Abstract
Medical specialty usage of COVID-19 survivors after hospital discharge is poorly understood. This study investigated medical specialty usage at 1–12 and 13–24 months post-hospital discharge in critically ill and non-critically ill COVID-19 survivors. This retrospective study followed ICU (N = 89) and non-ICU (N = 205) COVID-19 survivors who returned for follow-up within the Stony Brook Health System post-hospital discharge. Follow-up data including survival, hospital readmission, ongoing symptoms, medical specialty care use, and ICU status were examined 1–12 and 13–24 months after COVID-19 discharge. “New” (not previously seen) medical specialty usage was also identified. Essentially all (98%) patients survived. Hospital readmission was 34%, but functional status scores at discharge were not associated with hospital readmission. Many patients reported ongoing [neuromuscular (50%) respiratory (39%), chronic fatigue (35%), cardiovascular (30%), gastrointestinal (28%), neurocognitive (22%), genitourinary (22%), and mood-related (13%)] symptoms at least once 1–24 months after discharge. Common specialty follow-ups included cardiology (25%), vascular medicine (17%), urology (17%), neurology (16%), and pulmonology (14%), with some associated with pre-existing comorbidities and with COVID-19. Common new specialty visits were vascular medicine (11%), pulmonology (11%), and neurology (9%). ICU patients had more symptoms and follow-ups compared to the non-ICU patients. This study reported high incidence of persistent symptoms and medical specialty care needs in hospitalized COVID-19 survivors 1–24 months post-discharge. Some specialty care needs were COVID-19 related or exacerbated by COVID-19 disease while others were associated with pre-existing medical conditions. Longer follow-up studies of COVID-19 survivor medical care needs are necessary.
Supplementary Information
The online version contains supplementary material available at 10.1007/s11739-023-03195-x.
Keywords: Post-acute COVID-19 symptoms, Post-acute sequelae of COVID-19, Long COVID, COVID-19 sequela, Coronavirus disease 2019, SARS-CoV-2
Introduction
Many COVID-19 survivors exhibit persistent symptoms months after SARS-CoV-2 infection [1–6]. Respiratory difficulty, fatigue, headache, dyspnea, sweating, chest tightness, depression, and anxiety are commonly reported symptoms [7–10]. Some COVID-19 survivors also experienced neurocognitive and neuropsychiatric symptoms [11–16]. Studies to date include surveys of post-COVID-19 sequela, self-reporting of symptoms, cognitive testing, and clinical evaluations, among others. Whether these post-COVID-19 sequelae have led to seeking of medical care is unknown. As COVID-19 treatment continues to improve, more patients are surviving, and long COVID-19 sequelae are becoming more evident. It is thus important to study care utilization for long COVID-19 sequela.
In this study, we investigated medical referrals and health care usage of a group of ICU and non-ICU COVID-19 survivors [17, 18] to provide further insights into potential long-term COVID-19 medical issues and sequelae. Our approach attempts to demonstrate actual patient behavior and symptomology as documented during healthcare visits. Health-care provider referrals were those given at hospital discharge. Medical specialty care usage was tabulated at 1–12, and 13–24 months after COVID-19 hospital discharge. Comparisons were made with medical specialty care usage prior to COVID-19 to identify “new” COVID-19 related medical care usage.
Methods
This study was approved by the Stony Brook University Institutional Review Board with an exemption for informed consent. It followed the Strengthening of Reporting of Observational Studies in Epidemiology (STROBE) reporting guidelines for observational studies.
This is a retrospective follow-up study of two previously reported cohorts [17, 18] of ICU (N = 118) and non-ICU (N = 317) COVID-19 patients using chart reviews of the Electronic Medical Records (EMR), which also include uploaded paper charts and clinical notes. Patients were not specifically invited for post-discharge evaluation. SARS-CoV-2 infection, defined by a real-time polymerase chain reaction test, occurred between March 27, 2020 and August 11, 2020. The last day of follow-up was on June 30th, 2022. Follow-up time frame was 1–12 and 13–24 months after discharge. Data from 0–1 month was excluded to assess long-haul COVID-19, consistent with the definition by the Center for Disease Control and Prevent [19]. Chart review was performed by RJ, SP, and RK and was subsequently validated by BM and MB. Data were then analyzed by BM and MB. A consensus was reached among all members after data extraction and analysis.
Clinical data extracted by manual chart reviews included: (1) demographics: age, gender, ethnicity, and race; (2) comorbidities: obesity, hypertension, diabetes, smoking history, coronary artery disease (CAD), chronic obstructive pulmonary disorder (COPD), heart failure (HF) and chronic kidney disease (CKD); (3) longitudinal characteristics: survival, hospital readmission, ongoing symptoms (fatigue or neuromuscular, respiratory, cardiovascular, gastrointestinal, neurocognitive, genitourinary, and mood-related symptoms), and outpatient specialty visits (cardiology, vascular medicine, urology, neurology, pulmonology, gastroenterology, nephrology, orthopedics, and endocrinology pre- and post-COVID-19); (4) functional status scores: ICU Mobility Scale and Barthel Index as available from previous publications [20–28].
Survival was defined as evidence that a patient is alive over the 24-month period. Patients who returned beyond 24 months or confirmed alive via alternative documentation (phone call, non-medical visit records, etc.) were considered alive. Mortality was defined by confirmed EMR documentation. Patients discharged on comfort care measures or to hospice care were considered survivors unless otherwise documented. Symptoms were obtained only by chart review of outpatient EMR, excluding emergency room and inpatient symptoms. Criteria and definitions for these symptoms are listed in Supplemental Table 1.
