Abstract
Objective:
This prospective, randomized study aimed to compare anterior suprascapular nerve block versus interscalene block in terms of diaphragm paralysis in arthroscopic shoulder surgery.
Methods:
Fifty-two patients undergoing shoulder arthroscopy surgery were prospectively randomly assigned to interscalene block (n = 25) or anterior suprascapular nerve block groups (n = 27) (each group receiving 5 mL, 0.5% bupivacaine). The ipsilateral diaphragmatic excursion was assessed in all patients using ultrasound imaging before (baseline), 30 minutes, and 24 hours after block completion. Pain scores were recorded 1 hour preoperative, 30-60 minutes in the postoperative recovery unit, and at 6 and 24 hours postoperatively.
Results:
No complete paralysis was observed in either treatment group. The incidence of a partial decrease in diaphragm movements was significantly lower in the anterior suprascapular nerve block than in the interscalene block group (1 vs. 21 patients) (P < .01). Twenty-six patients in the anterior suprascapular nerve block and 4 in the interscalene block group had less than a 25% decrease in hemidiaphragmatic movements, 30 minutes after the blockade. Pain scores were similar in the 2 groups. However, mean pain scores at 24 hours postoperatively were significantly higher in the interscalene block than in the anterior suprascapular nerve block group (P < .05). Time to first pain post-block was significantly longer in the anterior suprascapular nerve block compared to the interscalene block group (677.04 ± 52.17 minutes vs. 479.2 ± 99.74 minutes, P < .05).
Conclusion:
Anterior suprascapular nerve block and interscalene block both appear to be clinically effective in providing postoperative analgesia for patients undergoing arthroscopic shoulder surgery under general anesthesia. However, the time to first pain is significantly longer with anterior suprascapular nerve block. Pain scores at 24 hours postoperatively were significantly lower in the anterior suprascapular nerve block compared to the interscalene block group. Diaphragmatic movements after anterior suprascapular nerve block were also better preserved at both 30 minutes after the block and 24 hours after surgery.
Level of Evidence:
Level I, Therapeutic Study
Keywords: Brachial plexus block, Postoperative pain, Respiratory paralysis, Shoulder joint-surgery
HIGHLIGHTS
Hemidiaphragmatic paralysis (HDP) is a challenging condition after the interscalene brachial plexus block, especially for respiratory compromised patients. This study aimed to compare the interscalene brachial plexus block (ISB) and anterior suprascapular nerve block (ASSB) in terms of diaphragm paralysis in shoulder arthroscopy.
The results show that the ASSB, even with a low volume of local anesthetic drug, seems to be effective in providing postoperative analgesia for patients undergoing arthroscopic shoulder surgery with less HDP.
The results from this study indicate that ASSB is an effective and safe alternative to ISB for arthroscopic shoulder surgery.
Introduction
The interscalene brachial plexus block (ISB) remains the gold standard for analgesia after shoulder surgery.1 Prior to the more common use of ultrasound (US), diaphragmatic paresis appeared to be an inevitable consequence of the ISB.2 Symptomatic dyspnea from hemidiaphragmatic paralysis (HDP) is a challenging condition, especially for respiratory-compromised patients. Dosage studies have shown that as little as 5 mL of local anesthetic (LA) may be sufficient for successful ISB.3,4 Another method of avoiding HDP is by increasing the distance between the LA and the phrenic nerve. Different block approaches that provide similarly efficient postoperative analgesia to that of ISB without causing HDP have been tested.5
The anterior suprascapular nerve block (ASSB) seems to be clinically promising in the context of arthroscopic shoulder surgeries, with no proven inferiority to ISB.6 Diaphragmatic and pulmonary functions seem to be well preserved with ASSB, although this still needs to be confirmed. Cadaver studies have demonstrated a 21% rate of phrenic nerve involvement with ASSB but failed to demonstrate a statistically significant difference and recommended that clinical trials be performed.7
In addition to effective pain relief of the blocks in the early postoperative period, peripheral nerve catheter techniques are used to prolong analgesia. While initial injection technique could initially spare phrenic nerve, because of the LA accumulation, HDP may occur with time.8 The method that will not affect the phrenic nerve at all and at the same time provide an effective analgesia is still under investigation.
