Abstract
This meta‐review aimed to appraise and synthesise findings from existing systematic reviews that measured the impact of compression therapy on venous leg ulcers healing. We searched five databases to identify potential papers; three authors extracted data, and a fourth author adjudicated the findings. The AMSTAR‐2 tool was used for quality appraisal and the certainty of the evidence was appraised using GRADEpro. Data analysis was undertaken using RevMan. We identified 12 systematic reviews published between 1997 and 2021. AMSTAR‐2 assessment identified three as high quality, five as moderate quality, and four as low quality. Seven comparisons were reported, with a meta‐analysis undertaken for five of these comparisons: compression vs no compression (risk ratio [RR]: 1.55; 95% confidence interval [CI] 1.34‐1.78; P < .00001; moderate‐certainty evidence); elastic compression vs inelastic compression (RR: 1.02; 95% CI: 0.96‐1.08; P < .61 moderate‐certainty evidence); four layer vs <four‐layer bandage systems (RR: 1.07; 95% CI: 0.82‐1.40; P < .63; moderate‐certainty evidence); comparison between different four‐layer bandage systems (RR: 1.08; 95% CI: 0.93‐1.25; P = .34; moderate‐certainty evidence); compression bandage vs compression stocking (RR 0.95; 95% CI 0.87‐1.03; P = .18; moderate‐certainty evidence). The main conclusion from this review is that there is a statistically significant difference in healing rates when compression is used compared with no compression, with moderate‐certainty evidence. Otherwise, there is no statistically different difference in healing rates using elastic compression vs inelastic compression, four layer vs <four‐layer bandage systems, different four‐layer bandage systems, or compression bandages vs compression stockings.
Keywords: compression bandages, compression therapy, healing, meta‐review, venous leg ulcers
1. INTRODUCTION
Venous leg ulcers (VLUs) are chronic wounds that occur within the lower region of the leg between the knee and ankle as a consequence of venous insufficiency. 1 Venous valve dysfunction, deep vein occlusion, and the failure of the calf muscle represent the mechanisms that cause venous insufficiency and associated venous hypertension. 2 , 3 Venous leg ulcers distress patients, cause pain, increase the risk of infection, can exude odour, and severely impact patients' mobility and quality of life. 4 , 5
The incidence of venous leg ulceration ranges between 1% and 3% in adults. 6 While the risk of VLU increases with age, 22% of individuals develop their first VLUs by 40 years of age and 13% before 30 years of age, negatively affecting their ability to work and participate in social activities. 7 The healing of VLU represents a notoriously slow process, 93% of VLUs will heal in 12 months and 7% remain unhealed after 5 years, while the recurrence rate within 3 months of healing is around 70%. 8
Compression therapy (CT) represents the standard of care for conservative treatment of VLU. 9 CT works by generating external pressure on the superficial veins and tissues, thereby assisting venous return. Improved venous return helps to reduce peripheral oedema and promotes lower limb wound healing. 10 Published healing rates of VLU managed with CT vary widely from 40% to 95%. 11 Clinicians can provide CT by three different techniques: bandage systems, stockings/hosiery, or active intermittent compression devices. 7 This meta‐review of existing systematic reviews considers the impact of CT on VLU healing.
2. RESEARCH QUESTION
The research questions explored in this meta‐review were as follows:
What is the effect of compression therapy on venous leg ulcer healing?
What is the effect of venous leg ulcer compression therapy on adverse events?
2.1. Aim
The aim of this meta‐review was to appraise and synthesise the evidence from existing systematic reviews that measured the impact of CT on VLU healing.
3. METHODS
We conducted a meta‐review of systematic reviews. Meta‐reviews aggregate the summarised results of systematic reviews and help to inform policy and practice decision‐making. 12 Similar to systematic reviews, meta‐reviews include selecting systematic reviews, quality appraisal of the reviews, providing results, giving an overview of results for practice, and research‐related implications. 13 Using the PICO framework 14 as a guide, this meta‐review appraised existing systematic reviews that measured CT's impact on venous leg ulcer healing.
The components of the PICO were:
Population: Patients with a venous leg ulcer
Intervention: CT, however, specified by the review author(s).
Comparison: Other intervention or none
Outcome: Primary—healing (time and rate). Secondary—adverse events
The author team followed the standard approach advocated for systematic reviews and used the Preferred Reporting Items for Systematic Reviews and Meta‐Analyses (PRISMA) guidelines 15 to guide the conduct and reporting of the meta‐review. The PRISMA refers to present records identified through all databases searched and is presented in Figure 1. The study protocol was pre‐registered with the International Prospective Register of Systematic Reviews (CRD 42021233417).
FIGURE 1.
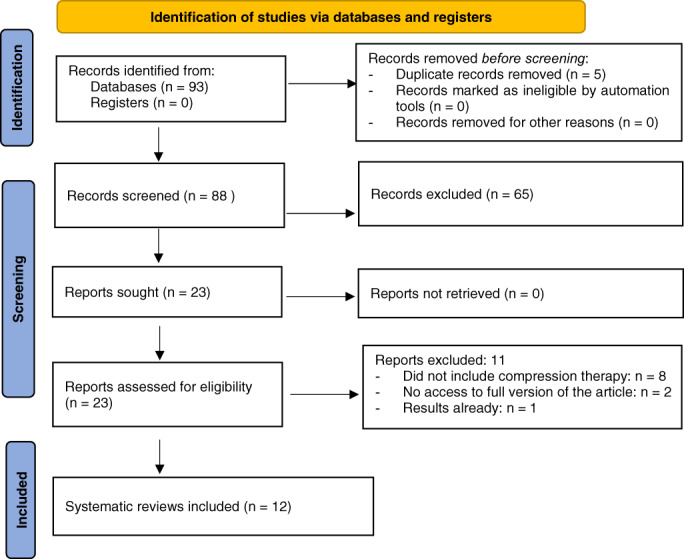
PRISMA 2020 flow diagram for study selection 31
3.1. Search strategy
The following inclusion criteria were used,
Published systematic reviews, with no geographic restriction for study sites.
Reviews are written in English.
Healing as a primary or secondary outcome.
Reviews only consider studies in adults (aged over 16 years).
Clinical setting of any type.
CT, however defined in the review.
The exclusion criteria were as follows,
An identified review included results from paediatric patients.
Non‐English reviews.
A Health Sciences Librarian advised on the literature search in July 2021. The primary search included five databases (MEDLINE (Ovid), EMBASE (Ovid), EBM Reviews, and Cochrane Library (Ovid), Cumulative Index to Nursing and Allied Health Literature (CINAHL), Web of Science). Search terms are in Table 1. To identify further published systematic reviews, secondary searches were included.
Reference lists of all included reviews
Grey literature using OpenGrey (www.opengrey.eu);
Conference proceedings, research reports.
TABLE 1.
Search terms used
| #1 Chronic Venous leg Ulcer OR Venous Leg Ulcer, OR Ulcers, leg ulcers |
| #2 Healing OR heal OR wound healing OR VLU healing |
| #3 Time to healing OR Time to heal |
| #4 Compression Therapy OR Compression therapies OR dressing, bandage OR Dressings, Bandages |
| #5 Venous Leg ulcer recurrence OR ulcer recurrence |
| #6: #1 OR #2 OR #3 OR#4 OR #5 |
| #7 effectiveness |
| #8: #6 AND #7 |
| #9 Wound care |
| #10: #8 AND #9 |
3.2. Screening
Four team members independently assessed the article titles and abstracts of existing systematic reviews. The same team then reviewed the full‐text versions of potentially relevant reviews against the inclusion/exclusion. To include a review, the four team members reached a consensus through discussion. A fifth team member adjudicated when the four reviewing team members could not agree on inclusion or exclusion of a specific review.
3.3. Data extraction
For included reviews, three authors extracted data independently using a purpose‐built and piloted data extraction table. The data extracted related to the review type, types of papers reviewed, sample, setting and population, intervention, control, and the results. A fourth author adjudicated on disagreements or discrepancies.
