Abstract
Frailty is a geriatric syndrome that leads to increased risk of hospitalization, disability, and death. The effect of plant-based diets defined by the quality of their plant foods is unclear. Our objective is to study the association between two plant-based diet indices and the occurrence of frailty among community-dwelling older adults in Spain. We analyzed data from 1880 individuals aged ≥ 60 years from the Spanish Seniors ENRICA-1 cohort. We used a validated diet history to build two indices: (a) the healthful Plant-based Diet Index (hPDI) where healthy plant foods received positive scores, whereas less-healthy plant foods and animal foods received reverse scores; and (b) the unhealthful Plant-based Diet Index (uPDI), with positive scores to less-healthy plant foods and reverse scores to animal and healthy plant foods. Incident frailty was defined with the Fried phenotype. Study associations were summarized with odds ratios (OR) and 95% confidence intervals (CI) obtained from multivariable logistic models. After 3.3 years of follow-up, 136 incident frailty cases were ascertained. Comparing the highest vs. the lowest tertile of adherence, the OR [95% CI] for frailty was 0.43 (0.25–0.74; p-trend = .003) for the hPDI, and 2.89 (1.73–4.84; p-trend < .001) for the uPDI. Higher consumption of healthy plant foods was inversely associated with frailty (0.39 [0.23–0.66; p-trend < 0.001]); higher consumption of unhealthy plant foods was associated with higher frailty risk (2.40 [1.23–4.71; p-trend = .01]). In older adults, the hPDI was associated with lower risk of frailty, while the opposite was found for the uPDI.
Supplementary Information
The online version contains supplementary material available at 10.1007/s11357-022-00614-3.
Keywords: Diet quality, Healthy aging, Physical impairment, Elderly, Pro-vegetarian pattern
Introduction
The world is aging rapidly. Older adults (≥ 60 years) were 1 billion people in 2019, and this number will increase by 34% in 2030 [1]. Consequently, health systems will face a growingly burden of age-related issues in the next years. One of the biggest threats to healthy aging is the frailty condition. Frailty is a geriatric syndrome that confers high vulnerability to stressors and leads to an increased risk of adverse health outcomes like disability, hospitalization, or death [2]. However, frailty is preventable and potentially reversible through interventions such as increasing physical activity or adequate nutrition [3–5].
There is growing interest on using diet to prevent frailty. So far, the available evidence suggests that higher consumption of fruits and vegetables [6–8] and higher adherence to diets rich in fruits, vegetables, legumes, and grains, and poor in red and processed meat such as the Mediterranean diet [9–12], the Baltic Sea Diet, and others [13–15] are all associated to lower risk of frailty.
The Plant-based Diet Indices (PDI), such as the healthful (hPDI) and the unhealthful (uPDI) indices, assess adherence to diets characterized by high consumption of plant-derived foods and lower consumption of animal-derived foods [16]. Although the hPDI share common characteristics with other healthy diets scores, unlike vegetarian diets, the hPDI focus on the quality of plant foods by assigning either positive scores to healthy plant foods (e.g., fruits, legumes, nuts) or reverse scores to less healthy plant foods (e.g., potatoes, sugar-sweetened beverages). In addition, animal-derived foods, while not excluded like in vegetarian diets, score inversely, even those typically associated to better health such as fish or dairy.
These novel indices have been associated with diabetes [16, 17], high blood pressure [18], cardiovascular disease [19], and mortality [20]. However, since their relationship with frailty has hardly ever been evaluated—and not in a Mediterranean population, we aimed to study the association between these two plant-based diet indices and the occurrence of frailty among community-dwelling older adults in Spain.
Methods
Study design and population
The Seniors ENRICA-1 is a cohort comprising 3289 non-institutionalized Spanish adults aged ≥ 60 years, recruited between 2008 and 2010 using multistage stratified random sampling and followed up in 2012. Details on the methodology have been previously reported [21]. Briefly, trained personnel performed sequentially: (1) a computer-assisted telephone interview about sociodemographic characteristics, health behaviors, and physician-diagnosed morbidity; (2) a home visit to collect biological samples that were sent to a central laboratory; (3) a second home visit to perform a physical examination and a computer-assisted face-to-face diet history.
The Seniors ENRICA-1 study was approved by the Clinical Research Ethics Committee of La Paz University Hospital in Madrid (study registration: NCT02804672). Participants provided written informed consent.
Study variables
Plant-based diets
Food consumption was obtained using a validated computerized face-to-face diet history (DH-ENRICA) developed from that used in the European Prospective Investigation into Cancer and Nutrition (EPIC) cohort study in Spain (22). Standard food composition tables were used to estimate nutrient and energy intake [22].
We calculated the hPDI and the uPDI as described by Satija et al. [16] (Online Resource 1). We allocated each food consumed into 18 food groups under three blocks: healthy plant foods (whole grains, fruits, vegetables, nuts, legumes, vegetable oils, and coffee and tea); unhealthy plant foods (fruit juices, sugar-sweetened beverages, refined grains, potatoes, and sweets and desserts), and animal foods (animal fats, dairy, eggs, fish and seafood, meat, and miscellaneous animal-based foods). Each food group was divided into quintiles of consumption and scored between one (worst) and five (best). For the hPDI, healthy plant foods were given positive scores, while the unhealthy plant and animal foods were given reverse scores. For the uPDI, positive scores were given to unhealthy plant foods, and reverse scores to healthy plant and animal foods (Online Resource 2). The food groups were summed to obtain the indices. The scores range was 18 to 90.
Frailty assessment
Incident frailty was defined, according to Fried et al. [23], as developing at least three out of the following five criteria at follow-up (2012): (1) Exhaustion, responding affirmatively to any of these two statements adapted from the Center for Epidemiologic Studies Depression Scale [24]: “I feel that anything I do is a big effort” or “I feel that I cannot keep on doing things”, ≥ 3–4 days/week; (2) Low physical activity, walking ≤ 2.5 h/week (men) or 2 h/week (women) [25]; (3) Slow gait speed, being in the lowest cohort-specific quintile in a 2.44-m walking speed test adjusted for sex and height [26]; (4) Unintentional weight loss, defined as unintentional loss of ≥ 4.5 kg in the preceding year; and (5) Muscle weakness, defined as being in the lowest cohort-specific quintile of grip strength, adjusted for sex and BMI; strength was assessed as the highest of two consecutive measures in the dominant hand with a Jamar dynamometer [27].
