Abstract
Introduction
Studies show that physicians and medical trainees who identify as underrepresented in medicine or as women experience higher rates of microaggressions during patient encounters. We designed, implemented, and evaluated an active bystander training workshop focused on mitigating microaggressions using standardized patient (SP) methodology.
Methods
Internal medicine faculty members and chief residents led the workshop. Participants included 31 PGY 1 categorical and preliminary internal medicine residents. They participated in three case simulations with SPs involving microaggressions from patients toward a member of the health care team. Prior to the case simulations, a brief presentation outlined examples of microaggressions and reviewed the behavioral response framework WAKE (work with who you are, ask questions/make direct statements, involve key people, and employ distraction techniques). After each encounter, residents debriefed with an internal medicine faculty member and discussed questions related to each scenario.
Results
All 31 residents participated in the workshop and, before and after the activity, completed a survey that asked them to rank their agreement with statements via a Likert scale. Participants reported statistically significant improvement in recognizing microaggressions (12% reported increase, p = .002), the ability to respond to patients who exhibit microaggressions (23% reported increase, p < .001), and the ability to debrief with team members (20% reported increase, p < .001).
Discussion
SP simulations can be an effective teaching modality for microaggression response strategies during patient encounters. Additional studies are needed to further characterize the workshop's effect on other medical workforce trainees and retention of skills over time.
Keywords: Microaggression, Bystander Training, Anti-Racism, Bias, Case-Based Learning, Communication Skills, Diversity, Equity, Inclusion, Standardized Patient
Educational Objectives
By the end of this activity, learners will report improvement in their ability to:
-
1.
Identify microaggressions toward members of the health care team.
-
2.
Use WAKE (work with who you are, ask questions/make direct statements, involve key people, and employ distraction techniques) active bystander strategies to mitigate microaggressions in clinical encounters.
-
3.
Debrief with members of the health care team when microaggressions occur in clinical encounters.
Introduction
A diverse physician workforce is essential for optimizing patient care in the United States. Physicians who are underrepresented in medicine (URM) are more likely to choose primary care as their specialty and to care for groups that have been economically and socially marginalized.1 Studies have also demonstrated improved outcomes in myocardial infarctions among women2 when treated by women emergency room physicians and decreased mortality and readmission rates among hospitalized Medicare patients when under the care of women internists.3
Despite the contributions to patient care from physicians of diverse backgrounds, physicians and medical trainees who identify as URM, women, and other minoritized groups experience additional challenges in the medical profession. One factor is the minority tax, which is defined as the tax of extra responsibilities placed on URM faculty to facilitate institutional efforts to achieve diversity.4 URM faculty also spend more time in community work and caring for groups that have been economically and socially marginalized, which in turn may decrease time for scholarly activity and professional advancement in academic medicine.4 Women academic physicians also report higher rates of sexual harassment in the workplace5 and higher rates of maternal discrimination.6
URM and women faculty also report higher numbers of incidents of microaggressions during patient encounters.7,8 Microaggressions are defined as the everyday, subtle, intentional or unintentional behaviors that communicate some sort of bias toward historically marginalized groups.9 Multiple studies have demonstrated the negative effect of microaggressions on increased physician burnout, increased rates of depression, decreased academic performance, and decreased job satisfaction.8,10-12 URM and women physicians/trainees have expressed the need for institutional support in navigating microaggressions in the workplace and training environment.13 Those who witness microaggressions can play an important role in interrupting potentially hostile situations.14 Unfortunately, research on the bystander effect indicates that most people will fail to interrupt a microaggression for a variety of reasons, including a fear of getting involved in conflict, uncertainty regarding their own skills, and the belief that someone else is better equipped to respond.15-17
