Abstract
Objective
To examine the relationships between age, healthspan and chronic illness among former professional American-style football (ASF) players.
Methods
We compared age-specific race-standardised and body mass index-standardised prevalence ratios of arthritis, dementia/Alzheimer’s disease, hypertension and diabetes among early adult and middle-aged (range 25–59 years) male former professional ASF players (n=2864) with a comparator cohort from the National Health and Nutrition Examination Survey and National Health Interview Survey, two representative samples of the US general population. Age was stratified into 25–29, 30–39, 40–49 and 50–59 years.
Results
Arthritis and dementia/Alzheimer’s disease were more prevalent among ASF players across all study age ranges (all p<0.001). In contrast, hypertension and diabetes were more prevalent among ASF players in the youngest age stratum only (p<0.001 and p<0.01, respectively). ASF players were less likely to demonstrate intact healthspan (ie, absence of chronic disease) than the general population across all age ranges.
Conclusion
These data suggest the emergence of a maladaptive early ageing phenotype among former professional ASF players characterised by premature burden of chronic disease and reduced healthspan. Additional study is needed to investigate these findings and their impact on morbidity and mortality in former ASF players and other athlete groups.
Keywords: chronic, cardiovascular diseases, football, osteoarthritis
WHAT IS ALREADY KNOWN ON THIS TOPIC
While exposure to professional American style football (ASF) has been associated with a maladaptive multiorgan phenotype, data on the effects of ASF on healthspan and the premature occurrence of chronic illness remains understudied.
WHAT THIS STUDY ADDS
Our data suggest significantly foreshortened healthspan in former ASF players compared with the general population. This was driven by an increased prevalence of conditions typically associated with ageing including arthritis and dementia/Alzheimer’s disease across all age groups 25–59 years and hypertension and diabetes among players 25–29 years within a large cohort of early adult and middle-aged former professional ASF players.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
These results highlight the need to identify early adult and middle-aged players who may harbour cardiometabolic, orthopaedic and neurocognitive disease to consider early pharmacological and behavioural interventions to improve morbidity and mortality.
Introduction
Advancing age is a potent independent and non-modifiable risk factor for the development of many chronic diseases.1 General population studies consistently associate increases in cardiometabolic,2 neurocognitive3 and musculoskeletal pathology with increasing age.4 Although the precise mechanisms linking ageing to an increasing burden of chronic disease remain incompletely understood, biological mechanisms involving inflammation, proteostasis, macromolecular damage, dysregulated cellular metabolism and epigenetic influence have been proposed.5 While these mechanistic underpinnings of chronic disease are common consequences of ageing, early life environmental factors may dictate their magnitude and age of onset. To date, the degree to which specific early life exposures accelerate ageing, precipitate the premature onset of chronic disease, and thereby reduce healthspan (defined as the duration of life without chronic disease)6 remains incompletely understood.
Participation in American-style football (ASF) has been associated with the emergence of a multiorgan, maladaptive phenotype early in life. Specifically, ASF participation has been linked to the development of hypertension,7 pathological cardiac remodelling,8 vascular stiffening,9 and obesity.10 11 Studies establishing adverse cardiovascular relationships have focused almost exclusively on youthful men during their years of active ASF participation. Cognitive impairment also has been identified during active play12 13 and in postcareer years.14 15 In addition, high physical demands and associated traumatic joint injuries in ASF contribute to elevated rates of early total knee and hip arthroplasty in former ASF players compared with the general population.16 Accordingly, the impact of ASF participation on later life healthspan remains incompletely characterised and data comparing chronic disease burden among former ASF participants to people with no prior ASF exposure are lacking.
We hypothesised that ASF participation represents a risk factor for early ageing as reflected by the presence of premature chronic disease and reduced healthspan. Specifically, we hypothesised that former ASF participants would harbour a higher prevalence of common age-related chronic diseases compared with similarly aged men without ASF exposure. To address this hypothesis, we compared race-adjusted and body mass index (BMI)-adjusted disease prevalence estimates of self-reported arthritis, dementia/Alzheimer’s disease, hypertension and diabetes mellitus in a large cohort of former professional ASF participants to those derived from two independent, well-validated general community reference populations.
Methods
ASF sample
Former players who received compensation from the National Football League (NFL) after 1960 (the year hard plastic helmets were formally adopted17) were considered eligible for the Football Players Health Study (FPHS) at Harvard University.18 Home and email addresses were obtained from the NFL Players Association. A total of 15 070 former players received invitations to participate in either a hard copy or online questionnaire, out of which 4174 (27.7%) enrolled. A former player advisory board that represents the distribution of age, race and geographical region of professional ASF players offered feedback on the conceptual framework of chronic disease burden and healthspan.
General population samples
We used two surveys to capture general population distributions of four age-associated chronic illnesses. The first was the National Health and Nutrition Examination Survey (NHANES),19 a multiyear, stratified, clustered, four-stage sample that releases data in 2-year cycles. NHANES uses a probability-based sampling design that oversamples low-income individuals, non-Hispanic black and Mexican Americans, adults over age 60 and adolescents. We used NHANES demographic and health survey data from 2015 to 2016 and 2017 to 2018. We also accessed the 2019 National Health Interview Survey (NHIS),20 which collects demographic, socioeconomic, healthcare and mental and physical health data via interview. NHIS uses a multistage stratified and geographically clustered sampling strategy to ensure that NHIS is nationally representative of the most recent decennial census.
