Abstract
Objective
Polypharmacy management of recurrent pericarditis (RP) often involves long-term therapies, often with negative effects. Slow tapering of oral therapies is often required to avoid recurrence. A post hoc analysis of the phase III trial Rilonacept inHibition of interleukin-1 Alpha and beta for recurrent Pericarditis: a pivotal Symptomatology and Outcomes Study (RHAPSODY) evaluated investigator approaches to transitioning to IL-1 blockade monotherapy with rilonacept, which was hypothesised to allow accelerated withdrawal of common multidrug pericarditis regimens.
Methods
RHAPSODY was a multicentre (Australia, Israel, Italy, USA), double-blind, placebo-controlled, randomised-withdrawal trial in adults and adolescents with RP. Investigators initiated rilonacept at the labelled dose level and discontinued oral pericarditis therapies during the 12-week run-in; randomised patients received study drug as monotherapy. Time to rilonacept monotherapy was quantified in patients receiving multidrug regimens at baseline who achieved rilonacept monotherapy during run-in.
Results
In 86 enrolled patients, mean time to rilonacept monotherapy was 7.9 weeks, with no recurrences. Of these, 64% (n=55) entered on multidrug regimens: non-steroidal anti-inflammatory drugs (NSAIDs) plus colchicine (44% (24/55)), colchicine plus glucocorticoids (24% (13/55)), or NSAIDs, colchicine, plus glucocorticoids (33% (18/55)). Investigators transitioned patients receiving colchicine and glucocorticoids at baseline to rilonacept monotherapy without recurrence regardless of taper approach: sequential (n=14; median, 7.7 weeks) or concurrent (n=17; median, 8.0 weeks). Median time to rilonacept monotherapy was similar regardless of glucocorticoid dose and duration: ≤15 mg/day (n=21): 7.3 weeks; >15 mg/day (n=18): 8.0 weeks; long-term (≥28 days): 7.6 weeks.
Conclusions
Rapid discontinuation of oral RP therapies while transitioning to rilonacept monotherapy was feasible without triggering pericarditis recurrence.
Trial registration number
Keywords: pericarditis
WHAT IS ALREADY KNOWN ON THIS TOPIC
Management of recurrent pericarditis (RP) involves polypharmacy, including long-term glucocorticoid treatment, which is associated with adverse effects. Rapid tapering of glucocorticoids has been associated with increased risk of pericarditis recurrence, and so clinicians often slowly taper oral pericarditis therapies. The phase III trial Rilonacept inHibition of interleukin-1 Alpha and beta for recurrent Pericarditis: a pivotal Symptomatology and Outcomes study (RHAPSODY) demonstrated the efficacy and safety of rilonacept, an IL-1α and IL-1β cytokine trap, for RP.
WHAT THIS STUDY ADDS
RHAPSODY provided a controlled environment to test the hypothesis that efficacious IL-1 blockade may render standard therapies redundant, challenging the traditional slow-tapering approach. Of 86 patients participating in the RHAPSODY run-in period, >60% were taking combination therapies. This post hoc analysis of data from the phase III trial RHAPSODY assessed how study investigators transitioned patients with RP who were receiving common multidrug regimens to rilonacept monotherapy. Investigators successfully transitioned all patients receiving non-steroidal anti-inflammatory drugs, colchicine, and glucocorticoids at baseline to rilonacept monotherapy without recurrence using either a sequential (median, 7.7 weeks) or concurrent (median, 8.0 weeks) approach. In addition, rilonacept therapy allowed for rapid discontinuation of oral RP therapies without triggering pericarditis recurrence regardless of dose or duration of glucocorticoid treatment.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
These findings provide insight for clinicians transitioning patients with RP to rilonacept monotherapy, affirming a strategy of rapid cessation of oral therapies. These findings suggest efficacious IL-1 blockade may render standard oral therapies redundant, supporting accelerated withdrawal.
Introduction
Recurrent pericarditis (RP) is a debilitating disease with autoinflammation being one of the possible underlying pathogenic mechanisms. RP is characterised by repeated episodes of pericardial inflammation causing chest pain, ECG changes and pericardial effusion.1–3 Current management of RP includes treatment with non-steroidal anti-inflammatory drugs (NSAIDs), colchicine, systemic glucocorticoids; third-line medications include azathioprine and intravenous human immunoglobulins, alone and in various combinations.1 After the first episode, additional episodes occur in 15%–30% of patients, and management of RP often requires treatment lasting months to years.1 4 5 NSAIDs and colchicine are associated with gastrointestinal and renal side effects that limit use in some patients. Many patients require long-term use of glucocorticoids, which can cause serious adverse effects, including diabetes, hypertension, osteoporosis and adrenal insufficiency.6–12 A history of glucocorticoid treatment is an independent risk factor for pericarditis recurrence,13 and premature tapering of glucocorticoids may contribute to recurrence.1 For these reasons, guidelines recommend tapering glucocorticoids gradually, over several months.1 Considering the increased risk and seriousness of adverse events associated with long-term glucocorticoid treatment,14 15 a need exists for therapies that effectively prevent pericarditis recurrence while minimising glucocorticoid exposure.
The cytokine interleukin (IL) 1 is a key mediator in the inflammatory processes involved in RP.8 16 Rilonacept, an IL-1α and IL-1β cytokine trap, demonstrated efficacy and safety in patients with RP in the phase III Rilonacept inHibition of interleukin-1 Alpha and beta for recurrent Pericarditis: a pivotal Symptomatology and Outcomes Study (RHAPSODY).17 Rilonacept therapy rapidly resolved pericarditis episodes after initiation during the run-in period and significantly reduced the risk of pericarditis recurrence versus placebo during the placebo-controlled, randomised-withdrawal period.17 These data supported the US Food and Drug Administration approval of rilonacept as the first therapy indicated for RP.18 The non-specific anti-inflammatory mechanisms of standard oral therapies overlap the targeted immunomodulatory mechanism of rilonacept, and the randomised-withdrawal period was designed to compare rilonacept monotherapy with placebo. Investigators in RHAPSODY initiated rilonacept therapy by adding it to standard oral therapies and subsequently discontinuing standard oral therapies over 8 weeks.17 19 Tapering of oral therapies, including glucocorticoids, was designed to take place more rapidly than current clinical practice and guideline recommendations because the mechanism of action of rilonacept, that is, selective blockade of the IL-1 pathway, was hypothesised to be sufficient as monotherapy to control RP.1 19 This post hoc analysis provides empirical data describing how investigators managed NSAID, colchicine, and glucocorticoid therapies while transitioning patients to rilonacept monotherapy during the run-in period of RHAPSODY.
