Abstract
While radiological imaging is presented as two-dimensional images either on radiography or cross-sectional imaging, it is important for interpreters to understand three-dimensional anatomy and pathology. We hypothesized that virtual reality (VR) may serve as an engaging and effective way for trainees to learn to extrapolate from two-dimensional images to an understanding of these three-dimensional structures. We created a Google Cardboard Virtual Reality application that depicts intracranial vasculature and aneurysms. We then recruited 12 medical students to voluntarily participate in our study. The performance of the students in identifying intracranial aneurysms before and after the virtual reality training was evaluated and compared to a control group. While the experimental group’s performance in correctly identifying aneurysms after virtual reality educational intervention was better than the control’s (experimental increased by 5.3%, control decreased by 2.1%), the difference was not statistically significant (p-value of 0.06). Significantly, survey data from the medical students was very positive with students noting they preferred the immersive virtual reality training over conventional education and believed that VR would be a helpful educational tool for them in the future. We believe virtual reality can serve as an important tool to help radiology trainees better understand three-dimensional anatomy and pathology.
Keywords: Virtual Reality, Cerebral Aneurysms, Perception, CT Angiography
Introduction
Radiologists interpret imaging studies which present three-dimensional (3D) structures in two dimensions. A mastery of the full 3D anatomy is critical in understanding and correctly identifying imaging pathology, especially when they are shown in two-dimensional (2D) presentations [1–4]. The process of developing this anatomical proficiency is often difficult and time-consuming for junior trainees, taking years of arduous training and many various types of learning resources. It is imperative that methods of teaching 3D anatomy are developed in a simple, engaging, and intuitive fashion.
With the increasing presence and accessibility of rendering software and virtual reality (VR) [5, 6], 3D reconstructions are being increasingly used in clinical practice [7]. The use of virtual reality for clinical practice and educational purposes is newer with few medically validated software programs; however, existing virtual reality software has shown positive results, with users finding virtuality helpful and immersive in understanding anatomy [4, 8, 9]. There have been some forays into virtual reality for intracranial aneurysms, though these have largely been for surgical approach with less emphasis on identification on routine CT angiography [10, 11].
We hypothesize that virtual reality modules can improve trainee understanding of complex three-dimensional anatomy and corresponding pathology. For our pilot study, we used intracranial vasculature and aneurysms. We developed a virtual reality app for Google Cardboard [12] named VR Aneurysms and evaluated how it affected medical student performance in identifying aneurysms on cerebral CT angiography.
Methods
Developing the Virtual Reality App
This study was approved by the IRB at our institution. Using Materialise software [13], the three-dimensional anatomy of the head was reconstructed from CT angiography examinations. Intracranial arterial vasculature was isolated and segmented away from the other structures within the head. These structures were exported as object files (.obj) and imported into the Blender [14] graphics software where they were colorized, textured, smoothed, and shaded. Then, using tools from Blender, alternate object files were created containing realistic but simulated saccular aneurysms involving the anterior communicating artery, posterior communicating artery, carotid terminus, middle cerebral artery bifurcation, and basilar tip.
All of these object files were uploaded to Unity [15], a game development software. Using Unity and C# programming language, the major intracranial arteries and aneurysms were labeled by color and with a brief descriptive tag. This software was then exported as a Google Cardboard virtual reality app and uploaded publicly to the Android marketplace. Google Cardboard was chosen due to its inexpensiveness and portability. Google Cardboard is an affordable handheld device into which a smartphone can be inserted, and a virtual reality app can be run. While the software can be run on higher-end virtual reality devices, these devices require high-end computers as well as expensive and large virtual reality systems, which may be of less general utility in many educational settings.
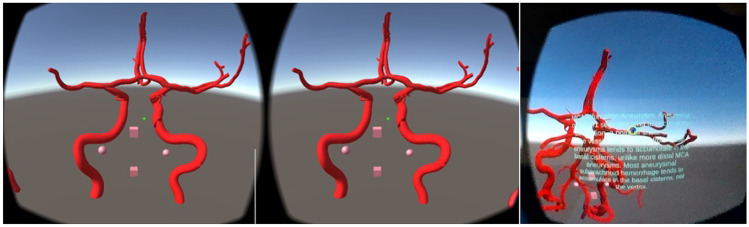
Trainees used either their own android phones or phones provided to them in conjunction with provided Google Cardboard devices to interact with the virtual reality app. Trainees were instructed to identify vascular structures and aneurysms from a checklist (Fig. 1) with proctor guidance (Fig. 2).
