Abstract
Objective:
The objective is to identify research priorities in prehospital care in Spain.
Method:
This was a Delphi-type study of three rounds with a panel of experts made up of members of the Red de Investigación en Emergencias Prehospitalarias (RINVEMER; Prehospital Emergency Research Network) Network and the Sociedad Española de Medicina de Urgencias y Emergencias (SEMES; Spanish Society of Emergency Medicine) Emergency Secretariat. In the first round, each participant identified up to 15 priorities. In the second round, they scored the 30 thematic areas on a Likert scale. In the third round, they ordered and scored from one to ten the first ten priorities among those that obtained a median greater than or equal to four in the second round. After adding the assigned scores, the ten priorities with the highest total score were obtained.
Results:
The ten identified research priorities were: special clinical codes and time-dependent conditions; mass-casualty incident (MCI) coordination and management; innovation in Emergency Medical Services (EMS); human factor in decision making; triage, analysis, and management of calls in the Emergency Call Center; new technologies, telemedicine, and emergencies; adverse events, clinical safety, and quality in emergencies; cardiac arrest; continuous education and training (methodology, quality, and evaluation); and big data and emergencies.
Conclusions:
The research priorities perceived by emergency professionals are related to clinical care and organizational aspects of EMS, in addition to the need to incorporate innovative aspects and new data analysis technologies.
Keywords: Delphi study, emergency systems, evidence-based medicine, research priorities
Introduction
Health care bases its progress on the lessons learned in daily clinical practice, as well as on applied research based on the principles of scientific evidence. However, this scientific approach has added difficulties in the field of prehospital emergencies, 1,2 and there are important controversies about different care aspects that have not been able to be supported on the basis of evidence-based medicine. 3,4 For example, being the highest percentage of patients treated on scene and transferred to the hospital by the non-critical emergency system, it has not been adequately demonstrated what the optimal management of this entire clinical care process is like from the point of view of type of resources, staff involved, or making transfer decisions. However, aspects that are adequately supported by the principles of evidence-based medicine, such as posttraumatic stress in health professionals who intervene in emergencies, are addressed anecdotally on a day-to-day basis. 5 For this reason, and as a first step, it is important to identify what would be, in the opinion of the experts, the main research priorities in this field in order to optimize research efforts and obtain results that are of practical application in daily clinical practice and in the management of health resources. The growing number of research papers by emergency professionals in Spain makes it even more necessary to guide research strategies to respond to the clinical, care, and organizational needs of emergency systems. 6 Even so, and taking data from Catalonia, it could be estimated that the percentage of prehospital emergency physicians who carry out research in Spain is still low. 7
Countries with a longer tradition in prehospital emergency research analyze over time how the research priorities perceived by groups of experts change, using the results as a guide to orient research policies in emergency systems. From the first studies to the current ones, some priorities have been maintained and others have been changing as new social needs evolve. 8
In one of the first studies carried out in this regard in 2011, a European research collaboration identified as research priorities, in order of importance: 9 type of staff, training, and the value of doctors at the prehospital level; advanced airway management; time window for critical interventions at the prehospital level; the role of prehospital ultrasound; and resource activation criteria for prehospital critical care units. Seven years later, another study served to advance knowledge of some of the aspects identified, 8 although others, such as the role of the doctor, continue to be an important field of study. 10
In 2016, a Netherlands study determined as research priorities: 11 home discharges, quality improvement measures, registration, and exchange of patient data; care and task substitution triage; and assessment of acute neurological signs and symptoms.
A more recent Netherlands study updated these research priorities, identifying the following as priorities: 12 not-conveyed patients, patient registration, and clinical data in the care chain; care coordination, interprofessional collaboration, care stratification, and triage; and classification of emergencies. In addition, they identify the vulnerable elderly population as a priority of special interest. The most interesting thing is that these studies serve as a reference so that researchers can design a research strategy within an appropriate time frame, in order to respond to the needs raised by professionals, which will inherently be linked to the improvement of prehospital health care for the benefit of patients and the management of health resources.