Specialty referrals were made by discharging physicians and tabulated from patient discharge paperwork. Outpatient specialty follow-up was defined as any office visit or telehealth encounter with a medical specialist. Scanned records from outside medical systems were also included. Additionally, some specialty visits were discerned from primary care or other specialty notes that mentioned outside specialist follow-up. Some specialties (namely vascular medicine) were routinely seen within 1 month of hospital discharge. These were tabulated as an exception to the 1-month cutoff criteria. Symptoms reported during those visits (0–1 month) were not included in analysis.
The ICU Mobility Scale (range: 0–10) is an 11-item categorical scale that measures the highest level of functional mobility of patients. The Barthel Index (modified range: 0–75) is an ordinal scale used to measure performance in activities of daily living (ADL), consisting of ten variables describing ADL and functional mobility. Higher scores indicate higher functioning for both scores.
Statistical analysis
Statistical analysis was performed using SPSS v26 (IBM, Armonk, NY) and SAS v9.4 (SAS Institute, Cary, NC). Demographics, comorbidities/risk factors, and symptoms at admission were compared between patients who returned and those who did not return using Chi-square tests and t-tests were used to compare age and functional status scores. Rates of hospital readmissions, ongoing symptoms, outpatient follow-up, and new specialty visits were compared among two time points (i.e., 1–12 months and 13–24 months) using generalized estimating equations (GEE) models. For the ICU vs non-ICU group, these same variables were compared using Chi-square tests. A p < 0.05 was considered statistically significant. Analysis was not adjusted for covariates due to the exploratory nature of this study and limited sample sizes.
Results
The return rate to our health system 1–24 months after COVID-19 hospitalization discharge was 68% (294/435). Ten additional patients either returned beyond 24 months or were confirmed alive by alternative methods without returning. Characteristics of patients who returned to our health system and those who did not were similar with a few exceptions (Supplemental Table 2). Patients who returned had higher proportions of non-Hispanics and Caucasians and had higher rates of hypertension, diabetes, CAD, COPD, HF, CKD, and smoking (all p < 0.05).
The return rates were 98% (N = 288) at 1–12 months and 62% (N = 182) at 13–24 months, with 60% (N = 176) returning more than once. Thirty percent (30%) of those who returned 1–24 months were ICU patients. ICU patients were significantly more likely to return than non-ICU patients (p < 0.05).
Mortality and hospital readmission
Over 98% (298/304) of patients survived. About one-third (N = 100/294) of patients were readmitted to the hospital, 52% of which were readmitted more than once. Six survivors received comfort care/hospice care after discharge.
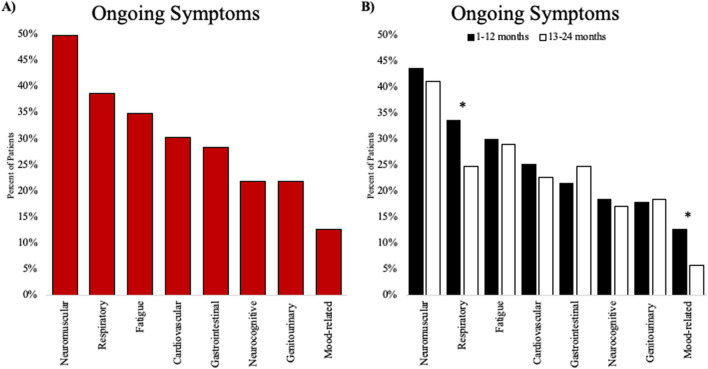
Ongoing symptoms
Neuromuscular (50%), respiratory (39%), fatigue (35%), cardiovascular (30%), gastrointestinal (28%), neurocognitive (22%), genitourinary (22%), and mood-related (13%) symptoms were common 1–24 months after discharge (Fig. 1A). Respiratory and mood-related symptoms were the only ones to decrease at 13–24 months (p = 0.04 and p = 0.01 respectively); all other symptoms persisted (Fig. 1B).
Fig. 1.
A Most common ongoing symptoms 1–24 months post-COVID-19 B Percentage of patients with ongoing symptoms at 1–12 and 13–24 months post-COVID-19. Some patients returned more than once and thus percentages may not sum up those in 1A. *Indicates respiratory and mood-related symptoms significantly decreased at 13–24 months (p = 0.04 and p = 0.01 respectively)
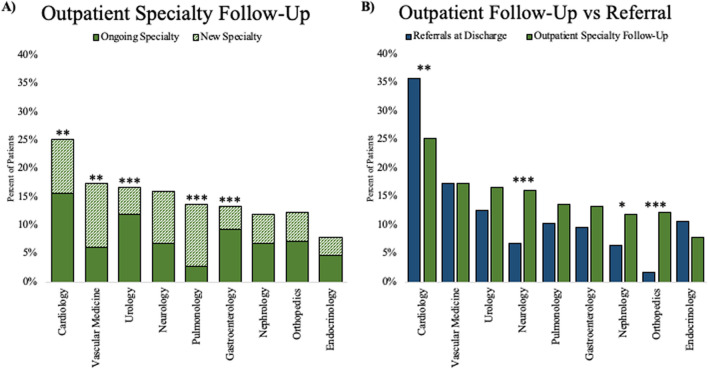
Specialty medical care needs
Common follow-up outpatient specialty visits included cardiology (25%), vascular medicine (17%), urology (17%), neurology (16%), pulmonology (14%), gastroenterology (13%), nephrology (12%), and orthopedics (12%) (Fig. 2A). Many outpatient specialty visits were associated with medical conditions prior to COVID-19 (ongoing specialty). Common new specialty visits were cardiology (10%), vascular medicine (11%), pulmonology (11%), and neurology (9%). Cardiology, urology, and gastroenterology visits were predominantly with ongoing specialists while most vascular medicine and pulmonology visits were new specialty visits (p < 0.01 for all). Neurology, nephrology, orthopedics, and endocrinology visits had similar proportions of new and ongoing specialty visits.
Fig. 2.