Fig. 1.
Example image of the VR android app Intracranial Aneurysms
Fig. 2.
Medical student virtual reality training with VR Aneurysms
Evaluating Performance in Identifying Aneurysms
Sixteen CT angiography exams of the head were collected and exported as DICOMs, 8 were normal exams, and 8 contained a single saccular aneurysm. Aneurysm cases were hand selected for their simple and relatively obvious appearance for a trainee. Aneurysm sac sizes ranged from 4 to 7 mm. The aneurysms included involved the anterior communicating artery, posterior communicating artery, middle cerebral artery bifurcation, posterior communicating artery, basilar tip, and V4 segment of the vertebral artery. The 16 exams were divided into two case sets with 8 exams each. Each case set contained 4 normal exams and 4 exams with aneurysms.
Twelve medical students voluntarily participated in our study. Six students were assigned to the control and 6 to the experimental group. Using the RadSimPE software [16], trainees were able to scroll through the images and either mark the location of an aneurysm or indicate there was not an aneurysm. Both the experimental and control groups underwent the first case set after which the experimental group underwent virtual reality training with VR aneurysms, while the control group was provided with a review article on cerebral aneurysms as an attentional control. Afterwards, both groups underwent case set 2. After the conclusion of the study, both the experimental group and control group were allowed to use the virtual reality training as well as read the review article.
Statistics
Performance in case set 2 was compared to case set 1 in both the experimental and control groups. The percentage of accurate localization or accurate declaration of no aneurysms was compared between the case sets using a one-tailed non-parametric Mann–Whitney U test [17].
Additionally, survey data (Table 1) was collected to evaluate the users’ experiences using a Likert response format, with 1 generally representing a poor experience, 3 a neutral experience, and 5 representing a good experience. Survey scores were evaluated by comparison of the mean values to the theoretical neutral mean of 3 using a one-tailed non-parametric Mann–Whitney U test. This method of analyzing the Likert-like response format was chosen due to the relatively low population size [18]. An α of 0.05 was chosen as the threshold for statistical significance.
Table 1.
Worksheet given to trainees to guide them through VR aneurysms software
| I. Vasculature | |
|---|---|
| a. | Vertebral artery (V4 segment) |
| b. | Posterior inferior cerebellar artery (PICA) |
| c. | Basilar artery |
| d. | Anterior inferior cerebellar artery (AICA) |
| e. | Superior cerebellar artery |
| f. | Posterior cerebral artery (PCA) |
| g. | Posterior communicating artery (PComm) |
| h. | Internal carotid artery (ICA) |
| i. | Middle cerebral artery (MCA) |
| j. | Anterior cerebral artery (ACA) |
| k. | Anterior communicating artery (AComm) |
| l. | Ophthalmic artery |
| m. | Orbitofrontal artery |
| II. Aneurysms | |
|---|---|
| a. | Basilar artery aneurysm |
| b. | Posterior communicating artery aneurysm |
| c. | Internal carotid artery terminus aneurysm |
| d. | Middle cerebral artery bifurcation aneurysm |
| e. | Anterior communicating artery aneurysm |
Results
The control group averaged correct aneurysm or lack of aneurysm localization in 18.8% of cases before intervention and 16.7% after intervention. The experimental group averaged 28.0% before intervention and 33.3% after intervention. The experimental group’s performance in case set 2 compared to case set 1 improved by 5.3%, while the control group decreased by 2.1%. The overall difference between the two groups’ performances was 7.4% with a p-value of 0.06 between the experimental and control groups.
