Abstract
Background
ST elevation myocardial infarction (STEMI) represents a cardiac emergency. Time to diagnosis, identification of culprit lesion, and intervention are important. Inferior STEMI represents a dilemma for cardiologists. The territory can be supplied by the right coronary artery (RCA) or the left circumflex coronary artery (LCx). Diagnostic algorithms have been proposed to predict the culprit artery.
Methods
We performed a single-centre retrospective cohort analysis of all patients admitted to our hospital from 2008 to 2020 with a diagnosis of inferior STEMI. We examined the diagnostic 12 lead ECG for quantification of ST elevation in leads II and III and compared this to culprit lesion found on angiography.
Results
There were 304 patients identified with STEMI in our database; 105 were found to have an inferior myocardial infarction by ECG criteria. Ninety-nine were included in our study with either RCA or LCx culprit lesions on angiography (82 males, 17 females). The average age of these patients was 64.9 years old. Sensitivity, specificity, positive predictive value and negative predictive value for ST elevation in lead II exceeding lead III predicting LCx culprit lesion was 0.32 (95% CI 0.13 to 0.57), 0.94 (95% CI 0.86 to 0.98), 0.55 (95% CI 0.29 to 0.78), 0.85 (95% CI 0.81 to 0.89), respectively. Sensitivity, specificity, positive predictive value and negative predictive value for ST elevation in lead III exceeding lead II predicting RCA culprit lesion was 0.94 (95% CI 0.86 to 0.98), 0.32 (95% CI 0.13 to 0.57), 0.85 (95% CI 0.81 to 0.89), 0.55 (95% CI 0.29 to 0.78), respectively.
Conclusions
In inferior STEMI, comparison of ST elevation in leads II and III can reliably predict culprit lesion artery and guide intervention.
Subject indexing
Culprit artery localisation, inferior stemi, ECG.
Keywords: Acute Coronary Syndrome, Chest Pain, Coronary Vessels, Myocardial Infarction
WHAT IS ALREADY KNOWN ON THIS TOPIC
In the setting of ST elevation myocardial infarction (STEMI), the distribution of ST elevation on the ECG localises the myocardial territory involved. However, the inferior territory can be supplied by either the right coronary artery (RCA) or the distal left circumflex artery (LCx).
Multiple diagnostic algorithms have been proposed to help predict the culprit artery in inferior STEMI. Knowledge of the culprit lesion location may help to reduce door-to-balloon time, thus improving outcomes.
WHAT THIS STUDY ADDS
This study supports the use of a limb lead algorithm for predicting culprit artery in inferior STEMI. Specifically, our retrospective review demonstrates that lead III ST elevation exceeding lead II ST elevation is a marker for RCA culprit lesion with high positive predictive values.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
We suggest that this justifies the use of the limb lead algorithm to localise culprit artery in cases of inferior STEMI. Further research will need to be done to assess whether this translates to an improvement in door-to-balloon time, morbidity, and mortality.
Introduction
The ECG is pivotal in defining ST elevation myocardial infarction (STEMI) and instrumental in determining interventional therapy.1 In the setting of STEMI, the distribution of ST elevation on the ECG localises the myocardial territory involved. This is particularly true in the case of anterior infarctions, which involve the left anterior descending artery. However, the inferior territory can be supplied by one of two arteries—70%–90% of the time it is supplied by the right coronary artery (RCA), but 8%–15% of the time it is supplied by the distal left circumflex artery (LCx), a branch of the left coronary artery.2 This represents a dilemma for cardiologists, as a choice must be made on whether to plan intervention for the left or right coronary circulations first. Time to diagnosis and intervention of the culprit lesion are important performance metrics of catheterisation laboratories as they correlate strongly with risk of adverse outcomes in STEMI.3 4 Knowledge of culprit lesion location may help reduce door-to-balloon time, thus improving outcomes. Multiple diagnostic algorithms have been proposed to help predict the culprit artery in inferior STEMI. A study performed by Zimetbaum et al suggested that ST elevation in lead III greater than lead II may predict RCA culprit lesion as opposed to a LCx culprit lesion.5 6 Alternatively, it has been proposed that II greater than III may predict LCx occlusion. Anecdotally, we noticed a preponderance of case series that questioned this concept. Accordingly, we analysed our prospectively collected STEMI Database to assess whether comparison of leads II and III, in the case of inferior STEMI, could distinguish a culprit artery in either the RCA or LCx.