Potential confounders
At baseline, participants reported their sex, age, educational level (primary or less, secondary, university), and other possible confounding factors: smoking status (never, former, current), recreational physical activity (Metabolic Equivalents of task-hours/week, METs*h/wk), energy intake (kcal/day), physician-diagnosed diseases (type 2 diabetes mellitus, cardiovascular disease, chronic lung disease, osteomuscular disease, cancer, and depression), number of medications taken (0, 1–3, 4–6, > 6; including any of the following: low-dose aspirin, beta-blockers, blockers of the renin-angiotensin system, diuretics, statins, insulin, oral antidiabetic drugs, antiplatelet medication, anticoagulant medication, and sleeping pills), and alcohol consumption (servings/day).
Hours of leisure-time physical activity were obtained with the Spanish-validated version of the EPIC-cohort questionnaires [28]. Energy and alcohol intake were estimated from the diet history. Alcohol serving was expressed as any volume of a drink containing 10 g of pure alcohol. Finally, the body mass index (BMI) was calculated as weight (kg) divided by squared height (m), both measured during the physical examination.
Statistical analyses
From the 3289 initial participants, we excluded at baseline 154 participants with any missing frailty data, 25 with missing BMI, 7 with implausible energy intakes (men: < 800 kcal or > 5000; women: < 500 kcal or > 4000 kcal), and 41 participants who were already frail. At the follow-up, in 2012, we excluded those who died (108), those who were lost to follow-up (662), and 412 with missing frailty data at this point. Therefore, the analytical sample comprised 1880 individuals (Online Resource 3). Participants’ characteristics were summarized using proportions for categorical variables and mean and standard deviation (SD) for continuous variables.
We used multivariable logistic regression models to evaluate associations between baseline tertiles of PDIs and incident frailty, which were summarized using odds ratios (OR) with 95% confidence intervals (CI). The lowest tertile of each PDI was used as reference. In addition, we evaluated associations between tertiles of the PDIs and the occurrence of each frailty criterion, in order to discern how these criteria behaved separately. Moreover, we assessed associations for healthy, unhealthy plant foods, and animal foods. Three progressively adjusted models were fit: Model 1, adjusted for sex, age, education, and alcohol intake; model 2, further adjusted for smoking status, BMI, energy intake, and physical activity; and model 3, further adjusted for chronic diseases and number of medications taken. We performed stratified analyses by sex and tested interaction terms to assess possible differential associations. No significant interaction was found, so we reported results for the total sample.
In secondary analyses: (1) We excluded pre-frail individuals (those meeting one or two frailty criteria) and participants with chronic diseases at baseline, as these conditions can lead to diet changes; (2) due to the close relation between frailty and poor health, we restricted the analyses to participants that self-reported good health and independence in instrumental activities of daily living (IADL); (3) we excluded “unintentional weight loss” from frailty criteria (the definition of frailty of ≥ 3 criteria remained unchanged), since a healthy diet could lead to weight changes [29]; (5) we built an alternative hPDI in which fish, eggs, and dairy products scored positively instead of reversely because these foods have been shown to be associated with healthy aging and lower frailty risk [30–32].
Statistical significance was established at two-sided p < 0.05. Analyses were performed using Stata, version 16.0 (Stata-Corp LLC, College Station, TX).
Results
Participants had a mean (SD) age of 68.7 (6.4) years, and 51.7% were women; corresponding figures were 59.7 (5.6) for the hPDI and 54.9 (5.3) for the uPDI. Compared to participants in the lowest tertile of the hPDI, those in the highest tertile were more likely to be women, non-smokers, to have lower BMI and less energy and alcohol intake, and to be more physically active, whereas those in the highest tertile of the uPDI were more often women and non-smokers, had lower education and energy intake (Table 1). Compared to participants in the analytical sample, those lost to follow-up or excluded due to missing frailty data were more likely to be women, have lower education, and have a BMI ≥ 30 (Online Resource 4).
Table 1.
Baseline characteristics of older adults participating in the Seniors ENRICA-1 cohort by tertiles of plant-based diet indices (N = 1880)
| Healthful Plant-based Diet Index | Unhealthful Plant-based Diet Index | Total | ||||||
|---|---|---|---|---|---|---|---|---|
| Tertile 1 (lowest) 41–55 p |
Tertile 2 56–61 p |
Tertile 3 (highest) 62–80 p |
Tertile 1 (lowest) 37–54 p |