The aim of the present study was to compare the ISB and ASSB in terms of diaphragm paralysis in shoulder arthroscopy operations.
Materials and Methods
This study was approved by the Koç University Committee on Human Research Ethics Committee (2020.010.IRB1.001), registered at clinicaltrials.gov (NCT04626869), and conducted from December 2020 to April 2021. The procedures were conducted in accordance with the Helsinki Declaration 2013. Fifty-four patients aged 18-70, patients with physical status I-III according to American Society of Anesthesiologists (ASA) and undergoing elective arthroscopic shoulder surgery under general anesthesia were included in the study. Exclusion criteria were body mass index (BMI) > 35 kg/m2 or the presence of pre-existing (obstructive or restrictive) pulmonary disease, pregnancy, allergy to LA, chronic pain condition requiring the use of opioids at home, or infection at the injection site. Written informed consent was obtained from all participants.
Patients were randomly divided into 2 groups using a computer-generated sequence of random numbers.
General anesthesia
Following standard monitoring (electrocardiogram (ECG), pulse oximetry, and Non-invasive blood pressure (NIBP)), general anesthesia was induced using intravenous (IV) propofol (1-3 mg/kg) and fentanyl (1 mcg/kg). Tracheal intubation was performed following IV rocuronium administration (0.6 mg/kg). Anesthesia was maintained with desflurane in an air–oxygen mixture. A continuous infusion of remifentanil (0.05 to 0.2 μg/kg/min) was used as required to maintain heart rate and mean blood pressure within 20% of pre-induction values. Anesthesia depth was monitored using a bispectral index (BIS) monitor, the desflurane level being adjusted to provide BIS values between 40 and 60. Invasive monitoring was performed through the radial artery cannula for blood pressure monitoring. Four milligrams of dexamethasone and 50 mg ranitidine were administered IV to all patients, who also received 800 mg ibuprofen and 1 g paracetamol IV as part of multimodal analgesia. Ondansetron 4 mg IV was administered to prevent postoperative nausea and vomiting. All patients were operated by the same surgeon.
Postoperative pain was measured using a numerical rating scale (NRS), on which current pain is indicated as 0 points for no pain and 10 points for the worst imaginable pain. Preoperative pain scores were also recorded. Pain scores were recorded on 1 hour preoperative, after 30 and 60 minutes at the postoperative recovery unit, and at 6 and 24 hours postoperatively on the ward. Times to the first analgesic requirement after surgery were also recorded.
Nerve block procedure
All patients were sedated with IV midazolam (1-2 mg) following standard ASA monitoring and oxygen administration by nasal cannula during nerve blocks.
Patients in the ASSB group were placed in a semi-sitting position with their heads facing the contralateral side. A pre-scan was performed with a linear US probe (GE Loqic P9 7-15 MHz, Korea). The US probe was placed over the suprascapular region in a coronal oblique manner. The suprascapular nerve immediately beneath the omohyoid muscle belly was identified. The suprascapular nerve block was performed using an in-plane approach with a needle through the catheter (Contiplex C, B. Braun, Melsungen, Germany) and injection of 5 mL of 0.5% bupivacaine (Figure 1A).
Figure 1.

A-B. (A) Sonogram of the suprascapular area. (B) Sonogram of the interscalene area. The needle approach is from the lateral aspect through the middle scalene muscle. ASM, anterior scalene muscle; ASSN, anterior suprascapular nerve; BP, brachial plexus; IJV, internal jugular vein; MSM, middle scalene muscle; OM, omohyoid muscle; SA, subclavian artery; SCM, sternocleidomastoid muscle.
The patients in the ISB group were placed in a semi-sitting position with their heads facing the contralateral side. A pre-scan was performed with a linear US probe (GE Loqic P9 7-15 MHz). The block was performed using an in-plane approach. The block needle (Contiplex C, B. Braun) was advanced in a lateral-to-medial direction. Bupivacaine 5 mL was injected once the needle tip was in close proximity to the brachial plexus at the level of C5 and C6 nerve roots (Figure 1B).
