Abstract
Objective:
Schools offer an ideal setting for childhood obesity interventions due to their access to children and adolescents. This review aimed to systematically review the impact of school-based intervention for the treatment of childhood obesity.
Design:
Eight databases were searched from inception till 30 May 2020. A revised Cochrane risk-of-bias tool and the Grading of Recommendations, Assessment, Development and Evaluations criteria were used to evaluate the risk of bias and overall evidence. Meta-analysis and meta-regression were performed on Stata software using the random effects model. Overall effect was evaluated using Hedges’ g, and heterogeneity was assessed using Cochran’s Q and I2.
Setting:
Cluster randomised controlled trials (cluster-RCT) delivered in school.
Participants:
Children and adolescents (6–18 years of age) with overweight and obesity.
Results:
Twelve cluster-RCT from seven countries with 1755 participants were included in the meta-analysis. School-based interventions for the treatment of childhood obesity reduced BMI and BMI z-scores with a medium effect (g = 0·52). Subgroup analyses showed greater effectiveness of brief school-based interventions and the interventions conducted in lower-middle to upper-middle economies. Meta-regression assessed the heterogeneity and the final model, with covariates of the type of economies and trial duration, accounted for 41·2 % of the variability. The overall quality of evidence was rated low because of the high risk of bias and inconsistency.
Conclusions:
School-based interventions are a possible approach to provide universal healthcare for the treatment of childhood obesity, and further well-designed cluster-RCT with longer follow-up are needed. This study is registered with PROSPERO (CRD42020160735).
Keywords: School-based, Obesity, Children, Adolescent
Globally, the number of children and adolescents (5–19 years) with obesity is estimated at 124 million, with a prevalence of 5·6 % in girls and 7·8 % in boys in 2016(1). Childhood obesity, typically defined by the BMI cut-off points specific for age and gender(2), increases the risks of being an adult with obesity(3), developing type 2 diabetes, hypertension, dyslipidaemia(4) and CHD(5–7). BMI reduction amongst individuals with childhood obesity reduces the risk of developing type 2 diabetes(4), hypertension and dyslipidaemia(5) in adulthood to a level comparable to those with normal weight. Hence, interventions for the treatment of childhood obesity are necessary.
Despite the extensive literature on childhood obesity treatments in healthcare settings and community-based interventions in schools, primary care and community sites(8–11), the evidence is primarily limited to well-funded clinical trials and poses limitations in scalability in practice(12). These limitations include the lack of resources when scaling out those interventions and present potential difficulties when delivered to a diverse population(13,14). Compared with randomised controlled trials (RCT) which determine the efficacy of an intervention given in a specific condition, cluster-RCT evaluate the effectiveness of an intervention in a real-world setting(15). Therefore, evidence gathered on cluster-RCT allows a better generalisation of results which could guide policy decisions in the translation of knowledge into practice(16).
To combat childhood obesity, the treatment should be an element of universal health coverage and integrated into existing systems where children spend most of their time to achieve maximum effectiveness(17). Based on Cochrane reviews of the treatment of childhood obesity, the use of diet, physical activity and behavioural interventions can improve BMI outcomes with no difference observed between treatments conducted in schools and other settings(8,9). School-based interventions for the treatment of childhood obesity allow access to children and adolescents who spend a considerable amount of time in school(18,19), including those from lower socio-economic status who may not seek healthcare(20). As many children and adolescents have meals in school which are equipped with facilities for physical activity, school-based interventions provide an avenue to increase the quality of their diet and physical activity duration(21). Parental involvement could be made possible by leveraging existing communication channels with parents to sustain behavioural changes at home(22). Though children and adolescents with overweight and obesity may face poorer self-perception(23) and discrimination from peers in school(24), school-based obesity interventions were found to improve the self-esteem of children and adolescents more than interventions delivered in a clinical setting(25).
Three systematic reviews and meta-analyses studied the effectiveness of school-based intervention for the treatment of childhood obesity(26–28), and two of the reviews found school-based interventions to be effective in reducing BMI outcomes(27,28). The reviews identified different components of parental involvement(28), educational interventions(27) and the combination of physical activity and educational interventions(26) which contributed to the reduction in BMI outcomes. Two reviews had differing findings on the duration required for significant changes in BMI of 6 months(27) and 1 year(26). Statistical heterogeneity was encountered in the reviews(26–28), and their analyses were limited to sensitivity analyses rather than exploring the effectiveness of interventional components through subgroup analyses. Based on the existing systematic reviews, firm conclusions could not be drawn on school-based interventions for the treatment of childhood obesity due to the following limitations. First, the reviews included obesity prevention trials which consisted of participants with normal weight(26–28). Second, the reviews had a specific focus on educational interventions(27) and interventions led by nurses(28) instead of a multicomponent approach delivered by various professionals. Third, separate analyses were conducted for trials which reported BMI and BMI z-scores, respectively, which led to inconclusive findings regarding the effectiveness of school-based interventions(27,28).
Therefore, this review aimed to systematically locate, appraise and review the evidence of the effectiveness of school-based interventions for the treatment of childhood obesity and to identify variations in the effect size attributed to the interventional characteristics of theoretical framework, type of professional support, duration of intervention, components and parental support. The results of this review can contribute to guiding the design of effective school-based interventions for the treatment of childhood obesity.
Method
The systematic review and meta-analysis are reported in accordance with the Preferred Reporting Items for Systematic Review and Meta-Analyses (PRISMA) (refer to PRISMA Checklist)(29). This review is registered in the International Prospective Register of Systematic Reviews (CRD42020160735).
The eligible trials were (i) cluster-RCT, (ii) included children and adolescents (aged 6–18 years) defined as overweight or obese using the BMI-for-age percentiles based on a reference population, (iii) interventions included which aimed towards the treatment of overweight and obesity, (iv) conducted in the school setting or carried out in the school vicinity and (v) measured primary outcomes of BMI and BMI z-score (refer to online supplementary material, Supplemental Table S1). Secondary outcomes were cardiovascular, metabolic, nutrition, physical activity, sedentary behaviour and psychosocial-related outcomes. Trials were excluded if the participants were diagnosed with any medical or psychiatric condition, received medication or underwent surgical intervention that may influence their weight. Obesity prevention studies and publications in languages other than English were excluded.
The review adopted the recommendations of the Cochrane Handbook for Systematic Reviews (2019)(30). First, the authors searched through eight databases (PubMed, Embase, CINAHL, Cochrane Library, PsycINFO, ProQuest, Scopus and Web of Science) from inception until 30 May 2020 according to the individual database’s subject terms and syntax rules (refer to online supplementary material, Supplemental Table S2). Second, the authors searched for ongoing and unpublished trials in various clinical trial registries. Third, the authors searched the reference list of relevant systematic reviews, selected trials, grey literature and targeted journals.
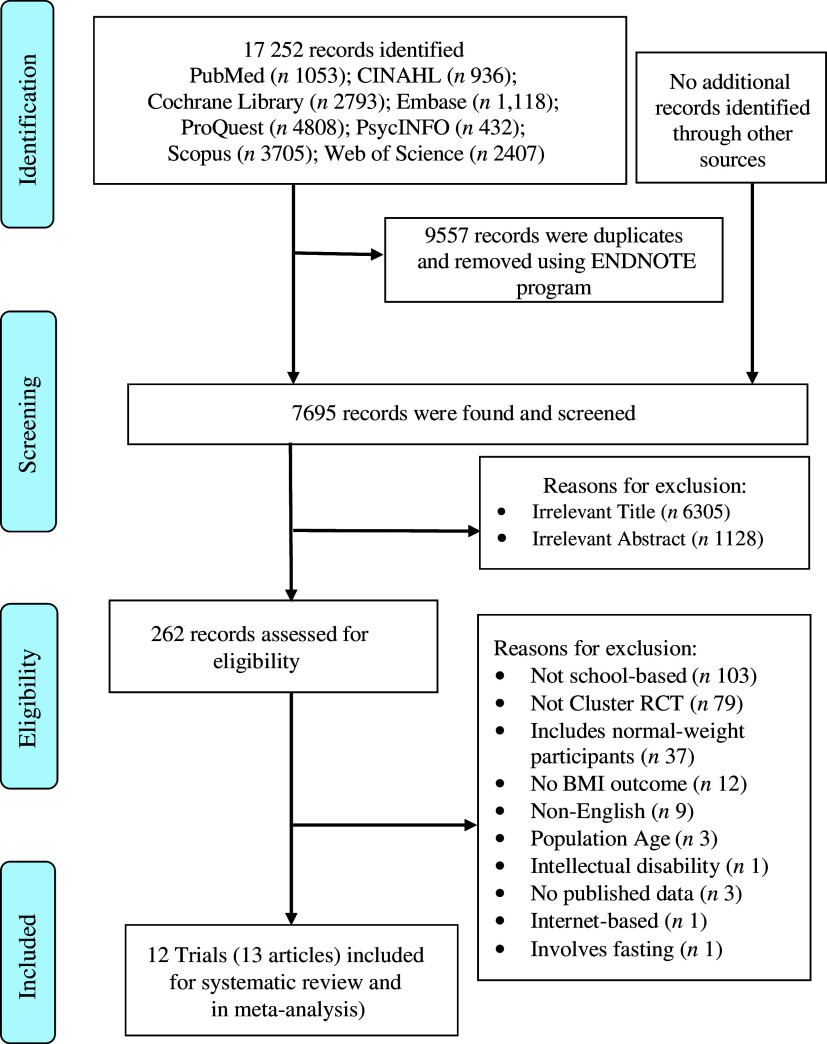
The study selection was conducted in four phases, which are graphically illustrated using the PRISMA flow diagram(29). First, all identified records from the eight databases were collated in EndNote version X9 (Thomson Reuters), and duplicates were removed. Second, two authors (T.J.H.H. and L.J.C.) independently screened the titles and abstracts to remove irrelevant records. Third, the two authors assessed the full-text articles independently based on the eligibility criteria. Studies were collated when multiple reports of the same study were identified. Last, the two authors compared their findings to verify if any articles were overlooked. The two authors resolved incongruity through discussion or with the involvement of a third author (L.Y.).
