Abstract
Pregnancy is a complex biological process. The establishment and maintenance of foetal–maternal interface are pivotal events. Decidual immune cells and inflammatory cytokines play indispensable roles in the foetal–maternal interface. The disfunction of decidual immune cells leads to adverse pregnancy outcome. Tumour necrosis factor (TNF)-α, a common inflammatory cytokine, has critical roles in different stages of normal pregnancy process. However, the relationship between the disorder of TNF-α and adverse pregnancy outcomes, including preeclampsia (PE), intrauterine growth restriction (IUGR), spontaneous abortion (SA), preterm birth and so on, is still indefinite. In this review, we thoroughly reviewed the effect of TNF-α disorder on pathological conditions. Moreover, we summarized the reports about the adverse pregnancy outcomes (PE, IUGR, SA and preterm birth) of using anti-TNF-α drugs (infliximab, etanercept and adalimumab, certolizumab and golimumab) currently in the clinical studies. Overall, IUGR, SA and preterm birth are the most common adverse pregnancy outcomes of anti-TNF-α drugs. Our review may provide insight for the immunological treatment of pregnancy-related complication, and help practitioners make informed decisions based on the current evidences.
Key words: Adverse pregnancy outcomes, anti-TNF-α drugs, TNF-α receptor, TNF-α
1. Introduction
The successful implantation of semi-allograft embryos into the endometrium of the parent body without being rejected by the mother depends on the maintenance of inflammatory and immune microenvironment of the foetal–maternal interface. The establishment and maintenance of foetal–maternal microenvironment require the function of immune cells and diverse cytokines (Refs 1, 2). The function of decidual immune cells has been thoroughly investigated. However, the role of inflammatory cytokines, especially tumour necrosis factor (TNF)-α, in foetal–maternal interface is still indefinite. TNF-α is a pivotal cytokine in immunological and inflammatory conditions at the foetal–maternal interface. In the first trimester of pregnancy and childbirth period, TNF-α mediated moderate proinflammatory and immune response, contributing to the embryo transfer, trophoblast cell function and labour, while in the middle and late trimester of pregnancy inhibitory inflammatory response makes for embryonic development (Refs 3, 4). Emerging studies evidenced that the imbalance of TNF-α in the foetal–maternal interface was related to adverse pregnancy outcomes, including preeclampsia (PE), intrauterine growth restriction (IUGR), spontaneous abortion (SA), preterm birth, etc. (Refs 5, 6).
2. TNF-α and TNF-R-dependent signalling
TNF-α gene, locating on chromosome 6p21.3, spans approximately 3 kb and has four exons. The fourth exon encodes for more than 80% of the secreted protein. TNF-α mainly comes from activated macrophages and T-lymphocytes (Ref. 7). Two forms of TNF-α co-exist in mammals, which are soluble TNF-α (sTNF-α) and transmembrane TNF-α (mTNF-α) (Ref. 8). mTNF-α, namely TNF-α precursor (233 amino acid residues (26 kDa)), is mainly synthesised by activated macrophages and transferred onto the cytomembrane. Subsequently, mTNF-α is cleaved off by metalloproteinases or TNF-α-converting enzyme (TACE, also named ADAM17) to release sTNF-α (157 amino acid residues (17 kDa)) from cells in the form of monomer and trimer (Ref. 9). sTNF-α primarily binds with TNF-α receptors 1 (TNF-R1) to medicate inflammatory immune response, while mTNF-α mainly interacts with TNF-α receptors 2 (TNF-R2) to involve in the cellular proliferation, survival and other biological effects. Meanwhile, mTNF-α cannot only act as a ligand binding with TNF-Rs in the manner of cell–cell contact, but also serves as a receptor transmitting outside-to-inside (reverse) signals back into the mTNF-α-bearing cells (Ref. 10). TNF-R1 (55 kDa), containing conserved death-domain (DD) motifs, and constitutively expressed in various cells, can be bound and activated by sTNF-α and mTNF-α. Concomitantly, TNF-R2 (75 kDa) contains one or more TNF-R-associated factor (TRAF)-interacting motifs, mainly exists in restricted neurons, immune cells and endothelial cells, and can only be activated primarily by mTNF-α (Ref. 11). At the foetal–maternal interface, TNF regulates the function of trophoblast cells and immune cells, including cell apoptosis, proliferation, inflammation, immune and tissue remodelling in TNF-R1 and TNF-R2-dependent signalling manners (Refs 12, 13).
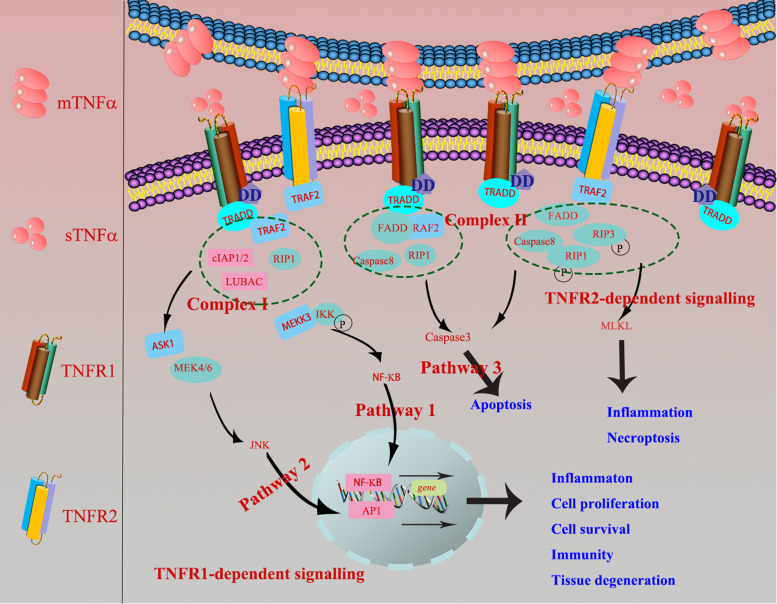
In terms of TNF-R1-dependent signalling, once binding with mTNF-α or sTNF-α, TNF-R1 recruits the adaptor protein TNF-R-associated DD (TRADD) or Fas-associating protein with a novel death domain (FFADD) via its DD motifs. Subsequently, it recruits complex I, namely serine/threonine kinase receptor interacting protein-1 (RIP-1), TRAF-2, as well as Cellular inhibitor of apoptosis 1 (cIAP1) and cIAP2. Then, it activates Nuclear factor kappaB (NF-κB) and c-Jun N-terminal kinase/activator protien-1 (JNK/AP1) signalling pathways and medicates the expression of targeted genes, finally involves in various biological processes, inducing inflammation, tissue degeneration, host defence, cell proliferation, cell survival and immunity (Refs 14, 15). Besides, TRADD can also recruit and form the complex II (FADD, RIP-A, TRAF-2 and caspase 8) to finally activate caspase 3 eliciting cell apoptosis. When it comes to TNF-R2-dependent signalling pathway, TNF-R2, primarily recruiting TRAF-2 via its TRAF domain, is restricted to bind with mTNF-α (Fig. 1), and further recruited the complex II and activated apoptosis, inflammation, cell migration and necroptosis (Ref. 16).