To date, an analysis of research priorities in prehospital emergencies has not been carried out in Spain, which would represent the first step for effective research focused on needs. The objective of this study is to identify research priorities in prehospital care in Spain, with a physician-staff Emergency Medical Services (EMS).
Methods
A three-round, Delphi-type study was designed with a panel of experts made up of members of the Red de Investigación en Emergencias Prehospitalarias (RINVEMER; Prehospital Emergency Research Network) Network and the Sociedad Española de Medicina de Urgencias y Emergencias (SEMES; Spanish Society of Emergency Medicine) Emergency Secretariat. These experts were selected by purposeful sampling among members of RINVEMER and SEMES with more than ten years of clinical experience in prehospital care and research interest and experience. Individuals not meeting these inclusion criteria were excluded.
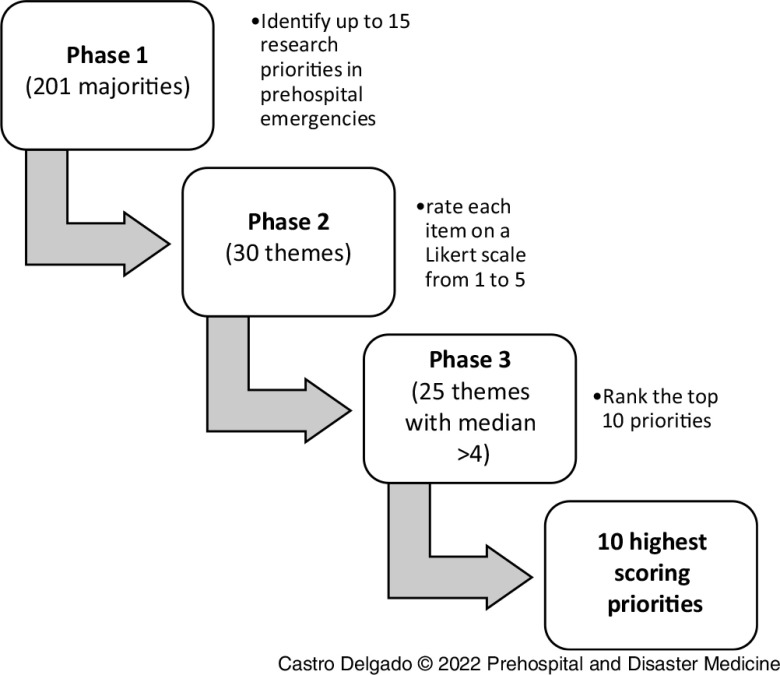
In the first round, each participant indicated a maximum of 15 research priorities that they considered relevant in Spain. After grouping them by topics, in the second round, the participants graded each of the priorities on a Likert scale from one to five. For the third round, those items whose median in the second round had been equal to or greater than four were selected, and the participants were asked to order the ten with the highest priority from highest to lowest, assigning ten points to the highest, and so on, until zero points to the tenth priority. In this third round, they were also asked to assess on a scale of one to five the weight that certain criteria had in choosing some priorities or others in order to weigh how that element had influenced the participants’ perception of the research priority. Figure 1 represents the flow of the three phases. The panel of experts was made up of 22 doctors and nurses who participated in all rounds. This study was approved by the Research Ethics Committee of the Principality of Asturias, Spain (code CEImpA 2022.200).
Figure 1.
Development of the Study.
Results
The participants included nine doctors and 13 nurses, with a mean of 20.4 (SD = 3.3) years of experience in prehospital emergencies.