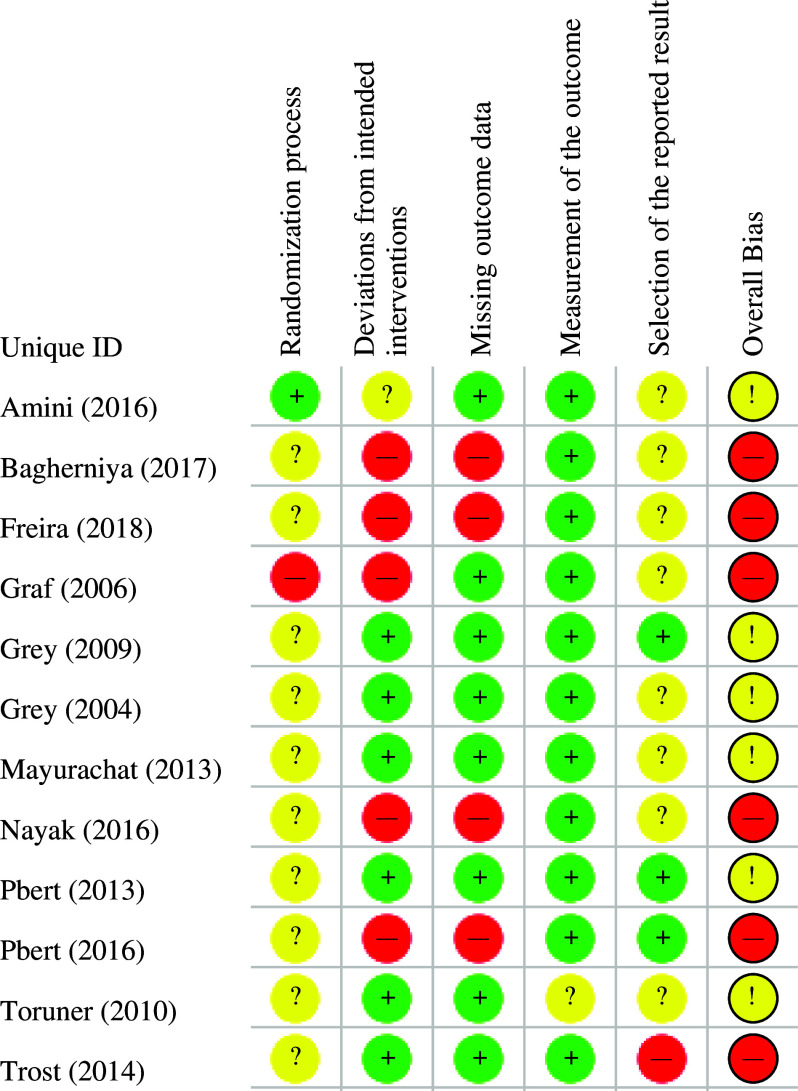
The revised Cochrane risk-of-bias (RoB 2.0) tool was used to identify the risk of bias among the selected trials(31). RoB 2.0 assessed individual randomised trials based on five domains of bias: bias arising from the randomisation process, bias due to deviations from intended intervention, bias due to missing outcome data, bias in the measurement of the outcome and bias in the selection of reported result. As this review only considered cluster-RCT, additional considerations were taken for the domain of randomisation that could arise from the timing of identification and recruitment of participants(32). For the domain of bias due to deviations from intended interventions, the review used signalling questions based on the effect of the assignment to intervention. The RoB 2.0 algorithmic tool proposed the risk of bias as (1) low risk of bias, (2) some concerns or (3) high risk of bias for each domain based on the responses to the signalling questions. Two authors independently responded to each of the signalling questions with (1) yes, (2) probably yes, (3) probably no, (4) no or (5) no information using the RoB 2.0 tool.
The Grading Recommendations, Assessment, Development and Evaluation (GRADE) system was used to assess the overall quality of the evidence(33). Each author rated the quality of evidence independently by considering five factors: (1) methodological limitation, (2) inconsistency, (3) indirectness, (4) imprecision and (5) publication bias. Any discrepancy between the results of the two authors for the risk of bias or the quality of evidence was resolved through discussion or by consultation with the third author (L.Y.).
The authors (T.J.H.H. and L.J.C.) independently extracted data from the included trials using a standardised data extraction form based on the Cochrane Handbook for Systematic Reviews of Interventions. The extracted data from the included trials included authors, year of publication, setting, inclusion criteria, sample, details of the intervention, control, outcomes, attrition rate, protocol, trial registration and grant support. The authors of the studies were contacted if information was missing or insufficient. The authors (T.J.H.H. and L.J.C.) compared their findings and verified them with the original publication to check for inconsistencies in the data extracted.
Meta-analysis and meta-regression were performed using Stata 16 software’s(34), Meta command procedures(35). The primary outcome was the change in BMI and BMI z-score between the intervention and control groups. Preference was given to the BMI outcome in studies that reported both BMI and BMI z-score, as BMI is superior in assessing the changes in adiposity(36). If the change in BMI or BMI z-score was not provided, the mean difference was calculated using the baseline(T1) and post-intervention’s(T2) mean and standard deviation using the formulas provided by the Cochrane Handbook for Systematic Reviews (2019). The sd of the mean difference was calculated as sd =
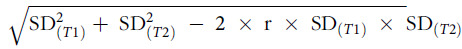 , where
, where
 represents sd at baseline and
represents sd at baseline and
 represents sd at post-intervention. The BMI correlation coefficients of 0·78, 0·84 and 0·83 were used to represent the 1-year duration of follow-up correlation for children (under 10 years), pubescents (10–14 years) and adolescents (above 14 to under 18 years), respectively(37). The standardised mean difference with inverse variance method was used to synthesise the outcomes of the BMI and BMI z-score. The review measured the magnitude of the intervention effect between the intervention and control groups using effect size expressed as Hedges (g), which are defined as very small (0·1), small (0·2), medium (0·5), large (0·8), very large (1·2) and huge (2·0)(38). The review used the random effects model, which assumes that the distribution of effect varies across studies, and the variation may arise from the intervention implementation and participants(39). Previous meta-analyses of children and adolescent weight management(26–28,40–43) reported a substantial statistical heterogeneity. Therefore, the Hedges’ random effects estimator was chosen because of its better performance compared with other estimators in the presence of between-study variance(44,45). A cumulative meta-analysis was conducted based on the year of publication to examine the accumulation of evidence over time by performing separate meta-analyses with the addition of one trial at each time(46). When two or more trials reported secondary outcomes using the same measures, the continuous data were analysed with mean difference, whereas continuous data were measured with a variety of measures that were analysed in standardised mean difference.
represents sd at post-intervention. The BMI correlation coefficients of 0·78, 0·84 and 0·83 were used to represent the 1-year duration of follow-up correlation for children (under 10 years), pubescents (10–14 years) and adolescents (above 14 to under 18 years), respectively(37). The standardised mean difference with inverse variance method was used to synthesise the outcomes of the BMI and BMI z-score. The review measured the magnitude of the intervention effect between the intervention and control groups using effect size expressed as Hedges (g), which are defined as very small (0·1), small (0·2), medium (0·5), large (0·8), very large (1·2) and huge (2·0)(38). The review used the random effects model, which assumes that the distribution of effect varies across studies, and the variation may arise from the intervention implementation and participants(39). Previous meta-analyses of children and adolescent weight management(26–28,40–43) reported a substantial statistical heterogeneity. Therefore, the Hedges’ random effects estimator was chosen because of its better performance compared with other estimators in the presence of between-study variance(44,45). A cumulative meta-analysis was conducted based on the year of publication to examine the accumulation of evidence over time by performing separate meta-analyses with the addition of one trial at each time(46). When two or more trials reported secondary outcomes using the same measures, the continuous data were analysed with mean difference, whereas continuous data were measured with a variety of measures that were analysed in standardised mean difference.
