Abstract
Since the first Federal Commission on Diabetes issued its report in 1975, the diabetes epidemic in the U.S. has accelerated, and efforts to translate advances in diabetes treatment into routine clinical practice have stalled. In 2021, the National Clinical Care Commission (NCCC) delivered a report to Congress that provided recommendations to leverage federal policies and programs to more effectively prevent and treat diabetes and its complications. In the five articles in this series, we present the NCCC’s evidence-based recommendations to 1) reduce diabetes-related risks, prevent type 2 diabetes, and avert diabetes complications through changes in federal policies and programs affecting the general population; 2) prevent type 2 diabetes in at-risk individuals through targeted lifestyle and medication interventions; and 3) improve the treatment of diabetes and its complications to improve the health outcomes of people with diabetes. In this first article, we review the successes and limitations of previous federal efforts to combat diabetes. We then describe the establishment of and charge to the NCCC. We discuss the development of a hybrid conceptual model that guided the NCCC’s novel all-of-government approach to address diabetes as both a societal and medical problem. We then review the procedures used by the NCCC to gather information from federal agencies, stakeholders, key informants, and the public and to conduct literature reviews. Finally, we review the NCCC’s three foundational recommendations: 1) improve the coordination of non–health-related and health-related federal agencies to address the social and environmental conditions that are accelerating the diabetes epidemic; 2) ensure that all Americans at risk for and with diabetes have health insurance and access to health care; and 3) ensure that all federal policies and programs promote health equity in diabetes.
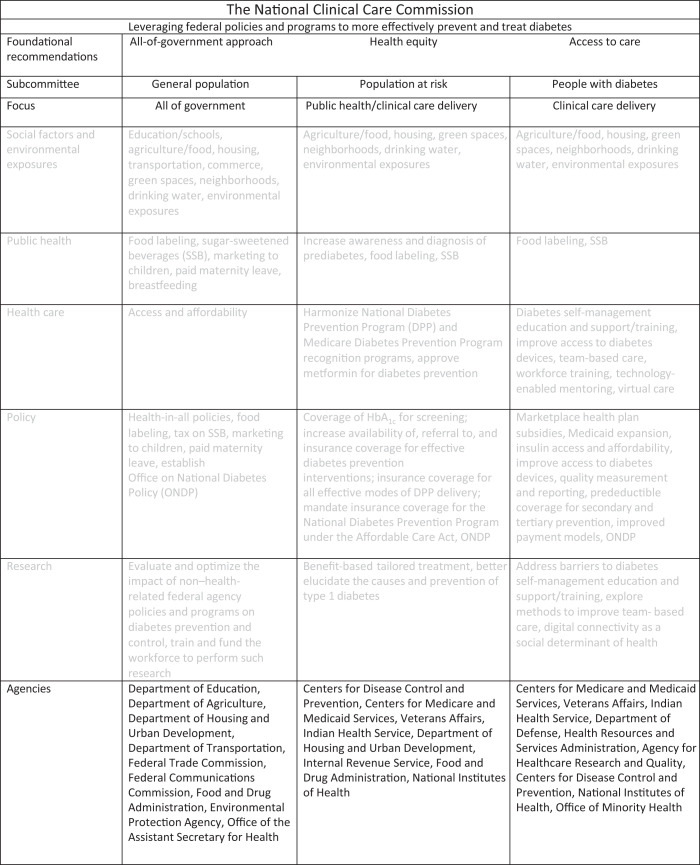
Graphical Abstract
Introduction
Someone in the U.S. is diagnosed with diabetes every 20 seconds. In 2021, more than 37 million Americans had diabetes (1–3). Of these, 28.7 million were diagnosed and 8.5 million were undiagnosed. In addition, 96 million American adults had prediabetes (2).
