Abstract
Background: Schizophrenia (SZ) is a severe psychiatric disorder typically characterized by multidimensional psychotic syndromes. Electroconvulsive therapy (ECT) is a treatment option for medication-resistant patients with SZ or treating acute symptoms. Although the efficacy of ECT has been demonstrated in clinical use, its therapeutic mechanisms in the brain remain elusive.
Objective: This study aimed to summarize brain changes on structural magnetic resonance imaging (sMRI) and functional MRI (fMRI) after ECT.
Methods: According to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines, a systematic review was carried out. The PubMed and Medline databases were systematically searched using the following medical subject headings (MeSH): (electroconvulsive therapy OR ECT) AND (schizophrenia) AND (MRI OR fMRI OR DTI OR DWI).
Results: This review yielded 12 MRI studies, including 4 with sMRI, 5 with fMRI and 3 with multimodal MRI. Increases in volumes of the hippocampus and its adjacent regions (parahippocampal gyrus and amygdala), as well as the insula and frontotemporal regions, were noted after ECT. fMRI studies found ECT-induced changes in different brain regions/networks, including the hippocampus, amygdala, default model network, salience network and other regions/networks that are thought to highly correlate with the pathophysiologic characteristics of SZ. The results of the correlation between brain changes and symptom remissions are inconsistent.
Conclusion: Our review provides evidence supporting ECT-induced brain changes on sMRI and fMRI in SZ and explores the relationship between these changes and symptom remission.
Keywords: Electroconvulsive therapy, schizophrenia, functional MRI, neuroimaging, hippocampus, connectivity
1. INTRODUCTION
Schizophrenia (SZ) is a severe psychiatric disorder typically characterized by multidimensional psychotic syndromes, such as positive and negative symptoms (i.e., delusion, hallucination and disorganized behaviour), as well as affective and cognitive disturbances [1]. Electroconvulsive therapy (ECT) is a treatment option for particular clinical conditions, such as catatonic symptoms, suicidality or acute symptoms [2]. In addition, accumulating evidence supports the use of ECT for medication-resistant patients with SZ [3]. A Cochrane review indicated that treatment with ECT significantly results in clinical improvement compared with placebo or sham ECT [4]. A meta-analysis suggests that ECT may represent an effective clozapine augmentation strategy in medication-resistant cases [5]. Recently, findings from a growing number of studies have suggested that ECT combined with antipsychotic medication may be considered an option for patients with SZ who show limited response to medication alone [6].
Although the efficacy of ECT has been demonstrated in clinical use, the therapeutic mechanisms in the brain remain elusive. One possible mechanism is neuroplasticity. This hypothesis is supported by findings from animal studies, indicating that electroconvulsive seizures (the analogy of ECT in animal models) affect many neuroplastic processes, including neurogenesis [7, 8], synaptogenesis [9], angiogenesis [10], gliogenesis [11] and other neuronal/axonal changes [12, 13]. Studies in humans have also reported the effects of ECT on neuroplasticity, including changes in hippocampal/amygdala volumes [14] and increases in the secretion of brain-derived neurotrophic factor (BDNF) [15]. In addition to neuroplasticity, several clinical studies have suggested that ECT may enhance dopamine D2 receptor efficacy [16]. Although the mechanism of ECT is complex, increasing evidence suggests that the reorganization of brain structure or connectivity by ECT may represent one of the mechanisms [14, 17, 18].
Neuroimaging is a robust technology and has recently been widely used to investigate the pathological mechanisms in the SZ brain [19]. Structural magnetic resonance imaging (sMRI) and functional MRI (fMRI) have revealed abnormalities in a multitude of regions and networks in SZ [20-24]. Structural morphometry studies showed widespread grey matter atrophy in cortical and subcortical regions, including the hippocampus, insula, thalamus, temporal and frontal lobes, in patients with SZ [25, 26]. Accumulating fMRI studies also identified aberrant functional connectivity (FC) among these regions [27-30], suggesting that psychotic syndromes in SZ may be related to disturbances in the cortico-cortical (subcortico-cortical) systems at the neuroimaging level [31]. These findings support a dysconnectivity hypothesis during the neural developmental process that has been demonstrated to be highly relevant to SZ neuropathology [32]. The dysconnectivity hypothesis posits that inefficient or ineffective interaction within large-scale functional networks is one of the indicators in the neuropathology of SZ [32].
To our knowledge, there is no review focusing on sMRI and fMRI changes in SZ patients following ECT. In this mini-review, we reported summaries of MRI studies that investigated brain changes due to ECT in patients with SZ from the following aspects: (1) ECT-induced structural changes in sMRI; (2) ECT-induced functional changes by fMRI; and (3) whether these changes correlate with symptom remission. An additional aim was to examine whether ECT outcomes can be predicted based on pre-ECT MRI. Finally, we sought to clarify some brain mechanisms of ECT.
2. METHODS
A systematic review of the international literature was performed based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (PRISMA flowchart, Fig. 1) [33]. Studies were selected through a standard search of the bibliographic search engines PubMed and Medline using the following medical subject headings (MeSH): (electroconvulsive therapy OR ECT) AND (schizophrenia) AND (MRI OR fMRI OR DTI OR DWI). The research focused on papers published up to 30 October 2020. Our inclusion criteria were as follows: (1) ECT-treated subjects were diagnosed with SZ; (2) SZ patients were scanned by sMRI or fMRI; (3) publications that were full-text articles (i.e., no abstracts, conference reports, or other publication types); (4) articles were written in English. The exclusion criteria were as follows: (1) studies that did not include patients with SZ who treated by ECT; (2) studies that did not use sMRI or fMRI or DTI; (3) articles that were reviews or case reports. Two researchers (YJ and CL) independently reviewed full-text articles to decide whether a study met the inclusion criteria of the review and discussed inconsistencies until consensus was obtained. The reference lists of the included papers were manually examined to increase the number of studies. Two researchers (YJ and HH) worked independently to extract study details, including demographics of participants, clinical information, ECT parameters (Table 1), MRI scanning information, image processing method and MRI main findings (Table 2). A third researcher (CL) reviewed the data extraction and resolved conflicts.
Fig. (1).
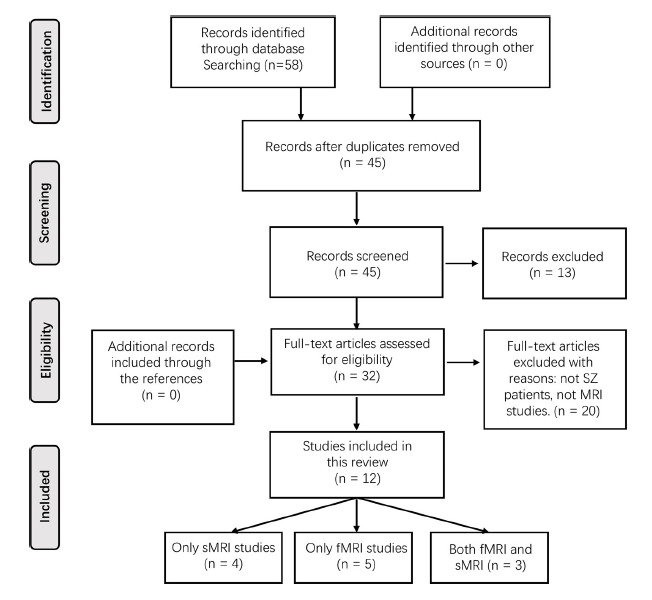
Flowchart illustrating the study selection. Abbreviations: sMRI: structural magnetic resonance imaging, fMRI: functional magnetic resonance imaging, SZ: schizophrenia.
Table 1.