To combat these realities, numerous educational initiatives have been developed to assist medical trainees in navigating microaggressions and discrimination during patient encounters and other educational settings.18-20 Active bystander or upstander training programs have also been effective in teaching allies, accomplices, and advocates how to best respond in these critical moments. Initially, active bystander intervention programs emerged as a popular strategy to combat sexual assault and violence on college campuses by focusing on the behavior of students outside the victim/perpetrator role.21 Studies have shown decreased rates of sexual violence and other forms of interpersonal violence on campuses after implementation of such programs.22,23 Due to its success on college campuses, active bystander intervention is also being modified to address other forms of oppression, including microaggressions related to racism, sexism, and other forms of prejudice in the clinical learning environment.20,24,25
In conjunction with the success of other bystander intervention trainings in medical education, we designed, taught, and evaluated an active bystander training workshop for internal medicine residents utilizing standardized patient (SP) methodology. SP methodology uses actors to portray a particular role in order to allow learners to interact with and experience certain scenarios prior to similar interactions on the wards.26 SP methodology is supported by social learning theory, which allows the learner to begin to build skills in a more controlled, lower-stakes environment prior to needing to recall those skills in the less controlled environment of the wards and clinics, where mistakes can have safety ramifications.26 In addition, using SP methodology in conjunction with reflection and feedback allows for setting a foundation for expert performance that can then be built upon over time.26
To our knowledge, our curriculum is the first to use SP methodology for medical trainees to practice bystander strategies to mitigate microaggressions during patient encounters. We chose SP methodology as it gave learners the opportunity to face microaggressions in a controlled, low-stakes environment and to build compassion and empathy for constructive responses. The workshop provided participants with interactive, case-based simulations in which they utilized the behavioral response framework WAKE (work with who you are, ask questions/make direct statements, involve key people, and employ distraction techniques) to respond to microaggressions from patients.27
Methods
Curriculum Context
Through the support of the North Carolina American College of Physicians Educational Innovation Grant program, funding was awarded to the Wake Forest internal medicine residency program leadership to support the development of novel curricula focusing on microaggressions. The workshop described here was specifically designed for the Learning Health Systems (LHS) curriculum, a lecture series for internal medicine interns. Throughout the year, this lecture series focused on several important topics to help coach interns on effective communication skills and understanding of health systems, quality improvement, evidence-based medicine, leadership, and lifelong learning in medicine.
As part of the LHS curriculum, our workshop provided learners with important communication skills that could be used with patients and with other colleagues in the medical center. Our team of internal medicine faculty and program leadership collaborated with the Wake Forest Baptist Medical Center Office of Inclusion and Diversity to develop an active bystander training focused on internal medicine residents. This training built on a previous institution-wide project, WAKE active bystander training,27 which was initially developed in 2018 to empower members of the health care team to respond to incivility (low-intensity deviant behavior with ambiguous intent to harm the target in violation of workplace norms of mutual respect),28 microaggressions, and hostile behaviors in the workplace. The training and WAKE behavioral response framework were based on the evidence-based strategies of the Green Dot bystander intervention program, developed to decrease sexual assault and violence on college campuses.22 Institutional survey data collected from 2020 to 2022 showed that 96% of 676 participants at Wake Forest Baptist Medical Center reported feeling comfortable applying the WAKE active bystander strategies after the training (M. Lane-Brown, MPH, D. McIntosh, PhD, S. M. Evans, MA, unpublished data, September 19, 2022). We presented the acronym WAKE27 to help residents remember strategies to respond to incidents of microaggression, as outlined below:
-
•
W: Work with who you are. Reflect your power and/or privilege as a bystander. It is important to remember that you do not have to be a superhero to make a difference, just yourself. When determining how to respond to a microaggression, consider the following questions:
-
○
“What are my strengths?”
-
○
“What tools am I most comfortable using?”
-
○
“What common ground do I have with the other person involved?”
-
○
“What is my connection to the issue?”
-
○
-
•
A: Ask questions and/or make direct statements. Ask clarification questions or directly respond to the perpetrator.
-
○
Examples of asking questions include:
-
▪
“What do you mean by that?”
-
▪
“Do you think everybody in that group is like that or is there someone in that particular group you are thinking of?”