A test for statistical heterogeneity was conducted using Cochran’s Q (χ2) with statistical significance of P < 0·1 because of its low statistical power in detecting true heterogeneity(47).
 statistics was used to evaluate inconsistency and was interpreted as not important (0–40 %), moderate heterogeneity (30–60 %), substantial heterogeneity (50–90 %) and considerable heterogeneity (75–100 %). Overlapping
statistics was used to evaluate inconsistency and was interpreted as not important (0–40 %), moderate heterogeneity (30–60 %), substantial heterogeneity (50–90 %) and considerable heterogeneity (75–100 %). Overlapping
 values were classified according to the direction and magnitude of treatment effect and the P-value of the χ2 test. Sensitivity analysis was conducted when heterogeneity was statistically significant to maintain homogeneity amongst the pooled trials(48). Subgroup analyses were conducted to identify the sources of heterogeneity related to trial characteristic, the classification of countries’ economies provided by the World Bank(49), trial duration, professional background delivering the intervention, number of sessions delivered and components of physical activity, nutrition education and parental involvement. In addition, Hedges random effects univariate meta-regression was performed to explore the potential sources of heterogeneity on the effect size of the change of BMI outcomes with variables similar to subgroup analyses and additional trial characteristics for year of publication, risk of bias, total sample size, total number of clusters and percentage of females recruited. Multivariate meta-regression analysis was conducted using a forward stepwise procedure of adding variables with P < 0·1, starting with the smallest P-value into the model(50).
values were classified according to the direction and magnitude of treatment effect and the P-value of the χ2 test. Sensitivity analysis was conducted when heterogeneity was statistically significant to maintain homogeneity amongst the pooled trials(48). Subgroup analyses were conducted to identify the sources of heterogeneity related to trial characteristic, the classification of countries’ economies provided by the World Bank(49), trial duration, professional background delivering the intervention, number of sessions delivered and components of physical activity, nutrition education and parental involvement. In addition, Hedges random effects univariate meta-regression was performed to explore the potential sources of heterogeneity on the effect size of the change of BMI outcomes with variables similar to subgroup analyses and additional trial characteristics for year of publication, risk of bias, total sample size, total number of clusters and percentage of females recruited. Multivariate meta-regression analysis was conducted using a forward stepwise procedure of adding variables with P < 0·1, starting with the smallest P-value into the model(50).
Results
The study selection process is illustrated in Fig. 1. A total of 17 252 records were identified from eight databases and screened to remove duplicates (n 9557). The remaining 7695 records were screened to remove the records with irrelevant titles (n 6305) and abstracts (n 1128). Full-text articles (n 262) were downloaded and assessed against the eligibility criteria of this review. The authors excluded 249 records based on the reasons outlined in Fig. 1. Supplemental Table S3 outlines the reasons for the exclusion of each record. The systematic review and meta-analysis included thirteen articles from twelve trials(51–63), in which one trial reported physical activity(52) and nutrition outcomes(53) in separate publications.
Fig. 1.
Selection of trials for inclusion in the systematic and meta-analysis
Table 1 outlines the characteristics of the twelve trials conducted in seven different countries amongst 1755 participants across the USA (n 5), Asia (n 5) and Europe (n 2). The trials were published between 2004 and 2017, and the sample size ranged from 41(56) to 334(51). The twelve cluster-RCT included a total of eighty-four clusters, with each comprising two clusters(56,58,62) to twelve clusters(51). All of the trials included participants with overweight and obesity status, except three trials, which targeted participants with overweight and a family history of diabetes (n 1)(54) and participants with overweight and obesity and a family history of diabetes (n 2)(56,57). The mean age of the participants ranged from 8·4 years(55) to 15·9 years(54). Only one trial with two publications exclusively recruited female participants(52,53).
Table 1.
Characteristics of selected cluster randomised controlled trials for school-based weight management
| Name (year), state, country | Population | Site, sample size (clusters) | Age, M (sd), % female | Intervention name, theoretical framework, curriculum type, duration | Control | Professional support | Outcomes | Attrition, n (%) | ITT/missing data management | Protocol/registration | GS |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Amini (2016)(51),Tehran, Iran | Age: 10–12 years, overweight and obese (WHO) | Schools, I: 167 (6), C: 167 (6) | I: 10·9 (NR), 46·1 %, C: 11·1 (NR), 52·1 % | NA, NA, after-school curriculum, 4·5 months | No intervention | Nutrition education instructors, physical activity coaches, and researchers | Anthropometric: BMI z-Score; BMI z-score mean difference, WC, HC, SFT; PA: Duration; SB: Duration; Dietary intake: kcal and 24-h recall | I: 5 (3·0 %), C: 3 (1·8 %) | N/N | N/Y | Y |
| Bagherniya et al. (2017, 2018)(52,53), Shahin Shahr, Iran | Age: 12–16 years, overweight and obese (WHO) | Schools, I: 87 (4), C: 85 (4) | I: 13·53 (0·67), 100 %, C: 13·35 (0·60), 100 % | NA, Social Cognitive Theory, after-school curriculum, 7·5 months | No intervention | Researcher, sports expert (counselling), and physical trainer | Anthropometric: BMI, WC; Psychosocial: Social Cognitive Theory Constructs on diet and PA | I: 14 (16·1 %), C: 4 (4·7 %) | N/N | N/Y | Y |
| Freira (2018)(54), Lisbon, Portugal | Age: 14–19 years, overweight (WHO) | Schools, I: 51 (4), C: 46 (4) | I: 16·15 (1·49), 66·7 %, C: 15·77 (1·04), 73·2 % | IMAGINE, motivational interview, during school curriculum, 6 months | Counselling for participants by nurse and resident paediatrician | Dietitians, paediatrician, and physical education teacher | Anthropometric: BMI z-score, AC, fat mass, muscular mass; cardiovascular measures: Blood pressure | I: 4 (8·7 %), C: 10 (19·6 %) | N/N | N/Y | Y |
| Graf (2006)(55), Cologne, Germany | Age: 6–11 years, overweight and obese (German Percentile) | Schools, I: 121 (3), C: 155 (4) | I: 8·7 (1·3), NR; non-part: 8·1 (1·2), NR; C: 8·5 (1·3), NR | StEP TWO (NR), after-school curriculum, 9 months | Regular school programme | Nutritionist, gymnasts, and medical doctor | Anthropometric: BMI & mean difference, BMI z-score & mean difference; cardiovascular measures: Blood pressure, heart rate | I: 81 (66·9 %), C: 10 (6·5) | N/N | N/N | NR |
| Grey (2004)(56), New Haven, USA | Age: 10–14 years, obese
 95th percentile, Family history of T2DM
95th percentile, Family history of T2DM |
Schools, I: 22 (1), C: 19 (1) | I: 12·4 (1·2), 63·6 %, C: 12·6 (0·8), 63·2 % | NA, Coping Skills Training, after-school curriculum, 12 months | Same programme with intervention group, without use of Coping Skills Training | Dietitian, exercise interventionist, and research coordinator | Anthropometric: BMI; metabolic outcomes: OGTT, HbA1c; PA: RGSA; health behaviours: HPLP; dietary intake: CATCH; Psychosocial: CDI | I: 0, C: 0 | N/N | N/N | Y |