3.4. Quality assessment
For quality assessment, we used the 16‐item AMSTAR‐2 tool as it enables a reliable and swift quality appraisal of systematic reviews. 16 The 16 questions included relating to the review question, methods, search strategy, data extraction, data analysis, and risk of bias. Two authors completed the AMSTAR‐2 tool, with a third intervening where disagreements or discrepancies occurred. While not giving an overall score, the AMSTAR‐2 tool allowed the group to determine an overall quality rating for each included review. In addition, the certainty of the evidence related to each of the main outcomes was evaluated by using GRADE (Grades of Recommendation, Assessment, Development, and Evaluation). This certainty of the evidence was assessed against five principle domains: (a) limitations in design and implementation; (b) indirectness of evidence or generalisability of findings; (c) inconsistency of results, for example, unexplained heterogeneity and inconsistent findings; (d) imprecision of results where confidence intervals (CIs) are wide; and (e) publication bias. 17
3.5. Synthesis
After removing duplicate data from studies included in multiple reviews, where appropriate meta‐analysis statistical synthesis was undertaken using RevMan. 18 Relative risks (RR) and 95% CIs were calculated for dichotomous outcomes, and mean differences and 95% CI were calculated for continuous outcomes. Results of comparable trials were pooled using a fixed‐effect model and 95% CI. Heterogeneity was investigated by calculating the I 2 statistic. 17
4. RESULTS
4.1. Overview of all included studies
Figure 1 outlines the flow of articles through the screening process that led to the inclusion of 12 systematic reviews. 19 , 20 , 21 , 22 , 23 , 24 , 25 , 26 , 27 , 28 , 29 , 30 Table 2 identifies the nine excluded studies and the reason for exclusion from the final screening step.
TABLE 2.
Excluded studies
| Author | Reason for exclusion |
|---|---|
| Norman, Westby 32 | Relates to dressings rather than compression bandages |
| Palfreyman, Nelson 33 | Relates to dressings rather than compression bandages |
| Palfreyman, Nelson 34 | Relates to dressings rather than compression bandages |
| Bouza, Muñoz 35 | Relates to dressings rather than compression bandages |
| Turner‐Boutle, Fletcher 36 | Could not access the full version of the article |
| de Carvalho 37 | Could not access the full version of the article |
| Jull, Slark 38 | Not directly focused on compression therapy and healing |
| Health Quality Ontario 39 | Focused on prevention rather than treatment |
| Nelson and Bell‐Syer 40 | Focused on prevention rather than treatment |
| Valle, Maruthur 41 | Relates to dressings rather than compression bandages |
| Nelson 42 | Repeating results of already included systematic review |
4.2. Review characteristics
Table 3 provides a summary of the included reviews' characteristics. Twelve systematic reviews met the inclusion criteria, 83% (N = 10) of which included meta‐analyses. 19 , 20 , 21 , 22 , 23 , 24 , 25 , 28 , 29 , 30 Publication dates ranged between 1997 and 2021. Review authors represented several countries, but most authors originated from the United Kingdom (N = 9, 75%). 20 , 22 , 23 , 25 , 26 , 27 , 28 , 29 , 30
TABLE 3.
Characteristics of included reviews
| Author | Types of studies in the SR | Sample, setting and population |
|---|---|---|
| De Carvalho, Peixoto 21 | 4LB vs SSBs | Seven RCTs undertaken in Europe, one in Asia, and one in North America. One thousand four hundred and thirty‐five patients: 657 (45.78%) male and 778 (54.48%) female, average age 70 (range 23‐97) years, with venous disease and had an ABI >0.9 mm Hg treated using 4LB and 726 using SSB. |
| Fletcher, Cullum 22 | Compression for healing of venous leg ulcers | Twenty‐four RCTs with six unpublished studies:
|
| Goka, Poku 23 | Multicomponent compression systems | Three multicentre RCTs Belgium, Canada, Germany, Italy, the Netherlands, United Kingdom, and United States, the United Kingdom. One thousand five hundred nine patients, Aged between 62.5 years to 76.9 years. Ulcer duration and measurements (5.8 months to 48.8 months and 7 cm2 to 11.8 cm2). |
| Mauck, Asi 24 | Compression stockings vs compression bandages, | Thirty‐eight eligible studies: 36 unique studies in 34 published articles:
|
| O'Meara, Cullum 19 | Compression bandage or compression stockings compared with no compression or an alternative type of compression | Forty‐eight RCTs reporting 59 comparisons (4321 participants in total). |
| Cullum, Nelson 28 | Compression bandaging or stocking | Twenty‐three RCTs
|
| O'Meara | Two types of compression for the treatment of VLU | Six trials (797 patients): Four trials conducted in the United Kingdom and two in mainland Europe. All trials were individually randomised and recruited participants with VLU
|
| Amsler, Willenberg 19 | Stocking based compression vs bandages | Eight trials. All studies were prospective and open‐label. Randomization was in two parallel groups except for one study which had a cross‐over design. Studies included a total of 692 patients, 277 men, and 359 women. The overall mean patient age was 60.7 years with a range per study between 56 and 65 years.
|
| Stather, Petty 26 | Velcro‐based wrap devices | Sixteen studies:
|
| Welsh 27 | Both elastic and inelastic components (mixed‐component systems MCSs). |
Eight publications: Four of the papers used ulcer healing as an outcome for the proposed efficacy |
| Palfreyman, Lochiel 25 | Compression therapies. | Eight trials involving 750 participants within the United States and United Kingdom. |
| Shi, Dumville 29 | Compression bandages or stockings vs no compression | Of the 14 included studies (all RCTs), 13 had a parallel‐group design, and one applied a cross‐over design. The median follow‐up duration was 12 weeks (range: 1 day to 12 months). Included a total of 1391 participants with venous leg ulcers (median study sample size: 51 participants; range: 11‐321). Across the eight studies that specified participant sex, 526 (50.1%) participants were male and 524 (49.9%) were female. The average participant age was specified in 11 studies, with a median of 70.1 years (range: 58.0‐76.5 years) |
Abbreviations: ABI, ankle brachial index; 4LB, four‐layer bandage; LBB, long stretch bandage; MCS, mixed‐component systems; RCT, randomized controlled trial; SR, systematic review; SSBs, short‐stretch bandages; VLU, venous leg ulcers.
Nine reviews 19 , 20 , 21 , 22 , 23 , 25 , 28 , 29 , 30 included only randomized controlled trials (RCTs), one review included RCTs and Cochrane reviews, 24 one review included RCTs, audit, and case series, 26 and one review included RCTs, cohort studies, case series, and qualitative studies. 27 The mean sample size across nine reviews was 93 (±92) and ranged from 15 232 patients 26 to 3785 20 patients across the reviews (see Table 3).
4.3. Type of CT
The type of CT varied between the reviews (see Supplementary document).
4.4. Primary outcome: Wound healing
4.4.1. Comparison 1: Compression vs no compression (10 trials; 768 participants)
Outcome: Wounds healed
Figure 2 presents the results for the meta‐analysis of studies comparing compression with no compression. The I 2 is 59%, indicating moderate heterogeneity among the studies; therefore, a fixed‐effects model was used for the meta‐analysis. A total of 61% (n = 236/385) of participants in the compression group healed, compared with 39% (n = 151/383) of participants in the no compression group (RR: 1.55; 95% CI 1.34‐1.78; P < .00001; moderate‐certainty evidence, downgraded twice for high risk of performance and detection bias) (Table 4).
FIGURE 2.
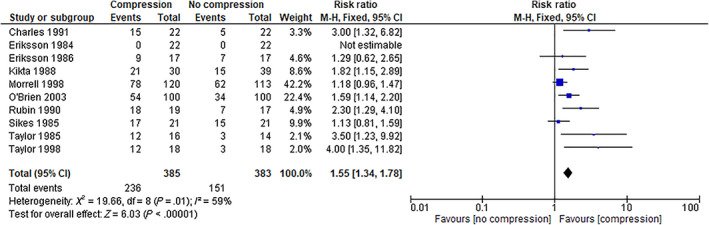
Forest plot: Compression vs no compression, outcome: Wound healed. CI, confidence interval
TABLE 4.
Included studies: Compression vs no compression
| Author | Comparison | Total participants | Number achieving healing | |
|---|---|---|---|---|
| Compression | No compression | |||
| Charles 43 | Short‐stretch bandage vs usual treatment | 44 | 15/22 | 5/22 |
| Eriksson 44 | Two‐layer bandage vs procine or aluminium foil dressing | 44 | 0/22 | 0/22 |
| Eriksson 45 | Compression vs no compression | 34 | 9/17 | 7/17 |
| Kikta, Schuler 46 | Unna's boot vs Duoderm hydrocolloid dressing | 69 | 21/30 | 15/39 |
| Morrell, King 47 | Compression vs usual treatment | 233 | 78/120 | 62/113 |
| O'Brien, Grace 48 | Four‐layer bandage vs no compression | 200 | 54/100 | 34/100 |
| Rubin, Alexander 49 | Unna's boot vs polyurethane foam dressing | 36 | 18/19 | 7/17 |
| Sikes 50 | Unna's boot vs dressings | 42 | 17/21 | 15/21 |
| Taylor 51 | Four‐layer bandage vs usual treatment | 30 | 12/16 | 3/14 |
| Taylor, Taylor 52 | Compression vs usual treatment | 36 | 12/18 | 3/18 |
| Total | 768 | 236/385 | 151/383 | |
4.4.2. Comparison 2: Elastic compression vs inelastic compression (33 trials; 3346 participants)
Outcome: Wounds healed
Figure 3 presents the results for the meta‐analysis of the studies comparing elastic compression with inelastic compression. The I 2 is 61%, indicating moderate heterogeneity among the studies; therefore, a fixed‐effects model was used for the meta‐analysis. A total of 54.3% (n = 959/1764) of participants in the compression group healed, compared with 54.9% (n = 870/1582) of participants in the no compression group (RR: 1.02; 95% CI: 0.96‐1.08; P < .61 moderate‐certainty evidence, downgraded twice for high risk of performance and detection bias). This indicates no statistically significant difference in healing rates between the two study groups, with moderate certainty (Table 5).