Demographics of participants, clinical information and ECT parameters for each included study.
| Study | Participants | ECT | |||||||
|---|---|---|---|---|---|---|---|---|---|
| ECT Patients | Comparisons | Diagnosis | Age, Years: Mean (s.d.) | Female | Medication | Clinical Assessment (PANSS Total Score) | Electrode Placement | Mean (s.d.) Number of ECT Interventions | |
| Wolf et al. [34] | 8 SZ, 2 scans | 10 MDD, 2 scans; 10 HC, 1 scan |
DSM-IV | 31.1 (8.4) | 3 | Yes | Pre-ECT: 76.4 (22.0); Post-ECT: 35.8 (29.3); Reduction: 87.5% |
RUL | 12.4 (1.8) |
| Wang et al. [35] | 21 SZ, 2 scans | 21 SZ (no ECT), 2 scans; 23 HC, 1 scan |
SCID-I/P | 29.29 (7.1) | 11 | Yes | Pre-ECT: 71.6 (8.4); Post-ECT: 49.7 (9.6); Reduction: 52.6% |
BL | 11.5 (1.1) |
| Gong et al. [36] | 33 TRS, 1 scan; 20 AE, 1 scan; 4 SA, 1 scan. |
None | DSM-IV-TR | TRS, 31.5 (10.6); AE, 27.5 (6.0); SA, 34.5 (9.7) |
TRS, 9; AE, 9; SA, 2 |
Yes | Pre-ECT: TRS, 94.2 (18.0); AE, 101.1 (22.6); SA, 88.3 (21.9); Post-ECT: TRS, 51.6 (16.9); AE, 52.8 (14.6); SA, 54.5 (23.2); Reduction: TRS, 67.4%; AE, 67.5%; SA, 62.8% |
BL | 10.5 (2.4) |
| Xi et al. [37] | 57 SZ, 1 scan | None | DSM-IV-TR | RS: 31.0 (10.2); NRS: 29.7 (8.5) |
20 | Yes | Pre-ECT: RS, 94.1 (19.2); NRS, 98.7 (21.0); Post-ECT: RS, 40.0 (7.1); NRS, 63.7 (13.8); Reduction: RS, 84.7%; NRS, 51.0% |
UL | SR, 10.3 (2.0); NSR, 10.0 (2.9) |
| Huang et al. [38] | 21 SZ, 2 scans | 21 SZ (no ECT), 2 scans; 23 HC, 1 scan |
SCID-I/P | 29.29 (7.1) | 11 | Yes | Pre-ECT: 71.6 (8.4); Post-ECT: 49.7 (9.6); Reduction: 52.6% |
BL | 11.5 (1.1) |
| Li et al. [39] | 34 SZ, 29 SZ had 2 scans | 34 HC, 1 scan | SCID-I/P | 29.35 (8.47) | 24 | Yes | Pre-ECT: 82.43 (7.28); Post-ECT: 55.93 (12.26); Reduction: 42.4% |
BL | 9.1 (1.1) |
| Sambataro et al. [40] | 8 SZ, 2 scans | 10 MDD, 2 scans; 10 HC, 1 scan |
DSM-IV | 31.1 (8.4) | 3 | Yes | Pre-ECT: 76.4 (22.0); Post-ECT: 35.8 (29.3); Reduction: 87.5% |
RUL | 12.4 (1.8) |
| Wang et al. [41] | 21 SZ, 2 scans | 21 SZ (no ECT), 2 scans; 23 HC, 1 scan |
SCID-I/P | 29.29 (7.1) | 11 | Yes | Pre-ECT: 71.6 (8.4); Post-ECT: 49.7 (9.6); Reduction: 52.6% |
BL | 11.5 (1.1) |
| Yang et al. [42] | 47 SZ, 2 scans | none | ICD-10 | 30.23 (9.65) | 16 | Yes | Pre-ECT: 94.62 (18.87); Post-ECT: 51.62 (16.16); Reduction: 67.81%, range from 32% to 100% |
BL | 9.15 (2.21) |
| Thomann et al. [43] | 9 SZ, 2 scans | 12 MDD, 2 scans; 9 HC, 1 scan |
DSM-IV | 34.2 (12.3) | 3 | Yes | 4 response; 5 partial response |
RUL | 11.3 (1.7) |
| Jiang et al. [44] | 21 SZ, 2 scans | 21 SZ (no ECT), 2 scans; 23 HC, 1 scan |
SCID-I/P | 29.29 (7.1) | 11 | Yes | Pre-ECT: 71.6 (8.4); Post-ECT: 49.7 (9.6); Reduction: 52.6% |
BL | 11.5 (1.1) |
| Jiang et al. [45] | 21 SZ, 2 scans | 21 SZ (no ECT), 2 scans; 23 HC, 1 scan |
SCID-I/P | 29.29 (7.1) | 11 | Yes | Pre-ECT: 71.6 (8.4); Post-ECT: 49.7 (9.6); Reduction: 52.6% |
BL | 11.5 (1.1) |
Abbreviations: TRS: treatment-resistant schizophrenia, AE: schizophrenia patients with an acute episode, SA: schizophrenia patients with suicide attempts, MDD: major depressive disorder, HC: healthy control, RS: Responders, NRS: Non-Responders, BL: bilateral, RUL: right unilateral
Table 2.
MRI scanning information, image processing method and main MRI findings for each study.
| Study | Scan Since ECT | Images |
Image
Processing Methods |
Longitudinal Changes | Prediction | ||
|---|---|---|---|---|---|---|---|
| Structural MRI | Functional MRI | Correlation with Symptoms | |||||
| Wolf et al. [34] | S1: within 5 days before ECT; S2: 6-8 days after ECT. |
T1w MRI. | T1w MRI: Source-based morphometry (SBM). | ECT led to an increase in structural network strength in the MTL network and left DLPFC network. | No analysis. | There was a significant negative correlation between PANSS total score differences and left DLPFC network strength change. | No analysis. |
| Wang et al. [35] | S1: 24 h before ECT; S2: 24-48 h after ECT. |
T1w MRI. | T1w MRI: VBM analysis. | ECT induced increased volumes in bilateral parahippocampal gyrus/hippocampus, right temporal gyrus, and right insula. | No analysis. | There was a significant positive correlation of GM volume change in the right parahippocampal gyrus/hippocampus with the reduction of positive subscore. | No analysis. |
| Gong et al. [36] | Not reported. | T1w MRI, diffusion MRI. | Multi-parametric MRI-based radiomic features selection and SVR model. | No analysis. | No analysis. | No analysis. | The multi-parametric MRI-based radiomic model, including four structural features from the left inferior frontal gyrus, right insula, left middle temporal gyrus and right superior temporal gyrus and six diffusion features from tracts connecting frontal or temporal gyrus, possessed the RMSE of 14.98 in the test cohort. The Pearson's correlation coefficients between predicted and actual values were 0.777. |
| Xi et al. [37] | Not reported. | T1w MRI. | T1w MRI: VBM analysis and logistic regression model (LRM)/SVM. | No analysis. | No analysis. | No analysis. | The regularized multivariate LRM discriminated responders from nonresponders, with an accuracy of 90.91% in the training data and 87.59% in the validating data. The accuracy of the SVM in the training set was 90.91%, and the accuracy in the validation set was 91.78%. |
| Huang et al. [38] | S1: 24 h before ECT; S2: 24-48 h after ECT. |
rsfMRI. | rsfMRI: Voxel-wise global functional connectivity density (gFCD). | No analysis. | After ECT, gFCD increased in the DMN regions (medial frontal cortex and precuneus). | No significant correlations. | No analysis. |
| Li et al. [39] | Not reported. | rsfMRI. | rsfMRI: ICA, SVM pattern classification, and FC analysis. | No analysis. | After ECT, the DMN (posterior cingulate cortex), the temporal lobe network (left superior temporal gyrus) and the frontal-parietal network (right angular gyrus and middle frontal gyrus) increased, meanwhile, the FC in the corticostriatal network (right anterior cingulate cortex), the language network (left middle temporal gyrus) and the DMN (right precuneus) decreased. | No analysis. | No analysis. |
| Sambataro et al. [40] | S1: within 5 days before ECT; S2: 6-8 days after ECT. |
rsfMRI. | rsfMRI: ICA. | No analysis. | ECT resulted in increased independent component loadings in the MPFC within the DMN. | No significant correlations. | No analysis. |
| Wang et al. [41] | S1: 24 h before ECT; S2: 24-48 h after ECT. |
rsfMRI. | rsfMRI: Seed-based FC. | No analysis. | ECT induced increased FC between the right thalamus and right putamen and decreased FC between the thalamus and sensory cortex. | No significant correlations. | No analysis. |
| Yang et al. [42] | All patients underwent MRI scanning on the day before their first ECT session and the day after their last ECT session. | rsfMRI. | rsfMRI: ROI-based FC, LASSO feature selection and linear regression predictive model. | No analysis. | The FC between the right amygdala and left hippocampus decreased after ECT compared with the baseline. | The change of FC between the amygdala and hippocampus was positively correlated with the reduction of the PANSS total score. | The correlation coefficient between the predictive and real values of cross-validation was 0.7165. |
| Thomann et al. [43] | S1: within 5 days before ECT; S2: 6-8 days after ECT. |
T1w MRI, rsfMRI. | T1w MRI: VBM analysis; rsfMRI: Seed-based FC analysis. |
After ECT, increased GM volumes were found in the right amygdala, anterior part of hippocampus and insula. | RUL ECT was associated with changes in FC between the right amygdala and other cortical brain regions. However, these changes were not diagnosis-specific between SZ and major depression. | No significant correlations. | No analysis. |