Fig. 1.
TNF-R1-dependent signalling: once TNF-R1 binds mTNF-α or sTNF-α, it recruits the adaptor protein TRADD or FFADD via its DD motifs. Subsequently, it recruits complex I, namely serine/threonine kinase receptor interacting protein-1 (RIP-1), TNF-R-associated factor 2 (TRAF-2), as well as cIAP1 and cIAP2. Then, it activates NF-κB and JNK/AP1 signalling pathways and medicates the expression of targeted genes, finally involves in various biological processes, inducing inflammation, tissue degeneration, host defence, cell proliferation, cell survival and immunity. Besides, TRADD can also recruit and form the complex II (FADD, RIP-A, TRAF-2 and caspase 8) to finally activate caspase 3 eliciting cell apoptosis (Ref. 2). TNF-R2-dependent signalling: TNF-R2 is restricted to bind with mTNF-α, primarily recruiting TRAF-2 via its TRAF domain, which further causes the recruitment of complex II and activation of apoptosis, inflammation and necroptosis.
3. TNF-α in adverse pregnancy outcomes
3.1. TNF-α and preeclampsia
PE is a characteristic complication of pregnancy and mainly occurs after 20 weeks of gestation, with a worldwide incidence rate of 5–8%. PE is one of the leading causes of maternal/foetal death during the gestation period (Refs 17, 18). The clinical manifestations of mothers are newly occurring hypertension and proteinuria, severely affecting the heart, liver, brain, lung, blood vessels and other organs (Refs 19, 20). Placental ischaemia and hypoxia induce the release of bioactive factors, including proinflammatory factors (TNF-α, interleukin (IL)-1β, IL-6, IL-12, interferon-λ), mediating extensive damages to the maternal vascular endothelium and causing the typical symptoms of PE. The pathogenesis of PE can be summarized as insufficient trophoblast invasion, disorder of systemic inflammatory response and immune regulation, and the dysfunction of angiogenesis and endothelial cells (Refs 21, 22).
Gelber et al. demonstrated that the increase of TNF-α may induce a secondary decrease in vascular endothelial growth factor (VEGF) and other angiogenic factors and eventually lead to placental dysplasia (Ref. 23). In addition, TNF-α can increase the cytotoxicity of natural killer cells (NK cells), trophoblast death and endothelial activation in the placenta, aggravate the dysfunction of endothelial cells, increasing adhesion molecules release and endothelial cells permeability in the cardiovascular system (Ref. 24). Another important role of TNF-α in PE patients is to stimulate B cells to produce autoantibodies against the angiotensin II type 1 (AT1) receptor. By binding and activating the AT1 receptor, TNF-α leads to the chronotropic response of heart, causing increased blood pressure (Ref. 25). In summary, the imbalance of foetal–maternal interface microenvironment caused by the change of TNF-α levels is closely related to the occurrence and development of PE.
3.2. TNF-α and intrauterine growth restriction
IUGR is defined as an impairment of the foetus's expected growth potential and an estimated foetal weight of less than 10% small for gestational age. Abnormalities in maternal nutrition, placental transport and the genetic potential of the foetus may lead to abnormal growth and development of the foetus.
Azizieh and Raghupathy et al. found that the expression of TNF-α in peripheral blood monocytes of IUGR patients was higher than that of normal pregnant women, illustrating the potential role of TNF-α in the occurrence of IUGR (Ref. 26). However, the specific mechanism of immunological studies about TNF-α in IUGR is limited. Foetal vascular disease is the pathogenic mechanism of IUGR. TNF-α directly damages endothelial cells, impairs the invasion and fusion of trophoblast cells (Refs 27, 28), and damages the remodelling of spiral arteries. In addition, TNF-α can also interfere with blood coagulation system, leading to placental thrombosis and aggravating placental hypoperfusion (Refs 29, 30). Therefore, these indicated that TNF-α is closely associated with IUGR and skeletal retardation. Elfayomy et al. demonstrated that Anti-Müllerian hormoneo (AMH), IL-6 and TNF-α in serum of IUGR were higher than that of normal pregnancy, which may serve as useful biochemical markers for IUGR. Nevertheless, reports about IUGR investigation are rare (Ref. 31). It is worth noting that more clinical studies are needed to identify them as diagnosis, treatment and prevention of biomarkers for IUGR. In mice, blocking TNF-α can improve spiral artery remodelling and pregnancy outcomes (Ref. 23). Therefore, TNF-α provides new options for the treatment and prevention of IUGR. At present, there have been only a few studies about the TNF family in IUGR, and the role of TNF in the pathogenesis of IUGR needs further investigation in the future.
3.3. TNF-α and spontaneous abortion
SA is one of the most common pregnancy complications, defined as the loss of a natural pregnancy before 20 weeks (Ref. 32). The epilogue of SA is complex and mainly includes genetic, anatomical, endocrine, immune, infection-related inflammation and psychological factors (Ref. 33). Given the postponement of the age of childbirth, changes in lifestyle and the influence of social and psychological factors, the incidence of SA is increasing year by year. The specific mechanism has not yet been fully clarified yet. In recent years, the relationship between the TNF-α and SA has attracted wide attention.
The abnormal expression of TNF-α is closely related to the occurrence of SA. For example, Jang et al. reported that TNF-α polymorphism is a genetic risk factor for SA, and TNF-α-863C > A variant is associated with an increased risk of SA (Ref. 34). In addition, the rate of SA in pregnant mouse models was observed to increase when the expression of TNF-α was upregulated (Ref. 35). At present, an increasing number of studies have shown that SA is associated with abnormal maternal immune function caused by the imbalance in Th1/Th2 and Th17/Treg ratio (Refs 36, 37). In addition, normal pregnancy involves complex interactions between the trophoblast, decidua and maternal immune cells. TNF-α also affects decidualization and function of decidual cells, thereby changing the microenvironment of foetal–maternal interface, thus mediating the occurrence of abortion. Fonseca et al. found that the high expression of TNF-α in decidual tissue of abortion can inhibit the differentiation of embryonic stem cells and impair decidualization, thus interfering with blastocyst implantation and/or pregnancy maintenance (Ref. 38). The latest research of Yang et al. showed that dNK cells highly express TNF-α in spontaneously aborted tissues, and TNF-α induces the upregulation of arylhydrocarbon receptor expression in dNK cells, thereby enhancing the cytotoxicity of decidual Natural Killer Cells (dNK cells) and making dNK cells develop an immune response to foetus, resulting in SA (Ref. 39). Further studies have found that reducing the cytotoxicity of dNK cells, thereby inhibiting the expression of Th1 cytokines, such as TNF-α, is conducive to creating a microenvironment at the foetal–maternal interface and maintaining pregnancy (Ref. 40). In addition, compared with normal pregnancy, the expression levels of TNF-α in peripheral blood and decidual tissue of patients with SA were abnormally increased, and TNF-α affects the function of decidual stromal cells by downregulating the expression of nucleotide oligomerisation domain 1, leading to SA (Refs 41, 42).
