Abstract
The U.S. is experiencing an epidemic of type 2 diabetes. Socioeconomically disadvantaged and certain racial and ethnic groups experience a disproportionate burden from diabetes and are subject to disparities in treatment and outcomes. The National Clinical Care Commission (NCCC) was charged with making recommendations to leverage federal policies and programs to more effectively prevent and control diabetes and its complications. The NCCC determined that diabetes cannot be addressed simply as a medical problem but must also be addressed as a societal problem requiring social, clinical, and public health policy solutions. As a result, the NCCC’s recommendations address policies and programs of both non–health-related and health-related federal agencies. The NCCC report, submitted to the U.S. Congress on 6 January 2022, makes 39 specific recommendations, including three foundational recommendations that non–health-related and health-related federal agencies coordinate their activities to better address diabetes, that all federal agencies and departments ensure that health equity is a guiding principle for their policies and programs that impact diabetes, and that all Americans have access to comprehensive and affordable health care. Specific recommendations are also made to improve general population-wide policies and programs that impact diabetes risk and control, to increase awareness and prevention efforts among those at high risk for type 2 diabetes, and to remove barriers to access to effective treatments for diabetes and its complications. Finally, the NCCC recommends that an Office of National Diabetes Policy be established to coordinate the activities of health-related and non–health-related federal agencies to address diabetes prevention and treatment. The NCCC urges Congress and the Secretary of Health and Human Services to implement these recommendations to protect the health and well-being of the more than 130 million Americans at risk for and living with diabetes.
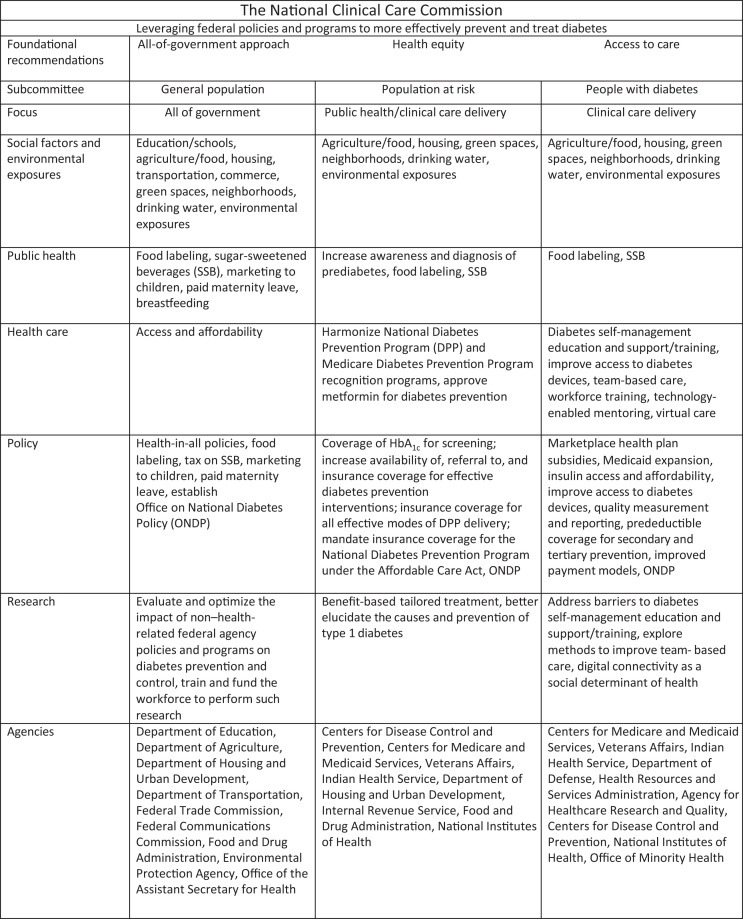
Graphical Abstract
Introduction
Diabetes is a major clinical and public health problem in the U.S. The disease and its complications affect millions of Americans of all ages, lead to preventable suffering and death, impact families, contribute to health inequities, and impose an enormous financial burden on our nation. The number of Americans with diabetes and its complications has grown each year despite advances in prevention and treatment (1,2).