Diabetes is associated with unique complications that affect the eyes, kidneys, and nerves and increase the risk of cardiovascular disease, including stroke and myocardial infarction. Diabetes also contributes to death from cancer and infectious diseases (4). Indeed, diabetes increases the risk of death from COVID-19 by two- to threefold (5).
The costs of diabetes in the U.S. are enormous. In 2017, the total cost of diabetes was estimated to be $327 billion. This included $237 billion in direct medical costs (the costs of medical care for people with diabetes) and $90 billion in indirect costs (the costs to society of lost productivity due to illness, disability, and premature mortality) (2). Two-thirds of the direct costs of diabetes were paid by Medicare or Medicaid (6). Caring for people with diabetes in the U.S. accounts for one of every four health care dollars (6,7).
History of Federal Efforts to Combat Diabetes in the U.S.
In 1974, The National Diabetes Mellitus Research and Education Act (Public Law 93-354) established the National Commission on Diabetes. It formulated the Long-Range Plan to Combat Diabetes in the United States (8), which addressed diabetes as a medical condition requiring medical care. The Long-Range Plan had a profound impact on diabetes research and programs and on the treatment of diabetes and its complications. The National Institutes of Health (NIH) established Diabetes Research and Training Centers to conduct research on diabetes, support model care demonstration programs, expand the diabetes workforce, and provide continuing education. The Long-Range Plan also recommended that the NIH support the Diabetes Control and Complications Trial to test the glucose hypothesis, i.e., that hyperglycemia causes the microvascular complications of diabetes and that intensive glycemic management can prevent them (9). In addition, the Long-Range Plan established the National Diabetes Information Clearinghouse and the National Diabetes Data Group to provide accurate statistics on diabetes to support public policy. At the Centers for Disease Control and Prevention (CDC), the Long-Range Plan called for the creation of Diabetes Control Programs within state health departments that were subsequently expanded to all 50 states, the District of Columbia, and several U.S. territories. It also established diabetes health care, education, and control programs within the Veterans Health Administration and the Indian Health Service. Finally, it created the Diabetes Mellitus Interagency Coordinating Committee (DMICC) to share information and coordinate activities across several federal agencies.
Remaining Challenges and Emerging Threats
It is now recognized that social and environmental factors influence the risk of type 2 diabetes and its treatment and that these factors must be addressed by federal policies and programs (10). Individuals who have less education, lower incomes, less wealth, food and housing insecurity, and who live in rural areas have higher rates of type 2 diabetes and higher rates of diabetes complications. Rates of type 2 diabetes are higher in physical environments that lack playgrounds, parks, and walkability and in areas that expose people to environmental toxins. Poor social cohesion, marginalization, historical trauma, and structural racism also contribute to the diabetes epidemic by increasing exposure to unhealthy environments and conditions (11,12).
In addition, efforts to translate advances in diabetes treatment into routine clinical practice have stalled (13). Only one in four adults with diabetes achieves recommended standards of diabetes care (14), and this level of performance has remained essentially unchanged for a decade (15). In addition, improvements in diabetes care have not been evenly distributed across the U.S. population (11). The same lower-income individuals and racial and ethnic groups that experience higher diabetes prevalence have higher rates of preventable, severe, and costly complications, including blindness, kidney failure, amputations, myocardial infarctions, and strokes. In high-income countries like the U.S., more than half of the preventable burden of diabetes is attributable to nonclinical social and environmental factors (16,17). The other half is attributable to lack of access to affordable, quality care and to failings in the design of the health care delivery system (16,17), one that is more geared to reactive, acute care than to proactive, team-based preventive care.