In the first round, 201 research priorities were obtained, which were later grouped into 30 topics. The themes that were repeated the most were those related to: initial care for severe trauma (14); special clinical codes and time-dependent conditions (10); adverse events, clinical safety, and quality in emergencies (9); physiology of medical transport (9); cardiorespiratory arrest (9); first aid, cardiopulmonary resuscitation (CPR) at school and population, and use of the automated external defibrillator (AED) (8); triage, analysis, and call management in the Emergency Call Center (8); management in emergency systems and out-of-hospital resources (8); and coordination and management in mass-casualty incidents (MCIs) (7). Table 1 shows the results of the first round. In the second round, the participants rated their perception of their research priority on a Likert scale from one to five, with the highest scores being: initial care for severe trauma; special clinical codes and time-dependent conditions; adverse events, clinical safety, and quality in emergencies; cardiac arrest; coordination and management in IMV; and innovation in EMS. The complete results are reflected in Table 2. For round three, the 25 topics that obtained a median greater than or equal to four were selected. Each participant selected ten of the topics and assigned scores from zero (10th) to ten points (1st). In this way, the ten research priorities in prehospital emergencies were finally identified that, according to the panel of experts, should be taken into consideration in Spain, the following being the ones that obtained the highest scores: special clinical codes and time-dependent conditions (114 points); MCI coordination and management (91 points); innovation in EMS (73 points); the human factor in decision making (72 points); and triage, analysis, and call management in the Emergency Call Center (69 points). The complete results are reflected in Table 3, including global results and for doctors and nurses. There were no differences in these top five research priorities between doctors and nurses. In the top ten, doctor would include “management in emergency systems and prehospital resources;” “initial care for severe trauma;” and “prehospital ultrasound” but would exclude “adverse events, clinical safety, and quality in emergencies;” “human factor in decision making;” and “big data and emergencies.” In the case of nurses, they would include “simulation in emergencies” and “telephone CPR” but would exclude “continuous education and training (methodology, quality, and evaluation)” and “cardiac arrest.” Globally, no differences were found in doctors’ and nursing scores (P = .84), and only one item had statistical difference (“continuous education and training [methodology, quality, and evaluation]) scoring higher with doctors (P = .04); Table 4.
Table 1.
Results of the First Round Grouped into Topics
| 30 PRIORITIES | No. of Responses |
|---|---|
| Severe Trauma Care | 14 |
| Special Clinical Codes and Time-Dependent Conditions | 10 |
| Adverse Events, Clinical Safety, and Quality in Emergencies | 9 |
| Physiology of Medical Transport | 9 |
| Cardiac Arrest | 9 |
| First Aid and Cardiopulmonary Resuscitation (CPR) in School and Population: Use of the Automated External Defibrillator (AED) | 8 |
| Triage Analysis and Management of Calls in the Emergency Call Center | 8 |
| Management in Emergency Systems and Prehospital Resources | 8 |
| Coordination and Management in Mass-Casualty Incidents (MCIs) | 7 |
| New Technologies, Telemedicine, and Emergencies | 7 |
| Prehospital Stroke Care | 7 |
| Continuous Education and Training (Methodology, Quality, and Evaluation) | 6 |
| Big Data and Emergencies | 6 |
| Job Satisfaction and Burn-Out | 6 |
| Triage in Mass-Casualty Incidents (MCIs) | 5 |
| Prehospital Ultrasound | 5 |
| Human Factor in Decision Making | 5 |
| Organization of Severe Trauma Care | 4 |
| Innovation in Emergency Medical Services (EMS) | 4 |
| Simulation in Emergencies | 3 |
| Telephone CPR | 3 |
| Mechanical Ventilation in Emergencies | 3 |
| Emergency Information Systems | 3 |
| Prehospital Care for Acute Coronary Syndrome | 3 |
| Emotional Management and Communication with Patients | 3 |
| Epidemiology in Emergencies | 3 |
| Prognosis and Quality of Life after Cardiac Arrest | 2 |
| Use of Blood Products in Out-Patient Care | 2 |
| Head Injury | 1 |
| Smart Ambulances | 1 |
Table 2.