Measures
Age was determined using date of birth for football participants, and survey age for general population participants. We restricted datasets to men between the ages of 25–59. The minimum age was chosen to match the youngest FPHS participant to ensure full capture of pathology related to ASF exposure. A maximal age of 59 was selected to reflect the end of ‘middle-age’,21 22 and to minimise the powerful impact of older age on disease prevalence. Age was stratified into 25–29, 30–39, 40–49 and 50–59 years. ASF players responded to survey questions that queried professional playing career length. Position was divided into linemen (defensive line, linebacker and offensive line) and non-linemen (defensive back, kicker/punter, quarterback, running back, tight end, wide receiver and special teams only). Race for former football players was assigned as previously described,23 whereby players chose the category that best described their race/ethnicity and were further classified into black, white or other. Due to the low representation of non-black and non-white football players in the NFL (and consequently FPHS), we restricted datasets to black and white individuals, excluding Asian, Native Hawaiian/Pacific Islander, Latino, American Indian/Alaskan Native, other or ‘declined to answer’ participants. BMI was calculated using the self-reported weight and height for ASF players and NHIS participants.24 For NHANES, height and weight were collected during the clinical assessment. BMI was categorised into <25.0, 25.0–30.0 and >30.0.
We used self-reported data on four chronic diseases, including arthritis, hypertension/high blood pressure and diabetes mellitus from FPHS, NHANES and NHIS, and dementia/Alzheimer’s disease captured in FPHS and NHIS. Disease status phrasing across the cohorts is summarised as follows. For dementia/Alzheimer’s disease, both FPHS and NHIS identically asked ‘Has a healthcare provider ever told you that you have had dementia (Alzheimer’s disease)’, thus combining dementia and Alzheimer’s Disease into a single outcome. The arthritis question in FPHS, NHANES and NHIS were all phrased as ‘Has a healthcare provider ever told you that you have had arthritis?’
For high blood pressure/hypertension in NHANES, we used: (1) ‘Because of your high blood pressure/hypertension, have you ever been told to take prescribed medicine?’ and (2) ‘Are you now taking prescribed medicine?’. For NHIS, high blood pressure/hypertension was queried as: (1) ‘Have you ever been told by a doctor or other health professional that you had hypertension, also called high blood pressure?’ and (2) ‘Are you NOW taking any medication prescribed by a doctor for your high blood pressure?’. For diabetes mellitus, NHANES asked the following: (1) ‘Have you ever been told by a doctor or health professional that you have diabetes or sugar diabetes?’, (2) ‘Are you now taking diabetic pills to lower your blood sugar?’ and (3) ‘Are you using injectable insulin to lower your blood sugar?’ NHIS phrased questions on diabetes mellitus status as: (1) ‘Has a doctor or other health professional EVER told you that you had diabetes?’; (2) ‘Are you NOW taking diabetic pills to lower your blood sugar?’ and (3) ‘Insulin can be taken by shot or pump. Are you NOW taking insulin?’. FPHS participants were asked ‘Has a medical provider ever recommended or prescribed medication for [condition]’ and ‘Are you currently taking medication [for that condition]?’ We used their responses to the conditions ‘high blood pressure’ and ‘diabetes or high blood sugar.’ For both diabetes/high blood sugar and high blood pressure/hypertension, participants who answered affirmatively to any disease-specific question were assigned that diagnosis.
NHIS was used to compare race-adjusted and BMI-adjusted dementia/Alzheimer’s disease prevalence between FPHS and the general population, since this was not asked in NHANES. For the other three individual conditions we compared with NHANES because the question phrasing to define the outcome in NHIS was somewhat different from FPHS. We used the NHIS dataset to study race-adjusted and BMI-adjusted healthspan (defined as the duration of lifespan free from chronic disease), because it contained data on all conditions. To assess the effect of the different wording between NHIS and NHANES to define hypertension and diabetes, we compared race-adjusted and BMI-adjusted prevalence estimates in NHANES and NHIS in the subset used for our analyses.