Tertile 2 55–59 p |
Tertile 3 (highest) 60–75 p |
|||
| n (%) | 429 (22.82) | 765 (40.69) | 686 (36.49) | 879 (46.76) | 639 (33.99) | 362 (19.26) | 1880 (100) | |
| Index score, range (18–90), mean (SD) | 52.43 (2.62) | 58.60 (1.71) | 65.56 (3.22) | 50.32 (3.13) | 56.83 (1.37) | 62.38 (2.52) | hPDI 59.73 (5.63) |
uPDI 54.85 (5.32) |
| Sex, women, n (%) | 177 (41.26) | 385 (50.33) | 409 (59.62) | 425 (48.35) | 340 (53.21) | 206 (56.91) | 971 (51.65) | |
| Age, years, mean (SD) | 67.86 (6.29) | 69.33 (6.76) | 68.38 (5.91) | 68.02 (6.01) | 68.79 (6.59) | 69.93 (6.68) | 68.65 (6.38) | |
| Education, n (%) | ||||||||
| ≤ Primary | 216 (50.35) | 414 (54.12) | 367 (53.50) | 443 (50.40) | 347 (54.30) | 207 (57.18) | 997 (53.03) | |
| Secondary | 120 (27.97) | 186 (24.31) | 163 (23.76) | 220 (25.03) | 163 (25.51) | 86 (23.76) | 469 (24.95) | |
| University | 93 (21.68) | 165 (21.57) | 156 (22.74) | 216 (24.57) | 129 (20.19) | 69 (19.06) | 414 (22.02) | |
| Smoking status, n (%) | ||||||||
| Current | 62 (14.45) | 97 (12.68) | 62 (9.04) | 102 (11.60) | 72 (11.27) | 47 (12.98) | 221 (11.76) | |
| Former | 137 (31.93) | 233 (30.46) | 207 (30.17) | 299 (34.02) | 195 (30.52) | 83 (22.93) | 577 (30.69) | |
| Never | 230 (53.61) | 435 (56.86) | 417 (60.79) | 478 (54.38) | 372 (58.22) | 232 (64.09) | 1082 (57.55) | |
| BMI, kg/m2, n (%) | ||||||||
| < 25 | 71 (16.55) | 150 (19.61) | 147 (21.43) | 174 (19.80) | 118 (18.47) | 76 (20.99) | 368 (19.57) | |
| 25–29.9 | 212 (49.42) | 391 (51.11) | 334 (48.69) | 430 (48.92) | 338 (52.90) | 169 (46.69) | 937 (49.69) | |
| ≥ 30 | 146 (34.03) | 224 (29.28) | 205 (29.88) | 275 (31.29) | 183 (28.64) | 117 (32.32) | 575 (30.59) | |
| Energy intake, kcal/day, mean (SD) | 2335 (550) | 2053 (554) | 1815 (499) | 2142 (566) | 1971 (545) | 1863 (559) | 2031 (569) | |
| Alcohol intake, servings/day, mean (SD) | 1.35 (2.09) | 1.03 (1.74) | 0.89 (1.61) | 1.06 (1.70) | 1.07 (1.82) | 0.99 (1.94) | 1.05 (1.79) | |
| Physical activity, METs*h/wk, mean (SD) | 20.97 (15.82) | 21.78 (15.32) | 22.29 (15.16) | 22.78 (15.45) | 20.77 (14.20) | 21.14 (17.01) | 21.78 (15.38) | |
| Prevalent diseases, n (%) | ||||||||
| Cardiovascular diseasea | 22 (5.13) | 39 (5.10) | 36 (5.25) | 45 (5.12) | 34 (5.32) | 18 (4.97) | 97 (5.16) | |
| Type 2 diabetes mellitus | 74 (17.25) | 117 (15.29) | 93 (13.56) | 129 (14.68) | 103 (16.12) | 52 (14.36) | 284 (15.11) | |
| Cancer | 9 (2.10) | 13 (1.70) | 12 (1.75) | 18 (2.05) | 8 (1.25) | 8 (2.21) | 34 (1.81) | |
| Chronic lung diseaseb | 24 (5.59) | 68 (8.89) | 51 (7.43) | 63 (7.17) | 47 (7.36) | 33 (9.12) | 143 (7.61) | |
| Osteomuscular diseasec | 188 (43.82) | 366 (47.84) | 339 (49.42) | 409 (46.53) | 311 (48.67) | 173 (47.79) | 893 (47.50) | |
| Depression | 33 (7.69) | 51 (6.67) | 54 (7.87) | 60 (6.83) | 44 (6.89) | 34 (9.39) | 138 (7.34) | |
| Medicines per day, n (%) | ||||||||
| 0 | 121 (28.21) | 202 (26.41) | 181 (26.38) | 236 (26.85) | 167 (26.13) | 101 (27.90) | 504 (26.81) | |
| 1–3 | 233 (54.31) | 399 (52.16) | 361 (52.62) | 469 (53.36) | 342 (53.52) | 182 (50.28) | 993 (52.82) | |
| 4–6 | 68 (15.85) | 146 (19.08) | 118 (17.20) | 142 (16.15) | 120 (18.78) | 70 (19.34) | 332 (17.66) | |
| > 6 | 7 (1.63) | 18 (2.35) | 26 (3.79) | 32 (3.64) | 10 (1.56) | 9 (2.49) | 51 (2.71) | |
Abbreviations: BMI body mass index, p points, SD standard deviation
aIncluding myocardial infarction, stroke, and heart failure
bIncluding asthma and chronic obstructive pulmonary disease
cIncluding osteoarthritis, rheumatoid arthritis, and hip fracture
PDIs and frailty risk
We ascertained 136 frailty cases after a mean follow-up of 3.3 years. Study participants showed an inverse dose–response relationship between the hPDI and frailty: the full adjusted OR (95% CI) compared to the lowest of hPDI was 0.51 (0.31–0.84) for the second and 0.43 (0.25–0.74) for the highest tertile (p-trend = 0.003). Conversely, the uPDI showed a direct dose–response with frailty, with OR (95% CI) of 1.81 (1.12–2.94) and 2.89 (1.73–4.84) respectively (p-trend < 0.001) (Table 2).
Table 2.
Odds ratios (95% CI) for the occurrence of frailty by tertiles of plant-based diet indices and tertiles of total servings of food groups consumed, over 3.3 years of follow-up in the Seniors ENRICA-1 cohort (N = 1880)
| Plant-based diet indices or food groups consumed | ||||
|---|---|---|---|---|
| Tertile 1 (lowest) | Tertile 2 | Tertile 3 (highest) | p-trend | |
| Healthful Plant-based Diet Index | ||||
| 41–55 p | 56–61 p | 62–80 p | ||
| n/N | 30/309 | 54/701 | 52/870 | |
| Model 1a | Ref | 0.51 (0.32–0.81) | 0.44 (0.27–0.71) | 0.001 |
| Model 2b | Ref | 0.51 (0.32–0.84) | 0.42 (0.25–0.71) | 0.002 |
| Model 3c | Ref | 0.51 (0.31–0.84) | 0.43 (0.25–0.74) | 0.003 |
| Unhealthful Plant-based Diet Index | ||||
| 37–54 p | 55–59 p | 60–75 p | ||
| n/N | 34/764 | 55/772 | 47/344 | |
| Model 1a | Ref | 1.71 (1.08–2.68) | 2.68 (1.68–4.29) | < 0.001 |
| Model 2b | Ref | 1.80 (1.12–2.89) | 2.84 (1.72–4.71) | < 0.001 |