Results of the Second Round Scores
| PRIORITY | Median | IQR | COD |
|---|---|---|---|
| Severe Trauma Initial Care | 5 | 1 | 0.136 |
| Special Clinical Codes and Time-Dependent Conditions | 5 | 1 | 0.064 |
| Adverse Events, Clinical Safety, and Quality in Emergencies | 5 | 1 | 0.12 |
| Cardiac Arrest | 5 | 1 | 0.152 |
| Coordination and Management in Mass-Casualty Incidents (MCIs) | 5 | 1 | 0.088 |
| Innovation in Emergency Medical Services (EMS) | 5 | 1 | 0.112 |
| First Aid and CPR in the School and Population: AED Use | 4 | 2 | 0.19 |
| Triage Analysis and Management of Calls in the Emergency Call Center | 4 | 1 | 0.14 |
| Management in Emergency Systems and Prehospital Resources | 4 | 2 | 0.17 |
| New Technologies, Telemedicine, and Emergencies | 4 | 1 | 0.13 |
| Prehospital Stroke Care | 4 | 2 | 0.19 |
| Continuous Education and Training (Methodology, Quality, and Evaluation) | 4 | 1 | 0.18 |
| Big Data and Emergencies | 4 | 1 | 0.16 |
| Triage in Mass-Casualty Incidents (MCIs) | 4 | 1 | 0.18 |
| Prehospital Ultrasound | 4 | 2 | 0.22 |
| Human Factor in Decision Making | 4 | 1 | 0.17 |
| Organization of Care to Severe Trauma | 4 | 1 | 0.16 |
| Simulation in Emergencies | 4 | 2 | 0.18 |
| Telephone CPR | 4 | 1 | 0.18 |
| Mechanical Ventilation in Emergencies | 4 | 2 | 0.18 |
| Emergency Information Systems | 4 | 1 | 0.14 |
| Prehospital Care for Acute Coronary Syndrome | 4 | 2 | 0.18 |
| Emotional Management and Communication with Patients | 4 | 1 | 0.21 |
| Use of Blood Products in Out-Patient Care | 4 | 1 | 0.182 |
| Cranioencephalic Trauma | 4 | 2 | 0.21 |
| Prognosis and Quality of Life after Cardiac Arrest | 3.5 | 1 | 0.26 |
| Smart Ambulances | 3.5 | 2 | 0.28 |
| Physiology of Medical Transport | 3 | 2 | 0.32 |
| Job Satisfaction and Burn-Out | 3 | 2 | 0.26 |
| Epidemiology in Emergencies | 3 | 1 | 0.24 |
Abbreviations: IQR, interquartile range; COD, coefficient of dispersion; CPR, cardiopulmonary resuscitation; AED, automated external defibrillator.
Table 3.
Top Ten Research Priorities
| 10 Research Priorities in Prehospital Care in Spain | Total Score | Average Total (IC 95%) |
Average Doctors (IC 95%) |
Average Nurses (IC 95%) |
t (p) |
|---|---|---|---|---|---|
| Special Clinical Codes and Time-Dependent Conditions | 114 | 5.18 (3.35 to 7.01) |
7.22 (4.22 to 10.21) |
3.76 (1.47 to 6.05) |
2.08 (.050) |
| Coordination and Management of Mass-Casualty Incidents | 91 | 4.13 (2.48 to 5.79) |
4.44 (1.59 to 7.29) |
3.92 (1.57 to 6.26) |
2.08 (.75) |
| Innovation in Emergency Medical Services | 73 | 3.31 (1.58 to 5.05) |
3.55 (0.24 to 6.86) |
3.15 (0.86 to 5.43) |
2.08 (.81) |
| Human Factor in Decision Making | 72 | 3.27 (1.69 to 4.85) |
1.55 (-0.48 to 3.59) |
4.46 (2.21 to 6.70) |
2.08 (.057) |
| Cardiac Arrest | 71 | 3.22 (1.40 to 5.04) |
4.88 (1.27 to 8.50) |
2.07 (0.05 to 4.10) |
2.08 (.11) |
| Triage, Analysis, and Management of Calls in the Emergency Call Center | 69 | 3.16 (1.57 to 4.69) |
2.11 (-0.07 to 4.30) |
3.86 (1.50 to 6.18) |
2.08 (.26) |
| Continuous Education and Training (Methodology, Quality, and Evaluation) | 66 | 3.00 (1.65 to 4.34) |
