Abstract
The properties and utility of the Primary Care PTSD Screen for DSM-5 (PC-PTSD-5) remain unstudied in community-based populations. This study evaluates the performance of the PC-PTSD-5 to determine whether it can be used as a brief alternative to the PTSD Checklist for DSM-5 (PCL-5) in a large public hospital in the southeastern United States. Participants (N = 422; 92.7% Black; 85.8% female; Mage = 42.0 years, SDage = 13.4 years) completed the PCL-5 and PC-PTSD-5 after recruitment from medical clinic waiting rooms and admission lists. Using chance-corrected test quality indices and item response theory (IRT) analyses, we determined optimal cut-scores for screening and examined item performance. Approximately 45.0% of the sample screened positive for probable DSM-5 PTSD using the PCL-5. The PC-PTSD-5 demonstrated high internal consistency and strong associations with PCL-5 scores (total, r = .79; items, rs = .51–.61). A cut-score of one was optimally sensitive for screening (κ[1] = .96), and a cut-score of four had the highest quality of probable efficiency (κ[.5] = .66) for detecting self-reported DSM-5 PTSD on the PCL-5. IRT analyses indicated Item 1 (nightmares, intrusive memories) provided the most information, and other items may not be incrementally useful for this sample. Findings provide preliminary support for the use of the PC-PTSD-5 as a brief alternative to the PCL-5 among chronically trauma-exposed patients in the public healthcare setting.
Keywords: Posttraumatic stress disorder, PC-PTSD-5, Screening, Primary care, Safety net hospital, Healthcare
Introduction
Exposure to a traumatic event, defined as exposure to actual or threatened death, serious injury, or sexual violence, can contribute to the onset or worsening of myriad physical and mental health conditions (Kessler et al., 2017). Individuals who are socioeconomically vulnerable, such as those who are racially marginalized and/or live in poverty, are at greatest risk for experiencing trauma and its negative mental health consequences (Asnaani & Hall-Clark, 2017; Merrick et al., 2018). Located in underserved and urban areas, safety net hospitals, broadly defined as primarily publicly funded health systems that provide care regardless of insurance status or ability to pay (Hefner et al., 2021), often serve as the only option for regular healthcare for individuals with less access to socioeconomic resources (Nath et al., 2016). Thus, primary care, gynecology/obstetrics, and diabetes management clinics, among others, within safety net hospitals tend to provide regular medical care to patients who present with particularly high rates of trauma-related disorders, including current posttraumatic stress disorder (PTSD; 29.1%, Gillespie et al., 2009; Gluck et al., 2021; Mekawi et al., 2021).
Given the association between trauma and poor health outcomes, healthcare systems often serve as the first point of contact for individuals with trauma-related concerns. In recent years, healthcare providers have been encouraged to integrate trauma-informed principles in the care of marginalized patient populations (Ranjbar et al., 2020). Systematic PTSD screening is a trauma-informed practice, as healthcare providers are uniquely positioned to identify, assess, and treat trauma-related health conditions and can link patients to needed mental health services (Gluck et al., 2021; Langhinrichsen-Rohling et al., 2021). Identifying those with active PTSD symptoms within the scope of general medical care is especially important among racially minoritized and socioeconomically disadvantaged patients, as previous studies have documented high rates of undetected PTSD and low rates of mental health services utilization in these marginalized groups (Roberts et al., 2011). Although a wide range of psychological sequelae can result from trauma exposure, the current study focuses on PTSD symptoms due to their association with poor health outcomes and the relative infrequency of universal PTSD screening in health systems, and even trauma centers, in the United States (Beckett & Jacobs, 2014; deRoon-Cassini et al., 2019).
The PTSD Checklist for DSM-5 (PCL-5) is one of the most extensively used and researched PTSD symptom-based screeners in healthcare settings (Blevins et al., 2015; deRoon-Cassini et al., 2019). The PCL-5 is a 20-item self-report questionnaire used to determine the degree of trauma symptomatology and assign probable PTSD diagnoses based on Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5; American Psychiatric Association, 2013) criteria (Weathers et al., 2013a). The PCL-5 has demonstrated reliability and validity across studies and in a variety of samples, including patients receiving primary (Verhey et al., 2018) and specialty care (Kagee et al., 2021), individuals with traumatic injuries in an urban hospital (Geier et al., 2019), and undergraduate students (Blevins et al., 2015). Notably, a recent systematic review supports the PCL-5 as a measure of probable PTSD (Forkus et al., 2022), including in a sample of Black Americans seeking primary care (Mekawi et al., 2022). Yet, time constraints, literacy concerns, and low provider awareness and self-efficacy bar many health systems from enacting universal trauma exposure and/or symptom screening (Marsicek et al., 2019). The PCL-5 takes approximately five to ten minutes to complete and requires roughly a tenth grade reading level (Terhakopian et al., 2008), potentially limiting feasibility in under-resourced hospitals and clinics.
Despite practical limitations, PTSD screening remains a key component of providing holistic care, especially considering the high rates of trauma exposure and unmet treatment needs found among patients seeking care at safety net hospitals (Nobles et al., 2016). A brief alternative to the PCL-5 is the Primary Care PTSD Screen for DSM-5 (PC-PTSD-5; Prins et al., 2015), a dichotomously scored, 5-item PTSD screener designed for use in fast-paced primary care settings (Prins et al., 2003). To date, only a few studies have evaluated the performance of the PC-PTSD-5 in veteran (Bovin et al., 2021; Prins et al., 2016) and substance misusing (Patton et al., 2023) samples; none have examined the performance of the PC-PTSD-5 within general healthcare seeking samples. Of note, the predecessor of the PC-PTSD-5, the PC-PTSD, demonstrates strong predictive validity within both military (Calhoun et al., 2010; Prins et al., 2003) and civilian primary care patient samples (Freedy et al., 2010). The PC-PTSD was even considered the single best PTSD screener for use in primary care, given its brevity and equivalency to the civilian version of the PCL in terms of diagnostic efficiency, sensitivity, and specificity (Freedy et al., 2010).
However, results concerning the diagnostic accuracy of the PC-PTSD among racially marginalized individuals have been mixed. For example, Calhoun et al. (2010) found the PC-PTSD performed well for both White and Black veterans, and the optimal cut-score of three did not differ by race. Conversely, Hawn et al. (2020) suggested the PC-PTSD fails to effectively identify risk for PTSD among racially minoritized individuals. Findings indicate an optimal two-item threshold for White college students, while none of the item thresholds were associated with a PTSD diagnosis in those who self-identified as Black or Other (i.e., American Indian/Alaskan Native, Asian American, Hispanic/Latinx, Native/Pacific Islander, Multiracial, unknown racial identity; Hawn et al., 2020). In addition to the downstream consequences of systemic racism, such as heightened exposure to community-level trauma, Black Americans also encounter racial trauma, a form of race-based stress related to historical and ongoing discrimination (Comas-Díaz et al., 2019). The discrepant findings regarding the performance of the PC-PTSD among racially minoritized individuals warrant investigation into the PC-PTSD-5’s optimal cut-scores and item performance, based on probable DSM-5 PTSD status on the PCL-5, among predominantly Black patients at an urban, safety net hospital.
The Current Study
The properties and utility of the PC-PTSD-5 remain relatively unexplored in community-based populations. Evaluating the performance of the PC-PTSD-5 against a criterion of probable DSM-5 PTSD status measured by the PCL-5 is necessary to determine whether the PC-PTSD-5 can be used as a brief alternative to the PCL-5 in under-resourced health systems with high proportions of socioeconomically vulnerable and racially minoritized patients. Additionally, because the most clinically useful cut score may depend on population, setting, and screening goals (i.e., PTSD detection vs. resource conservation; Prins et al., 2016), further study into the optimal cut-score of the PC-PTSD-5 in trauma-exposed Black patients is needed. The current study evaluated PC-PTSD-5 correspondence with the PCL-5 to determine optimal cut-scores and item performance for use as a brief screener in a publicly funded, urban, safety net hospital.