| Model 3c | Ref | 1.81 (1.12–2.94) | 2.89 (1.73–4.84) | < 0.001 |
| Healthy plant foodsd | ||||
| n/N | 45/349 | 54/701 | 37/830 | |
| Model 1a | Ref | 0.65 (0.41–1.01) | 0.43 (0.27–0.69) | 0.001 |
| Model 2b | Ref | 0.70 (0.43–1.12) | 0.40 (0.23–0.67) | 0.001 |
| Model 3c | Ref | 0.71 (0.44–1.15) | 0.39 (0.23–0.66) | < 0.001 |
| Unhealthy plant foodse | ||||
| n/N | 49/717 | 52/737 | 35/426 | |
| Model 1a | Ref | 1.18 (0.77–1.81) | 1.74 (1.07–2.83) | 0.032 |
| Model 2b | Ref | 1.50 (0.93–2.42) | 2.40 (1.24–4.64) | 0.009 |
| Model 3c | Ref | 1.52 (0.93–2.48) | 2.40 (1.23–4.71) | 0.010 |
| Animal foodsf | ||||
| n/N | 56/704 | 47/677 | 33/499 | |
| Model 1a | Ref | 0.98 (0.64–1.50) | 1.20 (0.75–1.94) | 0.502 |
| Model 2b | Ref | 0.85 (0.54–1.35) | 0.95 (0.54–1.66) | 0.786 |
| Model 3c | Ref | 0.81 (0.51–1.30) | 0.89 (0.50–1.57) | 0.618 |
Abbreviations: BMI body mass index, CI confidence interval, p points, Ref. reference
aModel 1: Adjusted for sex, age, educational level (primary, secondary, university), alcohol consumption
bModel 2: Model 1 + smoking status (current, former, never), BMI (< 25, 25–29.9, ≥ 30), energy intake, physical activity
cModel 3: Model 2 + and prevalent diseases (type 2 diabetes mellitus, cardiovascular disease [myocardial infarction, stroke, or heart failure], chronic lung disease [asthma or chronic obstructive pulmonary disease], osteomuscular disease [osteoarthritis, rheumatoid arthritis or hip fracture], cancer and depression), medicines consumption (0, 1–3, 4–6, > 6)
dHealthy plant foods: whole grains, fruits, vegetables, nuts, legumes, vegetable oils, and coffee/tea
eUnhealthy plant foods: fruit juices, sugar-sweetened beverages, refined grains, potatoes, and sweets/desserts
fAnimal foods: fats, dairy products, eggs, fish and seafood, meat, and miscellaneous animal-based foods
Significance of bold entries is p < 0.05
The results remained robust in sensitivity analyses (Online Resource 5): (1) Excluding pre-frail participants (adjusted OR [95% CI] for the highest vs. lowest tertile: 0.40 [0.20–0.82] for hPDI, p-trend = 0.01; and 3.84 [1.96–7.50] for uPDI, p-trend < 0.001); (2) excluding participants with diagnosed chronic diseases (0.40 [0.18–0.88] for hPDI, p-trend = 0.02; and 3.03 [1.50–6.14] for uPDI, p-trend = 0.002); (3) among participants self-reportedly healthy and independent in IADL (0.29 [0.10–0.87] for hPDI, p-trend = 0.03; and 3.54 [1.28–9.78] for uPDI, p-trend = 0.01); (4) excluding “unintentional weight loss” from frailty criteria (0.53 [0.28–0.99], p-trend = 0.06 for hPDI; and 2.09 [1.17–3.74], p-trend = 0.01 for uPDI); (5) when using the alternative hPDI (0.40 [0.23–0.68], p-trend < 0.001).
Food groups and frailty risk
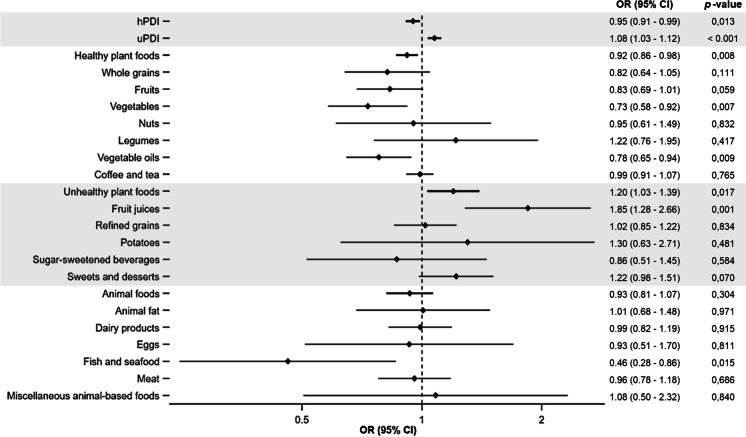
Four out of the 18 food groups were independently associated with lower frailty risk: vegetables (OR per 1-serving increase: 0.73 [0.58–0.92]), vegetable oils (0.78 [0.65–0.94]), and fish and seafood (0.46 [0.28–0.86]), while fruit juices were associated with greater frailty risk (1.85 [1.28–2.66]) (Fig. 1). Most of the association between the other food groups with frailty were in the expected direction (note the associations of whole grains, fruits, or sweets and desserts).
Fig. 1.
Odds ratio (95% CI) for the occurrence of frailty per each Plant-based Diet Index (1-unit increase), each food group, healthy plant food, unhealthy plant food, and animal food, over 3.3 years of follow-up in the Seniors ENRICA-1 cohort participants (N = 1880). Abbreviations: OR odds ratio, CI confidence interval, hPDI healthful Plant-based Diet Index, uPDI unhealthful Plant-based Diet Index. Adjusted for sex, age, educational level (primary, secondary, university), alcohol consumption, smoking status (current, former, never), BMI (< 25, 25–29.9, ≥ 30), energy intake, physical activity, prevalent diseases (type 2 diabetes mellitus, cardiovascular disease [myocardial infarction, stroke, or heart failure], chronic lung disease [asthma or chronic obstructive pulmonary disease], osteomuscular disease [osteoarthritis, rheumatoid arthritis or hip fracture], cancer and depression), number of medicines consumed (0, 1–3, 4–6, > 6)
In addition, we found an association between higher consumption of overall healthy plant food and lower risk of frailty (adjusted OR [95% CI] for highest vs. lowest tertile: 0.39 [0.23–0.66]; p-trend < 0.001). Conversely, higher consumption of unhealthy plant foods was associated with higher risk of frailty (2.40 [1.23–4.71]; p-trend = 0.01) (Table 2).
PDIs and frailty criteria
When we analyzed the association between the Fried criteria and PDIs (Table 3), we found an association between the uPDI and three criteria: exhaustion (adjusted OR [95% CI] for highest vs. lowest tertile: 1.72 [1.19–2.50], p-trend = 0.005), slow walking speed (1.60 [1.13–2.28], p-trend = 0.003), and unintentional weight loss (1.89 [1.21–2.97], p-trend = 0.006).
Table 3.