| Jiang et al. [44] | S1: 24 h before ECT; S2: 24-48 h after ECT. |
T1w MRI, rsfMRI. | T1w MRI: ROI-based GM volume analysis; rsfMRI: Seed-based FC. |
Increased GM volumes of the left insula and bilateral posterior insula (PIns) were found after ECT. | After ECT, decreased FCs between the PIns and middle occipital gyrus and obitofrontal cortex were found. | The PANSS reductions were correlated with the PIns volume increases and FC changes following ECT. | No analysis. |
| Jiang et al. [45] | S1: 24 h before ECT; S2: 24-48 h after ECT. |
T1w MRI, rsfMRI. | T1w MRI: longitudinal segmentation of hippocampal substructures by Freesurfer; rsfMRI: Seed-based FC. |
ECT-induced volume increases in the bilateral hippocampus and certain subfields for both the remitters and nonremitters. | After ECT, the remitters exhibited increased FC between the hippocampus and prefrontal cortex as well as between the hippocampus and regions in DMN. The nonremitters showed decreased FC in the hippocampus and primary sensory network. | The general psychopathology reductions were associated with the left CA4 volume increase and the FC between the left caudal hippocampus and right angular gyrus. | No analysis. |
Abbreviations: T1w MRI: T1 weighted structural MRI, rsfMRI: resting-state functional MRI, ICA: independent component analysis, SVM: support vector machine, SVR: support vector regression, FC: functional connectivity, VBM: voxel-based morphometry, GM: gray matter, ROI: region of interest, MTL: medial temporal lobe, DLPFC: dorsal lateral prefrontal cortex, DMN: default mode network, MPFC: medial prefrontal cortex.
3. RESULTS
Fig. (1) shows the procedure for study selection, which yielded 12 MRI studies comprising 4 with sMRI [34-37], 5 with fMRI [38-42] and 3 with multimodal MRI data [43-45]. Table 1 reports the demographics of the participants, clinical information and ECT parameters for each study. Table 2 describes the MRI scanning information, image processing method and summarized MRI main findings for each study.
3.1. Brain Structural MRI Changes Induced by ECT
Table 2 shows that five structural MRI studies investigated brain morphological changes before and after ECT intervention. Three studies used the data-driven method to investigate the voxel-wise grey matter (GM) volume changes within the whole brain [34, 35, 43]. Two studies applied the region of interest (ROI) -driven method to examine the volume changes in specific regions (hippocampus and insula) [44, 45]. All these studies show structural changes following ECT.
3.1.1. Hippocampus
Several studies [34, 35, 43, 45] have indicated ECT-induced volume changes in the hippocampus and its adjacent regions, including the parahippocampal gyrus and amygdala, in SZ patients (Table 2). A consistent increase in hippocampal volume was noted in patients with SZ following ECT compared with baseline [34, 35, 43, 45]. No studies have reported a reduced hippocampal volume after ECT. Consistent with the observation of increased volume in the hippocampus due to ECT, accumulated evidence has shown the same structural changes in major depressive disorder (MDD) patients undergoing ECT intervention [14, 17, 46]. Thomann et al. [43] and Wolf et al. [34] investigated structural changes in GM volume using two different MRI analysis methods. Using source-based morphometry (SBM) analysis, they reported that the medial temporal lobe network showed a significant volume increase in two diagnostic groups of SZ and MDD after unilateral ECT [34]. In another study [43], GM volumes quantified by voxel-based morphometry (VBM) were increased in the right anterior part of the hippocampus and right amygdala in both diagnostic groups following ECT. These findings suggested a shared mechanism of ECT action on hippocampal volume changes across clinical diagnoses. Recently, Wang et al. [35] compared the longitudinal GM volume changes between the two groups of SZ patients. One patient group received a four-week bitemporal ECT series in addition to antipsychotic drugs, and the other group only received antipsychotic treatment. The GM volumes were analysed by VBM. The hippocampus and bilateral parahippocampal gyrus exhibited increased volumes within ECT-treated patients, but a decrease amongst the patients treated only with antipsychotics. Based on the same dataset, Jiang et al. [45] analysed hippocampal substructures using FreeSurfer (version 6.0, http://surfer.nmr.mgh.harvard.edu/), another conventional tool to segment the hippocampus and estimate the volumes of subfields. The whole hippocampus was further segmented into twelve subfields for each hemisphere, including the hippocampal tail, subiculum, presubiculum, parasubiculum, cornu ammonis area 1 (CA1), CA3, CA4, hippocampal fissure, granular cell layer of the dentate gyrus (GC-MLDG), molecular layer, hippocampus-amyg- dala transition area (HATA) and fimbria. Statistical analyses revealed increased bilateral hippocampal whole volumes and certain subfields in SZ patients following ECT, which were not observed in patients treated exclusively with antipsychotics. These distinguished changes demonstrated that the increased hippocampal volume is the specific ECT effect rather than the effect of antipsychotic therapy. In total, neuroimaging findings provided strong evidence supporting the increased hippocampal volume induced by ECT, which is not dependent on stimulus site (unilateral or bilateral) or neuroimaging analytic methods.
3.1.2. Insula
Three of the previously published studies reported increased volume in the insula in SZ after ECT (Table 2). Using VBM analysis on structural MRI, Thomann et al. [43] and Wang et al. [35] found an increased GM volume of the voxels within the right insula in SZ at post-ECT compared with pre-ECT. Jiang et al. [44] functionally parcellated the bilateral insula into six subregions (i.e., the bilateral dorsal anterior [dAIns], ventral anterior [vAIns] and posterior insula [PIns]) using K-means clustering on fMRI. The averaged GM volume in each subregion was extracted. The ECT-treated patients with SZ exhibited an increased GM volume in the bilateral PIns, whereas SZ patients treated exclusively with antipsychotics showed decreased GM volume compared with pretreatment volume. Volume changes in the whole insula were analysed, yielding results consistent with those noted in the PIns.
3.1.3. Other Regions
In addition to focusing on the hippocampus and insula, two studies using the whole brain data-driven method found structural changes in frontal and temporal regions in patients with SZ after ECT intervention. For example, Wolf et al. reported that the left dorsal lateral prefrontal cortex (DLPFC) exhibited a volume increase in SZ patients treated by ECT [34]. Wang et al. found increased GM volumes in the right temporal pole and right superior temporal gyrus in SZ after ECT [35].
3.2. Brain Functional MRI Changes Induced by ECT
Table 2 shows that 8 functional MRI studies investigated ECT-induced brain functional changes. Three studies [38-40] used the data-driven method (independent component analysis [ICA] and global functional connectivity density [gFCD]) to investigate FC changes within the whole brain. Five studies applied the ROI-driven method (i.e., seed-based FC) to examine the changes in FC in specific regions (hippocampus, amygdala, insula and thalamus) [41-45]. All these studies reported functional MRI changes following ECT.
