Abstract
Objectives
An acute critical illness and secondary complications may necessitate a prolonged treatment on an intensive care unit (ICU). As long-term consequences, ICU survivors may suffer from both physical and psychological sequelae. To improve the aftercare of these patients, the present study aimed to assess the use of mental healthcare and associated factors following prolonged ICU stay.
Methods
N=197 patients with a primary diagnosis of critical illness polyneuropathy/myopathy were enrolled within 4 weeks (T1) and interviewed three (T2) and six (T3) months following the transfer from acute-care to postacute ICU. Symptoms and a current diagnosis of major depression/post-traumatic stress disorder (PTSD) were assessed using the Structured Clinical Interview for the Diagnostic and Statistical Manual of Mental Disorders. The potential need for mental healthcare, its current and past use and reasons for non-use were raised.
Results
Full syndromal and subsyndromal major depression/PTSD were diagnosed in 8.3%/15.6% at T2, 12.2%/23.5% at T3. About 29% of the patients reported mental healthcare utilisation. Considering somatic complaints, more important was a common reason for the non-use of mental healthcare. Female gender, previous mental healthcare, number of sepsis episodes and pension receipt increased the chance for mental healthcare utilisation, a pre-existing mental disorder decreased it.
Conclusion
Every fourth patient surviving prolonged ICU treatement makes use of mental healthcare. Particularly male patients with pre-existing mental disorders should be targeted preventively, receiving specific psychoeducation about psychological long-term sequelae and mental healthcare options post-ICU.
Trial registration number
DRKS00003386.
Keywords: Adult intensive & critical care, MENTAL HEALTH, Depression & mood disorders, PUBLIC HEALTH, REHABILITATION MEDICINE
STRENGTHS AND LIMITATIONS OF THIS STUDY.
The present study is a prospective cohort study, providing evidence on the rates and predictors of mental healthcare utilisation, following the discharge from a prolonged stay on intensive care unit.
Structured clinical interviews were applied for the assessement of a current diagnosis of major depression and post-traumatic stress disorder.
A quite homogeneous sample of patients with critical ilness polyneuropathy/critical illness myopathy was examined.
Main limitations affecting the generalisability of the present results are the monocentric design, a small sample size, high dropout rate (43.1%), high rate of men (73.1%) and the retrospective assessment of prior psychopathology.
Introduction
After discharge from the intensive care unit (ICU), survivors of an acute critical illness such as sepsis or acute respiratory distress syndrome (ARDS), may suffer from persisting physical, cognitive and psychological long-term dysfunctions.1 In the literature, the multiple, persisting physical and psychological symptoms following ICU discharge have been referred to as post-intensive care syndrome (PICS), corresponding to the definition by the Society of Critical Care Medicine.2 3 Frightening experiences during intensive care, consequences of medication, prolonged mechanical ventilation, invasive interventions and, finally, an ongoing, severe or even life-threatening illness may expose these patients to several alarming situations. These potentially traumatic experiences during intensive care may be associated with an increased risk for the development of mental disorders.4–8 About one-fifth to one-third of ICU survivors show clinically relevant symptoms of post-traumatic stress disorder (PTSD), anxiety6 7 9 or depression.4 5 Research has identified several major risk factors for PICS, including, for example, the acute psychological stress reaction on ICU (eg, perceived helplessness, perceived fear of death), pre-ICU psychological morbidity, recalled traumatic experiences from the ICU stay and medical variables (eg, length of mechanical ventilation, diagnosis of sepsis, functional status at discharge).4 7 8 10–12
Psychological long-term sequelae following intensive care may attenuate the therapy outcome and reduce health-related quality of life in the long-run.4 13 Consequently, ICU survivors with mental disorders require treatment by mental healthcare specialists in the post-ICU care, for example, psychotherapists, psychiatrists, psychosomatic physicians.14 Referrals for mental healthcare may help patients to recover from clinically relevant affective symptoms after discharge from ICU.15 Present findings suggest, although with conflicting results, that mental healthcare is effective, for example, with regards to PTSD symptom reduction and improvement of health-related quality of life, following the ICU stay.15–18 Although patients with ICU experiences were more than two times likely to visit a psychiatrist than patients without, there are still barriers for the use of mental healthcare.14 19 Above, a certain rate of patients in need for mental healthcare after ICU treatment does not receive any psychological support or at least patient education.19 20 One of the barriers to mental help seeking is that comorbid mental disorders are not adequately recognised or identified correctly by nurses or physicians, which is a well-known problem particularly in patients with somatic diseases.21 22 This may be explained by the assessment via self-report questionnaires or the use of healthcare administrative databases. Both data sources lack sufficient reliability of psychological diagnoses.23 Moreover, physicians prefer the less stigmatising diagnosis of adjustment disorder instead of major depressive disorder, which could impede access to mental healthcare utilisation.23 Another reason could be the unavailability of professional mental healthcare for ICU patients. In clinical practice, psychological support is predominantly provided by the ICU staff and/or pastoral counsellors instead of liaison services specialising in psychotherapy.24
Currently, little is known about the need for and utilisation of mental healthcare in patients after discharge from ICU, irrespective from anxiety and depression symptoms. Moreover, the utilisation of mental healthcare following the ICU discharge, and its association with sociodemographic, medical, contextual and psychological factors remain to be examined. It seems not clear whether ICU survivors with a high risk for the development of mental disorders (eg, those with a pronounced acute stress reaction on ICU),6 12 match those reporting the utilisation of mental healthcare.
Given the paucity of research, our study had the following aims: first, to assess the use of mental healthcare in patients diagnosed with PTSD or a major depression following ICU discharge, compared with other patients who might not have serious psychological sequelae. Second, to analyse associations between mental healthcare utilisation and sociodemographic, medical, contextual and psychological factors. Third, to examine reasons why patients in need do not use mental healthcare services. The findings of this study may help to raise awareness for mental healthcare utilisation in ICU survivors and identify barriers to adequate help- seeking in these patients. Facing the COVID-19 epidemic and the growing number of ICU survivors, the present findings may be of current clinical relevance and could contribute to a greater awareness for the need of patient education as well as mental healthcare in these patients by qualified staff.24
Materials and methods
Patient and public involvement
There was no patient involved in the development of the research questions, study design, recruitment to and conduct of the study. Results will be disseminated by correspondence with representatives of the self-help organisation German Sepsis Aid.
Study design
The present study was nested within a large monocentre, prospective cohort study, which was primarily designed to assess the rates and predictors of psychological long-term sequelae following long-term treatment on ICU.10 In previous publications on the same cohort, rates and predictors of post-traumatic stress and quality of life in family members,20 delayed onset PTSD,25 major depression26 and fatigue27 28 have been focused. The different study foci may explain the slight discrepancies in sample sizes between the current and previous studies.
The present study is an observational study with longitudinal data assessment. Transfer from intensive care in acute-care hospitals to the ICU in a post-acute rehabilitation clinic was defined as reference time T0. Patients were consecutively enrolled and explored within 4 weeks (T1), 3 months (T2) and 6 months (T3) following T0.10 Interviews were carried out face to face at T1 and via telephone at T2 and T3. The study was registered at the German Clinical Trials Register.
Participants and enrolment
Between January 2011 and February 2013, N=352 patients were screened for eligibility. Patients were recruited at a large tertiary care hospital with postacute ICUs, specialised on the weaning from long-term mechanical ventilation. The patients were admitted at an early postacute stage, to so-called phase B rehabilitation.29 At phase B, patients are dependent on professional nursing care, their ability to cooperate is impaired, and their level of consciousness is usually reduced.
