Abstract
Objectives
To evaluate the recapture of response with open-label (OL) ixekizumab (IXE) retreatment at week 104 in patients with axial spondyloarthritis who flared after withdrawal of IXE therapy.
Methods
COAST-Y (NCT03129100) is a phase III extension study that included a double-blind, placebo-controlled, randomised withdrawal-retreatment period (RWRP). Patients who achieved remission (Ankylosing Spondylitis Disease Activity Score (ASDAS) <1.3 (inactive disease, ID) at least once at week 16 or 20 and <2.1 (low disease activity, LDA) at both visits) were randomised 2:1 at week 24 to continue IXE or withdraw to placebo. Patients who subsequently flared were switched to OL IXE every 2 or 4 weeks (Q2W or Q4W) at the next visit. The proportions of patients who recaptured ASDAS LDA and ID were summarised for those who experienced flare.
Results
Of the 155 patients who entered the RWRP (placebo, n=53; IXE Q4W, n=48; IXE Q2W, n=54), 138 (89%) completed week 104. Of the placebo-treated patients (n=53), 28 (53%) experienced a flare during weeks 24–104; of these, 4 (14%) recaptured ASDAS LDA before retreatment with OL IXE, and 23 (82%) recaptured ASDAS LDA and 19 (68%) met ASDAS ID after retreatment. Of the continuously treated IXE patients (n=102), 13 experienced flare; 7 of 13 (54%) recaptured ASDAS LDA before switching to OL IXE retreatment, while 5 of 13 (38%) recaptured ASDAS LDA and 4 of 13 (31%) met ID after switching.
Conclusions
Ninety-six per cent of patients withdrawn to placebo recaptured at least ASDAS LDA and 71% recaptured ASDAS ID with IXE retreatment at week 104. This may provide support to patients who may require a brief interruption in therapy.
Keywords: Antirheumatic Agents; Spondylitis, Ankylosing; Biological Therapy; Immune System Diseases
WHAT IS ALREADY KNOWN ON THIS TOPIC
Previous randomised withdrawal studies of tumour necrosis factor inhibitors suggest continuous treatment is important in maintaining clinical response in patients with axial spondyloarthritis (axSpA) and that discontinuation may lead to loss of efficacy when restarted.
WHAT THIS STUDY ADDS
This is the first randomised withdrawal and retreatment study of an IL-17A antagonist in patients with axSpA.
The majority of patients who were rerandomised to placebo (ixekizumab withdrawal) and experienced a flare recaptured at least Ankylosing Spondylitis Disease Activity Score low disease activity with ixekizumab retreatment by week 104.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
These findings may provide important information regarding treatment decisions in case a treatment interruption is needed or requested by the patient.
Introduction
Patients with axial spondyloarthritis (axSpA) experience a high burden of disease and rely on long-term therapy for maintenance of disease control.1 2 The European Alliance of Associations for Rheumatology guidelines and current treat-to-target recommendations suggest that once a patient achieves a state of remission or low disease activity (LDA), physicians may taper, but not stop, treatment.3 However, patients frequently must pause active treatment due to elective surgery or in the event of an infection. During a follow-up period ranging from 36 to 52 weeks (with a median of 52 weeks), between 76% and 100% of patients with axSpA experience a flare after stopping or discontinuing an anti-tumour necrosis factor inhibitor (TNFi) without tapering.4 Thus, it is of importance for both physicians and patients to know that recapture of treatment response is possible after a pause, unexpected or otherwise, in therapy.
COAST-Y is the first study to evaluate the effect of continuing versus withdrawing an interleukin (IL)-17A antagonist, ixekizumab (IXE), on the maintenance of disease control in patients with radiographic (r) and non-radiographic (nr) axSpA through 104 weeks.5 The aim of the present analysis is to evaluate the recapture of response with open-label (OL) IXE retreatment at week 104 in patients with axSpA who flared after withdrawal of IXE therapy.