Odds ratios (95% CI) for the occurrence of each frailty criterion by tertiles of plant-based diet indices, over 3.3 years of follow-up in the Seniors ENRICA-1 cohort
| Plant-based diet indices | ||||
|---|---|---|---|---|
| Tertile 1 (lowest) | Tertile 2 | Tertile 3 (highest) | p-trend | |
| Exhaustion (N = 1880) | ||||
| n/N | 53/429 | 109/765 | 89/686 | |
| hPDI | Ref | 0.99 (0.67–1.46) | 0.83 (0.55–1.25) | 0.307 |
| n/N | 92/879 | 86/639 | 73/362 | |
| uPDI | Ref | 1.19 (0.85–1.66) | 1.72 (1.19–2.50) | 0.005 |
| Low physical activity (N = 1880) | ||||
| n/N | 80/429 | 122/765 | 94/686 | |
| hPDI | Ref | 0.89 (0.63–1.24) | 0.79 (0.55–1.14) | 0.212 |
| n/N | 123/879 | 114/639 | 59/362 | |
| uPDI | Ref | 1.29 (0.96–1.73) | 1.02 (0.70–1.47) | 0.630 |
| Low walking speed (N = 1855) | ||||
| n/N | 75/423 | 107/755 | 97/677 | |
| hPDI | Ref | 0.75 (0.53–1.05) | 0.85 (0.60–1.22) | 0.486 |
| n/N | 103/872 | 109/626 | 67/357 | |
| uPDI | Ref | 1.54 (1.14–2.09) | 1.60 (1.13–2.28) | 0.003 |
| Unintentional weight loss (N = 1858) | ||||
| n/N | 41/425 | 60/755 | 47/678 | |
| hPDI | Ref | 0.79 (0.51–1.23) | 0.70 (0.43–1.13) | 0.150 |
| n/N | 55/865 | 52/633 | 41/360 | |
| uPDI | Ref | 1.34 (0.89–2.01) | 1.89 (1.21–2.97) | 0.006 |
| Muscle weakness (N = 1877) | ||||
| n/N | 132/428 | 275/764 | 244/ 685 | |
| hPDI | Ref | 1.03 (0.77–1.38) | 1.06 (0.78–1.44) | 0.700 |
| n/N | 279/878 | 230/637 | 142/362 | |
| uPDI | Ref | 1.01 (0.82–1.33) | 1.01 (0.75–1.36) | 0.883 |
Abbreviations: BMI body mass index, CI confidence interval, hPDI healthful Plant-based Diet Index, Ref. reference, uPDI unhealthful Plant-based Diet Index
All models: adjusted for sex, age, educational level (primary, secondary, university), alcohol consumption, smoking status (current, former, never), BMI (< 25, 25–29.9, ≥ 30), energy intake, physical activity, prevalent diseases (type 2 diabetes mellitus, cardiovascular disease [myocardial infarction, stroke, or heart failure], chronic lung disease [asthma or chronic obstructive pulmonary disease], osteomuscular disease [osteoarthritis, rheumatoid arthritis, or hip fracture], cancer, and depression), medicines consumption (0, 1–3, 4–6, > 6)
Significance of bold entries is p < 0.05
Discussion
In this cohort of community-dwelling older adults in Spain, higher adherence to the hPDI was associated with lower frailty risk. On the contrary, higher adherence to the uPDI was associated with higher frailty risk. Results were in the same direction for robust, morbidity-free, IADL-independent participants, when “unintentional weight loss” was excluded from frailty criteria, and when some foods from animal origin scored positively in the hPDI (egg, fish, and dairy).
Our findings are of major importance because: (1) they highlight the differential health effect of consuming healthy plant-derived foods (e.g., vegetables, fruits, whole grains, nuts) over unhealthy plant-derived (e.g., refined grains, sugary beverages) and animal foods; (2) a healthful plant-based diet is aligned with the EAT-LANCET commission recommendations for the sustainability of food production systems, since this kind of diets are concordant with feasible dietary guidelines in most countries [33]; and (3) they shed light into the controversial perils of insufficient animal-based protein intake in older adults [34], as the hPDI does not exclude, but rather scores reversely animal food consumption.
To our knowledge, this is the first study that assesses the associations between plant-based diets and frailty in a Mediterranean older population. Nonetheless, our results are consistent with previous literature. One study in a cohort of 14,159 Chinese adults, aged 45–74 years, found that higher adherence to a healthy plant-based diet was associated with higher odds of healthy aging after 20 years (although the “healthy aging” criteria were different than the frailty phenotype used here) [35], and an analysis of pooled data from three European cohorts (Seniors ENRICA-1, 3C Bordeaux, and AMI) found an inverse dose–response relationship between consumption of fruits and vegetables and frailty risk [6]. Similar results were found in a cohort of US women aged > 60 years [8]. In addition to the protective effect of vegetables consumption, we also found an inverse association between vegetable oils and frailty. In Spain, the primary source of oil consumption is olive oil, in our cohort represents 90% of this group. In fact, a recent publication in the Seniors-ENRICA-1 cohort showed that the consumption of olive oil, especially virgin oil, was associated with lower risk of frailty (OR for ≈3 vs ≈1 tablespoons/day: 0.47 [0.29, 0.78]) in comparison with lower consumption [36].
In addition, in the same cohort, recent research showed that higher adherence to a Mediterranean lifestyle was associated with lower risk of frailty [37]. Specifically, the block of Mediterranean food consumption was independently associated with lower risk of frailty. Although the Mediterranean diet shares common components of the plant-based diet, they differ in some features such as the culinary traditions of the Mediterranean diet with the use of abundant extra-virgin olive oil and moderate wine drinking at meals (which is not included in the hPDI). Although, most of the functional properties of the plant-based foods included in both dietary patterns could explain the association with frailty, our results highlight that the quality of those plant-based foods is also important since unhealthy plant foods had the largest effect on frailty maybe due to the ultra-processed nature of most of the foods.
Our results for the uPDI and unhealthy plant foods are in the same direction of other studies suggesting that higher consumption of potatoes [38], sugar-sweetened beverages [39], and fruit juices [40] was associated with higher frailty risk.
Of note is that we did not find a clear association between animal-derived foods and frailty. This may be due to the myriad of foods included within this block, many of which have opposite effects. For instance, in the Seniors ENRICA-1 higher consumption of low-fat dairy products was inversely associated with frailty risk [41], and elevated intake of fish and blue fish was inversely associated with the accumulation of health deficits in older adults [30]; however, higher consumption of processed meat was associated with a higher frailty risk [10]. In fact, we found that a modified hPDI with positive scores to milk, eggs, and fish was more strongly and still inversely associated with frailty risk.
Finally, regarding each criterion of the frailty index, although the strength with which both indices were associated with frailty was similar, we found an inverse association only between the uPDI and some frailty criteria. This could indicate that the hPDI dietary pattern is most likely associated with the whole frailty syndrome since it better captures a patient’s overall health condition than its independent components.
Future studies should assess additional aspects for PDIs, such as its implementation along with caloric restrictions, different macronutrient balance, or changing time of eating; prior works have found that age-related impairments could be prevented with these strategies [42], and taking together, diet and its associated habits could complement each other to manage healthy aging.
Plausible biological mechanisms
The protective effect of hPDI on frailty might be due to the nutrient intake from some of its components. For example, the antioxidant effects of vitamins C and E, carotenoids, and selenium from fruits and vegetables may protect against sarcopenia by reducing the exposure of muscle fibers to oxidative stress [43, 44]. In addition, the contribution of proteins from legumes and nuts could help prevent sarcopenia [44]. Other mechanisms underlying our findings could involve the potential anti-inflammatory effect of fruits, olive oil, unsaturated fatty acids, nuts, or coffee, which may help reduce the low-grade chronic inflammation associated with frailty [45–48].