Eligibility criteria
Inclusion criteria were the following: minimum age of 18 years, a primary diagnosis of a critical illness myopathy (CIM) and/or critical illness polyneuropathy (CIP) according to the International Classification of Diseases (ICD)-1030 (CIM/CIP: G72.80/G62.80), a negative delirium evaluation according to the Confusion Assessment Method for the Intensive Care Unit (CAM-ICU) during enrolment, length of ICU stay of at least 6 days, sufficient German language skills and approval of study participation via informed consent (either written or orally). Patients with a delirium at enrolment, assessed using the CAM-ICU at T1, were not included in the present study because they were not able to participate in the Structured Clinical Interview for the Diagnostic and Statistical Manual of Mental Disorders (SCID) interview. In case of a positive evaluation of the CAM-ICU, the measure was repeated again within a mean delay of 35.7 days (SD=23.3). These patients were excluded from further study participation. Delirium was defined as manifestation of an acute onset or fluctuations in the course of mental status (feature 1) and inattention (feature 2), plus either disorganised thinking (feature 3) or alteration in the level of consciousness (feature 4). Additionally, patients were excluded if they refused a further study participation, could not adequately communicate (eg, because of cognitive impairment, deafness, weakness, pain, delirium), died at follow-up or were not contactable again. Those patients were defined as dropouts (see also figure 1).
Figure 1.
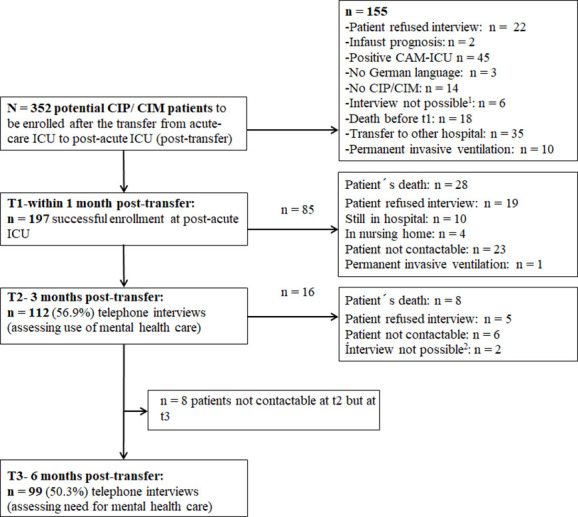
Flowchart showing the number of potentially to be enrolled patients, the number of recruited and followed-up patients at T1 (within 4 weeks following the transfer from acute-care ICU), T2 3 months (post-transfer) and T3 (6 months post-transfer). Finally, a sample of n=112 (T2)/ n=99 (T3) patients were analysed according to the rate of mental healthcare utilisation and associated risk factors. CAM-ICU, Confusion Assessment Method for the Intensive Care Unit; SCID, Structured Clinical Interview for DSM-IV.1 n=1 deaf mute, n=3 communication not possible because of pain, weakness, n=1 not available, n=1 refused communication,2 n=1 deaf, n=1 no communication possible after apoplex.
Study instruments
Clinical and sociodemographic characteristics: at enrolment, the medical history and sociodemographic data were extracted from the patients’ health records (medical comorbidities, history of sepsis, history of antibiotics, length of mechanical ventilation, length of ICU stay, medication, age, gender, partnership, education, documented history of anxiety disorder/depression/harmful alcohol consumption/harmful nicotine consumption, organic brain syndrome, the latter is defined as personality and behavioural disorders due to brain disease, damage and dysfunction according to ICD-10.30 Additionally, we documented whether patients were employed or received a pension (retirement, disability).
Contextual characteristic: the patients’ place of residence was retrieved and categorised as less or more than 20 000 inhabitants, whereas the latter refers to an urban environment.
Functional ability: the severity of functional disability was measured using the Barthel index at admission to and discharge from the post-acute ICU. The Barthel index assesses performance in activities of daily life in 11 domains (eg, faecal/urinary incontinence, help with grooming/ toilet use), with values ranging between 0 and 100. Additionally, the Early Rehabilitation Barthel index was used to measure seven additional domains (intensive care supervision, tracheostomy tube management, intermittent or continuous mechanical ventilation, confusion, behavioural disturbances, severe impairment of communication and dysphagia).31 A sum score was calculated ranging from a minimum value of −325 to a maximum of 100. Barthel indices ranging from negative values to 20 or 25 points correspond to the rehabilitation phase B in Germany.32 For both indices, higher scores represent better functional ability. Inter-rater reliability (r=0.95) and test–retest reliability have proven as very high (r=0.89).33
In order to assess symptoms of major depression and PTSD, we used both, questionnaires and a full structured interview by an expert as reference or ‘gold standard’, because the self-report measures alone may go along with a high false-positive rate of mental disorders. Therefore, we were able to detect how well both measures matched.
Acute stress: within 4 weeks following the transfer to post-acute ICU (T1), the German version of the Acute Stress Disorder Scale (ASDS) was applied in order to assess the severity of post-traumatic distress.34 The ASDS is a 19-item self-report questionnaire with very good reliability (Cronbach’s α=0.95), leading to a sum score ranging from 19 to 95. Higher scores represent greater acute stress symptoms, and a sum score of >56 hints towards the diagnosis of an acute stress disorder. Additionally, the diagnosis of an acute stress disorder was ascertained by using the Structured Clinical Interview (SCID-I) for the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) Axis I.35 Symptom clusters include trauma exposure (criterion A1) and stress reaction (criterion A2), dissociative symptoms (criterion B), re-experiencing (criterion C), avoidance (criterion D), increased arousal (criterion E), causing clinically significant impairment of a patient’s social and functional status (criterion F), with a duration of at least 2 days and no longer than 4 weeks (criterion G). In the present trial, the inter-rater agreement for the SCID-I can be evaluated as moderate to excellent (range of kappa scores: 0.61–0.83).36
PTSD symptoms: during the follow-up assessments at T2 and T3, the severity of posttraumatic stress was measured using the Post-Traumatic Stress Syndrome 10-Inventory (PTSS-10).37 38 PTSS-10 is a 10-item questionnaire assessing post-traumatic stress symptoms (eg, sleep disturbance, nightmares, depression, mood swings, muscular tension) on a 7-point Likert scale (1=never, 7=always). A sum score is calculated ranging between 10 and 70, with higher scores indicating greater post-traumatic stress. A cut-off score of more than 35 is considered to indicate a clinically relevant PTSD symptomatology.38 Internal consistency and stability of the PTSS-10 can be regarded as high (Cronbach’s α=0.92, test–retest reliability r=0.89).39 In the present study, Cronbach’s α was good (at T2: 0.82, at T3: 0.85), retest reliability was satisfying (Spearman’s ρ=0.69).
Additionally, the SCID-I was used in order to assess the diagnosis of PTSD or major depression, at T2 and T3. Criteria for PTSD are exposure to a traumatic event, stress reaction, re-experiencing, avoidance, increased arousal with a duration of more than 1 month and clinically significant distress in important areas of functioning. To assess the presence of a depressive disorder by using the SCID-I, the following symptoms were checked: depressed mood, diminished interest, weight loss/gain, insomnia/hypersomnia, psychomotor retardation, fatigue/loss of energy, feelings of worthlessness/guilt, diminished cognitive abilities, suicidal ideation, significant distress or impairment and a duration of the depressive symptoms of 2 weeks or longer.
Both, patients with a full syndromal and subsyndromal manifestation of acute stress disorder/major depression/PTSD were considered as cases. Patients with a subsyndromal diagnosis did not fulfil all criteria of one symptom cluster, or all symptom clusters were present, but the defined duration of disturbance was not reached, or all symptom clusters were present, but the disturbance did not cause clinically significant distress or impairment in important areas of functioning.
Recalled traumatic memories from ICU (eg, nightmares, severe anxiety/panic, severe pain, trouble to breathe/feelings of suffocation) were assessed according to the questionnaire by Stoll et al,38 both at T2 and T3. The scores were summed up (range: 0–4).
Social support: perceived social support by family members, friends and significant others was determined at both follow-up assessments (T2 and T3), using the Multidimensional Scale of Perceived Social Support (MSPSS). The MSPSS is a 12-item questionnaire, which is rated on a 7-point Likert scale (1=definitely no, 7=definitely yes). The scores of all the items are summed up to a total score (range: 12–84), with higher scores representing greater social support. In the present study, Cronbach’s α was very good with 0.90 at T2 and 0.88 at T3, retest reliability was satisfying (Spearman’s ρ=0.74).