Statistical analysis
We calculated age-specific, race-specific and BMI-specific prevalence rates for outcomes in NHANES, NHIS and FPHS. Raw NHIS and FPHS data were scaled to match the general population distribution captured by applying NHANES study-specified weights (combining two NHANES cycles according to NHANES procedures25) that reflect the general US male population between the ages of 25–59. Each age-specific, race-specific and BMI-specific prevalence was adjusted to the age, race and BMI distribution of the weighted NHANES population by scaling the age-specific prevalence rates to the distribution of race (black or white) and BMI (<25.0, 25.0–30.0 and >30.0 kg/m2) in NHANES. Significance was calculated using z-statistics for observed to expected ratios.26 To prevent overinflation of degree of observed significance that would occur if p values were based on a pseudopopulation that was larger than the original, we treated the NHANES-scaled general population estimates as the source of observed outcomes. Analyses were conducted using R Statistical Software27 and statistical significance was set at 0.0063 (p<0.05 divided by 8) to account for multiple comparisons.28
Results
At the time of entry, 2864 out of 4174 (68.6%) FPHS participants met inclusion criteria of being between the ages of 25 and 59. This former ASF player study population was 44±10 years of age, similar to both NHANES (42±10 years) and NHIS (43±10 years, table 1). In our study populations, 48.1% of FPHS participants were black, compared with 40.1% in NHANES and 13.5% in NHIS. BMI among the former ASF players (32±5 kg/m2) was higher than among both the NHANES (30±7) and NHIS (28±5) participants. The ASF players reported 6±4 years in the NFL with a majority (66%) playing a non-lineman position. In comparisons of the prevalence of the conditions by age in NHANES and NHIS, we found no statistical differences between prevalence by age group (online supplemental table 1), although the difference in hypertension among 40–49 years old was 6% higher in NHIS, which approached significance (p=0.06). The second largest difference in prevalence in any category between NHANES and NHIS was for diabetes among 50–59 years old that was 2.6% lower in NHIS.
Table 1.
Characteristics of the Football Players Health Study (FPHS), National Health and Nutrition Examination Survey (NHANES) and National Health Interview Survey (NHIS) cohorts
| FPHS | NHANES | NHIS | |
| 2015–2019 | 2015–2018 | 2019 | |
| N=2684 | N=1481 | N=6298 | |
| Age mean (SD (SD)) | 43.9 (9.6) | 42.3 (10.4) | 43.1 (10.2) |
| Age N (%) | |||
| 25–29* | 177 (6.6) | 209 (14.1) | 770 (12.2) |
| 30–39 | 834 (31.1) | 413 (27.9) | 1723 (27.4) |
| 40–49 | 712 (26.5) | 414 (28.0) | 1714 (27.2) |
| 50–59 | 961 (35.8) | 445 (30.0) | 2091 (33.2) |
| Race N (%) | |||
| Black | 1291 (48.1) | 617 (40.1) | 851 (13.5) |
| White | 1393 (51.9) | 920 (59.9) | 5447 (86.5) |
| Body mass index (BMI)† Mean (SD) | 31.69 (5.12) | 30.0 (7.1) | 28.4 (4.8) |
| BMI N (%) | |||
| 25–29 | 30.25 (4.37) | 27.9 (6.9) | 27.2 (5.0) |
| 30–39 | 31.43 (5.05) | 30.37 (8.0) | 27.7 (4.7) |
| 40–49 | 32.21 (5.33) | 30.99 (6.6) | 28.9 (4.7) |
| 50–59 | 31.84 (5.27) | 29.68 (6.3) | 28.9 (4.8) |
| Lineman status N (%) | |||
| Non-lineman | 1763 (65.69) | – | – |
| Lineman | 921 (34.31) | – | – |
| Years of play mean (SD) | 6.39 (3.9) | – | – |
| Healthspan status N (%)‡ | |||
| Diminished | 1458 (56.3) | – | 2308 (36.7) |
| Intact | 1132 (43.7) | – | 3982 (63.3) |
| Missing | 94 (3.5) | 8 (0.1) | |
| Dementia/Alzheimer’s disease N (%)‡ | |||
| No | 2628 (97.9) | – | 6280 (99.7) |
| Yes | 56 (2.1) | – | 10 (0.2) |
| Missing | – | – | 8 (0.1) |
| Arthritis N (%) | |||
| No | 1538 (57.3) | 1237 (80.5) | 5375 (85.3) |
| Yes | 1146 (42.7) | 298 (19.4) | 923 (14.7) |
| Missing | – | 2 (0.1) | – |
| Diabetes N (%) | |||
| No | 2477 (92.3) | 1363 (88.7) | 5853 (92.9) |
| Yes | 170 (6.3) | 122 (7.9) | 445 (7.1) |
| Missing | 37 (1.4) | 52 (3.4) | – |
| Hypertension N (%) | |||
| No | 1915 (71.3) | 1119 (72.8) | 4571 (72.6) |
| Yes | 747 (27.8) | 415 (27.0) | 1727 (27.4) |
| Missing | 22 (0.8) | 3 (0.2) | – |
*One FPHS participant was 24 years old.
†94 FPHS participants are missing BMI.
‡Healthspan and dementia/Alzheimer’s disease status could only be calculated for NHIS and not NHANES as NHANES does not include dementia/Alzheimer’s disease survey data that are comparable to FPHS.