The catheter system used involved a needle inserted through the catheter. The tip of the catheter was located at the site of the LA injection adjacent to the nerve structures, at the level of the C5 and C6 nerve roots in the ISB group and next to the suprascapular nerve in the ASSB group. Following both blocks, the catheters were covered in the same way using padded film dressings. In order to eliminate performance bias, all blocks were performed by the same experienced regional anesthesiologist. Diaphragm functions were evaluated by another anesthesiologist. The anesthesiologist who evaluated diaphragm functions and the pain nurses who recorded NRS scores in the postoperative period were blinded to the regional anesthesia technique employed.
Evaluation of diaphragm movement and respiratory function
Ipsilateral diaphragmatic excursion was assessed in all patients using US imaging before (baseline) and 30 minutes after block completion by a single anesthesiologist experienced in evaluating diaphragmatic motion using M-mode.9 Diaphragmatic movement was evaluated at the subcostal border with patients in a semi-sitting position. M-mode ultrasonography (GE Loqic P9) and a 2-5 MHz convex transducer were used. The US probe was placed between the mid-clavicular line and the anterior axillary line by directing it vertically and slightly cranially. The liver and spleen acted as an acoustic window. Diaphragm movement was measured in centimeters during quiet and deep breathing. The decrease in diaphragm motion was calculated as the percentage difference in diaphragm motion measured before and 30 minutes after the block. Each test was performed in triplicate, and the mean values were recorded. The severity of hemidiaphragmatic paresis was measured by the decrease in diaphragmatic excursion (calculated as a percentage difference) between baseline and 30 minutes after block completion. The values were classified as the complete, partial, or absence of hemidiaphragmatic paresis. A decrease in diaphragm movement between 75% and 100% was defined as complete paresis, a decrease between 25% and 75% as partial paresis, and a decrease less than 25% as no paresis.10 In order to investigate the effect of continuous LA drug administration on diaphragm movement via nerve catheter, the same procedure was repeated 24 hours after surgery.
Postoperative recovery unit monitoring
All patients’ pain scores were recorded on arrival at the postoperative recovery unit and after 30 and 60 minutes by pain nurses blinded to the group allocations. Patients with NRS scores of 4-6 received 25 mcg fentanyl IV, and those with scores of >6 received 50 mcg fentanyl IV. Total fentanyl doses administered in the postoperative recovery unit and side effects such as breathing difficulties were recorded. Patient-controlled analgesia (PCA) with LA delivered by the nerve catheter was initiated in the recovery room. The PCA device was programmed to deliver a continuous infusion of 4 mL of 0.2% bupivacaine and a bolus dose of 6 mL on demand with a 20-minute lock-out time.
Surgical ward follow-up
The same multimodal analgesia regimen was applied to all patients in the form of IV paracetamol 3 × 1 g, ibuprofen 2 × 400 mg and oral pregabalin 1 × 75 mg. In the case of patients with NRS of 4 or above, 1 mg/kg IV tramadol was planned as a rescue analgesic. Potential side effects that may develop due to the brachial plexus block (Horner’s syndrome, hoarseness, difficulty swallowing, and shortness of breathing) were also recorded.
Sample size calculation
Based on a pilot study performed with 10 patients per group, the difference between change percentages was 12% (with standard deviations of 20 and 20). Assuming a type I error (α) of 0.05 and power (1 − β) of 80%, the sample size for each group was calculated at a minimum of 24 members per group. To increase the power of the study and compensate for patient dropouts during surgery, we included 27 patients per group. Sample size calculation was performed using MedCalc Statistical Software version 19.1 (MedCalc Software bv, Ostend, Belgium; https://www.medcalc.org; 2019).
Statistical analysis
Statistical analysis was performed on IBM Statistical Package for the Social Sciences Statistics for Windows, Version 26.0 software (IBM Corp., Armonk, NY, USA). The normality of the distribution of continuous variables was investigated using the Shapiro–Wilk test. Descriptive statistics are presented as mean plus standard deviation for normally distributed variables and median (minimum-maximum) for non-normally distributed variables. Non-parametric statistical methods were employed for values with skewed distribution. The Mann–Whitney U-test was used to compare 2 non-normally distributed groups. The χ 2 test was applied for categorical variables, and the results were expressed as observation counts (and percentages). Two-sided P values lower than .05 were regarded as significant.