| Grey (2009)(57), New Haven, USA | Age: 12 years,
 85th percentile, family history of T2DM
85th percentile, family history of T2DM |
Schools, I: 112 (4), C: 86 (2) | I: 12·8 (0·7), 62·5 %, C: 12·6 (0·7), 41·9 % | NA, Coping Skills Training, during school curriculum, 12 months | Nutrition and exercise education, 8 sessions | Teachers | Anthropometric: BMI, WC; Metabolic and Lipids Outcomes: HOMA, fasting insulin, fasting lipids; physical activity: RGSA; health behaviours: HPLP; Psychosocial: CDI | I: 25 (22·3 %), C: 22 (25·6 %) | Y/Y | N/Y | Y |
| Mayurachat (2013)(58), Chiang Mai, Thailand | Age: 10–12 years, overweight and obese (WHO) | Schools, I: 68 (1), C: 68 (1) | I: 11·04 (0·56), 50 %, C: 11·03 (0·51), 35·3 % | NA, Theory of Planned Behaviour, during school curriculum, 4·5 months | Standard care, schools usual healthy eating programme | Research assistant | Anthropometric: BMI z-score; health behaviours: Intention to perform eating behaviours, Eating behaviours | I: 0 (0 %), C: 0 (0 %) | N/N | N/N | Y |
| Nayak et al (2016)(59), Udupi, India | Age: 10–16 years, overweight and obese (WHO) | Schools, I: 120 (5), C: 131 (5) | I: NR, 46·7 %, C: NR, 50·4 % | NA, NA, during and after-school curriculum, 6 months | No intervention | Physical activity instructor | Anthropometric: BMI, SFT; health behaviours: lifestyle practices; psychosocial: Children Self-Concept Scale | I: 30 (25·0 %), C: 27 (25·9 %) | N/N | N/N | NR |
| Pbert (2013)(61), Massachusetts, USA | Age: 14–17 years, overweight and obese,
 85th percentile (CDC)
85th percentile (CDC) |
Schools, I: 42 (4), C: 40 (4) | I: 15·9 (1·03), 64·3 %, C: 15·7 (1·01), 75·0 % | Lookin’ Good Feelin’ Good, Social Cognitive Theory, during school curriculum, 6 months | 6 individual visits to the school nurse | Nurse | Anthropometric: BMI, BMI z-score, WC; cardiovascular measures: blood pressure; health behaviours: YRBS; physical activity: Accelerometer; dietary intake: 24-h recall | I: 0, C: 0 | N/N | N/N | NR |
| Pbert (2016)(60), Massachusetts, USA | Age: 14–18 years, overweight and obese,
 85th percentile (CDC)
85th percentile (CDC) |
School, I: 58 (4), C: 68 (4) | I: 16·5 (1·23), 63·0 %, C: 16·3 (1·20), 61·4 % | Lookin’ Good Feelin’ Good, Social Cognitive Theory, during and after-school curriculum, 8 months | 12 individual visits to the school nurse | Nurse and school staff | Anthropometric: BMI, BMI z-score, WC; health behaviours: YRBS; physical activity: Accelerometer; dietary intake: 24-h recall | I: 0, C: 0 | N/N | N/Y | Y |
| Toruner (2010)(62), Ankara, Turkey | Age: 9–10 years, overweight and obese (Turkey) | Schools, I: 44 (1), C: 40 (1) | I: 9·34 (0·34), 46·3 %, C: 9·41 (0·27), 55 % | NA, Social Cognitive Theory, during school curriculum, 12 months | Wait-list control | Researchers | Anthropometric: BMI; health behaviours: Children knowledge on healthy lifestyle, parents knowledge of healthy lifestyle | I: 0, C: 0 | N/N | N/N | NR |
| Trost (2014)(63), Massachusetts, Rhode Island & Texas, USA | Age: 8–12 years, overweight and obese (CDC) | Schools and YMCA, I: 34 (6), C: 41 (5) | I: 10·1 (1·9), 56 %, C: 9·9 (1·5), 54 % | Join for ME, Family-based Treatment for Childhood Obesity, after-school curriculum, 4 months | Same programme with intervention group without game console | Trained facilitators | Anthropometric: BMI z-score; physical activity: accelerometer | I: 8 (23·5 %), C: 7 (17·1) | Y/Y | N/Y | Y |
AC, abdominal circumference; AMA, American Medical Association; CATCH, Child and Adolescent Trial for Cardiovascular Health; CDC, Centers for Disease Control and Prevention; CDI, Children’s Depression Inventory; HC, hip circumference; HOMA, Homoeostasis Model Assessment of Insulin Resistance; HPLP, Health Promoting Lifestyle Profile; N, No; NA, not applicable; non-part, non-participant; NR, not reported; OGTT, Oral Glucose Tolerance Test; PA, Physical Activity; RGSAS, Revised Godin-Shepard Activity; SB, Sedentary Behaviour; SFT, Skin Fold Thickness; T2DM, Type 2 Diabetes; WC, waist circumference; Y, Yes; YAQ, Youth/Adolescent Questionnaire; YRBS, Youth Risk Behaviour Survey.
Half of the trials (n 6, 50 %) were rated to have a high risk of overall bias, and the other half (n 6, 50 %) were rated as having some concerns (Fig. 2). In trials rated as having a high risk of overall bias, this was attributed to deviations from the intended interventions (n 5, 41·2 %), lack of intention-to-treat analysis (n 5, 41·2 %) and missing outcome data (n 4, 33·3 %) due to loss to follow-up, which differed between intervention and control groups. In trials rated as having some concerns for overall bias, this was mainly due to lack of information on the randomisation process (n 55, 41·2 %), as well as the lack of registration of a trial protocol (n 4, 33·3 %).
Fig. 2.
Risk of bias summary.  , Low risk;
, Low risk;  , some concerns;
, some concerns;  , high risk
, high risk
The quality of evidence evaluated using the GRADE system was graded low based on the domains of risk of bias and inconsistency (see online supplementary material, Supplemental Table S4). The risk of bias was downgraded as 50 % of the trials were rated high risk in the overall bias. Heterogeneity was considered significant with Cochran’s Q, P < 0·1 with substantial inconsistency of I2 = 88·9 %. Other domains of indirectness and imprecision were rated as insignificant. Egger’s regression asymmetry test (P = 0·68) was statistically insignificant, and the qualitative examination revealed a symmetrical funnel plot (see online supplementary material, Supplemental Figure S1), which suggested no evidence of small-study effects, including publication bias.
All trials’ clusters were conducted in schools with the exception of one trial, where clusters consisted of schools and the Young Men’s Christian Association(63). The school-based interventions included components of counselling (n 2)(54,61,63), nutrition education (n 1)(58), counselling and physical activity sessions (n 1)(60), nutrition education and physical activity sessions (n 4)(51–53,55,59) and a combination of nutrition education, physical activity sessions and counselling (n 4)(56,57,62,63) (see online supplementary material, Supplemental Table S5). Five trials had varying degrees of parental involvement, which included sessions conducted solely for parents (n 3)(51,55,59), to parents participating in sessions with their child (n 2)(52,53,63).
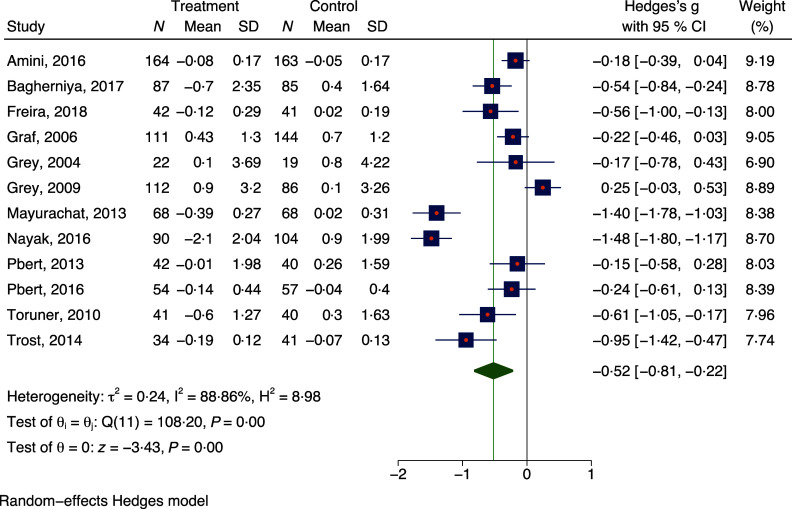
A meta-analysis was conducted to assess the effectiveness of school-based interventions for the treatment of childhood obesity compared with controls for all twelve trials (n 1755) on the measure of mean change in BMI outcomes from pre-intervention to post-intervention. The meta-analysis revealed a medium effect (g = 0·52) favouring school-based interventions (z = –3·43; P < 0·001; Fig. 3). Substantial statistical heterogeneity was noted and explored through sensitivity analysis and meta-regression (Q = 108·20; P < 0·1; I 2 = 88·9 %). Sensitivity analyses were conducted and did not have a remarkable impact on the effect size for BMI outcomes and statistical heterogeneity. Cumulative analysis by publication year revealed a trend favouring school-based interventions (see online supplementary material, Supplemental Figure S2).