Endpoints
Use of psychotherapy/need for psychotherapy: we used a self-developed questionnaire with three questions to assess the primary outcome. One question captured the current use of professional mental healthcare (‘Have you already consulted professional mental healthcare, such as psychotherapy, because of your current complaints?’). The question could be either answered with ‘yes’ or ‘no’. In case of ‘no’, patients were asked for reasons why a mental healthcare specialist (including specialists in psychosomatic, psychiatry, medical/clinical psychologists, neurologists) have not been addressed so far. The following reasons could be chosen: ‘I have not yet thought about it’; ‘I refuse help by a psychotherapist’. ‘I have not found a suitable psychotherapist’. ‘I have not got an appointment’. Additionally, patients could freely state other reasons.
In the second question, we asked whether the patients were interested in psychological support in the future and would need help to receive psychotherapy, that is, ‘Are you interested in receiving a list with addresses from outpatient psychotherapists, specialised in psychotraumatology, close to your home and do you need support to get an appointment with a mental healthcare specialist?’. Again, this question could be either answered ‘yes’ or ‘no’.
In the third question, we asked for patients’ experiences with psychotherapy during their life time, that is, ‘Have you ever consulted a psychotherapist or psychiatrist in your life time?’. The patients could answer ‘yes’ and provide information about the mental healthcare specialist (eg, psychotherapist, specialist in psychosomatics, psychiatrist, neurologist) or they could simply state ‘no’, without any further specification.
Sample size calculation
The present study originally intended to investigate the frequency of acute stress disorder and PTSD in chronically critically ill patients, following the prolonged stay on ICU.10 For this purpose, a sample size of at least 80 patients was calculated.10 For the present study, a post hoc power analysis for multiple linear regression models using G*Power, assuming a medium effect size (f² = 0.15), an α-significance level of 5%, five (T2) or six predictors (T3), revealed a statistical power of 89% at T2 (n=112 patients) and 81% at T3 (n=99 patients).40 According to a sensitivity analysis and given the sample sizes, as mentioned above, at least a medium effect size would be necessary in order to reach a statistical power of 80%.
Statistical analyses
Categorical variables (eg, number of patients in need for mental healthcare/number of patients with interest in a list of mental healthcare specialists, number of patients having already seeked mental healthcare) are displayed as (conditional) frequencies and percentages. Rates were calculated for the diagnosis of an acute stress disorder, PTSD and major depression. The reported reasons for the non-use of mental healthcare, thus, far were evaluated using a self-developed category system. For this purpose, frequencies were calculated. In order to identify factors associated with the use of mental healthcare (dependent variable), univariate logistic regression analyses were applied, with sociodemographic, contextual, medical and psychological factors as independent variables. Factors with a p value ≤0.141 were included in a multivariable logistic regression model with ‘Enter’ as the variable selection method. In case of continuous variables, z-standardised values were used. We calculated ORs and 95% CIs in order to assess the association between influencing factors and the chance for mental healthcare utilisation, both at T2 and T3. For comparing the sample characteristics between the study sample and the drop-outs, χ2 test, Fisher’s exact test and Mann-Whitney U test were used, if appropriate. Missing values were not replaced. All statistical analyses were realised using SPSS V.28.0.0.0, applying a significance level of p≤0.05. In order to avoid type I error in case of multiple tests, a Bonferroni-corrected p value was calculated, if appropriate.
Results
Sociodemographics and psychopathology
At T1, N=197 CIP/CIM patients could be successfully enrolled. Of these, 112 (56.9%) could be followed-up at T2 and 99 (50.3%) patients at T3 (see flowchart in figure 1). Fifty per cent of the N=197 recruited patients were between 55.9 and 66.1 years, with a median age of 61.4 years. Nearly three quarter (73.1%) were men, which is representative of the sample (N=352) approached initially. Among the enrolled patients, 68.6% were married or cohabited. The patient sample had a median Barthel index of −200.0 at admission, corresponding to phase B rehabilitation in Germany. More than two-thirds of the patients had a sepsis episode, mostly located at the respiratory tract (see table 1, online supplemental table S1). Accordingly, a majority of the patients (76.8%) suffered from an acute respiratory insufficiency (see online supplemental table S1). Nearly all patients (n=193, 98%) were mechanically ventilated. The most frequent comorbidity was hypertension (59.8%), followed by diabetes, left heart failure and atrial fibrillation. Every second patient had nine or more somatic diagnoses. More than three quarter (79.7%) of the patients had a prior psychiatric history. Most of them had an organic brain syndrome, followed by harmful nicotine consumption, major depressive disorder, harmful alcohol consumption and anxiety disorder. The median duration of ICU stay was 70 days and of mechnical ventilation it was 48 days (for further details, see table 1, online supplemental table S1. Patients who completed T2 and T3 had a significantly higher functional status and were more often higher educated than those who dropped out (see online supplemental table S2).
Table 1.
Baseline sociodemographic and clinical characteristics of the cohort of N=197 patients with the primary diagnosis of critical illness polyneuropathy (CIP) and/ or critical illness myopathy (CIM)
| Characteristic | Cohort N=197 |
| Age, years median (IQR), range (min, max) | 61.4 (55.9–66.1), 25.6, 71.9 |
| Gender, n (%) | |
| Male | 144 (73.1) |
| Female | 53 (26.9) |
| Family status, n (%) | |
| Single | 22 (11.2) |
| Married | 125 (63.5) |
| Cohabited | 10 (5.1) |
| Divorced/living apart | 28 (14.2) |
| Widowed | 12 (6.1) |
| Education, n (%)* | |
| <10 years | 74 (37.6) |
| ≥10 years | 113 (57.4) |
| ICU stay, days median (IQR), | 69.0 (49.5–100.0), |
| Range (min, max) | 12, 278 |
| Mechanical ventilation, days median (IQR), | 48.0 (33.0–73.5) |
| Range (min, max)† | 0, 236 |
| ICU stay in acute-care ICU, days median (IQR), | 35.0 (25.0–52.5) |
| Range (min, max) | 7, 232 |
| Mechanical ventilation in acute-care ICU | 31.0 |
| Days median (IQR) | (21.5–46.0), |
| Range (min, max) | 0, 232 |
| Sepsis, n (%) | |
| No sepsis | 59 (29.9) |
| Sepsis | 138 (70.1) |
| Barthel index, median (IQR), range (min, max) | |
| At admission at post-acute ICU | −200.0 (−225.0– −125.0), −275, 20 |
| At discharge from post-acute ICU | −35.0 (−90.0–5.0), −225, 100 |
| At discharge from rehabilitation hospital | 60.0 (−10.0–80.0), −225, 100 |
| Use of antibiotics, n (%) | 189 (97.4) |
| History of major depressive disorder | 49 (24.9) |
| History of anxiety disorder | 18 (9.1) |
| History of harmful alcohol consumption | 41 (20.8) |
| History of harmful nicotine consumption | 72 (36.5) |
| History of organic brain syndrome (F07.X) | 86 (43.7) |
All patients have been enrolled at a tertiary care hospital, within 4 weeks following the discharge from acute-care ICU (T0).
*n=6 missing values.
†n=193 patients received mechanical ventilation.
ICU, intensive care unit.
bmjopen-2022-063468supp001.pdf (136.4KB, pdf)
Information regarding the intensity of acute/post-traumatic stress symptoms and rates of acute stress disorder, major depression and PTSD are presented in online supplemental table 3. At T1, about every tenth patient (13.2%) was diagnosed with an acute stress disorder. 8.3% had a full syndromal or subsyndromal depressive disorder at T2, 12.2% at T3. Regarding a PTSD at T2/T3, a sub syndromal or full syndromal diagnosis was ascertained in 15.6%/23.5% of the patients. Rates of major depression and PTSD did not significantly differ with respect to mental healthcare utilisation.
Frequency of mental healthcare utilisation at T2 (3 months following the transfer from acute-care ICU)
Among the 112 patients who were followed up at T2, 30 (26.8%) reported that they already consulted a mental healthcare specialist for reasons of their current psychological complaints. Most of these patients consulted a clinical psychologist or psychotherapist during their rehabilitation (table 2). Of the 82 patients not consulting a mental healthcare specialist, about one quarter have not yet thought about it, and more than every second reported other reasons, for example, patients did not need it or somatic complaints were more important, among others (see table 3). We identified nine patients (8.3%) with major depression and 12 patients (11.0%) with PTSD who could be regarded as ‘missed’ patients, that is, they did not use mental healthcare despite an SCID-based major depression/PTSD diagnosis at T2 (online supplemental table 3).