Results
Fifty-four patients were randomly assigned to 1 or other of the 2 treatment groups. Fifty-two patients completed the study and were included in the final analysis (ISB = 25, ASSB = 27) (Figure 2). The cohorts were well balanced with no statistically significant differences in demographic data or preoperative measurements except for BMI values (Table 1).
Figure 2.
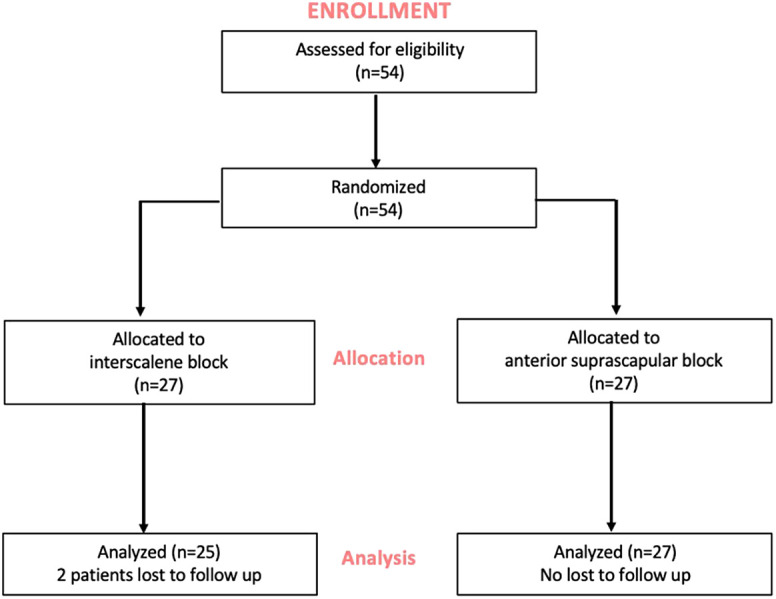
Consolidated standards of reporting trials statement flow diagram.
Table 1.
Demographic data, preoperative assessments, and surgical data
| Interscalene block group (n = 25) | Anterior suprascapular block group (n = 27) | P | |
|---|---|---|---|
| Age, years | 56.50 ± 9.6 | 52.56 ± 10.8 | .215 |
| Sex, male/female | 10/15 | 12/15 | .785 |
| Weight, kg | 78.8 ± 12.3 | 74.1 ± 21.2 | .097 |
| Height, cm | 168.7 ± 8.8 | 171.8 ± 10.3 | .135 |
| Body mass index, kg/m2 | 27 ± 3.6 | 24.2 ± 5 | .031 |
| ASA status, I/II/III | 12/8/5 | 14/11/2 | .399 |
| Preoperative baseline pain (NRS) at rest | 2.4 ± 2.4 | 1.7 ±2.0 | .479 |
| Duration of surgery, minutes | 75 ± 18 | 73 ± 12 | .238 |
| Duration of anesthesia, minutes | 113 ± 19 | 112 ± 13 | .547 |
| Type of surgery | |||
| Rotator cuff repair | 14 (56%) | 14 (52%) | |
| Calcific deposit debridement | 9 (36%) | 5 (19%) | |
| Bankart repair | 1 (4%) | 2 (7%) | |
| Global capsular release | 1 (4%) | 6 (22%) |
Values are shown as mean ± SD, median [interquartile range], or number (%).
Diaphragm movements differed significantly between the 2 groups compared to the control value (Table 2). No complete paralysis was observed in either treatment group. The incidence of a partial decrease in diaphragm movements was significantly lower in the ASSB group than in the ISB group (1 vs. 21 patients). Hemidiaphragmatic paresis at 30 minutes after the blockade was absent in 26 patients in the ASSB group and 4 in the ISB group (Figure 3). Diaphragm movements were still well preserved at a 24-hour examination in the ASSB group compared to the ISB group (Table 2).
Table 2.