Consistent with expectations of a screener (Raykov, 2016; Furr, 2018, pp. 456–460, 477–483), we expected the PC-PTSD-5 would be highly sensitive to detecting individuals on the low-to-moderate end of probable PTSD severity and planned to report which PC-PTSD-5 cut-score would optimize sensitivity. We hypothesized the PC-PTSD-5 would have good overall efficiency for detecting probable DSM-5 PTSD status from the PCL-5 in the current sample, and that the same cut-score of three in the literature on the use of PC-PTSD-5 in other populations would optimize the efficiency of detection of probable DSM-5 PTSD. We expected that PC-PTSD-5 items would have adequate discriminative ability, or provide adequate information, to distinguish between individuals with and without self-reported probable PTSD.
Material and Methods
Participants and Procedure
Data were collected as part of a large, ongoing study of trauma exposure and related symptoms in a healthcare-seeking population (Grady Trauma Project). Participants were recruited from waiting rooms at a publicly funded, safety-net hospital in the southeastern United States. Trained interns approached patients in the primary care, gynecology and obstetrics, and diabetes medical clinics regarding potential participation. During the COVID-19 pandemic, patients attending medical visits were contacted via telephone and invited to participate. Interns were undergraduate, postbaccalaureate, or graduate students and participated in didactics on research interviewing, shadowed visits, and were observed conducting interviews as training. Data collection and study procedures were approved by Emory University’s Institutional Review Board and the Grady Research Oversight Committee. The investigation was carried out in accordance with the latest version of the Declaration of Helsinki. Informed consent was obtained from all study participants after the nature of the procedures were explained. Trained interns verbally administered an interview with a variety of self-report questionnaires to consenting individuals; self-report measures were read aloud to all participants to increase accessibility and avoid the assumption that patient literacy levels matched those recommended for each measure. On average, this interview took approximately 45 to 75 min.
Between 2016 and 2021, 440 participants completed both the PC-PTSD-5 and the PCL-5. Fifteen participants were removed from the study due to an incomplete PCL-5, which rendered probable DSM-5 PTSD status unable to be computed. Three participants were removed because they denied trauma exposure, leaving a final sample of 422 participants. Participants were primarily Black (92.7%, n = 391) and female (85.8%, n = 362), with a mean age of 42.0 years (SD = 13.4 years). Most participants were high school graduates or equivalent (83.2%, n = 350), living in poverty (i.e., household monthly income of less than $2,000; 74.4%, n = 272), and unemployed (58.5%, n = 247).
All participants except one endorsed exposure to one or more trauma types (n = 421). One participant was removed from trauma type analyses due to inability to confirm trauma exposure based on missing data. Participants reported exposure to an average of nine trauma types (SD = 4.6). The most frequently reported trauma types were exposure to a serious accident, injury, or illness (84.8%, n = 358), witnessing interpersonal violence (80.6%, n = 340), being confronted with the murder of a family member (58.5%, n = 247), experiencing sexual violence (57.8%, n = 242), experiencing intimate partner violence (56.6%, n = 238), experiencing child emotional and/or physical abuse (54.0%, n = 228), and experiencing physical assault by someone other than a romantic partner (53.3%, n = 224).
Probable DSM-5 PTSD status was computed using participants’ scores on PCL-5 items, such that PCL-5 items rated two (Moderate) or higher were considered as “endorsed” symptoms. We followed the DSM-5 PTSD diagnostic rule requiring the presence of one re-experiencing symptom, one avoidance symptom, two negative alterations in cognition and mood symptoms, and two hyperarousal symptoms. According to this approach, 45.0% of the final sample (n = 190) met criteria for probable DSM-5 PTSD.
Measures
Traumatic Events Inventory
Lifetime history of trauma exposure was assessed using the Traumatic Events Inventory (Gillespie et al., 2009). The TEI is a 14-item measure that inquires about exposure to 24 different traumatic events individuals may have directly experienced, witnessed, or been confronted with. In the current study, each item was rated on a binary scale (0 = No, 1 = Yes). Participants who endorsed exposure to one or more traumatic events were included in analyses. Construct validity of this measure has been shown in the same hospital patient population (Mekawi et al., 2022).
PC-PTSD-5
The PC‐PTSD‐5 (Prins et al., 2015, 2016) was used to determine the presence of posttraumatic stress symptoms over the last month. Each of five items were rated on a binary scale (0 = No, 1 = Yes). Higher scores indicate increased posttraumatic stress symptoms. Internal consistency of PC-PTSD-5 items was high in this study (α = 0.80).
PCL-5
Posttraumatic stress symptoms were also assessed via the PCL-5 (Weathers et al., 2013b), a 20-item self-report measure that corresponds with DSM-5 diagnostic criteria for PTSD. Respondents indicate the extent to which they were bothered by each symptom in the last month. Items are rated on a five-point scale ranging from 0 (Not at all) to 4 (Extremely). The PCL-5 has demonstrated high internal consistency and test–retest reliability, as well as strong convergent and discriminant validity (Blevins et al., 2015; Bovin et al., 2016; Wortmann et al., 2016). In the current study, the internal consistency of the PCL-5 as indicated by Cronbach’s alpha was very high (α = 0.95).
Data Analysis
We conducted descriptive analyses using IBM SPSS Statistics Version 27, performance evaluation analyses using DAG-Stat (Mackinnon, 2000), and item response theory (IRT) analyses in Mplus (Version 8; Muthén & Muthén, 1998–2013). First, we computed scale-level descriptive statistics for all observed variables used and item-level descriptive statistics for the PC-PTSD-5 to assess internal consistency of items purportedly all measuring symptoms of PTSD. To briefly examine the association of observed PC-PTSD-5 scores to PCL-5 scores in a trauma-exposed, primarily Black, urban sample, we computed bivariate correlations between PC-PTSD-5 total and item scores with PCL-5 scores and probable DSM-5 PTSD status.
For each possible cut-point in PC-PTSD-5 total score, we computed diagnostic classification performance metrics. First, we calculated sensitivity ([SE]; i.e., probability of a positive PC-PTSD-5 result among positive PCL-5 cases), specificity ([SP]; i.e., probability of a negative PC-PTSD-5 result among negative PCL-5 cases), positive predictive value ([PPV]; i.e., probability that an individual in the sample has probable PTSD on the PCL-5 when the PC-PTSD-5 is positive), negative predictive value ([NPV]; i.e., probability that an individual in the sample does not have probable PTSD on the PCL-5 when the PC-PTSD-5 is negative), and efficiency or correct classification rate ([EFF]; i.e., the proportion of the total number of PC-PTSD-5 predictions of self-reported probable PTSD that were correct). For all these indices, we calculated the 95% confidence interval of the statistic using the method described by McKenzie et al. (1997).
The measures of test performance described previously are not adjusted for chance agreement between the test and the diagnosis, making them ambiguous indicators of diagnostic utility (Kraemer, 1992). In addition, we calculated test quality indices for sensitivity, specificity, and efficiency, a technique that has been used effectively to identify optimal cut-scores for measures of PTSD symptoms and compare their diagnostic utility (Calhoun et al., 2010; Weathers et al., 1996). We also computed weighted kappa coefficients (κ) as chance-corrected indicators of test quality (Agresti, 1990). These comparative measures of test quality with fixed endpoints (0 = change agreement to 1 = perfect agreement) can be used to compare the diagnostic utility of cut-points, items, or even different measures of PTSD. Because an “optimal” test may differ in its intended purpose and the perceived costs of false positives and negatives (e.g., detect everyone with possible PTSD regardless of false positives vs. diagnose clinically significant PTSD), weighted kappa coefficients were computed for each of the following test quality indices: optimally sensitive SE [κ(1)], optimally specific SP [κ(0)], and optimally efficient EFF [κ(0.5)]. Of these, the cut-point with optimal sensitivity would be most appropriate for using the PC-PTSD-5 as a screener.