Methods
The STEMI database at Brooke Army Medical Center (BAMC) is a prospectively gathered database consisting of a comprehensive recording of all patients presenting with a ‘CODE STEMI’ activation at BAMC between January 2008 and December 2020. The database includes data such as age, sex, coronary artery lesion, intervention, door-to-balloon time and outcome data. We retrospectively selected patients in this database if they presented with inferior STEMI based on 12-lead ECG evidence of ST elevation in leads II, III and/or aVF (two or more contiguous leads).
Patients were excluded if they did not meet STEMI criteria based on the fourth universal definition of myocardial infarction, no precatheterisation ECG was available, the CODE STEMI was cancelled, no culprit vessel was identified on angiography, or if they did not undergo emergent cardiac catheterisation.
Prior to knowledge of the angiographic results, each patient’s precatheterisation ECG was evaluated by two independent investigators (AF-S and AS). Using handheld callipers at a point 40 ms after the J-point and compared with the TP segment as the isoelectric baseline, the amount of ST elevation in leads II and III were measured and characterised as II>III or III>II. Separate from the ECG review and blinded to the patient demographics and ECG results, the angiography of those patients were independently reviewed by two investigators (AS, CP) to assess angiographically for the culprit artery (either LCx or RCA).
Standard methods were used to calculate sensitivity, specificity, and positive and negative predictive values. A 95% CI was chosen and assigned to these values. The STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) cohort reporting guidelines were used during review.7
Results
There were 304 patients identified with STEMI in our database, 105 of which were found to have an inferior myocardial infarction based on ECG criteria. Of these patients, 99 were included in our study as they had culprit arteries found on angiography (82 males, 17 females). Six were excluded from the study based on predefined criteria (figure 1). Of the patients excluded from the study, four did not have a precatheterisation ECG available for review, one did not have coronary angiography available in our system and one did not have a culprit lesion on angiography despite ECG evidence of inferior myocardial infarction. The average age of these patients was 64.9 years old with a range from 41 to 100 years old. For all but 12 patients this was their first myocardial infarction. Full patient demographics are available for review in table 1.
Figure 1.
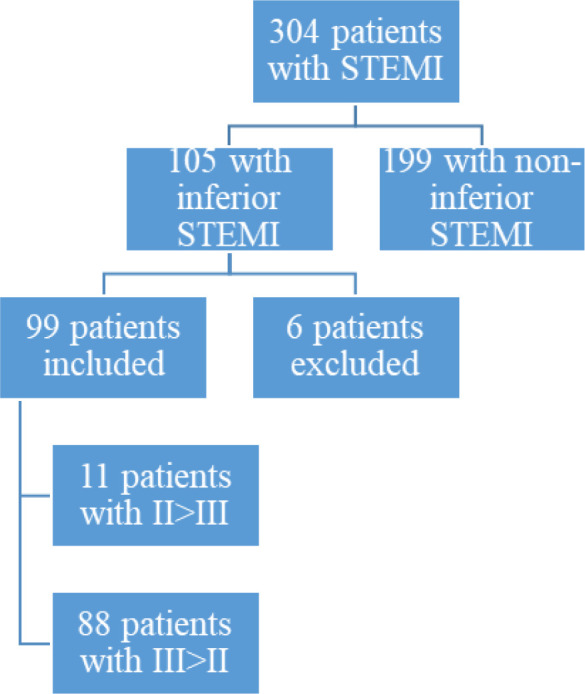
Methods leading to study population. STEMI, ST elevation myocardial infarction.
Table 1.