Table 2.
Frequency of patients consulting mental healthcare specialty, 3 (T2) and 6 (T3) months following the transfer from acute-care ICU
| Mental healthcare specialty consulted, n (%) | ||
| T2 n=30 | T3 n=29 | |
| Clinical psychologist/psychotherapist at rehabilitation hospital | 13 (43.3) | 11 (37.9) |
| General practitioner | 11 (36.7) | 11 (37.9) |
| Outpatient psychiatrist | 2 (6.7) | 4 (13.8) |
| Outpatient psychotherapist | 2 (6.7) | 3 (10.3) |
| Neck nose ear doctor | 1 (3.3) | – |
| Other* | 1 (3.3) | – |
The numbers refer to a sample of 30 patients at T2 and 29 patients at T3, reporting the consultation of a mental healthcare specialist.
*One patient was psychologist and made use of conversations with his/ her colleagues
ICU, intensive care unit.
Table 3.
Frequency of reasons for not consulting a mental healthcare specialist at T2 and T3
| Reasons why mental healthcare specialty was not consulted, n (%) | ||
| T2 n=82 | T3 n=70 | |
| I have not yet thought about mental healthcare. | 21 (25.6) | 13 (18.6) |
| I have not found an appropriate psychotherapist/or have not yet got an appointment. | 7 (8.5) | 5 (7.1) |
| I refuse psychotherapy. | 6 (7.3) | 12 (17.1) |
| Other reasons* | 46 (56.1) | 40 (57.1) |
| I do not need mental healthcare. | 29 (63.0) | 22 (55.0) |
| Somatic complaints are more important. | 8 (17.4) | 12 (30.0) |
| Family/ friends help me. | 4 (8.7) | – |
| Mental healthcare does not help. | 2 (4.3) | 1 (2.5) |
| I have other specialists/ physicians (eg, general practitioner) caring for me. | 1 (2.2) | 3 (7.5) |
| I have not yet had time. | – | 2 (5) |
The numbers refer to a sample of 82 patients at T2 and 70 patients at T3.
*n = 2 missing values.
At T2, 21 (18.8%) of the patients reported that they are interested in receiving a list with addresses from outpatient psychotherapists, close to their home. Thirty-nine patients (35.1%) reported having consulted a psychotherapist or psychiatrist in their life time.
Frequency of mental healthcare utilisation at T3 (6 months following the transfer from acute-care ICU)
Among the 99 patients with data at T3, 29 (29.3%) reported that they had already consulted a mental health specialist because of their current psychological complaints since they were transferred from acute-care ICU. Most of these patients consulted a clinical psychologist/psychotherapist (during their rehabilitation) (table 2). 70.7% of the patients have not visited a mental healthcare specialist. Less than one-fifth of those patients reported to have not yet thought about it and more than every second reported other reasons, why mental healthcare was not consulted, for example, patients reported that they did not need it or somatic complaints were more important, among others (table 3). We identified 7 patients (7.1%) with major depression and 12 patients (12.2%) with PTSD who could be regarded as ‘missed’ patients, that is, they reported no use of mental healthcare but presented a clinically relevant, SCID-based mental disorder at T2 and/or T3 (online supplemental table 3).
At T3, n=17 (17.3%) of the patients reported that they are interested in receiving a list with addresses from outpatient psychotherapists close to their home.
Sociodemographic, contextual, medical and psychological predictors for mental healthcare utilisation (3/T2 and 6/T3 months following the transfer from acute-care ICU)
In univariate regression analyses, several potential predictors (p≤0.1) for the use of mental healthcare services could be identified. At T2, female gender, a larger number of traumatic memories from ICU, previous use of psychotherapy and a pre-existing F-diagnosis (eg, major depression, anxiety disorders, substance use disorders) were associated with mental healthcare utilisation. At T3, pension receipt, the number of somatic comorbidities, number of sepsis episodes, a diagnosis of acute stress disorder/PTSD and a higher PTSS-10 score at T2 turned out to impact mental healthcare utilisation. Among the documented F-diagnoses, a pre-existing anxiety disorder increased and harmful nicotine consumption, by trend, decreased the use of mental healthcare services (online supplemental table 4).
In the final multivariable regression model, female gender (OR 2.860, CI 95% 1.037 to 7.883, p=0.042), previous psychotherapy (OR 3.083, 95% CI 1.169 to 8.135, p=0.023) and a pre-existing F-diagnosis (OR.270, 95% CI 0.091 to 0.802, p=0.081) were confirmed as significant predictors of mental healthcare utilisation at T2 (table 4). The number of sepsis episodes (OR 2.203, 95% CI 1.135 to 4.278, p=0.020) and pension receipt (OR 4.508, 95% CI 1.013 to 20.055, p=0.048) significantly increased the chance for mental healthcare utilisation at T3 (table 5). The model explained a variance of 25.2% (T2) and 32.4% (T3), respectively.
Table 4.
Association between the use of mental healthcare services at T2 as the primary outcome and sociodemographic, medical and psychological variables as independent variables, in a multivariable logistic regression model controlled for age and gender
| Multivariable logistic regression† (n=112) | |||
| OR | 95% CI | p value | |
| Age | 0.706 | .426 to 1.168 | 0.175 |
| Gender | 2.860 | 1.037 to 7.883 | .042* |
| Traumatic memories from ICU (T2)2 | 1.534 | .907 to 2.595 | 0.111 |
| Previous psychotherapy | 3.083 | 1.169 to 8.135 | .023* |
| Pre-existing F-diagnosis‡ | 0.270 | .091 to.802 | .018* |
| Cox & Snell R²/Nagelkerke R² | .171/0.252 | ||
Bold numbers indicate significance.
*p≤0.05.
†Method of multivariable logistic regression: enter, n=2 patients with missing values.
‡Including anxiety disorders, depressive disorders, harmful alcohol consumption, harmful nicotine consumption, organic brain syndrome, dementia, dissociative disorder of movement.
ICU, intensive care unit.
Table 5.
Association between the use of mental healthcare services at T3 as primary outcome and sociodemographic, medical and psychological variables as independent variables, in a multivariable logistic regression model corrected for age and gender
| Multivariable logistic regression† (n=99) | |||
| OR | 95% CI | p value | |
| Age | 1.069 | .539 to 2.119 | 0.849 |
| Gender | 0.765 | .206 to 2.847 | 0.690 |
| PTSS-10 score (T2) | 1.526 | .887 to 2.625 | 0.127 |
| Number of somatic comorbidities | 1.742 | .931 to 3.259 | 0.083 |
| Number of sepsis episodes | 2.203 | 1.135 to 4.278 | .020* |
| Pension receipt (yes) | 4.508 | 1.013 to 20.055 | .048* |
| Cox & Snell R²/Nagelkerke R² | .224/0.324 | ||
Bold numbers indicate significance.
*p≤0.05; Diagnosis of Acute Stress Disorder (T1) and diagnosis of PTSD (T2/T3) were not included in the final analyses due to small rates of occurrence and large confidence intervals.
†Method of multivariable logistic regression: Enter, n=99 patients.
PTSD, post-traumatic stress disorder; PTSS-10, Post-Traumatic Stress Syndrome 10-Inventory.
Discussion and conclusions
Discussion
In the present study, we examined the rate of patients utilising mental healthcare services following the long-term stay on ICU. We were further interested in factors associated with this utilisation. Our results show that about one quarter of the patients (27%–29%) reported the use of mental healthcare. Patients having experience with psychotherapy, a higher number of sepsis episodes and receiving a pension more likely reported the utilisation of mental healthcare services following ICU. Male gender and pre-existing F-diagnosis could be identified as impeding factors.