Diaphragm movements compared to the control value 30 minutes after block completion and at postoperative 24 hours (numbers of patients)
| Interscalene block group (n = 25) | Anterior suprascapular block group (n = 27) | P | |
|---|---|---|---|
| Complete/partial/absent | Complete/partial/absent | ||
| 30 minutes after block | 0/21/4 | 0/1/26 | <.001 |
| Postoperative 24 hours | 0/7/18 | 0/1/26 | <.001 |
Figure 3.
The severity of hemidiaphragmatic paresis in the two groups 30 min after the blockade.
Pain scores at preoperative assessment, in the PACU (on arrival and at 30 and 60 minutes), and at 6 hours postoperatively were similar in the 2 groups. However, mean pain scores at 24 hours postoperatively were significantly higher in the ISB group than in the ASSB group (Figure 4). Time to first pain post-block was significantly longer in the ASSB group compared to the ISB group (677.04 ± 52.17 minutes vs. 479.2 ± 99.74 minutes, respectively, P < .05). The amounts of LA delivered with the PCA device in the first 24 hours were similar (104.19 ± 37.12 in the ASSB group and 113.92 ± 34.88 in the ISB group). Postoperative fentanyl requirements in the PACU were similar in the 2 groups. None of the patients in the surgery ward required rescue tramadol.
Figure 4.
Average pain scores over time. *P < .05.
None of the patients in the treatment group developed symptomatic dyspnea. A statistically significant difference was observed only in the incidence of Horner syndrome in the ISB group compared to the ASSB group (5 vs. 2 patients). No other significant adverse events occurred in either group.
Discussion
This study demonstrates ASSB is a clinically effective option for pain management for arthroscopic shoulder surgeries when compared with ISB even with low LA drug volumes (5 mL). Not only that but more ASSB better preserves diaphragm movements. The time to first pain onset is also significantly longer with ASSB compared to ISB.
Diaphragmatic paresis appears to be an inevitable consequence of ISB with a high volume of LA, while symptomatic dyspnea deriving from HDP is a challenging condition, especially for respiratory-compromised patients.2 The phrenic nerve lies close (1.8-2.0 mm) to the C5 nerve root at the level of the cricoid cartilage. The distance from the brachial plexus increases as the phrenic nerve proceeds more medially into the root of the neck.11 More distal and lateral nerve block techniques have been tried in order to avoid HDP. The supraclavicular brachial plexus block with the “corner pocket” technique effectively reduced HDP in 1 study, although HDP was still present in 28% of patients.12 The superior trunk block also provided favorable results in terms of preserving diaphragmatic and respiratory functions.13 The superior trunk block with 15 mL LA causes less HDP, with only 23.7% of patients exhibiting no evidence of paresis as defined by a lower than 25% decrease in diaphragmatic excursion. One cadaver study reported that ASSB with 5 mL of a mixture containing methylene blue resulted in retrograde staining of parts of the brachial plexus and of the phrenic nerve in 20% of cases.14 Cadaver studies have their limitations and staining of a nerve does not always correlate with clinical findings. Our results show that diaphragmatic functions were preserved in 96% (26/27) of patients in the ASSB group but in only 8% (4/25) of those in the ISB group when a low volume of LA (5 mL) was used.
The optimal doses of LA for regional anesthesia in shoulder arthroscopies in the literature vary considerably. Both Gautier et al3 and Riazi et al4 described 5 mL of LA as clinically effective. However, 10-15 mL is generally used in standard practice.15 The principal reason for this is fear of a clinically significant decrease in the duration and potency of perioperative analgesia.16 A recent cadaveric study reported that just 4.2 mL dye is sufficient to stain the suprascapular nerve while sparing the phrenic nerve.17 There may therefore be a significant risk of block failure in less experienced hands. If the purpose is only postoperative analgesia, and not surgical anesthesia, then our results show, in agreement with the previous literature, that a low volume of LA is sufficient and has an acceptable safety profile.