Methods
Study design
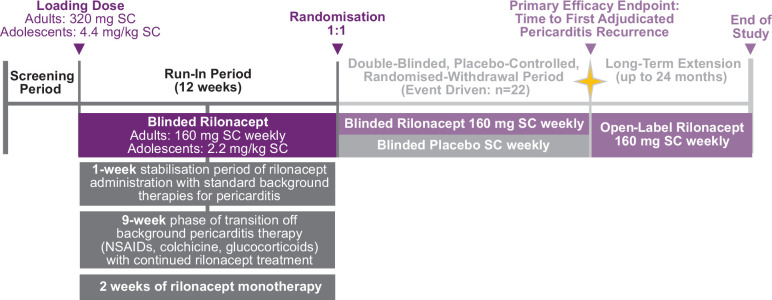
The study design and CONSORT diagram of RHAPSODY were reported previously.20 Briefly, this was a phase III, multicentre, double-blind, placebo-controlled, randomised-withdrawal trial conducted in Australia, Israel, Italy and the USA. Patients were screened for up to 4 weeks to determine trial eligibility and then entered a 12-week run-in period. Adult patients (≥18 years of age) received an initial loading dose of rilonacept 320 mg subcutaneously at baseline, followed by a 160 mg dose administered once weekly throughout the run-in. Adolescent patients (≥12 years to <18 years of age) received an initial loading dose of rilonacept 4.4 mg/kg subcutaneously at baseline, followed by a 2.2 mg/kg dose administered once weekly throughout the run-in.
The run-in period was followed by a randomised-withdrawal period, during which eligible patients were randomised to receive continued rilonacept or placebo. Once the prespecified number of adjudicated pericarditis recurrences had accrued, the randomised-withdrawal phase was closed, and eligible patients had the option to continue open-label rilonacept during a long-term extension.
The goal of the run-in period was to prepare patients for randomisation to rilonacept or placebo at week 12. To accomplish this and to ensure clinical stability on rilonacept monotherapy at randomisation, attainment of rilonacept monotherapy was required by week 10. The run-in period included a 1-week stabilisation period of rilonacept administration with standard oral therapies (NSAIDs, colchicine, glucocorticoids), a 9-week phase of transition off oral therapies with continued rilonacept treatment, and 2 weeks of rilonacept monotherapy (figure 1). The study protocol did not stipulate specific timing or dosing guidance during the transition, but it did require that patients reach monotherapy rilonacept by week 10 and continue through week 12 to qualify for randomisation. The protocol recommended that once clinical stability had been achieved, investigators should begin with glucocorticoid tapering (from week 1 up to week 9), while tapering of NSAID and colchicine should begin later (weeks 4–10), unless earlier dose reduction was needed. The guidelines for background medication taper and discontinuation are shown in table 1.
Figure 1.
Study design of Rilonacept inHibition of interleukin-1 Alpha and beta for recurrent Pericarditis: a pivotal Symptomatology and Outcomes study (RHAPSODY) run-in period. NSAID, non-steroidal anti-inflammatory drug; SC, subcutaneous.
Table 1.
Proposed medication tapering schedule
| Pericarditis medication | Starting dose (mg) | Week 1 (mg) | Week 2 (mg) | Week 3 (mg) | Week 4 (mg) | Week 5 (mg) | Week 6 (mg) | Week 7 (mg) | Week 8 (mg) | Week 10 |
| Prednisone | 60 | 30 | 20 | 15 | 10 | 7.5 | 5 | 2.5 | 1 | Stop |
| 50 | 25 | 20 | 15 | 10 | 7.5 | 5 | 2.5 | 1 | Stop | |
| 40 | 20 | 15 | 15 | 10 | 7.5 | 5 | 2.5 | 1 | Stop | |
| 35 | 17.5 | 15 | 10 | 7.5 | 5 | 2.5 | 1 | Stop | ||
| 30 | 15 | 10 | 10 | 7.5 | 5 | 2.5 | 1 | Stop | ||
| 25 | 12.5 | 10 | 10 | 7.5 | 5 | 2.5 | 1 | Stop | ||
| 20 | 10 | 7.5 | 7.5 | 7.5 | 5 | 2.5 | 1 | Stop | ||
| 15 | 7.5 | 7.5 | 5 | 5 | 2.5 | 2.5 | 1 | Stop | ||
| 12.5 | 7.5 | 7.5 | 5 | 5 | 2.5 | 2.5 | 1 | Stop | ||
| 10 | 5 | 5 | 5 | 2.5 | 2.5 | 1 | Stop | |||
| 7.5 | 5 | 5 | 2.5 | 2.5 | 2.5 | 1 | Stop | |||
| 5 | 2.5 | 2.5 | 2.5 | 1 | Stop | |||||
| 2.5 | 2 | 2 | 1 | Stop | ||||||
| Analgesics | Start taper or stop | Taper or stop | Taper or stop | Taper or stop | Taper or stop | Taper or stop | Taper or stop | Taper or stop | Stop | |
| NSAIDs | Start taper | Taper or stop | Taper or stop | Taper or stop | Taper or stop | Stop | ||||
| Colchicine | Start taper | Taper or stop | Taper or stop | Taper or stop | Taper or stop | Stop |
NSAIDs, non-steroidal anti-inflammatory drugs.
Patients
The study enrolled adult and adolescent (≥12 years of age) patients with a diagnosis of recurrent idiopathic or postcardiac injury pericarditis, defined as two or more recurrences after the first pericarditis episode. Eligible patients could be taking any combination of NSAIDs, colchicine or glucocorticoids. Eligible patients were required to have 1 day or more with pericarditis pain severity 4 or greater on an 11-point Numerical Rating Scale and C reactive protein level of at least 1.0 mg/dL within 7 days before first administration of rilonacept. Pericarditis recurrence required these scores for pericarditis signs/symptoms, whereas clinical response required a pericarditis pain severity score of 2 or less with a C reactive protein level ≤0.5 mg/dL.