Following Hawn et al. (2020), we repeated the above analyses with each PC-PTSD-5 item to examine the potential differential performance of individual PC-PTSD-5 items. As an extension, we also evaluated PC-PTSD-5 item performance using a latent approach by conducting an IRT analysis. An IRT model with a single PTSD latent factor was specified using all five PC-PTSD-5 items. Parameters were estimated with mean- and variance-adjusted weighted least squares (WLSMV) because it is recommended for categorical variables (Muthén & Muthén, 1998–2013) and maximum likelihood (ML) does not generate model fit statistics in Mplus when using categorical indicators. Missing data were handled using pairwise deletion due to the small proportion of missing data in the study (e.g., one respondent did not answer PC-PTSD-5 Item 4; Covariance Coverage = 0.998–1.00) and the inability to use full information maximum likelihood (FIML) with the WLSMV estimator. Model fit was evaluated using multiple indices following best practices (Brown, 2015): chi-square test (χ2, p ≥ 0.05 good fit), comparative fit index (CFI ≥ 0.95 good fit; Hu & Bentler, 1999), Tucker-Lewis index (TLI ≥ 0.95 good fit; Hu & Bentler, 1999), standardized root mean square residual (SRMR < 0.08; Hu & Bentler, 1999), and root mean square error of approximation (RMSEA; close fit if p > 0.05, poor fit if upper limit of 90% confidence interval ≥ 0.10; Browne & Cudeck, 1993; Kline, 2011).
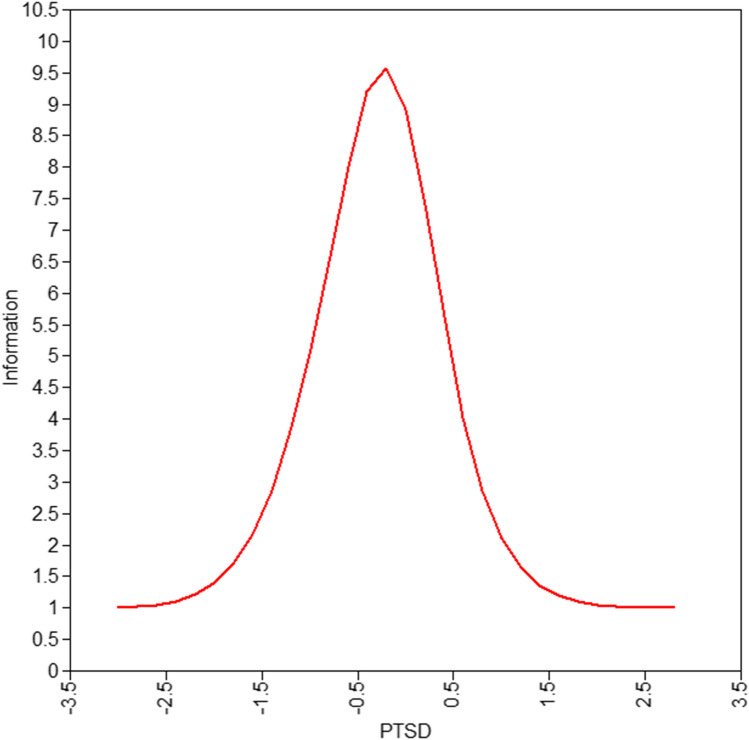
For the present study, IRT models non-linear associations between a participant’s response to PC-PTSD-5 items and their estimated level of the unidimensional latent trait of PTSD (θ). We first examined the Test Information Function (TIF) to evaluate the overall amount of information the whole PC-PTSD-5 provides about one’s PTSD severity, and at which level of PTSD (range of θ) the PC-PTSD-5 is most precise (Reeve, 2003). Like for most screeners, we would hypothesize that the PC-PTSD-5 provides the most information at a low-to-moderate level of PTSD severity, in order to capture as many people in need of follow-up as possible (Raykov, 2016).
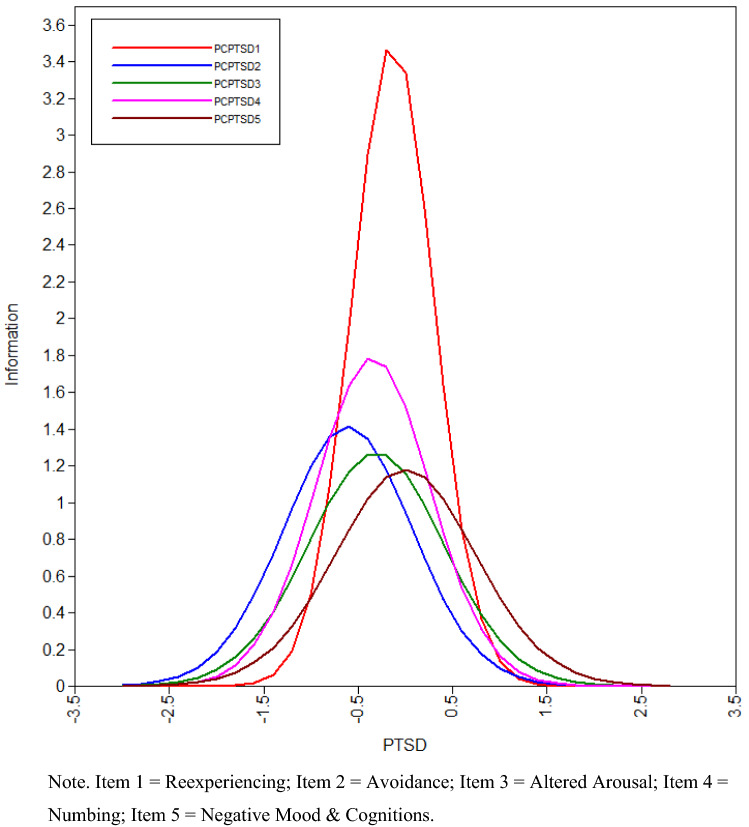
To add to our collective understanding of how the PC-PTSD-5 is functioning in a primarily Black sample, we also examined the Item Information Function (IIF) that shows the extent to which each item contributes to the overall score on the latent trait of PTSD (Hambleton & Jones, 1993) and at which level of PTSD an item is most precise (Reeve, 2003). Higher peaks on the IIC indicate greater discrimination and can be compared between items to identify which are relatively better at discriminating and which, if any, items are less appropriate or underperforming for detecting PTSD in a Black sample. Much like the whole measure, we would expect to see peaks further to the left on the x-axis indicating better discrimination between individuals at lower levels of PTSD (Furr, 2018; Raykov, 2016).
Results
Internal Consistency
Correlational analyses indicated evidence of internal consistency of the PC-PTSD-5 in the present sample, including high coefficient alpha, large and significant item-total correlations, and an appropriate range of inter-item correlations. See Table 1 for scale descriptive statistics for total and sub-scale scores for PCL-5 and total and item-level scores for PC-PTSD-5. See Table 2 for inter-item and item-total correlations for PC-PTSD-5 and bivariate correlations with PCL-5.
Table 1.