The critical time in arthroscopic shoulder surgery patients is when the effect of the block wears off. Dexamethasone has been shown to be effective in enhancing the effect and prolonging the duration of analgesia.18 We, therefore, administered dexamethasone to both patient groups. The mean time to first pain in the ASSB was 12 hours, significantly longer than in the ISB group, at 7 hours. Continuous nerve catheters are used to prolong the duration of analgesia and facilitate rehabilitation after shoulder arthroscopies. Another question that has not been fully answered is whether HDP may occur with continuous blockade due to LA accumulation.8 Diaphragm movements at 24 hours postoperatively indicated that there was still a 15% decrease with ISB, compared to 4% in the ASSB group. No patients in either group reported breathing difficulties during follow-up. Examination of pain scores at 24 hours showed that despite decreases in both groups, NRS scores were significantly lower in the ASSB group. Our results show that the anterior suprascapular nerve catheter is more effective for 24-hour postoperative pain control and that it preserves diaphragmatic movements better even with continuous LA administration via catheter.
The innervation of the shoulder is complex.19 Sensory innervation is from the axillary, lateral pectoral, subscapular, and suprascapular nerves. The suprascapular nerve branches out from the upper trunk, and the first 3 nerves originate from the lateral and posterior cords of the brachial plexus.20 A previous cadaver study showed that the posterior division of the upper trunk lies in close approximation to the suprascapular nerve.21 Local anesthetic delivered to the anterior suprascapular nerve is likely to spread to the posterior division of the upper trunk. The posterior division eventually gives rise to the axillary and subscapular nerves that also contribute to shoulder innervation. This mechanism may explain the comprehensive analgesic efficacy of the anterior approach of the suprascapular nerve block.22 An additional factor that may impact analgesic efficacy is that the sensory branches of the suprascapular nerve are more common and numerous than previously described, particularly in terms of the acromial structures.23 Performing an ASSB may provide more complete analgesia compared to posterior ASSB.
There are a number of limitations to this study. First, although not clinically significant, preoperative baseline pain scores in the suprascapular group were lower than in the interscalene group. The second limitation is that all blocks were performed by the same experienced anesthesiologist. Although this reduces performance bias and enhances study validity, it may nevertheless limit the generalizability of the study findings. Although the number of cuff repairs is the same in both groups, the other types of elective surgeries seem to be different between groups, which may influence postoperative pain. The study could be more powerful if all surgeries would be cuff repairs. Although same for both groups, there are different medications used after the procedures for analgesia which makes it difficult to evaluate the nominative effects of block methods. Body mass index was also significantly higher in the ISB group. High BMI index patients are clearly prone to complications and are difficult to perform. We did not see any complications or failed blocks difference between groups. Finally, more detailed respiratory functions like tidal volume and forced vital capacity were not evaluated.
The search for a diaphragm-sparing nerve block for shoulder surgery is still continuing. Even a minimal risk of HDP may be potentially threatening, particularly in the case of patients with pre-existing pulmonary compromise. Studies have stated that the target endpoint for HDP should be 0%.18 Although the level of phrenic nerve involvement after ASSB with 5 mL of LA is not zero, this nevertheless appears to be a promising clinical result.
In conclusion, both the ASSB and ISB appear to be clinically effective in providing postoperative analgesia for patients undergoing arthroscopic shoulder surgery under general anesthesia. Moreover, the time to first pain is significantly longer with ASSB. Pain scores at 24 hours postoperatively were significantly lower in the ASSB group compared to the ISB group. Diaphragmatic movements after ASSB were also better preserved at both 30 minutes after the block and 24 hours after surgery.
Footnotes
Ethics Committee Approval: Ethical committee approval was received from the Koç University Committee on Human Research Ethics Committee (Approval no: 020.010.IRB1.001).
Informed Consent: Written informed consent was obtained from all participants.
Author Contributions: Concept - A.T.D., S.K.C., Ö.E.; Design - A.T.D., S.K.C., Ö.E.; Supervision - Y.G., Ö.E., M.D.; Materials - Ö.K.; Data Collection and/or Processing - A.T.D., S.K.C., Ö.K.; Analysis and/or Interpretation - A.T.D., S.K.C.; Literature Review - A.T.D., S.K.C., Ö.K.; Writing - A.T.D., S.K.C., Y.G., Ö.E., M.D.; Critical Review - Y.G., Ö.E., M.D.