-
▪
-
○
Examples of direct statements include:
-
▪
“You know the truth is that [assumption, stereotype, label] makes me uncomfortable. Thanks for your understanding.”
-
▪
“You know, I was just reading about this, and I was surprised to find that ‘X’ is actually true.”
-
▪
-
○
-
•
K: Involve key people. Share the situation that made you uncomfortable with a supervisor, power broker, or someone with influence. You can get a key person involved in several different ways, including a direct conversation, but also through nonverbal cues such as eye contact or a gesture that indicates they need to do something. Examples of involving key people include:
-
○
Recruiting a colleague who you know will say something.
-
○
Expressing your concerns in an evaluation.
-
○
Documenting (when possible) the incident that you witnessed.
-
○
-
•
E: Employ distraction techniques. Change the subject. This deflection strategy does not directly address the issue; however, it is very effective if you are not sure how to best interrupt a microaggression. The distraction technique is very effective in stopping the microaggression and giving the offender a moment to recognize that their comments are unwelcome. Some examples of deploying a distraction include:
-
○
Interrupting the person speaking and redirecting to the task at hand.
-
○
Using body language, such as sighing deeply or shaking your head.
-
○
Humor, sarcasm, or just changing the subject to a completely different topic (“Did anyone see the game last night? It was really good!”) can be effective. Remember that if you are uncomfortable with the comments being made, others are too, and they will likely follow your lead (“I did see the game, it was great! Are you a fan?”).
-
○
Implementation and Logistics
Faculty members and chief residents in general internal medicine led the sessions, which involved three workshops executed on three different dates. Each session lasted 2.5 hours, with 10-12 PGY 1 internal medicine resident participants in each session. PGY 1 residents were required to attend the workshop but not required to complete a preassignment or review other preparation materials prior to the workshop.
We spent the first 30 minutes of the session administering a preactivity survey (Appendix A) and delivering a brief introductory presentation (Appendix B). The presentation began by outlining learning objectives and defining microaggressions. We reviewed the importance of mitigating microaggressions and how repeated microaggressions were associated with physician burnout, depression, decreased academic performance, and decreased job satisfaction. Subsequently, we presented the WAKE acronym as a potential framework to respond to microaggressions both in the moment and after the incident. In the didactic presentation, we used two example cases involving microaggressions, with implementation of WAKE active bystander strategies in those scenarios. We discussed these example scenarios with the residents without the use of SPs. Finally, we outlined the schedule for the SP encounters and debriefing sessions.
Appendix C describes logistical information, including props needed to prepare the simulation room for each patient encounter. We used a total of three cases; each case involved simulated patient encounters in which a patient expressed a microaggression toward the resident or a team member. Two resident participants were in each room at a time. We encouraged each resident to take the lead on a case at least once, while the other resident acted as a bystander. We did not prearrange the participants based on their demographic information or identity, as we did not want to single out residents based on their race, ethnicity, or gender. We provided patient background information on the door of each exam room, as outlined in Appendix D.
Although the primary objective was for learners to practice WAKE active bystander strategies in response to microaggression, the task of obtaining a history and physical was indicated on the door instructions of each case. Our goal was for the residents to treat the simulation as a regular clinical encounter without expecting a microaggression to occur at a certain time during their evaluation of the SP. Six rooms ran concurrently, with one SP in each room. Each case lasted up to 10 minutes. After each case concluded, the resident group received verbal feedback from the SPs and then went to a debriefing room with the faculty facilitator to debrief for 15 minutes prior to rotating to the next case.
We recruited faculty and chief residents with an interest in diversity, equity, and inclusion for the workshop. Prior to the session, the facilitators reviewed the introductory presentation (Appendix B), their assigned case (Appendix E), and associated debriefing questions with sample answers and points of discussion (Appendix F). During the workshop, each facilitator observed each resident group during each encounter, provided specific feedback to the resident group, and led the discussion questions after each case.