The social and environmental conditions that shape people’s daily experiences across their life span have a huge impact on whether people develop diabetes or suffer from its complications (3). Accordingly, diabetes in the U.S. cannot simply be addressed as a medical problem. It must also be addressed as a societal problem involving diverse sectors including food, housing, commerce, transportation, and the environment (1,4). The recommendations of the National Clinical Care Commission (NCCC) are rooted in the understanding that to improve the health outcomes of people at risk for and with diabetes, all of these sectors must be engaged. The recommendations of the NCCC are informed by both the Socioecological Model and the Chronic Care Model and are aligned with a “health-in-all-policies” approach (1,4,5).
The NCCC was charged by Congress to make recommendations to leverage federal policies and programs to more effectively prevent and treat diabetes and its complications. The NCCC formed three subcommittees to make recommendations 1) at the general population level’ 2) for high-risk individuals with prediabetes; and 3) for people with diabetes and its complications. It surveyed federal agencies and conducted follow-up meetings with representatives from 10 health-related and 11 non–health-related federal agencies. It held 12 public meetings, solicited public comments, met with numerous stakeholders and key informants, and performed comprehensive literature reviews (1,4).
The recommendations of the NCCC focused on federal policies and programs and were prioritized according to the strength of evidence, the recommendations’ reach and scope, practicability, likely effectiveness and safety, affordability, and impact on health equity. The NCCC Final Report, which was transmitted to Congress in January 2022, included 39 specific recommendations. In this article we briefly summarize the Commission’s recommendations and propose steps for developing and implementing a new national strategy to coordinate federal efforts to prevent and control diabetes in the U.S.
Foundational Recommendations
To improve diabetes awareness, prevention, and treatment, all three NCCC subcommittees recognized that federal efforts must involve multisector engagement and trans-agency collaboration, address social determinants of health and health equity, and improve access to health care. Accordingly, the NCCC made three foundational recommendations (1,6):
Non–health-related and health-related federal agencies should coordinate their activities to comprehensively address diabetes prevention and treatment.
Health equity should be addressed in all federal policies and programs that impact people at risk for or with diabetes.
All people at risk for and with diabetes should have access to comprehensive, high-quality, and affordable health care.
The Commission also developed recommendations to address 1) population-wide policies and federal programs that can affect diabetes prevention and treatment; 2) diabetes prevention in populations at high risk for developing type 2 diabetes; and 3) the treatment of diabetes and its complications. These are discussed in detail in other articles in this series (7–12). We summarize key recommendations below.
Recommendations for Population-Wide Policies and Programs
To delay, prevent, and control diabetes, and to reduce racial, ethnic, and income-related disparities in diabetes treatment and outcomes, changes must be made in the social and environmental contexts in which U.S. residents live, learn, work, and play. Such changes cannot be accomplished by health-related federal agencies alone. Federal agencies whose policies and programs shape the social and environmental contexts that influence diabetes incidence, treatment, and complications must also be actively engaged (7,8). To address this critical need, the NCCC recommends:
Updating and revising the U.S. Department of Agriculture’s nutrition assistance programs to promote both food security and dietary quality across the life span.
Increasing breastfeeding rates and duration through effective federal programs and paid maternity leave.
Implementing federal strategies to encourage the consumption of water rather than sugar-sweetened beverages.
Updating the Food and Drug Administration’s food and beverage labeling policies and practices to ensure that labels are science-based, clear, direct, and not misleading so individuals can identify and reduce consumption of foods and beverages associated with a higher burden of diabetes.
Providing the Federal Trade Commission with the authority and resources to regulate the food and beverage industry’s marketing and advertising to children, who lack the skills to determine if they are being deceived.