Methods
Patients
COAST-Y (NCT03129100) enrolled patients (n=773) from any of the three originating studies: two on r-axSpA (COAST-V, NCT02696785; COAST-W, NCT02696798) and one on nr-axSpA (COAST-X, NCT02757352). Complete eligibility criteria for the three originating studies and COAST-Y have been published.5–8
Study design
COAST-Y is a long-term extension study that contained an OL lead-in period and a double-blind, placebo-controlled, randomised withdrawal-retreatment period (RWRP) (online supplemental figure 1).5 Patients entered a 24-week lead-in period (weeks 0–24) and continued either 80 mg IXE every 2 weeks (Q2W) or every 4 weeks (Q4W). Patients who continuously received blinded placebo up to the completion of COAST-X were assigned to IXE Q4W during the lead-in period of COAST-Y. Patients from COAST-V and COAST-W continued on the same treatment they were receiving at the end of the originating trial.
ard-2022-222731supp001.pdf (519.8KB, pdf)
On completion of the lead-in period at week 24, patients who achieved remission (n=155) (defined as an Ankylosing Spondylitis Disease Activity Score (ASDAS) of <1.3 at least once at week 16 or week 20 and <2.1 at both visits) entered the RWRP. Patients were randomly assigned in equal proportions to continue blinded IXE Q4W, continue blinded IXE Q2W or withdraw to placebo. Thus, the observed withdrawal period occurred after the 24-week lead-in, for 80 weeks between week 24 and week 104.
Patients who experienced a flare (defined as an ASDAS of ≥2.1 at two consecutive visits or an ASDAS of >3.5 at any visit during the RWRP between weeks 24 and 104) were retreated in an OL manner at the next visit with the same dose of IXE dosing regimen received during the lead-in period.
Outcomes
The primary outcome of COAST-Y was the proportion of patients in the randomised withdrawal population who did not experience a flare during the RWRP; the results have previously been published.5 This analysis describes the recapture rates at week 104 of patients who were rerandomised to either placebo (IXE withdrawal) or IXE who experienced a flare. A recapture of treatment response refers to a patient achieving either ASDAS LDA or ASDAS inactive disease (ID) following retreatment with IXE therapy during the RWRP. Other outcomes of COAST-Y at week 104 included the proportion of flare-free patients in the combined IXE Q2W and IXE Q4W group, IXE Q4W group, and IXE Q2W group versus those withdrawn to placebo group.
Statistical analysis
The proportions of patients who experienced a flare and recaptured ASDAS LDA and ASDAS ID before or after OL IXE retreatment are reported using descriptive statistics. A post-hoc assessment was conducted to evaluate the ASDAS disease activity category at the individual patient-level from weeks 24 to 64. The Kaplan-Meier product limit method was used to estimate the time to flare. Individual patient-level data on the ASDAS disease activity response status during the COAST-Y study (weeks 0–104) are visually presented for patients who entered the RWRP (n=155). Post-hoc assessments were also conducted to evaluate potential predictors of flare. Due to a small number of patients experiencing flares with continuous IXE treatment, the two IXE treatment groups (IXE Q4W and IXE Q2W) were pooled into a combined IXE group. Post-hoc analyses were conducted to evaluate potential predictors of flare. Variables with p values <0.2 were entered into the multivariate logistic model for stepwise selection, with a p value of 0.1 a criterion for removal and stay. Interaction of each of the variables of interest with IXE treatment withdrawal was also evaluated in an individual logistic regression model. Variables and their corresponding interaction were entered into the multivariate logistic regression model for variables found in the stepwise selection procedure; a backward selection was used to build the final model.
Patient and public involvement
Patients were not involved in the design or conduct of the study, development of outcomes, or dissemination of study results.
Results
Patients
Of the 773 patients enrolled in COAST-Y, 741 completed the 24-week lead-in period and 155 patients met the criteria for remission and entered the RWRP. Of these, 138 patients completed week 104. Baseline demographics and disease characteristics of patients who entered the RWRP (n=155) were balanced across treatment arms (online supplemental table 1).
ard-2022-222731supp003.pdf (42.1KB, pdf)
Incidence rates of flare through 104 weeks
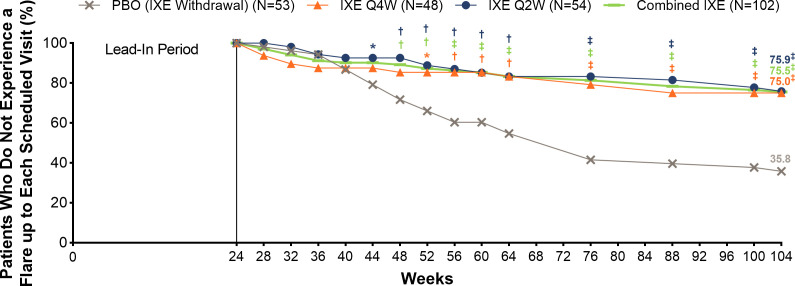
At week 104, significantly more patients in the combined IXE group (75.5%, p<0.001; IXE Q4W: 75.0%, p<0.001; IXE Q2W: 75.9%, p<0.001) remained flare-free versus placebo (figure 1). Notably, 35.8% of patients receiving placebo never experienced flare.