All sessions took place at the Wake Forest School of Medicine Center for Experiential and Applied Learning. Staff identified SPs based on their age range. We wrote the cases so that the SP could identify as a man or a woman. We trained a total of 17 SPs for this event (six SPs per session). Recruitment criteria and training methodology are outlined in Appendix G. Participating internal medicine faculty and the SP coordinator trained all SPs during a 1-hour session via WebEx. We reviewed all cases in detail during the training, and the SPs were given an opportunity to ask questions.
When preparing for a similar activity at another institution, it is essential to recognize the importance of the SP training. The SPs who participated in our activity were accustomed to encounters that focused on clinical skills and were often encouraged to ad-lib dialogue in those cases. When training SPs, it is important to emphasize that microaggression statements need to be said as written for the cases to be effective educational tools. We found the training session to be an invaluable asset in conveying the objectives and nuances of each case. Furthermore, since the cases contain sensitive material, it is important to appreciate that SPs may not be comfortable saying each statement outlined in the cases. Our SP training session spent a significant amount of time in open discussion, which encouraged participating SPs to clarify and/or raise concerns about the content of each case. In our workshop, the SPs did not raise any concerns with the cases.
SPs maintained character for 2 hours and completed their case three times each session. Since faculty were observing the SP encounters and assessing whether a WAKE behavioral response strategy was used, we did not require the SPs to provide feedback via a global assessment or checklist. After each case, the SPs were given an opportunity to discuss the microaggression response tactics chosen by the residents and to comment on how it made them feel as patients. This allowed the residents to reflect on how their behavioral response strategy might be perceived by a patient who has exhibited a microaggression. While no formal debriefing occurred, the SPs were given an opportunity to provide feedback following each session.
After the cases and debriefing sessions had concluded, participating residents and faculty spent the last 5 minutes of the activity engaging in a brief large-group discussion. Participants also completed a postsurvey. Before and after the activity, all participants completed pre- and postsurveys (Appendix A), which were delivered through a QR code connecting to a Microsoft survey. We did not collect identifying information in either survey to maintain anonymity among participants. Since both surveys were administered through a QR code software, all responses were anonymous, and respondents did not have a unique identifier to link their pre- and postsurvey responses. We used Wilcoxon rank sum tests to determine statistical significance between the pre- and postsurvey responses. We asked questions 1-5 in both surveys, while questions 6 and 7 were optional and available in the postsurvey only via free response. We chose self-assessment as our primary outcome measure to facilitate feedback on the workshop and to assess the residents’ experience with microaggressions and their confidence in responding to microaggressions in the future. All statistical analysis was performed using SAS 9.4 (SAS Institute).
Results
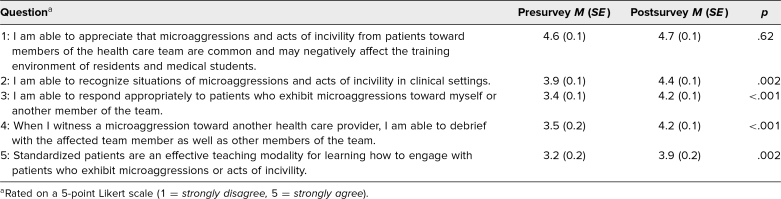
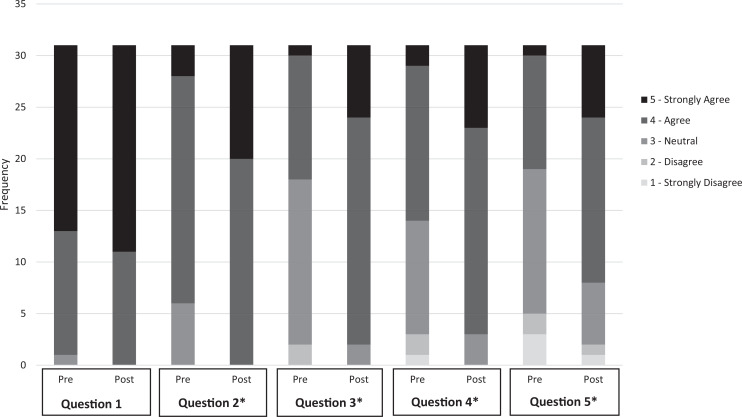
A total of 31 categorical and preliminary internal medicine PGY 1 residents participated in the workshop and completed the pre- and postsurveys. The Table shows the mean responses before and after the activity rated on a 5-point Likert scale (1 = strongly disagree, 5 = strongly agree). The Figure shows a histogram of the Likert-scale responses before and after the activity for each question.