Acknowledgments: We would like to thank Dr. Arzu Baygul for her valuable contribution to the statistical analysis.
Declaration of Interests: The authors have no conflicts of interest to declare.
Funding: The authors declared that this study has received no financial support.
References
- 1. Fredrickson MJ, Krishnan S, Chen CY. Postoperative analgesia for shoulder surgery: a critical appraisal and review of current techniques. Anaesthesia. 2010;65(6):608 624. ( 10.1111/j.1365-2044.2009.06231.x) [DOI] [PubMed] [Google Scholar]
- 2. Urmey WF, Talts KH, Sharrock NE. One hundred percent incidence of hemidiaphragmatic paresis associated with interscalene brachial plexus anesthesia as diagnosed by ultrasonography. Anesth Analg. 1991;72(4):498 503. ( 10.1213/00000539-199104000-00014) [DOI] [PubMed] [Google Scholar]
- 3. Gautier P, Vandepitte C, Ramquet C, DeCoopman M, Xu D, Hadzic A. The minimum effective anesthetic volume of 0.75% ropivacaine in ultrasound-guided interscalene brachial plexus block. Anesth Analg. 2011;113(4):951 955. ( 10.1213/ANE.0b013e31822b876f) [DOI] [PubMed] [Google Scholar]
- 4. Riazi S, Carmichael N, Awad I, Holtby RM, McCartney CJ. Effect of local anaesthetic volume (20 vs 5 ml) on the efficacy and respiratory consequences of ultrasound-guided interscalene brachial plexus block. Br J Anaesth. 2008;101(4):549 556. ( 10.1093/bja/aen229) [DOI] [PubMed] [Google Scholar]
- 5. Kim BG, Han JU, Song JH, Yang C, Lee BW, Baek JS. A comparison of ultrasound-guided interscalene and supraclavicular blocks for post-operative analgesia after shoulder surgery. Acta Anaesthesiol Scand. 2017;61(4):427 435. ( 10.1111/aas.12864) [DOI] [PubMed] [Google Scholar]
- 6. Wiegel M, Moriggl B, Schwarzkopf P, Petroff D, Reske AW. Anterior suprascapular nerve block versus interscalene brachial plexus block for shoulder surgery in the outpatient setting: a randomized controlled patient- and assessor-blinded trial. Reg Anesth Pain Med. 2017;42(3):310 318. ( 10.1097/AAP.0000000000000573) [DOI] [PubMed] [Google Scholar]
- 7. Blasco L, Laumonerie P, Tibbo M.et al. Ultrasound-guided proximal and distal suprascapular nerve blocks: a comparative cadaveric study. Pain Med. 2020;21(6):1240 1247. ( 10.1093/pm/pnz157) [DOI] [PubMed] [Google Scholar]
- 8. Tran DQ, Layera S, Bravo D, Cristi-Sanchéz I, Bermudéz L, Aliste J. Diaphragm-sparing nerve blocks for shoulder surgery, revisited. Reg Anesth Pain Med. 2019. ( 10.1136/rapm-2019-100908) [DOI] [PubMed] [Google Scholar]
- 9. Boussuges A, Gole Y, Blanc P. Diaphragmatic motion studied by m-mode ultrasonography: methods, reproducibility, and normal values. Chest. 2009;135(2):391 400. ( 10.1378/chest.08-1541) [DOI] [PubMed] [Google Scholar]
- 10. Renes SH, Rettig HC, Gielen MJ, Wilder-Smith OH, van Geffen GJ. Ultrasound-guided low-dose interscalene brachial plexus block reduces the incidence of hemidiaphragmatic paresis. Reg Anesth Pain Med. 2009;34(5):498 502. ( 10.1097/AAP.0b013e3181b49256) [DOI] [PubMed] [Google Scholar]
- 11. Kessler J, Schafhalter-Zoppoth I, Gray AT. An ultrasound study of the phrenic nerve in the posterior cervical triangle: implications for the interscalene brachial plexus block. Reg Anesth Pain Med. 2008;33(6):545 550. [PubMed] [Google Scholar]