3.2.1. Default Mode Network
The default mode network (DMN), which is composed of the posterior cingulate cortex (PCC), medial prefrontal cortex (MPFC), angular gyrus and medial temporal lobes, is involved in monitoring self-referential mental processes [47]. Disruption of the DMN is associated with pathological processes in SZ [48-50]. Huang et al. [38] applied gFCD, a data-driven graph-based measure of whole-brain FC, to quantify the centrality of the brain network voxelwise [51]. Regions with high gFCD values have been previously reported to be functional network hubs that play prominent roles in cognitive, affective and sensory functions [52]. Huang et al. found that compared with routine pharmacotherapy, SZ patients receiving 4 weeks of ECT plus antipsychotics exhibited increased gFCD within the DMN regions, including the left precuneus, ventral medial cortex and dorsal prefrontal cortex [38]. Consistent with Huang et al.’s study, Sambataro and colleagues used another data-driven method, i.e., the ICA, to examine the functional network changes after ECT intervention [40]. They also found increased IC loading in the MPFC in SZ patients following ECT [40]. In addition, Li et al. found DMN FC changes (enhanced FC in the left PCC and reduced FC in the right precuneus) after ECT intervention [39].
3.2.2. Salience Network
The salience network (SN), which includes the insula, anterior cingulate cortex (ACC) and temporoparietal junction (TPJ), plays a crucial role in detecting, filtering and integrating salient signals from external and interoceptive environments [53]. SN dysfunctions in SZ have been widely reported in previous studies [30, 54, 55]. Jiang et al. found that compared to pharmacotherapy alone, SZ patients exhibited decreased FC between the insula and middle occipital gyrus as well as orbitofrontal cortex following ECT plus antipsychotic treatment [44]. Consistent with Jiang et al., Li et al. found decreased connectivity in the ACC after ECT intervention [39]. This phenomenon was not observed in the SZ group treated with antipsychotics alone.
3.2.3. Functional Connectivity with Hippocampus and Amygdala
Using seed-based FC analysis with the right amygdala as the seed region, Thomann et al. found that right unilateral (RUL) ECT induced FC reductions between the right amygdala and cortical regions in the ipsilateral hemisphere, including the right TPJ, the right MPFC, the right DLFPC and bilateral posterior insula [43]. In addition, RUL ECT increased the FC between the right amygdala and the hypothalamus. These researchers observed that these FC changes were not diagnosis-specific in SZ and MDD. Yang and colleagues also reported reduced FC between the right amygdala and left hippocampus after bitemporal ECT compared with pre-ECT [42]. A recent study classified the 21 SZ patients who received ECT intervention into responders (n=10) and nonresponders (n=11), according to the 50% reduction ratio in Positive And Negative Syndrome Scale (PANSS) total scores after the 4-week bitemporal ECT intervention [45]. Comparisons of FC (seed at the hippocampus) longitudinal changes between ECT responders and nonresponders revealed that responders showed increased FC between the hippocampus and prefrontal cortex and regions within the DMN, whereas nonresponders exhibited decreased FC between the hippocampus and regions in the primary sensory network [45].
3.2.4. Others
Li et al. also found increased FC in the temporal lobe network and frontal-parietal network as well as decreased FC in the language network after ECT intervention in SZ patients [39]. In addition, Wang et al. reported that ECT induced increased FC between the right thalamus and right putamen and decreased FC between the thalamus and sensory cortex in SZ patients [41].
3.3. Correlation Between Brain Changes and Symptom Remission
Although several studies [38, 40, 41, 43] reported that no significant correlation was observed between brain changes and clinical symptoms, some studies have found significant correlations between ECT-induced brain changes and symptom remissions after ECT intervention [34, 35, 42, 44, 45]. For example, Wang et al. observed a significant positive correlation between the GM volume change in the right parahippocampal gyrus/hippocampus and the reduction of positive symptoms [35]. Jiang et al. also observed that volume increases in the hippocampal subfield (i.e., left CA4) and FC between the left caudal hippocampus and right angular gyrus were associated with general psychopathology reductions [45]. Yang et al. reported that the change in FC between the amygdala and hippocampus was positively correlated with a reduction in the PANSS total score [42]. In addition to the hippocampus, the volume and FC changes in the posterior insula were correlated with PANSS reductions [44]. Moreover, the left DLPFC network change was negatively associated with PANSS total score changes [34].
3.4. Predictive Performance for the ECT Outcomes using the Baseline MRI
Three of the published studies [36, 37, 42] focused on predicting ECT outcomes using baseline MRI features. Xi et al. [37] classified 57 SZ patients who received ECT combined with antipsychotics into 28 responders and 29 nonresponders. Based on the structural features from the VBM, they found that both the logistic regression model and support vector machine obtained great accuracies of 87.59% and 91.78%, respectively, in the validation dataset. Gong et al. [36] used a multiparametric MRI-based radiomic model to extract the MRI features at baseline and then imported them to a support vector regression model, a machine learning technique, to predict a continuous improvement in symptoms after ECT (i.e., PANSS total score reductions). They found that multimodal MRI features (including four structural MRI features from the left inferior frontal gyrus, right insula, left middle temporal gyrus and right superior temporal gyrus and six diffusion MRI features from tracts connecting the frontal or temporal gyrus) predicted the ECT outcomes, as identified by a significant correlation between predicted and actual values of treatment response. In another work, Yang et al. found that FCs that were distributed within the orbital prefrontal cortex and temporal regions showed a predictive ability for ECT outcomes [42].
4. DISCUSSION
To the best of our knowledge, this is the first review that explores brain structural and functional MRI changes in patients with SZ following ECT intervention. The main results of our study highlight that ECT induces an increase in volumes of the hippocampus and its adjacent regions (parahippocampal gyrus and amygdala) as well as the insula and frontotemporal regions. Regarding fMRI results, consistent improvement in FC within the DMN regions (MPFC and PCC) and a reduction in FC between the SN and other brain regions were noted. Some changes in FC between the hippocampus and amygdala and cortical regions are not consistent in terms of FC increases or decreases. In addition, there seemed to be some changes in FC in other networks, such as the temporal lobe network, frontal-parietal network and language network, as well as the thalamic-cortical/subcortical network. Moreover, ECT-related changes in the hippocampus/amygdala and insula were significantly correlated with ECT outcomes (i.e., PANSS score reductions). Finally, the pre-ECT MRI features seem to be predictive of response to treatment. However, these results should be further identified, given the limited sample size for prediction.
4.1. Structural Plasticity
We found that structural changes after ECT intervention are not widely distributed in the brain but are localized in specific regions that are thought to be highly correlated with the pathophysiologic characteristics of SZ. Volume reductions in the hippocampus, parahippocampal gyrus, amygdala, insula and frontal and temporal lobes in SZ have been demonstrated in prior studies [25, 56]. One possible explanation for volumetric increases is neuroplasticity. Deficits in neuroplasticity have long been documented in SZ and other psychiatric disorders [57]. Moreover, numerous studies have shown that neurogenesis [7, 8], synaptogenesis [9], angiogenesis [10], gliogenesis [11] and other neuronal/axonal changes [12, 13] are induced by electroconvulsive seizures in animal models of ECT. These processes involving neuroplastic changes may contribute to ECT-induced structural changes. In addition to neuroplasticity, edema might be one of the reasons for ECT-induced volume increments. However, several MRI studies suggested that edema does not seem to be a primary cause because no evidence of ECT-related alterations in water content was found using T2 relaxometry [58], FLAIR [59] and DTI [60]. This notion needs to be verified in ECT-treated patients with SZ.