To the best of our knowledge, our study was the first to examine the use of mental healthcare in patients after prolonged ICU stay. Indeed, patient data on mental healthcare utilisation in patients with or without a PTSD or major depression following ICU discharge are still lacking. In our study, the rates of mental healthcare utilisation lie within the range of median point prevalences for PTSD and depression following ICU discharge.4–8 A similar rate of 30% (at the 24-month follow-up) was found in patients surviving acute lung injury,42 while another study reported lower rates (eg, 11.8%) as compared with our rates of 27% to 29%.43 However, the latter study assessed the lifetime-prevalence of recourse to psychotherapy in a well-informed, general population with high-quality insurance cover in France, limiting the comparability with our ICU sample.43 It is well known that patients with a history of a critical illness and intensive care are more likely to visit a mental healthcare specialist (eg, psychiatry) than the general population.14 Nevertheless, it can be assumed that the actual need for healthcare utilisation is even higher than the current use of it. In this regard, nearly two-thirds (63.8%) of hospital physicians reported a moderate or strong need for psychological support in their ICU patients.24
The high self-reported rates of 26.8% at T2 and 29.3% at T3, as found in our present study, may be explained by the fact that we did not differentiate between reference to a psychotherapist, psychiatrist, psychosomatic physician or neurologist, but rather summarised these professions as providers of mental healthcare in general. It is conceivable that, in our sample, the high rate of patients suffering from neurological disorders (24.1%) was already treated by in/outpatient neurologists, who probably also cared for unspecific symptoms like sleep disturbance or psychiatric symptoms, for example, by prescribing psychotropic drugs.44
However, in our study, about every tenth patient with a clinically relevant PTSD/depression had not received mental healthcare so far. As main reasons, the patients reported that they had not yet thought about mental healthcare or they did not need mental healthcare because somatic complaints were more important. The focus on the physical aspects of recovery is consistent with Atkin’s biopsychosocial model of recovery for children surviving an acute life-threatening critical illness.45 According to this model, the emotional and social processing can only be achieved when the physical health or ‘new normal’ is restored.
Furthermore, it can be assumed that patients surviving prolonged intensive care are not well informed about mental long-term sequelae possibly occurring following ICU treatment. One reason may be that physicians in the ICU setting lack sufficient knowledge about the assessment of psychological sequelae after intensive care. Another interesting finding is that more patients affected with major depression were correctly allocated to mental healthcare than patients with PTSD. This discrepancy alludes that awareness for PTSD should be raised, both in physicians and patients.22 In addition, there seems to be a lack of knowledge about mental healthcare options. Following, after-care should include a regular monitoring of clinically relevant symptoms of mental disorders in all patients following a prolonged ICU stay. The latter could be realised, for example, by the patients’ general practitioner, at least in the first year following ICU discharge.46 This is in line with the fact that, in our present study, a large number of patients received psychological support by their general practitioner following the ICU stay, which comprised periodic contacts, referrals to specialists and prescription of medication.47
On the one hand, about every tenth patient in need (with a diagnosed PTSD and/or major depression) did not receive appropriate help. On the other hand, quite a high rate of patients (for PTSD: 21.1%, for major depression: 25.7%) used mental healthcare although no PTSD and/or major depression was diagnosed. This result may underline the peculiarity of the present setting, that is, treatment in a rehabilitation hospital with integrated care by clinical psychologists and neuropsychologists.
The present study revealed that women more often made use of mental healthcare consultation following a prolonged ICU stay compared with men. Although female gender was repeatedly associated with an increased risk for mental disorders in the general population,48 it could not be identified as consistent predictor in the ICU population.6 9 The inconsistency of results may be related to the kind of mental disorders, which have been assessed in previous studies. While affective disorders are more prevalent in women, some mental disorders are more prevalent in men (eg, substance use disorders) or similarly prevalent in both men and women (eg, psychosis).49 50 In our study, we only assessed symptoms and the diagnoses of PTSD as well as major depression, which may explain the finding that female gender is associated with increased mental healthcare utilisation. Additionally, it should be noticed that women tend to identify sources of stress more clearly and use functional coping strategies such as seeking help by mental healthcare specialists more often than men.51 In contrast, men have been described as being more prone to emotional inhibition and increased substance abuse in case of stress.48 52 53
Moreover, we found an impact of pension receipt, increasing the probability of mental healthcare utilisation by the factor 4. Two explanations may be relevant for this effect. First, the receipt of a disability pension demands regular assessment by a mental healthcare specialist and necessitates treatment by a respective specialist. Second, it is known that mental disorders are among the most frequent reasons for pension receipt, leading to a higher mental healthcare utilisation.54
Medical variables, for example, number of somatic comorbidities and number of sepsis episodes, seem to have a greater impact on the use of mental healthcare than sociodemographic factors. It has been previously shown that medical comorbidities constitute a risk factor for the development of mental disorders.55 Medically ill patients with comorbid mental disorders are often exposed to stigmatisation, a worse quality of care, higher hospitalisation rates and an increased mortality.56 57 It is conceivable that the burden of medical illnesses and diminished quality of life make these patients more vulnerable to the development of mental disorders.
Above, sepsis turned out to be associated with an increased risk for PTSD,10 58 promoting the need for mental healthcare. Sepsis, multiple-organ dysfunction and peripheral circulatory failure may increase the risk of traumatic experiences on ICU (eg, respiratory distress, panic, pain), which can trigger a massive stress response and an overexposure to important stress mediators such as epinephrine and cortisol.59 Moreover, additional catecholamines are often required, leading to an intensification of the stress response. This may foster the formation and consolidation of traumatic memories and could increase the risk of PTSD in these patients.60
As psychological factors, an acute stress disorder/PTSD turned out to be significantly associated with the use of mental healthcare services. These patients may be more vulnerable for higher intensive care distress, anxiety and delirious symptoms.12 This may lead to clinically relevant affective symptoms following ICU discharge, requiring the use of mental healthcare services, as in the present sample of ICU patients. Accordingly, recent evidence showed that panic symptoms were positively associated with the utilisation of mental health services.61
Nevertheless, we could find that a pre-existing F-diagnosis (according to ICD-10) decreased the probability of mental healthcare utilisation by 73%. This may be mainly attributed to the kind of diagnoses documented in the patients’ health records. Particularly, substance use disorders, such as harmful nicotine consumption, were considered as mental disorders in the present study. The latter display rather socially accepted disorders, going along with little insight into the need for change and low therapy motivation. Above, the stigma perceived by these people and lack of adequate mental healthcare services may additionally contribute to a decreased help seeking.62 Finally, substance use disorders can be seen as a result of dysfunctional coping strategies applied for the purpose of experiential avoidance and to relieve emotional and physical discomfort. Other findings suggest smoking as a means of self-medication of psychiatric symptoms.63 The latter is contradictory to the intentions of psychotherapy and psychological support, as supplied by mental healthcare specialists.
In contrast, a pre-existing anxiety disorder increased the use of mental healthcare in our study. This finding is supported by the fact that anxiety disorders often go along with substantial comorbidity and cause significant disability in everyday life.64 In line, research corroborated that not the characteristics of the specific disorder per se but the psychiatric comorbidity and perceived disability influence the use of mental healthcare.65
Moreover, pre-existing mental disorders are often associated with the prior use of psychological support, as shown by the positive impact of previous psychotherapy on the current use of mental healthcare in our sample. Previous evidence hints towards a positive effect of the internalised representations of the psychotherapeutic relationship on the therapy outcome. Therefore, it can be supposed that patients with positive representations of a past psychotherapy are more likely to seek mental help again.66
The final regression models only explained a small proportion of variance in the use of mental healthcare services (25% and 32%). Hence, above and beyond the considered variables, other factors may play a more prominent role in the use of mental healthcare services. One major factor could be the availability of mental healthcare services, determining the access to this type of treatment.43 One indirect measure for the availability and use of mental healthcare may be the place of residence. In the present study, the impact of the place of residence on mental healthcare utilisation could be ruled out. A recent systematic review also showed only a little effect of urban/rural residence on treatment-seeking rates.61 However, direct information on the access to psychotherapy was not retrieved. Therefore, in particular, contextual level factors (eg, the availability of services, geographical accessibility of those services, characteristics of services such as accessibility for handicapped) should be evaluated in future examinations on this topic.61 Above, future research should further investigate which patients were referred to which kind of treatment (whether psychiatrist, psychotherapist or both, psychopharmacological vs non-pharmacological treatment, respectively) and whether the specific referral was appropriate with respect to the management of mental disorders.