Descriptive statistics for PC-PTSD-5 and PCL-5
| Variable | Items | N | M | SD | Possible range | Range | Skewness | Kurtosis | α |
|---|---|---|---|---|---|---|---|---|---|
| PC-PTSD-5 | |||||||||
| Total Scale | 5 | 437 | 2.94 | 1.82 | 0–5 | 0–5 | −0.33 | −1.36 | .80 |
| 1. Nightmares/Intrusive Memories | – | 437 | 0.55 | 0.50 | 0–1 | 0–1 | −0.21 | −1.97 | – |
| 2. Internal/External Avoidance | – | 437 | 0.69 | 0.46 | 0–1 | 0–1 | −0.83 | −1.32 | – |
| 3. Hypervigilance/Startle | – | 437 | 0.60 | 0.49 | 0–1 | 0–1 | −0.40 | −1.85 | – |
| 4. Emotional Numbness/Withdrawal | – | 436 | 0.62 | 0.49 | 0–1 | 0–1 | −0.48 | −1.78 | – |
| 5. Persistent Guilt/Distorted Blame | – | 437 | 0.50 | 0.50 | 0–1 | 0–1 | −0.01 | −2.01 | – |
| PCL-5 | |||||||||
| Total Scale | 20 | 422 | 31.49 | 21.19 | 0–80 | 0–77 | 0.30 | −1.05 | .954 |
| REX Subscale | 5 | 422 | 7.72 | 6.12 | 0–20 | 0–20 | 0.39 | −1.06 | .904 |
| AV Subscale | 2 | 422 | 3.81 | 2.80 | 0–8 | 0–8 | 0.00 | −1.38 | .847 |
| NACM Subscale | 7 | 422 | 10.56 | 8.07 | 0–28 | 0–28 | 0.33 | −1.08 | .895 |
| AAR Subscale | 6 | 420 | 9.44 | 6.60 | 0–24 | 0–24 | 0.28 | −1.10 | .862 |
REX, Reexperiencing; AV, Avoidance; NACM, Negative alterations in cognition and mood; AAR, Alterations in arousal and reactivity
Table 2.
PC-PTSD-5 inter-item correlations and bivariate correlations with PCL-5 and probable DSM-5 PTSD status
| Variable | PC-PTSD-5 Item | PC-PTSD-5 Total | ||||
|---|---|---|---|---|---|---|
| 1. Reexperiencing | 2. Avoidance | 3. Altered Arousal | 4. Numbing | 5. Negative Mood & Cognitions | ||
| Item 1 | – | .797 | ||||
| Item 2 | .522 | – | .706 | |||
| Item 3 | .451 | .430 | – | .736 | ||
| Item 4 | .506 | .340 | .486 | – | .753 | |
| Item 5 | .476 | .366 | .370 | .465 | – | .725 |
| PCL-5 REX | .604 | .503 | .546 | .476 | .492 | .707 |
| PCL-5 AV | .416 | .483 | .375 | .414 | .379 | .555 |
| PCL-5 NACM | .558 | .418 | .508 | .601 | .595 | .725 |
| PCL-5 AAR | .563 | .469 | .627 | .617 | .481 | .744 |
| PCL-5 Total | .617 | .512 | .596 | .613 | .568 | .784 |
| Probable DSM-5 PTSD status | .544 | .490 | .508 | .539 | .445 | .680 |
N = 437 for inter-item and item-total PC-PTSD-5 correlations; N = 422 for correlations with PCL-5 scales. All correlation coefficients were statistically significant at p < .001
REX, Reexperiencing; AV, Avoidance; NACM, Negative alterations in cognition and mood; AAR, Alterations in arousal and reactivity
Using PC-PTSD-5 to Determine Probable PTSD Status on the PCL-5
Beginning with correlational analyses (Table 2), individual PC-PTSD-5 items had significant observed relationships with PCL-5 total and subscale scores and probable DSM-5 PTSD status. However, these were slightly weaker than expected for associations with another measure of the same construct. Overall, PC-PTSD-5 items produced higher correlations with their corresponding PCL-5 subscales compared to PCL-5 scores on less theoretically related PTSD symptom clusters. Unsurprisingly, total PC-PTSD-5 scores were more strongly correlated with the PCL-5 total and subscale scores than individual PC-PTSD-5 items. PC-PTSD-5 total scores had a moderately high correlation with probable DSM-5 PTSD derived from PCL-5.
Next, we inspected the test performance indices (Table 3) and chance-corrected indices of test quality (κ). The optimally sensitive cut-score that administrators may select for inclusive screening purposes was one, which had 96% quality of sensitivity and 12% quality of specificity, at the cost of large numbers of false positives. This cut-score detected approximately 99% of individuals in the sample with probable DSM-5 PTSD from the PCL-5. Test performance indices revealed there is a 52% probability (PPV) of a true positive screen when the PC-PTSD-5 score is at least one and an 98% probability (NPV) of a true negative screen when the PC-PTSD-5 score is zero. In replicating the identification of an optimally efficient PC-PTSD-5 like in other studies, we identified a cut-score of four provided the best overall agreement with probable DSM-5 PTSD from the PCL-5. At the item-level, Item 1 (nightmares intrusive memories) was superior to all other items in terms of calibrated overall efficiency and specificity, while Item 2 (avoidance) was superior to all other items in terms of sensitivity.
Table 3.
Diagnostic efficiency of PC-PTSD-5 total score cut-points and items for detecting probable DSM-5 PTSD status on PCL-5
| Variable | Test performance index | Test quality index | ||||||
|---|---|---|---|---|---|---|---|---|
| SE | SP | PPV | NPV | EEF | κ(1) | κ(0) | κ(.5) | |
| PC-PTSD total score cut-points | ||||||||
| Score ≥ 1* | .99 (.97–1.00) | .24 (.18–.30) | .52 (.46–.57) | .98 (.90–1.00) | .58 (.53–.63) | .96 | .12 | .21 (.16–.27) |
| Score ≥ 2 | .97 (.94–.99) | .48 (.41–.54) | .60 (.55–.66) | .96 (.90–.99) | .70 (.66–.74) | .90 | .28 | .43 (.36–.50) |
| Score ≥ 3 | .94 (.90–.97) | .67 (.60–.73) | .70 (.64–.75) | .93 (.88–.97) | .79 (.75–.83) | .85 | .45 | .59 (.52–.66) |
| Score ≥ 4 | .86 (.80–.90) | .81 (.75–.85) | .78 (.72–.84) | .87 (.82–.92) | .83 (.79–86) | .72 | .61 | .66 (.59–.73) |
| PC-PTSD items | ||||||||
| Item 1 | .86 (.80–.90) | .69 (.62–.74) | .69 (.63–.75) | .85 (.80–.90) | .76 (.72–.80) | .68 | .44 | .53 (.45–.61) |
| Item 2 | .94 (.90–.97) | .51 (.45–.58) | .61 (.55–.67) | .92 (.85–.96) | .71 (.66–.75) | .81 | .30 | .43 (.36–.51) |
| Item 3 | .88 (.82–.92) | .62 (.55–.68) | .65 (.59–.71) | .86 (.80–.91) | .74 (.69–.78) | .70 | .37 | .48 (.41–.56) |
| Item 4* | .91 (.86–.95) | .62 (.55–.68) | .66 (.60–.72) | .89 (.84–.94) | .75 (.70–.79) | .76 | .38 | .51 (.43–.58) |
| Item 5 | .76 (.69–.82) | .69 (.63–.75) | .67 (.60–.73) | .78 (.71–.83) | .72 (.67–.76) | .50 | .40 | .44 (.36–.53) |
N = 422 except when designated by *N = 421. PC-PTSD-5 cut-scores are designated by Score ≥ number (possible PC-PTSD-5 total scores are 0–5). Parentheses indicate 95% confidence interval
SE, Sensitivity; SP, Specificity; PPV, Positive predictive value; NPV, Negative predictive value; EFF, Efficiency/Correct classification rate; κ(1) = quality of SE; κ(0) = quality of SP; κ(.5) = quality of EFF
IRT Analysis
The IRT model had adequate fit according to some (CFI = 0.990, TLI = 0.980, SRMR = 0.039) but not all (χ2 = 18.58, p = 0.002; RMSEA = 0.079, 90% CI [0.043-0.119]) fit statistics. Factor loadings and discrimination (a) and difficulty (b) parameters are presented in Table 4. The Test Information Function (TIF) and Item Information Function (IIF) are presented in Figs. 1 and 2. The overall test appeared to be most precise at the level of low-to-moderate PTSD severity (θ = -0.5–0), as expected for a screener (Fig. 1). Results revealed that only one item (Item 1; nightmares, intrusive memories) was identified as being adequately discriminant (a ≥ 2). Item 1 was most frequently endorsed by individuals with the underlying trait of PTSD as measured by this model, which echoes its overall quality of efficiency for accurately predicting probable DSM-5 PTSD status, as described earlier. All other PC-PTSD-5 items demonstrated moderately low (1 ≥ a < 2) discrimination parameters (Table 4), indicating that their endorsement may not provide as much information about the latent trait of PTSD or differentiate between individuals with differences in presence of PTSD as much as expected. The binary nature of PC-PTSD-5 items may have contributed to this result if there was not adequate variance within responses to a singular item to capture wide-ranging levels of the latent trait of PTSD within the IRT framework.