4.55 (2.21 to 6.89 |
1.93 (0.33 to 3.51) |
2.08 (.04)* |
| New Technologies, Telemedicine, and Emergencies | 65 | 2.95 (1.37 to 4.53) |
3.22 (0.95 to 3.28) |
2.76 (0.35 to 5.21) |
2.08 (.77) |
| Adverse Events, Clinical Safety, and Quality in Emergencies | 64 | 2.90 (1.23 to 4.57) |
1.66 (-0.50 to 3.84) |
3.76 (1.23 to 6.29) |
2.08 (.20) |
| Big Data and Emergencies | 58 | 2.63 (1.16 to 4.10) |
1.11 (-0.18 to 2.41) |
3.69 (1.39 to 5.98) |
2.08 (.07) |
Table 4.
Doctors’ and Nurses’ Top Ten Priorities and Their Position Variation compared with Global Results
| DOCTORS | NURSES | ||||
|---|---|---|---|---|---|
| Top Ten | Total Score | Position Variation | Top Ten | Total Score | Position Variation |
| Special Clinical Codes and Time-Dependent Conditions | 65 | = | Human Factor in Decision Making | 58 | ↑3 |
| Cardiac Arrest | 44 | ↑2 | Coordination and Management of Mass-Casualty Incidents | 51 | = |
| Continuous Education and Training (Methodology, Quality, and Evaluation) | 41 | ↑4 | Triage, Analysis, and Management of Calls in the Emergency Call Center | 50 | ↑3 |
| Coordination and Management of Mass-Casualty Incidents | 40 | ↓2 | Special Clinical Codes and Time-Dependent Conditions | 49 | ↓3 |
| Innovation in Emergency Medical Services | 32 | ↓2 | Adverse Events, Clinical Safety, and Quality in Emergencies | 49 | ↑4 |
| New Technologies, Telemedicine, and Emergencies | 29 | ↑2 | Big Data and Emergencies | 48 | ↑4 |
| Management in Emergency Systems and Prehospital Resources | 27 | ↑6 | Innovation in Emergency Medical Services | 41 | ↓4 |
| Organization of Severe Trauma Care | 25 | ↑3 | Simulation in Emergencies | 40 | ↑4 |
| Prehospital Ultrasound | 20 | ↑7 | New Technologies, Telemedicine, and Emergencies | 36 | ↓1 |
| Triage, Analysis, and Management of Calls in the Emergency Call Center | 19 | ↓2 | Telephone CPR | 36 | ↑4 |
Regarding the motivations that served to determine the research priorities and assign the corresponding scores in each of the phases of the study, the elements that had the greatest weight were personal interest in the subject, the importance of the problem in terms of severity for the patient, and the level of scientific knowledge on the subject. The complete evaluations are reflected in Table 5.
Table 5.
Motivations for Deciding Research Priorities in Prehospital Care in Spain
| Motivation | Average | Mean Deviation | Median | IQR | COD |
|---|---|---|---|---|---|
| Personal Interest in the Topic | 4.54 | 0.61 | 5 | 1 | 0.09 |
| Significance of the Problem in terms of Severity for the Patient | 4.36 | 0.63 | 4.5 | 1 | 0.14 |
| Level of Scientific Knowledge on the Subject | 4.27 | 0.46 | 4 | 1 | 0.09 |
| Insufficient Transfer of Knowledge to Clinical Practice | 4.09 | 0.66 | 4 | 1 | 0.15 |
| Clinical Frequency | 4.04 | 0.78 | 4 | 1 | 0.19 |
| Insufficient Degree of Knowledge on the Subject | 3.95 | 0.79 | 4 | 1.75 | 0.19 |
| Level of Clinical and Scientific Controversy | 3.68 | 0.67 | 4 | 1 | 0.14 |
Abbreviations: IQR, interquartile range; COD, coefficient of dispersion.