The present results should be critically evaluated within methodological shortcomings, limiting the generalisability. First of all, the present study is a reanalysis of a data set originally collected in order to investigate the rates and predictors of acute and PTSD in patients following prolonged critical illness.10 The generalisability is restricted to patients treated at a rehabilitation hospital with an integrated care by clinical psychologists and psychotherapists. Both supposedly raised awareness for psychological distress and the need for psychological support by psychoeducating intensive care physicians and affected patients. In line with the study protocol, patients with a diagnosed acute stress disorder were informed about the diagnosis and were offered an appointment with a clinical psychologist. This may have led to a quite high number of patients using mental healthcare in our present study. At T2 and T3, patients with the diagnosis of a PTSD or major depression during the SCID were informed about it and offered support by receiving addresses from outpatient psychotherapists. However, data did not show a systematic impact of request for support at T2 and help seeking at T3.
We included a rather small number of patients with a primary diagnosis of CIP/CIM, because there was a high dropout rate in this patient population due to an increased mortality risk and risk for medical complications.67 Consequently, only a small rate of patients showed a full syndromal manifestation of PTSD or major depression. In addition, the sample was biased towards older and male patients, which may have led to distorted response rates. Furthermore, we did not conduct the full SCID-I interview, and our assessment was based on the DSM-IV and not the DSM-V. Thus, the discrepancy between patients making use of mental healthcare and those who actually need it could not be fully described in the present study. Moreover, some patients presumably do not know what psychotherapy actually is. Thus, these patients may not have clearly understood the question whether psychotherapy has already been used. In general, conclusions should be drawn with the utmost caution because information on prior psychopathology and prior use of psychotherapy were assessed retrospectively and may be prone to memory bias. Furthermore, one may assume that specialists other than mental health professionals may have avoided making and documenting a diagnosis of mental disorders—partly because of their uncertainty about the diagnosis as well as treatment of psychological comorbidities or because they wanted to avoid stigmatisation of their patients.68 Thus, the diagnoses retrieved from the patient’s health records may not be sufficiently reliable and could have led to an underestimation of the frequency of pre-existing mental disorders.
Finally, it should be noted that the study was actually planned to assess the rate and predictors of PTSD following the long-term treatment on ICU in chronically critically ill patients.10 The findings were dated to be almost 10 years old, which could restrict their generalisability to a non-pandemic situation. Currently, during the COVID-19 epidemic, healthcare professionals are faced with a high stress load, which may have affected the perception of the need for mental healthcare of somatically ill patients.69 70 Taken the psychological burden in patients surviving protracted mechanical ventilation and ICU stay due to a COVID-19 infection, we decided to reanalyse our data focusing on mental healthcare utilisation in a comparable group of patients. More than three quarter of our patients suffered from an acute respiratory insufficiency, which may lead to ARDS. ARDS displays a common lung disease following the infection with the SARS-CoV-2,71 necessitating mechanical ventilation to maintain adequate gas exchange.72
Conclusions
Our results suggest that about one quarter of patients surviving prolonged ICU stay utilises mental healthcare services in the follow-up. There is a discrepancy between the need for and the reality of care in at least every tenth of these patients. Mental healthcare is more frequently used by women, patients receiving a pension, patients with a higher number of sepsis episodes and with previous experience in psychotherapy. Factors impeding the utilisation of mental healthcare are male gender and pre-existing F-diagnoses, in particular, harmful nicotine consumption.
The findings allude that patients should be routinely screened for major depression and post-traumatic distress at discharge from ICU. Assessment should be repeated regularly at least during the first year following the ICU discharge. Additionally, factors promoting and impeding mental healthcare should be acquired since they may give hints towards how to better motivate patients in seeking appropriate mental healthcare. Particularly, patients should at least be asked about previous experiences with psychotherapy. As a priority, men and patients with previous mental disorders, primarily harmful nicotine consumption, should be sensitised and educated about mental health problems following the prolonged ICU treatment. Specialised and tailored education programmes should be designed in order to support patients in need but with little use of mental healthcare services.
Practice implications and innovation
Our findings emphasise that structured case management, caring for patients surviving prolonged ICU treatment, should improve education and awareness about both post-traumatic distress and major depression in these patients.61 Additionally, patients’ access to psychotherapists and other mental healthcare specialists should be fostered.19 In future research, appropriate rehabilitation programmes addressing these psychological long-term sequelae should be installed and evaluated, particulary in the most vulnerable and affected patient groups.3 Furthermore, patient education should inform these patients about their potential risk for the development of a mental disorder after ICU, and which services for mental healthcare exist. In this regard, it should also be clarified what mental healthcare comprises, and which kind of mental healthcare is appropriate in terms of both relevance and adequate duration, depending on the mental distress and problems following prolonged intensive care. Education about the psychological burdens and disorders might reduce barriers for adequate help seeking. Finally, strategies to address potential healthcare inequities for men and elderly ICU patients as well as patients with certain pre-existing mental disorders (eg, substance use disorers) require further evaluation.61 Currently, new approaches using behavior change techniques (eg, active problem-solving, active assistance, reinforcement of positive male traits, improvement in mental health knowledge, positive role models) have been developed and may contribute to an improvement in male help-seeking interventions.73
Supplementary Material
Acknowledgments
We would like to thank Stefan Rückriem, Sara Wüstemann, Corinna Klotzsche and Clara Buck for their great support in patient enrolment. We are also grateful to Katja Petrowski for giving scientific advice on the realisation of the present study.
Footnotes
Contributors: All co-authors substantially contributed to the conception and design, drafting and final approval of the present work. G-BW and JR planned and conceptualised the present study and methodology. Both were responsible for data curation and analyses, visualisation and writing of the original manuscript draft. G-BW is the responsible guarantor of the present study, conducting the study, controlling data access, analyses and decision to publish. KW and BS supervised the realisation of the present study and reviewed the final manuscript.
Funding: This study was supported by the German Federal Ministry of Education and Research grant (01EO1002).
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available upon reasonable request and will be available in a public, open access repository after acceptance of the manuscript.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study involves human participants and was approved by Ethics Committee of the Jena University Hospital, EK: 3278-10/11/11. Participants gave informed consent to participate in the study before taking part.