Regarding the uPDI, the often high refined and added sugar content, but low in fiber, of its components might contribute to its detrimental association with frailty [49]. Low dietary fiber has been found to be correlated to higher postprandial glycemia [50]. If plasma glucose levels are maintained over time, they could be a risk factor for frailty in non-diabetic older adults [51]. In addition, these sugars are risk factors for health issues which have been also associated to higher frailty risk, like insulin resistance and metabolic syndrome [52] or dysregulation of the glucose hormones dynamics [53].
On the other hand, the food groups included in the uPDI are deficient in certain ingredients, being perhaps related to the subsequent frailty risk, too. Refined grains lack both germ and bran, which are the primary source of several phytochemicals and other antioxidants (e.g., flavonoids, zeaxanthin, lutein, and β-cryptoxanthin) [54]. Similarly, fruit juices lack phytochemicals and fiber that whole fruits hold. A diet rich in these foods rather than its complete counterparts might lack enough antioxidant and anti-inflammatory molecules, which would redound in long-term poorer physical health. However, it is certain that refined grains alone were not associated to frailty in our study, maybe because the individual effect of food groups is small when we account holistically for dietary patterns, and they were one of the primary sources of vegetal protein in a previous study using this cohort evaluating the role of vegetable vs. animal proteins and healthy aging [53]. Additionally, functional foods could play antagonic or summatory effects on health, for example modulating the epigenome [55] and ultimately health. Anyway, further research is needed to understand the underlying mechanisms of the PDIs-frailty association.
Strengths and limitations
Strengths of this study include its prospective design, the use of measured data whenever possible (e.g., gait speed, grip strength, and BMI), and the reliance in validated tools when collecting self-reported information (e.g., food consumption was recorded with a validated diet history) [22]. Nevertheless, some limitations should be noted. First, self-reported data on diet, physical activity, and chronic diseases could lead to some misclassification and bias. However, if it were the case, it would most likely be non-differential, thus driving the study associations towards the null. Second, lifestyle was only assessed at one point; hence, we cannot evaluate the effect of lifestyle changes. Third, it is possible for a healthy diet to be framed in a healthy lifestyle that also influences frailty risk. Fourth, the analytical sample came from community-dwelling older adults; therefore, our results are not generalizable to institutionalized older adults. Finally, the presence of residual confounding cannot be ruled out; however, we did adjust for the most relevant confounders. Thus, further adjustment would not likely change the direction of associations.
Conclusion
In this cohort of community-dwelling Spanish older adults, higher adherence to the hPDI was associated with lower frailty risk, while the opposite was found for the uPDI. These results should be confirmed on other older populations within and without the Mediterranean basin; if this is the case, older adults adhering to a diet rich in healthy plants could be reassured that their diet protects them from physical impairment and frailty.
Supplementary Information
Below is the link to the electronic supplementary material.
Funding
Open Access funding provided thanks to the CRUE-CSIC agreement with Springer Nature. This work was supported by the Institute of Health Carlos III; the Secretary of R + D + I; the European Regional Development Fund/European Social Fund (FIS grant numbers 19/319, 20/896, FI29/00162 to MDV); the National Plan on Drugs (grant number 2020/17); Fundación Soria Melguizo (MITOFUN project); Ministry of Science, Innovation and Universities (grant number RYC 2018-02069I to MSP); Universidad Autónoma de Madrid (FPI contract to ACC). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Declarations
Conflict of interest
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.World Health Organization. Decade of healthy ageing: plan of action. 2020 [cited 2021 Aug 19]. Available from: https://www.who.int/publications/m/item/decade-of-healthy-ageing-plan-of-action.
- 2.Morley JE, Vellas B, van Kan GA, Anker SD. Frailty consensus: a call to action. J Am Med Dir Assoc. 2013;14(6):392–397. doi: 10.1016/j.jamda.2013.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dent E, Martin FC, Bergman H, Woo J, Romero-Ortuno R, Walston JD. Management of frailty: opportunities, challenges, and future directions. The Lancet. 2019;394(10206):1376–1386. doi: 10.1016/S0140-6736(19)31785-4. [DOI] [PubMed] [Google Scholar]
- 4.Oliveira JS, Pinheiro MB, Fairhall N, Walsh S, Chesterfield Franks T, Kwok W, et al. Evidence on physical activity and the prevention of frailty and sarcopenia among older people: a systematic review to inform the World Health Organization physical activity guidelines. J Phys Act Health. 2020;17(12):1247–1258. doi: 10.1123/jpah.2020-0323. [DOI] [PubMed] [Google Scholar]
- 5.Ortolá R, García-Esquinas E, García-Varela G, Struijk EA, Rodríguez-Artalejo F, López-García E. Influence of changes in diet quality on unhealthy aging: the Seniors-ENRICA cohort. Am J Med. 2019;132(9):1091–1102.e9. doi: 10.1016/j.amjmed.2019.03.023. [DOI] [PubMed] [Google Scholar]
- 6.García-Esquinas E, Rahi B, Peres K, Colpo M, Dartigues JF, Bandinelli S, et al. Consumption of fruit and vegetables and risk of frailty: a dose-response analysis of 3 prospective cohorts of community-dwelling older adults. Am J Clin Nutr. 2016;104(1):132–142. doi: 10.3945/ajcn.115.125781. [DOI] [PubMed] [Google Scholar]
- 7.Rashidi Pour Fard N, Amirabdollahian F, Haghighatdoost F. Dietary patterns and frailty: a systematic review and meta-analysis. Nutr Rev. 2019;77(7):498–513. doi: 10.1093/nutrit/nuz007. [DOI] [PubMed] [Google Scholar]