Figure 1.
Proportion (%) of patients who remained flare-free through 104 weeks. *P<0.05, †P<0.01, ‡P<0.001 versus IXE withdrawal (placebo). IXE, ixekizumab; PBO, placebo; Q2W, every 2 weeks; Q4W, every 4 weeks.
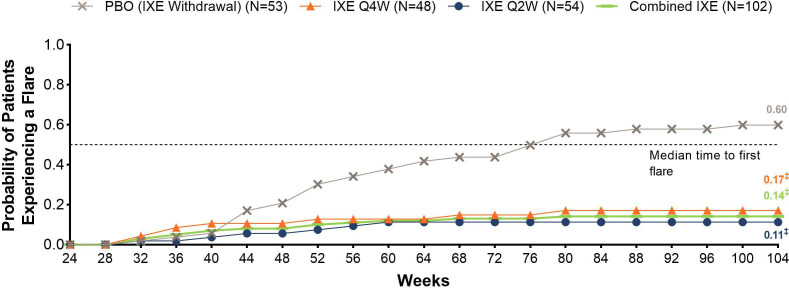
At week 104, the Kaplan-Meier estimate of median time to first flare was 52.1 weeks for placebo (IXE withdrawal). Continuing IXE treatment significantly delayed time to flare versus withdrawal to placebo for the combined IXE, IXE Q4W and IXE Q2W groups (p<0.001 for all; figure 2).
Figure 2.
Kaplan-Meier estimate of time to first flare (weeks) through 104 weeks for patients who were randomised to placebo (IXE withdrawal) or continuous IXE. ‡P<0.001 versus placebo (IXE withdrawal). IXE, ixekizumab; N, number of patients; PBO, placebo; Q2W, every 2 weeks; Q4W, every 4 weeks.
When the incidence of a flare was assessed using ASDAS worsening of ≥0.9 points, at week 104, significantly more patients in the combined IXE group (68.2%, p<0.001; IXE Q4W: 73.2%, p<0.001; IXE Q2W: 63.8%, p<0.001) remained flare-free versus placebo (20.8%; online supplemental figure 2). A total of 22% of patients receiving placebo never experienced a flare.
ard-2022-222731supp002.pdf (105.1KB, pdf)
Recapture of treatment response before or after IXE retreatment
Of the placebo (IXE withdrawal)-treated patients (n=53), a total of 28 patients experienced a flare and were retreated with OL IXE (table 1). Around 96% (27 of 28) of these patients recaptured ASDAS LDA by week 104; 4 patients recaptured ASDAS LDA before retreatment and 23 patients recaptured that response within 16 weeks of retreatment.
Table 1.
Recapture of treatment response before or after switching to OL IXE through 104 weeks among patients randomised to placebo (IXE withdrawal) who experienced a flare and were retreated
| Total patients who flared and were switched to OL IXE retreatment | Placebo (IXE withdrawal) (N=28) | |
| ASDAS disease activity status | LDA | ID |
| Recaptured response before OL IXE retreatment, n | 4 | 1 |
| Recaptured response with OL IXE retreatment (≤16 weeks), n | 23 | 14 |
| Recaptured response with OL IXE retreatment (>16 weeks), n | 0 | 5 |
| Total patients who recaptured response by week 104, n (%) | 27/28 (96) | 20/28 (71) |
In each column, the denominator is 28. A total of 4 patients met the criteria for flare and were not retreated. 20 patients had achieved ASDAS ID, while 8 patients achieved ASDAS LDA before flare and OL IXE retreatment.
ASDAS, Ankylosing Spondylitis Disease Activity Score; ID, inactive disease; IXE, ixekizumab; LDA, low disease activity including ID; N, number of patients in the analysis population; OL, open-label.
Of the placebo-treated patients who experienced a flare, 71% (20 of 28) recaptured ASDAS ID by week 104; 1 patient recaptured response before retreatment, 14 patients recaptured ASDAS ID within 16 weeks of OL IXE, while 5 patients recaptured an ASDAS ID response after 16 weeks of OL IXE retreatment.