FIGURE 3.
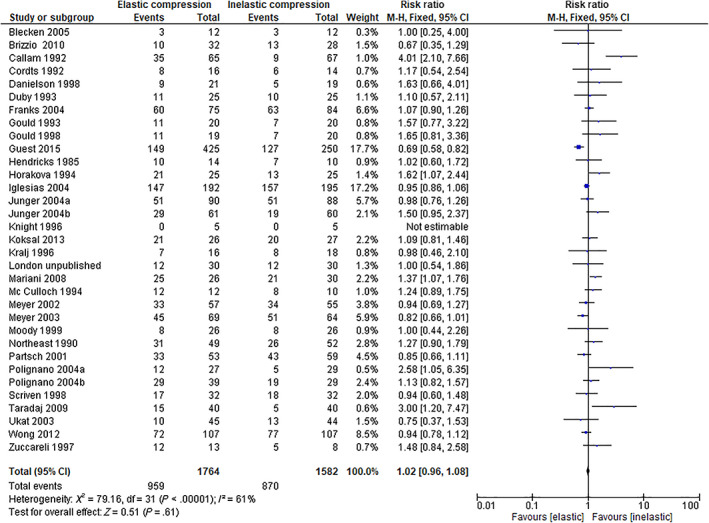
Forest plot: Elastic compression vs inelastic compression, outcome: Wound healed. CI, confidence interval
TABLE 5.
Studies comparing elastic compression with inelastic compression
| Author | Comparison | Total participants | Number achieving healing | |
|---|---|---|---|---|
| Elastic | Inelastic | |||
| Blecken, Villavicencio 53 | Four‐layer bandage vs compression boots | 24 | 3/12 | 3/12 |
| Brizzio, Amsler 54 | Compression stocking vs inelastic compression | 60 | 10/32 | 13/28 |
| Callam, Harper 55 | Three‐layer elastic compression vs three‐layer inelastic compression | 132 | 35/65 | 9/67 |
| Cordts, Hanrahan 56 | Duoderm plus compression vs inelastic compression | 30 | 8/16 | 6/14 |
| Danielsen, Madsen 57 | Four‐layer high compression vs inelastic compression | 40 | 9/21 | 5/19 |
| Duby 58 | Four‐layer high compression vs inelastic compression | 50 | 11/25 | 10/25 |
| Franks, Moody 59 | Four‐layer high compression vs inelastic compression | 159 | 60/75 | 63/84 |
| Gould 60 | Three‐layer elastic compression vs three‐layer inelastic compression | 40 | 11/20 | 7/20 |
| Gould, Campbell 61 | Three‐layer elastic compression vs three‐layer inelastic compression | 39 | 11/19 | 7/20 |
| Guest, Ayoub 62 | Four‐layer and two‐layer compression vs inelastic compression | 675 | 149/425 | 127/250 |
| Hendricks and Swallow 63 | Elastic support stocking vs inelastic compression | 24 | 10/14 | 7/10 |
| Horakova 64 | Elastic support stocking vs inelastic compression | 50 | 21/25 | 13/25 |
| Iglesias, Nelson 65 | Four‐layer compression vs inelastic compression | 387 | 147/192 | 157/195 |
| Jünger, Wollina 66 | Compression vs inelastic compression | 178 | 51/90 | 51/88 |
| Junger 67 | Compression stockings vs inelastic compression | 121 | 29/61 | 19/60 |
| Knight 68 | Elastic compression vs inelastic compression | 10 | 0/5 | 0/5 |
| Koksal and Bozkurt 69 | Hydrocolloid and compression vs inelastic compression | 51 | 21/26 | 20/27 |
| Kralj 70 | Multilayer compression vs inelastic compression | 34 | 7/16 | 8/18 |
| London et al Unpublished | Multilayer compression vs inelastic compression | 60 | 12/30 | 12/30 |
| Mariani 71 | Two‐stocking system vs inelastic compression | 56 | 25/26 | 21/30 |
| McCulloch, Marler 72 | Intermittent pneumatic compression vs inelastic compression | 22 | 12/12 | 8/10 |
| Meyer, Burnand 73 | Three‐layer elastic compression vs three‐layer inelastic compression | 112 | 33/57 | 34/55 |
| Meyer, McGuinness 74 | Four‐layer high compression vs inelastic compression | 133 | 45/69 | 51/64 |
| Moody 75 | Two‐layer elastic compression vs two‐layer inelastic compression | 52 | 8/26 | 8/26 |
| Northeast 76 | Multilayer elastic compression vs inelastic compression | 101 | 31/49 | 26/52 |
| Partsch, Damstra 77 | Multilayer elastic compression vs inelastic compression | 112 | 33/53 | 43/59 |
| Polignano, Bonadeo 78 | Compression stocking vs inelastic compression | 56 | 12/27 | 5/29 |
| Polignano, Guarnera 79 | Four‐layer high compression vs inelastic compression | 68 | 29/39 | 19/29 |
| Scriven, Taylor 80 | Multilayer elastic compression vs inelastic compression | 64 | 17/32 | 18/32 |
| Taradaj 81 | Compression stockings vs inelastic compression | 80 | 15/40 | 5/40 |
| Ukat, Konig 82 | Four‐layer high compression vs inelastic compression | 89 | 10/45 | 13/44 |
| Wong, Andriessen 83 | Four‐layer high compression vs inelastic compression | 214 | 72/107 | 77/107 |
| Zuccarelli 84 | Elastic compression vs inelastic compression | 21 | 12/13 | 5/8 |
| Total | 3346 | 959 | 870 | |
4.4.3. Comparison 3: Comparison four layers vs <4 layers bandage systems (eight trials; 971 participants)
Outcome: Wound healed
Figure 4 presents the results for the meta‐analysis of studies comparing four layers with <4 layer bandage systems. The I 2 is 74%, therefore a fixed‐effects model was used for the meta‐analysis. A total of 50% (n = 244/486) of participants in the four‐layer group healed, compared with 49% (n = 236/485) of participants in <4 layer group (RR: 1.07; 95% CI: 0.82‐1.40; P < .63; moderate‐certainty evidence, downgraded twice for high risk of performance and detection bias). This indicates no statistically significant difference in healing rates between the two study groups, with moderate certainty (Table 6a).
FIGURE 4.
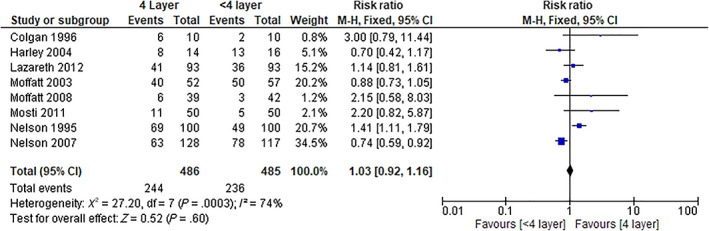
Forest plot: Comparison between four layers vs <4 layer bandage systems, outcome: Wounds healed. CI, confidence interval
TABLE 6a.
Studies comparing four layers vs <four layers bandage systems
| Author | Comparison | Total participants | Number achieving healing | |
|---|---|---|---|---|
| Intervention | Control | |||
| Colgan 85 | Four‐layer bandage vs single bandage | 20 | 6/10 | 2/10 |
| Harley 86 | Four‐layer bandage vs two layer | 30 | 13/16 | 8/14 |
| Lazareth, Moffatt 87 | Four‐layer bandage vs less than four‐layer bandage | 186 | 41/93 | 36/93 |
| Moffatt, McCullagh 88 | Four‐layer bandage vs two layer | 109 | 50/57 | 40/52 |
| Moffatt, Edwards 89 | Four‐layer bandage vs two layer | 81 | 3/42 | 6/39 |
| Mosti, Crespi 90 | Four‐layer bandage vs two layer | 100 | 5/50 | 11/50 |
| Nelson 91 | Four‐layer bandage vs single bandage | 200 | 69/100 | 49/100 |
| Nelson, Prescott 92 | Four‐layer bandage vs single layer | 245 | 78/117 | 63/128 |
| Total | 971 | 486 | 485 | |
4.4.4. Comparison 4: Comparison between different four‐layer bandage systems (two trials; 267 participants)
Outcome: Wound healed
Figure 5 presents the results for the meta‐analysis of studies comparing different four‐layer bandage systems. The I 2 is 8%, indicating there might not be important heterogeneity among the studies, therefore a fixed‐effects model was used for the meta‐analysis. A total of 74% (n = 99/134) of participants in system 1 healed, compared with 68% (n = 91/133) of participants in system 2 (RR: 1.08; 95% CI: 0.93‐1.25; P = .34; moderate‐certainty evidence, downgraded twice for high risk of performance and detection bias). This indicates no statistically significant difference in healing rates between the two study groups, with moderate certainty (Table 6b).
