Abstract
Purpose:
The aim of this study was to provide insight for the feasibility and outcomes of hybrid (combination of in-person office and Internet-based appointments) audiology services.
Method:
This pilot included two phases. First, we surveyed audiologists regarding what elements of a best-practice, in-person delivery of a hearing intervention could be delivered via Internet-based appointments. Next, we piloted the feasibility and assessed outcomes of the procedures identified. Ten first-time hearing aid users aged 70 years and older were fit with Phonak Audeo M90-312T hearing aids. Two Internet-based follow-up appointments were completed using the myPhonak app. We administered the Hearing Handicap Inventory for the Elderly–Screening Version (HHIE-S), the Client Oriented Scale of Improvement (COSI), the Quick Speech-in-Noise Test (QuickSIN), and real-ear aided responses (REARs) to determine whether participants experienced improvements on hearing-related outcomes. The Telehealth Acceptance Questionnaire (TAQ) and the Visit-Specific Satisfaction Questionnaire (VSQ-9) were administered to gauge comfort with telehealth and satisfaction with Internet-based appointments.
Results:
Survey results revealed that after an initial in-person appointment, nearly all follow-up hearing intervention components could be delivered remotely. We performed Wilcoxon signed-ranks tests to determine if the baseline and outcome results differed for outcomes. Baseline scores improved after 6 weeks (ps = .02 and. 005 for QuickSIN and HHIE-S) for speech-in-noise performance and self-perceived hearing difficulties. REARs from 500 to 4000 Hz measured after 6 weeks did not differ from baseline (ps = .612 and .398 for the right and left ears), suggesting no significant deviation from prescriptive targets because of remote fitting adjustments. All participants reported improvement in COSI goals after the intervention. TAQ results suggested that comfort with telehealth improved after attending Internet-based appointments (p = .005). VSQ-9 results revealed no differences in reported patient satisfaction between in-person and Internet-based appointments.
Conclusions:
We were able to develop a feasible hybrid audiology service delivery model for older adults. Our results enhance the evidence base for the implementation of telehealth audiology services.
Age-related hearing loss (ARHL) is a chronic disability and a major public health concern. As the U.S. population ages, hearing loss prevalence will nearly double by the year 2060 (Goman et al., 2017). Despite the availability of efficacious interventions such as hearing aids and other hearing-assistive technologies, the majority of older adults who have hearing loss go untreated. In the United States, numerous factors including high costs, stigma, lack of awareness, and accessibility problems hinder the uptake of hearing loss intervention. Although the focus of many studies is on hearing aid uptake (Garstecki & Erler, 1998; Gopinath et al., 2011; Knudsen et al., 2010), ARHL is a chronic condition, and intervention must also include evidence-based approaches that include provision of hearing devices, along with self-management supports (Barnett et al., 2017).
U.S. adults also face structural barriers to accessing comprehensive hearing health care (HHC), including high costs and difficulty navigating the HHC system (National Academies of Sciences Engineering and Medicine, 2016). Telehealth service delivery is a potential solution to some of the barriers preventing older adults from accessing and adopting hearing loss interventions. Technological advances in hearing aids and telecommunications have recently allowed for the widespread availability of telehealth audiology applications, which pose to improve both access and affordability of hearing aids and related clinical services for those with ARHL. Telehealth audiological service delivery is utilized by audiologists in a variety of settings, including private, university-based, and Veterans Affairs clinics (Angley et al., 2017; Campos & Ferrari, 2012; Gladden et al., 2015), through both asynchronous communication with patients (e.g., messages, e-mails, and fine-tuning adjustments sent via hearing aid manufacturer smartphone apps) and synchronous, face-to-face care with an HHC provider delivered over a smart device and a live video platform.
Telehealth applications for accessing health care services have expanded rapidly in availability and scope over the course of the last 10 years. A large body of systematic reviews summarized in an evidence map by the Agency for Healthcare Research and Quality demonstrated positive patient outcomes for several chronic conditions, such as chronic obstructive pulmonary disease and respiratory disease, when managed via telehealth (Totten et al., 2016). The existing literature also describes the use of telehealth audiology services for hearing aid fittings, follow-up hearing aid fine-tuning, and postfitting self-management supports (Angley et al., 2017; Campos & Ferrari, 2012; Tao et al., 2018). Angley et al. (2017) found few technology issues and high patient satisfaction among adults (M age = 62 years, age range: 34–77 years) tasked with home installation of remote hearing aid fitting software and participation in remote hearing aid fitting appointments, demonstrating the feasibility of remote hearing aid programming via telehealth applications. In a recent systematic review, Tao et al. (2018) applied the Preferred Reporting Items for Systematic Review and Meta-Analysis methodological standards to evaluate studies focused on remote delivery of hearing aid services. The authors concluded that telehealth delivery of audiology services appears to have similar outcomes as in-office services in terms of feasibility, quality, and effectiveness. However, most of the included studies examined service delivery via the telephone or video conferencing.
More recently, Convery et al. (2020) assessed usability of an asynchronous smartphone application (ReSound Assist) in a group of 15 adults with a median age of 67 years (age range: 22–83 years). Of the 15 intervention participants, 12 used the application, and 11 were able to successfully send a request and upload programmed fine-tuning changes to their hearing aids. Participants also rated the application as highly usable in terms of effectiveness, efficiency, and satisfaction, as measured by a modified Telehealth Usability Scale. Compared to a control condition of in-office care, participants assigned to the application intervention also displayed no significant differences in hearing aid outcomes (Abbreviated Profile of Hearing Aid Benefit, Satisfaction With Amplification in Daily Life, speech understanding in noise, and mean hours of daily hearing aid use as measured by data logging). Synchronous services were not assessed in the study by Convery et al. To our knowledge, no studies have specifically focused on the use of synchronous smart device–based hearing aid interventions in older adults aged > 70 years.
Some evidence exists that suggests that older adults with hearing loss use the Internet in higher numbers than the general population. Hearing aid users surveyed in Sweden (age range: 75–96 years) had 1.74 higher odds (confidence interval [1.23, 3.17]) of reporting Internet use than other groups (Thorén et al., 2013), and those with slight hearing loss surveyed in the United Kingdom (age range: 50–74 years) were more likely than those with no hearing loss to use the Internet (Henshaw et al., 2012). However, a qualitative study conducted by Chandra and Searchfield (2016) revealed several themes related to awareness, uncertainty, and a lack of confidence among adults aged 64–81 years with regard to using the Internet to access hearing aid services. Many participants were unaware that hearing aid services could be accessed online and did not know where to find more information. Furthermore, participants questioned the validity of an online hearing aid fitting and expressed concern that their follow-up needs might not be addressed. An overall distrust in an online clinician or sales representative due to lack of face-to-face contact was another primary concern. Finally, participants demonstrated an overall lack of familiarity and comfort using the Internet or smart device applications as a whole. Although telehealth audiology service delivery is readily available and studies demonstrate that it is an efficacious intervention (Angley et al., 2017; Campos & Ferrari, 2012; Tao et al., 2018), there remains a gap in our understanding of what barriers and facilitators exist for older adults with regard to using Internet-based telehealth audiology services.
In addition to patient experiences, HHC providers have also reported various facilitators and barriers to Internet-based service delivery. In a systematic review, Ravi et al. (2018) identified five studies that investigated audiologists' knowledge and perceptions of telehealth audiology. Findings revealed that, although HHC providers, on the whole, had positive attitudes toward acceptance of using telehealth with their patients, they identified numerous barriers to the effective implementation of widespread telehealth audiology adoption. Specifically, limitations in infrastructure (Internet connectivity and technology availability to patients) were cited as a primary barrier. Concerns regarding the accuracy of diagnostic tests and the abilities of patients to easily access and use telehealth were also reported. The authors concluded that knowledge gaps exist in the implementation of telehealth audiology services, particularly regarding audiologists' attitudes and perceptions (Ravi et al., 2018). Taken together, the telehealth audiology literature to date suggests a need for more studies examining the utility of remote technologies for delivering comprehensive HHC services from the perspective of both the patient and the audiologist.