Reducing exposure to environmental toxins associated with diabetes (polluted air, contaminated water, and pollutants in the land) and exposure to endocrine-disrupting chemicals through Environmental Protection Agency programs and policies.
Improving the built environment to enhance walkability, green spaces, physical activity resources, and active transport opportunities through programs and policies of the Department of Transportation.
Expanding housing opportunities in health-promoting environments for low-income individuals and families through programs of the Department of Housing and Urban Development and the Internal Revenue Service.
The NCCC also recommends that the federal government support research to increase our understanding of the social and environmental conditions associated with the risk of diabetes and its complications and to evaluate the impact of interventions on diabetes-related outcomes (7,8).
Recommendations for Diabetes Prevention in People at High Risk
These NCCC recommendations focus on lifestyle change programs and medications that have the greatest likelihood of preventing diabetes in those who are at high risk for type 2 diabetes, specifically people with prediabetes, and on access to, participation in, and sustainability of these interventions. Unfortunately, most people with prediabetes are not aware they have it, and most do not engage in preventive interventions (9,10). Thus, the NCCC recommends:
Increasing awareness of prediabetes and the availability of effective lifestyle intervention programs, in particular the National Diabetes Prevention Program (DPP) and the Medicare DPP.
Covering hemoglobin A1c as a screening test for prediabetes.
Adopting clinical quality measures, such as those recommended by the American Medical Association, that assess screening for prediabetes, interventions for prediabetes, and retesting of patients with prediabetes to serve as an impetus for continuous quality improvement.
Providing insurance coverage for proven effective in-person, telehealth, and virtual delivery modalities for diabetes prevention.
Approving the Medicare DPP as a permanent covered benefit.
Streamlining and harmonizing the recognition and payment processes for DPPs.
Improving payment models and payment levels for DPP providers to ensure program sustainability.
Incentivizing state Medicaid programs to provide coverage for the National DPP.
Providing additional support for federal programs that focus on type 2 diabetes prevention.
Providing funding to the National Institutes of Health to facilitate a third party to collect, analyze, and summarize available data for a Food and Drug Administration application to consider approval of metformin for diabetes prevention in high-risk patients with prediabetes.
The NCCC also recommends that research be supported to develop new and better methods for preventing type 1 and type 2 diabetes (9,10).
Recommendations for Diabetes Treatment and Complications
The biggest problem in diabetes treatment and the prevention of diabetes complications in the U.S. is the gap between the resources available to people with diabetes and the resources they actually receive. This gap results in many people with diabetes developing preventable complications. The NCCC’s recommendations for diabetes treatment and complications focus on what can be done at the federal level to bridge this gap (11,12):
At the patient level, the NCCC recommends reducing barriers and streamlining administrative processes to facilitate the delivery of diabetes self-management training, increasing patient engagement, ensuring access to affordable medications (including insulin), and regularly updating eligibility criteria for diabetes supplies, technologies, and devices.
At the practice level, the NCCC recommends developing capacity to support technology-enabled interventions, increasing access to virtual care for all patients with diabetes, and enhancing programs that support team-based care.
At the health system level, the NCCC recommends addressing health care workforce needs by directing training programs funded by the Department of Health and Human Services to identify workforce needs and to train individuals to meet those needs in the diabetes workforce and by implementing new payment models to sustain team-based care.
At the health policy level, the NCCC recommends providing insurance coverage at no out-of-pocket cost for high-value diabetes treatments and services and developing a quality measure that enhances patient safety by encouraging treatment deintensification in patients at high risk for severe hypoglycemia.
The NCCC also recommends that research be supported to identify and address barriers to uptake of diabetes self-management education and support, address digital connectivity as a social determinant of health, and identify methods to enhance team-based care (11,12).