Discussion
Most of the studies carried out to date in relation to establishing research priorities in prehospital care have been carried out in the Nordic countries, with an important research trajectory in this regard. For the first time in Spain, this study addresses the research priorities in prehospital care perceived by a group of experts. Being the first, it is not possible to analyze trends in Spain over recent years, but it is possible to compare these results with studies previously carried out in other countries. The results found are somewhat similar to those obtained in the 2011 European study, where aspects related to time-dependent conditions or specific technical aspects are identified as research priorities. 9 The fact that special clinical codes and time-dependent conditions is the element with the highest score highlights two aspects: on the one hand, it is a field that is related to resource management, but also, to specific clinical aspects. Therefore, these results would be more similar to the new needs identified in more recent studies, where aspects related to resource management and coordination have more weight. As identified by other studies that analyze trends in research priorities in prehospital emergencies, in the last ten years, it has been observed a change in interest from specific medical aspects to aspects more related to care coordination and the organization of EMS.
Although in many previous studies, the need to investigate the issue of non-conveyed patients has been highlighted, in this case, this aspect has not been relevant. This may be due to the presence of a doctor in the Advanced Life Support units, which means that the medical decision to discharge “on scene” may be considered adequate by the mere fact that it was made by a physician, which probably, according to the interviewees, does not require further analysis. In this regard, results found do take into account the human factors linked to decision making, due again to the fact of the need to study what aspects determine the making of certain decisions over others. 13
The fact that the coordination and management of MCIs is an aspect identified as relevant in the field of investigation may be due to the history that exists, in Spain, in relation to the MCIs and recent terrorist attacks 14 whose responses perhaps are perceived as little analyzed and with room for improvement.
The need to innovate in EMS may be determined by the fact that professionals perceive that the current structure of EMS must be adapted to new technologies that facilitate resource management, already mentioned in another item, and decision making (also mentioned as another item). Perhaps there is a feeling among professionals that EMS may be late in adapting to new social needs, hence the need to increase research in aspects related to innovation in EMS to develop new tools adapted to a changing reality. This aspect is also related to other identified priorities, such as “new technologies, telemedicine, and emergencies” or “big data and emergencies,” perhaps because the COVID-19 pandemic has allowed health professionals to identify niches of innovation in EMS useful for the whole health system. 15
Also related to “resource management, decision making, and new technologies” is the priority “triage, analysis, and management of calls in the Emergency Call Center.” Appropriate resource management seems to be a recurring concern among emergency professionals, since they move in an environment with scarce resources that must be used and positioned in the most effective and efficient way possible. 16 In addition, there are multiple studies that link new technologies, big data, and artificial intelligence (identified as a priority) with the management of calls and the sending of resources by the Emergency Call Center. 17,18 Therefore, there are links between research priorities, which highlights the need for a cross-sectional approach as one of the elements to consider in prehospital emergency research.
In relation to specific diseases, only “cardiac arrest” appears among the top ten research priorities. This may be due to the fact that the periodic updating of these guidelines makes emergency professionals aware of the constant need to seek the best health care for cardiac arrest.
That “adverse events, clinical safety, and quality in emergencies” also appears among the top ten priorities highlights a need perceived as important within the care field of prehospital emergencies, as shown by some publications in this regard, 19 with a significant room for improvement. “Continuous training” also appears in the top ten priorities, a fact that shows the commitment of emergency professionals to their on-going training, making it necessary to seek the best technical options in terms of new teaching methodologies. 20,21
In the latest European study in this regard, they identify a priority that they consider to be of special interest: care for vulnerable elderly people. 12 This aspect, which is increasingly common in the daily work of emergency systems, 22,23 has not been identified in this study.