A manualized, best-practices, comprehensive HHC approach was implemented in a large, multisite, randomized clinical trial, Aging and Cognitive Health Evaluation in Elders (ACHIEVE; Clinicaltrials.gov Identifier: NCT03243422, NIA R01AG055426, R01AG060502) that began in January 2018. ACHIEVE recruited 977 cognitively intact older adults with mild–moderate hearing loss who were randomized to receive either in-person, best-practices hearing aid intervention or a successful aging education active control and who are being followed for 3 years to assess cognitive, social functioning, physical functioning, and quality of life outcomes (Deal et al., 2018; Sanchez et al., 2020). Although the results of ACHIEVE are yet to be determined, the comprehensive HHC approach is time consuming, involving four office-based visits over the course of 8–10 weeks, with additional office-based follow-ups every 6 months over the course of 3 years. There is a need to determine the feasibility of streamlining and adapting the ACHIEVE Hearing Intervention (Sanchez et al., 2020), particularly considering advances made in the use of the telehealth technologies to deliver many components of the hearing intervention remotely.
With reference to the Consolidated Framework for Implementation Research (Damschroder et al., 2009) and guidelines for adapting manualized interventions (Goldstein et al., 2012), we engaged in a phased approach to gather information to systemically modify and streamline the manualized conventional ACHIEVE Hearing Intervention (Sanchez et al., 2020) for implementation leveraging current telehealth technologies. Our phased approached had two objectives. First, in Phase 1, we surveyed the ACHIEVE audiologists to evaluate their perspectives regarding what essential components of a comprehensive hearing intervention could be delivered via the Internet and what facilitators and barriers exist for the widespread delivery of Internet-based audiology services. Second, in Phase 2, we report a pilot feasibility study, in which we sought to evaluate hearing-related outcomes and to determine patients' comfort level with telehealth technology and preferences for service delivery pre- and postdelivery of hearing aid services via a streamlined ACHIEVE hybrid (combination of in-person and Internet-based) audiology service delivery model. All procedures utilized in the two phases described below were approved by the University of South Florida Institutional Review Board prior to initiation of any study activities.
Phase 1. Audiologist Survey and Development of the Hybrid Audiology Service Delivery Model
We invited the seven ACHIEVE study audiologists to provide perspectives on Internet-based HHC delivery to inform the protocols of a hybrid in-office/Internet-based telehealth hearing aid service delivery model. At the time of this phase in our study, there were seven licensed audiologists across four ACHIEVE study sites: (a) University of Mississippi Medical Center in Jackson, Mississippi; (b) Wake Forest Baptist Medical Center in Winston–Salem, North Carolina; (c) Johns Hopkins University in Baltimore, Maryland; and (d) University of Minnesota in Minneapolis, Minnesota. All seven audiologists were invited to participate in the survey, and all seven agreed.
We collected quantitative and qualitative data from the audiologists through administration of an online survey via the Qualtrics platform. The survey asked questions evaluating perceptions of the overall importance of integral hearing aid intervention procedures, including selection and fitting via real-ear measures, orientation and use, treatment goal setting, and person-centered counseling, along with the feasibility and comfort levels with delivering these procedures through an Internet-based telehealth delivery model. The surveys were separated into four feedback sections, with each section matched to the procedures performed at each ACHIEVE Hearing Intervention visit (Sessions A, B, C, and D; see the work of Sanchez et al., 2020, for details). Questions posed for each procedure were phrased as such: “In a best-practices hearing aid intervention protocol, should (this procedure) be considered (a) mandatory, (b) optional, or (c) not included?” followed by rating the feasibility of delivering each procedure through a telehealth model: “Could (this procedure) be delivered (a) in-office only, (b) Internet-based telehealth, or (c) not sure?” The audiologists were asked to assume the following when considering the delivery of a particular component via telehealth: (a) The participant is willing to adapt to remote services, (b) both the clinician and the participant have the appropriate technology to deliver services remotely, and (c) proper training will be provided to the clinician before administering these procedures. Each item included an open-ended text entry response where audiologists were encouraged to provide qualitative comments, suggestions, and other feedback, to be analyzed and triangulated with the survey responses. These text entry spaces were also provided to capture as many opinions as possible for each procedure, including additions, modifications, and/or substitutions for performing the procedure.
The survey data were collated and exported into a Microsoft Excel spreadsheet for analysis. Quantitative data (survey descriptive statistics), along with qualitative data (open-ended comments from the audiologists about each procedure), were included. The audiologists were provided a respondent ID, and each survey session was separated into a worksheet tab. Two independent raters (H.N. and T.H.C.) identified common themes through highlighting similar comments among audiologists. Themes were identified based on word repetition/frequency and key words in context (e.g., “barriers,” “Wi-Fi connection,” and “Bluetooth”).
Core components of the intervention were identified, and responses indicated that many services, including the setting of individualized goals via the Client Oriented Scale of Improvement (COSI; Dillon et al., 1997), hearing aid orientation, hearing aid interviews, self-report outcomes assessments, physical fit checks, visual checks, data logging, and programming adjustments, were believed to be feasible to be completed online by at least one of the audiologists (see Table 1). Audiologists also provided commentary on how they believe their patients would accept hybrid services. Survey results and identified themes were discussed with ACHIEVE audiologists through a 2-hr synchronous video conference and incorporated into the hybrid audiology service delivery model, described below in Phase 2 of this project. The themes identified beyond the survey items included (a) navigating hearing difficulties and ensuring adequate volume during a remote session, (b) management of participants who may forget or not accurately remember previously discussed information, (c) troubleshooting Internet connectivity, (d) troubleshooting Bluetooth complications, and (e) reasons for interim in-office visits.
Table 1.
Audiologist survey results (n = 7).