Establishment of and Charge to the NCCC
Because it had been nearly 50 years since the first National Commission on Diabetes issued its report, the U.S. Congress recognized the urgent need to reassess and update the federal response to the diabetes epidemic. In 2018, in response to the National Clinical Care Commission Act (Public Law 115–80), the Secretary of Health and Human Services established the NCCC to provide recommendations to leverage federal policies and programs to more effectively prevent and control diabetes and its complications (18). The NCCC included 12 private-sector members with expertise in medicine, nursing, pharmacy, patient advocacy, and public health and 11 individuals representing federal agencies, including the Agency for Healthcare Research and Quality (AHRQ), the CDC, the Centers for Medicare and Medicaid Services (CMS), the Department of Defense (DoD), the Department of Veterans Affairs (VA), the Food and Drug Administration, the Health Resources and Services Administration, the Indian Health Service, the NIH, the Office of Minority Health, and the U.S. Department of Agriculture (USDA).
The NCCC was charged with evaluating and making recommendations to Congress and the Secretary of Health and Human Services regarding:
Federal programs that focus on preventing and reducing the incidence of diabetes in the U.S.
Current activities and gaps in federal policies and programs to support clinicians in providing integrated, high-quality care to individuals with diabetes and its complications.
Improvement in, and improved coordination of, federal education and awareness activities related to the prevention and treatment of diabetes and its complications, including the appropriate use of new and existing technologies.
Methods for outreach and dissemination of education and awareness materials funded by the federal government.
Opportunities for consolidation of inappropriately overlapping or duplicative federal programs related to diabetes and its complications.
The NCCC’s Approach to Its Charge
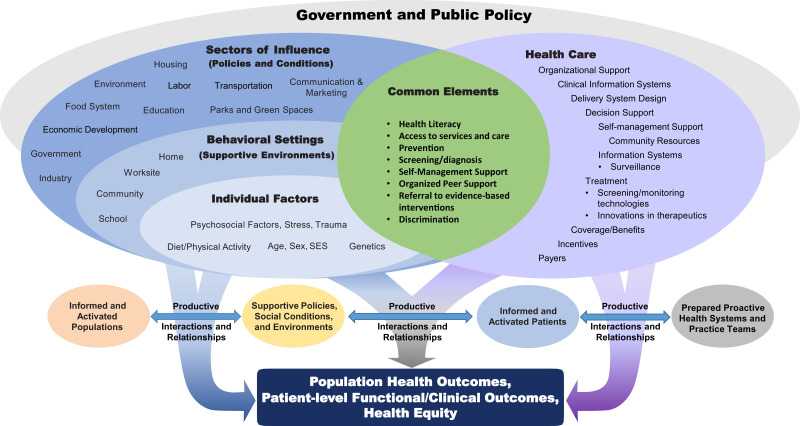
Early on, the NCCC recognized that diabetes is both a societal problem requiring a trans-sectoral all-of-government approach to prevention and treatment and a health condition requiring complex medical care. Accordingly, the NCCC approached its duties using a framework that combined elements of the Socioecological Model (19) and the Chronic Care Model (20) (Fig. 1).
Figure 1.
The NCCC framework for diabetes prevention and control: the combined Socioecological Model and Chronic Care Model for diabetes. SES, socioeconomic status.
The Socioecological Model highlights ways in which social factors, environmental exposures, community attributes, and group characteristics interact to influence the health of individuals. Preventing and successfully treating diabetes and its complications requires supportive environments and salutary social conditions at multiple levels and in many settings. Success also hinges on individuals having access to comprehensive, affordable, and high-quality health care. The Chronic Care Model identifies six categories of clinical practice change that can lead to improvements in health outcomes for people with diabetes. While these two models have distinct elements, some elements are common to both, including health literacy, access to services, self-management support, organized peer support, and mitigating the negative impact of discrimination.
The logic of the NCCC’s framework is that diabetes can be prevented and controlled only by supportive policies and programs that improve social conditions and environments, prepared and proactive health systems, and practice teams that provide accessible, high-quality care. The NCCC thus sought to make recommendations to improve diabetes-related population health, improve clinical outcomes and quality-of-life for individuals at risk for and with diabetes and ensure greater diabetes-related health equity.