Demographics of included patients with inferior STEMI
| Category | II>III n=11 | III>II n=88 | LCx n=18 | RCA N=81 |
| Average age (years) | 65 | 62 | 63 | 65 |
| Average BMI | 27.85 | 28.73 | 28.17 | 28.69 |
| DM type 2 | 5 (45%) | 20 (23%) | 5 (28%) | 19 (24%) |
| HTN | 7 (64%) | 66 (75%) | 12 (67%) | 60 (75%) |
| HLD | 8 (73%) | 64 (73%) | 12 (67%) | 59 (74%) |
| Previous AMI | 1 (9%) | 11 (13%) | 3 (17%) | 9 (11%) |
| Smoking | 5 (45%) | 36 (41%) | 9 (50%) | 32 (40%) |
AMI, acute myocardial infarction; BMI, body mass index; DM, diabetes mellitus; HLD, hyperlipidemia; HTN, hypertension; LCx, left circumflex coronary artery; RCA, right coronary artery; STEMI, ST elevation myocardial infarction.
Of the 99 patients that were ultimately included in the study, 11 patients had ST elevation in lead II greater than in lead III. Six of these patients had an LCx culprit lesion and five had an RCA culprit lesion. Eighty-eight patients had ST elevation in lead III greater than in lead II. Thirteen of these patients had an LCx culprit lesion and 75 had an RCA culprit lesion (table 2).
Table 2.
Association between culprit lesion artery and lead elevation of II versus III
| Culprit lesion | II>III N=11 |
III>II N=88 |
| LCx | 6 | 13 |
| RCA | 5 | 75 |
LCX, left circumflex coronary artery; RCA, right coronary artery.
Overall, patient characteristics were fairly similar between those with a LCx and those with a RCA lesion with regard to average age, bod mass index and diagnosis of diabetes mellitus type 2. There was a higher percentage of patients with a previous acute myocardial infarction and smoking status in the LCx culprit lesion group. However, the percentage of patients with a diagnosis of hypertension or a diagnosis of hyperlipidaemia was higher in the RCA culprit lesion group (table 1).
Sensitivity, specificity, positive predictive value (PPV) and negative predictive value for ST elevation in lead II exceeding lead III predicting LCx culprit lesion was 0.32 (95% CI 0.13 to 0.57), 0.94 (95% CI 0.86 to 0.98), 0.55 (95% CI 0.29 to 0.78), 0.85 (95% CI 0.81 to 0.89), respectively (table 3). Sensitivity, specificity, PPV and negative predictive value for ST elevation in lead III exceeding lead II predicting RCA culprit lesion was 0.94 (95% CI 0.86 to 0.98), 0.32 (95% CI 0.13 to 0.57), 0.85 (95% CI 0.81 to 0.89), 0.55 (95% CI 0.29 to 0.78), respectively (table 4).
Table 3.
ST elevation in lead II>lead III as a predictor of LCx culprit lesion
| TP | FP | FN | TN | Sensitivity (95% CI) | Specificity (95% CI) | Positive predictive value (95% CI) | Negative predictive value (95% CI) |
| 6 | 5 | 13 | 75 | 0.32 (0.13 to 0.57) | 0.94 (0.86 to 0.98) | 0.55 (0.29 to 0.78) | 0.85 (0.81 to 0.89) |
FN, false negative; FP, false positive; LCX, left circumflex coronary artery; TN, true negative; TP, true positive.
Table 4.
ST elevation in lead III >lead II as a predictor of RCA culprit lesion
| TP | FP | FN | TN | Sensitivity (95% CI) | Specificity (95% CI) | Positive predictive value (95% CI) | Negative predictive value (95% CI) |
| 75 | 13 | 5 | 6 | 0.94 (0.86 to 0.98) | 0.32 (0.13 to 0.57) | 0.85 (0.81 to 0.89) | 0.55 (0.29 to 0.78) |
FN, False negative; FP, False positive; RCA, right coronary artery; TN, True negative; TP, True positive.