| Procedure | Importance (n) |
Feasibility (n) |
||||
|---|---|---|---|---|---|---|
| Mandatory | Optional | Not included | In-office | Online | Not sure | |
| Session A | ||||||
| 1. Electroacoustic verification | 6 | 1 | 0 | 7 | 0 | 0 |
| 2. COSI | 6 | 1 | 0 | 0 | 7 | 0 |
| 3. WRECD | 2 | 4 | 1 | 7 | 0 | 0 |
| 4. Speech mapping at 65-dB input | 6 | 1 | 0 | 7 | 0 | 0 |
| 5. Record real ear at 50 and 75 dB | 3 | 4 | 0 | 7 | 0 | 0 |
| 6. MPO | 7 | 0 | 0 | 7 | 0 | 0 |
| 7. Comfort scaling at 65 dB | 5 | 2 | 0 | 7 | 0 | 0 |
| 8. Comfort scaling at 75 dB | 4 | 3 | 0 | 7 | 0 | 0 |
| 9. Hearing aid orientation | 7 | 0 | 0 | 3 | 4 | 0 |
| Session B | ||||||
| Hearing aid fitting interview | 7 | 0 | 0 | 0 | 7 | 0 |
| Physical fit check | 7 | 0 | 0 | 5 | 2 | 0 |
| Visual check | 6 | 1 | 0 | 5 | 0 | 2 |
| Listening check | 7 | 0 | 0 | 7 | 0 | 0 |
| EAA | 3 | 4 | 0 | 7 | 0 | 0 |
| Data logging | 4 | 3 | 0 | 4 | 2 | 1 |
| Real ear following program adjustment | 2 | 5 | 0 | 6 | 1 | 0 |
| Session C | ||||||
| Hearing aid fitting interview | 6 | 1 | 0 | 0 | 7 | 0 |
| Physical fit check | 3 | 4 | 0 | 4 | 2 | 1 |
| Visual check | 6 | 1 | 0 | 3 | 3 | 0 |
| Listening check | 5 | 2 | 0 | 7 | 0 | 0 |
| EAA | 2 | 5 | 0 | 7 | 0 | 0 |
| Data logging | 4 | 3 | 0 | 3 | 4 | 0 |
| Real ear following program adjustment | 3 | 4 | 0 | 6 | 1 | 0 |
| Aided QuickSIN | 3 | 3 | 1 | 6 | 0 | 1 |
| IOI-CHI | 4 | 2 | 1 | 0 | 6 | 1 |
| COSI-GAF | 6 | 1 | 0 | 0 | 7 | 0 |
| Session D | ||||||
| Hearing aid fitting interview | 3 | 4 | 0 | 0 | 7 | 0 |
| Physical fit check | 1 | 6 | 0 | 4 | 2 | 1 |
| Visual check | 2 | 5 | 0 | 4 | 2 | 1 |
| Listening check | 2 | 5 | 0 | 7 | 0 | 0 |
| EAA | 0 | 7 | 0 | 7 | 0 | 0 |
| Data logging | 3 | 4 | 0 | 4 | 3 | 0 |
| Real ear following program adjustment | 3 | 4 | 0 | 7 | 0 | 0 |
| IOI-CHI | 3 | 2 | 2 | 0 | 5 | 2 |
| COSI-GAF | 4 | 2 | 1 | 0 | 6 | 1 |
Note. This table lists the procedures within each Aging and Cognitive Health Evaluation in Elders session (see the work of Sanchez et al., 2020, for details), followed by the survey response ratings of importance and feasibility of delivery via eAudiology. The numbers in Columns 2–5 reveal the number of audiologists (n = 7) who indicated that rating. COSI = Client Oriented Scale of Improvement; WRECD = wide-range real ear to coupler difference measurement; MPO = maximum power output measurement; EAA = electroacoustic analysis; QuickSIN = Quick Speech in Noise Test; IOI-CHI = International Outcome Inventory of Comprehensive Hearing Intervention; GAF = Goal Assessment Form measurement.
Phase 2. Feasibility and Pilot Study of the Hybrid Audiology Service Delivery Model
Guided by results of the audiologist survey and commentary, the hybrid audiology service delivery model consisted of in-person office appointments and Internet-based hearing aid follow-up appointments. The first in-person office visit (baseline) includes a comprehensive hearing evaluation and hearing aid fitting and orientation. Based on the audiologist survey and commentary, it was decided that the baseline and initial hearing aid fitting visit should occur in person. Following the baseline office visit, two biweekly Internet-based hearing aid follow-up appointments using the Remote Support feature of the myPhonak smartphone application were scheduled for patients to connect to using their personal devices. Audiologist feedback guided the step-by-step protocols for the Internet-based visits, including scripts and patient instructions. After 6–8 weeks of hearing aid use and completion of two Internet-based remote appointments, an in-person office visit was scheduled to measure outcomes associated with the hearing intervention, including self-report measures, aided functional testing, and verification of the hearing aid fitting, to confirm the remote adjustments did not deviate significantly from fitting targets, such that the patient benefit from amplification is negatively impacted. Details for each session of the hybrid audiology service delivery intervention assessed for feasibility with older adult, first-time hearing aid users are described in the Procedure section below.
Method
Participants
To assess the feasibility of our hybrid audiology service delivery model, we recruited a convenience sample of 10 first-time hearing aid users (six men and four women) over the age of 70 years from a clinical population (M age = 76 years, age range: 70–91 years). Additional inclusion criteria were self-reported access to a smartphone and a stable home Internet connection; at least a mild hearing loss (> 25 dB HL pure-tone average [PTA] for 500, 1000, 2000, and 4000 Hz) in the better ear; normal cognition as measured by the Mini Mental State Examination (MMSE), using a cutoff of ≥ 23 if education was reported as high school degree or less and ≥ 25 if some college or more (Folstein et al., 1973); and corrected vision better than 20/63 (as measured using the Minnesota Read Acuity Card; Calabrèse et al., 2016). Individuals were excluded if they presented with a bilateral conductive hearing loss (defined as a > 10-dB air–bone gap at two or more frequencies) or reported that they would not be willing to use hearing aids at least 4 hr per day throughout the study duration.
Measures
Participants completed a self-report questionnaire including demographic information such as age, race/ethnicity, education level, and hearing health history. They also completed both objective and subjective outcome measures to determine the feasibility of the use of a hybrid service delivery model. Objective outcome measures included real-ear aided responses (REARs), aided versus unaided speech-in-noise ability measured via the Quick Speech-in-Noise Test (QuickSIN; Killion et al., 2003), and mean hours of daily hearing aid wear via data logging through the manufacturer software. Data logging was used to guide counseling in the event that participants were using their hearing aids less than 4 hr per day. Subjective measures included the Hearing Handicap Inventory for the Elderly–Screening Version (HHIE-S; Lichtenstein et al., 1988; Ventry & Weinstein, 1983), the COSI (Dillon et al., 1997), the Telehealth Acceptance Questionnaire (TAQ; Wade et al., 2012), and the Visit-Specific Satisfaction Questionnaire (VSQ-9; American Medical Group Association, n.d.). Each of these measures is described below.
REARs
Probe microphone measurements of real-ear output were performed on all participants to verify the REARs from a 65 dB SPL input signal matched to the National Acoustics Laboratories' nonlinear (NAL-NL2) prescribed aided output response target (Keidser et al., 2011). Operational tolerance ranges were within 5 and −8 dB from 250 to 3000 Hz and within 10 and −13 dB at 4000 Hz (ANSI S3.22-2003). Minor fluctuations from these ranges were accepted due to adjustments requested to accommodate participants' sound quality preferences or the inability to reach targets due to severity of high-frequency hearing loss. REARs were measured in-office at the initial hearing aid visit during the baseline visit and at a 6- to 8-week in-office outcomes assessment visit following two sessions of Internet-based audiology service delivery.
HHIE-S
The HHIE-S (Lichtenstein et al., 1988; Ventry & Weinstein, 1983) was administered to measure self-perceived hearing impairment and to determine if expected reductions in self-perceived hearing difficulties were evident following hearing aid intervention using a hybrid audiology service delivery model. The 10-item questionnaire is highly reliable (r = .97), with scores ranging from 0 to 40 (higher scores indicate greater self-perceived hearing difficulties). Scores of ≥ 10 suggest significant hearing problems warranting a referral for a full audiometric evaluation (American Speech-Language-Hearing Association, 1997).
COSI
The COSI (Dillon et al., 1997) is an open-ended self-report outcome assessment that focuses on patient-set goals and their attainment. Specific hearing-related goals are defined and prioritized by the patient, and following a sustained period of intervention use, they estimate the degree of improvement and final communication ability for each goal. The COSI is a reliable clinical outcome measure (improvement, r = .73; final ability, r = .84) that is correlated with other measures of hearing intervention benefit such as the HHIE-S and the Profile of Hearing Aid Benefit (Dillon et al., 1997).