Methods
The NCCC formed three subcommittees focused on 1) population-wide strategies to prevent and control diabetes; 2) targeted diabetes prevention strategies for individuals with prediabetes; and 3) the treatment of diabetes and its complications in individuals with diabetes. The subcommittees gathered information from federal agencies, stakeholders, key informants, and the public; conducted systematic searches and reviews of the scientific literature; and drafted preliminary recommendations. The next three articles in this series summarize the findings and recommendations of each subcommittee. The final article summarizes the conclusions and recommendations of the NCCC. Some of the issues identified by the NCCC were relevant to all types of diabetes, and some were specific to type 1 or type 2 diabetes. For recommendations relevant to all types of diabetes, the term “diabetes” has been used. For recommendations relevant only to type 1 or type 2 diabetes, those terms have been used.
The NCCC reviewed programs and policies of federal departments and agencies that support diabetes-related public health efforts, perform administrative roles that impact diabetes care, deliver or pay for health care, and conduct diabetes-related research. Recognizing that the diabetes epidemic in the U.S. is driven in part by social, economic, and environmental factors, the NCCC also obtained information from non–health-related federal agencies whose policies and programs affect diabetes risk and outcomes. Health-related and non–health-related federal agencies contacted and interviewed by the NCCC are listed in Supplementary Table 1.
In 2019, to gather information, the NCCC developed a survey and distributed it to nine health-related and three non–health-related federal agencies, including the USDA, DoD, and the Federal Bureau of Prisons. The survey solicited information about policies and programs relevant to diabetes and any evaluations of their impact. The three subcommittees reviewed agencies’ responses and, when needed, sought clarifications and requested additional information. The subcommittees also requested information about programs and policies from other agencies and departments that did not receive the survey (Supplementary Table 1).
The subcommittees identified stakeholder organizations whose missions overlapped the NCCC’s charge and sought their input through conference calls and written communication. The subcommittees also consulted with key informants whose subject matter expertise was relevant to the work of the NCCC. Between 2019 and May 2021, the NCCC received presentations from more than 50 key informants using both teleconferencing methods and written communications. Each subcommittee also developed a list of questions to guide literature searches relevant to their focus areas. Librarians at the National Library of Medicine conducted the searches, and the subcommittees reviewed the relevant publications.
The three subcommittees met regularly and used an iterative process to develop recommendations. The subcommittees reported their progress, shared their findings, and presented draft recommendations at public meetings. All recommendations addressed federal policies and programs and were prioritized according to strength of evidence, the recommendations’ reach and scope, practicability, likely effectiveness and safety, affordability, and impact on health equity. In compliance with the Federal Advisory Committee Act requirements, all deliberations that involved the entire NCCC were open to the public. Twelve such meetings took place. In addition, the NCCC sought public input through Federal Register Notices, written comments submitted prior to public meetings, verbal presentations at NCCC meetings, and e-mail comments sent directly to the NCCC. The NCCC reviewed all public comments to inform their recommendations and, when appropriate, responses were integrated into its report. The subcommittees presented and received feedback on their near-final recommendations at the NCCC’s next-to-last public meeting on 22 June 2021, and at its final public meeting on 8 September 2021, the NCCC reviewed and voted unanimously to approve the final recommendations (21).
Foundational Recommendations to Address Diabetes Prevention and Treatment
Historically, the prevention and treatment of diabetes have been considered medical problems requiring medical interventions. In its deliberations, the NCCC concluded that many other factors beyond the clinical care setting impact diabetes prevention and treatment and contribute to health disparities, including social determinants of health (SDOH), lack of engagement and collaboration across health-related and non–health-related federal agencies, and barriers to access to health care. Accordingly, the NCCC made three foundational recommendations to 1) address social and environmental factors through trans-agency engagement and collaboration; 2) promote access to health care; and 3) advance health equity in diabetes.