A Common ongoing and new outpatient specialty visits. B Outpatient follow-up visits compared to referrals at hospital discharge. * p < 0.05, ** p < 0.01, *** p < 0.001 between ongoing and new specialty visits, or between referral at discharge and specialty follow-up
Fewer patients went to see cardiology specialty compared to referrals at hospital discharge (p < 0.01), whereas more patients went to see neurology (p < 0.001), nephrology (p < 0.05), and orthopedics (p < 0.001) specialties compared to referrals at hospital discharge (Fig. 2B).
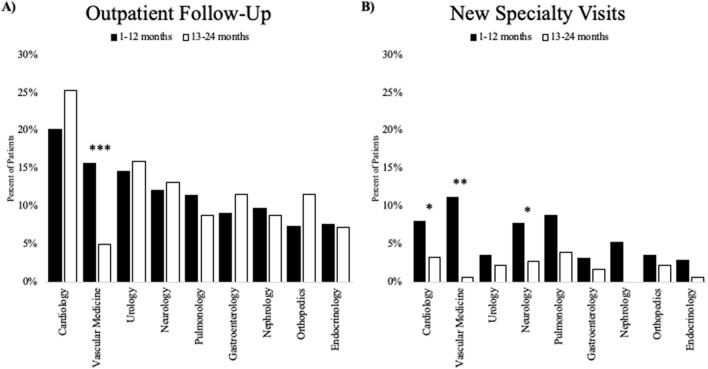
Vascular medicine follow-up visit rate at 1–12 months was higher than that at 13–24 months (p < 0.001, Fig. 3A). Other specialty visits had similar rates across the two time periods. Cardiology, vascular medicine, and neurology had more “new” specialty visits at 1–12 months compared to those at 13–24 months (p < 0.05 for all, Fig. 3B). New pulmonology visits were trending more at 1–12 months compared to those at 13–24 months (p = 0.06). All other new specialty visits were similar across both time periods (p > 0.05).
Fig. 3.
A Most common outpatient follow-up specialty seen at both time periods post-COVID-19. B Most common new (not associated with pre-existing comorbidities) outpatient follow-up specialty seen at both time periods post-COVID-19. * p < 0.05, ** p < 0.01, *** p < 0.001
ICU vs non-ICU
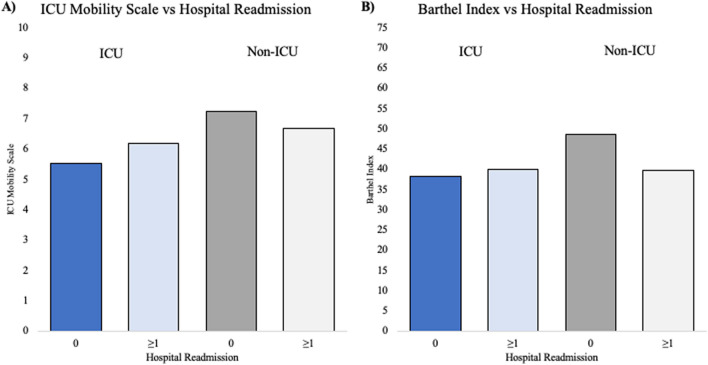
Compared to the ICU group (N = 89), the non-ICU group (N = 205) was older (64.6 ± 1.2, 57.6 ± 1.3 years old, p < 0.001), consisted of more non-Hispanic’s (71% vs 56%, p < 0.05) and more Caucasian’s (64% vs 47%, p < 0.01), had fewer males (48% vs 65%, p < 0.01), and had higher prevalence of HF, asthma, CKD, and smoking (all p < 0.05, Supplemental Table 3). Hypertension, diabetes, obesity, CAD, and COPD across both periods were not different between groups (p > 0.05). Surprisingly, more non-ICU patients were readmitted to the hospital than ICU patients (42% vs 15%, p < 0.001). Hospital readmission was not associated with functional status at hospital discharge as measured by ICU mobility scores and Barthel indices for both ICU and non-ICU group (p > 0.05, t test, Fig. 4).
Fig. 4.
A ICU mobility scores of patients with 0 hospital readmissions and ≥ 1 hospital readmissions. B Barthel Index scores of patients with 0 hospital readmissions and ≥ 1 hospital readmissions
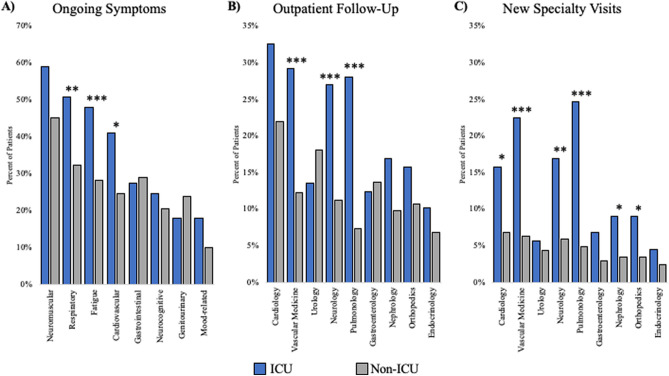
ICU patients exhibited significantly more ongoing chronic fatigue (p < 0.001), respiratory (p < 0.001), and cardiovascular symptoms (p < 0.05, Fig. 5A), but similar gastrointestinal and neurocognitive, genitourinary, and mood-related symptoms (p > 0.05) compared to the non-ICU group. Neuromuscular symptoms trended higher in ICU patients (p = 0.06). The ICU group made significantly more visits to vascular medicine, neurology, and pulmonology (p < 0.05, Fig. 5B), but a similar number of urology, gastroenterology, nephrology, orthopedics, and endocrinology visits (p > 0.05) compared to the non-ICU group. Cardiology visits were higher in ICU patients but did not reach statistical significance (p = 0.054). The ICU group made significantly more new specialty visits to cardiology, vascular medicine, neurology, pulmonology, nephrology, and orthopedics (p < 0.05, Fig. 5C), but a similar number of new urology, gastroenterology, orthopedics, and endocrinology visits compared to the non-ICU group (p > 0.05).