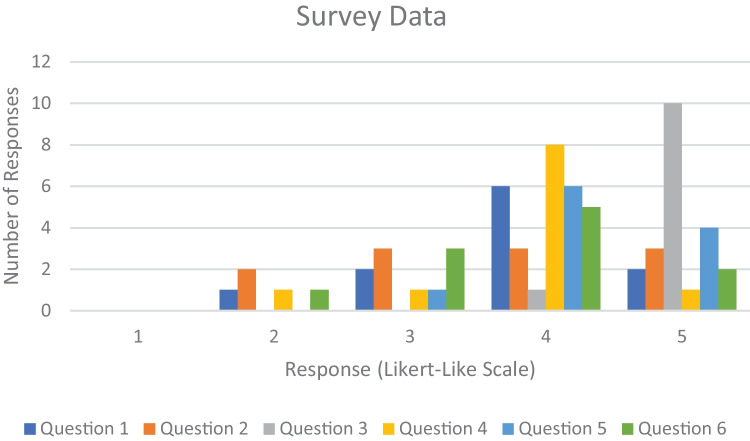
Except for survey question two (about trainee confidence after virtual reality), survey data was all statistically significantly positive with p-values below 0.05, (Table 2, Fig. 3). Trainees positively responded to the novel nature of virtual reality and were optimistic about its ability to teach complex anatomy and imaging pathology.
Table 2.
Survey questions given to participants
| Question | p-value |
|---|---|
| 1. The virtual reality module was helpful for learning the skills needed to identify cerebral vasculature and cerebral aneurysms | 0.006 |
| 2. This virtual reality module made me more confident in identifying cerebral aneurysms | 0.079 |
| 3. In my prior course work and self-study, I have not experienced the equivalent of a virtual reality module for how to identify a cerebral aneurysm | 0.00004 |
| 4. Compared with conventional learning materials (including printed and/or electronic textbooks and case files), the virtual reality module provided a more effective way to develop the skills needed to identify cerebral aneurysms | 0.00212 |
| 5. I think virtual reality modules would be a helpful way to learn about additional topics in radiology | 0.00017 |
| 6. Participation in this study was an overall positive experience | 0.01659 |
Fig. 3.
Survey responses. Please see Table 1 for a list of survey questions
Discussion
On survey data, the trainees all felt that the virtual reality educational experience was a valuable educational technique and viewed their experience as positive. Subjective verbal feedback demonstrated excitement, enthusiasm, and optimism about the potential for virtual reality in their future education.
Our data showed an improvement in the virtual reality experimental group compared to the control group, though not statistically significant. One of the factors that may have played into this includes a low sample size, largely influenced by COVID-19 pandemic restrictions on educational activities. Additionally, our subjects consisted of medical students who were largely inexperienced with reading cross-sectional imaging and required extra time during the assessment. While survey data did show that trainees overall felt improved confidence in identifying aneurysms, this was not statistically significant. We hope to expand this module to radiology trainees across multiple institutions to assess the role of VR education in novice cross-sectional and experienced cross-sectional radiology physicians.
Three-dimensional reconstruction provides an alternative way of understanding complex 3D anatomy for trainees, radiologists, and clinicians alike. Several 3D reconstruction tools exist such as volume rendering [19], shaded surface rendering [20], and cinematic rendering [21]. Volume-rendered techniques assign color and transparency to objects within the scan data based on Hounsfield units or MR intensity units. This allows color and transparency encoding of various tissues: bones are beige, muscles are red, and vessels are white. Shaded surface rendering techniques in 2D create a surface map of the object with limited shading or occlusion without transparency, useful for evaluating fine surface detail, such as bone fractures. Cinematic rendering uses high computational power available in modern GPUs to take the digital model and virtually light surface textures by bouncing billions of virtual photons off the virtual surface, creating lifelike or photorealistic textures and internal reflections [22].
Virtual reality rendering engine quality falls between the quality of 2D volume rendering and offline cinematic rendering [23]. The advantage of virtual reality is the use of stereoscopic vision to create a volume render pair for both the left and right eye. The same shading and transparency that can be performed for volume rendering are essentially created for both eyes and projected within the headset. Virtual reality provides an additional tool for 3D visualization, and compared to reconstructions on a computer screen, VR reconstructions may result in a more immersive and interactive environment. Not only can the user rotate the model, but they can approach or walk around the teaching object in virtual space. Users may also interact with the data, such as grasping or zooming in, and further immerse themselves in a simulated surgical view of the aneurysm.
Virtual reality is much more available now than previously, and users can access virtual reality through their smartphones. We intentionally chose a low-cost virtual reality environment to make the educational experience more distributable to any user with a modern phone. Results of our survey suggest that virtual reality provides an interactive and engaging way for trainees to understand complex anatomy and pathology. Virtual reality software provides the opportunity for annotated anatomy and pathology as well as comparison to imaging studies such as radiography, CT, and MRI.