Analyses
This post hoc analysis evaluated path and time to rilonacept monotherapy in a group of patients who were receiving combination therapy with NSAIDs, colchicine, and/or glucocorticoids at baseline and who achieved rilonacept monotherapy during the run-in period. Of the 86 subjects that enrolled in the trial, 64% (n=55) entered on multidrug regimens. An ad hoc analysis was performed to assess the length of time necessary to achieve monotherapy. Patients were divided into three groups based on type of combination therapy: NSAID and colchicine double therapy; colchicine and glucocorticoid double therapy; and NSAID, colchicine and glucocorticoid triple therapy. Time to rilonacept monotherapy was also evaluated in patients with long-term (≥28 days) glucocorticoid treatment, with or without other pericarditis treatments, and in subgroups based on glucocorticoid dose (≤15 mg/day (median study dose) or >median study dose), annualised incidence (<2 episodes, 2–4 episodes, or >4 episodes) and disease duration (<1 year, 1–2 years, or >2 years). In patients receiving treatment with both colchicine and glucocorticoids, time to rilonacept monotherapy was assessed in subgroups stratified by taper approach. Those who completed tapering of glucocorticoid prior to beginning colchicine dose reduction/discontinuation were considered to have a ‘sequential’ taper. Those who began colchicine dose reduction/discontinuation during glucocorticoid taper were considered to have a ‘concurrent’ taper. Although sample size is small in this study, the mean was close to median for most continuous variables. In general, continuous variables are presented with descriptive mean and SD. In case mean deviates dramatically from median, median (Q1, Q3) is presented. For time to monotherapy, descriptive statistic is summarised and median (Q1, Q3) is presented.
Results
Eighty-six patients enrolled in the trial and participated in the run-in. Mean (SD) total number of prestudy recurrences, including index and qualifying episodes, was 4.7 (1.7). Mean (SD) duration of disease was 2.4 (3.1) years and mean (SD) duration of prior glucocorticoid treatment was 19.9 (36.3) weeks.
Of 86 enrolled patients, 79 were receiving background therapy at baseline. Of these 79 patients, 74 achieved rilonacept monotherapy. The 5 patients not achieving rilonacept monotherapy did not have pericarditis recurrence; discontinuation was due to adverse events (n=3), positive result on tuberculosis testing (n=1), and sponsor decision (n=1).17 Of the 79 patients receiving background pericarditis therapy at baseline, 55 (69%) had been receiving double or triple combination treatment for RP at baseline and achieved rilonacept monotherapy during the run-in period. Of these patients, 44% (24/55) were treated with NSAIDs plus colchicine, 24% (13/55) with colchicine plus glucocorticoids, and 33% (18/55) with NSAIDs, colchicine and glucocorticoids. Baseline demographic and clinical characteristics of these patients are shown in table 2.
Table 2.
Demographic and clinical characteristics of the patients receiving double or triple combination treatment for recurrent pericarditis at baseline
| Characteristic | NSAID + colchicine (n=24) |
Colchicine + corticosteroid (n=13) |
Colchicine + corticosteroid + NSAID (n=18) |
| Age, years, mean (SD) | 44.6 (13.41) | 43.5 (16.4) | 42.3 (14.7) |
| Age, years, no. (%) | |||
| 12–17 | 1.0 (4.2) | 0 | 1.0 (5.6) |
| 18–64 | 22.0 (91.7) | 12.0 (92.3) | 17.0 (94.4) |
| 65–78 | 1.0 (4.2) | 1.0 (7.7) | 0 |
| Female sex, no. (%) | 19.0 (79.2) | 7.0 (53.8) | 11.0 (61.1) |
| Race*, no. (%) | |||
| White | 23.0 (95.8) | 12.0 (92.3) | 16.0 (88.9) |
| Black/African American | 1.0 (4.2) | 0 | 2.0 (11.1) |
| Other | 0 | 1.0 (7.7) | 0 |
| Aetiology, no. (%) | |||
| Idiopathic | 20.0 (83.3) | 9.0 (69.2) | 15.0 (83.3) |
| Postpericardiotomy syndrome | 3.0 (12.5) | 4.0 (30.8) | 3.0 (16.7) |
| Dressler’s syndrome† | 1.0 (4.2) | 0 | 0 |
| Duration of prior treatment with corticosteroids, weeks, mean (SD) | 0 | 12.0 (17.7) | 11.5 (25.4) |
| Total episodes, including index and qualifying, no., mean (SD) | 4.8 (1.8) | 4.2 (0.93) | 4.5 (0.99) |
| Duration of disease, years, mean (SD) | 3.6 (4.75) | 1.0 (0.4) | 1.4 (0.9) |
| Recurrent episodes per year, mean (SD) | 3.8 (5.1) | 5.5 (2.9) | 5.6 (5.9) |
| Pain rating (qualifying episode), Numerical Rating Scale Score‡, mean (SD) | 6.9 (1.9) | 5.1 (1.3) | 6.5 (1.7) |
| Standard C reactive protein (qualifying episode), mg/dL, mean (SD) | 5.2 (6.4) | 7.5 (7.3) | 7.9 (7.4) |
| Pericarditis manifestations (qualifying episode), no. (%) | |||
| Pericardial effusion§ no. (%) | 6.0 (25.0) | 7.0 (53.8) | 7.0 (38.9) |
| Pericardial rub, no. (%) | 3.0 (12.5) | 1.0 (7.7) | 5.0 (27.8) |
| ST elevation or PR depression, no. (%) | 3.0 (12.5) | 3.0 (23.1) | 4.0 (22.2) |
| Pericarditis treatment at baseline, n (%) | |||
| Non-opioid analgesics | 4.0 (16.7) | 0 | 0 |
| Opioid analgesics | 4.0 (16.7) | 0 | 0 |
| Aspirin | 2.0 (8.3) | 0 | 1.0 (5.6) |
| Other NSAIDs¶ | 22.0 (91.7) | 0 | 17.0 (94.4) |
| Colchicine | 24.0 (100) | 13.0 (100) | 18.0 (100) |
| Oral corticosteroids | 0 | 13.0 (100) | 18.0 (100) |
| Other | 0 | 1.0 (7.7) | 1 (5.6) |
*Race was reported by patient.