When analyzing differences between doctors and nurses, although global differences have not been found, some slight differences can be explained by the fact that both groups may have different approaches towards the patient. Nurses ranked top human factor, and did not rank prehospital ultrasound, which nowadays is more linked in Spain to a doctor responsibility. In the case of doctors, the top ranked “special clinical codes and time-dependent conditions” is more linked to a clinical approach and to organizational structure.
In relation to personal motivations to identify research priorities, as expected, personal interest in the topic plays a predominant role. The importance of this factor lies in the fact that a personal interest can drive interesting research avenues. In any case, the severity of the patient and the level of scientific knowledge on the subject also obtained high scores.
More than ever, it is necessary to adapt emergency systems to a changing reality, both in economic and social, demographic, and public health terms, and to integrate them into a network health system where primary care plays an important role. And this can only be done by properly monitoring the health needs of the population and the research priorities perceived by professionals.
Limitations
As limitations of this study, the results have been found in one specific country with a physician-staffed EMS, so these results may not be applicable to other countries or circumstances. Also, as any other Delphi study, they are based on experts’ perceptions that are not representative of an entire population, but may help to figure out general results and design strategic actions.
Conclusion
The top research priorities in prehospital care in Spain perceived by doctors and nurses are related to clinical care and organizational aspects of EMS, in addition to the need to incorporate innovative aspects and new data analysis technologies. Specifically, special clinical codes and time-dependent conditions, coordination and management of MCIs, innovation in EMS, and human factor in decision making are the top-ranked priorities.
Acknowledgements
The authors acknowledge the Red de Investigación en Emergencias Prehospitalarias (RINVEMER; Prehospital Emergency Research Network) Network and the Sociedad Española de Medicina de Urgencias y Emergencias (SEMES; Spanish Society of Emergency Medicine) Emergency Secretariat, and especially all the members who have selflessly collaborated in this study to design future research lines of action in prehospital care in Spain.
Conflicts of interest/Funding
None declared. The authors have no financial or other interest that should be known by the readers related to this document.
References
- 1. Castro Delgado R, Arcos Gonzalez P. Difficulties and challenges of clinical research in out-of-hospital emergency settings. Emergencies. 2022;34(4):314–316. [PubMed] [Google Scholar]
- 2. McLean SA, Maio RF, Spaite DW, Garrison HG. Emergency medical services outcomes research: evaluating the effectiveness of prehospital care. Prehosp Emerg Care. 2002;6(2 Suppl):S52–56. [DOI] [PubMed] [Google Scholar]
- 3. University of Sheffield Medical Care Research Unit. Building the evidence base in pre-hospital urgent and emergency care. A review of research evidence and priorities for future research. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/216064/dh_117198.pdf. Accessed September 2022.