FIGURE 5.
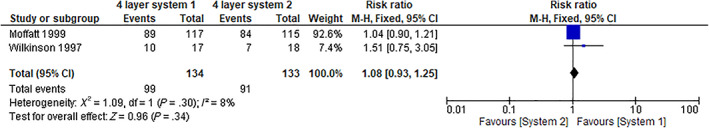
Forest plot: Comparison between different four‐layer bandage systems, outcome: Wounds healed. CI, confidence interval
TABLE 6b.
Studies comparing between different four‐layer bandage systems
4.4.5. Comparison 5: Comparison between different elastic compression bandage systems (two trials; 176 participants)
Outcome: Wound healed
Two trials 95 , 96 were not included in a meta‐analysis as they reported too dissimilar elastic compression bandages systems (see Tables 6c and 7). Milic, Zivic 95 compared a multilayer bandaging system with a heelless open‐toed elastic compression device knitted in tubular form and elastic bandages vs a multilayer bandaging system with elastic bandages only. The healing rate was 71% (n = 53/75) in the multilayer bandaging system and 33% (n = 25/75) in the multilayer bandaging system with elastic bandages only. Travers 96 compared three layers of elastic high compression vs a single bandage. None of the participants in either group healed.
TABLE 6c.
Studies comparing between different elastic compression bandage systems
| Author | Comparison | Total Participants | Number Achieving Healing | |
|---|---|---|---|---|
| Intervention | Control | |||
| Milic, Zivic 95 | Multilayer bandaging system with the Tubulcus (a heelless open‐toed elastic compression device knitted in tubular form) and elastic bandages vs control group (patients treated with a multilayer bandaging system with elastic bandages only) | 150 | 53/75 | 25/75 |
| Travers 96 | Three‐layer elastic high compression vs single bandage | 26 | 0/13 | 0/13 |
TABLE 7.
Studies comparing compression bandage with compression stocking
| Author | Comparison | Total participants | Numbers achieving healing | |
|---|---|---|---|---|
| Bandage | Stocking | |||
| Ashby, Gabe 97 | Four‐layer bandage vs stocking | 453 | 157/223 | 163/230 |
| Brizzio 98 | Compression bandage vs stocking | 35 | 8/14 | 19/21 |
| Brizzio, Amsler 54 | Short‐stretch bandage vs stocking | 60 | 13/28 | 10/32 |
| Dolibog, Franek 99 | Four‐layer bandage vs stocking | 48 | 2/25 | 5/23 |
| Finlayson, Courtney 100 | Four‐layer bandage vs stocking | 103 | 41/53 | 33/50 |
| Hendricks and Swallow 63 | Unna's boot vs stocking | 24 | 7/10 | 10/14 |
| Horakova 64 | Compression bandage vs stocking | 50 | 13/25 | 21/25 |
| Jünger, Wollina 66 | Compression bandage vs stocking | 178 | 51/88 | 51/90 |
| Jünger 2004c | Short‐stretch bandage vs stocking | 121 | 19/60 | 29/61 |
| Koksal and Bozkurt 69 | Unna's boot vs stocking | 51 | 20/27 | 21/26 |
| Milic, Zivic 11 | Bandage & stocking vs stocking alone | 131 | 63/89 | 13/42 |
| Polignano, Bonadeo 78 | Unna's boot vs stocking | 56 | 5/29 | 12/27 |
| Szewczyk, Jawień 101 | Two‐layer bandage vs stocking | 31 | 10/16 | 8/15 |
| Szewczk (2010b) | Four‐layer bandage vs stocking | 46 | 19/31 | 8/15 |
| Taradaj 81 | Short‐stretch bandage vs stocking | 80 | 5/40 | 15/40 |
| Total | 1575 | 467 | 464 | |
4.4.6. Comparison 6: Comparison: compression bandage vs compression stocking (15 trials; 1575 participants)
Outcome: Wounds healed
Figure 5 presents the results for the meta‐analysis of studies exploring compression bandage vs compression stocking. The I 2 is 67%, indicating moderate heterogeneity among the studies; therefore, a fixed‐effects model was used for the meta‐analysis. A total of 57% (n = 467/813) of participants in the compression bandage group healed, compared with 61% (n = 464/762) of participants in the compression stocking (RR 0.95; 95% CI 0.87‐1.03; P = .18; moderate‐certainty evidence, downgraded twice for high risk of performance and detection bias). This indicates no statistically significant difference in healing rates between the two study groups, with moderate certainty (Figure 6).
FIGURE 6.
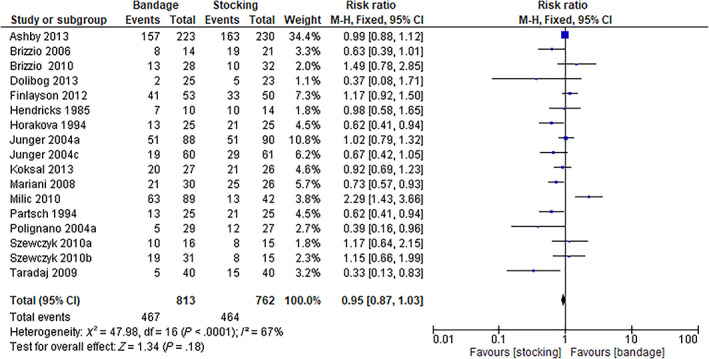
Comparison: Compression bandage vs compression stocking, outcome: Wound healed. CI, confidence interval
4.4.7. Comparison 7: Comparison between different types of inelastic compression systems (1 trial; 38 participants)
Outcome: Wound healed
One study compared different types of inelastic compression systems. In DePalma (1999), adjustable compression boots were compared with paste bandages. A total of 89% (n = 17/19) of participants in the Thera‐Boot group healed, compared with 58% (n = 11/19) of participants in the Unna boot group.
4.5. Secondary outcome: Adverse events
Device‐related adverse events reported mainly included pain and maceration with a low incidence rate. Data from two RCTs (Moffatt 2008, Vanscheidt 2012) showed no significant differences in the occurrence of one or more adverse events between two layers bandages and four layers bandages or two layers (Two layers vs four layers: 50% vs 50%; RR = 1.0; P = .903).
4.6. Quality appraisal
Table 8 shows the results of the quality appraisal. Three reviews were assessed as high quality, 20 , 24 , 29 five as moderate quality, 21 , 23 , 25 , 28 , 30 and four as low quality. 19 , 22 , 26 , 27
TABLE 8.
Quality assessment of the included reviews using the AMSTAR‐2 tool (n = 12)
| AMSTAR items | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Authors | Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | Q9 | Q10 | Q11 | Q12 | Q13 | Q14 | Q15 | Q16 | Rating |
| Amsler, Willenberg 19 | Y | Y | Y | PY | Y | Y | N | Y | N | N | Y | Y | Y | Y | N | Y | Low quality |
| Cullum, Nelson 28 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | N | Y | Moderate quality |
| De Carvalho, Peixoto 21 | Y | N | Y | PY | N | Y | PY | Y | Y | N | Y | Y | Y | Y | N | Y | Moderate quality |
| Goka, Poku 23 | Y | N | Y | Y | Y | Y | N | Y | Y | N | Y | Y | Y | N | N | Y | Moderate quality |
| Mauck, Asi 24 | Y | N | Y | PY | Y | Y | PY | Y | Y | Y | Y | Y | Y | Y | Y | Y | High quality |
| O'Meara, Cullum 20 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | High quality |
| O'meara, Tierney 30 | Y | Y | Y | Y | Y | N | PY | Y | Y | N | Y | Y | Y | Y | Y | Y | Moderate quality |
| Palfreyman, Lochiel 25 | Y | N | Y | PY | Y | Y | Y | Y | Y | N | Y | Y | Y | Y | N | N | Moderate quality |
| Stather, Petty 26 | Y | N | Y | PY | Y | Y | PY | Y | N | N | NMC | NMC | N | N | N | N | Low quality |
| Welsh 27 | Y | N | Y | PY | N | N | N | Y | Y | N | NMC | NMC | N | N | N | Y | Low quality |
| Fletcher, Cullum 22 | Y | N | Y | Y | Y | Y | N | Y | N | N | Y | N | Y | Y | N | Y | Low quality |
| Shi, Dumville 29 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | NMC | NMC | Y | Y | Y | Y | High quality |
| Percentage of reviews completely meeting each criterion | 100 | 42 | 100 | 50 | 83 | 79 | 33 | 100 | 75 | 33 | 75 | 67 | 83 | 75 | 33 | 83 | |
Note: Bold items are AMSTAR‐2 critical domains.