Table 4.
PC-PTSD-5 IRT factor loadings and difficulty and discrimination parameters
| PTSD by | Standardized factor loading | SE | R2 | Discrimination a | Difficulty b |
|---|---|---|---|---|---|
| Item 1: Reexperiencing | .897** | .031 | 0.81 | 2.033** | −0.144* |
| Item 2: Avoidance | .791** | .040 | 0.63 | 1.291** | −0.631** |
| Item 3: Altered arousal | .782** | .040 | 0.61 | 1.256** | −0.315** |
| Item 4: Numbing | .825** | .038 | 0.68 | 1.457** | −0.361** |
| Item 5: Negative mood & cognitions | .764** | .042 | 0.58 | 1.182** | −0.011 |
N = 437
*p < .05; **p < .01
Fig. 1.
Test information function (IIF) for PC-PTSD-5
Fig. 2.
Item information function (IIF) for PC-PTSD-5 items
Next, IRT results showed a low-to-moderate difficulty of endorsing PC-PTSD-5 items (Table 4). The level of PTSD required for 50% of respondents to endorse individual PC-PTSD-5 items was at or slightly below the mean of the latent trait of PTSD in the sample, which is consistent with expectations for a screener that is intended to capture any person with symptoms. According to the difficulty parameters (b; Table 4), there was some heterogeneity in difficulty. Item 2 (avoidance) was the easiest item, requiring very low levels of PTSD to endorse. Items 1 (nightmares, intrusive memories), 3 (hypervigilance, startle), and 4 (emotional numbness, withdrawal) required low-mild levels of PTSD to endorse, while item 5 (persistent guilt, distorted blame) required mild-moderate levels of PTSD to endorse.
Discussion
This study is the first to evaluate the PC-PTSD-5 in a largely minoritized, low resourced patient sample using chance corrected test quality indices and IRT analyses. Broadly, results were highly consistent across analyses and provided preliminary support for the use of the PC-PTSD-5 as a brief alternative to the PCL-5 among trauma-exposed Black patients seeking medical services from an urban, public healthcare setting. When used as a screener in this sample of predominantly Black women with limited socioeconomic resources, a cut-score of one was found to have optimal sensitivity, and detected nearly all individuals (96%) with probable PTSD from the PCL-5. In fact, the cut-score of one yielded even higher levels of sensitivity to probable DSM-5 PTSD in our sample than reported in recent manuscripts on primarily White individuals and college students (Hawn et al., 2020). This finding that the PC-PTSD-5 was very sensitive to probable PTSD in trauma-exposed Black individuals adds to the literature on measure performance and appropriate use, particularly as a screener, in this population.
Contextualizing our results within the current body of literature that has reported optimally efficient cut-scores, a PC-PTSD-5 cut-score of four in our sample yielded comparable efficiency found via the PC-PTSD in other populations, including veterans (Calhoun et al., 2010; Prins et al., 2003, 2016) and civilians seeking substance abuse treatment (van Dam et al., 2010). As is the case often between demographic groups, this threshold varies from the Prins et al.’s (2016) PC-PTSD-5 optimal cut-score of three in a primarily White, male veteran sample. Additional research is necessary to determine whether current results generalize to other diverse groups and settings. Potential moderators of inconsistent cut-scores across studies and samples may include demographics factors (e.g., race, gender, socioeconomic status) and setting, but also factors such as modality, carryover effects, and interviewer-participant characteristics which are relevant to the administration method used in the current study.
We should note that although a threshold of one on the PC-PTSD-5 was found to be optimally sensitive in the current sample, the prevalence of PTSD in different populations could affect the PPV and NPV. For example, if screening in a setting with a much lower base rate of probable PTSD, there may be a lower probability that individuals with higher PC-PTSD-5 scores actually have PTSD. Although many healthcare systems may utilize a PC-PTSD-5 cut-score that is optimally sensitive because it is important to avoid missing individuals in need of care (i.e., false negatives), cut-scores can be adjusted according to the unique needs of particular health systems and differing applications. Regardless, the PC-PTSD-5 cannot be used as an independent means of diagnosing PTSD and should be followed by a referral to complete a comprehensive psychological assessment with a structured interview of trauma-related symptoms to differentially diagnose PTSD.
When looking at the individual items of the PC-PTSD-5, IRT results indicated that Item 1 (nightmares, intrusive memories) appeared to be doing the heavy lifting, providing nearly double the information about PTSD as any of the other four items. The relatively lower discriminative ability (a < 2) of items 2–5 on the PC-PTSD-5 also indicates that they may not be as clinically useful above and beyond screening for re-experiencing symptoms in this population. This was consistent with the internal consistency results (α = 0.80) that showed PC-PTSD-5 items were highly inter-related with one another, meaning not all items may be necessary to accurately screen for probable PTSD. This evokes two crucial take-home points: (1) Using Item 1 of the PC-PTSD-5 is likely to be nearly as sensitive as the whole measure to screen in this primarily Black sample; (2) Screening particularly for re-experiencing symptoms may be even more important for detecting probable PTSD in Black populations.
Interestingly, avoidance was endorsed by most individuals in the sample, including many with no or very low levels of probable PTSD. This finding is consistent with the high sensitivity and low specificity of avoidance symptoms on the PCL-5 in both college student and community samples (Silverstein et al., 2020). This item’s high sensitivity and low specificity may demonstrate the transdiagnostic nature of avoidance, in that it could be capturing individuals without PTSD who are using normative and adaptive safety behaviors for their environment (e.g., vigilance or avoidance of potential threats). This result could also reflect unique characteristics of the present sample, such as self-protective attempts to not think about or encounter psychologically threatening stimuli that are more pervasive and generalized. The relatively higher difficulty of Item 5 (guilt, blame) highlights that assessing only for feelings of guilt and distorted blame in trauma-exposed Black populations could result in missing individuals with lower levels of PTSD who would still benefit from follow-up assessment and intervention.
The above findings highlight areas of potential difference in symptom-level expression depending on cultural background variables that need to be explored. We could not compare populations in the current study to understand if cultural or demographic differences (in expression or endorsement) were the reason for lower item performance. Future research is needed to determine if items are comparatively less informative in a sample of primarily Black women versus others, as well as to more broadly explore cultural differences in expression and endorsement of PTSD symptoms, especially given the differences in PTSD conceptualizations (e.g., inclusion of negative emotions and blame) between the DSM-5 and the International Classification of Diseases, 11th Edition (ICD-11; World Health Organization, 2019). Future uses of IRT with the PC-PTSD-5 in other demographic groups are needed to contextualize our findings. It will be important for these studies to examine if items do indeed differ in the amount of information they provide across racial groups, and if so, employ IRT to select more appropriate items from the 20-item pool for detecting PTSD in a Black sample.