Fig. 5.
A Ongoing symptoms in ICU and non-ICU cohorts. B Most common outpatient follow-ups in ICU and non-ICU cohorts. C Most common new specialty in ICU and non-ICU cohorts. *p < 0.05, **p < 0.01, ***p < 0.001
Discussion
This study followed hospitalized COVID-19 patients with respect to medical referrals and specialty care usage at 1–24 months after discharge. The major findings were: (i) for those who returned, essentially all patients survived; (ii) hospital readmission was 34% but functional status scores at discharge were not associated with hospital readmission; (iii) between 13 and 50% of patients reported at least one ongoing symptoms (respiratory, gastrointestinal, neuromuscular, chronic fatigue symptoms) at follow-up which, other than respiratory and mood-related symptoms, persisted over time; (iv) common follow-up visits included to cardiology, vascular medicine, urology, and neurology; some of which were associated with pre-existing medical conditions while others appeared COVID-19 related; (v) there was good follow-up compliance of discharge referrals; (vi) most specialty follow-ups, other than vascular medicine, remained stable over time; and notably “new” vascular medicine follow-ups decreased over time; and (vii) the ICU group had more symptoms and follow-up medical visits compared to the non-ICU group. In this cohort, most hospitalized COVID-19 patients during the early pandemic survived 1–24 months post-discharge but many patients experienced persistent symptoms and sought new subspecialty care.
Mortality, major medical events, and readmission
The post-COVID-19 mortality rate has been reported to be 0% to 37% at about 6 months post-infection in a meta-analysis study [29]. The mortality rate of our hospitalized COVID-19 patients at 24 months follow-up was < 2%. Although it is possible that patients who did not return to our health system might have a higher mortality rate, it is unlikely as the no-return group had lower rates of pre-existing comorbidities and fewer ICU patients compared to the return group. Differences in findings among different studies are likely multifactorial, which include, but are not limited to, differences in patient profiles, geographical regions affected, duration of the pandemic, and follow-up time. It is likely that our cohorts were comparatively healthier because most of our patients were functionally independent prior to COVID-19 hospitalization [17, 18]. Nonetheless, about one-third of patients were readmitted to the hospital within 24 months of COVID-19 hospital discharge. The reasons for hospital readmission are multifactorial and heterogenous, making it difficult to summarize as a cohort summary. A previous study reported a 30% readmission rate among COVID-19 survivors 140 days (mean follow-up time) post-infection [30].
Symptomatic resolution
Neuromuscular, respiratory, fatigue, and cardiovascular symptoms were the most common in our cohort, consistent with previous long COVID studies [31–38]. Some COVID-19 symptoms, specifically respiratory and fatigue, have been reported to persist 1 year post-COVID-19 [39, 40], justifying the need for longer-term follow-ups. We found that respiratory and mood-related symptoms decreased over time up to 24 months, indicative of partial symptom resolution. Most symptoms however, had not completely resolved even at 24 months, suggesting persistent COVID-19 sequela. It is possible that some symptoms might be related to ongoing medical needs that predated SARS-CoV-2 infection or might be exacerbated by COVID-19 illness. Additionally, some symptoms might have been due to newly developed medical conditions unrelated to COVID-19 illness or hospitalization. It is difficult to discern the sources of these symptoms. Additional and longer-term follow-up studies are needed.
Another consideration is the role of anxiety in post-COVID-19 symptomology as uncertainty, social media hype, and misinformation during the pandemic may have led patients to develop psychosomatic rather than true physiological symptoms. It is possible that anxiety was underreported or unrealized by patients and instead reported as physical symptoms. The psychological reaction to the symptoms is difficult to discern.
Specialty follow-ups
A novelty of our study is the longitudinal assessment of medical subspecialty care received by COVID-19 survivors at follow-up. The high rates of pulmonologist, cardiologist, and nephrologist, neurologist, and vascular medicine visits are consistent with commonly reported organ system involvement in acute COVID-19 [41–46]. Some of these medical usages could be associated with ongoing medical needs which might have been exacerbated by COVID-19, while others were associated with new subspecialist needs due to new problems caused by COVID-19. The high proportion of new vascular medicine and pulmonology specialty visits suggests the latter. This likely reflects high rates of persistent respiratory symptoms as well as increased concerns for post-COVID thrombotic events. Conversely, cardiology, urology, and gastroenterology visits were predominantly associated with pre-existing comorbidities. The exact reasons for new specialty visits and re-hospitalizations after illness is not known. Reasons for seeking medical care could be associated with COVID-19, exacerbated by COVID-19, or pre-existing or new medical conditions unrelated to COVID-19. We separated new visits and visits due to existing conditions to provide insight. However, additional studies are needed. Comparison with other acute infections such as influenza could provide additional insight.
Akin to symptom persistence, it is not surprising that most outpatient specialty visits continued into the second year. Decreased vascular medicine visits likely reflect less concern for thromboembolic events beyond 1 year after hospital discharge and is consistent with medical guidelines [47]. It is also possible that continued follow-up was precautionary to ensure patient recovery into the second year. Furthermore, more new cardiology, vascular, neurology, and pulmonology visits during the first 12 months may reflect immediate post-COVID concerns, likely related to high rates of neuromuscular, respiratory, fatigue, and cardiovascular symptoms. The persistence of these symptoms and medical specialty visits suggests they are associated with COVID-19 infection although exacerbation of pre-existing conditions cannot be ruled out. Post-discharge rehabilitation measures may help to reduce symptoms and medical specialty care usage.