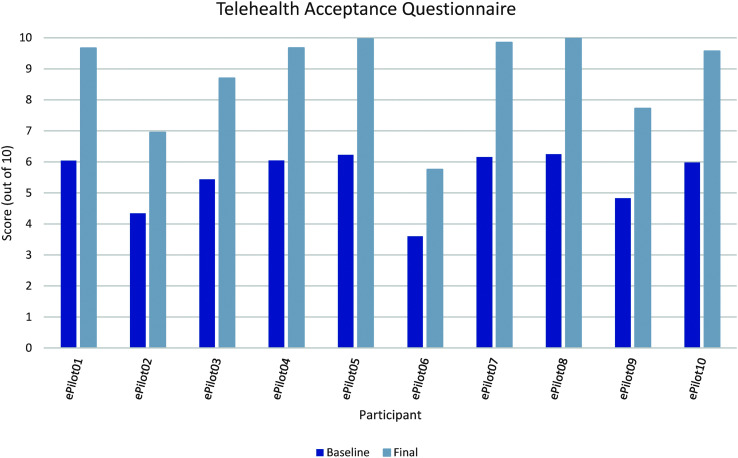
TAQ
The TAQ (Wade et al., 2012), based on the technology acceptance model (Davis, 1986; King & He, 2006), includes eight 5-point Likert-type questions intended to measure the telehealth technology's perceived usefulness ease-of-use scale (Wade et al., 2012). TAQ items assess aspects of telehealth use by posing questions such as, “Using the telehealth equipment will save time in having regular appointments,” and “Learning to operate the telehealth equipment will be easy for me.” Scores on the TAQ range from 0 to 10, with higher scores indicating greater telehealth acceptance. The TAQ was administered to determine whether acceptance (perceived usefulness and/or ease of use of telehealth technology) changed as a result of participating in Internet-based hearing aid follow-up appointments.
VSQ-9
The VSQ-9 (American Medical Group Association, n.d.) is a widely used clinical tool that assesses how patients evaluate their medical care experiences. Individuals are instructed to rate nine different aspects of care (e.g., convenience of appointment, personal manner of the provider, length of wait time to see the provider, skills of the provider, and overall visit satisfaction) using 5-point scale responses ranging from poor to excellent. In this study, the VSQ-9 was administered to determine whether differences in patient satisfaction existed based on type of appointment attended.
Procedure
Participants attended a baseline in-person office visit where eligibility was determined through administration of the MMSE (Folstein et al., 1973), the use of the Minnesota Read Acuity Card, and completion of a comprehensive hearing assessment. The hearing assessment included otoscopy to determine the health of the outer ear and auditory ear canal, tympanometry to determine the motility of the tympanic membrane, and pure-tone and speech audiometry. Pure-tone and speech audiometry were conducted in a double-walled, sound-treated booth using an Interacoustics Equinox clinical audiometer and ER-3A insert earphones. Pure-tone air- and bone-conduction thresholds were measured using the modified Hughson–Westlake procedure (Carhart & Jerger, 1959). Speech audiometry in quiet included speech recognition threshold measurement and suprathreshold word recognition in quiet assessment using Northwestern University ordered-by-difficulty monosyllabic words (Hurley & Sells, 2003). Unaided speech-in-noise ability was measured using the QuickSIN (Killion et al., 2003). Masking was used as needed for pure-tone and speech audiometry procedures.
Following eligibility determination, they were fit with bilateral Phonak Audeo M90-312T receiver-in-canal hearing aids using appropriate receiver length and dome coupling as ascertained by the attending clinician. We conducted electroacoustic analysis at the baseline and outcomes assessment visits to ensure the hearing aids were within ANSI S3.22-2003–specified acceptable tolerances using an Audioscan Verifit2 hearing instrument verification system. Hearing aids were fit to NAL-NL2 prescriptive targets (Keidser et al., 2011), and REARs were verified using an Audioscan Verifit2 hearing aid analyzer and fitting system. Following hearing aid fitting and fine-tuning, participants received a comprehensive hearing aid orientation that included instructions and practice for insertion and removal of devices, cleaning and battery care, phone use, and information for follow-up visits. Participants also received a thorough, hands-on telehealth education session, which included downloading the myPhonak application to their personal smart device, connecting hearing aids to their smart device, and connecting to a Remote Support session with a clinician. To ensure that participants were able to use the telehealth technology, clinicians engaged in a “Say, Do, Watch” process for each stage of the orientation using a scripted checklist. For example, an explanation was provided on how to connect to a Remote Support session (“Say”) while demonstrating the steps in the office (“Do”). Before moving on to the next skill, the clinician then asked the participant to teach-back the skill that was just covered (“Watch”). The use of a standardized manual of operations, counseling scripts, and procedural checklists was implemented to ensure that the telehealth education session was delivered as intended to each participant. Each participant was also provided written materials of topics covered during the baseline appointment (e.g., audiogram and explanation of hearing loss, COSI goals, and step-by-step hearing aid and myPhonak instructions), adapted from the Hearing Loss Toolkit for Self-Management (Arnold et al., 2019). Including the comprehensive hearing assessment, hearing aid fitting and orientation, and telehealth education session, the mean initial in-office visit time was 120 min (SD = 30.6 min, range: 85–186 min). At this baseline visit, subjective measures were also administered (HHIE-S, COSI, TAQ, and VSQ-9).
Two subsequent Remote Support follow-up visits were scheduled at biweekly intervals after the initial in-office visit. These appointments were scheduled at the end of the in-person baseline office visit, and reminder calls were sent to the participants 1 day prior to the scheduled Internet-based session. At the time of the Remote Support appointments, the participant was contacted through the Phonak Target software and was notified through their myPhonak smart device application that the hearing care provider was contacting them. Once the connection was made between the provider and the participant, a brief interview was conducted to assess how the participant has been doing with their new hearing aids. COSI goals were reviewed with participants at each Internet-based Remote Support visit to assess goal progress and to offer solutions for persisting difficulties. When Internet bandwidth at the participant's residence was not initially strong enough to support a remote session, troubleshooting techniques were used to ensure adequate Internet connectivity. Hearing aid fine-tuning and programming changes occurred based on the participant's self-report. All participants requested an increase in the global gain at the first Remote Support session. Data logging was also collected at each Remote Support appointment to document average daily hearing aid usage, and participants were counseled regarding increasing wear time when data logging showed < 4 hr mean daily use. Averaged across both remote sessions for all 10 participants, the mean Remote Support visit completion time was 28.75 min (SD = 16.7 min, range: 16–71 min).
Final objective and subjective outcomes were measured in-office between 6 and 8 weeks after the initial baseline visit. REARs were completed to examine the fine-tuning and programming changes completed through the Internet-based follow-up appointments contributed to significant deviations from the initial fitting. Aided QuickSIN testing was also completed at this visit to compare to the baseline unaided results. To assess COSI goal attainment, participants answered the following two questions for each of their goals: (a) “Rate the degree of change in your hearing ability since your first visit for this goal,” and (b) “In this situation, how much of the time are you now able to hear?” Participants also completed the HHIE-S and the TAQ in response to their experience with their hearing aids and telehealth use to compare to baseline scores. The VSQ-9 was administered after each appointment: For in-person office visits, participants completed it using pen and paper, and for Internet-based visits, the attending clinician sent the VSQ-9 via the myPhonak smartphone app. All participants also completed a 6-month follow-up session following the in-person outcomes assessment visit, delivered via an Internet-based Remote Support appointment. During the 6-month follow-up, participants were asked about their experience with hearing aids and if they needed any assistance or programming adjustments. Finally, participants were given information regarding long-term hearing aid follow-up and released from the study. Participants were able to keep the hearing instruments used in exchange for their participation at no out-of-pocket cost, minus future upkeep and audiological follow-up as needed.
Data Analysis
For the feasibility assessment data, descriptive statistics for demographic variables and mean audiometric thresholds were calculated. Wilcoxon signed-ranks tests were performed to determine if the baseline and outcomes assessment results differed for the QuickSIN, REARs, the HHIE-S, and the TAQ and if patient satisfaction differences were evident between in-person and Internet-based appointments as measured by the VSQ-9. Individual COSI goal attainment responses were compared with initial goals to determine the degree of improvement for each COSI goal. Statistical analyses were conducted using IBM SPSS Statistics 26.