Fig. 3.
Forest plot of effect size change in BMI outcomes for school-based interventions and control groups
The exploration of intervention characteristics was conducted using subgroup analyses (Table 2). Significant subgroup differences (Q = 24·0, P = < 0·01) were found between the types of economies where the trial was conducted with large effects for lower-middle to upper-middle economies (g = 0·84) and a small effect for high-income economies (g = 0·27). The subgroup analysis of intervention length revealed a subgroup difference based on intervention duration (Q = 24·0, P = < 0·05) with a medium effect for trials of 6 months or less (g = 0·79) and a small effect for trials of more than 6 months (g = 0·24). School-based interventions with parental involvement (g = 0·59), nutrition education (g = 0·59) and focus on individual participants yielded a larger effect size compared with their counterparts despite the lack of a substantial subgroup difference.
Table 2.
Subgroup analyses of school-based weight management interventions
| Subgroups | No of studies (Ref) | No of participants (intervention/control) | g | 95 % CI | Within-group Q | P | Subgroup difference Q | P | |
|---|---|---|---|---|---|---|---|---|---|
| Comparators | Passive comparator | 6 (51–53,55,58,59,62) | 561/604 | 0·73 | –1·19, 0·27 | 71·52 | <0·01‡ | ||
| Active comparator | 6 (54,56,57,60,61,63) | 306/284 | 0·28 | –0·60, 0·04 | 21·97 | <0·01‡ | 2·44 | 0·12 | |
| Counselling | With counselling | 5 (52–54,60,62) | 266/263 | 0·43 | –0·60, –0·25 | 4·21 | 0·38 | ||
| Without counselling | 7 (51,55–59,63) | 601/625 | 0·59 | –1·09, –0·09 | 103·94 | <0·01‡ | 0·37 | 0·55 | |
| Curriculum | During school | 5 (54,57,58,61,62) | 305/275 | 0·49 | –1·03, –0·05 | 50·77 | <0·01‡ | ||
| After school | 4 (51–53,55,63) | 418/452 | 0·39 | –0·67, –0·11 | 11·28 | <0·05† | |||
| During and after school | 2 (59,60) | 144/161 | 0·86 | –2·09, 0·36 | 25·09 | <0·01‡ | 0·61 | 0·74 | |
| Economies | Lower-middle to upper-middle economies | 5 (51–53,58,59,62) | 450/460 | 0·84 | –1·34, –0·33 | 60·70 | <0·01‡ | ||
| High-income economies | 7 (54–57,60,61,63) | 417/428 | 0·27 | –0·54, 0·01 | 22·01 | <0·01‡ | 3·81 | < 0·1* | |
| Intervention length (months) | 6 months or less | 6 (51,54,58,59,61,63) | 440/457 | 0·79 | –1·25, –0·32 | 67·16 | <0·01‡ | ||
| More than 6 months | 6 (52,53,55–57,60,62) | 427/431 | 0·24 | –0·48, –0·00 | 17·91 | <0·01‡ | 4·14 | 0·04† | |
| Focus of intervention | Individual | 6 (54,56,58,60,61,63) | 262/266 | 0·59 | –0·99, –0·19 | 29·56 | <0·01‡ | ||
| Group | 6 (51–53,55,57,59,62) | 605/622 | 0·46 | –0·93, 0·01 | 72·73 | <0·01‡ | 0·18 | 0·67 | |
| Number of sessions | 40 sessions or less | 7 (51,54,57,58,61–63) | 503/479 | 0·50 | –0·91, –0·09 | 59·49 | <0·01‡ | ||
| More than 40 sessions | 5 (52,53,55,56,59,60) | 364/409 | 0·54 | –1·03, –0·06 | 44·47 | <0·01‡ | 0·02 | 0·89 | |
| Nutrition education | With nutrition education | 9 (51–53,55–59,62,63) | 729/750 | 0·59 | –0·97, –0·20 | 104·64 | <0·01‡ | ||
| Without nutrition education | 3 (54,60,61) | 138/138 | 0·31 | –0·55, –0·06 | 2·01 | 0·37 | 1·43 | 0·23 | |
| Parental involvement | No parental involvement | 5 (54,57,58,60,61) | 318/292 | 0·42 | –0·96, 0·13 | 49·92 | <0·01‡ | ||
| Parental involvement | 7 (51–53,55,56,59,62,63) | 549/596 | 0·59 | –0·95, –0·24 | 55·36 | <0·01‡ | 0·29 | 0·59 | |
| Physical activity | With physical activity | 9 (51–53,55–57,59,60,62,63) | 715/739 | 0·45 | –0·79, –0·12 | 79·27 | <0·01‡ | ||
| Without physical activity | 3 (54,58,61) | 152/149 | 0·71 | –1·43, 0·01 | 19·92 | <0·01‡ | 0·40 | 0·53 | |
| Professional | Medical and health science professionals | 8 (51–56,59–61) | 255/235 | 0·45 | –0·76, –0·14 | 54·74 | <0·01‡ | ||
| Educators and trained staff | 4 (57,58,62,63) | 612/653 | 0·67 | –1·35, 0·01 | 53·19 | <0·01‡ | 0·32 | < 0·57 | |
| Size per cluster | 25 participants or less | 7 (51–54,56,60,61,63) | 445/446 | 0·38 | –0·60, –0·17 | 12·49 | <0·1* | ||
| More than 25 participants | 5 (55,57–59,62) | 422/442 | 0·69 | –1·34, –0·03 | 108·20 | <0·01‡ | 0·74 | 0·39 | |
| Theoretical framework | With theoretical framework | 9 (52–54,56–58,60–63) | 502/477 | 0·48 | –0·80, –0·17 | 57·78 | <0·01‡ | ||
| Without theoretical framework | 3 (51,55,59) | 365/411 | 0·62 | –1·46, 0·22 | 50·29 | <0·01‡ | 0·09 | 0·77 |
P < 0·1.
P < 0·05.
P < 0·01.
Univariate analysis observed an increase in BMI outcomes (
 = 0·09; 95 % CI 0·00, 0·19; P = 0·046) for every month of increase in trial duration. The univariate analysis suggested a decrease in BMI outcomes (
= 0·09; 95 % CI 0·00, 0·19; P = 0·046) for every month of increase in trial duration. The univariate analysis suggested a decrease in BMI outcomes (
 = 0·55; 95 % CI –1·08, –0·03; P = 0·039) for weight management interventions delivered in lower-middle to upper-middle economies compared with those delivered in high-income economies (Table 3). The two covariates were incorporated in the multivariate meta-regression model and explained almost half of the heterogeneity (R2 = 41·9 %, P = 0·03).
= 0·55; 95 % CI –1·08, –0·03; P = 0·039) for weight management interventions delivered in lower-middle to upper-middle economies compared with those delivered in high-income economies (Table 3). The two covariates were incorporated in the multivariate meta-regression model and explained almost half of the heterogeneity (R2 = 41·9 %, P = 0·03).
Table 3.