Of the patients who were continuously treated with IXE (IXE Q4W, n=48; IXE Q2W, n=54), a total of 13 patients experienced a flare and were retreated with OL IXE (IXE Q4W, n=7; IXE Q2W, n=6, table 2). Around 92% (12 of 13) of patients recaptured ASDAS LDA by week 104 (IXE Q4W, n=7; IXE Q2W, n=5); seven patients recaptured ASDAS LDA before OL IXE retreatment, two patients recaptured within 16 weeks, while three patients recaptured an ASDAS LDA response after 16 weeks of OL IXE retreatment.
Table 2.
Recapture of first treatment response before or after switching to OL IXE through 104 weeks among patients continuously treated with IXE who experienced a flare and were switched to OL IXE
| Total patients who flared and were switched to OL IXE retreatment | Continuous IXE (N=13) | |
| ASDAS disease activity status | LDA | ID |
| Recaptured response before OL IXE retreatment, n | 7 | 1 |
| Recaptured response with OL IXE retreatment (≤16 weeks), n | 2 | 3 |
| Recaptured response with OL IXE retreatment (>16 weeks), n | 3 | 1 |
| Total patients who recaptured response by week 104, n (%) | 12/13 (92) | 5/13 (38) |
In each column, the denominator is 13. Only one patient met the criteria for flare and was not retreated. Six patients had achieved ASDAS ID and seven patients achieved ASDAS LDA before flare and OL IXE retreatment.
ASDAS, Ankylosing Spondylitis Disease Activity Score; ID, inactive disease; IXE, ixekizumab; LDA, low disease activity including ID; N, number of patients in the analysis population; OL, open-label.
A total of 5 (IXE Q4W, n=3; IXE Q2W, n=2) out of 13 (IXE Q4W, n=7; IXE Q2W, n=6) patients continuously treated with IXE, who experienced a flare and were retreated, recaptured an ASDAS ID response by week 104; one patient recaptured ASDAS ID before OL IXE retreatment, three patients recaptured within 16 weeks of retreatment, while one patient recaptured ASDAS ID after 16 weeks of OL IXE retreatment.
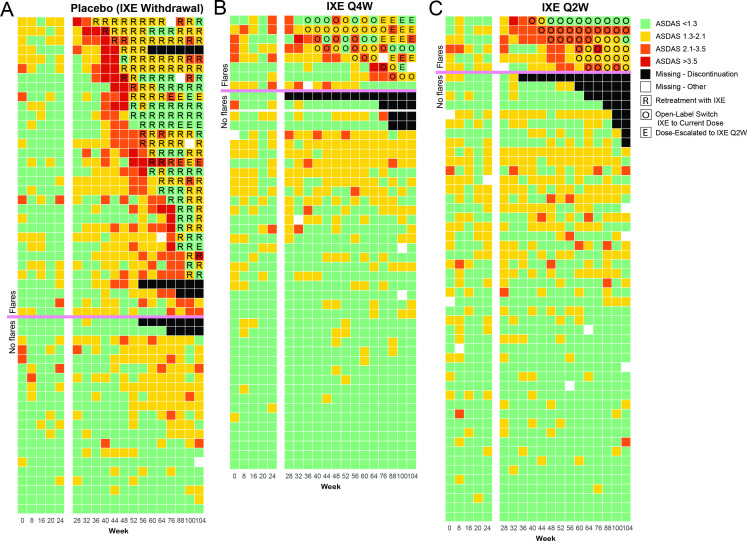
Sustainability of treatment response
Heatmaps were generated to show the maintenance of ASDAS status through 104 weeks among patients who were randomised to placebo, IXE Q4W or IXE Q2W at week 24 (figure 3). Individual patient ASDAS disease activity, as ASDAS ID (ASDAS <1.3) (green), ASDAS LDA (ASDAS ≥1.3 and <2.1) (yellow), ASDAS high disease activity (ASDAS ≥2.1 and <3.5) (orange) and ASDAS very high disease activity (ASDAS ≥3.5) (red), is shown for patients who did and did not experience a flare in disease activity, at 4-weekly intervals from weeks 24–64 and weeks 100–104 of COAST-Y and at 12-weekly intervals from weeks 64 to 100. Each row corresponds to one patient, with patients organised in order of descending disease activity. In addition, patients who experienced a flare in disease activity and were retreated with OL IXE (figure 3A) or were switched to OL IXE (figure 3B, C) are presented at the top of the heatmap. The heatmap diagrams illustrate that the majority of patients who achieve ASDAS LDA or lower at week 24 sustain that treatment response through 104 weeks of COAST-Y.
