Clinical guidelines recommend screening for prediabetes in asymptomatic adults ≤70 years of age (1,2). Three laboratory measurements are used for screening: HbA1c, fasting glucose (FG), and 2-h postload glucose. American Diabetes Association guidelines require two positive tests, either two different tests or repeated measures of the same test, to diagnose diabetes. However, only one positive test is recommended to diagnose prediabetes (2), resulting in a large and heterogenous population with prediabetes (3). It is unclear if a two-test approach could improve the specificity of prediabetes definitions in the general population. To better quantify prognosis in different definitions of prediabetes, we characterized patterns of progression from prediabetes to diabetes or remission to normoglycemia in the community-based Atherosclerosis Risk in Communities (ARIC) study. We also examined subsequent long-term morbidity and mortality associated with patterns of progression or remission.
We conducted an analysis of 7,926 adults without diabetes (aged 48–68 years) from the ARIC study visit 2 (V2) (1990–1992) and visit 4 (V4) (1996–1998). Participants were classified by impaired FG (IFG) 100–125 mg/dL and HbA1c 5.7–6.4% at V2. We calculated 6-year risk of progression to diabetes and regression to normoglycemia (FG <100 mg/dL and 2-h postload glucose <140 mg/dL).
For long-term outcomes, participants were classified by the V2 categories of HbA1c and FG and also by change in FG (the only glycemic marker available at both visits): 1) stable normal FG (NFG) (<100 mg/dL at both visits), 2) progression to IFG (<100 mg/dL at V2 but 100–125 mg/dL at V4), 3) remission of IFG (100–125 mg/dL at V2 but <100 mg/dL at V4), and 4) persistent IFG (100–125 mg/dL at both visits).
Participants were followed through 2019 (maximum 29.9 years) for incident diabetes, heart failure (HF), atherosclerotic cardiovascular disease (ASCVD), and mortality. Participants were followed through 2017 for kidney failure (KF) (permanent dialysis, kidney transplantation, or estimated glomerular filtration rate <15 mL/min/1.73 m2) from the U.S. Renal Data System. Incident diabetes was defined as self-report of physician-diagnosed diabetes or use of glucose-lowering medications during any follow-up visit or annual phone call.
Of 7,926 participants at V2, 57% had normoglycemia, 27% had isolated elevated FG, 6% had isolated elevated HbA1c, and 10% had elevations on both tests. Compared with normoglycemia, participants with elevations in both FG and HbA1c at V2 had the highest risk of long-term outcomes: hazard ratio (HR) 5.87 (95% CI 5.30–6.52) for diagnosed diabetes, 2.25 (95% CI 1.78–2.85) for KF, 1.75 (95% CI 1.54–1.98) for HF, 1.87 (95% CI 1.65–2.11) for ASCVD, and 1.46 (95% CI 1.34–1.58) for mortality.
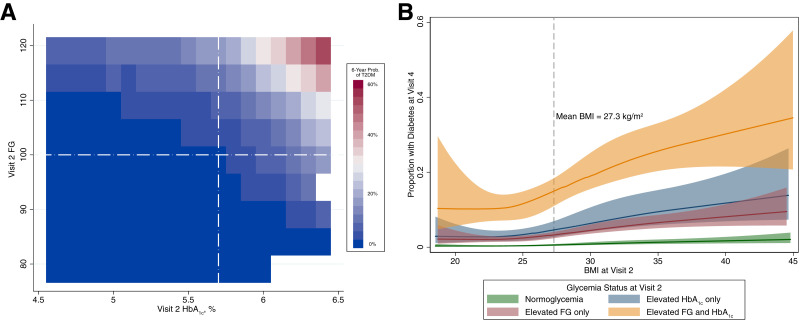
The 6-year risk of diabetes was 3.5% in participants with isolated IFG, 4.9% with isolated elevated HbA1c, and 15.2% with elevations in both. BMI was strongly associated with diabetes, particularly in people with IFG and elevated HbA1c (Fig. 1).
Figure 1.
Adjusted 6-year probability of progression to diabetes by FG and HbA1c (A) and glycemic status and BMI (B) from ARIC V2 (1990–1992) to V4 (1996–1998). Results were adjusted for age, sex, and race. Dashed lines represent cutoffs for prediabetes categories. T2DM, type 2 diabetes mellitus.