Results of univariate and multivariate meta-regression
| Independent variable (units) | Univariate meta-regression | Multivariate meta-regression* | ||||||
|---|---|---|---|---|---|---|---|---|

|
se | 95 % CI | P | Adjusted

|
se | 95 % CI | P | |
| Year of publication (years) | −0·04 | 0·35 | −0·11, 0·02 | 0·20 | ||||
| Economies (based on World Bank) | ||||||||
| High-income economies (Ref) | ||||||||
| Lower-middle to upper-middle economies | −0·55 | 0·26 | −1·08, –0·03 | 0·04† | −0·45 | 0·25 | −0·94, 0·05 | 0·08 |
| Duration of trial (months) | 0·09 | 0·47 | 0·00, 0·19 | 0·046† | 0·08 | 0·04 | −0·01, 0·16 | 0·09 |
| Risk of bias (RoB 2.0) | −0·16 | 0·32 | −0·78, 0·46 | 0·62 | ||||
| Mean age of sample (year) | 0·03 | 0·06 | −0·09, 0·16 | 0·61 | ||||
| Size of cluster | −0·01 | 0·01 | −0·03, 0·01 | 0·29 | ||||
| Total sample size | 0·00 | 0·00 | −0·00, 0·00 | 0·85 | ||||
| Total clusters | 0·00 | 0·04 | −0·08, 0·09 | 0·95 | ||||
| Total female recruited (%) | 0·00 | 0·01 | −0·01, 0·03 | 0·36 | ||||
| Focus of intervention | ||||||||
| Group (Ref) | ||||||||
| Individual | −0·13 | 0·32 | −0·75, 0·49 | 0·67 | ||||
| Professional | ||||||||
| Medical and health science professionals (Ref) | ||||||||
| Educators and trained staff | −0·21 | 0·32 | −0·85, 0·43 | 0·52 | ||||
| Total no. of Session | −0·00 | 0·00 | −0·01, 0·01 | 0·74 | ||||
| Physical activity | ||||||||
| With physical activity (Ref) | ||||||||
| Without physical activity | −0·26 | 0·36 | −0·97, 0·45 | 0·47 | ||||
| Counselling | ||||||||
| Without counselling (Ref) | ||||||||
| With counselling | 0·17 | 0·32 | −0·45, 0·79 | 0·60 | ||||
| Curriculum | ||||||||
| During school hours (Ref) | ||||||||
| After school hours | 0·08 | 0·35 | −0·60, 0·76 | 0·81 | ||||
| During and after school hours | −0·38 | 0·46 | −1·28, 0·51 | 0·40 | ||||
| Nutrition Education | ||||||||
| With nutrition education (Ref) | ||||||||
| Without nutrition education | 0·27 | 0·36 | −0·43, 0·97 | 0·45 | ||||
| Parental involvement | ||||||||
| With parental involvement (Ref) | ||||||||
| No Parental Involvement | 0·18 | 0·32 | −0·44, 0·80 | 0·57 | ||||
Ref, Reference.
Explained variance, R2 = 41·20 %, P = 0·018;
 -coefficient.
-coefficient.
P < 0·05.
Seven selected trials assessed thirteen secondary outcomes (see online supplementary material, Supplemental Table S6). Under nutrition outcomes, a significantly lower energy intake of 50·09 kcal (95 % CI –79·3, –20·9), favouring school-based interventions, was observed compared with controls. A very large effect on increasing fruit and vegetable intake (g = 2·55) and a large effect on decreasing junk food intake (g = 1·05) were observed, favouring school-based interventions compared with controls. A large effect was observed favouring school-based interventions for dietary self-efficacy (g = 0·86) under the category of psychosocial-related outcomes.
Discussion
This meta-analysis quantitatively synthesised the body of evidence of twelve cluster-RCT examining the effects of school-based interventions for the treatment of childhood obesity. The result of the meta-analysis suggests that school-based interventions are possible approaches for the treatment for childhood obesity with effectiveness comparable to other meta-analytic reviews involving behavioural interventions(64) and lifestyle interventions(65). Subgroup analyses showed greater effectiveness of brief school-based interventions and interventions conducted in lower-middle to upper-middle economies. Meta-analyses of the secondary outcomes found school-based interventions resulted in positive behavioural changes of lower energetic consumption, reduced junk food intake and a greater intake of fruits and vegetables.
Consistent with other meta-analytic reviews on the treatment of paediatric obesity(9,64) and school-based interventions(27), the subgroup analysis of this review indicated that brief school-based interventions of 6 months or shorter observed a greater reduction in BMI outcomes. In addition, this review found a positive association between trial duration and BMI outcomes, which suggests the potential effectiveness of school-based obesity treatment during the initial phase. The lower reduction in BMI outcomes for obesity treatment trials beyond 6 months may not be attributed to the failure of the intervention, but rather to the weight regain following weight loss due to physiological adaptations(66), and the seasonal increases in BMI during school holidays(67). This stresses the need for interventions to focus on the maintenance of weight reduction(9).
Despite school-based interventions being placed in a unique position to allow children and adolescents to be monitored for any possible relapse throughout the schooling years, the degree of attrition varied from 0 % to 66·9 % between trials and three trials reported the longest trial duration of only 1 year(56,57,62). Additionally, trials reported challenges in implementing school-based interventions due to the lack of prioritisation of attending intervention sessions over supplementary lessons after school(57,59), and a perception that participants lacked interest in addressing obesity(55). Trials which reported no attrition integrated the intervention into existing school hours and conducted sessions during non-essential classes(60,61), and after-school care settings through active video games to sustain participants’ interest(63). Partnership between healthcare providers and stakeholders in education is integral to ensure interventions for the treatment of childhood obesity are sustained throughout the schooling years(14).
To a certain extent, the duration of the intervention and the type of economies where the trial was conducted explained the substantial statistical heterogeneity amongst the pooled trials. Trials in lower-middle to upper-middle income economies had a larger effect where the control group received no intervention or utilised a wait-list control(51–53,58,59,63). This finding was consistent with the previous Cochrane review, where the subgroup analysis found larger effects when no interventions were delivered to the control group and a smaller effect when the control group received an active intervention(8). The findings from this review of selecting trials using a cluster-RCT design likely mirrored the standard of care of public health programmes available in schools to address childhood obesity in the respective economies. With the exception of one trial(55), the control group of trials in high-income economies received dietary and physical activity sessions(56,57,63), or leveraged on existing healthcare services in schools for weight management(54,60,61) which resulted in a smaller effect size. The observed differences in the standard of usual care suggest separate immediate approaches to address childhood obesity. For lower- to middle-income economies, resources would be needed to establish evidence-based interventions using approaches adapted to the existing school systems to ensure programme sustainability, as part of the universal healthcare coverage(12). High-income economies should make alterations to strengthen existing school-based interventions and ensure up-to-date practices in reducing childhood obesity.
School-based interventions for the treatment of childhood obesity utilised a combination of nutrition education, physical activity, counselling and parental involvement. Determining the effectiveness of a particular component was not possible considering the clinical heterogeneity amongst the trials. Consistent with other meta-analytic reviews on school-based interventions(26–28,40–43) and treatment on childhood obesity(8,9,64), this review encountered statistical heterogeneity among the pooled trials. Attempts were made to explore the heterogeneity, but to a large extent, the variation remains unexplained and requires further investigation.
Interestingly, the subgroup analysis revealed that the use of educators and trained staff had a large effect on the reduction of BMI outcomes. Although more studies are needed to ascertain the effectiveness of school-based interventions conducted by educators and trained staff, this approach has the potential for scalability to provide universal healthcare coverage for the treatment of childhood obesity(17), given the shortage of healthcare professionals(68). Nonetheless, professionals in medical and health science can play a pivotal role in weight management because of their in-depth understanding of healthcare knowledge and, more importantly, the understanding of the social determinants of health(69). The trials that used professionals in medical and health science were able to provide individual problem-solving sessions and tailor the healthcare interventions to ensure participation in weight management(54,60,61).
The strength of this review includes the use of a meta-analytic approach to synthesise the evidence for the effectiveness of school-based intervention for the treatment of childhood obesity from eight databases using a comprehensive and rigorous search strategy. However, this review has limitations. First, only trials published in English were included with evidence limited to USA, Europe and Asia, and lower-middle to high-income economies. Second, the quality of evidence is low, and substantial statistical heterogeneity was found amongst the included trials, with a great portion of the heterogeneity remaining unexplained. Third, the results of this meta-analysis are subject to ecological fallacy and/or Simpson’s paradox as with any meta-analysis(70). Hence, the results need to be interpreted with caution.
Given the low quality of evidence for school-based intervention for the treatment of childhood obesity, this review has essential implications for future research. More high-quality cluster-RCT with longer follow-up are needed to determine the optimal duration of childhood obesity treatment and maintenance, and the appropriate combination of components. Special attention needs to be given to the randomisation process for cluster-RCT with an emphasis on missing data management, including the use of an intention-to-treat analysis according to the recommendations of the Consolidated Standards of Reporting Trials (CONSORT) for cluster-RCT(71). The review highlights the need to conduct trials using the cluster-RCT design to allow better generalisation of results in the real-world setting. These cluster-RCT should have multiple clusters to allow a comparison of the interventions delivered by professionals in medical and health science against those delivered by educators and trained staff and to identify the maximum number of participants for each staff to deliver treatment successfully. A cost-effectiveness analysis would provide essential knowledge for scaled-up interventions, especially in developing countries. Such knowledge would allow the achievement of universal healthcare coverage, one of the UN’ Sustainable Developmental Goals(72).
