis R.S., et al. in 2018 40th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC) IEEE; 2018. Rapid anxiety and depression diagnosis in young children enabled by wearable sensors and machine learning. [DOI] [PubMed] [Google Scholar]
- 40.McGinnis R.S., et al. Rapid detection of internalizing diagnosis in young children enabled by wearable sensors and machine learning. PLoS ONE. 2019;14(1) doi: 10.1371/journal.pone.0210267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Zhang Y., et al. Relationship between major depression symptom severity and sleep collected using a wristband wearable device: multicenter longitudinal observational study. JMIR Mhealth Uhealth. 2021;9(4):e24604. doi: 10.2196/24604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Matcham F., et al. Remote assessment of disease and relapse in major depressive disorder (RADAR-MDD): a multi-centre prospective cohort study protocol. BMC Psychiatry. 2019;19(1):1–11. doi: 10.1186/s12888-019-2049-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hoogerhoud A., et al. Short-term effects of electroconvulsive therapy on subjective and actigraphy-assessed sleep parameters in severely depressed inpatients. Depress Res. Treat. 2015;2015 doi: 10.1155/2015/764649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Pittig A., Hoyer J., Noack R. Smart-glass guided exposure for anxiety disorders: a proof-of-concept study. Cogn. Behav. Pract. 2021 [Google Scholar]
- 45.Dillon A., et al. Smartphone applications utilizing biofeedback can aid stress reduction. Front. Psychol. 2016;7:832. doi: 10.3389/fpsyg.2016.00832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Sundaravadivel Prabha, Wilmoth Parker, Fitzgerald Ashton. 2021 22nd International Symposium on Quality Electronic Design (ISQED) IEEE; 2021. SolicitudeSavvy: an IoT-based edge intelligent framework for monitoring anxiety in real-time. [Google Scholar]
- 47.Yadav Megha, Behzadan Amir, Chaspari Theodora. 2019 First International Conference on Transdisciplinary AI (TransAI) IEEE; 2019. Speak Up! Studying the interplay of individual and contextual factors to physiological-based models of public speaking anxiety. [Google Scholar]
- 48.Narziev N., et al. STDD: short-term depression detection with passive sensing. Sensors. 2020;20(5):1396. doi: 10.3390/s20051396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hao T., et al. in AMIA Annual Symposium Proceedings. American Medical Informatics Association; 2017. StressHacker: towards practical stress monitoring in the wild with Smartwatches. [PMC free article] [PubMed] [Google Scholar]
- 50.Azevedo R.T., et al. The calming effect of a new wearable device during the anticipation of public speech. Sci. Rep. 2017;7(1):1–7. doi: 10.1038/s41598-017-02274-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wang R., et al. Tracking depression dynamics in college students using mobile phone and wearable sensing. Proc. ACM Interact., Mobile, Wearable Ubiquitous Technol. 2018;2(1):1–26. [Google Scholar]
- 52.Funane T. in 2015 37th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC) IEEE; 2015. Wearable near-infrared spectroscopy neuroimaging and its applications. [DOI] [PubMed] [Google Scholar]
- 53.McGinnis E.W., et al. Wearable sensors detect childhood internalizing disorders during mood induction task. PLoS ONE. 2018;13(4) doi: 10.1371/journal.pone.0195598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Gu Jun, et al. 2017 International Conference on Cyber-Enabled Distributed Computing and Knowledge Discovery (CyberC) IEEE; 2017. Wearable social sensing and its application in anxiety assesment. [Google Scholar]
- 55.Powell A., et al. Wearable technology to assess bradykinesia and immobility in patients with severe depression undergoing electroconvulsive therapy: a pilot study. J. Psychiatr. Res. 2020;130:75–81. doi: 10.1016/j.jpsychires.2020.07.017. [DOI] [PubMed] [Google Scholar]
- 56.Cormack F., et al. Wearable technology for high-frequency cognitive and mood assessment in major depressive disorder: longitudinal observational study. JMIR Ment. Health. 2019;6(11):e12814. doi: 10.2196/12814. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.