4.2. ECT Modulates Functional Connectivity of Brain Networks
The brain ‘dysconnectivity hypothesis’ posits that SZ is a psychiatric disorder characterized by disrupted interactions between functionally integrated networks, such as the DMN, SN, and frontotemporal network. Abnormal FCs within/between these brain networks are associated with psychiatric symptoms and cognitive impairments in individuals with SZ. The DMN plays a critical role in monitoring internal events during self-referential mental processes [61]. Although increased and decreased FC of the DMN has been frequently reported in patients with SZ [19, 62], a recent review summarized that hyperconnectivity characterizes compensatory recruitment of DMN hub regions in the SZ early stage, whereas hypoconnectivity is associated with deterioration of function in the later stage of the illness [63]. Huang et al. found that the functional integration of the DMN could be restored in medication-resistant and later illness stage patients with SZ after ECT [38]. They proposed that the “normalization” of DMN hypoconnectivity might be a potential mechanism of ECT [38]. Jiang et al. observed increased FC between the hippocampus and the DMN as well as the dorsolateral prefrontal cortex [45]. The hippocampus, which is also considered one of the DMN regions, is critical for memory encoding and retrieval functions [64]. The dorsolateral prefrontal cortex is a core node of the central executive network (CEN) that is responsible for interfacing with the external stimulus [31]. These results suggest that ECT reinforces connectivity within the DMN and between the DMN and CEN to modulate information integration between the internal- and external-based mental landscapes, thus may relieve the symptoms of SZ [45]. In addition to the DMN and CEN, ECT also modulates the integration of interoceptive events and external stimuli by the regulation of FCs between the insula and orbitofrontal and primary cortex [44]. Moreover, the relationship between ECT-induced changes in FCs and symptom reduction has been elucidated [44]. Although some interpretations are speculative, these studies support that ECT modulates the functional interactions between large-scale brain networks, thereby alleviating symptoms [38-40, 44, 45].
4.3. Transdiagnostic Effects of ECT on Brain
To date, several studies have identified the transdiagnostic effects of ECT on brain structure and functional networks in patients with SZ and MDD [34, 40, 43]. First, a network or system comprising the medial temporal lobe, predominantly in the hippocampus, parahippocampus and amygdala, showed a similar pattern of structural change (increased volume) in both SZ and MDD [34, 35, 43, 45]. This finding is highly consistent with previous studies reporting ECT-induced volume increases in the transdiagnostic groups [34, 35, 43, 45]. This finding suggested the transdiagnostic effects of ECT, at least in specific regions. In addition, ECT regulated internetwork connectivity in DMN in both SZ and MDD [38-40, 65]. As the anterior hub of the DMN, the MPFC has been consistently involved in the pathophysiology of both SZ and MDD [66, 67]. Dysconnectivity of the MPFC may abnormally mediate self-referential cognitive and emotional processing, which are altered in both disorders [31]. Huang et al. reported enhanced FC in the MPFC in SZ patients following ECT [38]. Sambataro et al. also found that FC in the MPFC was enhanced in both SZ and MDD after ECT [40]. However, it is unknown how ECT leads to clinical improvement in disorders via these altered FCs.
4.4. Limitations
Several limitations of the included studies should be noted. The first limitation is the small sample size. Because patients who receive ECT are mostly patients with acute symptoms, it is difficult to perform MRI scans at several time points. The largest study included only 29 patients who had two MRI scans (before and after ECT). The small sample size limits the reliability and sensitivity for detecting ECT-related changes and correlations with symptoms. Fortunately, this limitation may be addressed by the Global ECT-MRI Research Collaboration (GEMRIC) [68]. The second limitation involves antipsychotics. Most of the patients had already received antipsychotics before and during ECT. Although some studies included patients only treated with antipsychotic medications as the control group, it is difficult to eradicate the effects of concomitant antipsychotics during the ECT course. Therefore, it is difficult to claim that all of the alterations in these studies were fully attributed to the effects of ECT. The third limitation is the parameter of ECT. Most studies were performed with the bitemporal placement of electrodes. Three studies were performed with unilateral placement. In addition to electrode placement, the total number of ECT sessions was different for each patient. However, the effects of different parameters do not seem to be evaluated in the data analysis. Given the efficacy and tolerance of ECT, it is possible that ECT with different parameters may have different impacts on the brain structures and functions. At last, the limits are for MRI methods. Structural MRI data were analysed by conventional ROI-driven methods and data-driven methods, such as voxel-based morphometry. For fMRI data, FCs were evaluated by several methods, including ICA, voxelwise gFCD, and seed-based FC. In the predictive analysis, logistic regression, support vector machine and support vector regression were used for predictive models. Although multiple methods comprehensively explore brain information, the consistency of the results still needs further verification. In addition to the data analysis, multimodal MRI can reveal complementary characteristics about brain structures or functions. Only three studies measured structural and functional brain changes simultaneously based on multimodal MRI data. Due to the limited studies discussed above, we summarized MRI works examining structural and functional changes separately. In future works, multimodal MRI investigations are necessary to provide complementary information about brain structure, function, and coupling, which aids in improving the knowledge of the complex brain mechanism of ECT.
There are also several limitations of this review. First, it is difficult to conduct a systematic meta-analysis because several studies used different imaging modalities and analytical approaches. Second, specific studies, such as conference reports, abstracts and articles published in non-English, were not included in our review. In addition, unpublished or unreported negative results potentially influenced our conclusions. Two studies only included pre-ECT MRI scans. These studies were also included because they contributed to the predictive performance of ECT outcomes. Third, this review was not able to determine whether the placement of electrodes of ECT has a specific effect on brain changes due to the limited sample size of previous studies. Finally, several studies had identical or overlapping samples of patients. All these studies were mentioned in this review because they dealt with different scientific questions using different analysis methods or different modal MRIs.
CONCLUSION
Our review summarized sMRI and fMRI changes in SZ patients following ECT. These sMRI studies consistently found ECT-induced volume increases in the hippocampus and adjacent areas as well as the insula. fMRI studies found ECT-induced changes in different brain regions/networks that are thought to be highly correlated with the pathophysiologic characteristics of SZ. The results of the correlation between brain changes and symptom remissions are inconsistent. In the future, improving the understanding of the mechanism related to medication-resistant in SZ would contribute to the neurobiological substrates of the ECT.
CONSENT FOR PUBLICATION
Not applicable.
STANDARDS OF REPORTING
PRISMA guidelines & methodology was followed.
FUNDING
This work was partly supported by the grant from the National Key R&D Program of China (No. 2018YFA0701400), grants from the National Natural Science Foundation of China (No. grant number: U2033217, 61933003, 62003076, 62003058 and 81471638), the CAMS Innovation Fund for Medical Sciences (CIFMS) (No. 2019-I2M-5-039) and the project from China Postdoctoral Science Foundation (BX2021078). The funder has no other role in this study.
ACKNOWLEDGEMENTS
Declared none.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
SUPPLEMENTARY MATERIAL
PRISMA checklist is available on the publisher’s website along with the published article.