bjsports-2022-106021supp001.pdf (43.5KB, pdf)
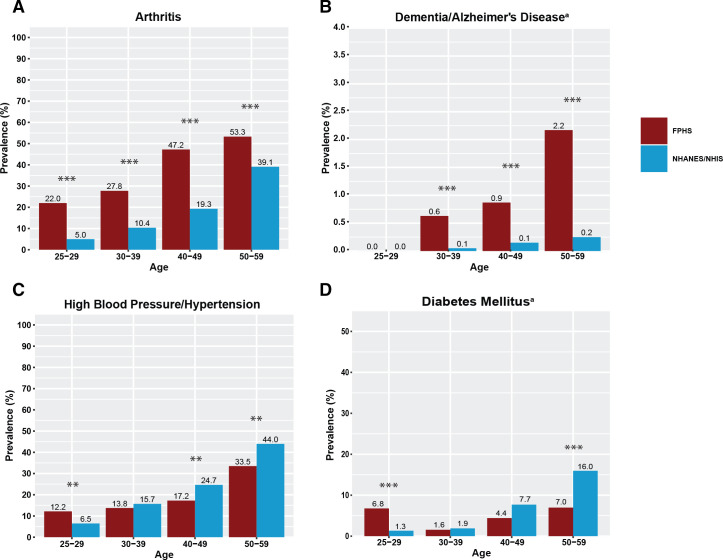
The overall unadjusted prevalence of freedom from chronic disease and disease-specific unadjusted prevalence estimates for arthritis, dementia/Alzheimer’s disease, hypertension and diabetes mellitus for each cohort are shown in table 1. Age-stratified prevalence estimates of each race-adjusted and BMI-adjusted chronic condition are shown in figure 1 and standardised prevalence ratios are listed in online supplemental table 2. Arthritis (figure 1A) and dementia/Alzheimer’s disease (figure 1B) were directly related to age and were more prevalent among former ASF athletes than among the general population across all age groups, except in the 25–29 age group among whom neither cohort reported dementia/Alzheimer's disease cases. Hypertension and diabetes mellitus followed a different trajectory. For hypertension, there was a statistically significant twofold higher prevalence among ASF athletes in the youngest age group (25–29 years) compared with the general population, but in older groups the prevalence was higher in the general population (figure 1C). In similar fashion, the prevalence of diabetes mellitus among former ASF players was significantly higher compared with the general population among the youngest age group, after which prevalence estimates were similar until the highest age group (50–59 years) where the prevalence in the general population was significantly higher than in former ASF players (figure 1D).
Figure 1.
Race-adjusted and BMI-adjusted prevalence estimates for each chronic condition in former professional American-style football players versus the general population. (A) Arthritis (Football Players Health Study (FPHS) and National Health and Nutrition Examination Survey (NHANES)); (B) Dementia/Alzheimer’s disease (FPHS and National Health Interview Survey (NHIS)); (C) Hypertension/High Blood Pressure (FPHS and NHANES and (D) Diabetes Mellitus (FPHS and NHANES). Signficance values have been adjusted using the Bonferonni correction for multiple comparisons. **p<0.0013; ***p<0.00013 after multiple comparisons correction. aAxes for B, C have been expanded for visibility. BMI, body mass index.
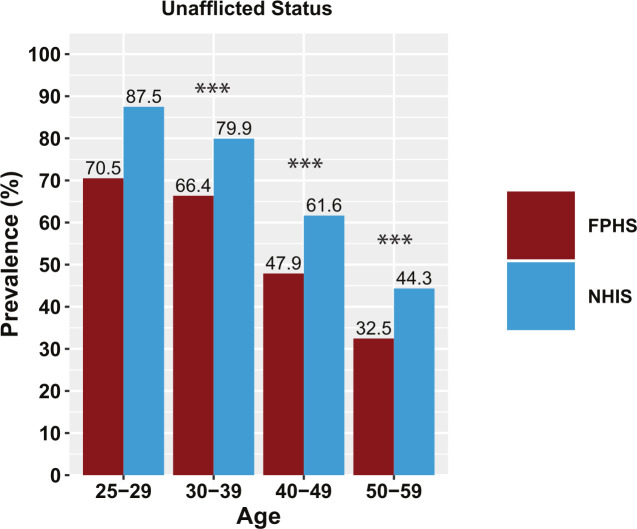
Freedom from the four chronic diseases of interest—that is, intact healthspan adjusted for race and BMI—is shown in figure 2 and online supplemental table 2. As anticipated, intact healthspan declined with increasing age among former ASF players and the general population. However, the prevalence of intact healthspan was significantly lower among former ASF players of all ages compared with the general population except the youngest age group. The decline in prevalent intact healthspan appeared to be shifted roughly a decade earlier among former ASF players. Specifically, the 66% intact healthspan prevalence among former ASF players in the 30–39 years age group was similar to 40–49 years old men in the general population (62%). Similarly, the 48% prevalence of intact healthspan of former ASF players in their 40s mirrored that among men from the general population who were a decade older (44% among NHIS participants aged 50–59). Among football players only, linemen showed significantly diminished healthspan compared with non-linemen in all but the 50–59 age group (figure 3).
Figure 2.
Race-adjusted and BMI-adjusted prevalence estimates for intact healthspan status for the Football Players Health Study (FPHS) and National Health Interview Survey (NHIS). Signficance values have been adjusted using the Bonferonni correction for multiple comparisons. ***p<0.00013 after multiple comparisons correction. BMI, body mass index.
Figure 3.