†The cause of the Dressler syndrome was catheter ablation for atrial fibrillation.
‡Scores on the Numerical Rating Scale for pain range from 0 to 10, with higher scores indicating greater pain severity.
§Pericardial effusion was defined as new or worsening pericardial effusion, independent of the imaging method.
¶Non-steroidal anti-inflammatory drugs.
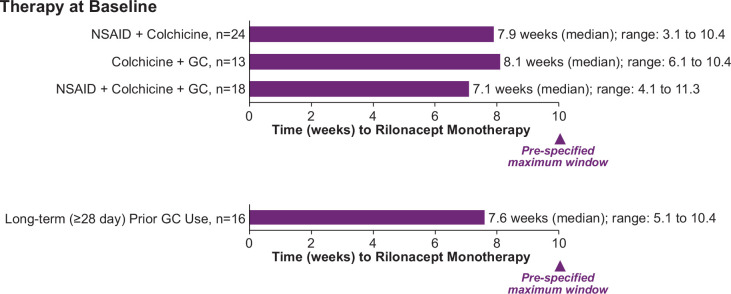
Despite the protocol-specified requirement that patients reach monotherapy rilonacept by week 10 to qualify for randomisation (after 2 weeks of monotherapy), median time to rilonacept monotherapy ranged from 7.1 weeks to 8.1 weeks for patients in the three groups (NSAID plus colchicine and glucocorticoid; colchicine plus glucocorticoid; NSAID plus colchicine; figure 2). Physicians in this study chose to transition their patients to rilonacept monotherapy approximately 2 weeks faster on average than the protocol-stipulated maximum-allowed timeframe to qualify for randomisation. Patients with RP previously treated with long-term (≥28 days) glucocorticoids (n=16) were transitioned by investigators to rilonacept monotherapy in a median of 7.6 weeks (figure 2). Patients treated with ≤15 mg/day (median study dose; n=21) or >median study dose (n=18) glucocorticoids were transitioned to rilonacept monotherapy in a median of 7.3 weeks and 8.0 weeks, respectively.
Figure 2.
Median time to rilonacept monotherapy, by therapy combination at baseline. GC, glucocorticoid; NSAID, non-steroidal anti-inflammatory drug.
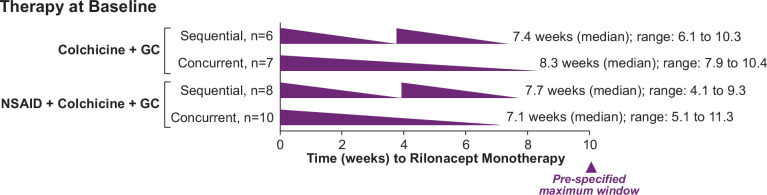
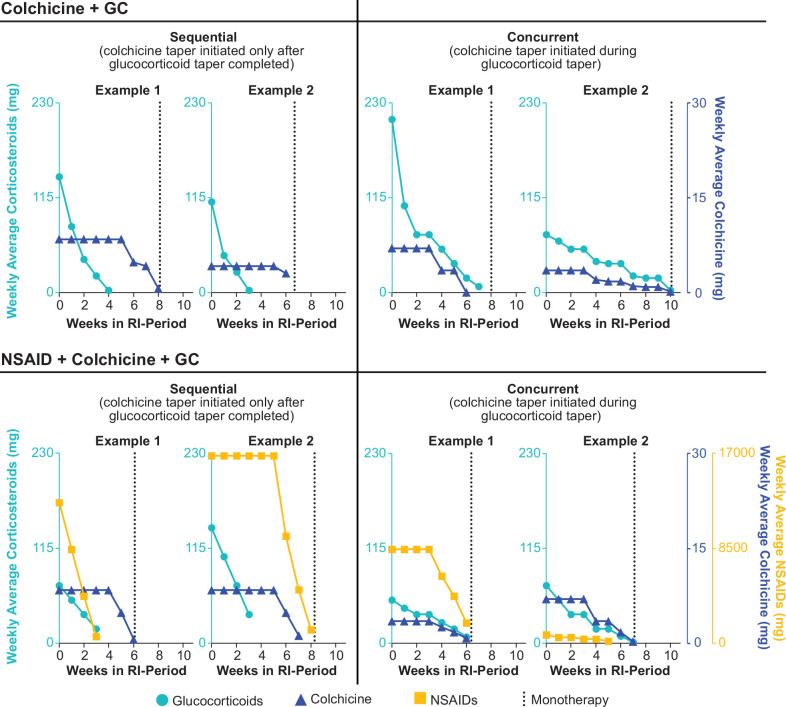
Patients receiving both colchicine and glucocorticoids (n=31) were transitioned from background therapies in similar proportions either sequentially (n=14, 45.2%) or concurrently (n=17, 54.8%). Regardless of taper approach, investigators transitioned all patients to rilonacept monotherapy within similar timeframes: sequential (n=14; median, (Q1, Q3), 7.7 (6.1, 8.3) weeks) and concurrent (n=17; median (Q1, Q3), 8.0 (7.1,10.0) weeks) (figure 3). Patients receiving colchicine and glucocorticoids at baseline demonstrated comparable transition time to rilonacept monotherapy (n=24; median (Q1, Q3), 7.9 (5.9, 9.9) weeks). Figure 4 provides examples of representative approaches that investigators took while transitioning patients off standard oral therapies. Of note, there were no pericarditis recurrences during transition to monotherapy.
Figure 3.
Median time to rilonacept monotherapy in patients receiving treatment with colchicine and glucocorticoids at baseline, by taper approach. GC, glucocorticoid; NSAID, non-steroidal anti-inflammatory drug.
Figure 4.
Representative approaches to tapering NSAIDs, colchicine and glucocorticoids. Because these data represent weekly average doses, some data points do not reach zero at the final tapering time point; however, complete taper was achieved. GC, glucocorticoid; NSAID, non-steroidal anti-inflammatory drug; RI, run-in.