REFERENCES
- 1.van der Meer L., Costafreda S., Aleman A., David A.S. Self-reflection and the brain: a theoretical review and meta-analysis of neuroimaging studies with implications for schizophrenia. Neurosci. Biobehav. Rev. 2010;34(6):935–946. doi: 10.1016/j.neubiorev.2009.12.004. [DOI] [PubMed] [Google Scholar]
- 2.Pompili M., Lester D., Dominici G., Longo L., Marconi G., Forte A., Serafini G., Amore M., Girardi P. Indications for electroconvulsive treatment in schizophrenia: a systematic review. Schizophr. Res. 2013;146(1-3):1–9. doi: 10.1016/j.schres.2013.02.005. [DOI] [PubMed] [Google Scholar]
- 3.Lally J., Tully J., Robertson D., Stubbs B., Gaughran F., MacCabe J.H. Augmentation of clozapine with electroconvulsive therapy in treatment resistant schizophrenia: A systematic review and meta-analysis. Schizophr. Res. 2016;171(1-3):215–224. doi: 10.1016/j.schres.2016.01.024. [DOI] [PubMed] [Google Scholar]
- 4.Tharyan P., Adams C.E. Electroconvulsive therapy for schizophrenia. Cochrane Database Syst. Rev. 2005;2:CD000076. doi: 10.1002/14651858.CD000076.pub2. [DOI] [PubMed] [Google Scholar]
- 5.Petrides G., Malur C., Braga R.J., Bailine S.H., Schooler N.R., Malhotra A.K., Kane J.M., Sanghani S., Goldberg T.E., John M., Mendelowitz A. Electroconvulsive therapy augmentation in clozapine-resistant schizophrenia: a prospective, randomized study. Am. J. Psychiatry. 2015;172(1):52–58. doi: 10.1176/appi.ajp.2014.13060787. [DOI] [PubMed] [Google Scholar]
- 6.Ali S.A., Mathur N., Malhotra A.K., Braga R.J. Electroconvulsive Therapy and Schizophrenia: A Systematic Review. Mol. Neuropsychiatry. 2019;5(2):75–83. doi: 10.1159/000497376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Madsen T.M., Treschow A., Bengzon J., Bolwig T.G., Lindvall O., Tingström A. Increased neurogenesis in a model of electroconvulsive therapy. Biol. Psychiatry. 2000;47(12):1043–1049. doi: 10.1016/S0006-3223(00)00228-6. [DOI] [PubMed] [Google Scholar]
- 8.Perera T.D., Coplan J.D., Lisanby S.H., Lipira C.M., Arif M., Carpio C., Spitzer G., Santarelli L., Scharf B., Hen R., Rosoklija G., Sackeim H.A., Dwork A.J. Antidepressant-induced neurogenesis in the hippocampus of adult nonhuman primates. J. Neurosci. 2007;27(18):4894–4901. doi: 10.1523/JNEUROSCI.0237-07.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chen F., Madsen T.M., Wegener G., Nyengaard J.R. Repeated electroconvulsive seizures increase the total number of synapses in adult male rat hippocampus. Eur. Neuropsychopharmacol. 2009;19(5):329–338. doi: 10.1016/j.euroneuro.2008.12.007. [DOI] [PubMed] [Google Scholar]
- 10.Hellsten J., West M.J., Arvidsson A., Ekstrand J., Jansson L., Wennström M., Tingström A. Electroconvulsive seizures induce angiogenesis in adult rat hippocampus. Biol. Psychiatry. 2005;58(11):871–878. doi: 10.1016/j.biopsych.2005.05.023. [DOI] [PubMed] [Google Scholar]
- 11.Wennström M., Hellsten J., Ekdahl C.T., Tingström A. Electroconvulsive seizures induce proliferation of NG2-expressing glial cells in adult rat hippocampus. Biol. Psychiatry. 2003;54(10):1015–1024. doi: 10.1016/S0006-3223(03)00693-0. [DOI] [PubMed] [Google Scholar]
- 12.Vaidya V.A., Siuciak J.A., Du F., Duman R.S. Hippocampal mossy fiber sprouting induced by chronic electroconvulsive seizures. Neuroscience. 1999;89(1):157–166. doi: 10.1016/S0306-4522(98)00289-9. [DOI] [PubMed] [Google Scholar]
- 13.Zhao C., Warner-Schmidt J., Duman R.S., Gage F.H. Electroconvulsive seizure promotes spine maturation in newborn dentate granule cells in adult rat. Dev. Neurobiol. 2012;72(6):937–942. doi: 10.1002/dneu.20986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wilkinson S.T., Sanacora G., Bloch M.H. Hippocampal volume changes following electroconvulsive therapy: a systematic review and meta-analysis. Biol. Psychiatry Cogn. Neurosci. Neuroimaging. 2017;2(4):327–335. doi: 10.1016/j.bpsc.2017.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rocha R.B., Dondossola E.R., Grande A.J., Colonetti T., Ceretta L.B., Passos I.C., Quevedo J., da Rosa M.I. Increased BDNF levels after electroconvulsive therapy in patients with major depressive disorder: A meta-analysis study. J. Psychiatr. Res. 2016;83:47–53. doi: 10.1016/j.jpsychires.2016.08.004. [DOI] [PubMed] [Google Scholar]
- 16.Grover S., Hazari N., Kate N. Combined use of clozapine and ECT: a review. Acta Neuropsychiatr. 2015;27(3):131–142. doi: 10.1017/neu.2015.8. [DOI] [PubMed] [Google Scholar]
- 17.Takamiya A., Chung J.K., Liang K.C., Graff-Guerrero A., Mimura M., Kishimoto T. Effect of electroconvulsive therapy on hippocampal and amygdala volumes: systematic review and meta-analysis. Br. J. Psychiatry. 2018;212(1):19–26. doi: 10.1192/bjp.2017.11. [DOI] [PubMed] [Google Scholar]
- 18.Gbyl K., Videbech P. Electroconvulsive therapy increases brain volume in major depression: a systematic review and meta-analysis. Acta Psychiatr. Scand. 2018;138(3):180–195. doi: 10.1111/acps.12884. [DOI] [PubMed] [Google Scholar]
- 19.Fornito A., Zalesky A., Pantelis C., Bullmore E.T. Schizophrenia, neuroimaging and connectomics. Neuroimage. 2012;62(4):2296–2314. doi: 10.1016/j.neuroimage.2011.12.090. [DOI] [PubMed] [Google Scholar]
- 20.Dong D., Wang Y., Chang X., Jiang Y., Klugah-Brown B., Luo C., Yao D. Shared abnormality of white matter integrity in schizophrenia and bipolar disorder: A comparative voxel-based meta-analysis. Schizophr. Res. 2017;185:41–50. doi: 10.1016/j.schres.2017.01.005. [DOI] [PubMed] [Google Scholar]
- 21.Dong D., Luo C., Guell X., Wang Y., He H., Duan M., Eickhoff S.B., Yao D. Compression of Cerebellar Functional Gradients in Schizophrenia. Schizophr. Bull. 2020. p. sbaa016. [DOI] [PMC free article] [PubMed]
- 22.Fitzsimmons J., Kubicki M., Shenton M.E. Review of functional and anatomical brain connectivity findings in schizophrenia. Curr. Opin. Psychiatry. 2013;26(2):172–187. doi: 10.1097/YCO.0b013e32835d9e6a. [DOI] [PubMed] [Google Scholar]
- 23.Molent C., Olivo D., Wolf R.C., Balestrieri M., Sambataro F. Functional neuroimaging in treatment resistant schizophrenia: A systematic review. Neurosci. Biobehav. Rev. 2019;104:178–190. doi: 10.1016/j.neubiorev.2019.07.001. [DOI] [PubMed] [Google Scholar]
- 24.Jiang Y., Luo C., Li X., Li Y., Yang H., Li J., Chang X., Li H., Yang H., Wang J., Duan M., Yao D. White-matter functional networks changes in patients with schizophrenia. Neuroimage. 2019;190:172–181. doi: 10.1016/j.neuroimage.2018.04.018. [DOI] [PubMed] [Google Scholar]
- 25.Jiang Y., Luo C., Li X., Duan M., He H., Chen X., Yang H., Gong J., Chang X., Woelfer M., Biswal B.B., Yao D. Progressive reduction in gray matter in patients with schizophrenia assessed with MR imaging by using causal network analysis. Radiology. 2018;287(2):633–642. doi: 10.1148/radiol.2017171832. [DOI] [PubMed] [Google Scholar]