Discussion
Given that the inferior myocardium is supplied by the RCA in over 70% of patients, the ideal algorithm to identify culprit artery in inferior STEMI should first be able to identify RCA lesions with high confidence. Our study demonstrates that ST elevation in lead III versus lead II is highly sensitive (94% sensitivity) with a high PPV (85% PPV) for identifying RCA culprit lesions. Using lead III>II is an ideal algorithm to identify RCA culprit lesions as evidenced by a recent large meta-analysis.8 This can then be augmented by additional criteria such as reciprocal ST depression in aVL and lead I to improve specificity, as a number of studies have shown.8
In addition to identifying RCA culprit lesions, the perfect algorithm would also be able to identify LCx culprit lesions with high confidence. Our study demonstrates that the specificity of ST elevation in lead II>lead III was also quite high (94% specificity). Our data are in accordance with multiple previous studies shown in table 5.8 This table includes the sensitivity, specificity, PPV and negative predictive value for 18 studies that have previously investigated this diagnostic algorithm for predicting culprit lesion in inferior STEMI (specifically using III>II to predict RCA culprit lesion).
Table 5.
Compilation of data from various studies using ST elevation in lead III >lead II as a predictor of RCA culprit lesion
| Study | TP | FP | FN | TN | Sensitivity (95% CI) | Specificity (95% CI) |
Positive predictive value (95% CI) | Negative predictive value (95% CI) |
| Ahahs9 | 44 | 2 | 2 | 8 | 0.96 (0.85 to 0.99) | 0.80 (0.44 to 0.97) | 0.96 (0.84 to 0.99) | 0.80 (0.44 to 0.96) |
| Almansori10 | 464 | 82 | 75 | 89 | 0.86 (0.83 to 0.89) | 0.52 (0.44 to 0.60) | 0.85 (0.82 to 0.88) | 0.54 (0.46 to 0.62) |
| Baptista11 | 34 | 9 | 4 | 6 | 0.89 (0.75 to 0.97) | 0.40 (0.16 to 0.68) | 0.79 (0.64 to 0.90) | 0.60 (0.27 to 0.86) |
| Chia12 | 70 | 2 | 2 | 18 | 0.97 (0.90 to 1.00) | 0.90 (0.68 to 0.99) | 0.97 (0.89 to 1.00) | 0.90 (0.69 to 0.98) |
| Chiang13 | 31 | 6 | 1 | 2 | 0.97 (0.84 to 1.00) | 0.25 (0.03 to 0.65) | 0.84 (0.67 to 0.93) | 0.67 (0.13 to 0.98) |
| Fiol14 | 44 | 4 | 6 | 9 | 0.88 (0.76 to 0.95) | 0.69 (0.39 to 0.91) | 0.92 (0.79 to 0.97) | 0.60 (0.33 to 0.83) |
| Herz15 | 53 | 1 | 13 | 16 | 0.80 (0.69 to 0.89) | 0.94 (0.71 to 1.00) | 0.98 (0.89 to 1.00) | 0.55 (0.36 to 0.73) |
| Huang16 | 160 | 1 | 6 | 27 | 0.96 (0.92 to 0.99) | 0.96 (0.81 to 1.00) | 0.99 (0.96 to 1.00) | 0.82 (0.64 to 0.92) |
| Jin17 | 288 | 8 | 40 | 96 | 0.88 (0.84 to 0.91) | 0.92 (0.85 to 0.97) | 0.97 (0.95 to 0.99) | 0.71 (0.62 to 0.78) |
| Kabakci18 | 114 | 10 | 9 | 16 | 0.93 (0.87 to 0.97) | 0.62 (0.85 to 0.97 | 0.92 (0.85 to 0.96) | 0.64 (0.43 to 0.81) |
| Kanei19 | 81 | 8 | 5 | 12 | 0.94 (0.87 to 0.98) | 0.60 (0.36 to 0.81) | 0.91 (0.83 to 0.96) | 0.71 (0.44 to 0.89) |
| Nair20 | 23 | 3 | 2 | 2 | 0.92 (0.74 to 0.99) | 0.40 (0.05 to 0.85) | 0.88 (0.69 to 0.97) | 0.50 (0.09 to 0.91) |
| Sun21 | 57 | 9 | 13 | 11 | 0.81 (0.70 to 0.90) | 0.55 (0.32 to 0.77) | 0.86 (0.75 to 0.93) | 0.46 (0.26 to 0.67) |
| Taglieri22 | 248 | 46 | 22 | 49 | 0.92 (0.88 to 0.95) | 0.52 (0.41 to 0.62) | 0.84 (0.80 to 0.88) | 0.69 (0.57 to 0.79) |
| Verouden23 | 750 | 103 | 145 | 133 | 0.84 (0.81 to 0.86) | 0.56 (0.50 to 0.63) | 0.88 (0.86 to 0.90) | 0.48 (0.42 to 0.54) |
| Wong24 | 142 | 11 | 8 | 16 | 0.95 (0.90 to 0.98) | 0.59 (0.39 to 0.78) | 0.93 (0.87 to 0.96) | 0.67 (0.45 to 0.84) |
| Zhan25 | 115 | 15 | 2 | 3 | 0.98 (0.94 to 1.00) | 0.17 (0.04 to 0.41) | 0.88 (0.81 to 0.93) | 0.60 (0.17 to 0.93) |
| Zimetbaum5 | 38 | 0 | 14 | 17 | 0.73 (0.59 to 0.84) | 1.00 (0.80 to 1.00) | 1.00 (0.89 to 1.00) | 0.55 (0.36 to 0.72) |
| Total | 2756 | 320 | 369 | 530 | ||||
| 3076 (3>2) | 899 (2>3) | |||||||
FN, False negative; FP, False positive; RCA, right coronary artery; TN, True negative; TP, True positive.