In conclusion, the abnormal upregulation of TNF-α expression can affect multiple key links in the normal pregnancy process. TNF-α mediates the occurrence of SA by affecting the balance of Th1/Th2 and Th17/Treg cells, endometrial decidualization, cytotoxicity of dNK cells and the function of decidual stromal cells. Further in-depth research on the specific mechanism of TNF-α-mediated SA will help reduce the incidence of SA and benefit women of childbearing age.
3.4. TNF-α and preterm birth
Preterm birth is defined as less than 37 full weeks or 259 full days of termination of pregnancy according to the WHO definition (Ref. 43). Generally speaking, preterm birth has a negative impact on the health of premature infants and causes a burden on the family of premature infants and society. Preterm birth is related to genetic factors, inflammation and immunity (Ref. 44). On the one hand, premature rupture of membranes (PROM) is one of the causes of premature delivery.
In a mouse model, upregulated TNF-α and IL-6 in placental tissue lead to PROM (Ref. 45). Wang et al. proved that the increase in the apoptosis of foetal membrane cells caused by TNF-α was related to PROM, further resulting in preterm birth (Ref. 46). On the other hand, abnormal uterine contractility also leads to premature birth. Many studies have demonstrated that TNF-α has a certain correlation with the contractility of the myometrium, mainly by affecting the expression of progesterone (PG) and Matrix Metallopeptidase 9 (MMP9). The increase in the expression and sensitivity of PG and MMP9 in the myometrium will lead to uterine contraction and delivery (Refs 47, 48). Specifically, TNF-α has been reported to reduce the activity and expression of NAD+-dependent 15-hydroxyprostaglandin dehydrogenase (PGDH) in trophoblast cells, resulting in maternal PE and premature delivery (Ref. 49). Recent advances have shown that the TNF family may regulate macrophage dysfunction leading to preterm birth, but the specific molecular mechanism needs further study.
3.5. TNF-α and other adverse pregnancy outcomes
Lan et al. reported that elevated levels of TNF-α and Th1/Th2 ratio are positive with embryo arrest rate (Ref. 50). Li et al. firstly found that TNF-α gene polymorphisms are associated with an increased risk of recurrent abortion (Ref. 51). Subsequently, other team further demonstrated the high expression of TNF-α in decidua tissue and peripheral blood of recurrent abortion (Ref. 41).
In conclusion, successful pregnancy requires foetal–maternal immune cross-talk between decidual immune cells and inflammatory cytokines. The dysregulation of TNF-α may leads to adverse pregnancy outcomes. During the pregnancy process, high TNF-α concentration not only increases the cytotoxicity of NK cells and stimulates B cells, but also breaks the balance of Th1/Th2 and Th17/Treg cells, increases trophoblast death, impairs its invasion and fusion, damages endothelial cells, and affects decidualization. Thus, above mechanisms induce pregnancy complications, namely, PE, IUGR, SA and preterm birth. Even though, the special mechanism of TNF-α needs further investigation.
4. Effect of anti-TNF-α drugs on adverse pregnancy outcomes
Rheumatoid arthritis (RA), inflammatory bowel disease (IBD), psoriatic arthritis (PsA), etc., are common inflammatory diseases. Women with chronic inflammatory diseases more likely suffer from adverse pregnancy outcomes. Specialists often propose that treatments are applied to limit the exacerbation of disease during pregnancy. For example, methotrexate (MTX) is the preferred drug for RA. However, MTX is a contraindicated drug during pregnancy owing to the teratogenicity and easily entering breast milk (Ref. 52). At present, anti-TNF-α drugs (infliximab (IFX), adalimumab (ADA), etanercept (ETA), golimumab and certolizumab) have been widely applied to clinical inflammatory diseases, such as Crohn's disease, ulcerative colitis, RA and so on. However, the influence of those drugs on adverse pregnancy outcomes for pregnant women with inflammatory diseases has hardly been explored. On the one side, the anti-TNF-α drugs cannot be interrupted especially in the acute phase of the inflammatory diseases. On the other side, inflammatory diseases are easily lead to adverse pregnancy outcomes. Therefore, it is indispensable and worthy to statistic and analyze the effect of anti-TNF-α drug on the adverse pregnancy outcomes. In this review, we summarize the reports about the adverse pregnancy outcomes (PE, IUGR, SA and preterm birth) of using anti-TNF-α drugs (infliximab, etanercept and adalimumab, certolizumab and golimumab) currently in the clinical studies (Table 1).
Table 1.
The statistics of anti-TNFα drug (infliximab, adalimumab, etanercept, golimumab and certolizumab) on the pregnancy outcome (live birth, PE, IUGR, SA, preterm birth and other pregnancy outcomes)
| Anti-TNF-α | Pregnancy outcome | Abortion rate | Number | Disease | References | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Live birth | PE | IUGR | SA | Preterm birth | Other | 1st trim | 2nd/3rd trim | ||||
| Infliximab | 1526/1850 | No report | 12.1% | 9.2% | Congenital anomalies (2.0%) | No report | No report | 1850 | CD/UC | (Ref. 54) | |
| Infliximab | 64/96 | No report | 14/96 | No report | No report | No report | 96 | RA/CD | (Ref. 55) | ||
| Infliximab | 10/10 | No report | No report | No report | 3/10 | No report | No report | 10 | IBD | (Ref. 56) | |
| Infliximab | 32/42 | No report | No report | No report | No report | No report | No report | 42 | IBD | (Ref. 65) | |
| Infliximab | 1740/2017 | No report | No report | No report | 104/1754 | No report | No report | 2017 | IBD | (Ref. 81) | |
| Infliximab | 220/252: 69/72 | No report | No report | 28/252; 3/72 | No report | No report | No report | 252 (maternal); 72 (paternal) | CD | (Ref. 57) | |
| Infliximab | 413/495 | No report | No report | 43/495 | 63/407 | No report | No report | 495 | IBD | (Ref. 82) | |
| Infliximab | 46/59 | No report | No report | 10/59 | 8/59 | No report | No report | 59 | IBD | (Ref. 83) | |
| Infliximab | 155/194 | No report | No report | 15/194 | 21/194 | No report | No report | 194 | IBD | (Ref. 72) | |
| Infliximab | 117/151 | No report | No report | 11/151 | 16/151 | No report | No report | 151 | IBD | (Ref. 72) | |
| Infliximab | 55/82 | No report | No report | 11/82 | No report | No report | No report | 82 | CD | (Ref. 55) | |
| Infliximab | No report | No report | No report | No report | 7/83 | No report | No report | 83 | IBD | (Ref. 84) | |
| Infliximab | 4/17 | No report | No report | 1/17 | No report | No report | No report | 17 | RA | (Ref. 85) | |