The findings of this review highlight the potential for school-based interventions in treating childhood obesity. This review provides valuable information for policymakers regarding contextual factors designing school-based interventions, with consideration on the contextual appropriateness to ensure the sustainability of the programme. Ideally, the school-based intervention should be incorporated into existing systems by conducting it during school curriculum hours or during an after-school programme, to reduce the attrition of participants, and involving professionals in medical and health sciences in the delivery of the programme. Where resources are limited, involving educators and staff trained to deliver treatment of childhood obesity may be a possibility. For practitioners, delivering school-based interventions should utilise a combination of nutrition, physical activity, counselling and parental involvement components. Follow-up is required to monitor for weight regain and to engage children during school holidays.
In conclusion, school-based interventions for the treatment of childhood obesity can potentially reduce BMI and BMI z-score outcomes through the use of a variety of components, such as physical activity, nutrition education, counselling and parental involvement. Findings from this review suggest that the duration of the intervention is negatively associated with the effectiveness of the intervention and that the type of economy where the trial is conducted contributes to the heterogeneity of the meta-analysis. Given the low quality of evidence, high-quality trials are needed with longer periods of follow-up to better compare the cost-effectiveness between the types of professions delivering school-based interventions. School-based intervention is a possible approach to provide universal healthcare to end childhood obesity.
Acknowledgements
Acknowledgements: None. Financial support: This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors. Conflict of interest: The authors declare no competing interests. Authorship: T.J.H.H. and L.Y. conceptualised and designed the study. T.J.H.H. and L.J.C. conducted the systematic literature search. T.J.H.H., L.J.C. and L.Y. performed the title and abstract screening, data extraction and data analysis. T.J.H.H., L.J.C. and L.Y. participated in the reference editing. T.J.H.H. wrote and formatted the article, and all authors read and approved the final version of the article. Ethics of human subject participation: Not applicable.
Supplementary material
For supplementary material accompanying this paper visit https://doi.org/10.1017/S1368980021001117.
click here to view supplementary material
References
- 1. Abarca-Gómez L, Abdeen ZA, Hamid ZA et al. (2017) Worldwide trends in body-mass index, underweight, overweight, obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128.9 million children, adolescents, adults. Lancet 390, 2627–2642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Cole TJ & Lobstein T (2012) Extended international (IOTF) body mass index cut-offs for thinness, overweight and obesity. Pediatr Obes 7, 284–294. [DOI] [PubMed] [Google Scholar]
- 3. Ward ZJ, Long MW, Resch SC et al. (2017) Simulation of growth trajectories of childhood obesity into adulthood. N Engl J Med 377, 2145–2153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Juonala M, Magnussen CG, Berenson GS et al. (2011) Childhood adiposity, adult adiposity, cardiovascular risk factors. N Engl J Med 365, 1876–1885. [DOI] [PubMed] [Google Scholar]
- 5. Li S, Chen W, Srinivasan SR et al. (2012) Relation of childhood obesity/cardiometabolic phenotypes to adult cardiometabolic profile: the Bogalusa Heart Study. Am J Epidemiol 176, S142–S149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Tirosh A, Shai I, Afek A et al. (2011) Adolescent BMI trajectory, risk of diabetes versus coronary disease. N Engl J Med 364, 1315–1325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Baker JL, Olsen LW & Sørensen TIA (2007) Childhood body-mass index and the risk of coronary heart disease in adulthood. N Engl J Med 357, 2329–2337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Al-Khudairy L, Loveman E, Colquitt JL et al. (2017) Diet, physical activity and behavioural interventions for the treatment of overweight or obese adolescents aged 12 to 17 years. Cochrane Database Syst Rev 6, CD012691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Mead E, Brown T, Rees K et al. (2017) Diet, physical activity, behavioural interventions for the treatment of overweight or obese children from the age of 6 to 11 years. Cochrane Database Syst Rev. Published online: 22 June 2017. doi: 10.1002/14651858.CD012651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Moores CJ, Bell LK, Miller J et al. (2018) A systematic review of community-based interventions for the treatment of adolescents with overweight, obesity. Obes Rev 19, 698–715. [DOI] [PubMed] [Google Scholar]
- 11. Sargent GM, Pilotto LS & Baur LA (2011) Components of primary care interventions to treat childhood overweight and obesity: a systematic review of effect. Obes Rev 12, e219–e235. [DOI] [PubMed] [Google Scholar]
- 12. World Health Organization (2016) Consideration of the Evidence on Childhood Obesity for the Commission on Ending Childhood Obesity: Report of the ad hoc Working Group on Science and Evidence for Ending Childhood Obesity. Geneva: WHO. [Google Scholar]
- 13. Aarons GA, Sklar M, Mustanski B et al. (2017) “Scaling-out” evidence-based interventions to new populations or new health care delivery systems. Implementation Sci 12, 111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Dietz WH, Baur LA, Hall K et al. (2015) Management of obesity: improvement of health-care training, systems for prevention, care. Lancet 385, 2521–2533. [DOI] [PubMed] [Google Scholar]
- 15. Cook AJ, Delong E, Murray DM et al. (2016) Statistical lessons learned for designing cluster randomized pragmatic clinical trials from the NIH Health Care Systems Collaboratory Biostatistics, Design Core. Clin Trials 13, 504–512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Freemantle N & Strack T (2010) Real-world effectiveness of new medicines should be evaluated by appropriately designed clinical trials. J Clin Epidemiol 63, 1053–1058. [DOI] [PubMed] [Google Scholar]
- 17. World Health Organization (2016) Report of the Commission on Ending Childhood Obesity. Geneva: WHO. [Google Scholar]
- 18. Patton GC, Sawyer SM, Santelli JS et al. (2016) Our future: a Lancet commission on adolescent health and wellbeing. Lancet 387, 2423–2478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Gortmaker SL, Swinburn BA, Levy D et al. (2011) Changing the future of obesity: science, policy, action. Lancet 378, 838–847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Safron M, Cislak A, Gaspar T et al. (2011) Effects of school-based interventions targeting obesity-related behaviors, body weight change: a systematic umbrella review. Behav Med 37, 15–25. [DOI] [PubMed] [Google Scholar]
- 21. De Bourdeaudhuij I, Van Cauwenberghe E, Spittaels H et al. (2011) School-based interventions promoting both physical activity and healthy eating in Europe: a systematic review within the HOPE project. Obes Rev 12, 205–216. [DOI] [PubMed] [Google Scholar]
- 22. Smith J, Wohlstetter P, Kuzin CA et al. (2011) Parent involvement in urban charter schools: new strategies for increasing participation. Sch Community J 21, 71–94. [Google Scholar]
- 23. Ottova V, Erhart M, Rajmil L et al. (2012) Overweight and its impact on the health-related quality of life in children and adolescents: results from the European KIDSCREEN survey. Qual Life Res 21, 59–69. [DOI] [PubMed] [Google Scholar]
- 24. Analitis F, Velderman MK, Ravens-Sieberer U et al. (2009) Being bullied: associated factors in children and adolescents 8 to 18 years old in 11 European countries. Pediatrics 123, 569–577. [DOI] [PubMed] [Google Scholar]
- 25. King JE, Jebeile H, Garnett SP et al. (2020) Physical activity based pediatric obesity treatment, depression, self-esteem and body image: a systematic review with meta-analysis. Mental Health Phys Activity 19, 100342. [Google Scholar]
- 26. Gonzalez-Suarez C, Worley A, Grimmer-Somers K et al. (2009) School-based interventions on childhood obesity: a meta-analysis. Am J Prev Med 37, 418–427. [DOI] [PubMed] [Google Scholar]
- 27. Sbruzzi G, Eibel B, Barbiero SM et al. (2013) Educational interventions in childhood obesity: A systematic review with meta-analysis of randomized clinical trials. Prev Med 56, 254–264. [DOI] [PubMed] [Google Scholar]
- 28. Schroeder K, Travers J & Smaldone A (2016) Are school nurses an overlooked resource in reducing childhood obesity? A systematic review and meta-analysis. J Sch Health 86, 309–321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Moher D, Liberati A, Tetzlaff J et al. (2009) Preferred reporting items for systematic reviews, meta-analyses: the PRISMA statement. J Clin Epidemiol 62, 1006–1012. [DOI] [PubMed] [Google Scholar]
- 30. Higgins JPT, Thomas J, Chandler J et al. (2019) Cochrane Handbook for Systematic Reviews of Interventions. Chichester: John Wiley & Sons. [Google Scholar]
- 31. Sterne JAC, Savović J, Page MJ et al. (2019) RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ 366. [DOI] [PubMed] [Google Scholar]
- 32. Eldridge S, Campbell M, Campbell M et al. (2016) Revised Cochrane risk of bias tool for randomized trials (RoB 2.0): Additional considerations for cluster-randomized trials. https://drive.google.com/file/d/0B7IQVI0kum0kd2VaX1VrTkh1ZFk/view (accessed May 2020).