Results
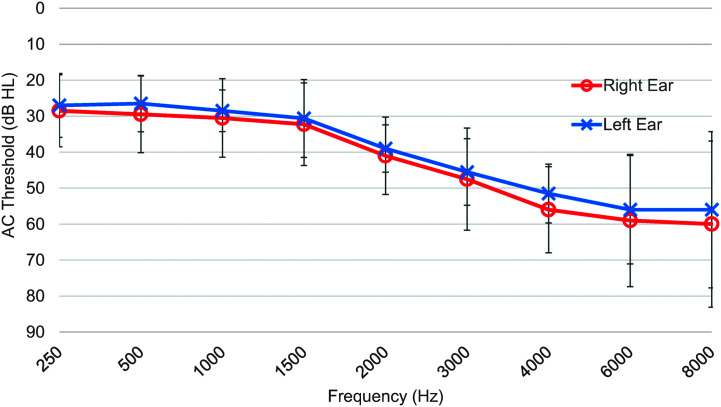
Table 2 displays individual participant demographic data. Participants were primarily non-Hispanic and White (n = 8), and all reported at least a high school education or greater. Air-conduction pure-tone testing revealed mean 500, 1000, 2000, and 4000 Hz PTAs of 39 and 36 dB HL for the right and left ears, respectively. Mean audiometric thresholds from 250 to 8000 Hz are displayed in Figure 1. All participants were able to connect to both scheduled Remote Support sessions using the myPhonak app, with the exception of Pilot10, whose bandwidth at the time of the second Remote Support session was too limited to allow for remote connection to the fitting software. This visit was conducted via the telephone, as the participant did not have any requests for programming adjustments at that time.
Table 2.
Patient demographics.
| Patient ID | Age (years) | Sex | Education | Race | Ethnicity |
|---|---|---|---|---|---|
| Pilot01 | 74 | Female | Graduate degree | White | Not Hispanic or Latino |
| Piot02 | 79 | Male | Some professional school after college | White | Hispanic/Latino |
| Pilot03 | 70 | Male | Some college | White | Not Hispanic or Latino |
| Pilot04 | 78 | Male | Bachelor's degree | White | Not Hispanic or Latino |
| Pilot05 | 70 | Female | High school diploma | White | Not Hispanic or Latino |
| Pilot06 | 79 | Female | Graduate degree | White | Not Hispanic or Latino |
| Pilot07 | 75 | Female | Bachelor's degree | White | Not Hispanic or Latino |
| Pilot08 | 69 | Male | Some professional school after college | White | Not Hispanic or Latino |
| Pilot09 | 75 | Male | Some college | Black/African American | Not Hispanic or Latino |
| Pilot10 | 91 | Male | Graduate Degree | White | Not Hispanic or Latino |
Note. This table displays the individual participant demographic characteristics.
Figure 1.
Means and standard deviations for pure-tone air-conduction (AC) thresholds from 250 to 8000 Hz for 10 older adult participants.
Objective Outcomes
Wilcoxon signed-ranks tests were performed to determine if the baseline and outcomes assessment results differed for the QuickSIN and REARs. Overall, participants had better speech-in-noise performance in the aided condition measured at the outcomes assessment visit (mean signal-to-noise ratio [SNR] = 5.0 dB, SD = 4.41 dB) compared to baseline (mean SNR = 7.75 dB, SD = 5.74 dB, p = .02).
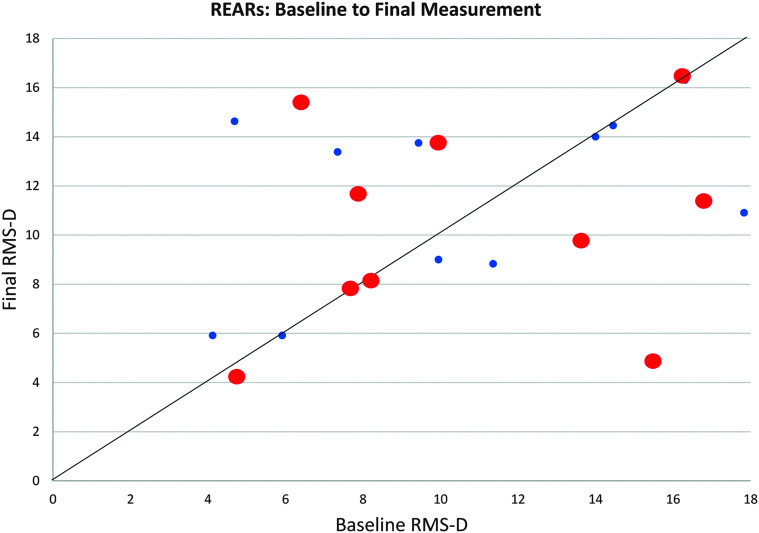
Mean REAR values obtained across the four-frequency PTA from 500 to 4000 Hz measured at the outcomes assessment visit did not differ from baseline REARs (ps = .61 and .40 for the right and left ears, respectively), suggesting no significant deviation from the initial fit as a result of Remote Support hearing aid programming adjustments. As noted previously, at the time of first fit, participants were fit to target gain from 250 to 4000 Hz using NAL-NL2 gain targets. After REARs were measured to verify the fitting, global gain was reduced to 80% (to allow for acclimatization, at the request of the participant), with the goal of increasing global gain at a subsequent fitting appointment to 100% target. Each participant requested some degree of fine-tuning at a follow-up appointment, and primary requests resulted in an increase in global gain, with eight participants fit to 100% and one participant set to 90% target gain at the first or second Remote Support appointment. Pooled mean REAR values for left and right ears from all 10 participants are shown in Figure 2. Scores represent the root-mean-square difference average, comparing the probe microphone–measured real-ear output to a 65–dB SPL input signal against NAL-NL2 prescriptive targets (McCreery et al., 2013).
Figure 2.
Individual real-ear aided response (REAR) results for both right (bigger circles in red) and left (smaller circles in blue) ears (N = 10, 20 ears total) at baseline (x-axis) compared to final measurement (y-axis). The REARs compared to NAL-NL2 targets were compared by calculating the root-mean-square using the difference between the mean measured output at 500, 1000, 2000, and 4000 Hz and the NAL-NL2 targeted level across those frequencies (McCreery et al., 2013). There were seven fittings essentially unchanged from baseline to final measurement. There were seven fittings closer to target at baseline, and six fittings were adjusted over the intervention period leading to REARs closer to the prescriptive target. No significant differences were seen between baseline and final REARs. RMS-D = root-mean-square difference.
Subjective Outcomes
Wilcoxon signed-ranks tests were used to measure differences between subjective baseline and outcomes assessment results for the HHIE-S and the TAQ, as well as to compare patient satisfaction for in-person versus Internet-based appointments as measured by the VSQ-9. Mean HHIE-S total scores measured at the outcomes assessment visit (M = 3.2, SD = 3.67) demonstrated improvement compared to baseline (M = 19, SD = 5.43, p = .005), indicating that participants showed fewer self-perceived hearing difficulties after hearing aid use for 6–8 weeks. Mean total TAQ scores also demonstrated improvement from the baseline (M = 5.49, SD = 0.92) to the outcomes assessment visit (M = 8.79, SD = 1.48, p = .005), suggesting that participants' perception of the usefulness and ease of use of telehealth technology increased after taking part in Internet-based hearing aid fitting appointments using the Remote Support feature of the myPhonak smart device application (see Figure 3). VSQ-9 results revealed ceiling effects in that all participants rated each nine items as “excellent” after each session, regardless of whether the appointment was held in person or through Remote Support. Finally, all participants additionally reported improvement in COSI goals throughout the 6 weeks, with the majority rating their final ability for each goal as either “slightly” or “much better” (n = 8) and being able to hear in each identified situation “most (75%) of the time” or “almost always (95%) of the time” (n = 9).