| Infliximab | 67/83 | No report | No report | 9/83 | 16/66 | No report | No report | 83 | IBD | (Ref. 86) | |
| Adalimumab | 65/74 | No report | No report | No report | No report | 40% | 2nd:16%, 3rd:44% | 74 | RA | (Ref. 61) | |
| Adalimumab | No significant differences were found in pregnancy and foetal outcomes when compared to the general population | 7/7 | 2nd:4/7 | 7 | IBD | (Ref. 65) | |||||
| Adalimumab | 24/28 | No report | No report | 2/28 | 4/24 | No report | No report | 28 | IBD | (Ref. 87) | |
| Adalimumab | 45/53 | 5/53 | 2/53 | Stillbirth (1/53) | CD/UC/RA | (Ref. 88) | |||||
| Adalimumab | 35/47 | No report | No report | No report | No report | No report | No report | No report | 41+6 (immunoglobulin and non-immunoglobulin) | RMA and implantation failure | (Ref. 89) |
| Adalimumab | 221/257 | No report | No report | 25/257 | 24/213 | Teratogenesis: 22/221 | No report | No report | 257 | RA/ CD | (Ref. 62) |
| Etanercept | 2169/3048 | No report | No report | 590/3048 | No report | Artificial abortion: 265/3048 | No report | No report | 3048 | CIA | (Ref. 90) |
| Etanercept | 66% | No report | No report | 20% | No report | Teratogenesis (Ref. 1) | No report | No report | 56 | CIA | (Ref. 58) |
| Etanercept | 1354/1835 | No report | No report | 306/1835 | No report | Artificial abortion: 168/1835 | No report | No report | 1835 | PsA | (Ref. 90) |
| Etanercept | 16/17 | No report | No report | 2/17 | No report | No report | No report | 17 | RA/ankylosing spondylitis/PsA | (Ref. 91) | |
| Etanercept | No report | No report | No report | No report | 19/106 | No report | No report | 140 | RA | (Ref. 82) | |
| Etanercept | No report | No report | No report | 2/15 | 1/15 | No report | No report | 15 | RA | (Ref. 70) | |
| Etanercept | No report | No report | No report | 0/10 | 1/10 | No report | No report | 10 | RA | (Ref. 70) | |
| Etanercept | 85/95 | No report | No report | 10/95 | No report | Gestational hypertension: 1/95 | No report | No report | 95 | Refractory innate immunity RMA | (Ref. 74) |
| Etanercept | 6/6 | No report | No report | 0/6 | No report | No report | No report | 6 | SpA | (Ref. 73) | |
| Etanercept | 1/1 | No report | No report | 0/1 | No report | No report | No report | 1 | JIA | (Ref. 73) | |
| Etanercept | 0/1 | No report | No report | 1/1 | No report | 1/1 | No report | 1 | PsA | (Ref. 73) | |
| Etanercept | 0/2 | No report | No report | 1/2 | No report | Early termination of pregnancy (1/2) | 2/2 | No report | 2 | RA | (Ref. 73) |
| Etanercept | 2/2 | No report | No report | No report | No report | No report | No report | 2 | RA | (Ref. 85) | |
| Golimumab | 143/208 | No report | 4/208 | 47/208 | 5/208 | 38/183 | 0/183 | 208 | RA and IBD | (Ref. 92) | |
| Golimumab | No report | No report | No report | 32.5% | No report | No report | No report | 40 | UC | (Ref. 93) | |
| Certolizumab | 26/47(55.3%) | No report | No report | No report | No report | No report | No report | No report | RA | (Ref. 93) | |
| Certolizumab | 459/538 | 5/538 | 5/538 | 47/538 | No report | Serious maternal infections (Ref. 22), gestational diabetes (Ref. 6), induced abortion (Ref. 27), stillbirth (Ref. 5) | No report | No report | 538 | RA/ CD | (Ref. 69) |
| Certolizumab | No report | No report | No report | 2/25 | 2/25 | Premature rupture of the membranes (Ref. 9), light-for-date (Ref. 7) | No report | No report | 25 | RA | (Ref. 70) |
| Certolizumab | 254/339 | 6/339 | 6/339 | 84/339 | No report | Stillbirth (Ref. 1), placental abnormalities (Ref. 4), infection (Ref. 5), disease flare (Ref. 10), gestational diabetes (Ref. 5), congenital malformation (Ref. 8) | No report | No report | 339 | RA (118), CD (192), other (Ref. 29) | (Ref. 71) |
| Certolizumab | 8/17 | No report | No report | 1/17 | No report | Low birth weight (1/17) | No report | No report | 17 | IBD | (Ref. 72) |
PE, preeclampsia; IUGR, intrauterine growth restriction; SA, spontaneous abortion; CD, Crohn's disease; UC, ulcerative colitis; RA, rheumatoid arthritis; IBD, inflammatory bowel disease; IFX, infliximab; ETA, etanercept; ADA, adalimumab; CZP, certolizumab-pegol.
4.1. Infliximab and adverse pregnancy outcomes
IFX is the first anti-TNF-α drug to be approved to apply to IBD, PsA and RA. Truta and Geldhof et al. reported that preterm births and IUGR rate are increased in the IFX group (P < 0.049) (Refs 53, 54). Katz et al. collected the outcome data of 96 women who were exposed to IFX, the result showed that live birth rate is 67% (64/96), the percent of SA is 15% (14/96) and termination of treatment is 19% (18/96) (Ref. 55). Geldhof et al. retrospectively analyzed the Janssen's global safety surveillance databases and the pregnancy outcomes of 1725 patients exposed to IFX. In total, 1549/1875 (82.61%) were reported as live births, 226/1875 (12.1%) were reported as RA, 143/1549 (9.2%) were reported as preterm births, and the prevalence of IUGR is ⩽1.1% (Ref. 54). However, a retrospective study by Mahadevan et al. reported that three infants were preterm birth and one is low-birth weight in all 10 pregnancies that exposed to IFX (Ref. 56). In those data, there is no doubt that some pregnant women choose early termination of pregnancy. Lichtenstein et al. analyzed the data in the TREAT Registry (1999–2012) and concluded that the rates of miscarriage (10% versus 6.7%) and neonatal complications (6.9% versus 10%) have no statistic difference in IFX exposure and IFX non-exposure patients (Ref. 57). Overall, IFX may increase the risk of preterm birth, caesarean delivery, and low birth weight, teratogenesis and stillbirth are rarely reported (Refs 53, 58).
IFX, an immunoglobulin antibody, has difficulty in passing through the maternal placenta during the first trimester of pregnancy, while at the end of the second and the third trimesters, it often transfers through the placenta. IFX has been detected in serum of child at 6 weeks of age, whose mother was exposed to IFX (Ref. 59). Another case reported that all eight patients with IFX treatment delivered healthy children, and the IFX levels were higher in infant than that of in mother. Besides, the IFX levels take 2–8 months to be completely cleared owing to the immature reticuloendothelial system. In fact, Julsgaard et al. detected IFX exists in infants until 12 months of age (Ref. 60). Hence, the use of IFX during pregnancy is a worthy consideration. Of course, these studies arised from differences in their design and small sample size often incites controversy surrounding. But current guidelines propose that pregnant women are advised to terminate IFX exposure in the third trimester of pregnancy (Ref. 61).