Table. Pre- and Postactivity Responses to Self-Assessment Questionnaire (N = 31).
Figure. Pre- and postactivity responses to self-assessment questionnaire. Asterisk (*) indicates statistical significance between pre- and postsurvey responses ( p < .01).
According to the postactivity survey, participants reported significant improvement in recognizing microaggressions (12% reported increase, p = .002), the ability to respond to patients who exhibit microaggressions (23% reported increase, p < .001), and the ability to debrief with team members (20% reported increase, p < .001). On average, respondents reported a 22% increase in agreement that SPs were an effective teaching method for microaggressions ( p = .002). Notably, most participants either agreed or strongly agreed that microaggressions were common and negatively affected the training environment; this metric did not improve after the activity.
Based on the free-response feedback, 16 out of 31 residents commented that the activity was useful for their professional development. When asked what in particular was useful for their professional development, five out of 31 participants wrote that they could better identify microaggressions in patient settings and felt that they could better respond to them in real time. Eight out of 31 participants noted that the debriefing sessions were particularly helpful, and four out of 31 respondents mentioned that SP methodology was helpful for practicing skills in addressing microaggressions. Examples of participant free-response feedback included the following:
-
•
“Debriefing the situation and discussing strategies to deal with difficult situations.”
-
•
“Recognizing microaggressions and some techniques on how to respond to them.”
-
•
“I thought the standardized patient encounters and debriefing was helpful.”
-
•
“I now feel as though I have the tools to address microaggressions that I encounter.”
When asked for suggestions on improving the session, three out of 31 participants suggested more SP case scenarios as an area of improvement, and three out of 31 participants mentioned that the activity would be even more useful earlier in the year.
Discussion
Given the well-documented frequency of microaggressions and the long-term emotional and professional implications, it is vital to develop educational innovations to promote inclusivity and to combat microaggressions in the clinical setting. To address this systemwide problem, we developed and implemented a workshop to teach microaggression response skills using SP methodology. Our findings suggest that residents felt they were better able to recognize situations of microaggressions in clinical settings, respond appropriately to patients who exhibited microaggressions toward a member of the health care team, and debrief with the medical team afterward. In the presurvey, most participants acknowledged that microaggressions were common and negatively affected the training environment; this metric did not improve after the workshop. This suggests that while medical trainees realize the impact of microaggressions, they may not possess the tools required to mitigate microaggressions in clinical encounters.
Our educational innovation provides unique contributions to the literature. First, our workshop utilizes SP methodology specifically to teach bystander strategies for microaggressions. This expanded the role of SPs to teach not only clinical skills but also behavioral response and communication skills that can be used when patients commit microaggressions. Overall, the activity was well received. Furthermore, participants were more likely to report that SP methodology was an effective modality to teach microaggression response skills after the workshop. Given that many medical providers report inaction to witnessed microaggressions in clinical encounters, SP methodology may provide a more interactive alternative to traditional bystander intervention workshops by giving participants an opportunity to practice in a simulated environment. Prior studies utilizing role-playing to teach microaggression response have suggested that such interactive activities increase awareness of microaggressions, provide learners with an opportunity to use strategies in a safe space,29 and provide actionable skills for situations that most learners are already experiencing in clinical settings.18
Furthermore, the WAKE active bystander acronym provides an additional response framework that emphasizes the personal strengths of the bystander. This encourages colleagues to reflect on the ways they can uniquely intervene in the situation using their power and privilege. For educators interested in replicating this activity at their institution, the WAKE active bystander strategies can be utilized; however, the SP cases provided could also be used with other effective behavioral response frameworks in the medical education literature, such as the 5 D's (direct, distract, delegate, delay, and display discomfort)24 and VITALS (validate, inquire, take time, assume, leave opportunities, speak up).25 The SP cases and WAKE active bystander strategies could also be applied to other health care professional trainees.