Developing and Implementing a National Diabetes Strategy
The NCCC report provides the framework for a novel, comprehensive national strategy to prevent and treat diabetes. It includes specific recommendations for both non–health-related and health-related federal agencies to address the diabetes epidemic. An integral part of this strategy is to establish an Office of National Diabetes Policy (ONDP) (1,13). Modeled on the successful Office of National AIDS Policy, this office will leverage and coordinate work across health- and non–health-related federal agencies to positively change the social and environmental conditions that are enabling the type 2 diabetes epidemic. The NCCC recommends that the ONDP be established at a level above the Department of Health and Human Services and that it be provided with resources to facilitate its effectiveness and enable accountability. This Office will monitor and report progress on the implementation of the NCCC’s recommendations, coordinate federal policies and programs that impact diabetes prevention and control, and report to the Congress and the public on an annual basis. This National Diabetes Strategy should prioritize the following (1,13):
Ensuring that the policies and programs of both non–health-related and health-related federal agencies are coordinated to improve social and environmental conditions that contribute to diabetes incidence and adversely impact its treatment.
Ensuring that achieving health equity is a guiding principle for all federal policies and programs addressing diabetes.
Implementing policies to ensure that all Americans at risk for and with diabetes have access to comprehensive and affordable health care.
Expanding and strengthening policies and programs to increase awareness of and the diagnosis of prediabetes and the availability of, referral to, and insurance coverage for intensive lifestyle intervention programs for diabetes prevention.
Facilitating the Food and Drug Administration review and approval of metformin for diabetes prevention.
Increasing the size, makeup, and competence of the workforce to treat diabetes and its complications.
Implementing new payment models to support access to lifesaving medications and proven effective treatments for diabetes and its complications at no out-of-pocket cost.
Next Steps
Adopting the NCCC’s recommendations can substantially reduce diabetes incidence, complications, and costs in the U.S. However, enabling the frameshift needed to translate these recommendations into policy will require substantial political resolve (13). Some of the NCCC’s recommendations will require new legislation. Others will require administrative action and rulemaking at the level of agencies or departments. Still others, such as mandating front-of-package labeling, may require input from the Department of Justice.
Policy makers, diabetes stakeholders (including patient organizations and organizations of physicians, nurses, dietitians, social workers, diabetes educators, pharmacists, and nurse practitioners), health plans, health departments, community organizations such as the YMCA, and more and more Americans are recognizing how social and environmental conditions shape health. The COVID-19 pandemic has led many to reckon with the consequences of the nation’s failure to implement an all-of-government approach to disease prevention and treatment. By recommending health-in-all-policies and an equity-based approach to governance, and by making recommendations specific to non–health-related and health-related federal agencies, the NCCC Report has the potential to contribute to meaningful change. The potential costs and consequences of the federal government not comprehensively addressing diabetes prevention and treatment are substantial. The NCCC urges Congress and the Secretary of Health and Human Services to promptly implement the Commission’s recommendations to coordinate federal policies and programs to prevent and control diabetes, to protect the health and well-being of current and future generations of Americans at risk for diabetes, and to improve the health of millions of Americans with diabetes.
Article Information
Acknowledgments. The NCCC acknowledges Alicia A. Livinski and Nancy L. Terry, biomedical librarians from the National Institutes of Health Library, Division of Library Services, Office of Research Services, who performed the literature searches. The NCCC also thanks Yanni Wang (International Biomedical Communications) and Heather Stites (University of Michigan) for their editorial assistance.
Funding. The NCCC was supported through a Joint Funding Agreement among eight federal agencies: The Agency for Healthcare Research and Quality (AHRQ), the Centers for Disease Control and Prevention (CDC), the Centers for Medicare and Medicaid Services (CMS), the Food and Drug Administration (FDA), the Health Resources and Services Administration (HRSA), the Indian Health Service (IHS), the National Institutes of Health (NIH), and the Office of Minority Health (OMH). The Office of the Assistant Secretary for Health (OASH), the Office of Disease Prevention and Health Promotion (ODPHP), and the Office on Women’s Health (OWH) provided management staff and contractor support.