4.2. Adalimumab and adverse pregnancy outcomes
Prospective controlled observational cohort study from the University of California San Diego showed that the live birth of ADA-exposed group is 221/257 (85.9%), which is comparative to that in the healthy pregnancy group [198/225 (88%)]. In the live birth, infants of 22/221 (10%) ADA-exposed women in the first-trimester were diagnosed with a major birth structural defect (OR 1.10, 95% CI 0.45–2.73) while this ratio in healthy group was 12/198 (6.1%) (OR 1.43, 95% CI 0.33–6.27). Meanwhile, HR for SA in ADA-exposed group was higher than that of healthy group (95% CI 0.96–18.95). The reason may be that ADA-exposed group are more likely to terminate pregnancy considering the potential harm for fetus. Besides, the likelihood of preterm birth of patients in ADA-exposed group is higher than that of in healthy group (HR 2.59, 95% CI 1.22–5.50) (Ref. 62). A prospective study compared the level of TNF-α in pregnant women between ADA-treatment group and IFX-exposed group. It manifested that at birth, ADA in cord blood of pregnant women with ADA-treatment group was obviously lower than IFX-exposed group, and in third stage pregnancy, the transportation of IFX is exponential in the placenta while the linear growth transfer of ADA is restricted, which implied that the residual ADA is more likely to reduce the relapse risk of mother (Ref. 63). Interestingly, Winger et al. reported that ADA treatment can improve pregnancy rates of women undergoing IVF via change the ratio of Th1 and Th2 (Ref. 64). ADA treatment has been reported that there are no significant differences in pregnancy and foetal outcomes when compared to the general population (Ref. 65). They can induce SA and preterm birth in three different trimesters of gestation as the medicine of RA (Refs 61, 62, 66).
4.3. Certolizumab and adverse pregnancy outcomes
Certolizumab-pegol (CZP) is mainly used for patients with severe plaque psoriasis. CZP is a pegylated humanised anti-TNF-α antigen-binding fragment, and cannot bind with the Fc receptor of neonatal (Refs 64, 67). Thus, penetration of placenta, breast milk content, and oral bioavailability are all low (Ref. 68). At present, there are few large-scale data about the pregnancy outcomes of CZP exposure. Clowse et al. reported that of 538 patients with known outcomes of CZP exposure, 459 were live births, 47 were SA and 8 were congenital malformations according to the prospective and retrospective data from the UCB Pharma safety databases (Ref. 69). Besides, the serious maternal infections, gestational diabetes, stillbirth, premature rupture of the membranes, stillbirth, placental abnormalities, infection, disease flare, gestational diabetes, congenital malformation and low birth weight have also been reported in the process of CZP for the therapy of RA and IBD (Refs 69–72).
4.4. Etanercept/golimumab and adverse pregnancy outcomes
Apart from IBD, PsA and RA, ETA has been widely used in chronic inflammatory arthritis, juvenile idiopathic arthritis and ankylosing spondylitis. SA and preterm birth are the most common adverse pregnancy outcomes, and SA often occurs in the first trimester of pregnancy (Ref. 73). Noteworthly, one gestational hypertension has been reported in the treatment of refractory recurrent SA (Ref. 74). The data from Italian rheumatology centres show that the live births were 66%, and the SA was 20% in the 79 exposed pregnancies, including 56 pregnant women exposed to ETA, 13 to ADA, 3 to IFX, 2 to CZP, etc. (Ref. 58). Golimumab was approved by the FDA in April 2009 as a treatment for moderately to severely active RA in combination with MTX (Ref. 58). The report of golimumab is relatively less. It is no doubt that both golimumab and certolizumab can induce IUGR, SA and preterm birth.
Overall, the most common adverse pregnancy of above anti-TNF-α drugs is IUGR, SA and preterm birth. ETA and golimumab mainly induce early abortion, while ADA increases the risk of abortion in any phase of pregnancy. Apart from certolizumab, no case about PE complication of other drugs is reported. Teratogenesis and stillbirth are mainly related to IFX and certolizumab. One report about gestational hypertension has been proposed in the use of ETA. The live birth of both drugs is relatively high. How to balance the advantages and disadvantages of the drugs and which medications should be chosen at different trimester of pregnancy have no consensus in the clinical studies. Our review may aid clinicians and women of childbearing age in their inflammatory disease's treatment.
4.5. Effect of anti-TNF-α drugs on immune system suppression
Anti-TNF-α drugs can decrease the activation of NK cells. Nocturne et al. reported that NK cell function was impaired in the anti-TNF group compared with MTX group during the treatment of RA (20.9 versus 31.3%, P = 0.04) (Ref. 75). Defendenti et al. detected B-cell subsets in bone marrow and peripheral blood of IBD patients, which showed that anti-TNF-α drugs inhibit the production of B cells in bone marrow and have no influence in circulating B cells (Ref. 76). Anti-TNF-α drugs treatment significantly decreased circulating Th17, Tfh and other pro-inflammatory immune cells, but highly increased circulating Treg and Breg levels (Refs 77, 78). In addition, anti-TNF-α drugs can inhibit proinflammatory macrophages polarisation (Ref. 79). The above immune system suppression from anti-TNF-α drugs may well explain the adverse pregnancy outcomes.
5. Future challenges
It has been demonstrated that high disease activity has been found to have little effect on pregnancy outcomes of IUGR, while the potential use of anti-TNF-α drugs can control disease outbreaks and severity during pregnancy (Ref. 80). At present, there is a lack of consensus on recommendations for the use of these drugs during pregnancy. Hence, it is a big challenge to carefully weigh the benefits and risk of anti-TNF-α drugs exposed to the mother and infant. The problem and puzzle about anti-TNF-α drug on the pregnancy outcome are whether the drug induces infertility (Ref. 1); whether the drug causes adverse pregnancy outcomes in different time of conception (Ref. 2); whether the drug can lead to foetal abnormalities and other potential complications (Ref. 3). Large-scale and long-time clinical data on its impact on pregnancy outcomes are indispensable in the future.
Acknowledgements
We are grateful for the support of the National Natural Science Foundation of China (grant number 82071655, 81860276); Key Research and Development Program of Hubei Province (grant number 2020BCB023); Young Teacher Qualification Project of the Fundamental Research Funds for the Central Universities (2042020kf0088); China Medical Association Clinical Medical Research Special Fund Project (grant number 17020310700); the Fundamental Research Funds for the Central Universities (grant number 2042020kf1013); Educational and Teaching Reform Research Project (grant number 413200095); Graduate credit course projects (grant number 413000206).
Conflict of interest
None.