A trend was observed towards shorter median time to monotherapy in patients with a prestudy annualised incidence of fewer than two episodes per year (median, 6.1 (Q1–Q3, 4.1–8.1) weeks; n=23) than in patients with 2–4 episodes per year (median, 8.3 (Q1–Q3, 7.0–10.0) weeks; n=23) or in those with more than four episodes per year (median, 8.1 (Q1–Q3, 6.6–9.9); n=28). A trend was also observed towards shorter median time to monotherapy in patients with disease duration longer than 2 years (median, 6.1 (Q1–Q3, 4.3–9.3) weeks; n=25) than in patients with disease duration of 1–2 years (median, 8.0 (Q1–Q3, 6.1–9.7) weeks; n=26) or less than 1 year (median, 8.0 (Q1–Q3, 6.7–10.0) weeks; n=23).
Discussion
Patients entering RHAPSODY were acutely symptomatic despite oral multidrug therapy. Because rilonacept, which is an IL-1α and IL-1β cytokine trap, directly targets the disease mechanism, it had been hypothesised in the trial design that the various standard oral therapies would no longer be needed and could be withdrawn relatively rapidly after rilonacept initiation. This proved to be the case, as these therapies were withdrawn, and rilonacept monotherapy was achieved in a median of 7.9 weeks without pericarditis recurrence.17 Rapid resolution of acute episodes shortly after initiation of rilonacept during the run-in period indicates that the targeted IL-1 blockade was both necessary and sufficient to control disease. While it may be more difficult to make conclusions from a post hoc analysis, this analysis revealed the practice patterns clinicians who were initiating rilonacept treatment and transitioning patients off oral therapies took to manage RP medications with the goal of attaining rilonacept monotherapy. Investigators transitioned patients to monotherapy rilonacept over a similar period (just <2 months) in groups of patients receiving combination treatment with commonly used oral therapies for RP (including patients receiving long-term glucocorticoid treatment), regardless of which management approach (sequential or concurrent) was used.
Given the chronicity of RP, clinicians face a conundrum when considering glucocorticoids for disease management: practice guidelines note that chronic use of glucocorticoids is associated with serious side effects, yet the data also show that discontinuation of treatment with glucocorticoids may increase the risk of pericarditis recurrence. Guidelines encourage minimising the risk of recurrence by gradually tapering off glucocorticoids: decreasing the dose by 1–2.5 mg per day every 2–6 weeks over several months when the dose is less than 15 mg/day.1 A retrospective claims database study demonstrated that each additional week of glucocorticoid treatment is associated with a 1.11-fold higher risk of related adverse events,15 a risk profile suggesting that, if possible, glucocorticoids should be rapidly tapered to reduce such events.
By contrast, use of rilonacept in RHAPSODY allowed for rapid glucocorticoid tapering without precipitating pericarditis recurrence. While clinicians often taper oral therapies taken to manage RP slowly, per available guidelines, those guidelines do not take into consideration a highly targeted, single-agent treatment such as rilonacept. In RHAPSODY, ceasing oral therapies at a rate faster than is usual in clinical practice was possible because of the overlapping and targeted disease coverage provided by rilonacept. Specifically, in patients who had been receiving glucocorticoids in combination with other treatments before study entry—including patients on long-term glucocorticoid therapy—investigators withdrew background treatments after rilonacept initiation (an overlapping approach) on the way to rilonacept monotherapy, which was achieved in a median of 7.1–8.1 weeks; the investigators chose concurrent more often than sequential tapering. This clinical trial observation, taken together with previous findings from studies using anakinra,21–23 provides evidence that could support a clinical practice management strategy of more rapid cessation of oral therapies when IL-1 blockade is used to manage RP, potentially minimising adverse events associated with prolonged glucocorticoid exposure. In addition, the safety profile of rilonacept17 and once-weekly administration provide additional advantages to transitioning to rilonacept.
RHAPSODY is the first IL-1 antagonist clinical trial in pericarditis in which all patients were treated with monotherapy (the Anakinra Treatment of Recurrent Idiopathic Pericarditis (AIRTRIP) tudy did not require discontinuation of colchicine treatment during the randomised-withdrawal period).23 Interestingly, the RHAPSODY investigators made the transition to rilonacept monotherapy in less than the maximum time stipulated by the protocol. In this study, rilonacept initiation in patients who had been experiencing pericarditis recurrence despite oral therapies resulted in rapid resolution of pericarditis episodes (average of 5 days to treatment response) during the run-in period.17 This observation may have increased investigator confidence to discontinue oral therapies more rapidly than they might have in their usual clinical practice without the benefit of rilonacept coverage. Although the protocol provided general guidelines for drug management, the investigators were free to use their clinical judgement while discontinuing oral therapies. Therefore, results of this post hoc analysis may more closely mirror real-world clinical tapering practice than would have been expected from a typical clinical trial. Thus, these findings can inform clinical practice and future studies of rilonacept in patients with RP. The ongoing long-term extension of RHAPSODY is designed to provide additional information regarding duration of rilonacept use and possible strategies for cessation of RP pharmacotherapy.
Limitations of this post hoc analysis of RHAPSODY trial data include the small patient population analysed, clinician preference, lack of run-in period events (difficult to show differences), lack of long-term follow-up, and discontinued participation of some patients during the run-in period.
Conclusion
In this post hoc analysis of RHAPSODY data, investigators initiating rilonacept treatment in patients with RP rapidly transitioned the patients from oral multidrug therapy (including long-term glucocorticoid treatment) to rilonacept monotherapy. Patients experienced rapid treatment response to rilonacept therapy and discontinued treatment with NSAIDs, colchicine, and/or glucocorticoids in a median of 7.1–8.1 weeks without recurrence of pericarditis, regardless of whether a sequential or concurrent tapering approach was employed. This analysis provides additional insight for clinicians considering even more rapid cessation of oral therapies when incorporating rilonacept into the treatment paradigm for patients with RP.
Acknowledgments
The authors thank the patients, along with their families and caregivers, who participated in the RHAPSODY Trial; Lucia Trotta, MD, clinical trial personnel; the C5Research group at Cleveland Clinic. PCC, MD, thanks research nurse coordinator Danielle Kellner. The authors also thank Callie Grimes, PhD, of Peloton Advantage, LLC, an OPEN Health company for medical writing assistance, and Kiniksa Pharmaceuticals Corp for funding.