One of the earliest studies to put forth a diagnostic algorithm for discerning culprit artery in inferior STEMI was Zimetbaum et al who analysed 69 patients with inferior wall STEMI to assess for ECG abnormalities that would predict the culprit artery. They found a 100% PPV of ST elevation in lead III exceeding lead II for RCA culprit lesion.2 This is in accordance with our findings of an 84% PPV. Additionally, Zimetbaum et al found a 100% specificity of III>II and RCA culprit lesions; none of the 17 patients in the study with LCx culprit lesion had ST elevation in lead III exceeding the elevation in lead II.5 This is also in accordance with our data in which only 25% of our patients with LCx culprit lesion had lead III elevation greater than lead II elevation.
When comparing our findings to the studies summarised in table 5, our data are mostly in agreement. In particular, sensitivity and PPV for III>II predicting RCA culprit artery are high. The specificity of this algorithm in our study was lower than those in table 5, likely driven by our low overall number of both II>III ECGs and LCx culprit lesions.
We find it most clinically relevant to examine PPV, as we anticipate this algorithm will be most often used when a cardiologist needs to make a rapid decision of which coronary artery to plan for intervention based on ECG data. In this sense, both II>III predicting LCx culprit artery and III>II predicting RCA culprit artery perform well, with high PPVs.
Our data and interpretation is potentially limited by our small sample size, in particular our small number of cases in which ST elevation in lead II exceeded lead III. In addition, our review is a retrospective analysis of prospectively gathered data. Some of the other studies cited in table 5 also used different leads to complement their analysis which may account for the improved sensitivity for LCx obstruction using vector analysis.5 8–25 A potential area for future study could be assessing if the ratio of lead II and III elevations can be used to guide order of vessel evaluation in the setting of inferior STEMI and if this results in a shorter door-to-balloon time.
Conclusion
Timely localisation of the culprit artery in STEMI is important as time is myocardium. In the setting of inferior STEMI this can be challenging as both the RCA and LCx arteries can supply the same vascular territory leading to ST elevations in similar limb leads. Our retrospective review demonstrates that in the setting of inferior STEMI, lead III elevation exceeding lead II elevation is a marker for RCA culprit lesion with high PPVs. Conversely, lead II elevation exceeding lead III elevation is a marker for LCx culprit lesion, although with a lower PPV. This may allow for shorter door-to-balloon times as the angiographer can plan intervention more precisely before angiography. However, further study is needed in order to evaluate if this meaningfully impacts door-to-balloon time, morbidity and mortality.
Footnotes
Contributors: All authors contributed equally to the manuscript. AF-S and AS carried out the initial analyses, drafted the manuscript, and reviewed and revised the manuscript. CP and JEA contributed to the design of the study and review and editing of the manuscript. AS is the guarantor of this manuscript. All authors approved the final manuscript.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: The view(s) expressed here are those of the author(s) and do not reflect the official policy or position of Brooke Army Medical Center, Walter Reed National Military Medical Center, the US Army Medical Department, the US Army Office of the Surgeon General, the Department of the Army, or the Department of Defense or the US government.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement
Data are available on reasonable request.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
A research protocol was approved by the locally appointed ethics committee.Ethics and Ethics committee approval: The study obtained Ethics approval from the Office of the IRB at Brooke Army Medical Center (Protocol #904658). Participants were not required to give informed consent prior to taking part because of the retrospective nature of the study.