References
- 1.Pollheimer J et al. (2018) Regulation of placental extravillous trophoblasts by the maternal uterine environment. Frontiers in Immunology 9, 2597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Krieg S and Westphal L (2015) Immune function and recurrent pregnancy loss. Seminars in Reproductive Medicine 33, 305–312. [DOI] [PubMed] [Google Scholar]
- 3.Pantham P, Aye IL and Powell TL (2015) Inflammation in maternal obesity and gestational diabetes mellitus. Placenta 36, 709–715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sargent IL, Borzychowski AM and Redman CW (2006) NK cells and human pregnancy – an inflammatory view. Trends in Immunology 27, 399–404. [DOI] [PubMed] [Google Scholar]
- 5.Alijotas-Reig J et al. (2017) Tumor necrosis factor-alpha and pregnancy: focus on biologics. An updated and comprehensive review. Clinical Reviews in Allergy & Immunology 53, 40–53. [DOI] [PubMed] [Google Scholar]
- 6.Ghazanfari T et al. (2020) Indicated and non-indicated antibiotic administration during pregnancy and its effect on pregnancy outcomes: role of inflammation. International Immunopharmacology 89, 107081. [DOI] [PubMed] [Google Scholar]
- 7.Holbrook J et al. (2019) Tumour necrosis factor signalling in health and disease. F1000Research 8, 111–118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Black RA et al. (1997) A metalloproteinase disintegrin that releases tumour-necrosis factor-alpha from cells. Nature 385, 729–733. [DOI] [PubMed] [Google Scholar]
- 9.Jang DI et al. (2021) The role of tumor necrosis factor alpha (TNF-alpha) in autoimmune disease and current TNF-alpha inhibitors in therapeutics. International Journal of Molecular Sciences 22, 2719–2722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Horiuchi T et al. (2010) Transmembrane TNF-alpha: structure, function and interaction with anti-TNF agents. Rheumatology 49, 1215–1228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hsu H, Xiong J and Goeddel DV (1995) The TNF receptor 1-associated protein TRADD signals cell death and NF-kappa B activation. Cell 81, 495–504. [DOI] [PubMed] [Google Scholar]
- 12.Ye W et al. (2020) Adenosine A3 receptor mediates ERK1/2- and JNK-dependent TNF-alpha production in Toxoplasma gondii-infected HTR8/SVneo human extravillous trophoblast cells. Korean Journal of Parasitology 58, 393–402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Haider S and Knofler M (2009) Human tumour necrosis factor: physiological and pathological roles in placenta and endometrium. Placenta 30, 111–123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lee JW et al. (2019) TLR4 (toll-like receptor 4) activation suppresses autophagy through inhibition of FOXO3 and impairs phagocytic capacity of microglia. Autophagy 15, 753–770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wallach D (2016) The cybernetics of TNF: old views and newer ones. Seminars in Cell & Developmental Biology 50, 105–114. [DOI] [PubMed] [Google Scholar]
- 16.Medler J and Wajant H (2019) Tumor necrosis factor receptor-2 (TNFR2): an overview of an emerging drug target. Expert Opinion on Therapeutic Targets 23, 295–307. [DOI] [PubMed] [Google Scholar]
- 17.Dasinger JH, Abais-Battad JM and Mattson DL (2020) Influences of environmental factors during preeclampsia. American Journal of Physiology. Regulatory, Integrative and Comparative Physiology 319, R26–R32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lin LT et al. (2016) Increased risk of intracranial hemorrhage in patients with pregnancy-induced hypertension: a nationwide population-based retrospective cohort study. Medicine 95, e3732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Smith TA et al. (2015) Immunomodulatory role of vitamin D in the pathogenesis of preeclampsia. Expert Review of Clinical Immunology 11, 1055–1063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Carter W et al. (2017) A narrative synthesis of factors that affect women speaking up about early warning signs and symptoms of pre-eclampsia and responses of healthcare staff. BMC Pregnancy and Childbirth 17, 63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Shaw J et al. (2016) Inflammatory processes are specifically enhanced in endothelial cells by placental-derived TNF-alpha: implications in preeclampsia (PE). Placenta 43, 1–8. [DOI] [PubMed] [Google Scholar]
- 22.Kim J et al. (2017) Aspirin prevents TNF-alpha-induced endothelial cell dysfunction by regulating the NF-kappaB-dependent miR-155/eNOS pathway: role of a miR-155/eNOS axis in preeclampsia. Free Radical Biology & Medicine 104, 185–198. [DOI] [PubMed] [Google Scholar]
- 23.Gelber SE et al. (2015) Prevention of defective placentation and pregnancy loss by blocking innate immune pathways in a syngeneic model of placental insufficiency. Journal of Immunology 195, 1129–1138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chen LM et al. (2010) IL-6, TNFalpha and TGFbeta promote nonapoptotic trophoblast deportation and subsequently causes endothelial cell activation. Placenta 31, 75–80. [DOI] [PubMed] [Google Scholar]
- 25.Novotny S et al. (2013) CD4( + ) T cells play a critical role in mediating hypertension in response to placental ischemia. Journal of Hypertension 2, 14873–14882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Azizieh FY and Raghupathy RG (2015) Tumor necrosis factor-alpha and pregnancy complications: a prospective study. Medical Principles and Practice: International Journal of the Kuwait University, Health Science Centre 24, 165–170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cotechini T et al. (2014) Inflammation in rat pregnancy inhibits spiral artery remodeling leading to fetal growth restriction and features of preeclampsia. Journal of Experimental Medicine 211, 165–179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cotechini T and Graham CH (2015) Aberrant maternal inflammation as a cause of pregnancy complications: a potential therapeutic target? Placenta 36, 960–966. [DOI] [PubMed] [Google Scholar]
- 29.Hunt JS, Atherton RA and Pace JL (1990) Differential responses of rat trophoblast cells and embryonic fibroblasts to cytokines that regulate proliferation and class I MHC antigen expression. Journal of Immunology 145, 184. [PubMed] [Google Scholar]
- 30.Bevilacqua MP et al. (1986) Recombinant tumor necrosis factor induces procoagulant activity in cultured human vascular endothelium: characterization and comparison with the actions of interleukin 1. Proceedings of the National Academy of Sciences of the United States of America 83, 4533–4537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Elfayomy AK et al. (2013) Serum levels of adrenomedullin and inflammatory cytokines in women with term idiopathic intrauterine growth restriction. Journal of Obstetrics and Gynaecology 33, 135–139. [DOI] [PubMed] [Google Scholar]