- 33. Guyatt GH, Oxman AD, Schünemann HJ et al. (2011) GRADE guidelines: a new series of articles in the Journal of Clinical Epidemiology. J Clin Epidemiol 64, 380–382. [DOI] [PubMed] [Google Scholar]
- 34. StataCorp (2019) Stata: Release 16. College Station, TX: StataCorp LLC. [Google Scholar]
- 35. StataCorp (2019) Stata Meta-Analysis Reference Manual. Texas: Stata Press. [Google Scholar]
- 36. Cole TJ, Faith MS, Pietrobelli A et al. (2005) What is the best measure of adiposity change in growing children: BMI, BMI%, BMI z-score or BMI centile? Eur J Clin Nutr 59, 419–425. [DOI] [PubMed] [Google Scholar]
- 37. Bayer O, Krüger H, Von Kries R et al. (2011) Factors associated with tracking of BMI: a meta-regression analysis on BMI tracking. Obesity 19, 1069–1076. [DOI] [PubMed] [Google Scholar]
- 38. Hedges LV & Olkin I (1985) Estimation of a single effect size: parametric and nonparametric methods. In Statistical Methods for Meta-Analysis, pp. 75–106 [Hedges LV & Olkin I, editors]. San Diego: Academic Press. [Google Scholar]
- 39. Borenstein M, Hedges LV, Higgins JPT et al. (2009) Fixed-Effect Versus Random-Effects Models. Introduction to Meta-Analysis. Chichester: John Wiley & Sons, Ltd. [Google Scholar]
- 40. Guerra PH, Nobre MRC, da Silveira JAC et al. (2014) School-based physical activity, nutritional education interventions on body mass index: a meta-analysis of randomised community trials — Project PANE. Prev Med 61, 81–89. [DOI] [PubMed] [Google Scholar]
- 41. Oosterhoff M, Joore M & Ferreira I (2016) The effects of school-based lifestyle interventions on body mass index and blood pressure: a multivariate multilevel meta-analysis of randomized controlled trials. Obes Rev 17, 1131–1153. [DOI] [PubMed] [Google Scholar]
- 42. Harris KC, Kuramoto LK, Schulzer M et al. (2009) Effect of school-based physical activity interventions on body mass index in children: a meta-analysis. Can Med Assoc J 180, 719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Lavelle HV, Mackay DF & Pell JP (2012) Systematic review and meta-analysis of school-based interventions to reduce body mass index. J Public Health 34, 360–369. [DOI] [PubMed] [Google Scholar]
- 44. Hedges LV & Olkin I (1990) Statistical Methods for MetaAnalysis. Orlando: Academic Press. [Google Scholar]
- 45. Veroniki AA, Jackson D, Viechtbauer W et al. (2016) Methods to estimate the between-study variance, its uncertainty in meta-analysis. Res Synthesis Meth 7, 55–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Lau J, Schmid CH & Chalmers TC (1995) Cumulative meta-analysis of clinical trials builds evidence for exemplary medical care. J Clin Epidemiol 48, 45–57. [DOI] [PubMed] [Google Scholar]
- 47. Higgins JP, Thompson SG, Deeks JJ et al. (2003) Measuring inconsistency in meta-analyses. BMJ 327, 557–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Higgins JPT, & Green S (2011) Cochrane Handbook for Systematic Reviews of Interventions The Cochrane Collaboration. https://training.cochrane.org/handbook/archive/v5.1/ (accessed May 2020).
- 49. World Bank (2020) World Bank Country and Lending Groups. https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups (accessed July 2020).
- 50. Ranganathan P, Pramesh CS & Aggarwal R (2017) Common pitfalls in statistical analysis: Logistic regression. Perspect Clin Res 8, 148–151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Amini M, Djazayery A, Majdzadeh R et al. (2016) A school-based intervention to reduce excess weight in overweight and obese primary school students. Biol Res Nurs 18, 531–540. [DOI] [PubMed] [Google Scholar]
- 52. Bagherniya M, Darani FM, Sharma M et al. (2018) Assessment of the efficacy of physical activity level and lifestyle behavior interventions applying social cognitive theory for overweight and obese girl adolescents. J Res Health Sci 18, e00409. [PMC free article] [PubMed] [Google Scholar]
- 53. Bagherniya M, Sharma M, Mostafavi DF et al. (2017) School-Based nutrition education intervention using social cognitive theory for overweight, obese Iranian adolescent girls: a cluster randomized controlled trial. Int Q Community Health Educ 38, 37–45. [DOI] [PubMed] [Google Scholar]
- 54. Freira S, Lemos MS, Fonseca H et al. (2018) Anthropometric outcomes of a motivational interviewing school-based randomized trial involving adolescents with overweight. Eur J Pediatr 1–10. [DOI] [PubMed] [Google Scholar]
- 55. Graf C, Koch B, Bjarnason-Wehrens B et al. (2006) Who benefits from intervention in, as opposed to screening of, overweight, obese children? Cardiol Young 16, 474–480. [DOI] [PubMed] [Google Scholar]
- 56. Grey M, Berry D, Davidson M et al. (2004) Preliminary testing of a program to prevent type 2 diabetes among high-risk youth. J Sch Health 74, 10–15. [DOI] [PubMed] [Google Scholar]
- 57. Grey M, Jaser SS, Holl MG et al. (2009) A multifaceted school-based intervention to reduce risk for type 2 diabetes in at-risk youth. Prev Med 49, 122–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Mayurachat K, Warunee F, Jutamas C et al. (2013) An intervention study of changing eating behaviors and reducing weight in Thai children aged 10–12. Pac Rim Int J Nursing Res 17, 317–328. [Google Scholar]
- 59. Nayak BS & Bhat VH (2016) School based multicomponent intervention for obese children in Udupi district, South India – a randomized controlled trial. J Clin Diagn Res: JCDR 10, SC24–SC28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Pbert L, Druker S, Barton B et al. (2016) A School-Based program for overweight, obese adolescents: a randomized controlled trial. J Sch Health 86, 699–708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Pbert L, Druker S, Gapinski MA et al. (2013) A school nurse-delivered intervention for overweight and obese adolescents. J Sch Health 83, 182–193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Toruner EK & Savaser S (2010) A controlled evaluation of a school-based obesity prevention in Turkish school children. J Sch Nurs 26, 473–482. [DOI] [PubMed] [Google Scholar]
- 63. Trost SG, Sundal D, Foster GD et al. (2014) Effects of a pediatric weight management program with and without active video games a randomized trial. JAMA Pediatr 168, 407–413. [DOI] [PubMed] [Google Scholar]
- 64. Peirson L, Fitzpatrick-Lewis D, Morrison K et al. (2015) Treatment of overweight and obesity in children and youth: a systematic review and meta-analysis. CMAJ Open 3, E35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Kitzmann KM, Dalton Iii WT, Stanley CM et al. (2010) Lifestyle interventions for youth who are overweight: a meta-analytic review. Health Psychol 29, 91. [DOI] [PubMed] [Google Scholar]
- 66. Greenway FL (2015) Physiological adaptations to weight loss and factors favouring weight regain. Int J Obes 39, 1188–1196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Baranowski T, O’Connor T, Johnston C et al. (2013) School year versus summer differences in child weight gain: a narrative review. Child Obes 10, 18–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Tsolekile LP, Abrahams-Gessel S & Puoane T (2015) Healthcare professional shortage and task-shifting to prevent cardiovascular disease: implications for low- and middle-income countries. Curr Cardiol Rep 17, 115. [DOI] [PubMed] [Google Scholar]
- 69. Schroeder K, McCormick R, Perez A et al. (2018) The role and impact of community health workers in childhood obesity interventions: a systematic review and meta-analysis. Obes Rev 19, 1371–1384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Cooper H & Patall EA (2009) The relative benefits of meta-analysis conducted with individual participant data versus aggregated data. Psychol Meth 14, 165–176. [DOI] [PubMed] [Google Scholar]
- 71. Campbell MK, Piaggio G, Elbourne DR et al. (2012) Consort 2010 statement: extension to cluster randomised trials. BMJ 345, e5661. [DOI] [PubMed] [Google Scholar]
- 72. Desa UN (2016) Transforming our world: The 2030 agenda for sustainable development. https://www.unfpa.org/sites/default/files/resource-pdf/Resolution_A_RES_70_1_EN.pdf (accessed June 2020).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
For supplementary material accompanying this paper visit https://doi.org/10.1017/S1368980021001117.
click here to view supplementary material