Interestingly, there were some mismatches between specialist visits and specialist referral rates, which could indicate unanticipated patient needs. When taken together with ongoing symptom complaints, this mismatch may serve as an objective measure of symptom-driven behavior and highlights which sequelae need additional attention. For example, more neurology, nephrology, and orthopedic follow-ups compared to referrals could suggest that these sequelae were relatively unforeseen during the acute phase of COVID-19 and were at least partially driven by ongoing symptoms. Conversely, less cardiology follow-ups compared to referrals might suggest that cardiovascular sequalae were not as severe as discharge physicians suspect or might have a delayed onset. Thus, patient would likely benefit from targeted rehabilitation therapy that addresses these unanticipated needs. These findings need to be independently verified using larger and multiple institutional data.
ICU vs non-ICU
The ICU cohort had a higher incidence of ongoing symptoms and subspecialty visits compared to the non-ICU group as expected. Greater neuromuscular and fatigue symptoms, along with greater neurology and orthopedic specialists visits is likely suggestive of post-Intensive Care Syndrome (PICS) [48]. Surprisingly, despite greater ongoing symptoms and specialist visits, all our ICU patients survived whereas only 97% of our non-ICU patients survived at 24-month follow-up. Surprisingly, more non-ICU patients were readmitted to the hospital than ICU patients. There might be a few reasons for this unexpected finding. First, it might be that in-hospital mortality selected for a healthier returning ICU cohort who were less susceptible to long-term morbidity and mortality after hospital discharge. This is supported by the fact that returning ICU patients were significantly younger and more functionally independent prior to COVID-19 than the non-ICU patients [17, 18]. Second, ICU patients received significantly more supplemental oxygen, durable medical equipment (DME), and medical follow-up recommendations than non-ICU patients [17, 18]. Thus, ICU patients might have received more vigilant, hands-on health management and rehabilitation that was protective against long-term mortality. Indeed, despite having greater ongoing symptoms, the ICU patients were not more likely to die suggesting that they might healthier and able to better withstand illnesses and/or they might receive better ongoing treatment.
Functional status scores
We found post-COVID-19 hospital readmission was not associated with ICU mobility and Barthel Index scores at hospital discharge, which is somewhat surprising as it has been shown that low scores on functional status at discharge is linked to longitudinally worse outcomes and increased morbidity [49, 50]. It is possible that patients with worse functional status received greater rehabilitation services, thus reducing the difference in morbidity that would be otherwise expected between ICU and non-ICU patients. The small sample size did not allow for adjustment for confounding covariates, such as age, pre-COVID status, comorbidity.
Limitations
This study has several limitations. This is a single site with a small sample size. This study is limited to patients who returned to our health system for any medical reason. Demographics of the patients who did and did not return were similar which minimized some unintentional biases. Nonetheless, it is possible that some patients who did not return had milder COVID-19 disease, and some might have died. Some symptoms were not well defined in the EMR and were difficult to classify into discrete categories. Thus, we relied on broad symptom categorization which might have considerable overlap that was difficult to differentiate. It is challenging to discern whether specialty follow-ups were related to pre-existing conditions, COVID-19 disease, or unrelated new medical conditions. Further prospective studies are needed to distinguish medical care need due to COVID-19 and pre-existing conditions.
Some COVID-19 symptoms might be over-reported or exaggerated due to heightened media attention, sensitivity, and anxiety around COVID-19 disease. Conversely, other symptoms might be underreported due to anti-anxiety medication use or by patients reporting only specialty-related complaints and not others. Objective measures are needed to assess long COVID-19 symptoms.
Analysis with respect to vaccination status was not performed because vaccination status was not consistently reported in EMR data. For example, patients who received vaccination from other healthcare providers were not consistently documented in our EMR. This is an inherent limitation of our healthcare system. Finally, the retrospective nature of this study could result in unintentional patient selection bias and confounds. Future studies need to include larger multiple site prospective studies.
Conclusions
This study reported high incidence of persistent symptoms and medical specialty care utilization in hospitalized COVID-19 survivors 1–24 months post-discharge. Common follow-up visits were cardiology, vascular medicine, urology, neurology, nephrology, gastroenterology and pulmonology, some were COVID-19 related or exacerbated by COVID-19 disease while others were associated with pre-existing medical conditions. Additional follow-up studies are needed to evaluate the long-term medical care needs of COVD-19 survivors.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
We thank all the doctors, nurses and clinical scientists who worked in the hospital during the period of patient recruitment as well as the patients who were involved in this study
Author contributions
Benjamin Musheyev, Montek S Boparai, Rebeca Janowicz, Stacey Pamlanye, Reona Kimura, and Wei Hou conceptualized and analyzed the data and drafted the paper. Tim Q. Duong conceptualized, wrote/edited the paper, and supervised the work.
Funding
None.
Availability of supporting data
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Competing interests
All authors declare no competing interests.
Ethical approval and consent to participate
Approval of the ethics committee of Stony Brook University Hospital.
Consent for publication
All authors consent to publish.