- 4. Brown KM, Macias CG, Dayan PS, et al. The development of evidence-based prehospital guidelines using a GRADE based methodology. Prehosp Emerg Care. 2014;18(Suppl 1):3–14. [DOI] [PubMed] [Google Scholar]
- 5. Sterud T, Ekeberg Ø, Hem E. Health status in the ambulance services: a systematic review. BMC Health Serv Res. 2006;6:82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Castejón de la Encina E, Delgado Sánchez R, Ayuso Baptista F, López Mesa F, Castro Delgado R. Origin of the Prehospital Emergency Research Network (RINVEMER): bibliometric analysis of scientific production in prehospital emergencies. Emergencies. 2022;34:209–219. [PubMed] [Google Scholar]
- 7. Escalada X, Sánchez P, Hernández R, et al. Prehospital emergency services in Catalonia: the SEPHCAT analysis. Emergencies. 2020;32(2):90–96. [PubMed] [Google Scholar]
- 8. Bache KG, Rehn M, Thompson J. Seven years since defining the top five research priorities in physician-provided pre-hospital critical care - what did it lead to and where are we now? Scand J Trauma Resusc Emerg Med. 2018;26(1):101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Fevang E, Lockey D, Thompson J, Lossius HM; Research Collaboration Torpo. The top five research priorities in physician-provided pre-hospital critical care: a consensus report from a European research collaboration. Scand J Trauma Resusc Emerg Med. 2011;19:57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Rehn M, Bache KG, Lossius HM, Lockey D. Top five research priorities in physician-provided pre-hospital critical care - appropriate staffing, training, and the effect on outcomes. Scand J Trauma Resusc Emerg Med. 2020;28(1):32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. van de Glind I, Berben S, Zeegers F, et al. A national research agenda for pre-hospital emergency medical services in the Netherlands: a Delphi-study. Scand J Trauma Resusc Emerg Med. 2016;24:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Vloet LCM, Hesselink G, Berben SAA, Hoogeveen M, Rood PJT, Ebben RHA. The updated national research agenda 2021-2026 for prehospital emergency medical services in the Netherlands: a Delphi study. Scand J Trauma Resusc Emerg Med. 2021;29(1):162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Al -Azri NH. How to think like an emergency care provider: a conceptual mental model for decision making in emergency care. Int J Emerg Med. 2020;13(1):17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Sala Sanjaume J, Morales Álvarez J, Castillo Paramio X. 17 A. Terrorist attack in Barcelona: first impressions. Emergencies. 2017;29:301–302. [PubMed] [Google Scholar]
- 15. Castro Delgado R, Delgado Sánchez R, Duque del Río MC, Arcos González P. Potential capacity of an emergency dispatch center to predict admissions to hospitals and intensive care units due to COVID-19. Emergencies. 2021;33(5):369–374. [PubMed] [Google Scholar]
- 16. Jagtenberg CJ, Vollebergh MAJ, Uleberg O, Røislien J. Introducing fairness in Norwegian air ambulance base location planning. Scand J Trauma Resusc Emerg Med. 2021;29(1):50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Ceklic E, Tohira H, Ball S, et al. A predictive ambulance dispatch algorithm to the scene of a motor vehicle crash: the search for optimal over and under triage rates. BMC Emerg Med. 2022;22(1):74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Wibring K, Lingman M, Herlitz J, et al. The potential of new prediction models for emergency medical dispatch prioritization of patients with chest pain: a cohort study. Scand J Trauma Resusc Emerg Med. 2022;30(1):34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Galván Núñez P, Santander Barrios MD, Villa Álvarez MC, Castro Delgado R, Alonso Lorenzo JC, Arcos González P. Results of the provisional establishment of a voluntary and anonymous system for reporting patient safety incidents in the SAMU of Asturias. Emergencies. 2016;28(3):146–152. [PubMed] [Google Scholar]
- 20. Castro Delgado R, Fernández García L, Cernuda Martínez JA, Cuartas Álvarez T, Arcos González P. Training of medical students for mass casualty incidents using table-top gamification. Disaster Med Public Health Prep. 2022. Epub ahead of print. [DOI] [PubMed]
- 21. Ferrandini Price M, Escribano Tortosa D, Nieto Fernandez-Pacheco A, et al. Comparative study of a simulated incident with multiple victims and immersive virtual reality. Nurse Educ Today. 2018;71:48–53. [DOI] [PubMed] [Google Scholar]
- 22. Harthi N, Goodacre S, Sampson F, Alharbi R. Research priorities for prehospital care of older patients with injuries: scoping review. Age Ageing. 2022;51(5):afac108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Goldstein J, McVey J, Ackroyd-Stolarz S. The role of Emergency Medical Services in geriatrics: bridging the gap between primary and acute care. CJEM. 2016;18(1):54–61. [DOI] [PubMed] [Google Scholar]