Abbreviations: N, no; NMC, no meta‐analysis conducted; PY, partial yes; Y, yes.
Of the 16 AMSTAR‐2 items, all included reviews expressed the research question in PICO format (Q1 = 100%), and identified the selection of the study designs for inclusion (Q3 = 100%). Only three studies 20 , 25 , 28 provided a list of excluded studies, justified the exclusions, and three reviews 20 , 24 , 28 , 29 reported on the sources of funding for the studies included in their review.
5. DISCUSSION
The aim of this meta‐review was to appraise and synthesise the evidence from existing systematic reviews to understand the impact that CT has on VLU healing. Twelve published systematic reviews were included, and the type of CT varied between the reviews. A number of comparisons are made in this meta‐review: Compression system vs no compression; elastic compression vs inelastic compression, four layers vs <four layers bandage systems; comparison between different four‐layer bandage systems; comparison between different elastic compression bandage systems; compression bandage vs compression stocking; and comparison between different types of inelastic compression systems. CT represents the gold standard for VLU management. The goal of any system is to deliver therapeutic compression during mobility and rest. 102 The key finding to emerge from the review is that there is moderate‐certainty evidence of the effect of compression bandages on the healing of VLU when compared with no compression. However, the identified reviews do not conclude which compression systems represent the most effective for healing VLU. In CT, the main indicators for elasticity/inelasticity are characterised by pressure and stiffness. 2 , 3 The fact that these parameters are almost never reported in the studies' results is our lack of complete knowledge of the elasticity/inelasticity of the compression bandages and its appropriate application. Correctly applied CT is essential in both the preventive and therapeutic care of VLUs. 9 , 24 Therefore, healthcare providers' knowledge of bandage materials and their practical ability have an important role in applying adequate pressure successfully. It is not clear in the included studies whether CT was applied by specific expert healthcare providers. It can therefore be assumed that all the studies that do not report pressure and stiffness have poor value. In this study, the only conclusion that can be made from the studies we have is that compression is better than no compression in achieving ulcer healing. No conclusion can be made regarding the superiority of elastic or inelastic material in increasing healing rate because of methodological flaws of the published studies. Rather than advocate one system, it seems more sensible to promote the correct use of any properly applied high CT device. Furthermore, it is essential to consider patient compliance. To facilitate effective CT, the clinician might select the ideal bandage, and obtain the necessary skills for correct application. A clinician might also consider concerns about patient compliance with CT to maximise the probability of wound healing.
In this meta‐review, the certainty of the body of evidence was assessed as per the GRADE approach. This approach helps define the extent to which one can be confident that an estimate of effect or association is close to the true quantity of specific interest. 103 Appropriate use of GRADE is important because reliable recommendations require reliable assessments of the certainty of the evidence and therefore require that all steps be carried out in a systematic and transparent manner. 104 The more serious the limitations within the individual studies, the more likely it is that the certainty of the evidence will be downgraded. In all cases, if a reason is found to downgrade the evidence, it should be classified as “serious” (downgrade by one level) or “very serious” (downgrade by two levels). Evidence from the primary outcome of this meta‐review was downgraded twice for the high risk of bias because of performance and detection bias. Because of poorly reporting of allocation concealment, blinding (both participants and personnel), and blinding of outcome assessment, evidence quality was downgraded. Lack of blinding can introduce bias, particularly when outcomes are subjective, and may lead to potential overestimation of the effect of the intervention, resulting in a bias in favour of the intervention. 105 However, blinding of participants and caregivers is difficult to achieve in wound care; nonetheless, blinding of outcome assessors is possible. For our primary outcome, this meta‐review showed that there was moderate‐certainty evidence of the effect of CT. The quality of evidence indicates moderate confidence in the effect estimate. This means that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it may be substantially different. 106
In terms of the AMSTAR‐2, the quality assessment varied across the systematic reviews. Most of the systematic reviews (N = 5, 42%) were of moderate quality and four reviews were of low quality. It is interesting to see that some of these systematic reviews were published in earlier years, meaning that a possible explanation for these results is that reviews were published before the AMSTAR‐2 quality assessment tool was conceived. Therefore, researchers did not have this quality guide available to them when writing their reviews. Another possible explanation is that systematic review methodology has advanced greatly in the past two decades, so it is not surprising that some of the older reviews did not score as highly as well as more recent ones. Furthermore, it is not unexpected that most of the high‐quality systematic reviews were Cochrane reviews. This is because Cochrane reviews are commonly suggested to be of a higher methodological quality. In the literature, it is suggested that for a critical assessment of the quality of non‐Cochrane reviews, users should first look at the database of abstracts of reviews of effectiveness. 107 , 108 Cochrane systematic reviews are recognised as high‐quality systematic reviews. Cochrane systematic reviews take a comprehensive, critical approach to the evidence for policy, practice, and research purposes, while at the same time, the rigour of its methods is widely acknowledged and updated periodically in the light of new evidence. 109 What is clear is that researchers need to consider all quality assessment criteria when they are conducting a systematic review.
6. CONCLUSION
This meta‐review sets out to determine the impact of CT on VLU healing by synthesising the data from existing systematic reviews. Twelve systematic reviews met the inclusion criteria. The type of CT varied between the reviews. We made seven comparisons and found that there is moderate‐certainty evidence that VLU probably heals when CT is used regardless of the type of compression system, providing it can achieve sustained graduated compression. Further meta‐reviews, which focus on challenges faced by health care professionals and patients when using CT, need to be undertaken.
CONFLICT OF INTEREST
The authors declare no conflicts of interest.
Supporting information
Appendix S1. Supporting information.
Patton D, Avsar P, Sayeh A, et al. A meta‐review of the impact of compression therapy on venous leg ulcer healing. Int Wound J. 2023;20(2):430‐447. doi: 10.1111/iwj.13891
DATA AVAILABILITY STATEMENT
Data sharing not applicable to this article as this study is a meta review.
REFERENCES
- 1. Valencia IC, Falabella A, Kirsner RS, et al. Chronic venous insufficiency and venous leg ulceration. J Am Acad Dermatol. 2001;44:401‐421. doi: 10.1067/mjd.2001.111633 [DOI] [PubMed] [Google Scholar]
- 2. Gloviczki P, Gloviczki ML. Evidence on efficacy of treatments of venous ulcers and on prevention of ulcer recurrence. Perspect Vasc Surg Endovasc Ther. 2009;21:259‐268. doi: 10.1177/1531003510373660 [DOI] [PubMed] [Google Scholar]
- 3. Simon DA, Dix FP, McCollum CN. Management of venous leg ulcers. BMJ. 2004;328:1358‐1362. doi: 10.1136/bmj.328.7452.1358 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Herber OR, Schnepp W, Rieger MA. A systematic review on the impact of leg ulceration on patients' quality of life. Health Qual Life Outcomes. 2007;5:44. doi: 10.1186/1477-7525-5-44 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Persoon A, Heinen MM, van der Vleuten CJ, et al. Leg ulcers: a review of their impact on daily life. J Clin Nurs. 2004;13:341‐354. doi: 10.1046/j.1365-2702.2003.00859.x [DOI] [PubMed] [Google Scholar]
- 6. Agale S. Chronic leg ulcers: epidemiology, aetiopathogenesis, and management. Ulcers. 2013;2013:413604. doi: 10.1155/2013/413604 [DOI] [Google Scholar]
- 7. Alavi A, Sibbald RG, Phillips TJ, et al. What's new: management of venous leg ulcers: treating venous leg ulcers. J Am Acad Dermatol. 2016;74:643‐664. doi: 10.1016/j.jaad.2015.03.059 [DOI] [PubMed] [Google Scholar]
- 8. Franks PJ, Barker J, Collier M, et al. Management of patients with venous leg Ulcers: challenges and current best practice. J Wound Care. 2016;25(suppl 6):S1‐s67. doi: 10.12968/jowc.2016.25.Sup6.S1 [DOI] [PubMed] [Google Scholar]
- 9. Andriessen A, Apelqvist J, Mosti G, et al. Compression therapy for venous leg ulcers: risk factors for adverse events and complications, contraindications ‐ a review of present guidelines. J Eur Acad Dermatol Venereol. 2017;31:1562‐1568. doi: 10.1111/jdv.14390 [DOI] [PubMed] [Google Scholar]