Our reliance on self-report questionnaires as criterion represents a limitation of the current study. Following Forkus et al. (2022) systematic review, the present study used the PCL-5 and the DSM-5 diagnostic rule to approximate probable DSM-5 PTSD status as a criterion to evaluate the performance of the PC-PTSD-5. Research on the strength of the PCL-5 as a criterion for probable PTSD in Black Americans is sparse (Mekawi et al., 2022). Also, this study solely intended to evaluate the performance of the PC-PTSD-5 in terms of probable DSM-5 PTSD determined via the PCL-5 given its widespread use in primary care; we do not intend to imply screening scores from the PC-PTSD-5 or PCL-5 are equivalent to a PTSD diagnosis. Future studies should replicate the present study by examining PC-PTSD-5 scores in relation to a PTSD diagnosis obtained through psychometrically validated structured interview such as the Clinician Administered PTSD Scale for DSM-5 (CAPS-5; Weathers et al., 2013a).
Moreover, our findings reflect the study population, a group of primarily low-income Black women seeking care from a safety net hospital in a large city in the southeast region of the United States. Given what is known about stigma associated with mental health concerns within the Black community (Ward et al., 2013), it is possible that participants may have not disclosed or downplayed the presence or severity of PTSD symptoms during the assessment. Perhaps, participants found it more socially acceptable to report avoidance as compared to other PTSD symptoms (i.e., intrusions, negative alterations in cognitions and mood, alterations in arousal or reactivity). More research is needed to explore participants’ perceptions of and reasons to endorse PC-PTSD-5 items and whether this varies by racial background. Results may not generalize to patients of different demographic backgrounds (e.g., men, college students), patients who are insured or seeking care at private hospitals, or patients in other geographic regions. In addition, future studies may consider validating the PC-PTSD-5 for use in detecting individuals with subthreshold PTSD, or those who are symptomatic but do not meet full PTSD criteria, as they may also benefit from intervention.
Primary care settings are the first avenue through which many individuals disclose mental health concerns and gain access to treatment through referral. It is essential that a PTSD screener demonstrates adequate sensitivity among a demographically similar sample before standard use in a particular patient population (or that differences in sensitivity among demographic groups are well-documented in the broader literature) to prevent under-identification of possible PTSD in certain groups, which may ultimately lead to delayed treatment, lengthier chronicity, increased impairment, and poorer health outcomes. It is also important to echo the mixed performance of the PC-PTSD-5 for non-White individuals in the extant literature, which in combination with our findings, indicates that the PC-PTSD-5, like all other psychological symptom measures, should not be interpreted using a one-size-fits-all metric. If feasible, health systems should evaluate PC-PTSD-5’s performance within their patient population prior to use as a universal PTSD screener. Because public health systems are often under-resourced and over-burdened, we acknowledge this recommendation as idyllic; therefore, at minimum, systems should consider their patient population, best practices regarding referral, and hospital resources when choosing screeners or cut scores for probable PTSD.
Given the systemic issues that lower access to psychological services and healthcare for Black women, it is even more crucial that brief screeners, like the PC-PTSD-5, can reliably detect possible PTSD during primary care encounters. Given public health systems predominantly care for underserved and socioeconomically vulnerable populations with considerable barriers to receiving follow-up mental health services, the ability to refer to an integrated behavioral health team is especially important within safety net primary care clinics (Miller et al., 2013). Ultimately, regardless of whether a patient chooses to engage with further mental health services or trauma-focused treatment, screening for PTSD symptoms is critical within primary care, as provider awareness of a patient’s trauma history and current level of symptoms can add context to the patient’s health history and presenting concern, thereby enhancing the providers’ case conceptualization and treatment plan and strengthening the patient-provider relationship (Lewis et al., 2019).
Conclusions
Aside from further evaluating the properties of the relatively new PC-PTSD-5, the present study contributes substantially to the literature on assessment of PTSD within racially marginalized populations. We found the PC-PTSD-5 as a whole to have utility for detecting probable DSM-5 PTSD status on the PCL-5 in a sample of trauma-exposed and primarily Black women, with a cut-score of one optimizing sensitivity for screening. In comparing to literature on optimally efficient cut-scores, we found a cut-score of four was optimally efficient in our sample, and the PC-PTSD-5 had suboptimal performance for detecting PTSD if the widely used cut-score of three was applied. IRT analyses indicated that the PC-PTSD-5 as a whole was most precise at low-to-moderate levels of PTSD, and Item 1 (nightmares, intrusive memories) was the only item with adequate discriminative ability. Overall, our findings suggest that the PC-PTSD-5 can function as a brief alternative to the PCL-5, although items 2-5 may not be adding useful information above and beyond Item 1 within our population. Thus, the PC-PTSD-5 has the potential to benefit both patients and providers by circumventing reported barriers to PTSD screening within primary care. Future research should include larger samples with mixed demographic characteristics and the use of clinician-administered diagnostic interviews (i.e., CAPS-5; Weathers et al., 2013a) to compare the properties of the PC-PTSD-5 and items across cultures and settings. There is also a need for cross-cultural measurement invariance testing and continued IRT on the PC-PTSD-5 to better understand presence and reasons for differential performance across racially marginalized groups. Without accurate and reliable assessment tools, an empirically supported understanding of the etiology of PTSD cannot be attained, and intervention efficiency cannot be adequately measured. We hope the present research inspires further evaluation of the efficacy of PTSD assessment tools for disadvantaged populations at risk for PTSD.
Acknowledgements
This content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. We would like to thank the entire Grady Trauma Project team for their assistance in data collection and management for this project as well as the Grady Trauma Project participants for their willingness to be involved in our research.
Author Contributions
All authors contributed to the study conception and design. Material preparation and data analysis were performed by EL and JP, respectively. The first draft of the manuscript was written by EL and JP. All authors commented on previous versions of the manuscript. VM and AP acquired funding. All authors read and approved the final manuscript.
Funding
This work was supported by the National Institute of Mental Health (MH115174), National Institute on Aging (AG062334), and National Center for Complementary & Integrative Health (K23-AT009713).
Data Availability
The data that support the findings of this study are available from the corresponding author, EL, upon reasonable request.
Code Availability
N/A.
Declarations
Conflict of interest
Emma C. Lathan, Jessica M. Petri, Tamara Haynes, Stan C. Sonu, Yara Mekawi, Vasiliki Michopoulos, and Abigail Powers have no conflicts of interest to disclose.
Ethical Approval
This study followed ethical guidelines and was approved by Emory University Institutional Review Board and the Grady Hospital Oversight Committee. The investigation was carried out in accordance with the latest version of the Declaration of Helsinki.
Consent to Participate
Informed consent was obtained from all study participants after the nature of the procedures were explained.
Consent for Publication
All authors have read the manuscript and agree to it being submitted for publication. All individuals listed as authors meet the appropriate authorship criteria.