Figure 3.
Heatmap diagram showing ASDAS disease activity status through 104 weeks among patients randomised to (A) placebo (IXE withdrawal), (B) IXE Q4W or (C) IXE Q2W at week 24. Each row corresponds to an individual patient and each column corresponds to a specific week of COAST-Y. ASDAS, Ankylosing Spondylitis Disease Activity Score; IXE, ixekizumab; Q2W, every 2 weeks; Q4W, every 4 weeks.
Predictors of flare
Post-hoc analysis for the randomised withdrawal-retreatment intention-to-treat population was conducted to identify patient characteristics that were associated with flare (online supplemental tables 2–4). Multivariate model analysis identified the ASDAS area under the curve between weeks 0 and 24 of COAST-Y as being associated with flare (OR 1.08, 95% CI 1.03 to 1.14; online supplemental table 3).
ard-2022-222731supp004.pdf (46.9KB, pdf)
ard-2022-222731supp005.pdf (22.8KB, pdf)
ard-2022-222731supp006.pdf (24.1KB, pdf)
In addition, when the interaction of treatment by the potential predictors of flare was assessed, treatment (IXE withdrawal) and ASDAS area under the curve were identified as predictors of flare (online supplemental table 4). A significant interaction of IXE withdrawal by symptom duration at the beginning of COAST-Y was also observed, indicating longer symptom duration (≥5 years) was associated with flare in patients who were withdrawn to placebo, whereas this association was not observed in patients who continued IXE treatment.
Discussion
COAST-Y is the first study to compare the maintenance of disease control in patients with axSpA who continued versus those who withdrew an IL-17A antagonist (IXE) after having achieved remission. This analysis demonstrates that the majority of patients who were withdrawn from IXE to placebo and experienced a flare recaptured either ASDAS LDA or ID within 16 weeks of OL IXE retreatment.
Over half of the patients who were withdrawn to placebo and experienced flare recaptured ASDAS ID before or within 16 weeks of retreatment. Almost all (96%) placebo-treated patients who experienced a flare recaptured ASDAS LDA by week 104, with 4 out of 28 patients regaining ASDAS LDA before any retreatment at all. While the population of patients who flared in patients randomised to blinded IXE was smaller (n=13), one has to wonder if the nocebo effect was in play once they went on blinded IXE, as 92% did recapture ASDAS LDA once they were on OL IXE and 38% recaptured ASDAS LDA by week 104.
Some studies assessing the maintenance of ASDAS ID or remission following withdrawal of active treatment also assessed predictors of remission or ID. In ABILITY-3, younger age (continuous variable), male sex and positive human leukocyte antigen B27 (HLA-B27) were found to be predictors of ASDAS ID.9 In RE-EMBARK, male sex and age <40 years were significant predictors of regaining ID following a flare and subsequent 12-week retreatment with etanercept.10 In contrast, although the present analysis did not assess predictors of ASDAS ID, we report that ASDAS area under the curve was one of the characteristics associated with flare, meaning that patients with higher disease activity over time were more likely to experience a flare than those with consistently low disease activity. A 2016 systematic review noted that the time under remission before tapering of TNFi was associated with a better outcome; however, no clear predictors have yet been identified.4 This may be somewhat attributable to the lack of a clear consensus regarding the definition of a flare in patients with axSpA.
Expected or otherwise, patients sometimes pause or stop biologic medications, and clinicians and patients may have concerns about recapturing efficacy when drugs are restarted. Therefore, understanding the recapture of LDA or remission after treatment interruption may help guide treatment decisions. The present findings may be of relevance to patients who may need temporary withdrawal of therapy due to pregnancy, relevant concomitant disease or surgery, for example.
Possible limitations of this analysis include the fact that different studies use different definitions of flare and remission, which limits direct comparisons among analyses.11 The ASDAS definition of flare was not used in the present study and it is worth noting that some patients who were ASDAS=2.0 and moved to ASDAS=2.1 at two consecutive visits did not experience a flare according to the ASDAS definition. It is also important to note that the method of active treatment discontinuation in the present study is not in line with what is recommended for clinical practice (tapering of treatment).