Figure 3.
Individual total scores on the Telehealth Acceptance Questionnaire (TAQ) at baseline and at the final outcomes assessment visit for 10 participants. TAQ total scores are calculated on a Likert-type scale from 0 to 10, with 0 = not accepting of telehealth and 10 = comfortable with telehealth.
Discussion
We were able to incorporate the perspectives of audiologists, obtained in Phase 1 of this work, into adapting a fully in-person, best-practices hearing intervention into a hybrid, combination of in-person and Internet-based telehealth audiology service delivery model. The feasibility of the hybrid service delivery model was assessed in Phase 2 of this work by administering the intervention protocol to a small sample of well-educated older adults with mild–moderate hearing loss. In line with the systematic review by Ravi et al. (2018), the audiologists surveyed expressed concerns over Internet-based service delivery infrastructure, particularly on the patient side. Primary concerns involved troubleshooting technology (Wi-Fi and Bluetooth) and ensuring that patients could hear and understand the clinician over a remote connection. With these concerns in mind, the results of the feasibility study allowed for the demonstration of expected improvements in hearing-related objective and subjective outcomes. Participants reported lower self-perceived hearing handicap and successful goal attainment after receiving the hybrid intervention. Participants also demonstrated listening in noise improvements in an aided versus unaided condition as measured by the QuickSIN. Furthermore, there was no evidence of significant deviation in gain from NAL-NL2 prescriptive targets, fit in-office, following two Internet-based hearing aid follow-up appointments where programming adjustments were made. For some participants, larger individual differences were seen (up to 10 dB): As individuals acclimated to using hearing aids, they requested increases in gain at subsequent appointments. This is not outside of what would typically happen in a clinical setting, as patients can take several weeks to become adjusted to using hearing aids, particularly those with age-related moderate and poorer hearing losses (Keidser et al., 2008).
Our findings were consistent with previous studies of Internet-based hearing aid delivery. Although there are limited studies that investigated how remote programming impacts objective outcomes, a study by Venail et al. (2019) found excellent reliability between real-ear insertion gain and speech understanding in noise (intraclass correlation coefficient = .92, 95% confidence interval [.87, .95]) for 52 adult hearing aid users randomized to in-person or remote hearing aid programming. Similarly, Convery et al. (2020) revealed no significant differences (p = .61) when comparing speech perception in noise performance between experienced hearing aid users randomized to traditional in-office care versus delivery of care through an asynchronous hearing aid smartphone application (n = 15 per group). In this study, REARs did not differ significantly from the baseline fitting to NAL-NL2 prescriptive targets, and our participants experienced improvements in speech perception in noise performance similar to results seen in studies referenced above following both in-person and telehealth delivered care.
Regarding hearing-related subjective outcomes, older adult participants in this study experienced a significant decrease in self-perceived hearing handicap as measured by the HHIE-S, consistent with findings from previous studies of telehealth audiology service delivery. For example, in a retrospective case–control study of over 42,000 Veterans who received either telehealth or traditional in-person HHC, mean International Outcome Inventory for Hearing Aids (Cox & Alexander, 2002) total scores did not differ significantly based on mode of HHC delivery, with both groups demonstrating improvements in hearing aid satisfaction (p > .05; Pross et al., 2016). Convery et al. (2020) also saw improvements on the Abbreviated Profile of Hearing Aid Benefit (Cox & Alexander, 1995) among participants randomized to smartphone application–based hearing aid appointments similar to those receiving in-person office care. We also found that older adults included in this study experienced increased perceived usability and comfort with telehealth technology following participation in Internet-based hearing aid follow-up appointments. This finding is consistent with findings from a qualitative analysis of telehealth barriers, facilitators, and advantages specific to geriatric patients during the COVID-19 pandemic, which revealed that telehealth acceptance and uptake were rapid and ongoing among older adults (Goldberg et al., 2021). Finally, our participants were highly satisfied with both in-person and Internet-based appointments, anecdotally noting that remote visits were more convenient with regard to reduced travel times and increased comfort. Our findings echo those reported by Hantke et al. (2020) in a survey of 40 older adults receiving video teleconference–based psychiatry services during the COVID-19 pandemic.
Our study had some limitations. First, our study sample for the assessment of the feasibility of the service delivery model was too small to draw conclusions regarding generalizability to a broader population. We did not include or randomize participants to a control group or condition with which to compare outcomes, which is necessary for inferring causality. Furthermore, this sample lacked diversity in that most participants were well-educated, non-Hispanic/Latino Whites. Outcomes may differ based on degree of education, particularly comfort with using telehealth technology as measured by the TAQ. The audiologists surveyed were all intervention providers for the ACHIEVE trial, and thus, we cannot state that the procedures identified as being feasible for online delivery are the same as those that might be selected by audiologists in different practice settings (e.g., private practice, Veterans Affairs, ENT, or hospital). Finally, we only evaluated Internet-based delivery of hearing aid follow-up services using a single manufacturer's technology. Hearing aid user outcomes and audiologist opinions might differ based on manufacturer smart device applications in terms of usability, features, and connectivity.
Conclusions
Although telehealth audiology service delivery is readily available and studies suggest that it is an efficacious intervention (Angley et al., 2017; Campos & Ferrari, 2012; Tao et al., 2018), there remains a critical gap in the current evidence as to whether or not comprehensive hearing intervention can be feasibly and effectively delivered using telehealth services and if this mode of delivery will result in similar communication or quality of life improvements seen for standard-of-care, in-office services. Considering the relatively low uptake of HHC among older adults who could stand to benefit from a comprehensive hearing intervention and the potential for telehealth audiology services to make HHC more accessible, particularly for older adults, there is a need for systematic development of potentially efficacious service delivery models.
Given that we had been successful in the development and implementation of the manualized, comprehensive ACHIEVE Hearing Intervention (Sanchez et al., 2020) to provide best-practices HHC to older adults at multiple clinical sites, we believed that a logical next step was to determine the feasibility of leveraging telehealth technologies to develop a streamlined hybrid service delivery model. This work was done in two phases, with the first phase involving surveying seven experienced ACHIEVE audiologists to inform the development of the streamlined hybrid ACHIEVE Hearing Intervention approach; the feasibility study demonstrated that the expected subjective and objective outcomes were attainable in a small group of older individuals. Although further research will be necessary in a larger scale, controlled studies of the comparative effectiveness of a hybrid model versus a conventional in-person office service delivery model, the feasibility work reported here was an important first step in the development of evidence-based HHC service delivery options.
Author Contributions
Michelle L. Arnold: Conceptualization (Lead), Data curation (Supporting), Investigation (Lead), Project administration (Lead), Writing – original draft (Lead), Writing – review & editing (Lead). Breanne R. Schwartz: Conceptualization (Supporting), Data curation (Equal), Investigation (Supporting), Project administration (Supporting), Writing – original draft (Supporting). Haley Neil: Conceptualization (Supporting), Data curation (Supporting), Investigation (Supporting), Project administration (Equal), Writing – original draft (Supporting), Writing – review & editing (Supporting). Theresa H. Chisolm: Conceptualization (Supporting), Funding acquisition (Lead), Methodology (Equal), Resources (Equal), Supervision (Equal), Writing – original draft (Supporting), Writing – review & editing (Supporting). Victoria A. Sanchez: Conceptualization (Equal), Data curation (Equal), Investigation (Equal), Methodology (Equal), Project administration (Lead), Resources (Equal), Writing – original draft (Supporting), Writing – review & editing (Supporting).