References
- 1.Thygesen K, Alpert JS, Jaffe AS. Executive Group of behalf of the Joint European Society of Cardiology (ESC)/American College of Cardiology (ACC)/American Heart Association (AHA)/World Heart Federation (WHF) Task Force for the Universal Definition of Myocardial Infarction. Fourth Universal Definition of Myocardial Infarction. J Am Coll Cardiol 2018;72:2231–64. [DOI] [PubMed] [Google Scholar]
- 2.Murkherjee D, Bates ER, Roffi M. Cardiovascular catheterization and intervention: a textbook of coronary, peripheral, and structural heart disease. CRC Press, 2010. [Google Scholar]
- 3.Foo CY, Bonsu KO, Nallamothu BK, et al. Coronary intervention door-to-balloon time and outcomes in ST-elevation myocardial infarction: a meta-analysis. Heart 2018;104:1362–9. 10.1136/heartjnl-2017-312517 [DOI] [PubMed] [Google Scholar]
- 4.Jneid H, Addison D, Bhatt D. AHA/ACC clinical performance and quality measures for adults with ST-elevation and Non–ST-Elevation myocardial infarction: a report of the American College of Cardiology/American heart association Task force on performance measures. Circulation: Cardiovascular Quality and Outcomes 2017;2017:10. [DOI] [PubMed] [Google Scholar]
- 5.Zimetbaum PJ, Krishnan S, Gold A, et al. Usefulness of ST-segment elevation in lead III exceeding that of lead II for identifying the location of the totally occluded coronary artery in inferior wall myocardial infarction. Am J Cardiol 1998;81:918–9. 10.1016/S0002-9149(98)00013-7 [DOI] [PubMed] [Google Scholar]
- 6.Tierala I, Nikus KC, Sclarovsky S, et al. Predicting the culprit artery in acute ST-elevation myocardial infarction and introducing a new algorithm to predict infarct-related artery in inferior ST-elevation myocardial infarction: correlation with coronary anatomy in the HAAMU trial. J Electrocardiol 2009;42:120–7. 10.1016/j.jelectrocard.2008.12.009 [DOI] [PubMed] [Google Scholar]
- 7.von Elm E, Altman DG, Egger M, et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement. 2007;18:800–4. 10.1097/EDE.0b013e3181577654 [DOI] [PubMed] [Google Scholar]
- 8.Liang H, Wu L, Li Y, et al. Electrocardiogram criteria of limb leads predicting right coronary artery as culprit artery in inferior wall myocardial infarction: a meta-analysis. Medicine 2018;97:24(e10889). 10.1097/MD.0000000000010889 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ahahs A, Al-Jumaily S. Electrocardiographic criteria for predicting site of coronary artery occlusion in acute inferior wall myocardial infarction. Med J Babylon 2011;8:286–94. [Google Scholar]
- 10.Almansori M, Armstrong P, Fu Y, et al. Electrocardiographic identification of the culprit coronary artery in inferior wall ST elevation myocardial infarction. Can J Cardiol 2010;26:293–6. 10.1016/S0828-282X(10)70392-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Baptista SB, Farto e Abreu P, Loureiro JR, et al. Electrocardiographic identification of the infarct-related artery in acute inferior myocardial infarction. Rev Port Cardiol 2004;23:963–71. [PubMed] [Google Scholar]
- 12.Chia BL, Yip JW, Tan HC, et al. Usefulness of St elevation II/III ratio and ST deviation in lead I for identifying the culprit artery in inferior wall acute myocardial infarction. Am J Cardiol 2000;86:341–3. 10.1016/S0002-9149(00)00929-2 [DOI] [PubMed] [Google Scholar]
- 13.Chiang C, Ku P, Huang T. Ekg criteria predict infarct-related artery of inferior wall AMI. Acta Cardiologica Sinica 2006;22:67. [Google Scholar]