- 12. Kang RA, Chung YH, Ko JS, Yang MK, Choi DH. Reduced hemidiaphragmatic paresis with a “corner pocket” technique for supraclavicular brachial plexus block: single-center, observer-blinded, randomized controlled trial. Reg Anesth Pain Med. 2018;43(7):720 724. ( 10.1097/AAP.0000000000000795) [DOI] [PubMed] [Google Scholar]
- 13. Kang R, Jeong JS, Chin KJ.et al. Superior trunk block provides noninferior analgesia compared with interscalene brachial plexus block in arthroscopic shoulder surgery. Anesthesiology. 2019;131(6):1316 1326. ( 10.1097/ALN.0000000000002919) [DOI] [PubMed] [Google Scholar]
- 14. Sehmbi H, Johnson M, Dhir S. Ultrasound-guided subomohyoid suprascapular nerve block and phrenic nerve involvement: a cadaveric dye study. Reg Anesth Pain Med. 2019;44(5):561 564. ( 10.1136/rapm-2018-100075) [DOI] [PubMed] [Google Scholar]
- 15. Rohrbaugh M, Kentor ML, Orebaugh SL, Williams B. Outcomes of shoulder surgery in the sitting position with interscalene nerve block: a single-center series. Reg Anesth Pain Med. 2013;38(1):28 33. ( 10.1097/AAP.0b013e318277a2eb) [DOI] [PubMed] [Google Scholar]
- 16. Fredrickson MJ, Abeysekera A, White R. Randomized study of the effect of local anesthetic volume and concentration on the duration of peripheral nerve blockade. Reg Anesth Pain Med. 2012;37(5):495 501. ( 10.1097/AAP.0b013e3182580fd0) [DOI] [PubMed] [Google Scholar]
- 17. Maikong N, Kantakam P, Sinthubua A, Mahakkanukrauh P, Tran Q, Leurcharusmee P. Cadaveric study investigating the phrenic-sparing volume for anterior suprascapular nerve block. Reg Anesth Pain Med. 2021;46(9):769 772. ( 10.1136/rapm-2021-102803) [DOI] [PubMed] [Google Scholar]
- 18. Rosenfeld DM, Ivancic MG, Hattrup SJ.et al. Perineural versus intravenous dexamethasone as adjuncts to local anaesthetic brachial plexus block for shoulder surgery. Anaesthesia. 2016;71(4):380 388. ( 10.1111/anae.13409) [DOI] [PubMed] [Google Scholar]
- 19. Aszmann OC, Dellon AL, Birely BT, McFarland EG. Innervation of the human shoulder joint and its implications for surgery. Clin Orthop Relat Res. 1996;330(330):202 207. ( 10.1097/00003086-199609000-00027) [DOI] [PubMed] [Google Scholar]
- 20. Tran DQ, Elgueta MF, Aliste J, Finlayson RJ. Diaphragm-sparing nerve blocks for shoulder surgery. Reg Anesth Pain Med. 2017;42(1):32 38. ( 10.1097/AAP.0000000000000529) [DOI] [PubMed] [Google Scholar]
- 21. Hanna A. The SPA arrangement of the branches of the upper trunk of the brachial plexus: a correction of a longstanding misconception and a new diagram of the brachial plexus. J Neurosurg. 2016;125(2):350 354 Epub 2015 Nov 27. ( 10.3171/2015.5.JNS15367) [DOI] [PubMed] [Google Scholar]
- 22. Auyong DB, Hanson NA, Joseph RS, Schmidt BE, Slee AE, Yuan SC. Comparison of anterior suprascapular, supraclavicular, and interscalene nerve block approaches for major outpatient arthroscopic shoulder surgery: a randomized, double-blind, noninferiority trial. Anesthesiology. 2018;129(1):47 57. ( 10.1097/ALN.0000000000002208) [DOI] [PubMed] [Google Scholar]
- 23. Vorster W, Lange CP, Briët RJ.et al. The sensory branch distribution of the suprascapular nerve: an anatomic study. J Shoulder Elbow Surg. 2008;17(3):500 502. ( 10.1016/j.jse.2007.10.008) [DOI] [PubMed] [Google Scholar]



 Content of this journal is licensed under a
Content of this journal is licensed under a 