- 10. Nair B. Compression therapy for venous leg ulcers. Indian Dermatol Online J. 2014;5:378‐382. doi: 10.4103/2229-5178.137822 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Milic DJ, Zivic SS, Bogdanovic DC, et al. The influence of different sub‐bandage pressure values on venous leg ulcers healing when treated with compression therapy. J Vasc Surg. 2010;51:655‐661. doi: 10.1016/j.jvs.2009.10.042 [DOI] [PubMed] [Google Scholar]
- 12. Aromataris E, Fernandez R, Godfrey C, et al. Summarizing systematic reviews: methodological development, conduct and reporting of an umbrella review approach. Int J Evid Based Healthc. 2015;13:132‐140. doi: 10.1097/XEB.0000000000000055 [DOI] [PubMed] [Google Scholar]
- 13. Smith V, Devane D, Begley CM, Clarke M. Methodology in conducting a systematic review of systematic reviews of healthcare interventions. BMC Med Res Methodol. 2011;11:15. doi: 10.1186/1471-2288-11-15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Schardt C, Adams MB, Owens T, Keitz S, Fontelo P. Utilization of the PICO framework to improve searching PubMed for clinical questions. BMC Med Inform Decis Mak. 2007;7:16. doi: 10.1186/1472-6947-7-16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta‐analyses: the PRISMA statement. BMJ. 2009;339:b2535. doi: 10.1136/bmj.b2535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Shea B, Reeves B, Wells G, et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non‐randomised studies of healthcare interventions, or both. BMJ. 2017;358:j4008. doi: 10.1136/bmj.j4008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Higgins J, Green S. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. Chichester, UK: The Cochrane Collaboration; 2011. [Google Scholar]
- 18. Review Manager R . The Nordic Cochrane Centre, The Cochrane Collaboration. Version 5.3. ed. Copenhagen, Denmark: The Nordic Cochrane Centre: The Cochrane Collaboration, 2014. [Google Scholar]
- 19. Amsler F, Willenberg T, Blättler W. In search of optimal compression therapy for venous leg ulcers: a meta‐analysis of studies comparing diverse [corrected] bandages with specifically designed stockings. J Vasc Surg. 2009;50:668‐674. doi: 10.1016/j.jvs.2009.05.018 [DOI] [PubMed] [Google Scholar]
- 20. O'Meara S, Cullum N, Nelson EA, et al. Compression for venous leg ulcers. Cochrane Database Syst Rev. 2012;11:CD000265. doi: 10.1002/14651858.CD000265.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. De Carvalho MR, Peixoto BU, Silveira IA, et al. A meta‐analysis to compare four‐layer to short‐stretch compression bandaging for venous leg ulcer healing. Ostomy Wound Manage. 2018;64:30‐37. [PubMed] [Google Scholar]
- 22. Fletcher A, Cullum N, Sheldon TA. A systematic review of compression treatment for venous leg ulcers. BMJ. 1997;315:576‐580. doi: 10.1136/bmj.315.7108.576 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Goka EA, Poku E, Thokala P, et al. Clinical and economic impact of a two‐layer compression system for the treatment of venous leg ulcers: a systematic review. Wounds. 2020;32:11‐21. [PubMed] [Google Scholar]
- 24. Mauck KF, Asi N, Elraiyah TA, et al. Comparative systematic review and meta‐analysis of compression modalities for the promotion of venous ulcer healing and reducing ulcer recurrence. J Vasc Surg. 2014;60:71S‐90S.e71‐72. doi: 10.1016/j.jvs.2014.04.060 [DOI] [PubMed] [Google Scholar]
- 25. Palfreyman SJ, Lochiel R, Michaels JA. A systematic review of compression therapy for venous leg ulcers. Vasc Med. 1998;3:301‐313. doi: 10.1177/1358836x9800300406 [DOI] [PubMed] [Google Scholar]
- 26. Stather PW, Petty C, Howard AQ. Review of adjustable velcro wrap devices for venous ulceration. Int Wound J. 2019;16:903‐908. doi: 10.1111/iwj.13116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Welsh L. What is the existing evidence supporting the efficacy of compression bandage systems containing both elastic and inelastic components (mixed‐component systems)? A systematic review. J Clin Nurs. 2017;26:1189‐1203. doi: 10.1111/jocn.13611 [DOI] [PubMed] [Google Scholar]
- 28. Cullum N, Nelson EA, Fletcher AW, et al. Compression for venous leg ulcers. Cochrane Database Syst Rev. 2001;2:CD000265. doi: 10.1002/14651858.Cd000265 [DOI] [PubMed] [Google Scholar]
- 29. Shi C, Dumville JC, Cullum N, et al. Compression bandages or stockings versus no compression for treating venous leg ulcers. Cochrane Database Syst Rev. 2021;7:CD013397. doi: 10.1002/14651858.CD013397.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. O'meara S, Tierney J, Cullum N, et al. Four layer bandage compared with short stretch bandage for venous leg ulcers: systematic review and meta‐analysis of randomised controlled trials with data from individual patients. BMJ. 2009;338:b1344. doi: 10.1136/bmj.b1344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi: 10.1136/bmj.n71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Norman G, Westby MJ, Rithalia AD, et al. Dressings and topical agents for treating venous leg ulcers. Cochrane Database Syst Rev. 2018;6:CD012583. doi: 10.1002/14651858.CD012583.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Palfreyman SJ, Nelson EA, Lochiel R, et al. Dressings for healing venous leg ulcers. Cochrane Database Syst Rev. 2006;3:CD001103. doi: 10.1002/14651858.CD001103.pub2 [DOI] [PubMed] [Google Scholar]
- 34. Palfreyman S, Nelson EA, Michaels JA. Dressings for venous leg ulcers: systematic review and meta‐analysis. BMJ. 2007;335:244. doi: 10.1136/bmj.39248.634977.AE [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Bouza C, Muñoz A, Amate JM. Efficacy of modern dressings in the treatment of leg ulcers: a systematic review. Wound Repair Regen. 2005;13:218‐229. doi: 10.1111/j.1067-1927.2005.130302.x [DOI] [PubMed] [Google Scholar]
- 36. Turner‐Boutle M, Fletcher A, Sheldon T, et al. Compression therapy for venous ulcers: a systematic review. Nurs Times. 1997;93:52‐53. [PubMed] [Google Scholar]
- 37. de Carvalho MR. Comparison of outcomes in patients with venous leg ulcers treated with compression therapy alone versus combination of surgery and compression therapy: a systematic review. J Wound Ostomy Continence Nurs. 2015;42:42‐46. doi: 10.1097/won.0000000000000079 [DOI] [PubMed] [Google Scholar]
- 38. Jull A, Slark J, Parsons J. Prescribed exercise with compression vs compression alone in treating patients with venous leg ulcers: a systematic review and meta‐analysis. JAMA Dermatol. 2018;154:1304‐1311. doi: 10.1001/jamadermatol.2018.3281 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Health Quality Ontario HQO . Compression stockings for the prevention of venous leg ulcer recurrence: a health technology assessment. Ont Health Technol Assess Ser. 2019;19:1‐86. [PMC free article] [PubMed] [Google Scholar]
- 40. Nelson EA, Bell‐Syer SE. Compression for preventing recurrence of venous ulcers. Cochrane Database Syst Rev. 2014;4:CD002303. doi: 10.1002/14651858.CD002303.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Valle MF, Maruthur NM, Wilson LM, et al. Comparative effectiveness of advanced wound dressings for patients with chronic venous leg ulcers: a systematic review. Wound Repair Regen. 2014;22:193‐204. doi: 10.1111/wrr.12151 [DOI] [PubMed] [Google Scholar]
- 42. Nelson EA. Venous leg ulcers. BMJ Clin Evid. 2011;2011:1902. [PMC free article] [PubMed] [Google Scholar]
- 43. Charles H. Compression healing of ulcers. J Dist Nurs. 1991;10(3):4‐8. [Google Scholar]
- 44. Eriksson G, Eklund AE, Lidén S, Zetterquist S. Comparison of different treatments of venous leg ulcers: a controlled study using stereophoto grammetry. Curr Ther Res. 1984;35:678‐684. [Google Scholar]
- 45. Eriksson G. Comparison of two occlusive bandages in the treatment of venous leg ulcers. Br J Dermatol. 1986;114:227‐230. doi: 10.1111/j.1365-2133.1986.tb02801.x [DOI] [PubMed] [Google Scholar]
- 46. Kikta MJ, Schuler JJ, Meyer JP, et al. A prospective, randomized trial of Unna's boots versus hydroactive dressing in the treatment of venous stasis ulcers. J Vasc Surg. 1988;7:478‐483. [PubMed] [Google Scholar]
- 47. Morrell CJ, King B, Brereton L. Community‐based leg ulcer clinics: organisation and cost‐effectiveness. Nurs Times. 1998;94:51‐54. [PubMed] [Google Scholar]
- 48. O'Brien JF, Grace PA, Perry IJ, et al. Randomized clinical trial and economic analysis of four‐layer compression bandaging for venous ulcers. Br J Surg. 2003;90:794‐798. doi: 10.1002/bjs.4167 [DOI] [PubMed] [Google Scholar]
- 49. Rubin JR, Alexander J, Plecha EJ, et al. Unna's boot vs polyurethane foam dressings for the treatment of venous ulceration. A randomized prospective study. Arch Surg. 1990;125:489‐490. doi: 10.1001/archsurg.1990.01410160075016 [DOI] [PubMed] [Google Scholar]
- 50. Sikes E. Evaluation of a transparent dressing in the treatment of stasis ulcers of the lower limb. J Enterostomal Ther. 1985;12:116‐120. doi: 10.1097/00152192-198507000-00027 [DOI] [PubMed] [Google Scholar]
- 51. Taylor A. A prospective study to compare healing rates and associated treatment costs for current management of venous leg ulcers in the community and a four‐layer compression bandage regime. Paper presented at: Proceedings of the 4th European Conference on Advances in Wound Management; Macmillan Magazines, London; 1995:199‐200.