Footnotes
Contributors: Material contributions to this manuscript include AB, JFP, ALK, MI, PCC and LZ (trial design), JFP, AW and LZ (protocol authorship), AW, JFP (supervision/monitoring centres), LZ, AW, JFP, AK and MI (data analysis), all authors (interpretation of results), AB, JFP, ALK and MI (writing manuscript), JFP (guarantor), all authors (editing/review of manuscript), the RHAPSODY investigators who provided and cared for study patients, the patients and their caregivers, and the employees of Kiniksa Pharmaceuticals who contributed to the conduct and analyses of the trial and the writing of the manuscript.
Funding: This study was sponsored by Kiniksa Pharmaceuticals.
Competing interests: AB reports institutional funding from Kiniksa Pharmaceuticals as an investigative site; an unrestricted research grant from Sobi and Acarpia; and travel and accommodation for advisory committee from Sobi and Kiniksa Pharmaceuticals. AW reports personal fees from Kiniksa Pharmaceuticals during the conduct of the study and personal fees from Kiniksa Pharmaceuticals outside the submitted work. AW is a former employee of Kiniksa Pharmaceuticals; the work here was completed during his employment. SAL reports consultant fees for Kiniksa Pharmaceuticals, Sobi Pharmaceuticals and Medtronic. AA reports grants and personal fees from Kiniksa Pharmaceuticals during the conduct of the study; grants and personal fees from Olatec, Serpin, Novartis and Janssen; and personal fees from Novo-Nordisk and Cromos Pharma outside the submitted work. PCC reports grants and personal fees from Kiniksa Pharmaceuticals; grants from Novartis Pharmaceuticals; and personal fees from Sobi Pharmaceuticals outside the submitted work. LZ reports personal fees and other from Kiniksa Pharmaceuticals outside the submitted work. ML reports grants and advisory board, consulting, and other fees from Kiniksa Pharmaceuticals outside the submitted work and consulting fees from Sobi Pharmaceuticals outside the submitted work. BSL reports personal fees from Kiniksa Pharmaceuticals during the conduct of the study. DL reports personal fees from Regeneron outside the submitted work. SN reports grants and personal fees from Kiniksa Pharmaceuticals during the conduct of the study; grants and personal fees from AstraZeneca, Anthera, Resverlogix, Sanofi-Regeneron and Esperion; personal fees from Akcea, Eli Lilly, Omthera, Merck, Takeda, CSL Behring and Boehringer Ingelheim; and grants from Amgen, Novartis, Cerenis, The Medicines Company, Liposcience, Roche and InfraReDx outside the submitted work. ALK reports grants and other from Kiniksa Pharmaceuticals during the conduct of the study and other fees from Cardiol Therapeutics, Sobi Pharmaceuticals and Pfizer Pharmaceuticals outside the submitted work. MI reports other fees from Kiniksa Pharmaceuticals and Sobi outside the submitted work. JFP reports personal fees and other from Kiniksa Pharmaceuticals outside the submitted work and is a patent inventor on pending patent applications licensed to Kiniksa Pharmaceuticals covering methods of using rilonacept for treating recurrent pericarditis.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement
Data are available in a public, open access repository. Data are available upon reasonable request. De-identified participant data will be available, one year after study completion, upon reasonable written request to researchers whose proposed use of the data has been approved. Requests may be directed to Dr John F Paolini, ORCID ID: 0000-0001-7622-8851. Data will not be provided to requesters with potential or actual conflicts of interest, including individuals requesting access for commercial, competitive or legal purposes. Data access may be precluded for studies in which clinical data were collected subject to legal, contractual or consent provisions that prohibit transfer to third parties. All those receiving access to data will be required to enter into a Data Use Agreement (DUA), which shall contain terms and conditions that are customary for similar agreements and similar companies in the industry. Data available to the public including the study protocol can be found at: (data set) Klein AL, Imazio M, Cremer P, et al. Phase 3 trial of interleukin-1 trap rilonacept in recurrent pericarditis. N Engl J Med 2021;384:31-41. DOI: 10.1056/NEJMoa2027892.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study involves human participants and was approved by Bellberry Human Research Ethics Committee123 Glen Osmond Road Eastwood, South Australia, 5063 AustraliaMonash Health Ethics Committee Level 2, I BlockMonash Medical Centre246 Clayton Road, Clayton, Victoria, 3168 AustraliaTasmania Health and Medical Human Research Ethics Committee Office of Research Services University of Tasmania Private Bag 01Hobart, Tasmania, 7001Australia Monash Health Ethics Committee Level 2, I Block Monash Medical Centre 246 Clayton Road Clayton, Victoria, 3168 Australia Ethics Committee of Milano Area 1 c/o ASST Fatebenefratelli SaccoP.O. L. Sacco - Via G.B. Grassi n. 74 Milan, Lombardy 20157 Italy IRCCS Ospedale Pediatrico Bambino GesùViale Ferdinando Baldelli 