- 14.Fiol M, Cygankiewicz I, Carrillo A, et al. Value of electrocardiographic algorithm based on "ups and downs" of ST in assessment of a culprit artery in evolving inferior wall acute myocardial infarction. Am J Cardiol 2004;94:709–14. 10.1016/j.amjcard.2004.05.053 [DOI] [PubMed] [Google Scholar]
- 15.Herz I, Assali AR, Adler Y, et al. New electrocardiographic criteria for predicting either the right or left circumflex artery as the culprit coronary artery in inferior wall acute myocardial infarction. Am J Cardiol 1997;80:1343–5. 10.1016/S0002-9149(97)00678-4 [DOI] [PubMed] [Google Scholar]
- 16.Huang X, Ramdhany SK, Zhang Y, et al. New ST-segment algorithms to determine culprit artery location in acute inferior myocardial infarction. Am J Emerg Med 2016;34:1772–8. 10.1016/j.ajem.2016.06.005 [DOI] [PubMed] [Google Scholar]
- 17.Jin J, Qü P. Value of electrocardiogram in predicting infarction related artery in inferior wall acute myocardial infarction. J Dalian Med Univer 2012;34:52–5. [Google Scholar]
- 18.Kabakci G, Yildirir A, Yildiran L, et al. The diagnostic value of 12-lead electrocardiogram in predicting infarct-related artery and right ventricular involvement in acute inferior myocardial infarction. Ann Noninvasive Electrocardiol 2001;6:229–35. 10.1111/j.1542-474X.2001.tb00113.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kanei Y, Sharma J, Diwan R, et al. St-Segment depression in aVR as a predictor of culprit artery and infarct size in acute inferior wall ST-segment elevation myocardial infarction. J Electrocardiol 2010;43:132–5. 10.1016/j.jelectrocard.2009.09.003 [DOI] [PubMed] [Google Scholar]
- 20.Nair R, Glancy DL. Ecg discrimination between right and left circumflex coronary arterial occlusion in patients with acute inferior myocardial infarction: value of old criteria and use of lead aVR. Chest 2002;122:134–9. 10.1378/chest.122.1.134 [DOI] [PubMed] [Google Scholar]
- 21.Sun T-W, Wang L-X, Zhang Y-Z. The value of ECG lead aVR in the differential diagnosis of acute inferior wall myocardial infarction. Intern Med 2007;46:795–9. 10.2169/internalmedicine.46.6411 [DOI] [PubMed] [Google Scholar]
- 22.Taglieri N, Saia F, Alessi L, et al. Diagnostic performance of standard electrocardiogram for prediction of infarct related artery and site of coronary occlusion in unselected STEMI patients undergoing primary percutaneous coronary intervention. Eur Heart J Acute Cardiovasc Care 2014;3:326–39. 10.1177/2048872614530665 [DOI] [PubMed] [Google Scholar]
- 23.Verouden NJ, Barwari K, Koch KT, et al. Distinguishing the right coronary artery from the left circumflex coronary artery as the infarct-related artery in patients undergoing primary percutaneous coronary intervention for acute inferior myocardial infarction. Europace 2009;11:1517–21. 10.1093/europace/eup234 [DOI] [PubMed] [Google Scholar]
- 24.Wong TW, Huang XH, Liu W, et al. New electrocardiographic criteria for identifying the culprit artery in inferior wall acute myocardial infarction-usefulness of T-wave amplitude ratio in leads II/III and T-wave polarity in the right V5 lead. Am J Cardiol 2004;94:1168–71. 10.1016/j.amjcard.2004.07.086 [DOI] [PubMed] [Google Scholar]
- 25.Zhan Z-qun, Wang W, Dang S-yi, et al. Electrocardiographic characteristics in angiographically documented occlusion of the dominant left circumflex artery with acute inferior myocardial infarction: limitations of St elevation III/II ratio and ST deviation in lateral limb leads. J Electrocardiol 2009;42:432–9. 10.1016/j.jelectrocard.2009.03.015 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are available on reasonable request.