The present analysis demonstrated that patients continuously treated with IXE were less likely to experience flare compared with patients receiving placebo (IXE withdrawal). The vast majority of patients withdrawn from IXE to placebo recaptured at least LDA and over half of those patients met the criteria for ID with IXE retreatment. These data may provide support to patients who require interruption in active therapy.
Acknowledgments
The authors thank Ann Leung MS of Syneos Health and Stephanie Strakbein MS of Eli Lilly and Company for statistical support, and Edel Hughes PhD of Eli Lilly and Company for writing and editorial support.
Footnotes
Handling editor: Josef S Smolen
Presented at: Portions of this work have been presented as an abstract/poster at the European Alliance of Associations for Rheumatology Annual Meeting 2022,12 the Rheumatology Winter Clinical Symposium Annual Meeting 2022 and the State of Texas Association of Rheumatologists Annual Meeting 2022, the 13th International Congress on Spondyoarthrides 2022, and the Florida Society of Rheumatology Annual Meeting 2022.
Contributors: Eli Lilly contributed to the study design, data collection, data analysis, data interpretation, preparation of the manuscript and the decision to submit the paper for publication. FEVdB contributed to study design. DP contributed to acquisition of data. SLL and SYP contributed to analysis of data. All authors contributed to the interpretation of data. All authors had full access to all the data in the study, reviewed the drafts and approved the final version of the manuscript. RBML is guarantor of the work.
Funding: This work was supported by Eli Lilly and Company (Indianapolis, Indiana, USA).
Competing interests: RBML reports grants or contracts from AbbVie, Galapagos, Pfizer and UCB; personal fees from AbbVie, Celgene, Eli Lilly and Company, Galapagos, Gilead, Janssen, Novartis, Pfizer and UCB; consulting fees from Rheumatology Consultancy; and is a EULAR council member. DP reports grants or contracts from AbbVie, Eli Lilly and Company, MSD, Novartis and Pfizer; personal fees from AbbVie, Biocad, Eli Lilly and Company, Gilead, GlaxoSmithKline, Janssen, MSD, Novartis, Pfizer, Samsung Bioepis and UCB; and speaking fees and/or honoraria from AbbVie, Bristol Myers Squibb, Eli Lilly and Company, MSD, Novartis, Pfizer and UCB. PR reports research grants from Janssen and Novartis; speaking fees and/or honoraria from Abbott, AbbVie, Amgen, Bristol Myers Squibb, Celgene, Eli Lilly and Company, Janssen, Novartis and Pfizer; travel support from Janssen; and participated on an advisory board for Abbott, AbbVie, Amgen, Bristol Myers Squibb, Celgene, Eli Lilly, Janssen, Novartis and Pfizer. FEVdB reports grant support from Merck and consulting fees from AbbVie, Amgen and Eli Lilly and Company. RB, SLL, JRL and SYP are employees of Eli Lilly and Company and own stock or stock options. LG reports grants or contracts from Novartis and Pfizer; personal fees from AbbVie, Galapagos, Janssen, Eli Lilly and Company, Pfizer, UCB and Galapagos; and participates in a leadership or fiduciary role in ACR, SPARTAN and ASAS.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available upon reasonable request. Lilly provides access to all individual participant data collected during the trial, after anonymisation, with the exception of pharmacokinetic or genetic data. Data are available to request 6 months after the indication studied has been approved in the USA and EU and after primary publication acceptance, whichever is later. No expiration date of data requests is currently set once data are made available. Access is provided after a proposal has been approved by an independent review committee identified for this purpose and after receipt of a signed data sharing agreement. Data and documents, including the study protocol, statistical analysis plan, clinical study report, blank or annotated case report forms, will be provided in a secure data sharing environment. For details on submitting a request, see the instructions provided at www.vivli.org.
Ethics statements
Patient consent for publication
Not required.
Ethics approval
This study involves human participants. COAST-Y was approved by the main ethics committee Schulman Associates IRB, Cincinnati, Ohio, USA (IRB # 201607390) and the study was approved by the ethical review boards at each of 127 total participating sites. Participants gave informed consent to participate in the study before taking part.