41 Rome, Lazio, 00146 Italy Comitato Etico Regionale della Liguria Segreteria c/o U.O. Affari Generali e Legali Opsedale Policlinico San Martino, IRCCS L.go R. Benzi 10 Genova, Liguria, 16132 Italy Ethics Committee of AOU ""Città della Salute e della Scienza di Torino"" c/o Presidio Ospendaliero Molinette Padiglione beige - 3 PianoCorso Bramante 88Turin, Piedmont, 10126ItalyInstitutional Helsinki Committee Galilee Medical Center1 Ben Tzvi Boulevard Nahariya, 2210001IsraelInstitutional Helsinki Committee Sheba Medical Center at Tel-HashomerDerech Sheba 2 Ramat-Gan, 52621Israel Institutional Helsinki Committee Ha’Emek Medical Center 21 Rabin Road Afula, 18101 Israel Institutional Helsinki Committee Bnai Zion Medical Center 47 Golomb Street Haifa, 31048 Israel Institutional Helsinki Committee Shaare Zedek Medical Center 12 Shmuel Bait Street Jerusalem, 9103102 Israel Institutional Helsinki Committee Ziv Medical Center Derech Ha’RambamSafed, 13100 Israel Institutional Helsinki Committee Hadassah Medical Center Mount Scopus Hadassah Har Hazofirm Jerusalem, 91240 Israel Institutional Helsinki Committee Rambam Medical Center Haaliya Hashniya Street Haifa, 31096 Israel Institutional Helsinki Committee Wolfson Medical Center,62 Halohamim StreetHolon, 58100 Israel Institutional Helsinki Committee Assaf Harofeh Medical Center Beer Yaakov Tzarin, 70300 Israel Institutional Helsinki Committee Rabin Medical Center 39 Jabotinski Street Petach Tikva, 49100 Israel Rochester Regional Health IRB Office of Human Research Protections 1425 Portland Avenue Rochester, NY, 14621 USA Western Institutional Review Board (WIRB)1019 39th Avenue. SE Suite 120 Puyallup, WA, 98374 USA Quorum Institutional Review Boarda 1501 Fourth Avenue Seattle, WA, 98101 USA Mayo Clinic Institutional Review Board (IRB) 200 First Street SW Rochester, MN, 55905 USA Quorum Institutional Review Boarda 1501 Fourth Avenue Seattle, WA, 98101 USA Cincinnati Children’s Hospital Medical Center Institutional Review Board 3333 Burnet Avenue, S10.300 Cincinnati, OH, 45229 USA Vanderbilt Human Research Protections Program 1313 21st Avenue, South, Suite 504 Nashville, TN, 37232 USA Quorum Institutional Review Boarda 1501 Fourth Avenue Seattle, WA, 98101 USA The University of Vermont Committee on Human Research in the Medical Sciences 213 Waterman Building 85 South Prospect Street Burlington, VT, 05405 USA Quorum Institutional Review Boarda 1501 Fourth Avenue Seattle, WA, 98101 USA Cleveland Clinic Institutional Review Board Cleveland Clinic 9500 Euclid Avenue, OS-1 Cleveland, OH, 44195 USA Oklahoma University Health Science Center Institutional Review Board 1105 N. Stonewall Avenue Library Building Room 176 Oklahoma City, OK, 73117 USA Intermountain Healthcare IRB 5171 S. Cottonwood St., Suite 400 Murray, UT, 84107 USA Office of Research Compliance Division of Human Subject Protections Stony Brook University Stony Brook, NY, 11794 USA Cedars-Sinai Institutional Review Board (IRB) Office of Research Compliance and Quality Improvement 6500 Wilshire Boulevard., Suite 1800 Los Angeles, CA, 90048 USA Western Institutional Review Board (WIRB) 1019 39th Avenue SE Suite 120 Puyallup, WA, 98374 USA Icahn School of Medicine IRB 345 East 102 Street Suite 200 New York, NY, 10029 USA Beth Israel Deaconess Medical Center CCI/IRB330 Brookline Avenue Boston, MA, 02215 USA Advarra Institutional Review Board 6940 Columbia Gateway Drive Suite 110 Columbia, MD, 21046 USA. This study involves human participants and was approved by the following Ethics Committees and Institutional Review Boards with each respective ID numbers in parentheses: Bellberry Human Research Ethics Committee (Application #: 2018-11-1015AA-PRE-1); Monash Health (HREC Reference #: HREC/48510/MonH-2019-162416(v1) Monash Health Local Reference: RES-19-0000035A); Comitato Etico Milano Area 1 - ASST Sacco Fatebenefratelli (16462/2019); Comitato Etico dell’IRCCSOspedale Pediatrico Bambino Gesù (Prot. Nr. 950); Comitato Etico InteraziendaleA.O.U. Città della Salute e della Scienza di Torino (2019/ST/010); Galilee Medical Center EC (0204-18-NHR); Institutional Helsinki Committee, The Chaim Sheba Medical Center (5854-19-SMC); HaEmek Medical Center EC (0007-19-EMC); Bnai ZionMedical Center EC (006-19-BNZ); Shaare Zedek Medical Center EC (0046-19-SZMC);Ziv Medical Center Local EC (0006-19-ZIV); Rambam Medical Center Ethics Committee (0059-19-RMB); Edith Wolfson MC Local EC (0012-19-WOMC); Rabin Medical Center Local EC (0148-19-RMC); Western Institutional Review Board (20190577); Quorum Review IRB (33633/1; 33633/2; 33633/3; 33633/6; 33633/7); Advarra Institutional Review Board (Pro00035076); Mayo Clinic IRB (Mod18-009973-30); Cincinnati Childrens Hospital Medical Center IRB (2019-0583); University of Vermont Committee on Human Research in the Medical Sciences (MOD00005516);Cleveland Clinic Institutional Review Board (FWA 00005367); Cedars-Sinai Medical Center Office of Research Compliance and Quality Improvement (RNI00002653); Mount Sinai School of Medicine Program for the Protection of Human Subjects (IRB-19-02794). Participants gave informed consent to participate in the study before taking part.