- 52. Taylor AD, Taylor RJ, Marcuson RW. Prospective comparison of healing rates and therapy costs for conventional and four‐layer high‐compression bandaging treatments of venous leg ulcers. Phlebology. 1998;13:20‐24. doi: 10.1177/026835559801300105 [DOI] [Google Scholar]
- 53. Blecken SR, Villavicencio JL, Kao TC. Comparison of elastic versus nonelastic compression in bilateral venous ulcers: a randomized trial. J Vasc Surg. 2005;42:1150‐1155. doi: 10.1016/j.jvs.2005.08.015 [DOI] [PubMed] [Google Scholar]
- 54. Brizzio E, Amsler F, Lun B, et al. Comparison of low‐strength compression stockings with bandages for the treatment of recalcitrant venous ulcers. J Vasc Surg. 2010;51:410‐416. doi: 10.1016/j.jvs.2009.08.048 [DOI] [PubMed] [Google Scholar]
- 55. Callam MJ, Harper DR, Dale JJ, et al. Lothian and Forth Valley leg ulcer healing trial, part 1: elastic versus non‐elastic bandaging in the treatment of chronic leg ulceration. Phlebology. 1992;7:136‐141. doi: 10.1177/026835559200700402 [DOI] [Google Scholar]
- 56. Cordts PR, Hanrahan LM, Rodriguez AA, et al. A prospective, randomized trial of Unna's boot versus Duoderm CGF hydroactive dressing plus compression in the management of venous leg ulcers. J Vasc Surg. 1992;15:480‐486. [PubMed] [Google Scholar]
- 57. Danielsen L, Madsen SM, Henriksen L. Venous leg ulcer healing: a randomized prospective study of long‐stretch versus short‐stretch compression bandages. Phlebology. 1998;13:59‐63. doi: 10.1177/026835559801300206 [DOI] [PubMed] [Google Scholar]
- 58. Duby T, Hoffman D, Cameron J, Doblhoff‐Brown D, Cherry G, Ryan T. A randomized trial in the treatment of venous leg ulcerscomparing short stretch bandages, 4 layer bandage system, and a long stretch paste bandage system. Wounds. 1993;5:276‐279. [Google Scholar]
- 59. Franks PJ, Moody M, Moffatt CJ, et al. Randomized trial of cohesive short‐stretch versus four‐layer bandaging in the management of venous ulceration. Wound Repair Regen. 2004;12:157‐162. doi: 10.1111/j.1067-1927.2004.012206.x [DOI] [PubMed] [Google Scholar]
- 60. Gould D, Campbell S, Harding EF. Short stretch vs. long stretch bandages in the management of chronic venous leg ulcers. Phlebology. 1993;8:43. [Google Scholar]
- 61. Gould DJ, Campbell S, Newton H, et al. Setopress vs elastocrepe in chronic venous ulceration. Br J Nurs. 1998;7:66‐70, 72‐63. doi: 10.12968/bjon.1998.7.2.66 [DOI] [PubMed] [Google Scholar]
- 62. Guest J, Ayoub N, McIlwraith T, et al. Health economic burden that wounds impose on the National Health Service in the UK. BMJ Open. 2015;5:e009283. doi: 10.1136/bmjopen-2015-009283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Hendricks WM, Swallow RT. Management of stasis leg ulcers with Unna's boots versus elastic support stockings. J Am Acad Dermatol. 1985;12:90‐98. doi: 10.1016/s0190-9622(85)70015-1 [DOI] [PubMed] [Google Scholar]
- 64. Horakova M, Partsch H. Venous leg ulcers: are compression bandages indicated? Phlebologie. 1994;47:53‐57. [Google Scholar]
- 65. Iglesias C, Nelson EA, Cullum NA, et al. VenUS I: a randomised controlled trial of two types of bandage for treating venous leg ulcers. Health Technol Assess. 2004;8:iii, 1‐105. doi: 10.3310/hta8290 [DOI] [PubMed] [Google Scholar]
- 66. Jünger M, Wollina U, Kohnen R, Rabe E. Efficacy and tolerability of an ulcer compression stocking for therapy of chronic venous ulcer compared with a below‐knee compression bandage: results from a prospective, randomized, multicentre trial. Curr Med Res Opin. 2004;20:1613‐1623. doi: 10.1185/030079904x4086 [DOI] [PubMed] [Google Scholar]
- 67. Junger M, Partsch H, Ramelet AA, Zuccarelli F. Efficacy of a ready‐made tubular compression device versus short‐stretch compression bandages in the treatment of venous leg ulcers. Wounds. 2004;16:313‐320. [Google Scholar]
- 68. Knight C, McCulloch J. A comparative study between two compression systems in the treatment of venous insufficiency in leg ulcers. Paper presented at: 9th Annual Symposium on Advanced Wound Care and 6th Annual Medical Research Forum on Wound Repair; Wayne, Pennsylvania; 1996; April 20‐24; Atlanta.
- 69. Koksal C, Bozkurt AK. Combination of hydrocolloid dressing and medical compression stockings versus Unna's boot for the treatment of venous leg ulcers. Swiss Med Wkly. 2003;133:364‐368. [DOI] [PubMed] [Google Scholar]
- 70. Kralj B, Kosicek M. 60. Randomised comparative trial of single‐layer andmulti‐layer bandages in the treatment of venous leg ulcer. Paper presented at: Proceedingsof the 6th European Conference on Advances in Wound Management; 1996:158‐160.
- 71. Mariani F, Mattaliano V, Mosti G, et al. The treatment of venous leg ulcers with a specifically designed compression stocking kit. Phlebologie. 2008;37:191‐197. [Google Scholar]
- 72. McCulloch JM, Marler KC, Neal MB, et al. Intermittent pneumatic compression improves venous ulcer healing. Adv Wound Care. 1994;7:22‐24. [PubMed] [Google Scholar]
- 73. Meyer FJ, Burnand KG, Lagattolla NR, et al. Randomized clinical trial comparing the efficacy of two bandaging regimens in the treatment of venous leg ulcers. Br J Surg. 2002;89:40‐44. doi: 10.1046/j.0007-1323.2001.01936.x [DOI] [PubMed] [Google Scholar]
- 74. Meyer FJ, McGuinness CL, Lagattolla NR, et al. Randomized clinical trial of three‐layer paste and four‐layer bandages for venous leg ulcers. Br J Surg. 2003;90:934‐940. doi: 10.1002/bjs.4173 [DOI] [PubMed] [Google Scholar]
- 75. Moody M. Comparison of Rosidal K and SurePress in the treatment of venous leg ulcers. Br J Nurs. 1999;8:345‐355. doi: 10.12968/bjon.1999.8.6.6660 [DOI] [PubMed] [Google Scholar]
- 76. Northeast A, Layer GT, Wilson NM, Browse NL, Burnand KG. Increased Compression Expedites Venous Ulcer Healing. London, UK: Royal Society of Medicine Venous Forum; 1990. [Google Scholar]
- 77. Partsch H, Damstra RJ, Tazelaar DJ, et al. Multicentre, randomised controlled trial of four‐layer bandaging versus short‐stretch bandaging in the treatment of venous leg ulcers. Vasa. 2001;30:108‐113. doi: 10.1024/0301-1526.30.2.108 [DOI] [PubMed] [Google Scholar]
- 78. Polignano R, Bonadeo P, Gasbarro S, et al. A randomised controlled study of four‐layer compression versus Unna's Boot for venous ulcers. J Wound Care. 2004;13:21‐24. doi: 10.12968/jowc.2004.13.1.26563 [DOI] [PubMed] [Google Scholar]
- 79. Polignano R, Guarnera G, Bonadeo P. Evaluation of SurePress Comfort: a new compression system for the management of venous leg ulcers. J Wound Care. 2004;13:387‐391. doi: 10.12968/jowc.2004.13.9.26703 [DOI] [PubMed] [Google Scholar]
- 80. Scriven JM, Taylor LE, Wood AJ, Bell PR, Naylor AR, London NJ. A prospective randomised trial of four‐layer versus short stretch compression bandages for the treatment of venous leg ulcers. Ann R Coll Surg Engl. 1998;80:215‐220. [PMC free article] [PubMed] [Google Scholar]
- 81. Taradaj J, Franek A, Brzezinska‐Wcislo L, Blaszczak E, Polak A. Randomized trial of medical compression stockings versus two‐layer short‐stretch bandaging in the management of venous leg ulcers. Phlebologie. 2009;38:157‐163. [Google Scholar]
- 82. Ukat A, Konig M, Vanscheidt W, et al. Short‐stretch versus multilayer compression for venous leg ulcers: a comparison of healing rates. J Wound Care. 2003;12:139‐143. doi: 10.12968/jowc.2003.12.4.26490 [DOI] [PubMed] [Google Scholar]
- 83. Wong IK, Andriessen A, Charles HE, et al. Randomized controlled trial comparing treatment outcome of two compression bandaging systems and standard care without compression in patients with venous leg ulcers. J Eur Acad Dermatol Venereol. 2012;26:102‐110. doi: 10.1111/j.1468-3083.2011.04327.x [DOI] [PubMed] [Google Scholar]
- 84. Zuccarelli F, Allaert FA. Effectivity of support in the treatment of leg ulcers. A comparative multicentre study of elastic bandage (BIFLEX®) versus extensive bandage [Efficacité de la contention dans le traitement des ulcères de jambe. Etude multicentrique comparant une bande élastique (BIFLEX®) et une bande extensible]. Angeiologie. 1997;49:15‐18. [Google Scholar]
- 85. Colgan M, Teevan M, McBride C, O'Sullivan L, Moore D, Shanik G. Costcomparisons in the management of venous ulceration. In: Cherry GW, Gottrup F, Lawrence JC, Moffatt CJ, Turner TD, ed. Paper presented at: Proceedings of 5th European Conference on Advances in Wound Management, November 21‐24, 1995; Macmillan Magazines, Ltd, London; 1996:10.