The faculty debriefing structure posed some challenges. We discussed whether it would be beneficial for one attending to follow each group and discuss all three cases. Ultimately, we opted to assign one faculty facilitator to each case with rotating groups of trainees. Alternatively, this activity could be done with one facilitator discussing all three cases with one group of participants.
We did not preassign the learners based on demographics or other background characteristics, as we did not want to single out residents of certain identities to take the lead on cases. Most of our residents were White, native English speakers, which is why most of our cases focused on microaggressions directed at another physician rather than directed at the learner. Other programs that wish to recreate this workshop may consider assigning learners to specific cases. However, we found that not preassigning cases led to rich discussion and dialogue during the debriefing sessions. For instance, when a male resident was referred to as a nurse instead of a doctor in case 1, it allowed them to reflect on their privilege and recognize the harms of that microaggression over time. Furthermore, having residents of different backgrounds as bystanders also enriched the discussion, as they often voluntarily shared their lived experiences with the group.
Our workshop had several limitations. First, our results may have limited generalizability to other residency programs due to the small sample size of one trainee population. We also opted not to collect demographic information on the participants to protect privacy given the small sample size; therefore, conclusions on the efficacy of the training among certain groups cannot be inferred from our study. Second, since our survey responses were anonymously collected through a QR code, we were unable to pair our pre- and postsurvey responses in our statistical analysis, and so we used an unpaired statistical analysis. Future studies should consider collecting additional data from participants to further examine the effectiveness of the workshop. Third, the participants knew the faculty facilitators, which may have introduced positive or negative bias to the responses in the postsurvey. Fourth, our results relied on self-assessment by participants and did not include formal skills-based evaluations. While faculty facilitators did observe the participants during the SP encounters, we did not develop a standardized skills assessment for each case.
Our workshop builds on many excellent educational interventions and could be enhanced in several ways. Due to resident feedback expressing a need for more cases focusing on additional racial/ethnic groups, we created a fourth case, which can be found in Appendix E. We plan to utilize this case in addition to the others in a future workshop for PGY 1 interns. Additionally, longitudinal assessments could be developed to evaluate the workshop's effect on trainee ability over time. Finally, implementing the workshop with trainees in other health care professions and at other academic institutions would help determine the external validity of this educational approach. After successful implementation at Wake Forest, the workshop and its materials can now be used as a resource to help institutions create a more supportive environment for minoritized health care workers and develop a larger curriculum centered on anti-racism and diversity, equity, and inclusion in medicine.
Appendices
- Pre- and Postsurvey.docx
- Introductory Presentation.pptx
- Logistics.docx
- Door Instructions.docx
- SP Cases.docx
- Case Debriefing Q&A.docx
- SP Recruitment and Training.docx
All appendices are peer reviewed as integral parts of the Original Publication.
Acknowledgments
We would like to acknowledge the following individuals for their assistance in implementing this project: Hal Atkinson, MD, MS; Donna Williams, MD; Tonya Mock, Standardized Patient Program Coordinator; Peter Lichstein, MD; Rachel Wilson, DO; Allan Petty, DO; Nathan Roberts, MD; and Safoa Addo, MD.
Disclosures
None to report.
Funding/Support
This project was prepared with support from the Education Innovation Grant Program of the North Carolina Chapter of the American College of Physicians to Dr. M. Leila Famouri.
Prior Presentations
Famouri ML, Hernandez S, Omlor RL, et al. Using standardized patients to teach residents to navigate microaggressions in patient encounters. Poster presented at: Society of General Internal Medicine Annual Meeting; May 6-9, 2022; Orlando, FL.