- 26.Haijma S.V., Van Haren N., Cahn W., Koolschijn P.C., Hulshoff Pol H.E., Kahn R.S. Brain volumes in schizophrenia: a meta-analysis in over 18 000 subjects. Schizophr. Bull. 2013;39(5):1129–1138. doi: 10.1093/schbul/sbs118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dong D., Wang Y., Chang X., Luo C., Yao D. Dysfunction of large-scale brain networks in schizophrenia: A meta-analysis of resting-state functional connectivity. Schizophr. Bull. 2018;44(1):168–181. doi: 10.1093/schbul/sbx034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.He H., Luo C., Luo Y., Duan M., Yi Q., Biswal B.B., Yao D. Reduction in gray matter of cerebellum in schizophrenia and its influence on static and dynamic connectivity. Hum. Brain Mapp. 2019;40(2):517–528. doi: 10.1002/hbm.24391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Woodward N.D., Karbasforoushan H., Heckers S. Thalamocortical dysconnectivity in schizophrenia. Am. J. Psychiatry. 2012;169(10):1092–1099. doi: 10.1176/appi.ajp.2012.12010056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Huang H., Botao Z., Jiang Y., Tang Y., Zhang T., Tang X., Xu L., Wang J., Li J., Qian Z., Liu X., Wang H., Luo C., Li C., Xu J., Goff D., Wang J. Aberrant resting-state functional connectivity of salience network in first-episode schizophrenia. Brain Imaging Behav. 2020;14(5):1350–1360. doi: 10.1007/s11682-019-00040-8. [DOI] [PubMed] [Google Scholar]
- 31.Menon V. Large-scale brain networks and psychopathology: a unifying triple network model. Trends Cogn. Sci. 2011;15(10):483–506. doi: 10.1016/j.tics.2011.08.003. [DOI] [PubMed] [Google Scholar]
- 32.Pettersson-Yeo W., Allen P., Benetti S., McGuire P., Mechelli A. Dysconnectivity in schizophrenia: where are we now? Neurosci. Biobehav. Rev. 2011;35(5):1110–1124. doi: 10.1016/j.neubiorev.2010.11.004. [DOI] [PubMed] [Google Scholar]
- 33.Page M.J., McKenzie J.E., Bossuyt P.M., Boutron I., Hoffmann T.C., Mulrow C.D., Shamseer L., Tetzlaff J.M., Akl E.A., Brennan S.E., Chou R., Glanville J., Grimshaw J.M., Hróbjartsson A., Lalu M.M., Li T., Loder E.W., Mayo-Wilson E., McDonald S., McGuinness L.A., Stewart L.A., Thomas J., Tricco A.C., Welch V.A., Whiting P., Moher D. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372(71):n71. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wolf R.C., Nolte H.M., Hirjak D., Hofer S., Seidl U., Depping M.S., Stieltjes B., Maier-Hein K., Sambataro F., Thomann P.A. Structural network changes in patients with major depression and schizophrenia treated with electroconvulsive therapy. Eur. Neuropsychopharmacol. 2016;26(9):1465–1474. doi: 10.1016/j.euroneuro.2016.06.008. [DOI] [PubMed] [Google Scholar]
- 35.Wang J., Tang Y., Curtin A., Xia M., Tang X., Zhao Y., Li Y., Qian Z., Sheng J., Zhang T., Jia Y., Li C., Wang J. ECT-induced brain plasticity correlates with positive symptom improvement in schizophrenia by voxel-based morphometry analysis of grey matter. Brain Stimul. 2019;12(2):319–328. doi: 10.1016/j.brs.2018.11.006. [DOI] [PubMed] [Google Scholar]
- 36.Gong J., Cui L.B., Xi Y.B., Zhao Y.S., Yang X.J., Xu Z.L., Sun J.B., Liu P., Jia J., Li P., Yin H., Qin W. Predicting response to electroconvulsive therapy combined with antipsychotics in schizophrenia using multi-parametric magnetic resonance imaging. Schizophr. Res. 2020;216:262–271. doi: 10.1016/j.schres.2019.11.046. [DOI] [PubMed] [Google Scholar]
- 37.Xi Y.B., Cui L.B., Gong J., Fu Y.F., Wu X.S., Guo F., Yang X., Li C., Wang X.R., Li P., Qin W., Yin H. Neuroanatomical features that predict response to electroconvulsive therapy combined with antipsychotics in schizophrenia: a magnetic resonance imaging study using radiomics strategy. Front. Psychiatry. 2020;11:456. doi: 10.3389/fpsyt.2020.00456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Huang H., Jiang Y., Xia M., Tang Y., Zhang T., Cui H., Wang J., Li Y., Xu L., Curtin A., Sheng J., Jia Y., Yao D., Li C., Luo C., Wang J. Increased resting-state global functional connectivity density of default mode network in schizophrenia subjects treated with electroconvulsive therapy. Schizophr. Res. 2018;197:192–199. doi: 10.1016/j.schres.2017.10.044. [DOI] [PubMed] [Google Scholar]
- 39.Li P., Jing R.X., Zhao R.J., Ding Z.B., Shi L., Sun H.Q., Lin X., Fan T.T., Dong W.T., Fan Y., Lu L. Electroconvulsive therapy-induced brain functional connectivity predicts therapeutic efficacy in patients with schizophrenia: a multivariate pattern recognition study. NPJ Schizophr. 2017;3:21. doi: 10.1038/s41537-017-0023-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sambataro F., Thomann P.A., Nolte H.M., Hasenkamp J.H., Hirjak D., Kubera K.M., Hofer S., Seidl U., Depping M.S., Stieltjes B., Maier-Hein K., Wolf R.C. Transdiagnostic modulation of brain networks by electroconvulsive therapy in schizophrenia and major depression. Eur. Neuropsychopharmacol. 2019;29(8):925–935. doi: 10.1016/j.euroneuro.2019.06.002. [DOI] [PubMed] [Google Scholar]
- 41.Wang J., Jiang Y., Tang Y., Xia M., Curtin A., Li J., Sheng J., Zhang T., Li C., Hui L., Zhu H., Biswal B.B., Jia Q., Luo C., Wang J. Altered functional connectivity of the thalamus induced by modified electroconvulsive therapy for schizophrenia. Schizophr. Res. 2020;218:209–218. doi: 10.1016/j.schres.2019.12.044. [DOI] [PubMed] [Google Scholar]
- 42.Yang X., Xu Z., Xi Y., Sun J., Liu P., Liu P., Li P., Jia J., Yin H., Qin W. Predicting responses to electroconvulsive therapy in schizophrenia patients undergoing antipsychotic treatment: Baseline functional connectivity among regions with strong electric field distributions. Psychiatry Res. Neuroimaging. 2020;299:111059. doi: 10.1016/j.pscychresns.2020.111059. [DOI] [PubMed] [Google Scholar]
- 43.Thomann P.A., Wolf R.C., Nolte H.M., Hirjak D., Hofer S., Seidl U., Depping M.S., Stieltjes B., Maier-Hein K., Sambataro F., Wüstenberg T. Neuromodulation in response to electroconvulsive therapy in schizophrenia and major depression. Brain Stimul. 2017;10(3):637–644. doi: 10.1016/j.brs.2017.01.578. [DOI] [PubMed] [Google Scholar]
- 44.Jiang Y., Xia M., Li X., Tang Y., Li C., Huang H., Dong D., Jiang S., Wang J., Xu J., Luo C., Yao D. Insular changes induced by electroconvulsive therapy response to symptom improvements in schizophrenia. Prog. Neuropsychopharmacol. Biol. Psychiatry. 2019;89:254–262. doi: 10.1016/j.pnpbp.2018.09.009. [DOI] [PubMed] [Google Scholar]
- 45.Jiang Y., Xu L., Li X., Tang Y., Wang P., Li C., Yao D., Wang J., Luo C. Common increased hippocampal volume but specific changes in functional connectivity in schizophrenia patients in remission and non-remission following electroconvulsive therapy: A preliminary study. Neuroimage Clin. 2019;24:102081. doi: 10.1016/j.nicl.2019.102081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Yrondi A., Péran P., Sauvaget A., Schmitt L., Arbus C. Structural-functional brain changes in depressed patients during and after electroconvulsive therapy. Acta Neuropsychiatr. 2018;30(1):17–28. doi: 10.1017/neu.2016.62. [DOI] [PubMed] [Google Scholar]