Acknowledgments
Portions of this work were supported by National Institutes of Health/National Institute on Aging (R01AG055426). Hearing aids and related materials were provided at no cost to the researchers or the participants from Phonak LLC; however, the sponsoring manufacturer did not participate in the design, data collection or analysis, nor the reporting within this article. Portions of this work were presented at the American Auditory Society, 2020, Scottsdale, Arizona; the American Academy of Audiology, 2020, In-Person Session Cancelled (presented online); the University of South Florida Health Research Day, 2020, Tampa Florida; and Internet & Audiology Meeting, 2021. The authors give special recognition for significant contributions to the study, including help with data collection, entry, and management: Taylor Nye, Morgan Oktela, and Megan Tilley. The authors also give special recognition to the Aging and Cognitive Health Evaluation in Elders audiologists for their survey responses and input: Sarah Faucette, Laura Sherry, Elizabeth Anderson, Kerry Witherell, Kate Teece, Kaila Higuchi, and Jaime Hampton.
Funding Statement
Portions of this work were supported by National Institutes of Health/National Institute on Aging (R01AG055426). Hearing aids and related materials were provided at no cost to the researchers or the participants from Phonak LLC; however, the sponsoring manufacturer did not participate in the design, data collection or analysis, nor the reporting within this article. Portions of this work were presented at the American Auditory Society, 2020, Scottsdale, Arizona; the American Academy of Audiology, 2020, In-Person Session Cancelled (presented online); the University of South Florida Health Research Day, 2020, Tampa Florida; and Internet & Audiology Meeting, 2021. The authors give special recognition for significant contributions to the study, including help with data collection, entry, and management: Taylor Nye, Morgan Oktela, and Megan Tilley. The authors also give special recognition to the Aging and Cognitive Health Evaluation in Elders audiologists for their survey responses and input: Sarah Faucette, Laura Sherry, Elizabeth Anderson, Kerry Witherell, Kate Teece, Kaila Higuchi, and Jaime Hampton.
References
- American Medical Group Association. (n.d.). Vist-Specific Satisfaction Questionnaire (VSQ-9). Retrieved May 15, 2019, from https://www.rand.org/health-care/surveys_tools/vsq9.html
- American Speech-Language-Hearing Association. (1997). Guidelines for audiologic screening. http://asha.org/policy
- Angley, G. P. , Schnittker, J. A. , & Tharpe, A. M. (2017). Remote hearing aid support: The next frontier. Journal of the American Academy of Audiology, 28(10), 893–900. https://doi.org/10.3766/jaaa.16093 [DOI] [PubMed] [Google Scholar]
- Arnold, M. L. , Oree, P. , Sanchez, V. , Reed, N. S. , & Chisolm, T. H. (2019). Development and formative assessment of the Hearing Loss Toolkit for Self-Management. Seminars in Hearing, 40(1), 49–67. https://doi.org/10.1055/s-0038-1676783 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnett, M. , Hixon, B. , Okwiri, N. , Irungu, C. , Ayugi, J. , Thompson, R. , Shinn, J. B. , & Bush, M. L. (2017). Factors involved in access and utilization of adult hearing healthcare: A systematic review. The Laryngoscope, 127(5), 1187–1194. https://doi.org/10.1002/lary.26234 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calabrèse, A. , Cheong, A. M. Y. , Cheung, S.-H. , He, Y. , Kwon, M. , Mansfield, S. , Subramanian, A. , Yu, D. , & Legge, G. E. (2016). Baseline MNREAD measures for normally sighted subjects from childhood to old age. Investigative Ophthalmology and Visual Science, 57(8), 3836–3843. https://doi.org/10.1167/iovs.16-19580 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campos, P. D. , & Ferrari, D. V. (2012). Teleaudiology: Evaluation of teleconsultation efficacy for hearing aid fitting. Jornal da Sociedade Brasileira de Fonoaudiologica, 24(4), 301–308. https://doi.org/10.1590/S2179-64912012000400003 [DOI] [PubMed] [Google Scholar]
- Carhart, R. , & Jerger, J. F. (1959). Preferred method for clinical determination of pure-tone thresholds. Journal of Speech and Hearing Disorders, 24(4), 330–345. https://doi.org/10.1044/jshd.2404.330 [Google Scholar]
- Chandra, N. , & Searchfield, G. D. (2016). Perceptions toward Internet-based delivery of hearing aids among older hearing-impaired adults. International Journal of Audiology, 27(6), 441–457. https://doi.org/10.3766/jaaa.15058 [DOI] [PubMed] [Google Scholar]
- Convery, E. , McLelland, M. , & Groth, J. (2020). A smartphone app to facilitate remote patient–provider communication in hearing health care: Usability and effect on hearing aid outcomes. Telemedicine and e-Health, 26(6), 798–804. https://doi.org/10.1089/tmj.2019.0109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cox, R. M. , & Alexander, G. C. (1995). The Abbreviated Profile of Hearing Aid Benefit. Ear and Hearing, 16(2), 176–186. https://doi.org/10.1097/00003446-199504000-00005 [DOI] [PubMed] [Google Scholar]
- Cox, R. M. , & Alexander, G. C. (2002). The International Outcome Inventory for Hearing Aids (IOI-HA): Psychometric properties of the English version [El Inventario International de Resultados para Auxiliares Auditivos (IOI-HA): Propiedades psicometricas de la version en ingles]. International Journal of Audiology, 41(1), 30–35. https://doi.org/10.3109/14992020209101309 [DOI] [PubMed] [Google Scholar]
- Damschroder, L. J. , Aron, D. C. , Keith, R. E. , Kirsh, S. R. , Alexander, J. A. , & Lowert, J. C. (2009). Fostering implementation of health services research findings into practice: A consolidated framework for advancing implementation science. Implementation Science, 4, 50. https://doi.org/10.1186/1748-5908-4-50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis, F. D. (1986). A technology acceptance model for empirically testing new end-user information systems: Theory and results. MIT Libraries. http://hdl.handle.net/1721.1/15192
- Deal, J. A. , Goman, A. M. , Albert, M. S. , Arnold, M. L. , Burgard, S. , Chisolm, T. H. , Couper, D. , Glynn, N. W. , Gmelin, T. , Hayden, K. M. , Mosley, T. , Pankow, J. S. , Reed, N. S. , Sanchez, V. , Sharrett, A. R. , Thomas, S. D. , Coresh, J. , & Lin, F. R. (2018). Hearing treatment for reducing cognitive decline: Design and methods of the Aging and Cognitive Health Evaluation in Elders randomized controlled trial. Alzheimer's & Dementia: Diagnosis, Assessment, & Disease Monitoring, 4(1), 499–507. https://doi.org/10.1016/j.trci.2018.08.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dillon, H. , James, A. , & Ginis, J. (1997). Client Oriented Scale of Improvement (COSI) and its relationship to several other measures of benefit and satisfaction provided by hearing aids. Journal of the American Academy of Audiology, 8(1), 27–43. [PubMed] [Google Scholar]
- Folstein, M. F. , Folstein, S. E. , & McHugh, P. R. (1973). “Mini-mental state”: A practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research, 12(3), 189–198. https://doi.org/10.1016/0022-3956(75)90026-6 [DOI] [PubMed] [Google Scholar]
- Garstecki, D. S. , & Erler, S. F. (1998). Hearing loss, control, and demographic factors influencing hearing aid use among older adults. Journal of Speech, Language, and Hearing Research, 41(3), 527–537. https://doi.org/10.1044/jslhr.4103.527 [DOI] [PubMed] [Google Scholar]