Ethical Approval
The Wake Forest University Institutional Review Board deemed further review of this project not necessary.
Disclaimer
The statements, findings, conclusion, and recommendations are those of the authors and do not necessarily reflect the views of the North Carolina Chapter of the American College of Physicians.
References
- 1.Diversity in Medicine: Facts and Figures 2019—Figure 26. Primary care versus nonprimary care physicians by race/ethnicity, 2018. Association of American Medical Colleges. Accessed November 28, 2022. https://www.aamc.org/data-reports/workforce/interactive-data/figure-26-primary-care-versus-nonprimary-care-physicians-race/ethnicity-2018
- 2.Greenwood BN, Carnahan S, Huang L. Patient–physician gender concordance and increased mortality among female heart attack patients. Proc Natl Acad Sci U S A. 2018;115(34):8569–8574. 10.1073/pnas.1800097115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tsugawa Y, Jena AB, Figueroa JF, Orav EJ, Blumenthal DM, Jha AK. Comparison of hospital mortality and readmission rates for Medicare patients treated by male vs female physicians. JAMA Intern Med. 2017;177(2):206–213. 10.1001/jamainternmed.2016.7875 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rodríguez JE, Campbell KM, Pololi LH. Addressing disparities in academic medicine: what of the minority tax? BMC Med Educ. 2015;15:6. 10.1186/s12909-015-0290-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jagsi R, Griffith KA, Jones R, Perumalswami CR, Ubel P, Stewart A. Sexual harassment and discrimination experiences of academic medical faculty. JAMA. 2016;315(19):2120–2121. 10.1001/jama.2016.2188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Adesoye T, Mangurian C, Choo EK, et al; Physician Moms Group Study Group. Perceived discrimination experienced by physician mothers and desired workplace changes: a cross-sectional survey. JAMA Intern Med. 2017;177(7):1033–1036. 10.1001/jamainternmed.2017.1394 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chisholm LP, Jackson KR, Davidson HA, Churchwell AL, Fleming AE, Drolet BC. Evaluation of racial microaggressions experienced during medical school training and the effect on medical student education and burnout: a validation study. J Natl Med Assoc. 2021;113(3):310–314. 10.1016/j.jnma.2020.11.009 [DOI] [PubMed] [Google Scholar]
- 8.Hu YY, Ellis RJ, Hewitt DB, et al. Discrimination, abuse, harassment, and burnout in surgical residency training. N Engl J Med. 2019;381(18):1741–1752. 10.1056/NEJMsa1903759 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Limbong A. Microaggressions are a big deal: how to talk them out and when to walk away. NPR. June 9, 2020. Accessed November 28, 2022. https://www.npr.org/2020/06/08/872371063/microaggressions-are-a-big-deal-how-to-talk-them-out-and-when-to-walk-away
- 10.Ackerman-Barger K, Boatright D, Gonzalez-Colaso R, Orozco R, Latimore D. Seeking inclusion excellence: understanding racial microaggressions as experienced by underrepresented medical and nursing students. Acad Med. 2020;95(5):758–763. 10.1097/ACM.0000000000003077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Anderson N, Lett E, Asabor EN, et al. The association of microaggressions with depressive symptoms and institutional satisfaction among a national cohort of medical students. J Gen Intern Med. 2022;37(2):298–307. 10.1007/s11606-021-06786-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Silver JK, Bean AC, Slocum C, et al. Physician workforce disparities and patient care: a narrative review. Health Equity. 2019;3(1):360–377. 10.1089/heq.2019.0040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wheeler M, de Bourmont S, Paul-Emile K, et al. Physician and trainee experiences with patient bias. JAMA Intern Med. 2019;179(12):1678–1685. 10.1001/jamainternmed.2019.4122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kass D. Allies, advocates, and accomplices are critical to diversity and inclusion. ACEP Now. 2019;38(10):38. https://www.acepnow.com/article/allies-advocates-and-accomplices-are-critical-to-diversity-and-inclusion/ [Google Scholar]