Focus Area 1: Address SDOH by Improving Engagement and Coordination Across Federal Agencies
Background
To improve population health and reduce health disparities, SDOH, defined as the economic and social conditions that influence differences in health status, must be addressed at the individual, organizational, and policy levels (20). In 2020, the American Diabetes Association described the associations between SDOH and diabetes risk and outcomes (10), including potential mechanisms whereby SDOH can contribute to diabetes and its complications. That scientific review focused on socioeconomic position, health literacy, the food environment and food insecurity, and neighborhood and physical environments. While some of the mechanisms underlying the connection between these factors and health outcomes are still being elucidated, the NCCC recognized that the policies and programs of federal agencies profoundly affect SDOH and that improving social and environmental conditions can advance efforts to prevent and control diabetes. The NCCC also recognized that exposure to unhealthy social conditions and environments, and the attendant higher burden of diabetes, is one of the consequences of structural racism, i.e., the ways in which societies foster racial discrimination through discriminatory systems of education, economic opportunity, employment, and housing. Some have viewed racial discrimination as a thing of the past. Unfortunately, this view overlooks the impact of past practices on contemporary practices in both the public and private sectors and ignores the fact that many forms of discrimination still exist. Many of the NCCC’s recommendations address the consequences of structural racism and provide concrete, feasible, and promising approaches likely to advance health equity and improve population health (22). Accordingly, in addressing SDOH, the NCCC considered a number of relevant factors that are described below.
Socioeconomic Position
Education, wealth, income, and occupation are strong predictors of the onset of type 2 diabetes and the progression of diabetes (10). In the U.S., the age-adjusted prevalence of diagnosed diabetes is 75% higher for those with less than a high school education and 33% higher for those with a high school education compared with those with more than a high school education. Compared with those with high incomes, the prevalence of diabetes is 100% higher for those classified as poor, 74% higher for those classified as near poor, and 40% higher for those classified as middle income. Similarly, employment status (employed vs. unemployed), job stability, job type, and working conditions show graded associations with diabetes prevalence and complications. County-level unemployment and poverty are associated with a higher incidence of diabetes, and counties with more exercise opportunities, greater access to healthy food, and higher availability of primary care physicians have lower incidences of diabetes (23). Rural areas have a higher age-adjusted prevalence of diabetes than urban areas, and adults with diabetes in rural areas have had less improvement in cardiovascular risk factors over time and lower access to preventive services than their urban counterparts (24). Finally, low income and lack of access to maternity leave in the workplace present a potent barrier to maternal breastfeeding. Higher breastfeeding rates and greater breastfeeding duration are associated with less obesity in offspring and reductions in incident type 2 diabetes in postpartum women across the life span (25,26).
Health Literacy
Health literacy is defined as the degree to which individuals can find, understand, and use information and services to inform health-related decisions and actions (27,28). The relationships between SDOH, health literacy, and disparities in diabetes incidence and outcomes are well described (27). Limited health literacy independently contributes to type 2 diabetes incidence. Among individuals with diabetes, it is also associated with worse diabetes control and higher complication rates. Nearly half of individuals with diabetes have limited health literacy. High rates of limited health literacy are observed in racial and ethnic groups that are disproportionately affected by diabetes, those with language barriers and limited educational attainment, and among individuals with diabetes who are beneficiaries of federally funded programs including Medicaid and Medicare (29,30). Individuals with limited health literacy have less awareness of evidence-based strategies to prevent diabetes and less awareness of and ability to implement evidence-based strategies to manage their diabetes and prevent complications (31).
The Food Environment
Key dimensions of the food environment include food availability, accessibility, affordability, and quality as well as the marketing and commercial influences that drive consumption. The food environment influences individuals’ food and beverage choices, diet quality, and nutritional status (10). Marginalized communities are more likely to have poor access to healthy foods and abundant access to calorie-dense foods that are low in nutritional quality. They are also more likely to be exposed to the marketing of such foods. Greater access to healthy food outlets, higher availability of grocery stores and full-service restaurants, and lower availability of convenience stores and fast-food restaurants are associated with lower rates of type 2 diabetes (10).