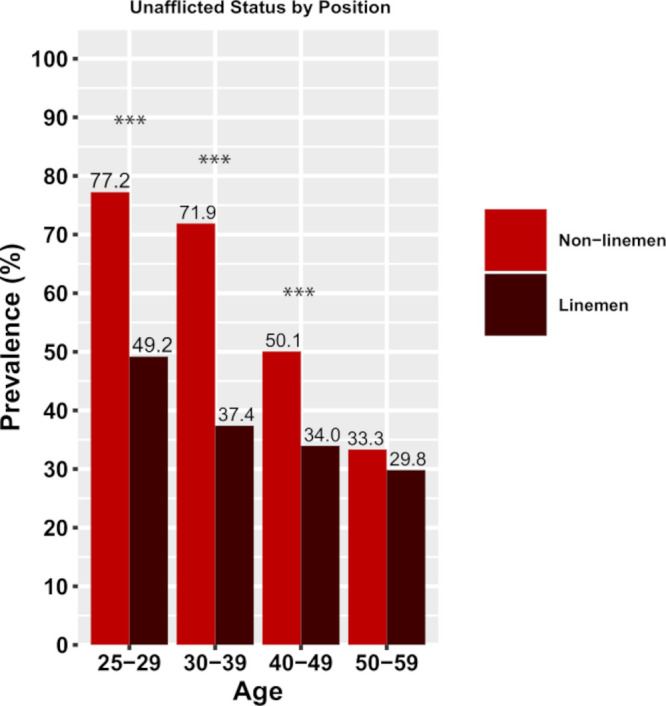
Race-adjusted and BMI-adjusted prevalence estimates for intact healthspan status among Football Player Health Study participants stratified by lineman position status. Signficance values have been adjusted using the Bonferonni correction for multiple comparisons. ***p<0.00013 after multiple comparisons correction. BMI, body mass index.
Discussion
This study compared chronic disease burden among former professional ASF players ages 25–59 with aged-matched estimates from the general population. As anticipated, we observed increasing race-adjusted and BMI-adjusted prevalence estimates of arthritis, dementia/Alzheimer’s disease, hypertension and diabetes mellitus with increasing age among both groups. However, comparative relationships between age and disease prevalence between the two groups differed by condition type. Arthritis and dementia/Alzheimer’s disease, chronic diseases associated with morbidity (ie, reduced quality of life), were consistently higher among former ASF players than the general population across the entire age span studied. In contrast, former ASF players harboured more hypertension and diabetes mellitus, cardiometabolic conditions closely linked to mortality (ie, duration of life) in the youngest age strata but had lower prevalence than the general population at older ages. Taken together, the prevalence of men with no chronic disease (ie, intact healthspan) was significantly lower among former ASF players, particularly among men that played at a lineman field position, compared with men of the same age without professional football exposure across the 35 year age span studied. This finding suggests that professional ASF participation should be considered a risk factor for reduced healthspan with contributions from the premature emergence of diseases that may impact both the quality and duration of life.
Advancing chronological age is a universal and non-modifiable risk factor for the development of many chronic diseases. Accordingly, we selected a relatively youthful cohort of former professional ASF players to maximise the impact of ASF exposure on chronic disease prevalence while minimising the impact of older age. Findings indicate that hypertension and diabetes mellitus are present at higher rates than expected in relatively young men during the immediate years after ASF career termination. Consistent with prior literature,25–27 this suggests an association between ASF participation and cardiometabolic disease which is the most common cause of death among former professional ASF players.28 This observation is clinically significant, as hypertension and diabetes mellitus increase mortality when manifested during early years independent of later life disease.29–32 Accordingly, our data suggest an important role for focused efforts to identify young former ASF players who harbour cardiometabolic disease with the goal of ensuring guideline-directed lifestyle and pharmaceutical intervention.33
Our finding that arthritis and dementia/Alzheimer’s disease, diseases that adversely impact quality of life, occur earlier among former ASF athletes than the general population is similarly important. Specifically, former ASF players appear to be at increased risk for premature cessation of healthspan compared with men without professional ASF exposure even if they have been shown to live as long or longer than the general population.28 34 Thus, former ASF players may spend higher percentages of their lifespans living with clinically relevant infirmities that have adverse impacts on daily function, healthcare utilisation and quality of life. This important finding raises the imperative to identify potential health consequences of professional ASF participation, to understand the pathophysiological underpinnings of these diseases, and to initiate both primary preventive and secondary therapeutic opportunities for intervention. While future confirmatory work is required, this paradigm may be applicable to former elite athletes from other collision and contacts sports (eg, rugby, ice hockey and European-style football/soccer) that predispose participants to orthopaedic injury and head trauma.
While this study was not designed to identify mechanisms underlying the premature emergence of chronic disease among former ASF players, several speculative comments are warranted. Potential ‘on the field’ risk factors including repetitive head impact and traumatic musculoskeletal injury may predispose players to subsequent neurocognitive impairment and arthritis, respectively. In addition, there are ‘off the field’ elements of professional ASF participation including deliberate weight gain,35–37 performance-enhancing supplement and non-steroidal anti-inflammatory use,38 39 and exposure to high intensity strength training that may contribute to an increased susceptibility to early life pathology.40 Race, while largely a social construct, has been shown to be a covariate associated with the cardiovascular response to ASF and may serve as an independent risk factor for aging.41 The extent to which ‘weathering’ stress, allostatic load and structural racism impact biological age of minority athletes merits special investigation.42 Determination of the causality and relative magnitudes of these risk factors coupled with a delineation of the underlying cellular and organ-specific pathophysiology represent important areas of future work.