- 8.Fung TT, Struijk EA, Rodriguez-Artalejo F, Willett WC, Lopez-Garcia E. Fruit and vegetable intake and risk of frailty in women 60 years old or older. Am J Clin Nutr. 2020;112(6):1540–1546. doi: 10.1093/ajcn/nqaa256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kojima G, Avgerinou C, Iliffe S, Walters K. Adherence to Mediterranean diet reduces incident frailty risk: systematic review and meta-analysis. J Am Geriatr Soc. 2018;66:783–788. doi: 10.1111/jgs.15251. [DOI] [PubMed] [Google Scholar]
- 10.Struijk EA, Hagan KA, Fung TT, Hu FB, Rodríguez-Artalejo F, Lopez-Garcia E. Diet quality and risk of frailty among older women in the Nurses’ Health Study. Am J Clin Nutr. 2020;111(4):877–883. doi: 10.1093/ajcn/nqaa028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lopez-Garcia E, Hagan KA, Fung TT, Hu FB, Rodríguez-Artalejo F. Mediterranean diet and risk of frailty syndrome among women with type 2 diabetes. Am J Clin Nutr. 2018;107(5):763–771. doi: 10.1093/ajcn/nqy026. [DOI] [PubMed] [Google Scholar]
- 12.Ntanasi E, Yannakoulia M, Kosmidis MH. Adherence to Mediterranean diet and frailty. J Am Med Dir Assoc. 2017;19(4):315–322.e2. doi: 10.1016/j.jamda.2017.11.005. [DOI] [PubMed] [Google Scholar]
- 13.León-Muñoz LM, Garcia-Esquinas E, Lopez-Garcia E, Banegas JR, Rodríguez-Artalejo F. Major dietary patterns and risk of frailty in older adults: a prospective cohort study. BMC Med. 2015;13(11). [DOI] [PMC free article] [PubMed]
- 14.Alaghehband FR, Erkkilä AT, Rikkonen T. Association of Baltic Sea and Mediterranean diets with frailty phenotype in older women Kuopio, OSTPRE-FPS study. Eur J Nutr. 2021;60:821–831. doi: 10.1007/s00394-020-02290-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ward RE, Orkaby AR, Chen J, Hshieh TT, Driver JA, Gaziano JM, et al. Association between diet quality and frailty prevalence in the physicians’ health study. J Am Geriatr Soc. 2020;68(4):770–776. doi: 10.1111/jgs.16286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Satija A, Bhupathiraju SN, Rimm EB, Spiegelman D, Chiuve SE, Borgi L, et al. Plant-based dietary patterns and incidence of type 2 diabetes in US men and women: results from three prospective cohort studies. Moore SC, editor. PLoS Med. 2016;13(6):e1002039. doi: 10.1371/journal.pmed.1002039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chen Z, Drouin-Chartier JP, Li Y, Baden MY, Manson JE, Willett WC, et al. Changes in plant-based diet indices and subsequent risk of type 2 diabetes in women and men: three U.S. prospective cohorts. Diabetes Care. 2021;44(3):663–71. doi: 10.2337/dc20-1636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Aljuraiban G, Chan Q, Gibson R, Stamler J, Daviglus ML, Dyer AR, et al. Association between plant-based diets and blood pressure in the INTERMAP study. BMJNPH. 2020;3(2):133–142. doi: 10.1136/bmjnph-2020-000077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Satija A, Bhupathiraju SN, Spiegelman D, Chiuve SE, Manson JE, Willett W, et al. Healthful and unhealthful plant-based diets and the risk of coronary heart disease in U.S. adults. J Am Coll Cardiol. 2017;70(4):411–22. doi: 10.1016/j.jacc.2017.05.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Baden MY, Liu G, Satija A, Li Y, Sun Q, Fung TT, et al. Changes in plant-based diet quality and total and cause-specific mortality. Circulation. 2019;140(12):979–991. doi: 10.1161/CIRCULATIONAHA.119.041014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rodríguez-Artalejo F, Graciani A, Guallar-Castillón P, León-Muñoz LM, Zuluaga MC, López-García E, et al. Rationale and methods of the study on nutrition and cardiovascular risk in Spain (ENRICA) Rev Esp Cardiolog English Ed. 2011;64(10):876–882. doi: 10.1016/j.recesp.2011.05.019. [DOI] [PubMed] [Google Scholar]
- 22.Guallar-Castillón P, Sagardui-Villamor J, Balboa-Castillo T, Sala-Vila A, ArizaAstolfi MJ, SarriónPelous MD, et al. Validity and reproducibility of a Spanish dietary history. Tomé D, editor. PLoS One. 2014;9(1):e86074. doi: 10.1371/journal.pone.0086074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56(3):M146–M157. doi: 10.1093/gerona/56.3.m146. [DOI] [PubMed] [Google Scholar]
- 24.Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1(3):385–401. [Google Scholar]
- 25.Washburn RA, Smith KW, Jette AM, Janney CA. The physical activity scale for the elderly (PASE): development and evaluation. Clin Epidemiol. 1993;46(2):153–162. doi: 10.1016/0895-4356(93)90053-4. [DOI] [PubMed] [Google Scholar]
- 26.Guralnik JM, Simonsick EM, Ferrucci L, Glynn RJ, Berkman LF, Blazer DG, et al. A Short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994;49(2):M85–94. doi: 10.1093/geronj/49.2.m85. [DOI] [PubMed] [Google Scholar]
- 27.Ottenbacher KJ, Branch LG, Ray L, Gonzales VA, Peek MK, Hinman MR. The reliability of upper- and lower-extremity strength testing in a community survey of older adults. Arch Phys Med Rehabil. 2002;83(10):1423–1427. doi: 10.1053/apmr.2002.34619. [DOI] [PubMed] [Google Scholar]
- 28.Wareham NJ, Jakes RW, Rennie KL, Schuit J, Mitchell J, Hennings S, et al. Validity and repeatability of a simple index derived from the short physical activity questionnaire used in the European Prospective Investigation into Cancer and Nutrition (EPIC) study. Public Health Nutr. 2003;6(4):407–413. doi: 10.1079/PHN2002439. [DOI] [PubMed] [Google Scholar]
- 29.León-Muñoz LM, Guallar-Castillón P, López-García E, Rodríguez-Artalejo F. Mediterranean diet and risk of frailty in community-dwelling older adults. J Am Med Dir Assoc. 2014;15(12):899–903. doi: 10.1016/j.jamda.2014.06.013. [DOI] [PubMed] [Google Scholar]
- 30.García-Esquinas E, Ortolá R, Banegas JR, Lopez-García E, Rodríguez-Artalejo F. Dietary n-3 polyunsaturated fatty acids, fish intake and healthy ageing. Int J Epidemiol. 2019;48(6):1914–1924. doi: 10.1093/ije/dyz196. [DOI] [PubMed] [Google Scholar]
- 31.Smith A, Gray J. Considering the benefits of egg consumption for older people at risk of sarcopenia. Br J Community Nurs. 2016;21(6):305–309. doi: 10.12968/bjcn.2016.21.6.305. [DOI] [PubMed] [Google Scholar]