Human and animal rights statement and Informed consent
This study was approved by the Stony Brook University Institutional Review Board (#2020-00207) with an exemption for informed consent.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Groff D, Sun A, Ssentongo AE, Ba DM, Parsons N, Poudel GR, Lekoubou A, Oh JS, Ericson JE, Ssentongo P, Chinchilli VM. Short-term and long-term rates of postacute sequelae of SARS-CoV-2 infection: a systematic review. JAMA Netw Open. 2021;4:e2128568. doi: 10.1001/jamanetworkopen.2021.28568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Augustin M, Schommers P, Stecher M, Dewald F, Gieselmann L, Gruell H, Horn C, Vanshylla K, Cristanziano VD, Osebold L, Roventa M, Riaz T, Tschernoster N, Altmueller J, Rose L, Salomon S, Priesner V, Luers JC, Albus C, Rosenkranz S, Gathof B, Fatkenheuer G, Hallek M, Klein F, Suarez I, Lehmann C. Post-COVID syndrome in non-hospitalised patients with COVID-19: a longitudinal prospective cohort study. Lancet Reg Health Eur. 2021;6:100122. doi: 10.1016/j.lanepe.2021.100122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kamal M, Abo Omirah M, Hussein A, Saeed H. Assessment and characterisation of post-COVID-19 manifestations. Int J Clin Pract. 2021;75:e13746. doi: 10.1111/ijcp.13746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Munblit D, Bobkova P, Spiridonova E, Shikhaleva A, Gamirova A, Blyuss O, Nekliudov N, Bugaeva P, Andreeva M, DunnGalvin A, Comberiati P, Apfelbacher C, Genuneit J, Avdeev S, Kapustina V, Guekht A, Fomin V, Svistunov AA, Timashev P, Subbot VS, Royuk VV, Drake TM, Hanson SW, Merson L, Carson G, Horby P, Sigfrid L, Scott JT, Semple MG, Warner JO, Vos T, Olliaro P, Glybochko P, Butnaru D, Sechenov Stop CRT. Incidence and risk factors for persistent symptoms in adults previously hospitalized for COVID-19. Clin Exp Allergy. 2021;51:1107–1120. doi: 10.1111/cea.13997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Willi S, Luthold R, Hunt A, Hanggi NV, Sejdiu D, Scaff C, Bender N, Staub K, Schlagenhauf P. COVID-19 sequelae in adults aged less than 50 years: a systematic review. Travel Med Infect Dis. 2021;40:101995. doi: 10.1016/j.tmaid.2021.101995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Huang L, Li X, Gu X, Zhang H, Ren L, Guo L, Liu M, Wang Y, Cui D, Wang Y, Zhang X, Shang L, Zhong J, Wang X, Wang J, Cao B. Health outcomes in people 2 years after surviving hospitalisation with COVID-19: a longitudinal cohort study. Lancet Respir Med. 2022 doi: 10.1016/s2213-2600(22)00126-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zeng N, Zhao YM, Yan W, Li C, Lu QD, Liu L, Ni SY, Mei H, Yuan K, Shi L, Li P, Fan TT, Yuan JL, Vitiello MV, Kosten T, Kondratiuk AL, Sun HQ, Tang XD, Liu MY, Lalvani A, Shi J, Bao YP, Lu L. A systematic review and meta-analysis of long term physical and mental sequelae of COVID-19 pandemic: call for research priority and action. Mol Psychiatry. 2022 doi: 10.1038/s41380-022-01614-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sanchez-Ramirez DC, Normand K, Zhaoyun Y, Torres-Castro R. Long-term impact of COVID-19: a systematic review of the literature and meta-analysis. Biomedicines. 2021 doi: 10.3390/biomedicines9080900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tran VT, Porcher R, Pane I, Ravaud P. Course of post COVID-19 disease symptoms over time in the ComPaRe long COVID prospective e-cohort. Nat Commun. 2022;13:1812. doi: 10.1038/s41467-022-29513-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Whitaker M, Elliott J, Chadeau-Hyam M, Riley S, Darzi A, Cooke G, Ward H, Elliott P. Persistent COVID-19 symptoms in a community study of 606,434 people in England. Nat Commun. 2022;13:1957. doi: 10.1038/s41467-022-29521-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Townsend L, Dyer AH, Jones K, Dunne J, Mooney A, Gaffney F, O'Connor L, Leavy D, O'Brien K, Dowds J, Sugrue JA, Hopkins D, Martin-Loeches I, Ni Cheallaigh C, Nadarajan P, McLaughlin AM, Bourke NM, Bergin C, O'Farrelly C, Bannan C, Conlon N. Persistent fatigue following SARS-CoV-2 infection is common and independent of severity of initial infection. PLoS ONE. 2020;15:e0240784. doi: 10.1371/journal.pone.0240784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mao L, Jin H, Wang M, Hu Y, Chen S, He Q, Chang J, Hong C, Zhou Y, Wang D, Miao X, Li Y, Hu B. Neurologic manifestations of hospitalized patients with coronavirus disease 2019 in Wuhan, China. JAMA Neurol. 2020;77:683–690. doi: 10.1001/jamaneurol.2020.1127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Carfi A, Bernabei R, Landi F, Gemelli Against C-P-ACSG. Persistent symptoms in patients after acute COVID-19. JAMA. 2020;324:603–605. doi: 10.1001/jama.2020.12603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Garrigues E, Janvier P, Kherabi Y, Le Bot A, Hamon A, Gouze H, Doucet L, Berkani S, Oliosi E, Mallart E, Corre F, Zarrouk V, Moyer JD, Galy A, Honsel V, Fantin B, Nguyen Y. Post-discharge persistent symptoms and health-related quality of life after hospitalization for COVID-19. J Infect. 2020;81:e4–e6. doi: 10.1016/j.jinf.2020.08.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Moghimi N, Di Napoli M, Biller J, Siegler JE, Shekhar R, McCullough LD, Harkins MS, Hong E, Alaouieh DA, Mansueto G, Divani AA. The neurological manifestations of post-acute sequelae of SARS-CoV-2 infection. Curr Neurol Neurosci Rep. 2021;21:44. doi: 10.1007/s11910-021-01130-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Iosifescu AL, Hoogenboom WS, Buczek AJ, Fleysher R, Duong TQ. New-onset and persistent neurological and psychiatric sequelae of COVID-19 compared to influenza: A retrospective cohort study in a large New York City healthcare network. Int J Methods Psychiatr Res. 2022 doi: 10.1002/mpr.1914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Musheyev B, Borg L, Janowicz R, Matarlo M, Boyle H, Singh G, Ende V, Babatsikos I, Hou W, Duong TQ. Functional status of mechanically ventilated COVID-19 survivors at ICU and hospital discharge. J Intensive Care. 2021;9:31. doi: 10.1186/s40560-021-00542-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Musheyev B, Janowicz R, Borg L, Matarlo M, Boyle H, Hou W, Duong TQ. Characterizing non-critically ill COVID-19 survivors with and without in-hospital rehabilitation. Sci Rep. 2021;11:21039. doi: 10.1038/s41598-021-00246-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Prevention CfDCa, Long COVID or Post-COVID Conditions, Accessed March 1st 2022.