- 86. Harley J, Harcourt D, Hutchinson B, McLean M, Long M. A comparative trial of long stretch compression bandaging versus multi‐layer compression bandaging in the treatment of chronic venous ulcers. Prim Int. 2004;12:6‐13. [Google Scholar]
- 87. Lazareth I, Moffatt C, Dissemond J, et al. Efficacy of two compression systems in the management of VLUs: results of a European RCT. J Wound Care. 2012;21:553‐554, 556, 558 passim. doi: 10.12968/jowc.2012.21.11.553 [DOI] [PubMed] [Google Scholar]
- 88. Moffatt CJ, McCullagh L, O'Connor T, et al. Randomized trial of four‐layer and two‐layer bandage systems in the management of chronic venous ulceration. Wound Repair Regen. 2003;11:166‐171. doi: 10.1046/j.1524-475x.2003.11303.x [DOI] [PubMed] [Google Scholar]
- 89. Moffatt CJ, Edwards L, Collier M, et al. A randomised controlled 8‐week crossover clinical evaluation of the 3M Coban 2 Layer Compression System versus Profore to evaluate the product performance in patients with venous leg ulcers. Int Wound J. 2008;5:267‐279. doi: 10.1111/j.1742-481X.2008.00487.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Mosti G, Crespi A, Mattaliano V. Comparison between a new, two‐component compression system with zinc paste bandages for leg ulcer healing: a prospective, multicenter, randomized, controlled trial monitoring sub‐bandage pressures. Wounds. 2011;23:126‐134. [PubMed] [Google Scholar]
- 91. Nelson E, Harper DR, Ruckley CV, Prescott RJ, Gibson B, Dale JJ. A randomised trial of single layer and multi‐layer bandages in the treatment of chronic venous ulceration. Phlebology. 1995;2(suppl 1):915‐916. [Google Scholar]
- 92. Nelson EA, Prescott RJ, Harper DR, et al. A factorial, randomized trial of pentoxifylline or placebo, four‐layer or single‐layer compression, and knitted viscose or hydrocolloid dressings for venous ulcers. J Vasc Surg. 2007;45:134‐141. doi: 10.1016/j.jvs.2006.09.043 [DOI] [PubMed] [Google Scholar]
- 93. Moffatt C, Simon DA, Franks PJ, et al. Randomised trial comparing two 4LB systems in the management of chronic leg ulceration. Phlebology. 1999;14:139‐142. [Google Scholar]
- 94. Wilkinson E, Buttfield S, Cooper S, et al. Trial of two bandaging systems for chronic venous leg ulcers. J Wound Care. 1997;6:339‐340. [DOI] [PubMed] [Google Scholar]
- 95. Milic DJ, Zivic SS, Bogdanovic DC, et al. A randomized trial of the Tubulcus multilayer bandaging system in the treatment of extensive venous ulcers. J Vasc Surg. 2007;46:750‐755. doi: 10.1016/j.jvs.2007.04.062 [DOI] [PubMed] [Google Scholar]
- 96. Travers J, Dalziel KL, Makin GS. Assessment of a new onelayer adhesive bandaging method in maintaining prolonged limb compression and effects on venous ulcer healing. Phlebology. 1992;7:59‐63. [Google Scholar]
- 97. Ashby RL, Gabe R, Ali S, et al. Clinical and cost‐effectiveness of compression hosiery versus compression bandages in treatment of venous leg ulcers (Venous leg Ulcer Study IV, VenUS IV): a randomised controlled trial. Lancet. 2013;383:871‐879. doi: 10.1016/s0140-6736(13)62368-5 [DOI] [PubMed] [Google Scholar]
- 98. Brizzio E, Blättler W, Rossi G, et al. Healing venous ulcers with different modalities of leg compression. Unexpected findings of a pilot study. Phlebologie. 2006;35:249‐255. [Google Scholar]
- 99. Dolibog P, Franek A, Taradaj J, et al. A randomized, controlled clinical pilot study comparing three types of compression therapy to treat venous leg ulcers in patients with superficial and/or segmental deep venous reflux. Ostomy Wound Manage. 2013;59:22‐30. [PubMed] [Google Scholar]
- 100. Finlayson KJ, Courtney MD, Gibb MA, et al. The effectiveness of a four‐layer compression bandage system in comparison with class 3 compression hosiery on healing and quality of life in patients with venous leg ulcers: a randomised controlled trial. Int Wound J. 2012;11:21‐27. doi: 10.1111/j.1742-481X.2012.01033.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. Szewczyk MT, Jawień A, Cierzniakowska K, et al. Comparison of the effectiveness of compression stockings and layer compression systems in venous ulceration treatment. Arch Med Sci. 2010;6:793‐799. doi: 10.5114/aoms.2010.17097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. Woo KY, Alavi A, Evans R, et al. New advances in compression therapy for venous leg ulcers. Surg Technol Int. 2013;23:61‐68. [PubMed] [Google Scholar]
- 103. Guyatt G, Oxman AD, Akl EA, et al. GRADE guidelines: 1. Introduction‐GRADE evidence profiles and summary of findings tables. J Clin Epidemiol. 2011;64:383‐394. doi: 10.1016/j.jclinepi.2010.04.026 [DOI] [PubMed] [Google Scholar]
- 104. Granholm A, Alhazzani W, Møller MH. Use of the GRADE approach in systematic reviews and guidelines. Br J Anaesth. 2019;123:554‐559. doi: 10.1016/j.bja.2019.08.015 [DOI] [PubMed] [Google Scholar]
- 105. Day SJ, Altman DG. Statistics notes: blinding in clinical trials and other studies. BMJ. 2000;321:504. doi: 10.1136/bmj.321.7259.504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106. Schunemann H, Guyatt G, Oxman A, eds. GRADE Handbook for Grading Quality of Evidence and Strength of Recommendations. Canada: The GRADE Working Group; 2013. [Google Scholar]
- 107. Petticrew M, Wilson P, Wright K, Song F. Quality of Cochrane reviews. Quality of Cochrane reviews is better than that of non‐Cochrane reviews. BMJ. 2002;324:545. doi: 10.1136/bmj.324.7336.545/a [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108. Goldkuhle M, Narayan V, Weigl A, et al. A systematic assessment of Cochrane reviews and systematic reviews published in high‐impact medical journals related to cancer. BMJ Open. 2018;8:e020869. doi: 10.1136/bmjopen-2017-020869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109. Bunn F, Trivedi D, Alderson P, et al. The impact of Cochrane Reviews: a mixed‐methods evaluation of outputs from Cochrane Review Groups supported by the National Institute for Health Research. Health Technol Assess. 2015;19:1‐99, v‐vi. doi: 10.3310/hta19280 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1. Supporting information.
Data Availability Statement
Data sharing not applicable to this article as this study is a meta review.