- 47.Garrity A.G., Pearlson G.D., McKiernan K., Lloyd D., Kiehl K.A., Calhoun V.D. Aberrant “default mode” functional connectivity in schizophrenia. Am. J. Psychiatry. 2007;164(3):450–457. doi: 10.1176/ajp.2007.164.3.450. [DOI] [PubMed] [Google Scholar]
- 48.Wang Y.M., Zou L.Q., Xie W.L., Yang Z.Y., Zhu X.Z., Cheung E.F.C., Sørensen T.A., Møller A., Chan R.C.K. Altered functional connectivity of the default mode network in patients with schizo-obsessive comorbidity: a comparison between schizophrenia and obsessive-compulsive disorder. Schizophr. Bull. 2019;45(1):199–210. doi: 10.1093/schbul/sbx194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hare S.M., Ford J.M., Mathalon D.H., Damaraju E., Bustillo J., Belger A., Lee H.J., Mueller B.A., Lim K.O., Brown G.G., Preda A., van Erp T.G.M., Potkin S.G., Calhoun V.D., Turner J.A. Salience-default mode functional network connectivity linked to positive and negative symptoms of schizophrenia. Schizophr. Bull. 2019;45(4):892–901. doi: 10.1093/schbul/sby112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hu M.L., Zong X.F., Mann J.J., Zheng J.J., Liao Y.H., Li Z.C., He Y., Chen X.G., Tang J.S. A review of the functional and anatomical default mode network in schizophrenia. Neurosci. Bull. 2017;33(1):73–84. doi: 10.1007/s12264-016-0090-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Tomasi D., Volkow N.D. Functional connectivity density mapping. Proc. Natl. Acad. Sci. USA. 2010;107(21):9885–9890. doi: 10.1073/pnas.1001414107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Tomasi D., Volkow N.D. Functional connectivity hubs in the human brain. Neuroimage. 2011;57(3):908–917. doi: 10.1016/j.neuroimage.2011.05.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Seeley W.W., Menon V., Schatzberg A.F., Keller J., Glover G.H., Kenna H., Reiss A.L., Greicius M.D. Dissociable intrinsic connectivity networks for salience processing and executive control. J. Neurosci. 2007;27(9):2349–2356. doi: 10.1523/JNEUROSCI.5587-06.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.He H., Yang M., Duan M., Chen X., Lai Y., Xia Y., Shao J., Biswal B.B., Luo C., Yao D. Music intervention leads to increased insular connectivity and improved clinical symptoms in schizophrenia. Front. Neurosci. 2018;11:744. doi: 10.3389/fnins.2017.00744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Chen X., Duan M., He H., Yang M., Klugah-Brown B., Xu H., Lai Y., Luo C., Yao D. Functional abnormalities of the right posterior insula are related to the altered self-experience in schizophrenia. Psychiatry Res. Neuroimaging. 2016;256:26–32. doi: 10.1016/j.pscychresns.2016.09.006. [DOI] [PubMed] [Google Scholar]
- 56.Smieskova R., Fusar-Poli P., Allen P., Bendfeldt K., Stieglitz R.D., Drewe J., Radue E.W., McGuire P.K., Riecher-Rössler A., Borgwardt S.J. The effects of antipsychotics on the brain: what have we learnt from structural imaging of schizophrenia?--a systematic review. Curr. Pharm. Des. 2009;15(22):2535–2549. doi: 10.2174/138161209788957456. [DOI] [PubMed] [Google Scholar]
- 57.Krystal J.H., Tolin D.F., Sanacora G., Castner S.A., Williams G.V., Aikins D.E., Hoffman R.E., D’Souza D.C. Neuroplasticity as a target for the pharmacotherapy of anxiety disorders, mood disorders, and schizophrenia. Drug Discov. Today. 2009;14(13-14):690–697. doi: 10.1016/j.drudis.2009.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Kunigiri G., Jayakumar P.N., Janakiramaiah N., Gangadhar B.N. MRI T(2) relaxometry of brain regions and cognitive dysfunction following electroconvulsive therapy. Indian J. Psychiatry. 2007;49(3):195–199. doi: 10.4103/0019-5545.37321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Nordanskog P., Dahlstrand U., Larsson M.R., Larsson E.M., Knutsson L., Johanson A. Increase in hippocampal volume after electroconvulsive therapy in patients with depression: a volumetric magnetic resonance imaging study. J. ECT. 2010;26(1):62–67. doi: 10.1097/YCT.0b013e3181a95da8. [DOI] [PubMed] [Google Scholar]
- 60.Jorgensen A., Magnusson P., Hanson L.G., Kirkegaard T., Benveniste H., Lee H., Svarer C., Mikkelsen J.D., Fink-Jensen A., Knudsen G.M., Paulson O.B., Bolwig T.G., Jorgensen M.B. Regional brain volumes, diffusivity, and metabolite changes after electroconvulsive therapy for severe depression. Acta Psychiatr. Scand. 2016;133(2):154–164. doi: 10.1111/acps.12462. [DOI] [PubMed] [Google Scholar]
- 61.Raichle M.E., Snyder A.Z. A default mode of brain function: a brief history of an evolving idea. Neuroimage. 2007;37(4):1083–1090. doi: 10.1016/j.neuroimage.2007.02.041. [DOI] [PubMed] [Google Scholar]
- 62.Narr K.L., Leaver A.M. Connectome and schizophrenia. Curr. Opin. Psychiatry. 2015;28(3):229–235. doi: 10.1097/YCO.0000000000000157. [DOI] [PubMed] [Google Scholar]
- 63.Fornito A., Bullmore E.T., Zalesky A. Opportunities and Challenges for Psychiatry in the Connectomic Era. Biol. Psychiatry Cogn. Neurosci. Neuroimaging. 2017;2(1):9–19. doi: 10.1016/j.bpsc.2016.08.003. [DOI] [PubMed] [Google Scholar]
- 64.Tamminga C.A., Stan A.D., Wagner A.D. The hippocampal formation in schizophrenia. Am. J. Psychiatry. 2010;167(10):1178–1193. doi: 10.1176/appi.ajp.2010.09081187. [DOI] [PubMed] [Google Scholar]
- 65.Leaver A.M., Espinoza R., Pirnia T., Joshi S.H., Woods R.P., Narr K.L. Modulation of intrinsic brain activity by electroconvulsive therapy in major depression. Biol. Psychiatry Cogn. Neurosci. Neuroimaging. 2016;1(1):77–86. doi: 10.1016/j.bpsc.2015.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Chen X., Liu C., He H., Chang X., Jiang Y., Li Y., Duan M., Li J., Luo C., Yao D. Transdiagnostic differences in the resting-state functional connectivity of the prefrontal cortex in depression and schizophrenia. J. Affect. Disord. 2017;217:118–124. doi: 10.1016/j.jad.2017.04.001. [DOI] [PubMed] [Google Scholar]
- 67.Jiang Y., Duan M., Chen X., Chang X., He H., Li Y., Luo C., Yao D. Common and distinct dysfunctional patterns contribute to triple network model in schizophrenia and depression: A preliminary study. Prog Neuropsychopharmacol Biol Psychiatry. 2017;79(Pt B):302-310. doi: 10.1016/j.pnpbp.2017.07.007. [DOI] [PubMed] [Google Scholar]
- 68.Oltedal L., Bartsch H., Sørhaug O.J., Kessler U., Abbott C., Dols A., Stek M.L., Ersland L., Emsell L., van Eijndhoven P., Argyelan M., Tendolkar I., Nordanskog P., Hamilton P., Jorgensen M.B., Sommer I.E., Heringa S.M., Draganski B., Redlich R., Dannlowski U., Kugel H., Bouckaert F., Sienaert P., Anand A., Espinoza R., Narr K.L., Holland D., Dale A.M., Oedegaard K.J. The Global ECT-MRI Research Collaboration (GEMRIC): Establishing a multi-site investigation of the neural mechanisms underlying response to electroconvulsive therapy. Neuroimage Clin. 2017;14:422–432. doi: 10.1016/j.nicl.2017.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
PRISMA checklist is available on the publisher’s website along with the published article.