References
- 1. Adler Y, Charron P, Imazio M, et al. 2015 ESC Guidelines for the diagnosis and management of pericardial diseases: The Task Force for the Diagnosis and Management of Pericardial Diseases of the European Society of Cardiology (ESC)Endorsed by: The European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J 2015;36:2921–64. 10.1093/eurheartj/ehv318 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Vecchié A, Chiabrando JG, Dell MS, et al. Clinical presentation and outcomes of acute pericarditis in a large urban hospital in the United States of America. Chest 2020;158:2556–67. 10.1016/j.chest.2020.07.039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Bizzi E, Picchi C, Mastrangelo G, et al. Recent advances in pericarditis. Eur J Intern Med 2022;95:24–31. 10.1016/j.ejim.2021.09.002 [DOI] [PubMed] [Google Scholar]
- 4. Imazio M, Brucato A, Cemin R, et al. A randomized trial of colchicine for acute pericarditis. N Engl J Med 2013;369:1522–8. 10.1056/NEJMoa1208536 [DOI] [PubMed] [Google Scholar]
- 5. Imazio M, Bobbio M, Cecchi E, et al. Colchicine in addition to conventional therapy for acute pericarditis: results of the colchicine for acute pericarditis (cope) trial. Circulation 2005;112:2012–6. 10.1161/CIRCULATIONAHA.105.542738 [DOI] [PubMed] [Google Scholar]
- 6. Hernández-Díaz S, Rodríguez LA. Association between nonsteroidal anti-inflammatory drugs and upper gastrointestinal tract bleeding/perforation: an overview of epidemiologic studies published in the 1990s. Arch Intern Med 2000;160:2093–9. 10.1001/archinte.160.14.2093 [DOI] [PubMed] [Google Scholar]
- 7. Imazio M, Gaita F, LeWinter M. Evaluation and treatment of pericarditis: a systematic review. JAMA 2015;314:1498–506. 10.1001/jama.2015.12763 [DOI] [PubMed] [Google Scholar]
- 8. Chiabrando JG, Bonaventura A, Vecchié A, et al. Management of Acute and Recurrent Pericarditis: JACC State-of-the-Art Review. J Am Coll Cardiol 2020;75:76–92. 10.1016/j.jacc.2019.11.021 [DOI] [PubMed] [Google Scholar]
- 9. Imazio M, Brucato A, Cumetti D, et al. Corticosteroids for recurrent pericarditis: high versus low doses: a nonrandomized observation. Circulation 2008;118:667–71. 10.1161/CIRCULATIONAHA.107.761064 [DOI] [PubMed] [Google Scholar]
- 10. Rice JB, White AG, Scarpati LM, et al. Long-term systemic corticosteroid exposure: a systematic literature review. Clin Ther 2017;39:2216–29. 10.1016/j.clinthera.2017.09.011 [DOI] [PubMed] [Google Scholar]
- 11. Broersen LHA, Pereira AM, Jørgensen JOL, et al. Adrenal insufficiency in corticosteroids use: systematic review and meta-analysis. J Clin Endocrinol Metab 2015;100:2171–80. 10.1210/jc.2015-1218 [DOI] [PubMed] [Google Scholar]
- 12. Bornstein SR, Allolio B, Arlt W, et al. Diagnosis and treatment of primary adrenal insufficiency: an endocrine Society clinical practice guideline. J Clin Endocrinol Metab 2016;101:364–89. 10.1210/jc.2015-1710 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Imazio M, Bobbio M, Cecchi E, et al. Colchicine as first-choice therapy for recurrent pericarditis: results of the core (colchicine for recurrent pericarditis) trial. Arch Intern Med 2005;165:1987–91. 10.1001/archinte.165.17.1987 [DOI] [PubMed] [Google Scholar]
- 14. Schwier NC, Luis SA, Hu X, et al. PCV5 risk factors associated with recurrence and Corticosteroid-Associated adverse events in patients with recurrent pericarditis. Value Health 2021;24:S67. 10.1016/j.jval.2021.04.345 [DOI] [Google Scholar]
- 15. Schwier NC, Luis SA, Hu X, et al. Risk factors associated with recurrence and corticosteroid-associated adverse events in patients with recurrent pericarditis [poster]. Presented at: Annual Meeting of the International Society for Pharmacoeconomics and Outcomes Research; May 17-20, 2021. [Google Scholar]
- 16. Dinarello CA, Simon A, van der Meer JWM. Treating inflammation by blocking interleukin-1 in a broad spectrum of diseases. Nat Rev Drug Discov 2012;11:633–52. 10.1038/nrd3800 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Klein AL, Imazio M, Cremer P, et al. Phase 3 trial of interleukin-1 trap rilonacept in recurrent pericarditis. N Engl J Med 2021;384:31–41. 10.1056/NEJMoa2027892 [DOI] [PubMed] [Google Scholar]
- 18. Regeneron Pharmaceuticals . Arcalyst [package insert]. Tarrytown, NY, 2016. [Google Scholar]
- 19. Klein AL, Lin D, Cremer PC, et al. Efficacy and safety of rilonacept for recurrent pericarditis: results from a phase II clinical trial. Heart 2020;107:488–96. 10.1136/heartjnl-2020-317928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Klein AL, Imazio M, Brucato A, et al. RHAPSODY: rationale for and design of a pivotal phase 3 trial to assess efficacy and safety of rilonacept, an interleukin-1α and interleukin-1β trap, in patients with recurrent pericarditis. Am Heart J 2020;228:81–90. 10.1016/j.ahj.2020.07.004 [DOI] [PubMed] [Google Scholar]
- 21. Finetti M, Insalaco A, Cantarini L, et al. Long-term efficacy of interleukin-1 receptor antagonist (anakinra) in corticosteroid-dependent and colchicine-resistant recurrent pericarditis. J Pediatr 2014;164:1425–31. 10.1016/j.jpeds.2014.01.065 [DOI] [PubMed] [Google Scholar]
- 22. Lazaros G, Vasileiou P, Koutsianas C, et al. Anakinra for the management of resistant idiopathic recurrent pericarditis. initial experience in 10 adult cases. Ann Rheum Dis 2014;73:2215–7. 10.1136/annrheumdis-2014-205990 [DOI] [PubMed] [Google Scholar]
- 23. Brucato A, Imazio M, Gattorno M, et al. Effect of anakinra on recurrent pericarditis among patients with colchicine resistance and corticosteroid dependence: the AIRTRIP randomized clinical trial. JAMA 2016;316:1906–12. 10.1001/jama.2016.15826 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are available in a public, open access repository. Data are available upon reasonable request. De-identified participant data will be available, one year after study completion, upon reasonable written request to researchers whose proposed use of the data has been approved. Requests may be directed to Dr John F Paolini, ORCID ID: 0000-0001-7622-8851. Data will not be provided to requesters with potential or actual conflicts of interest, including individuals requesting access for commercial, competitive or legal purposes. Data access may be precluded for studies in which clinical data were collected subject to legal, contractual or consent provisions that prohibit transfer to third parties. All those receiving access to data will be required to enter into a Data Use Agreement (DUA), which shall contain terms and conditions that are customary for similar agreements and similar companies in the industry. Data available to the public including the study protocol can be found at: (data set) Klein AL, Imazio M, Cremer P, et al. Phase 3 trial of interleukin-1 trap rilonacept in recurrent pericarditis. N Engl J Med 2021;384:31-41. DOI: 10.1056/NEJMoa2027892.