The funders had no role in the preparation, review, or approval of the manuscript or the decision to submit the manuscript for publication. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Health and Human Services or other departments and agencies of the federal government.
Duality of Interest. No potential conflicts of interest relevant to this article were reported.
Prior Presentation. Parts of this study were presented at the 82nd Scientific Sessions of the American Diabetes Association, New Orleans, LA, 3–7 June 2022.
Footnotes
C.P. was the Designated Federal Officer for the National Clinical Care Commission. All other authors were members of the National Clinical Care Commission.
Retired
This article is part of a special article collection available at https://diabetesjournals.org/collection/1586/The-Clinical-Care-Commission-Report-to-Congress.
References
- 1. Herman WH, Schillinger D, Bolen S, et al. The National Clinical Care Commission report to Congress: recommendations to better leverage federal policies and programs to prevent and control diabetes. Diabetes Care 2023;46:255–261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. National Clinical Care Commission . Report to Congress on Leveraging Federal Programs to Prevent and Control Diabetes and Its Complications, 2021. Chapter 1. Background. Accessed 19 July 2022. Available from https://health.gov/about-odphp/committees-workgroups/national-clinical-care-commission/report-congress
- 3. Hill-Briggs F, Adler NE, Berkowitz SA, et al. Social determinants of health and diabetes: a scientific review. Diabetes Care 2020;44:258–279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Herman WH, Bullock A, Boltri JM, et al. The National Clinical Care Commission report to Congress: background, methods, and foundational recommendations. Diabetes Care 2023;46:e14–e23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Lock K. Health impact assessment. BMJ 2000;320:1395–1398 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. National Clinical Care Commission . Report to Congress. Chapter 3. Foundational Recommendations to Address Diabetes. Accessed 19 July 2022. Available from https://health.gov/about-odphp/committees-workgroups/national-clinical-care-commission/report-congress
- 7. Schillinger D, Bullock A, Powell C, et al. The National Clinical Care Commission report to Congress: leveraging federal policies and programs for population-level diabetes prevention and control: recommendations from the National Clinical Care Commission. Diabetes Care 2023;46:e24–e38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. National Clinical Care Commission . Report to Congress on Leveraging Federal Programs to Prevent and Control Diabetes and Its Complications, 2021. Chapter 4. Population-Level Diabetes Prevention and Control. Accessed 19 July 2022. Available from https://health.gov/about-odphp/committees-workgroups/national-clinical-care-commission/report-congress
- 9. Boltri J, Tracer H, Strogatz D, et al. The National Clinical Care Commission report to Congress: leveraging federal policies and programs to prevent diabetes in people with prediabetes. Diabetes Care 2023;46:e39–e50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. National Clinical Care Commission . Report to Congress on Leveraging Federal Programs to Prevent and Control Diabetes and Its Complications, 2021. Chapter 5. Diabetes Prevention in Targeted Populations. Accessed 19 July 2022. Available from https://health.gov/about-odphp/committees-workgroups/national-clinical-care-commission/report-congress
- 11. Greenlee C, Bolen S, Chong W, et al. The National Clinical Care Commission report to Congress: leveraging federal policies and programs to improve diabetes treatment and reduce complications. Diabetes Care 2023;46:e51–e59 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. National Clinical Care Commission . Report to Congress on Leveraging Federal Programs to Prevent and Control Diabetes and Its Complications, 2021. Chapter 6. Treatment and Complications. Available from https://health.gov/about-odphp/committees-workgroups/national-clinical-care-commission/report-congress. Accessed 19 July 2022.
- 13. National Clinical Care Commission . Report to Congress on Leveraging Federal Programs to Prevent and Control Diabetes and Its Complications, 2021. Chapter 7. Looking Forward. Accessed 19 July 2022. Available from https://health.gov/about-odphp/committees-workgroups/national-clinical-care-commission/report-congress