We acknowledge several limitations. First, outcome data are based exclusively on self-report without medical record or clinician confirmation, which could introduce response bias via inaccurate reporting across all cohorts. However, we deliberately applied consistently conservative trait definitions which would result in a balanced underestimation of disease prevalence across player and general cohorts. Second, the FPHS chronic condition survey deliberately used identical terminology related to chronic illness (eg, ‘arthritis’ instead of osteoarthritis or rheumatoid arthritis; ‘diabetes or high blood sugar’ instead of type I or type II diabetes mellitus) as that employed in the general population cohorts to facilitate meaningful comparisons. Accordingly, we were unable to explore potentially important subtypes of pathology. Third, we acknowledge the possibility of selection bias within the ASF cohort and cannot exclude the possibility that ASF players harbouring more illness may have been more likely to enroll. However, prior work has shown that people with severe illness are less likely to join health studies,43 44 and we did not find universally increased chronic disease prevalence across all age strata but rather patterns that varied by condition. Fourth, we cannot exclude the possibility that the observed relative reduction of cardiometabolic disease among ageing former ASF players was in part driven by attrition due to earlier mortality among those most affected. Finally, we acknowledge that BMI represents an imperfect measure of body habitus and may have led to overestimates of obesity in the former professional football cohort.45 However, given that more accurate body composition variables were not available, BMI offered the best opportunity to account for the influence of body habitus differences despite the potential to introduce bias into BMI-adjusted estimates.
In conclusion, findings suggest that participation in professional ASF is associated with the premature onset of key chronic diseases that may increase both morbidity and risk for mortality. Further, the approximate 10-year reduction in intact healthspan in former ASF players suggests that professional ASF participation may represent a previously unidentified risk factor for early ageing. While our data suggest a link between ASF participation and a maladaptive early ageing phenotype, future work examining established biochemical, cellular and physiological signatures of ageing in this population is warranted.
Acknowledgments
The authors wish to acknowledge the study participants, advisors, and staff of the Football Players Health Study for their time and effort.
Footnotes
Twitter: @AdamTenfordeMD, @meaganwasfy
Correction notice: This article has been corrected since it published Online First. A typographical error in the figure 1 legend has been corrected.
Contributors: RG, TVS-P, ID, DM, JB, DK, DM, MMW, HAT, FES, AJW, JSG, RZ and AB contributed to the conception and design of the study; RG, TVS-P, JB, HL, MMW, FES, JSG and AB contributed to the acquisition and analysis of data; RG, TVS-P, MMW, FES, MMW, HAT, HL, JB, DM, AJW, HT, RZ and AB contributed to the drafting of text, tables and figures. RG acts as the guarantor of the study.
Funding: The Football Players Health Study is supported by the NFL Players Association. The NFL Players Association did not contribute to the design and conduct of the study; collection, management, analysis and interpretation of the data; preparation, review or approval of the manuscript; and decision to submit the manuscript for publication. This work received support from Harvard Catalyst | The Harvard Clinical and Translational Science Center (National Center for Advancing Translational Sciences, National Institutes of Health Award UL1 TR002541) and financial contributions from Harvard University and its affiliated academic healthcare centers.
Disclaimer: The content is solely the responsibility of the authors and does not necessarily represent the official views of Harvard Catalyst, Harvard University and its affiliated academic healthcare centres, or the National Institutes of Health.
Competing interests: The Football Players Health Study is supported by the NFL Players Association. The NFL Players Association did not contribute to the design and conduct of the study; collection, management, analysis and interpretation of the data; preparation, review or approval of the manuscript; and decision to submit the manuscript for publication. This work received support from Harvard Catalyst | The Harvard Clinical and Translational Science Center (National Center for Advancing Translational Sciences, National Institutes of Health Award UL1 TR002541) and financial contributions from Harvard University and its affiliated academic healthcare centers. The content is solely the responsibility of the authors and does not necessarily represent the official views of Harvard Catalyst, Harvard University and its affiliated academic healthcare centers, or the National Institutes of Health. The authors wish to acknowledge the study participants, advisors and staff of the Football Players Health Study for their time and effort.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
No data are available.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study involves human participants and was approved by Harvard T. H. Chan School of Public Health: # IRB18-1365; Beth Israel Deaconess Medical Center: IRB # 2014-P-000308; and Harvard Medical School: # IRB14-2691. Participants gave informed consent to participate in the study before taking part.