- Gladden, C. , Beck, L. , & Chandler, D. (2015). Tele-audiology: Expanding access to hearing care and enhancing patient connectivity. Journal of the American Academy of Audiology, 26(9), 792–799. https://doi.org/10.3766/jaaa.14107 [DOI] [PubMed] [Google Scholar]
- Goldberg, E. M. , Jiménez, F. N. , Chen, K. , Davoodi, N. M. , Li, M. , Strauss, D. H. , Zou, M. , Guthrie, K. , & Merchant, R. C. (2021). Telehealth was beneficial during COVID-19 for older Americans: A qualitative study with physicians. Journal of the American Geriatrics Society, 69(11), 3034–3043. https://doi.org/10.1111/jgs.17370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldstein, N. E. S. , Kemp, K. A. , Leff, S. S. , & Lochman, J. E. (2012). Guidelines for adapting manualized interventions for new target populations: A step-wise approach using anger management as a model. Clinical Psychologist, 19(4), 385–401. https://doi.org/10.1111/cpsp.12011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goman, A. M. , Reed, N. S. , & Lin, F. R. (2017). Addressing estimated hearing loss in adults in 2060. JAMA Otolaryngology—Head & Neck Surgery, 143(7), 733–734. https://doi.org/10.1001/jamaoto.2016.4642 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gopinath, B. , Schneider, J. , Hartley, D. , Teber, E. , McMahon, C. M. , Leeder, S. R. , & Mitchell, P. (2011). Incidence and predictors of hearing aid use and ownership among older adults with hearing loss. Annals of Epidemiology, 21(7), 497–506. https://doi.org/10.1016/j.annepidem.2011.03.005 [DOI] [PubMed] [Google Scholar]
- Hantke, N. , Lajoy, M. , Gould, C. E. , Magwene, E. M. , Sordahl, J. , Hirst, R. , & O'Hara, R. (2020). Patient satisfaction with geriatric psychiatry services via video teleconference. The American Journal of Geriatric Psychiatry, 28(4), 491–494. https://doi.org/10.1016/j.jagp.2019.08.020 [DOI] [PubMed] [Google Scholar]
- Henshaw, H. , Clark, D. P. A. , Kang, S. , & Ferguson, M. A. (2012). Computer skills and Internet use in adults aged 50–74 years: Influence of hearing difficulties. Journal of Medical Internet Research, 14(4), e113. https://doi.org/10.2196/jmir.2036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hurley, R. M. , & Sells, J. P. (2003). An abbreviated word recognition protocol based on item difficulty. Ear and Hearing, 24(2), 111–118. https://doi.org/10.1097/01.AUD.0000058113.56906.0D [DOI] [PubMed] [Google Scholar]
- Keidser, G. , Dillon, H. , Flax, M. , Ching, T. , & Brewer, S. (2011). The NAL-NL2 prescription procedure. Audiology Research, 1(1), 88–90. https://doi.org/10.4081/audiores.2011.e24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keidser, G. , O'Brian, A. , Carter, L. , McLelland, M. , & Yeend, I. (2008). Variation in preferred gain with experience for hearing-aid users. International Journal of Audiology, 47(10), 621–635. https://doi.org/10.1080/14992020802178722 [DOI] [PubMed] [Google Scholar]
- Killion, M. C. , Niquette, P. A. , Gudmundsen, G. I. , Revit, L. J. , & Banarjee, S. (2003). Development of a Quick Speech-in-Noise Test for measuring signal-to-noise ratio loss in normal-hearing and hearing-impaired listeners. The Journal of the Acoustical Society of America, 116(4), 2395–2405. https://doi.org/10.1121/1.1784440 [DOI] [PubMed] [Google Scholar]
- King, W. R. , & He, J. (2006). A meta-analysis of the technology acceptance model. Information & Management, 43(6), 740–755. https://doi.org/10.1016/j.im.2006.05.003 [Google Scholar]
- Knudsen, L. V. , Öberg, M. , Nielsen, K. , Naylor, G. , & Kramer, S. E. (2010). Factors influencing help seeking, hearing aid uptake, hearing aid use and satisfaction with hearing aids: A review of the literature. Trends in Amplification, 14(3), 127–154. https://doi.org/10.1177/1084713810385712 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lichtenstein, M. J. , Bess, F. H. , & Logan, S. A. (1988). Diagnostic performance of the Hearing Handicap Inventory for the Elderly (Screening Version) against differing definitions of hearing loss. Ear and Hearing, 9(4), 208–211. https://doi.org/10.1097/00003446-198808000-00006 [DOI] [PubMed] [Google Scholar]
- McCreery, R. W. , Bentler, R. A. , & Roush, P. (2013). Characteristics of hearing aid fittings in infants and young children. Ear and Hearing, 34(6), 701–710. https://doi.org/10.1097/AUD.0b013e31828f1033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Academies of Sciences Engineering and Medicine. (2016). Hearing health care for adults: Priorities for improving access and affordability. http://www.nap.edu/read/23446/chapter/1#ii [PubMed]
- Pross, S. E. , Bourne, A. L. , & Cheung, S. W. (2016). TeleAudiology in the Veterans Health Administration. Otology & Neurotology, 37(7), 847–850. https://doi.org/10.1097/MAO.0000000000001058 [DOI] [PubMed] [Google Scholar]
- Ravi, R. , Gunjawate, D. R. , Yerraguntla, K. , & Driscoll, C. (2018). Knowledge and perceptions of teleaudiology among audiologists: A systematic review. Journal of Audiology and Otology, 22(3), 120–127. https://doi.org/10.7874/jao.2017.00353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanchez, V. A. , Arnold, M. L. , Reed, N. S. , Oree, P. H. , Matthews, C. R. , Eddins, A. C. , Lin, F. R. , & Chisolm, T. H. (2020). The hearing intervention for the Aging and Cognitive Health Evaluation in Elders randomized controlled trial: Manualization and feasibility study. Ear and Hearing, 41(5), 1333–1348. https://doi.org/10.1097/AUD.0000000000000858 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tao, K. F. M. , Brennan-Jones, C. G. , Capobianco-Fava, D. M. , Jayakody, D. M. P. , Friedland, P. L. , Swanepoel, D. W. , & Eikelboom, R. H. (2018). Teleaudiology services for rehabilitation with hearing aids in adults: A systematic review. Journal of Speech, Language, and Hearing Research, 61(7), 1831–1849. https://doi.org/10.1044/2018_JSLHR-H-16-0397 [DOI] [PubMed] [Google Scholar]
- Thorén, E. S. , Öberg, M. , Wänström, G. , Andersson, G. , & Lunner, T. (2013). Internet access and use in adults with hearing loss. Journal of Medical Internet Research, 15(5), e91. https://doi.org/10.2196/jmir.2221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Totten, A. M. , Womack, D. M. , Eden, K. B. , McDonagh, M. S. , Griffin, J. C. , Grusing, S. , & Hersh, W. R. (2016). Telehealth: Mapping the evidence for patient outcomes from systematic reviews. https://www.ncbi.nlm.nih.gov/books/NBK379320/ [PubMed]
- Venail, F. , Picot, M. C. , Marin, G. , Falinower, S. , Samson, J. , Cizeron, G. , Balcon, M. , Blanc, D. , Bricaud, J. , Lorenzi, A. , Ceccato, J.-C. , & Puel, J.-L. (2019). Speech perception, real-ear measurements and self-perceived hearing impairment after remote and face-to-face programming of hearing aids: A randomized single-blind agreement study. Journal of Telemedicine and Telecare, 27(7), 409–423. https://doi.org/10.1177/1357633X19883543 [DOI] [PubMed] [Google Scholar]
- Ventry, I. M. , & Weinstein, B. E. (1983). Identification of elderly people with hearing problems. Asha, 25(7), 37–42. [PubMed] [Google Scholar]
- Wade, R. , Cartwright, C. , & Shaw, K. (2012). Factors relating to home telehealth acceptance and usage compliance. Risk Management and Healthcare Policy, 5, 25–33. https://doi.org/10.2147/RMHP.S30204 [DOI] [PMC free article] [PubMed] [Google Scholar]