Compared to preexisting virtual reality software programs, our software has a greater emphasis on anatomy as it relates to imaging and focuses on diagnosis rather than on anatomy visualization for treatment alone [8, 10, 11]. Additionally, unlike most surgical-focused virtual reality studies [24], our study includes both normal virtual angiography for educational intervention and normal CT angiography exams for assessment as well as virtual aneurysms and CT angiography with aneurysms. The presence of normal exams is more relevant for radiologists who interact with normal exams far more often than aneurysms and need to understand normal anatomy to correctly diagnose pathologic lesions.
Our study has several limitations. One of the limitations is the sample size used. The sample size was limited by the pandemic; the inherent complexity of setting up, administering, and proctoring with virtual reality devices; and the amount of time trainees require to evaluate aneurysms on CT angiography. That said, perception studies often have similar sample sizes [16]. Additionally, because of the length of time required to view the CT angiography exams, only 8 different aneurysms could be examined for a total of 16 cases. Because the trainees in our study were medical students, they required longer times to both view the virtual reality as well as review the CT images. If more experienced radiologists were recruited, study time likely would have been shorter allowing a larger sample size; however, we believe that imaging-inexperienced trainees are the ones that can benefit the most from virtual reality training as they have the least anatomic experience.
One of the limitations of virtual reality as a learning platform is that some users develop motion sickness-like symptoms. This can vary based on the refresh rate of the VR device. Some users may lack stereoscopic vision, limiting the immersive experience. Additionally, some users do not respond well to virtual reality and headsets and find the technology excessive or cumbersome. Additionally, Google Cardboard, the most economical option for virtual reality, has since been discontinued, and while stock is still available, virtual reality options in the future will likely be more expensive. Despite virtual reality not being the optimal tool for some, based on our survey data, we hope it will be useful and engaging to most students. Additionally, since virtual reality software has not been medically validated, caution is recommended in its use in clinical care, and virtual reality may be better utilized for educational purposes.
Virtual reality education can be expanded to include all parts of the body, especially areas with complex anatomy such as the spine, joints, cardiac anatomy, and mesenteric/splanchnic circulation. Creating an interactive virtual reality atlas may help students understand 3D anatomy and pathology and translate to improved perceptive and diagnostic performance on imaging.
Conclusions
While there was more improvement in the experimental group that underwent virtual reality training compared to the control group, it was not statistically significant, perhaps due to the low sample size. However, trainee survey and informal feedback were overwhelmingly positive with trainees believing virtual reality could be very helpful in their future education. We believe that virtual reality has an especially important role in teaching the anatomy and pathology of complex three-dimensional structures in imaging.
Acknowledgements
We would like to thank all the trainees that participated in our study.
This educational study was reviewed by our local IRB.
Data Availability
The data that support the findings of this study are available from the corresponding author, SB, upon reasonable request.
Declarations
Conflict of Interest
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Murakami T, Tajika Y, Ueno H, et al. An integrated teaching method of gross anatomy and computed tomography radiology. Anatomical sciences education. 2014;7(6):438–449. doi: 10.1002/ase.1430. [DOI] [PubMed] [Google Scholar]
- 2.Pommert A, Höhne KH, Burmester E, et al. Computer-Based anatomy: A prerequisite for Computer-Assisted radiology and surgery1. Academic Radiology. 2006;13(1):104–112. doi: 10.1016/j.acra.2005.08.034. [DOI] [PubMed] [Google Scholar]
- 3.Park MS, Brock A, Mortimer V, Taussky P, Couldwell WT, Quigley E. GoPro Hero cameras for creation of a three-dimensional, educational, neurointerventional video. Journal of digital imaging. 2017;30(5):561–565. doi: 10.1007/s10278-017-9948-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bouaoud J, El Beheiry M, Jablon E, et al. DIVA, a 3D virtual reality platform, improves undergraduate craniofacial trauma education. Journal of Stomatology, Oral and Maxillofacial Surgery. 2021;122(4):367–371. doi: 10.1016/j.jormas.2020.09.009. [DOI] [PubMed] [Google Scholar]
- 5.Evaluation of interaction techniques for a virtual reality reading room in diagnostic radiology. Proceedings of the 31st Annual ACM Symposium on User Interface Software and Technology; 2018.