When evaluating progression of FG (V2 to V4), most (55%) had stable NFG, 20% had persistent IFG, 10% progressed from NFG to IFG, and 15% experienced remission of IFG. Compared with stable NFG, participants with remission of IFG had no increased risk of mortality (HR 1.02, 95% CI 0.92–1.14), KF (HR 0.81, 95% CI 0.54–1.22), HF (HR 1.02, 95% CI 0.86–1.22), or ASCVD (HR 1.06, 95% CI 0.89–1.26), but they did have higher risk of progressing to diagnosed diabetes (HR 1.99, 95% CI 1.72–2.31). Participants with persistent IFG had increased risk of mortality (HR 1.18, 95% CI 1.07–1.30), KF (HR 1.49, 95% CI 1.10–2.01), HF (HR 1.39, 95% CI 1.20–1.61), ASCVD (HR 1.29, 95% CI 1.10–1.50), and incident diabetes (HR 4.18, 94% CI 3.71–4.71).
A confirmatory definition of prediabetes (elevations in both FG and HbA1c) identified individuals most likely to develop diabetes and long-term clinical outcomes. A substantial portion of our study population with prediabetic FG had normal FG at the 6-year follow-up visit, and they did not have increased risk of most long-term outcomes.
Current definitions of prediabetes identify approximately one-third of the population (88 million U.S. adults in 2018) (4) as eligible for lifestyle interventions like the Diabetes Prevention Program. These programs have been shown to be cost-effective at preventing or delaying the development of diabetes and its complications (5), and they are being implemented nationally in the U.S. Given the number of people eligible for diabetes prevention programs, risk stratification may be useful for programs with limited resources. Our results suggest that using a confirmatory (two-test) definition of prediabetes (both elevated HbA1c and FG) identified individuals at highest risk for developing diabetes; the addition of BMI further improved risk stratification. A single elevated FG in middle-aged adults was common, tended to resolve, and was not highly prognostic of future disease. Requiring two elevations in measures of glycemia to define prediabetes improves risk stratification for future diabetes and major clinical outcomes.
Article Information
Funding. A.S.W. was supported by National Institutes of Health National Heart, Lung, and Blood Institute grant T32 HL007024. E.S. was supported by the National Institutes of Health National Heart, Lung, and Blood Institute grant K24 HL152440 and National Institutes of Health National Institute of Diabetes and Digestive and Kidney Diseases grant R01 DK089174. J.B.E.-T. was supported by the National Institutes of Health National Heart, Lung, and Blood Institute grant K23 HL153774.
Some of the data reported here were supplied by the U.S. Renal Data System. The interpretation and reporting of these data are the responsibility of the authors and in no way should be seen as an official policy or interpretation of the U.S. government.
Duality of Interest. No potential conflicts of interest relevant to this article were reported.
Author Contributions. A.S.W. conducted the analyses and wrote the initial manuscript. All authors reviewed and edited the manuscript and provided detailed feedback. A.S.W. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
References
- 1. Davidson KW, Barry MJ, Mangione CM, et al.; US Preventive Services Task Force . Screening for prediabetes and type 2 diabetes: US Preventive Services Task Force recommendation statement. JAMA 2021;326:736–743 [DOI] [PubMed] [Google Scholar]
- 2. American Diabetes Association Professional Practice Committee . 2. Classification and diagnosis of diabetes: Standards of Medical Care in Diabetes—2022. Diabetes Care 2022;45(Suppl. 1):S17–S38 [DOI] [PubMed] [Google Scholar]
- 3. Echouffo-Tcheugui JB, Selvin E. Prediabetes and what it means: the epidemiological evidence. Annu Rev Public Health 2021;42:59–77 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Centers for Disease Control and Prevention (CDC) . National Diabetes Statistics Report, 2020. Atlanta, GA, Centers for Disease Control and Prevention, U.S. Dept of Health and Human Services, 2020 [Google Scholar]
- 5. Aroda VR, Knowler WC, Crandall JP, et al.; Diabetes Prevention Program Research Group . Metformin for diabetes prevention: insights gained from the Diabetes Prevention Program/Diabetes Prevention Program Outcomes Study. Diabetologia 2017;60:1601–1611 [DOI] [PMC free article] [PubMed] [Google Scholar]