References
- 1. Kuan V, Fraser HC, Hingorani M, et al. Data-Driven identification of ageing-related diseases from electronic health records. Sci Rep 2021;11:2938. 10.1038/s41598-021-82459-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Lloyd-Jones DM, Leip EP, Larson MG, et al. Prediction of lifetime risk for cardiovascular disease by risk factor burden at 50 years of age. Circulation 2006;113:791–8. 10.1161/CIRCULATIONAHA.105.548206 [DOI] [PubMed] [Google Scholar]
- 3. van der Flier WM, Scheltens P. Epidemiology and risk factors of dementia. J Neurol Neurosurg Psychiatry 2005;76 Suppl 5:v2–7. 10.1136/jnnp.2005.082867 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Lawrence RC, Felson DT, Helmick CG, et al. Estimates of the prevalence of arthritis and other rheumatic conditions in the United States. Part II. Arthritis Rheum 2008;58:26–35. 10.1002/art.23176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Kennedy BK, Berger SL, Brunet A, et al. Geroscience: linking aging to chronic disease. Cell 2014;159:709–13. 10.1016/j.cell.2014.10.039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Dzau VJ, Finkelman EM, Balatbat CA, et al. Achieving healthy human longevity: a global grand challenge. Sci Transl Med 2020;12. 10.1126/scitranslmed.abd3816. [Epub ahead of print: 21 Oct 2020]. [DOI] [PubMed] [Google Scholar]
- 7. Weiner RB, Wang F, Isaacs SK, et al. Blood pressure and left ventricular hypertrophy during American-style football participation. Circulation 2013;128:524–31. 10.1161/CIRCULATIONAHA.113.003522 [DOI] [PubMed] [Google Scholar]
- 8. Lin J, Wang F, Weiner RB, et al. Blood pressure and LV remodeling among American-Style football players. JACC Cardiovasc Imaging 2016;9:1367–76. 10.1016/j.jcmg.2016.07.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Kim JH, Sher S, Wang F, et al. Impact of American-style football participation on vascular function. Am J Cardiol 2015;115:262–7. 10.1016/j.amjcard.2014.10.033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Churchill TW, Krishnan S, Weisskopf M, et al. Weight gain and health affliction among former national football League players. Am J Med 2018;131:1491–8. 10.1016/j.amjmed.2018.07.042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Kim JH, Hollowed C, Liu C, et al. Weight gain, hypertension, and the emergence of a maladaptive cardiovascular phenotype among US football players. JAMA Cardiol 2019;4:1221–9. 10.1001/jamacardio.2019.3909 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Pryor J, Larson A, DeBeliso M. The prevalence of depression and concussions in a sample of active North American Semi-Professional and professional football players. J Lifestyle Med 2016;6:7–15. 10.15280/jlm.2016.6.1.7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Talavage TM, Nauman EA, Breedlove EL, et al. Functionally-detected cognitive impairment in high school football players without clinically-diagnosed concussion. J Neurotrauma 2014;31:327–38. 10.1089/neu.2010.1512 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Roberts AL, Pascual-Leone A, Speizer FE, et al. Exposure to American football and neuropsychiatric health in former national football League players: findings from the football players health study. Am J Sports Med 2019;47:2871–80. 10.1177/0363546519868989 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Guskiewicz KM, Marshall SW, Bailes J, et al. Association between recurrent concussion and late-life cognitive impairment in retired professional football players. Neurosurgery 2005;57:719–26. 10.1227/01.NEU.0000175725.75780.DD [DOI] [PubMed] [Google Scholar]
- 16. Tenforde AS, Cortez B, Baker J, et al. Prevalence of total hip and knee arthroplasty in former national football League players: comparison with the general US population and other populations of professional athletes. BMJ Open Sport Exerc Med 2020;6:e000833. 10.1136/bmjsem-2020-000833 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Harrison EA. The first concussion crisis: head injury and evidence in early American football. Am J Public Health 2014;104:822–33. 10.2105/AJPH.2013.301840 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Zafonte R, Pascual-Leone A, Baggish A, et al. The football players' health study at Harvard University: design and objectives. Am J Ind Med 2019;62:643–54. 10.1002/ajim.22991 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Chen T-C, Clark J, Riddles MK, et al. National health and nutrition examination survey, 2015-2018: sample design and estimation procedures. Vital Health Stat 2 2020;2:1–35. [PubMed] [Google Scholar]
- 20. Blewett LA, Dahlen HM, Spencer D, et al. Changes to the design of the National health interview survey to support enhanced monitoring of health reform impacts at the state level. Am J Public Health 2016;106:1961–6. 10.2105/AJPH.2016.303430 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Brim OG, Ryff CD, Kessler RC, eds. How Healthy Are We? A National Study of Well-Being at Midlife. Chicago: The University of Chicago Press, 2004. [Google Scholar]
- 22. Radler BT. The midlife in the United States (MIDUS) series: a national longitudinal study of health and well-being. Open Health Data 2014;2. 10.5334/ohd.ai [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Grashow R, Weisskopf MG, Baggish A, et al. Premortem chronic traumatic encephalopathy diagnoses in professional football. Ann Neurol 2020;88:106–12. 10.1002/ana.25747 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Mosteller RD. Simplified calculation of body-surface area. N Engl J Med 1987;317:1098. 10.1056/NEJM198710223171717 [DOI] [PubMed] [Google Scholar]