- 6.Douglas DB, Venets D, Wilke C, et al. Augmented reality and virtual reality: Initial successes in diagnostic radiology. State of the art virtual reality and augmented reality knowhow 2018
- 7.Wicky S, Blaser P, Blanc C, Leyvraz P, Schnyder P, Meuli R. Comparison between standard radiography and spiral CT with 3D reconstruction in the evaluation, classification and management of tibial plateau fractures. European radiology. 2000;10(8):1227–1232. doi: 10.1007/s003300000326. [DOI] [PubMed] [Google Scholar]
- 8.Rieger M, Gabl M, Gruber H, Jaschke WR, Mallouhi A. CT virtual reality in the preoperative workup of malunited distal radius fractures: preliminary results. European radiology. 2005;15(4):792–797. doi: 10.1007/s00330-004-2353-x. [DOI] [PubMed] [Google Scholar]
- 9.Immersive virtual reality for visualization of abdominal CT. Medical Imaging 2013: Image Perception, Observer Performance, and Technology Assessment; 2013. SPIE.
- 10.Alaraj A, Luciano CJ, Bailey DP, et al. Virtual reality cerebral aneurysm clipping simulation with real-time haptic feedback. Operative Neurosurgery. 2015;11(1):52–58. doi: 10.1227/NEU.0000000000000583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Li Z, Huo G, Feng Y, Ma Z. Application of virtual reality based on 3D-CTA in intracranial aneurysm surgery. Journal of Healthcare Engineering 2021;2021 [DOI] [PMC free article] [PubMed]
- 12.Google. Google Cardboard.
- 13.Materialise [program]. Leuven, Belgium.
- 14.Blender [program], 2021.
- 15.Unity [program], 2021.
- 16.Banerjee S, Auffermann WF. RadSimPE—a Radiology Workstation Simulator for Perceptual Education. Journal of Digital Imaging. 2021;34(4):1059–1066. doi: 10.1007/s10278-021-00489-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.McKnight PE, Najab J. Mann‐Whitney U Test. The Corsini encyclopedia of psychology 2010:1–1
- 18.Sullivan GM, Artino AR., Jr Analyzing and interpreting data from Likert-type scales. Journal of graduate medical education. 2013;5(4):541–542. doi: 10.4300/JGME-5-4-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cavalcanti M, Rocha S, Vannier M. Craniofacial measurements based on 3D-CT volume rendering: implications for clinical applications. Dentomaxillofacial Radiology. 2004;33(3):170–176. doi: 10.1259/dmfr/13603271. [DOI] [PubMed] [Google Scholar]
- 20.Perandini S, Faccioli N, Zaccarella A, Re T, Mucelli RP. The diagnostic contribution of CT volumetric rendering techniques in routine practice. Indian Journal of Radiology and Imaging. 2010;20(02):92–97. doi: 10.4103/0971-3026.63043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rowe SP, Fritz J, Fishman EK. CT evaluation of musculoskeletal trauma: initial experience with cinematic rendering. Emergency radiology. 2018;25(1):93–101. doi: 10.1007/s10140-017-1553-z. [DOI] [PubMed] [Google Scholar]
- 22.Caton MT, Jr, Wiggins WF, Nunez D. Three-dimensional cinematic rendering to optimize visualization of cerebrovascular anatomy and disease in CT angiography. Journal of Neuroimaging. 2020;30(3):286–296. doi: 10.1111/jon.12697. [DOI] [PubMed] [Google Scholar]
- 23.Dappa E, Higashigaito K, Fornaro J, Leschka S, Wildermuth S, Alkadhi H. Cinematic rendering–an alternative to volume rendering for 3D computed tomography imaging. Insights into imaging. 2016;7(6):849–856. doi: 10.1007/s13244-016-0518-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Greuter L, De Rosa A, Cattin P, Croci DM, Soleman J, Guzman R. Randomized study comparing 3D virtual reality and conventional 2D on-screen teaching of cerebrovascular anatomy. Neurosurgical Focus. 2021;51(2):E18. doi: 10.3171/2021.5.FOCUS21212. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author, SB, upon reasonable request.