- 20.Chen A, Zhao Z, Hou W, Singer AJ, Li H, Duong TQ. Time-to-death longitudinal characterization of clinical variables and longitudinal prediction of mortality in COVID-19 patients: a two-center study. Front Med (Lausanne) 2021;8:661940. doi: 10.3389/fmed.2021.661940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ende VJ, Singh G, Babatsikos I, Hou W, Li H, Thode HC, Singer AJ, Duong TQ, Richman PS. Survival of COVID-19 patients with respiratory failure is related to temporal changes in gas exchange and mechanical ventilation. J Intensive Care Med. 2021;36:1209–1216. doi: 10.1177/08850666211033836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hou W, Zhao Z, Chen A, Li H, Duong TQ. Machining learning predicts the need for escalated care and mortality in COVID-19 patients from clinical variables. Int J Med Sci. 2021;18:1739–1745. doi: 10.7150/ijms.51235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lam KW, Chow KW, Vo J, Hou W, Li H, Richman PS, Mallipattu SK, Skopicki HA, Singer AJ, Duong TQ. Continued in-hospital ACE inhibitor and ARB Use in hypertensive COVID-19 patients is associated with positive clinical outcomes. J Infect Dis. 2020;222:1256–1264. doi: 10.1093/infdis/jiaa447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Li X, Ge P, Zhu J, Li H, Graham J, Singer A, Richman PS, Duong TQ. Deep learning prediction of likelihood of ICU admission and mortality in COVID-19 patients using clinical variables. PeerJ. 2020;8:e10337. doi: 10.7717/peerj.10337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lu JQ, Musheyev B, Peng Q, Duong TQ. Neural network analysis of clinical variables predicts escalated care in COVID-19 patients: a retrospective study. PeerJ. 2021;9:e11205. doi: 10.7717/peerj.11205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Holu JY, Hou W, Duong TQ. Longitudinal prediction of hospital-acquired acute kidney injury in COVID-19: a two-center study. Infection. 2022;50:109–119. doi: 10.1007/s15010-021-01646-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Shen B, Hoshmand-Kochi M, Abbasi A, Glass S, Jiang Z, Singer AJ, Thode HC, Li H, Hou W, Duong TQ. Initial chest radiograph scores inform COVID-19 status, intensive care unit admission and need for mechanical ventilation. Clin Radiol. 2021;76:473.e471–473.e477. doi: 10.1016/j.crad.2021.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zhao Z, Chen A, Hou W, Graham JM, Li H, Richman PS, Thode HC, Singer AJ, Duong TQ. Prediction model and risk scores of ICU admission and mortality in COVID-19. PLoS ONE. 2020;15:e0236618. doi: 10.1371/journal.pone.0236618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ramzi ZS. Hospital readmissions and post-discharge all-cause mortality in COVID-19 recovered patients; A systematic review and meta-analysis. Am J Emerg Med. 2022;51:267–279. doi: 10.1016/j.ajem.2021.10.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ayoubkhani D, Khunti K, Nafilyan V, Maddox T, Humberstone B, Diamond I, Banerjee A. Post-COVID syndrome in individuals admitted to hospital with COVID-19: retrospective cohort study. BMJ. 2021 doi: 10.1136/bmj.n693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Michelen M, Manoharan L, Elkheir N, Cheng V, Dagens A, Hastie C, O'Hara M, Suett J, Dahmash D, Bugaeva P, Rigby I, Munblit D, Harriss E, Burls A, Foote C, Scott J, Carson G, Olliaro P, Sigfrid L, Stavropoulou C. Characterising long COVID: a living systematic review. BMJ Glob Health. 2021 doi: 10.1136/bmjgh-2021-005427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Romero-Duarte A, Rivera-Izquierdo M, Guerrero-Fernandez de Alba I, Perez-Contreras M, Fernandez-Martinez NF, Ruiz-Montero R, Serrano-Ortiz A, Gonzalez-Serna RO, Salcedo-Leal I, Jimenez-Mejias E, Cardenas-Cruz A. Sequelae, persistent symptomatology and outcomes after COVID-19 hospitalization: the ANCOHVID multicentre 6-month follow-up study. BMC Med. 2021;19:129. doi: 10.1186/s12916-021-02003-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Darcis G, Bouquegneau A, Maes N, Thys M, Henket M, Labye F, Rousseau AF, Canivet P, Desir C, Calmes D, Schils R, De Worm S, Leonard P, Meunier P, Moutschen M, Louis R, Guiot J. Long-term clinical follow-up of patients suffering from moderate-to-severe COVID-19 infection: a monocentric prospective observational cohort study. Int J Infect Dis. 2021;109:209–216. doi: 10.1016/j.ijid.2021.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Davis HE, Assaf GS, McCorkell L, Wei H, Low RJ, Re'em Y, Redfield S, Austin JP, Akrami A. Characterizing long COVID in an international cohort: 7 months of symptoms and their impact. EClinicalMedicine. 2021;38:101019. doi: 10.1016/j.eclinm.2021.101019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Huang C, Huang L, Wang Y, Li X, Ren L, Gu X, Kang L, Guo L, Liu M, Zhou X, Luo J, Huang Z, Tu S, Zhao Y, Chen L, Xu D, Li Y, Li C, Peng L, Li Y, Xie W, Cui D, Shang L, Fan G, Xu J, Wang G, Wang Y, Zhong J, Wang C, Wang J, Zhang D, Cao B. 6-month consequences of COVID-19 in patients discharged from hospital: a cohort study. The Lancet. 