Footnotes
Emma C. Lathan and Jessica M. Petri share joint first authorship.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Agresti A. Categorical data analysis. John Wiley & Sons; 1990. [Google Scholar]
- American Psychiatric Association . Diagnostic and statistical manual of mental disorders (DSM-5®) American Psychiatric Pub; 2013. [Google Scholar]
- Asnaani A, Hall-Clark B. Recent development in understanding ethnocultural and race differences in trauma exposure and PTSD. Current Opinion in Psychology. 2017;14:96–101. doi: 10.1016/j.copsyc.2016.12.005. [DOI] [PubMed] [Google Scholar]
- Beckett, L., & Jacobs, B. (2014). Chart: Trauma hospitals fail to screen for civilian PTSD. ProPublica. Retrieved from https://projects.propublica.org/graphics/ptsd
- Blevins CA, Weathers FW, Davis MT, Witte TK, Domino JL. The posttraumatic stress disorder checklist for DSM-5 (PCL-5): Development and initial psychometric evaluation. Journal of Traumatic Stress. 2015;28(6):489–498. doi: 10.1002/jts.22059. [DOI] [PubMed] [Google Scholar]
- Bovin MJ, Kimerling R, Weathers FW, Prins A, Marx BP, Post EP, Schnurr PP. Diagnostic accuracy and acceptability of the primary care posttraumatic stress disorder screen for the diagnostic and statistical manual of mental disorders (fifth edition) among US veterans. JAMA Network Open. 2021;4(2):e2036733. doi: 10.1001/jamanetworkopen.2020.36733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bovin MJ, Marx BP, Weathers FW, Gallagher MW, Rodriguez P, Schnurr PP, Keane TM. Psychometric properties of the PTSD checklist for diagnostic and statistical manual of mental disorders-fifth edition (PCL-5) in veterans. Psychological Assessment. 2016;28(11):1379–1391. doi: 10.1037/pas0000254. [DOI] [PubMed] [Google Scholar]
- Brown TA. Confirmatory factor analysis for applied research. 2. The Guilford Press; 2015. [Google Scholar]
- Browne MW, Cudeck R. Alternative ways of assessing model fit. In: Bollen KA, Long JS, editors. Testing structural equation models. Sage; 1993. pp. 136–162. [Google Scholar]
- Calhoun PS, McDonald SD, Guerra VS, Eggleston AM, Beckham JC, Straits-Troster K, The VA Mid-Atlanta MIRECC OEF.OIF Registry Workgroup Clinical utility of the primary care—PTSD screen among U.S. veterans who served since September 11, 2001. Psychiatry Research. 2010;178:330–335. doi: 10.1016/j.psychres.2009.11.009. [DOI] [PubMed] [Google Scholar]
- Comas-Díaz L, Hall GN, Neville HA. Racial trauma: Theory, research, and healing: Introduction to the special issue. The American Psychologist. 2019;74(1):1–5. doi: 10.1037/amp0000442. [DOI] [PubMed] [Google Scholar]
- deRoon-Cassini TA, Hunt JC, Geier TJ, Warren AM, Ruggiero KJ, Scott K, George J, Halling M, Jurkovich G, Fakhry SM, Zatzick D, Brasel KJ. Screening and treating hospitalized trauma survivors for posttraumatic stress disorder and depression. The Journal of Trauma and Acute Care Surgery. 2019;87(2):440–450. doi: 10.1097/TA.0000000000002370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forkus, S. R., Raudales, A. M., Rafiuddin, H. S., Weiss, N. H., Messman, B. A., & Contractor, A. A. (2022). The posttraumatic stress disorder (PTSD) checklist for DSM-5: A systematic review of existing psychometric evidence. Clinical Psychology: Science and Practice. Advance online publication. [DOI] [PMC free article] [PubMed]
- Freedy JR, Steenkamp MM, Magruder KM, Yeager DE, Zoller JS, Hueston WJ, Carek PJ. Post-traumatic stress disorder screening test performance in civilian primary care. Family Practice. 2010;27(6):615–624. doi: 10.1093/fampra/cmq049. [DOI] [PubMed] [Google Scholar]
- Furr RM. Psychometrics: An introduction. 3. Sage Publishing; 2018. [Google Scholar]
- Geier TJ, Hunt JC, Nelson LD, Brasel KJ, deRoon-Cassini T. Detecting PTSD in a traumatically injured population: The diagnostic utility of the PTSD Checklist for DSM-5. Depression and Anxiety. 2019;36(2):170–178. doi: 10.1002/da.22873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gillespie CF, Bradley B, Mercer K, Smith AK, Conneely K, Gapen M, Weiss T, Schwartz AC, Cubells JF, Ressler KJ. Trauma exposure and stress-related disorders in inner city primary care patients. General Hospital Psychiatry. 2009;31(6):505–514. doi: 10.1016/j.genhosppsych.2009.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gluck RL, Hartzell GE, Dixon HD, Michopoulos V, Powers A, Stevens JS, Fani N, Carter S, Schwartz AC, Jovanovic T, Ressler KJ, Bradley B, Gillespie CF. Trauma exposure and stress-related disorders in a large, urban, predominantly African-American, female sample. Archives of Women’s Mental Health. 2021 doi: 10.1007/s00737-021-01141-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hambleton RK, Jones RW. Comparison of classical test theory and item response theory and their applications to test development. Educational Measurement: Issues and Practice. 1993;12(3):38–47. doi: 10.1111/j.1745-3992.1993.tb00543.x. [DOI] [Google Scholar]
- Hawn SE, Cusack SE, George B, Sheerin CM, Spit for Science Working Group. Dick D, Amstadter AB. Diagnostic validity of the PC-PTSD screen in college students. Journal of American College Health. 2020 doi: 10.1080/07448481.2020.1841768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hefner JL, Hogan TH, Opoku-Agyeman W, Menachami N. Defining safety net hospitals in the health services research literature: A systematic review and critical appraisal. BMC Health Services Research. 2021;21:278. doi: 10.1186/s12913-021-06292-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6:1–55. doi: 10.1080/10705519909540118. [DOI] [Google Scholar]
- Kagee A, Bantjes J, Saal W, Sterley A. Predicting posttraumatic stress disorder caseness using the PTSD Checklist for DSM-5 among patients receiving care for HIV. Journal of Traumatic Stress. 2021 doi: 10.1002/jts.22654. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Aguilar-Gaxiola S, Alonso J, Benjet C, Bromet EJ, Cardoso G, Koenen KC. Trauma and PTSD in the WHO World Mental Health Surveys. European Journal of Psychotraumatology. 2017;8:1353383. doi: 10.1080/20008198.2017.1353383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kline RB. Principles and practice of structural equation modeling. 3. Guilford Press; 2011. [Google Scholar]
- Kraemer HC. Evaluating medical tests: Objective and quantitative guidelines. Sage Publications; 1992. [Google Scholar]
- Langhinrichsen-Rohling J, Schneider M, Selwyn CN, Lathan E, Sayegh L, Hamberger LK. Addressing intimate partner violence within the healthcare system. In: Geffner R, White JW, Hamberger LK, Rosenbaum A, Vaughan-Eden V, Vieth VI, editors. Handbook of interpersonal violence and abuse across the lifespan: a project of the national partnership to end interpersonal violence across the lifespan (NPEIV) Springer Nature; 2021. [Google Scholar]
- Lewis CL, Langhinrichsen-Rohling J, Selwyn CN, Lathan EC. Once BITTEN, twice shy: An applied trauma-informed healthcare model. Nursing Science Quarterly. 2019;32(4):291–298. doi: 10.1177/0894318419864344. [DOI] [PubMed] [Google Scholar]
- Mackinnon A. A spreadsheet for the calculation of comprehensive statistics for the assessment of diagnostic tests and inter-rater agreement. Computers in Biology and Medicine. 2000;30(3):127–134. doi: 10.1016/S0010-4825(00)00006-8. [DOI] [PubMed] [Google Scholar]
- Marsicek SM, Morrison JM, Manikonda N, O’Halleran M, Spoehr-Labutta Z, Brinn M. Implementing standardized screening for adverse childhood experiences in a pediatric resident continuity clinic. Pediatric Quality and Safety. 2019;4(2):e154–e154. doi: 10.1097/pq9.0000000000000154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKenzie DP, Vida S, Mackinnon AJ, Onghena P, Clarke DM. Accurate confidence intervals for measures of test performance. Psychiatry Research. 1997;69(2–3):207–209. doi: 10.1016/s0165-1781(96)02952-6. [DOI] [PubMed] [Google Scholar]
- Mekawi Y, Kuzyk E, Dixon HD, McKenna B, Camacho L, de Andino AM, Stevens J, Michopolous V, Powers A. Characterizing typologies of polytraumatization: A replication and extension study examining internalizing and externalizing psychopathology in an urban population. Clinical Psychological Science. 2021;9(6):1144–1163. doi: 10.1177/21677026211000723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mekawi Y, Silverstein MW, Walker A, Ishickwene M, Carter S, Michopolous V, Stevens JS, Powers A. Examining the psychometric properties of the PCL-5 in a Black community sample using item response theory. Journal of Anxiety Disorders. 2022 doi: 10.1016/j.janxdis.2022.102555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merrick MT, Ford DC, Ports KA, Guinn AS. Prevalence of adverse childhood experiences from the 2011–2014 behavioral risk factor surveillance system in 23 states. JAMA Pediatrics. 2018;172(11):1038–1044. doi: 10.1001/jamapediatrics.2018.2537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller BF, Talen MR, Patel KK. Advancing integrated behavioral health and primary care: The critical importance of behavioral health in health care policy. In: Talen MR, Burke Valeras A, editors. Integrated behavioral health in primary care: Evaluating the evidence, identifying the essentials. Springer Science Business Media; 2013. pp. 53–62. [Google Scholar]
- Muthén, L.K., & Muthén, B.O. (1998–2013). Mplus user’s guide, 7th ed. Muthén & Muthén.