Food Insecurity
Food insecurity (32,33) (the limited or uncertain ability to reliably access safe and nutritious food) is now recognized as a common and potent risk factor for developing type 2 diabetes and diabetes complications and as a contributor to socioeconomic, racial, and ethnic disparities in diabetes outcomes. Food insecurity compels individuals and families to consume low-cost and calorie-dense foods that increase the risk of type 2 diabetes and make the clinical management of diabetes more challenging (34–36). Food insecurity also forces individuals with diabetes to make difficult choices about paying for food, housing, monitoring devices, medicines, and medical care (33,37,38). Finally, abnormal metabolic programming associated with maternal undernutrition and poor dietary quality can result in trans-generational transmission of susceptibility to obesity and type 2 diabetes (39).
The Built Environment
The neighborhoods and physical environments in which people live, learn, work, and play have major impacts on their health. Greater neighborhood walkability and greater access to green spaces are associated with physical activity and diabetes outcomes (40–43). Residential segregation by socioeconomic position, race, and ethnicity produces patterns of unequal resource distribution that create and perpetuate health inequities.
Housing instability refers to a spectrum of conditions that range from homelessness, evictions, frequent moves, and trouble paying rent to living in crowded conditions. Housing instability makes it difficult to attend to preventive services and self-care and leads to worse prevention and control of diabetes and higher likelihood of complications (44–46). In 2020, over 580,000 people in the U.S. were homeless. In 2020, African Americans, who made up 14% of the U.S. population, accounted for 39% of people experiencing homelessness; Hispanics or Latinos, who made up 19% of the U.S. population, accounted for 23% of the homeless population (47). Among individuals with diabetes seen in community health centers, over one-third reported housing instability (48). In the VA health care system, veterans with diabetes who experienced homelessness had significantly worse glucose control than those who were housed (46). The landmark study of federally subsidized housing, Moving to Opportunity, demonstrated that moving from a neighborhood with a high level of poverty to one with a lower level of poverty was associated with a lower incidence of obesity and diabetes (49).
The Ambient Environment
Toxic environmental exposures are also associated with diabetes risk and complications. Exposures can be naturally occurring (e.g., arsenic in well water) or introduced into the environment through human activity (e.g., air pollution, industrial waste, exposure to endocrine-disrupting chemicals, and secondhand smoke) (50–54). Marginalized communities in the U.S. are disproportionately exposed to environmental agents associated with diabetes (55–57). Explanatory factors include closer proximity of these neighborhoods to pollution sources, poorer enforcement of regulations, and inadequate responses to community complaints. Industrial pollution of private wells is a major source of water contamination in American communities (58), and lead contamination of tap water is more prevalent in communities of color. Such contamination undermines efforts to promote drinking water rather than sugar-sweetened beverages. Chemicals from canned foods and plastic packaging and from skin and hair care products are important sources of exposure to endocrine-disrupting chemicals linked to diabetes (51,54).
The Role of Non–Health-Related Federal Agencies
To prevent and control diabetes and to reduce health disparities, changes must take place in the social and environmental contexts in which people live, learn, work, and play. Implementing changes only in those federal agencies that are accountable for health care concerns is not sufficient to address diabetes. Federal departments and agencies considered to be “non–health-related” but that have a role in shaping social and environmental conditions that influence population health must also be involved. These include agencies responsible for domains as varied as food and agriculture, education, housing, transportation, trade, commerce, and criminal justice. This inclusive “all-of-government approach” underlies the NCCC’s recommendations.