References
- 1. López-Medina C, Ramiro S, van der Heijde D, et al. Characteristics and burden of disease in patients with radiographic and non-radiographic axial spondyloarthritis: a comparison by systematic literature review and meta-analysis. RMD Open 2019;5:e001108. 10.1136/rmdopen-2019-001108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. van der Heijde D, Ramiro S, Landewé R, et al. 2016 update of the ASAS-EULAR management recommendations for axial spondyloarthritis. Ann Rheum Dis 2017;76:978–91. 10.1136/annrheumdis-2016-210770 [DOI] [PubMed] [Google Scholar]
- 3. Smolen JS, Schöls M, Braun J, et al. Treating axial spondyloarthritis and peripheral spondyloarthritis, especially psoriatic arthritis, to target: 2017 update of recommendations by an international task force. Ann Rheum Dis 2018;77:3–17. 10.1136/annrheumdis-2017-211734 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Navarro-Compán V, Plasencia-Rodríguez C, de Miguel E, et al. Anti-Tnf discontinuation and tapering strategies in patients with axial spondyloarthritis: a systematic literature review. Rheumatology 2016;55:1188–94. 10.1093/rheumatology/kew033 [DOI] [PubMed] [Google Scholar]
- 5. Landewé RB, Gensler LS, Poddubnyy D, et al. Continuing versus withdrawing ixekizumab treatment in patients with axial spondyloarthritis who achieved remission: efficacy and safety results from a placebo-controlled, randomised withdrawal study (COAST-Y). Ann Rheum Dis 2021;80:1022–30. 10.1136/annrheumdis-2020-219717 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. van der Heijde D, Cheng-Chung Wei J, Dougados M, et al. Ixekizumab, an interleukin-17A antagonist in the treatment of ankylosing spondylitis or radiographic axial spondyloarthritis in patients previously untreated with biological disease-modifying anti-rheumatic drugs (COAST-V): 16 week results of a phase 3 randomised, double-blind, active-controlled and placebo-controlled trial. Lancet 2018;392:2441–51. 10.1016/S0140-6736(18)31946-9 [DOI] [PubMed] [Google Scholar]
- 7. Deodhar A, Poddubnyy D, Pacheco-Tena C, et al. Efficacy and safety of Ixekizumab in the treatment of radiographic axial spondyloarthritis: sixteen-week results from a phase III randomized, double-blind, placebo-controlled trial in patients with prior inadequate response to or intolerance of tumor necrosis factor inhibitors. Arthritis Rheumatol 2019;71:599–611. 10.1002/art.40753 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Deodhar A, van der Heijde D, Gensler LS, et al. Ixekizumab for patients with non-radiographic axial spondyloarthritis (COAST-X): a randomised, placebo-controlled trial. Lancet 2020;395:53–64. 10.1016/S0140-6736(19)32971-X [DOI] [PubMed] [Google Scholar]
- 9. Sieper J, Landewé R, Magrey M, et al. Predictors of remission in patients with non-radiographic axial spondyloarthritis receiving open-label adalimumab in the ABILITY-3 study. RMD Open 2019;5:e000917. 10.1136/rmdopen-2019-000917 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Van den Bosch FWJ, Blanco F, Selema P. Predictors of maintaining inactive disease after etanercept withdrawal, and regaining inactive disease status after flare and retreatment, in adults with non-radiographic axial spondyloarthritis: results from RE-EMBARK. Arthritis Rheumatol 2020;72. [Google Scholar]
- 11. Lubrano E, Massimo Perrotta F, Manara M, et al. Predictors of loss of remission and disease flares in patients with axial spondyloarthritis receiving antitumor necrosis factor treatment: a retrospective study. J Rheumatol 2016;43:1541–6. 10.3899/jrheum.160363 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
ard-2022-222731supp001.pdf (519.8KB, pdf)
ard-2022-222731supp003.pdf (42.1KB, pdf)
ard-2022-222731supp002.pdf (105.1KB, pdf)
ard-2022-222731supp004.pdf (46.9KB, pdf)
ard-2022-222731supp005.pdf (22.8KB, pdf)
ard-2022-222731supp006.pdf (24.1KB, pdf)
Data Availability Statement
Data are available upon reasonable request. Lilly provides access to all individual participant data collected during the trial, after anonymisation, with the exception of pharmacokinetic or genetic data. Data are available to request 6 months after the indication studied has been approved in the USA and EU and after primary publication acceptance, whichever is later. No expiration date of data requests is currently set once data are made available. Access is provided after a proposal has been approved by an independent review committee identified for this purpose and after receipt of a signed data sharing agreement. Data and documents, including the study protocol, statistical analysis plan, clinical study report, blank or annotated case report forms, will be provided in a secure data sharing environment. For details on submitting a request, see the instructions provided at www.vivli.org.