- 32.Griebel CP et al. (2005) Management of spontaneous abortion. American Family Physician 72, 1243–1250. [PubMed] [Google Scholar]
- 33.Bulletti C, Flamigni C and Giacomucci E (1996) Reproductive failure due to spontaneous abortion and recurrent miscarriage. Human Reproduction Update 2, 118–136. [DOI] [PubMed] [Google Scholar]
- 34.Jang HG et al. (2016) Polymorphisms in tumor necrosis factor-alpha (−863C>A, −857C>T and + 488G>A) are associated with idiopathic recurrent pregnancy loss in Korean women. Human Immunology 77, 506–511. [DOI] [PubMed] [Google Scholar]
- 35.Samudra AN et al. (2018) CD39 and CD73 activity are protective in a mouse model of antiphospholipid antibody-induced miscarriages. Journal of Autoimmunity 88, 131–138. [DOI] [PubMed] [Google Scholar]
- 36.Alijotas-Reig J, Llurba E and Gris JM (2014) Potentiating maternal immune tolerance in pregnancy: a new challenging role for regulatory T cells. Placenta 35, 241–248. [DOI] [PubMed] [Google Scholar]
- 37.Wang WJ et al. (2013) Regulation of the expression of Th17 cells and regulatory T cells by IL-27 in patients with unexplained early recurrent miscarriage. Journal of Reproductive Immunology 99, 39–45. [DOI] [PubMed] [Google Scholar]
- 38.Fonseca BM et al. (2020) Decidual NK cell-derived conditioned medium from miscarriages affects endometrial stromal cell decidualisation: endocannabinoid anandamide and tumour necrosis factor-alpha crosstalk. Human Reproduction 35, 265–274. [DOI] [PubMed] [Google Scholar]
- 39.Yang SL et al. (2021) Kynurenine promotes the cytotoxicity of NK cells through aryl hydrocarbon receptor in early pregnancy. Journal of Reproductive Immunology 143, 103270. [DOI] [PubMed] [Google Scholar]
- 40.Huang Q et al. (2019) Effect of miR-30e regulating NK cell activities on immune tolerance of maternal-fetal interface by targeting PRF1. Biomedicine & Pharmacotherapy 109, 1478–1487. [DOI] [PubMed] [Google Scholar]
- 41.Li S et al. (2017) Expression level of TNF-alpha in decidual tissue and peripheral blood of patients with recurrent spontaneous abortion. Central-European Journal of Immunology 42, 156–160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Zhang Y et al. (2019) NOD1 modulates decidual stromal cell function to maintain pregnancy in the early trimester. Cell Biochemistry and Function 37, 464–473. [DOI] [PubMed] [Google Scholar]
- 43.Organization WH (1977) WHO: recommended definitions, terminology and format for statistical tables related to the perinatal period and use of a new certificate for cause of perinatal deaths. Modifications recommended by FIGO as amended October 14, 1976. Acta Obstetricia et Gynecologica Scandinavica 56, 247–253. [PubMed] [Google Scholar]
- 44.Gomez-Lopez N et al. (2020) Regulatory T cells play a role in a subset of idiopathic preterm labor/birth and adverse neonatal outcomes. Cell Reports 32, 107874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Li W et al. (2020) Upregulation of TNF-alpha and IL-6 induces preterm premature rupture of membranes by activation of ADAMTS-9 in embryonic membrane cells. Life Sciences 260, 118237. [DOI] [PubMed] [Google Scholar]
- 46.Wang XJ, Li L and Cui SH (2009) [Role of collagen III, CTGF and TNF-alpha in premature rupture of human fetal membranes]. Sichuan Da Xue Xue Bao 40, 658–661, 75. [PubMed] [Google Scholar]
- 47.Ulrich CC et al. (2019) Matrix metalloproteinases 2 and 9 are elevated in human preterm laboring uterine myometrium and exacerbate uterine contractility dagger. Biology of Reproduction 100, 1597–1604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Menon R et al. (2006) Analysis of association between maternal tumor necrosis factor-alpha promoter polymorphism (−308), tumor necrosis factor concentration, and preterm birth. American Journal of Obstetrics and Gynecology 195, 1240–1248. [DOI] [PubMed] [Google Scholar]
- 49.Pomini F, Caruso A and Challis JR (1999) Interleukin-10 modifies the effects of interleukin-1beta and tumor necrosis factor-alpha on the activity and expression of prostaglandin H synthase-2 and the NAD + -dependent 15-hydroxyprostaglandin dehydrogenase in cultured term human villous trophoblast and chorion trophoblast cells. Journal of Clinical Endocrinology and Metabolism 84, 4645–4651. [DOI] [PubMed] [Google Scholar]
- 50.Lan Y et al. (2021) Progesterone-induced blocking factor-mediated Th1/Th2 balance correlates with fetal arrest in women who underwent in vitro fertilization and embryo transfer. Clinical Immunology 232, 108858. [DOI] [PubMed] [Google Scholar]
- 51.Li HH et al. (2016) Association of TNF-alpha genetic polymorphisms with recurrent pregnancy loss risk: a systematic review and meta-analysis. Reproductive Biology and Endocrinology: RB&E 14, 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Vinet E et al. (2013) Induced abortions in women with rheumatoid arthritis receiving methotrexate. Arthritis Care & Research 65, 1365–1369. [DOI] [PubMed] [Google Scholar]
- 53.Truta B et al. (2020) Early discontinuation of infliximab in pregnant women with inflammatory bowel disease. Inflammatory Bowel Diseases 26, 1110–1117. [DOI] [PubMed] [Google Scholar]
- 54.Geldhof A et al. (2020) Exposure to infliximab during pregnancy: post-marketing experience. Drug Safety 43, 147–161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Katz JA et al. (2004) Outcome of pregnancy in women receiving infliximab for the treatment of Crohn's disease and rheumatoid arthritis. American Journal of Gastroenterology 99, 2385–2392. [DOI] [PubMed] [Google Scholar]
- 56.Mahadevan U et al. (2005) Intentional infliximab use during pregnancy for induction or maintenance of remission in Crohn's disease. Alimentary Pharmacology & Therapeutics 21, 733–738. [DOI] [PubMed] [Google Scholar]
- 57.Lichtenstein GR et al. (2018) Pregnancy outcomes reported during the 13-year TREAT registry: a descriptive report. American Journal of Gastroenterology 113, 1678–1688. [DOI] [PubMed] [Google Scholar]
- 58.Bazzani C et al. (2015) Prospectively-followed pregnancies in patients with inflammatory arthritis taking biological drugs: an Italian multicentre study. Clinical and Experimental Rheumatology 33, 688–693. [PubMed] [Google Scholar]
- 59.Vasiliauskas EA et al. (2006) Case report: evidence for transplacental transfer of maternally administered infliximab to the newborn. Clinical Gastroenterology and Hepatology 4, 1255–1258. [DOI] [PubMed] [Google Scholar]
- 60.Julsgaard M et al. (2016) Concentrations of adalimumab and infliximab in mothers and newborns, and effects on infection. Gastroenterology 151, 110–119. [DOI] [PubMed] [Google Scholar]