References
- 1.Devita M, Di Rosa E, Iannizzi P, et al. Cognitive and psychological sequelae of COVID-19: age differences in facing the pandemic. Front Psychiatry 2021;12:711461. 10.3389/fpsyt.2021.711461 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Needham DM, Davidson J, Cohen H, et al. Improving long-term outcomes after discharge from intensive care unit: report from a stakeholders' conference. Crit Care Med 2012;40:502–9. 10.1097/CCM.0b013e318232da75 [DOI] [PubMed] [Google Scholar]
- 3.Elliott D, Davidson JE, Harvey MA, et al. Exploring the scope of post-intensive care syndrome therapy and care: engagement of non-critical care providers and survivors in a second stakeholders meeting. Crit Care Med 2014;42:2518–26. 10.1097/CCM.0000000000000525 [DOI] [PubMed] [Google Scholar]
- 4.Davydow DS, Desai SV, Needham DM, et al. Psychiatric morbidity in survivors of the acute respiratory distress syndrome: a systematic review. Psychosom Med 2008;70:512–9. 10.1097/PSY.0b013e31816aa0dd [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Davydow DS, Gifford JM, Desai SV, et al. Depression in general intensive care unit survivors: a systematic review. Intensive Care Med 2009;35:796–809. 10.1007/s00134-009-1396-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Davydow DS, Gifford JM, Desai SV, et al. Posttraumatic stress disorder in general intensive care unit survivors: a systematic review. Gen Hosp Psychiatry 2008;30:421–34. 10.1016/j.genhosppsych.2008.05.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nikayin S, Rabiee A, Hashem MD, et al. Anxiety symptoms in survivors of critical illness: a systematic review and meta-analysis. Gen Hosp Psychiatry 2016;43:23–9. 10.1016/j.genhosppsych.2016.08.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rabiee A, Nikayin S, Hashem MD, et al. Depressive symptoms after critical illness: a systematic review and meta-analysis. Crit Care Med 2016;44:1744–53. 10.1097/CCM.0000000000001811 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Parker AM, Sricharoenchai T, Raparla S, et al. Posttraumatic stress disorder in critical illness survivors: a metaanalysis. Crit Care Med 2015;43:1121–9. 10.1097/CCM.0000000000000882 [DOI] [PubMed] [Google Scholar]
- 10.Wintermann G-B, Brunkhorst FM, Petrowski K, et al. Stress disorders following prolonged critical illness in survivors of severe sepsis. Crit Care Med 2015;43:1213–22. 10.1097/CCM.0000000000000936 [DOI] [PubMed] [Google Scholar]
- 11.Davydow DS, Hough CL, Langa KM, et al. Symptoms of depression in survivors of severe sepsis: a prospective cohort study of older Americans. Am J Geriatr Psychiatry 2013;21:887–97. 10.1016/j.jagp.2013.01.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wade DM, Howell DC, Weinman JA, et al. Investigating risk factors for psychological morbidity three months after intensive care: a prospective cohort study. Crit Care 2012;16:R192. 10.1186/cc11677 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Brown SM, Bose S, Banner-Goodspeed V, et al. Approaches to addressing Post-Intensive care syndrome among intensive care unit survivors. A narrative review. Ann Am Thorac Soc 2019;16:947–56. 10.1513/AnnalsATS.201812-913FR [DOI] [PubMed] [Google Scholar]
- 14.Kosilek RP, Baumeister SE, Ittermann T, et al. The association of intensive care with utilization and costs of outpatient healthcare services and quality of life. PLoS One 2019;14:e0222671. 10.1371/journal.pone.0222671 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Peris A, Bonizzoli M, Iozzelli D, et al. Early intra-intensive care unit psychological intervention promotes recovery from post traumatic stress disorders, anxiety and depression symptoms in critically ill patients. Crit Care 2011;15:R41. 10.1186/cc10003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gawlytta R, Niemeyer H, Böttche M, et al. Internet-Based cognitive-behavioural writing therapy for reducing post-traumatic stress after intensive care for sepsis in patients and their spouses (repair): study protocol for a randomised-controlled trial. BMJ Open 2017;7:e014363. 10.1136/bmjopen-2016-014363 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jones C. Over 20 years of ICU diary research 1999-2020. Intensive Crit Care Nurs 2021;64:102961. 10.1016/j.iccn.2020.102961 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bäckman CG, Orwelius L, Sjöberg F, et al. Long-Term effect of the ICU-diary concept on quality of life after critical illness. Acta Anaesthesiol Scand 2010;54:736–43. 10.1111/j.1399-6576.2010.02230.x [DOI] [PubMed] [Google Scholar]
- 19.Gehrke-Beck S, Bänfer M, Schilling N, et al. The specific needs of patients following sepsis: a nested qualitative interview study. BJGP Open 2017;1:bjgpopen17X100725. 10.3399/bjgpopen17X100725 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wintermann G-B, Weidner K, Strauß B, et al. Predictors of posttraumatic stress and quality of life in family members of chronically critically ill patients after intensive care. Ann Intensive Care 2016;6:69. 10.1186/s13613-016-0174-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ruttley A, Reid S. Depression in physical illness. Clin Med 2006;6:533–5. 10.7861/clinmedicine.6-6-533 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Smith JR, Workneh A, Yaya S. Barriers and facilitators to help-seeking for individuals with posttraumatic stress disorder: a systematic review. J Trauma Stress 2020;33:137–50. 10.1002/jts.22456 [DOI] [PubMed] [Google Scholar]
- 23.Rosenblat JD, Kurdyak P, Cosci F, et al. Depression in the medically ill. Aust N Z J Psychiatry 2020;54:346–66. 10.1177/0004867419888576 [DOI] [PubMed] [Google Scholar]
- 24.Niecke A, Hartog C, Deffner T, et al. Need for psychological support in intensive care : A survey among members of the German Society of Medical Intensive Care and Emergency Medicine. Med Klin Intensivmed Notfmed 2020;115:135–9. 10.1007/s00063-018-0523-x [DOI] [PubMed] [Google Scholar]
- 25.Wintermann G-B, Rosendahl J, Weidner K, et al. Risk factors of delayed onset posttraumatic stress disorder in chronically critically ill patients. J Nerv Ment Dis 2017;205:780–7. 10.1097/NMD.0000000000000714 [DOI] [PubMed] [Google Scholar]
- 26.Wintermann G-B, Rosendahl J, Weidner K, et al. Predictors of major depressive disorder following intensive care of chronically critically ill patients. Crit Care Res Pract 2018;2018:1–9. 10.1155/2018/1586736 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wintermann G-B, Rosendahl J, Weidner K, et al. Fatigue in chronically critically ill patients following intensive care - reliability and validity of the multidimensional fatigue inventory (MFI-20). Health Qual Life Outcomes 2018;16:37. 10.1186/s12955-018-0862-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wintermann G-B, Rosendahl J, Weidner K, et al. Self-Reported fatigue following intensive care of chronically critically ill patients: a prospective cohort study. J Intensive Care 2018;6:27. 10.1186/s40560-018-0295-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Schönle PW. Neurological Rehabilitation in Germany. In: Christensen A-LU BP, ed. The phase model international Handbook of neurological rehabilitation. New York: Springer, 2010: 327–38. [Google Scholar]
- 30.World Health O. ICD-10 : international statistical classification of diseases and related health problems : tenth revision. 2nd. Geneva: World Health Organization, 2004. [Google Scholar]
- 31.Rollnik JD. The early rehabilitation Barthel index (ERBI). Rehabilitation 2011;50:408–11. 10.1055/s-0031-1273728 [DOI] [PubMed] [Google Scholar]
- 32.Schönle PW. Frühe Phasen Der Neurologischen rehabilitation: Differentielle Schweregradbeurteilung bei Patienten in Der phase B (Frührehabilitation) und in Der phase C (Frühmobilisation/ Postprimäre rehabilitation) MIT Hilfe des Frühreha-Barthel-Index (FRB). Neurologie & Rehabilitation 1996;1:21–5. [Google Scholar]
- 33.Sullivan SB, Schmitz TJ. Physical rehabilitation. Philadelphia, PA: F.A. Davis, 2007. [Google Scholar]
- 34.Helfricht S, Landolt MA, Moergeli H, et al. Psychometric evaluation and validation of the German version of the acute stress disorder scale across two distinct trauma populations. J Trauma Stress 2009;22:476–80. 10.1002/jts.20445 [DOI] [PubMed] [Google Scholar]
- 35.Wittchen H-U, Zaudig M, Fydrich T. Strukturiertes Klinisches Interview für DSM-IV. Göttingen: Hogrefe, 1997. [Google Scholar]
- 36.Lobbestael J, Leurgans M, Arntz A. Inter-Rater reliability of the structured clinical interview for DSM-IV axis I disorders (SCID I) and axis II disorders (SCID II). Clin Psychol Psychother 2011;18:75–9. 10.1002/cpp.693 [DOI] [PubMed] [Google Scholar]
- 37.Raphael B, Lundin T, Weisaeth L. A research method for the study of psychological and psychiatric aspects of disaster. Acta Psychiatr Scand Suppl 1989;353:1–75. 10.1111/j.1600-0447.1989.tb03041.x [DOI] [PubMed] [Google Scholar]