- 32.Cuesta-Triana F, Verdejo-Bravo C, Fernández-Pérez C, Martín-Sánchez FJ. Effect of milk and other dairy products on the risk of frailty, sarcopenia, and cognitive performance decline in the elderly: a systematic review. Adv Nutr. 2019;10(suppl_2):S105–19. doi: 10.1093/advances/nmy105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Willett W, Rockström J, Loken B, Springmann M, Lang T, Vermeulen S, et al. Food in the Anthropocene: the EAT–Lancet Commission on healthy diets from sustainable food systems. The Lancet. 2019;393(10170):447–492. doi: 10.1016/S0140-6736(18)31788-4. [DOI] [PubMed] [Google Scholar]
- 34.Berrazaga I, Micard V, Gueugneau M, Walrand S. The role of the anabolic properties of plant- versus animal-based protein sources in supporting muscle mass maintenance: a critical review. Nutrients. 2019;11(8):1825. doi: 10.3390/nu11081825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zhou YF, Song XY, Wu J, Yuan JM, Pan A, Koh WP. Association between dietary patterns in midlife and healthy ageing in Chinese adults: the Singapore Chinese health study. J Am Med Dir Assoc. 2021;22(6):1279–1286. doi: 10.1016/j.jamda.2020.09.045. [DOI] [PubMed] [Google Scholar]
- 36.Donat-Vargas C, Dominguez LJ, Sandoval-Insausti H, Moreno-Franco B, Rodríguez-Ayala M, Rey-Garcia J, et al. Olive oil consumption is associated with lower frailty risk: a prospective cohort study of community-dwelling older adults. Age Ageing. 2021; In press. [DOI] [PubMed]
- 37.Maroto-Rodriguez J, Delgado-Velandia M, Ortolá R, García-Esquinas E, Martinez-Gomez D, Struijk EA, et al. A Mediterranean lifestyle and frailty incidence in older adults: the Seniors-ENRICA-1 cohort. J Gerontol: Ser A. 2021;glab292. [DOI] [PubMed]
- 38.O’Connell ML, Coppinger T, Lacey S, Walton J, Arsenic T, McCarthy AL. Associations between food group intake and physical frailty in Irish community-dwelling older adults. Nutr Metab Insights. 2021;14:117863882110064. doi: 10.1177/11786388211006447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Struijk EA, Rodríguez-Artalejo F, Fung TT, Willett WC, Hu FB, Lopez-Garcia E. Sweetened beverages and risk of frailty among older women in the Nurses’ Health Study: a cohort study. Brayne C, editor. PLoS Med. 2020;17(12):e1003453. doi: 10.1371/journal.pmed.1003453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ribeiro SML, Morley JE, Malmstrom TK, Miller DK. Fruit and vegetable intake and physical activity as predictors of disability risk factors in African-American middle-aged individuals. J Nutr Health Aging. 2016;20(9):891–896. doi: 10.1007/s12603-016-0780-4. [DOI] [PubMed] [Google Scholar]
- 41.Lana A, Rodriguez-Artalejo F, Lopez-Garcia E. Dairy consumption and risk of frailty in older adults: a prospective cohort study. J Am Geriatr Soc. 2015;63(9):1852–1860. doi: 10.1111/jgs.13626. [DOI] [PubMed] [Google Scholar]
- 42.Di Francesco A, Di Germanio C, Bernier M, de Cabo R. A time to fast. Science. 2018;362(6416):770–5. doi: 10.1126/science.aau2095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Semba RD, Lauretani F, Ferrucci L. Carotenoids as protection against sarcopenia in older adults. Arch Biochem Biophys. 2007;458(2):141–145. doi: 10.1016/j.abb.2006.11.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kojima G, Avgerinou C, Iliffe S, Jivraj S, Sekiguchi K, Walters K. Fruit and vegetable consumption and frailty: a systematic review. J Nutr Health Aging. 2018;22(8):1010–1017. doi: 10.1007/s12603-018-1069-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Liu RH. Health-promoting components of fruits and vegetables in the diet. Adv Nutr. 2013;4(3):384S–392S. doi: 10.3945/an.112.003517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Urpi-Sarda M, Casas R, Chiva-Blanch G, Romero-Mamani ES, Valderas-Martínez P, Arranz S, et al. Virgin olive oil and nuts as key foods of the Mediterranean diet effects on inflammatory biomarkers related to atherosclerosis. Pharmacol Res. 2012;65(6):577–583. doi: 10.1016/j.phrs.2012.03.006. [DOI] [PubMed] [Google Scholar]
- 47.Leitzmann C. Characteristics and health benefits of phytochemicals. Complement Med Res. 2016;23(2):69–74. doi: 10.1159/000444063. [DOI] [PubMed] [Google Scholar]
- 48.Marcos-Pérez D, Sánchez-Flores M, Proietti S, Bonassi S, Costa S, Teixeira JP, et al. Association of inflammatory mediators with frailty status in older adults: results from a systematic review and meta-analysis. GeroScience. 2020;42(6):1451–1473. doi: 10.1007/s11357-020-00247-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Laclaustra M, Rodriguez-Artalejo F, Guallar-Castillon P, Banegas JR, Graciani A, Garcia-Esquinas E, et al. Prospective association between added sugars and frailty in older adults. Am J Clin Nutr. 2018;107(5):772–779. doi: 10.1093/ajcn/nqy028. [DOI] [PubMed] [Google Scholar]
- 50.Sato K, Sasaki M, Nishimura M, Yamauchi T. Correlation between habitual dietary fibre intake and postprandial plasma glucose levels in early adulthood. Ann Hum Biol. 2019;46(4):340–346. doi: 10.1080/03014460.2019.1657949. [DOI] [PubMed] [Google Scholar]
- 51.Zaslavsky O, Walker RL, Crane PK, Gray SL, Larson EB. Glucose levels and risk of frailty. J Gerontol A Biol Sci Med Sci. 2016;71(9):1223–1229. doi: 10.1093/gerona/glw024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Pérez-Tasigchana RF, León-Muñoz LM, Lopez-Garcia E, Gutierrez-Fisac JL, Laclaustra M, Rodríguez-Artalejo F, et al. Metabolic syndrome and insulin resistance are associated with frailty in older adults: a prospective cohort study. Age Ageing. 2017;46(5):807–812. doi: 10.1093/ageing/afx023. [DOI] [PubMed] [Google Scholar]
- 53.Kalyani RR, Varadhan R, Weiss CO, Fried LP, Cappola AR. Frailty status and altered glucose-insulin dynamics. J Gerontol A Biol Sci Med Sci. 2012;67(12):1300–1306. doi: 10.1093/gerona/glr141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Liu RH. Whole grain phytochemicals and health. J Cereal Sci. 2007;46(3):207–219. [Google Scholar]
- 55.Lionetti V, Tuana BS, Casieri V, Parikh M, Pierce GN. Importance of functional food compounds in cardioprotection through action on the epigenome. Eur Heart J. 2019;40(7):575–582. doi: 10.1093/eurheartj/ehy597. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.