- Nath JB, Costigan S, Hsia RY. Changes in demographics of patients seen at federally qualified health centers, 2005–2014. JAMA Internal Medicine. 2016;176(5):712–714. doi: 10.1001/jamainternmed.2016.0705. [DOI] [PubMed] [Google Scholar]
- Nobles CJ, Valentine SE, Gerber MW, Shtasel DL, Marques L. Predictors of treatment utilization and unmet treatment need among individuals with posttraumatic stress disorder from a national sample. General Hospital Psychiatry. 2016;43:38–45. doi: 10.1016/j.genhosppsych.2016.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patton, S., Hinojosa, C. A., Lathan, E. C., Welsh, J., & Powers, A. (2023). Validating the Primary Care Posttraumatic Stress Disorder Screen for DSM-5 (PC-PTSD-5) in a substance misusing, trauma exposed, socioeconomically vulnerable patient population. Addictive Behaviors. [DOI] [PMC free article] [PubMed]
- Prins, A., Bovin, M. J., Kimerling, R., Kaloupek, D. G., Marx, B. P., Pless Kaiser, A., & Schnurr, P. P. (2015). The primary care PTSD screen for DSM-5 (PC-PTSD-5). [measurement instrument]. Retrieved from ptsd.va.gov. [DOI] [PMC free article] [PubMed]
- Prins A, Bovin MJ, Smolenski DJ, Marx BP, Kimerling R, Jenkins-Guarnieri MA, Kaloupek DG, Schnurr PP, Pless Kaiser A, Leyva YE, Tiet QQ. The primary care PTSD Screen for DSM-5 (PC-PTSD-5): Development and evaluation within a veteran primary care sample. Journal of General Internal Medicine. 2016;31(10):1206–1211. doi: 10.1007/s11606-016-3703-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prins A, Ouimette P, Kimerling R, Cameron RP, Hugelshofer DS, Shaw-Hegwer J, Thraikill A, Gusman FD, Sheikh JI. The primary care PTSD screen (PC-PTSD): Development and operating characteristics. Primary Care Psychiatry. 2003;9(1):9–14. doi: 10.1185/135525703125002350. [DOI] [Google Scholar]
- Ranjbar N, Erb M, Mohammad O, Moreno FA. Trauma-informed care and cultural humility in the mental health care of people from minoritized communities. Focus. 2020;18(8):8–15. doi: 10.1176/appi.focus.20190027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raykov T. Item response theory: Course book. Statistical Horizons; 2016. [Google Scholar]
- Reeve BB. Item response theory modeling in health outcomes measurement. Expert Review of Pharmacoeconomics & Outcomes Research. 2003;3:131–145. doi: 10.1586/14737167.3.2.131. [DOI] [PubMed] [Google Scholar]
- Roberts AL, Gilman SE, Breslau J, Breslau N, Koenen KC. Race/ethnic differences in exposure to traumatic events, development of post-traumatic stress disorder, and treatment-seeking for post-traumatic stress disorder in the United States. Psychological Medicine. 2011;41(1):71–83. doi: 10.1017/S0033291710000401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silverstein MW, Petri JM, Kramer LB, Weathers FW. An item response theory analysis of the PTSD checklist for DSM-5: Implications for DSM-5 and ICD-11. Journal of Anxiety Disorders. 2020;70:102190. doi: 10.1016/j.janxdis.2020.102190. [DOI] [PubMed] [Google Scholar]
- Terhakopian A, Sinaii N, Engel CC, Schnurr PP, Hoge CW. Estimating population prevalence of posttraumatic stress disorder: An example using the PTSD checklist. Journal of Traumatic Stress. 2008;21(3):290–300. doi: 10.1002/jts.20341. [DOI] [PubMed] [Google Scholar]
- van Dam D, Ehring T, Vedel E, Emmelkamp P. Validation of the primary care posttraumatic stress disorder screening questionnaire (PC-PTSD) in civilian substance use disorder patients. Journal of Substance Abuse Treatment. 2010;39(2):105–113. doi: 10.1016/j.jsat.2010.05.005. [DOI] [PubMed] [Google Scholar]
- Verhey R, Chibanda D, Gibson L, Brakarsh J, Seedat S. Validation of the posttraumatic stress disorder checklist – 5 (PCL-5) in a primary care population with high HIV prevalence in Zimbabwe. BMC Psychiatry. 2018 doi: 10.1186/s12888-018-1688-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ward, E. C., Wiltshire, J. C., Detry, M. A., & Brown, R. L. (2013). African American men and women’s attitude toward mental illness, perceptions of stigma, and preferred coping behaviors. Nursing Research, 62(3), 185–194. 10.1097/NNR.0b013e31827bf533 [DOI] [PMC free article] [PubMed]
- Weathers, F. W., Litz, B. T., Keane, T. M., Palmieri, P. A., Marx, B. P., & Schnurr, P. P. (2013b). The PTSD Checklist for DSM-5 (PCL-5). Scale retrieved from the National Center for PTSD at www.ptsd.va.gov.
- Weathers, F., Blake, D., Schnurr, P., Kaloupek, D., Marx, B., & Keane, T. (2013a). The clinician-administered PTSD scale for DSM-5 (CAPS-5). [Measurement Instrument]. Retrieved from www.ptsd.va.gov.
- Weathers FW, Litz BT, Keane TM, Herman DS, Steinberg HR, Huska JA, Kraemer HC. The utility of the SCL-90-R for the diagnosis of war-zone related posttraumatic stress disorder. Journal of Traumatic Stress. 1996;9(1):111–128. doi: 10.1007/BF02116837. [DOI] [PubMed] [Google Scholar]
- World Health Organization. (2019). International Statistical Classification of Diseases and Related Health Problems, 11th ed. Retrieved from https://icd.who.int/
- Wortmann JH, Jordan AH, Weathers FW, Resick PA, Dondanville KA, Hall-Clark B, Foa EB, Young-McCaughan S, Yarvis JS, Hembree EA, Mintz J, Peterson AL, Litz BT. Psychometric analysis of the PTSD Checklist-5 (PCL-5) among treatment-seeking military service members. Psychological Assessment. 2016;28(11):1392–1403. doi: 10.1037/pas000026. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author, EL, upon reasonable request.
N/A.