- 38.Stoll C, Kapfhammer HP, Rothenhäusler HB, et al. Sensitivity and specificity of a screening test to document traumatic experiences and to diagnose post-traumatic stress disorder in ARDS patients after intensive care treatment. Intensive Care Med 1999;25:697–704. 10.1007/s001340050932 [DOI] [PubMed] [Google Scholar]
- 39.Thulesius H, Håkansson A. Screening for posttraumatic stress disorder symptoms among Bosnian refugees. J Trauma Stress 1999;12:167–74. 10.1023/A:1024758718971 [DOI] [PubMed] [Google Scholar]
- 40.Faul F, Erdfelder E, Lang A-G, et al. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods 2007;39:175–91. 10.3758/BF03193146 [DOI] [PubMed] [Google Scholar]
- 41.Boer KR, van Ruler O, van Emmerik AAP, et al. Factors associated with posttraumatic stress symptoms in a prospective cohort of patients after abdominal sepsis: a nomogram. Intensive Care Med 2008;34:664–74. 10.1007/s00134-007-0941-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bienvenu OJ, Gellar J, Althouse BM, et al. Post-Traumatic stress disorder symptoms after acute lung injury: a 2-year prospective longitudinal study. Psychol Med 2013;43:2657–71. 10.1017/S0033291713000214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Briffault X, Sapinho D, Villamaux M, et al. Factors associated with use of psychotherapy. Soc Psychiatry Psychiatr Epidemiol 2008;43:165–71. 10.1007/s00127-007-0281-1 [DOI] [PubMed] [Google Scholar]
- 44.Altman MT, Knauert MP, Pisani MA. Sleep disturbance after hospitalization and critical illness: a systematic review. Ann Am Thorac Soc 2017;14:1457–68. 10.1513/AnnalsATS.201702-148SR [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Atkins E, Colville G, John M. A 'biopsychosocial' model for recovery: a grounded theory study of families' journeys after a Paediatric Intensive Care Admission. Intensive Crit Care Nurs 2012;28:133–40. 10.1016/j.iccn.2011.12.002 [DOI] [PubMed] [Google Scholar]
- 46.Ibrahim H, Athar S, Harhara T, et al. Post-Infectious and post-acute sequelae of critically ill adults with COVID-19. PLoS One 2021;16:e0252763. 10.1371/journal.pone.0252763 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Schmidt K, Worrack S, Von Korff M, et al. Effect of a primary care management intervention on mental health-related quality of life among survivors of sepsis: a randomized clinical trial. JAMA 2016;315:2703–11. 10.1001/jama.2016.7207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Jacobi F, Höfler M, Strehle J, et al. Twelve-months prevalence of mental disorders in the German Health Interview and Examination Survey for Adults - Mental Health Module (DEGS1-MH): a methodological addendum and correction. Int J Methods Psychiatr Res 2015;24:305–13. 10.1002/mpr.1479 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wittchen H-U, Jacobi F. Size and burden of mental disorders in Europe--a critical review and appraisal of 27 studies. Eur Neuropsychopharmacol 2005;15:357–76. 10.1016/j.euroneuro.2005.04.012 [DOI] [PubMed] [Google Scholar]
- 50.Wittchen HU, Jacobi F, Rehm J, et al. The size and burden of mental disorders and other disorders of the brain in Europe 2010. Eur Neuropsychopharmacol 2011;21:655–79. 10.1016/j.euroneuro.2011.07.018 [DOI] [PubMed] [Google Scholar]
- 51.Jerg-Bretzke L, Kempf M, Jarczok MN, et al. Psychosocial impact of the COVID-19 pandemic on healthcare workers and initial areas of action for intervention and Prevention-The egePan/VOICE study. Int J Environ Res Public Health 2021;18. 10.3390/ijerph181910531. [Epub ahead of print: 07 Oct 2021]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Dawson DA, Grant BF, Ruan WJ. The association between stress and drinking: modifying effects of gender and vulnerability. Alcohol Alcohol 2005;40:453–60. 10.1093/alcalc/agh176 [DOI] [PubMed] [Google Scholar]
- 53.Matud MP, Bethencourt JM, Ibáñez I. Gender differences in psychological distress in Spain. Int J Soc Psychiatry 2015;61:560–8. 10.1177/0020764014564801 [DOI] [PubMed] [Google Scholar]
- 54.Rahman S, Mittendorfer-Rutz E, Alexanderson K, et al. Disability pension due to common mental disorders and healthcare use before and after policy changes; a nationwide study. Eur J Public Health 2017;27:90–6. 10.1093/eurpub/ckw211 [DOI] [PubMed] [Google Scholar]
- 55.Härter M, Baumeister H, Reuter K, et al. Increased 12-month prevalence rates of mental disorders in patients with chronic somatic diseases. Psychother Psychosom 2007;76:354–60. 10.1159/000107563 [DOI] [PubMed] [Google Scholar]
- 56.Gervaix J, Haour G, Michel M, et al. Impact of mental illness on care for somatic comorbidities in France: a nation-wide hospital-based observational study. Epidemiol Psychiatr Sci 2019;28:495–507. 10.1017/S2045796018000203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Correll CU, Solmi M, Veronese N, et al. Prevalence, incidence and mortality from cardiovascular disease in patients with pooled and specific severe mental illness: a large-scale meta-analysis of 3,211,768 patients and 113,383,368 controls. World Psychiatry 2017;16:163–80. 10.1002/wps.20420 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Boer KR, Mahler CW, Unlu C, et al. Long-Term prevalence of post-traumatic stress disorder symptoms in patients after secondary peritonitis. Crit Care 2007;11:R30. 10.1186/cc5710 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Zhang Q, Dong G, Zhao X, et al. Prognostic significance of hypothalamic-pituitary-adrenal axis hormones in early sepsis: a study performed in the emergency department. Intensive Care Med 2014;40:1499–508. 10.1007/s00134-014-3468-4 [DOI] [PubMed] [Google Scholar]
- 60.Schelling G, Briegel J, Roozendaal B, et al. The effect of stress doses of hydrocortisone during septic shock on posttraumatic stress disorder in survivors. Biol Psychiatry 2001;50:978–85. 10.1016/S0006-3223(01)01270-7 [DOI] [PubMed] [Google Scholar]
- 61.Roberts T, Miguel Esponda G, Krupchanka D, et al. Factors associated with health service utilisation for common mental disorders: a systematic review. BMC Psychiatry 2018;18:262. 10.1186/s12888-018-1837-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Edlund MJ, Booth BM, Han X. Who seeks care where? utilization of mental health and substance use disorder treatment in two national samples of individuals with alcohol use disorders. J Stud Alcohol Drugs 2012;73:635–46. 10.15288/jsad.2012.73.635 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Lasser K, Boyd JW, Woolhandler S, et al. Smoking and mental illness: a population-based prevalence study. JAMA 2000;284:2606–10. 10.1001/jama.284.20.2606 [DOI] [PubMed] [Google Scholar]
- 64.Alonso J, Liu Z, Evans-Lacko S, et al. Treatment gap for anxiety disorders is global: results of the world mental health surveys in 21 countries. Depress Anxiety 2018;35:195–208. 10.1002/da.22711 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Hämäläinen J, Isometsä E, Sihvo S, et al. Use of health services for major depressive and anxiety disorders in Finland. Depress Anxiety 2008;25:27–37. 10.1002/da.20256 [DOI] [PubMed] [Google Scholar]
- 66.Geller J, Farber B. Factors influencing the process of internalization in psychotherapy. Psychotherapy Research 1993;3:166–80. 10.1080/10503309312331333769 [DOI] [Google Scholar]
- 67.Hermans G, De Jonghe B, Bruyninckx F, et al. Clinical review: critical illness polyneuropathy and myopathy. Crit Care 2008;12:238. 10.1186/cc7100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Sartorious N. Comorbidity of mental and physical diseases: a main challenge for medicine of the 21st century. Shanghai Arch Psychiatry 2013;25:68–9. 10.3969/j.issn.1002-0829.2013.02.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Laurent A, Fournier A, Lheureux F, et al. Mental health and stress among ICU healthcare professionals in France according to intensity of the COVID-19 epidemic. Ann Intensive Care 2021;11:90. 10.1186/s13613-021-00880-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Ornell F, Borelli WV, Benzano D, et al. The next pandemic: impact of COVID-19 in mental healthcare assistance in a nationwide epidemiological study. Lancet Reg Health Am 2021;4:100061. 10.1016/j.lana.2021.100061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Aslan A, Aslan C, Zolbanin NM, et al. Acute respiratory distress syndrome in COVID-19: possible mechanisms and therapeutic management. Pneumonia 2021;13:14. 10.1186/s41479-021-00092-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Ochiai R. Mechanical ventilation of acute respiratory distress syndrome. J Intensive Care 2015;3:25. 10.1186/s40560-015-0091-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Sagar-Ouriaghli I, Godfrey E, Bridge L, et al. Improving mental health service utilization among men: a systematic review and synthesis of behavior change techniques within interventions targeting help-seeking. Am J Mens Health 2019;13:1557988319857009. 10.1177/1557988319857009 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2022-063468supp001.pdf (136.4KB, pdf)
Data Availability Statement
Data are available upon reasonable request and will be available in a public, open access repository after acceptance of the manuscript.