2021;397:220–232. doi: 10.1016/s0140-6736(20)32656-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Petersen MS, Kristiansen MF, Hanusson KD, Danielsen ME, B AS, Gaini S, Strom M, Weihe P, Long COVID in the Faroe Islands: A Longitudinal Study Among Nonhospitalized Patients. Clin Infect Dis. 2021;73:e4058–e4063. doi: 10.1093/cid/ciaa1792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Logue JK, Franko NM, McCulloch DJ, McDonald D, Magedson A, Wolf CR, Chu HY. Sequelae in adults at 6 months after COVID-19 infection. JAMA Netw Open. 2021;4:e210830. doi: 10.1001/jamanetworkopen.2021.0830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Arnold DT, Hamilton FW, Milne A, Morley AJ, Viner J, Attwood M, Noel A, Gunning S, Hatrick J, Hamilton S, Elvers KT, Hyams C, Bibby A, Moran E, Adamali HI, Dodd JW, Maskell NA, Barratt SL. Patient outcomes after hospitalisation with COVID-19 and implications for follow-up: results from a prospective UK cohort. Thorax. 2021;76:399–401. doi: 10.1136/thoraxjnl-2020-215818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Boscolo-Rizzo P, Guida F, Polesel J, Marcuzzo AV, Capriotti V, D'Alessandro A, Zanelli E, Marzolino R, Lazzarin C, Antonucci P, Sacchet E, Tofanelli M, Borsetto D, Gardenal N, Pengo M, Tirelli G. Sequelae in adults at 12 months after mild-to-moderate coronavirus disease 2019 (COVID-19) Int Forum Allergy Rhinol. 2021;11:1685–1688. doi: 10.1002/alr.22832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bellan M, Baricich A, Patrucco F, Zeppegno P, Gramaglia C, Balbo PE, Carriero A, Amico CS, Avanzi GC, Barini M, Battaglia M, Bor S, Cantaluppi V, Cappellano G, Ceruti F, Chiocchetti A, Clivati E, Giordano M, Cuneo D, Gambaro E, Gattoni E, Loro A, Manfredi M, Morosini U, Murano F, Paracchini E, Patti G, Pinato DJ, Raineri D, Rolla R, Sainaghi PP, Tricca S, Pirisi M. Long-term sequelae are highly prevalent one year after hospitalization for severe COVID-19. Sci Rep. 2021;11:22666. doi: 10.1038/s41598-021-01215-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Chen T, Wu D, Chen H, Yan W, Yang D, Chen G, Ma K, Xu D, Yu H, Wang H, Wang T, Guo W, Chen J, Ding C, Zhang X, Huang J, Han M, Li S, Luo X, Zhao J, Ning Q. Clinical characteristics of 113 deceased patients with coronavirus disease 2019: retrospective study. BMJ. 2020 doi: 10.1136/bmj.m1091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, Wang B, Xiang H, Cheng Z, Xiong Y, Zhao Y, Li Y, Wang X, Peng Z. Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China. JAMA. 2020;323:1061–1069. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lu JQ, Lu JY, Wang W, Liu Y, Buczek A, Fleysher R, Hoogenboom WS, Zhu W, Hou W, Rodriguez CJ, Duong TQ. Clinical predictors of acute cardiac injury and normalization of troponin after hospital discharge from COVID-19. EBioMedicine. 2022 doi: 10.1016/j.ebiom.2022.103821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lu JY, Anand H, Frager SZ, Hou W, Duong TQ. Longitudinal progression of clinical variables associated with graded liver injury in COVID-19 patients. Hepatol Int. 2021;15:1018–1026. doi: 10.1007/s12072-021-10228-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lu JY, Babatsikos I, Fisher MC, Hou W, Duong TQ. Longitudinal clinical profiles of hospital vs. community-acquired acute kidney injury in COVID-19. Front Med (Lausanne) 2021;8:647023. doi: 10.3389/fmed.2021.647023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lu JY, Buczek A, Fleysher R, Hoogenboom WS, Hou W, Rodriguez CJ, Fisher MC, Duong TQ. Outcomes of Hospitalized Patients With COVID-19 With Acute Kidney Injury and Acute Cardiac Injury. Front Cardiovasc Med. 2021;8:798897. doi: 10.3389/fcvm.2021.798897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hong J, Ahn SY, Lee YJ, Lee JH, Han JW, Kim KH, Yhim HY, Nam SH, Kim HJ, Song J, Kim SH, Bang SM, Kim JS, Mun YC, Bae SH, Kim HK, Jang S, Park R, Choi HS, Kim I, Oh D, Korean Society of Hematology T, Hemostasis Working P Updated recommendations for the treatment of venous thromboembolism. Blood Res. 2021;56:6–16. doi: 10.5045/br.2021.2020083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Rawal G, Yadav S, Kumar R. Post-intensive care syndrome: an overview. J Transl Int Med. 2017;5:90–92. doi: 10.1515/jtim-2016-0016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Tipping CJ, Bailey MJ, Bellomo R, Berney S, Buhr H, Denehy L, Harrold M, Holland A, Higgins AM, Iwashyna TJ, Needham D, Presneill J, Saxena M, Skinner EH, Webb S, Young P, Zanni J, Hodgson CL. The ICU mobility scale has construct and predictive validity and is responsive. a multicenter observational study. Ann Am Thorac Soc. 2016;13:887–893. doi: 10.1513/AnnalsATS.201510-717OC. [DOI] [PubMed] [Google Scholar]
- 50.Torres OH, Francia E, Longobardi V, Gich I, Benito S, Ruiz D. Short- and long-term outcomes of older patients in intermediate care units. Intensive Care Med. 2006;32:1052–1059. doi: 10.1007/s00134-006-0170-1. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.