- 15.Darley JM, Latane B. Bystander intervention in emergencies: diffusion of responsibility. J Pers Soc Psychol. 1968;8(4):377–383. 10.1037/h0025589 [DOI] [PubMed] [Google Scholar]
- 16.Hortensius R, de Gelder B. From empathy to apathy: the bystander effect revisited. Curr Dir Psychol Sci. 2018;27(4):249–256. 10.1177/0963721417749653 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Emeghara U. Bystander effect and diffusion of responsibility. Simply Psychology. September 24, 2020. Accessed November 28, 2022. https://www.simplypsychology.org/bystander-effect.html
- 18.Sandoval RS, Afolabi T, Said J, Dunleavy S, Chatterjee A, Ölveczky D. Building a tool kit for medical and dental students: addressing microaggressions and discrimination on the wards. MedEdPORTAL. 2020;16:10893. 10.15766/mep_2374-8265.10893 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fisher HN, Chatterjee P, Shapiro J, Katz JT, Yialamas MA. “Let's talk about what just happened”: a single-site survey study of a microaggression response workshop for internal medicine residents. J Gen Intern Med. 2021;36(11):3592–3594. 10.1007/s11606-020-06576-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sotto-Santiago S, Mac J, Duncan F, Smith J. “I didn't know what to say”: responding to racism, discrimination, and microaggressions with the OWTFD approach. MedEdPORTAL. 2020;16:10971. 10.15766/mep_2374-8265.10971 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jouriles EN, Krauss A, Vu NL, Banyard VL, McDonald R. Bystander programs addressing sexual violence on college campuses: a systematic review and meta-analysis of program outcomes and delivery methods. J Am Coll Health. 2018;66(6):457–466. 10.1080/07448481.2018.1431906 [DOI] [PubMed] [Google Scholar]
- 22.Coker AL, Fisher BS, Bush HM, et al. Evaluation of the Green Dot bystander intervention to reduce interpersonal violence among college students across three campuses. Violence Against Women. 2015;21(12):1507–1527. 10.1177/1077801214545284 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Coker AL, Bush HM, Fisher BS, et al. Multi-college bystander intervention evaluation for violence prevention. Am J Prev Med. 2016;50(3):295–302. 10.1016/j.amepre.2015.08.034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.York M, Langford K, Davidson M, et al. Becoming active bystanders and advocates: teaching medical students to respond to bias in the clinical setting. MedEdPORTAL. 2021;17:11175. 10.15766/mep_2374-8265.11175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Walker VP, Hodges L, Perkins M, Sim M, Harris C. Taking the VITALS to interrupt microaggressions. MedEdPORTAL. 2022;18:11202. 10.15766/mep_2374-8265.11202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wilbur K, Elmubark A, Shabana S. Systematic review of standardized patient use in continuing medical education. J Contin Educ Health Prof. 2018;38(1):3–10. 10.1097/CEH.0000000000000190 [DOI] [PubMed] [Google Scholar]
- 27.Evans S. WAKE active bystander training. Presented at: Wake Forest Baptist Medical Center; 2019; Winston-Salem, NC. [Google Scholar]
- 28.Martin LD, Zadinsky JK. Frequency and outcomes of workplace incivility in healthcare: a scoping review of the literature. J Nurs Manag. 2022;30(7):3496–3518. 10.1111/jonm.13783 [DOI] [PubMed] [Google Scholar]
- 29.Carter BM, McMillian-Bohler J. Rewriting the microaggression narrative: enhancing nursing students’ ability to respond. Nurse Educ. 2021;46(2):96–100. 10.1097/NNE.0000000000000850 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
- Pre- and Postsurvey.docx
- Introductory Presentation.pptx
- Logistics.docx
- Door Instructions.docx
- SP Cases.docx
- Case Debriefing Q&A.docx
- SP Recruitment and Training.docx
All appendices are peer reviewed as integral parts of the Original Publication.