- 25. Tucker AM, Vogel RA, Lincoln AE, et al. Prevalence of cardiovascular disease risk factors among national football League players. JAMA 2009;301:2111–9. 10.1001/jama.2009.716 [DOI] [PubMed] [Google Scholar]
- 26. Selden MA, Helzberg JH, Waeckerle JF, et al. Cardiometabolic abnormalities in current National football League players. Am J Cardiol 2009;103:969–71. 10.1016/j.amjcard.2008.12.046 [DOI] [PubMed] [Google Scholar]
- 27. Borchers JR, Clem KL, Habash DL, et al. Metabolic syndrome and insulin resistance in division 1 collegiate football players. Med Sci Sports Exerc 2009;41:2105–10. 10.1249/MSS.0b013e3181abdfec [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Nguyen VT, Zafonte RD, Chen JT, et al. Mortality among professional American-style football players and professional American baseball players. JAMA Netw Open 2019;2:e194223. 10.1001/jamanetworkopen.2019.4223 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Gray L, Lee I-M, Sesso HD, et al. Blood pressure in early adulthood, hypertension in middle age, and future cardiovascular disease mortality: HAHS (Harvard alumni health study). J Am Coll Cardiol 2011;58:2396–403. 10.1016/j.jacc.2011.07.045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. McCarron P, Okasha M, McEwen J, et al. Blood pressure in early life and cardiovascular disease mortality. Arch Intern Med 2002;162:610–1. 10.1001/archinte.162.5.610 [DOI] [PubMed] [Google Scholar]
- 31. Dean H, Flett B. Natural history of type 2 diabetes diagnosed in childhood: long term follow-up in young adult years. Diabetes 2002;51:A24–5. [Google Scholar]
- 32. Eppens MC, Craig ME, Cusumano J, et al. Prevalence of diabetes complications in adolescents with type 2 compared with type 1 diabetes. Diabetes Care 2006;29:1300–6. 10.2337/dc05-2470 [DOI] [PubMed] [Google Scholar]
- 33. Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American heart association Task force on clinical practice guidelines. Hypertension 2018;71:e13–115. 10.1161/HYP.0000000000000065 [DOI] [PubMed] [Google Scholar]
- 34. Grashow RG, Roberts AL, Zafonte R, et al. Defining exposures in professional football: professional American-Style football players as an occupational cohort. Orthop J Sports Med 2019;7:232596711982921. 10.1177/2325967119829212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Kaiser GE, Womack JW, Green JS, et al. Morphological profiles for first-year national collegiate athletic association division I football players. J Strength Cond Res 2008;22:243–9. 10.1519/JSC.0b013e31815f5d97 [DOI] [PubMed] [Google Scholar]
- 36. Laurson KR, Eisenmann JC. Prevalence of overweight among high school football linemen. JAMA 2007;297:359–64. 10.1001/jama.297.4.363 [DOI] [PubMed] [Google Scholar]
- 37. Jonnalagadda SS, Rosenbloom CA, Skinner R. Dietary practices, attitudes, and physiological status of collegiate freshman football players. J Strength Cond Res 2001;15:507–13. [PubMed] [Google Scholar]
- 38. Tso J, Hollowed C, Liu C, et al. Nonsteroidal anti-inflammatory drugs and cardiovascular risk in American football. Med Sci Sports Exerc 2020;52:2522–8. 10.1249/MSS.0000000000002404 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Holmes N, Cronholm PF, Duffy AJ, et al. Nonsteroidal anti-inflammatory drug use in collegiate football players. Clin J Sport Med 2013;23:283–6. 10.1097/JSM.0b013e318286d0fa [DOI] [PubMed] [Google Scholar]
- 40. Baggish AL, Wang F, Weiner RB, et al. Training-specific changes in cardiac structure and function: a prospective and longitudinal assessment of competitive athletes. J Appl Physiol 2008;104:1121–8. 10.1152/japplphysiol.01170.2007 [DOI] [PubMed] [Google Scholar]
- 41. Forrester S, Jacobs D, Zmora R, et al. Racial differences in weathering and its associations with psychosocial stress: the cardia study. SSM Popul Health 2019;7:100319–3. 10.1016/j.ssmph.2018.11.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Geronimus AT, Hicken M, Keene D, et al. "Weathering" and age patterns of allostatic load scores among blacks and whites in the United States. Am J Public Health 2006;96:826–33. 10.2105/AJPH.2004.060749 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Weuve J, Tchetgen Tchetgen EJ, Glymour MM, et al. Accounting for bias due to selective attrition: the example of smoking and cognitive decline. Epidemiology 2012;23:119–28. 10.1097/EDE.0b013e318230e861 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Chatfield MD, Brayne CE, Matthews FE. A systematic literature review of attrition between waves in longitudinal studies in the elderly shows a consistent pattern of dropout between differing studies. J Clin Epidemiol 2005;58:13–19. 10.1016/j.jclinepi.2004.05.006 [DOI] [PubMed] [Google Scholar]
- 45. Provencher MT, Chahla J, Sanchez G, et al. Body mass index versus body fat percentage in prospective national football League athletes: overestimation of obesity rate in athletes at the National football League Scouting combine. J Strength Cond Res 2018;32:1013–9. 10.1519/JSC.0000000000002449 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bjsports-2022-106021supp001.pdf (43.5KB, pdf)
Data Availability Statement
No data are available.