- 61.Burmester GR et al. (2017) Adalimumab long-term safety: infections, vaccination response and pregnancy outcomes in patients with rheumatoid arthritis. Annals of the Rheumatic Diseases 76, 414–417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Chambers CD et al. (2019) Birth outcomes in women who have taken adalimumab in pregnancy: a prospective cohort study. PLoS ONE 14, e0223603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Kanis SL et al. (2018) Anti-TNF levels in cord blood at birth are associated with anti-TNF type. Journal of Crohn's & Colitis 12, 939–947. [DOI] [PubMed] [Google Scholar]
- 64.Winger EE et al. (2009) Treatment with adalimumab (Humira) and intravenous immunoglobulin improves pregnancy rates in women undergoing IVF. American Journal of Reproductive Immunology 61, 113–120. [DOI] [PubMed] [Google Scholar]
- 65.Schnitzler F et al. (2011) Outcome of pregnancy in women with inflammatory bowel disease treated with antitumor necrosis factor therapy. Inflammatory Bowel Diseases 17, 1846–1854. [DOI] [PubMed] [Google Scholar]
- 66.Weber-Schoendorfer C, Fritzsche J and Schaefer C (2011) Pregnancy outcomes in women exposed to adalimumab or infliximab: the experience of the Berlin Institute for Clinical Teratology and Drug Risk Assessment in Pregnancy – ScienceDirect. Reproductive Toxicology 31, 267–268. [Google Scholar]
- 67.Mariette X et al. (2018) Lack of placental transfer of certolizumab pegol during pregnancy: results from CRIB, a prospective, postmarketing, pharmacokinetic study. Annals of the Rheumatic Diseases 77, 228–233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Lee A and Scott LJ (2020) Certolizumab pegol: a review in moderate to severe plaque psoriasis. BioDrugs 34, 235–244. [DOI] [PubMed] [Google Scholar]
- 69.Clowse MEB et al. (2018) Pregnancy outcomes after exposure to certolizumab pegol: updated results from a pharmacovigilance safety database. Arthritis & Rheumatology 70, 1399–1407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Shimada H et al. (2019) Effect of biologic disease-modifying anti-rheumatic drugs for patients with rheumatoid arthritis who hope to become mothers. Clinical Rheumatology 38, 1453–1458. [DOI] [PubMed] [Google Scholar]
- 71.Clowse ME et al. (2015) Pregnancy outcomes in subjects exposed to certolizumab pegol. Journal of Rheumatology 42, 2270–2278. [DOI] [PubMed] [Google Scholar]
- 72.Marchioni RM and Lichtenstein GR (2013) Tumor necrosis factor-α inhibitor therapy and fetal risk: a systematic literature review. World Journal of Gastroenterology 19, 2591–2602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Berthelot JM et al. (2009) Exposition to anti-TNF drugs during pregnancy: outcome of 15 cases and review of the literature. Joint, Bone, Spine: Revue du Rhumatisme 76, 28–34. [DOI] [PubMed] [Google Scholar]
- 74.Fu J et al. (2019) A randomized controlled trial of etanercept in the treatment of refractory recurrent spontaneous abortion with innate immune disorders. Taiwanese Journal of Obstetrics & Gynecology 58, 621–625. [DOI] [PubMed] [Google Scholar]
- 75.Nocturne G et al. (2017) Impact of anti-TNF therapy on NK cells function and on immunosurveillance against B-cell lymphomas. Journal of Autoimmunity 80, 56–64. [DOI] [PubMed] [Google Scholar]
- 76.Defendenti C et al. (2018) Anti-tumour necrosis factor-alpha antibodies and B cell homeostasis in human inflammatory bowel diseases. International Immunopharmacology 54, 329–335. [DOI] [PubMed] [Google Scholar]
- 77.Chen R et al. (2021) Immunological changes in peripheral blood of ankylosing spondylitis patients during anti-TNF-alpha therapy and their correlations with treatment outcomes. Journal of Immunology Research 2021, 1017938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Salomon BL et al. (2018) Tumor necrosis factor alpha and regulatory T cells in oncoimmunology. Frontiers in Immunology 9, 444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Degboe Y et al. (2019) Polarization of rheumatoid macrophages by TNF targeting through an IL-10/STAT3 mechanism. Frontiers in Immunology 10, 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Mourabet EM et al. (2010) Anti-TNF antibody therapy for inflammatory bowel disease during pregnancy: a clinical review. Current Drug Targets 11, 234–241. [DOI] [PubMed] [Google Scholar]
- 81.Ghalandari N et al. (2020) Intrauterine exposure to biologics in inflammatory autoimmune diseases: a systematic review. Drugs 80, 1699–1722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Weber-Schoendorfer C et al. (2015) Pregnancy outcome after TNF-α inhibitor therapy during the first trimester: a prospective multicentre cohort study. British Journal of Clinical Pharmacology 80, 727–739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Verstappen SM et al. (2011) Anti-TNF therapies and pregnancy: outcome of 130 pregnancies in the British Society for Rheumatology Biologics Register. Annals of the Rheumatic Diseases 70, 823–826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.de Lima A et al. (2016) Tailored anti-TNF therapy during pregnancy in patients with IBD: maternal and fetal safety. Gut 65, 1261–1268. [DOI] [PubMed] [Google Scholar]
- 85.Roux CH et al. (2007) Pregnancy in rheumatology patients exposed to anti-tumour necrosis factor (TNF)-alpha therapy. Rheumatology 46, 695–698. [DOI] [PubMed] [Google Scholar]
- 86.Diav-Citrin O et al. (2014) Pregnancy outcome following gestational exposure to TNF-alpha-inhibitors: a prospective, comparative, observational study. Reproductive Toxicology 43, 78–84. [DOI] [PubMed] [Google Scholar]
- 87.Tan S et al. (2011) Gene expression in a rat model of type II diabetes mellitus: effects of environmental and gene influences on fetal development. Reproductive Toxicology 6, 21328–21336. [Google Scholar]
- 88.Kawai Y, Tsuchiya T and Aoki S (2019) Pregnancy outcomes of patients exposed to adalimumab in Japan. Digestive Diseases 37, 123–130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Mekinian A et al. (2016) Unexplained recurrent miscarriage and recurrent implantation failure: is there a place for immunomodulation? American Journal of Reproductive Immunology 76, 8–28. [DOI] [PubMed] [Google Scholar]
- 90.Carman WJ et al. (2017) Pregnancy and infant outcomes including major congenital malformations among women with chronic inflammatory arthritis or psoriasis, with and without etanercept use. Pharmacoepidemiology and Drug Safety 26, 1109–1118. [DOI] [PubMed] [Google Scholar]
- 91.Hoxha A et al. (2017) Pregnancy and foetal outcomes following anti-tumor necrosis factor alpha therapy: a prospective multicentre study. Joint, Bone, Spine: Revue du Rhumatisme 84, 169–173. [DOI] [PubMed] [Google Scholar]
- 92.Esslinger S et al. (2020) P599 trimester exposure and pregnancy outcomes in women exposed to golimumab: results from the company pharmacovigilance database. Journal of Crohn's and Colitis 14(Suppl. 1), S500–S01. [Google Scholar]
- 93.Lau A et al. (2014) THU0153 pregnancy outcomes in women exposed to the tumor necrosis factor inhibitor, golimumab. Annals of the Rheumatic Diseases 73(Suppl. 2), 232–233. [Google Scholar]