While some developed countries affirmatively addressed diabetes through trans-sectoral governmental activities, the U.S. has not. The U.S. generally lacks structures, policies, and practices to coordinate strategic planning across health- and non–health-related agencies. As a result, many non–health-related federal agencies may implement policies and programs that are antithetical to the missions and objectives of health-related federal agencies. To date, the federal government has not articulated health considerations or integrated them into non–health-related agency policies and programs. What little work has been done to facilitate trans-agency collaboration around diabetes prevention and treatment has been of a pilot nature and has lacked scale. A “health-in-all policies” approach can promote diabetes prevention and control by incorporating health considerations into policy decision-making across sectors with the goal of ensuring that decision makers are informed about the health, equity, and sustainability consequences of policies during the policy development process. The approach is based on the premise that health outcomes are dependent on social and environmental conditions shaped by decisions outside the health sector. Incorporating health and health equity considerations into decision-making across sectors requires changes in government organization and processes to facilitate intersectoral collaboration. A health-in-all policies approach takes into account the health implications of policy decisions, seeks synergies between health-related and non–health-related agencies, and avoids harmful health impacts and health inequities that can arise from the decisions of non–health-related agencies. Past successes of health-in-all policies include efforts to fluoridate tap water, restricting tobacco use in workplaces and public spaces, and requiring the use of seat belts and child car seats (59).
Health impact assessments are an evidence-based method to promote the health-in-all policies approach. Health impact assessments use an array of data sources, analytic methods, and inputs to determine the potential effects of proposed non–health-related policies, programs, and projects on the health of the entire population and the distribution of health across subpopulations.
The CDC has previously recommended that state and local governments adopt a health-in-all policies approach, but there has been no targeted or sustained effort to advance such an agenda at the federal level. There is no mandate that health impact assessments be considered at the legislative stage or that federal agencies adopt a health-in-all policies approach at the rulemaking stage. One example of this problem is the USDA Farm Bill, which authorizes support for major commodity crops including wheat, corn, rice, soybeans, peanuts, and sugar, but provides relatively little support for production of so-called specialty crops, including fresh fruits and vegetables. A similar problem has been identified in how the Department of Transportation funds infrastructure for automobiles versus bicycles and pedestrians.
The NCCC determined that the federal government can play a larger role in preventing and controlling diabetes by ensuring that non–health-related federal agencies conduct health impact assessments and consider their results when implementing policies, programs, and projects. The federal government should also ensure that non–health-related and health-related federal agencies establish methodologies for health impact assessments, develop and train the workforce needed to carry out health impact assessments, receive resources to conduct them, and determine mechanisms to adjudicate and implement them.
Coordination Across Federal Agencies
Currently, no federal entity is charged with leading trans-agency efforts to prevent and control diabetes. Originally mandated by Public Law 93–354 (60) and established in 1975 by the National Commission on Diabetes (61), the DMICC is chaired by the NIH’s National Institute of Diabetes and Digestive and Kidney Diseases to facilitate communication, collaboration, and coordination on diabetes-related policies, programs, and projects among federal agencies and to ensure that research activities are not duplicated. However, the DMICC includes only select agencies from the Department of Health and Human Services and the VA and only two non–health care-related departments (USDA and DoD) (61). While the DMICC has fostered diabetes education and biomedical, clinical, and translational research, it does not have authority over the participating agencies, and it lacks statutory authority to develop or implement a national diabetes strategy or action plan to leverage and coordinate the work of health-related and non–health-related federal agencies. In contrast, the Office of National AIDS Policy was established in 1993 as part of the White House Domestic Policy Council and was tasked with coordinating an integrated approach to the prevention and treatment of HIV/AIDS in the U.S. As such, the Office of National AIDS Policy works closely with many non–health-related federal agencies, such as the Department of Justice, the Department of Labor, and the Department of Housing and Urban Development, to achieve the goals of the National HIV/AIDS Strategy and end the HIV epidemic in the U.S.
The NCCC made the following foundational recommendation.
The NCCC recommends the creation of an Office of National Diabetes Policy (ONDP) to develop and implement a National Diabetes Strategy. This office will leverage and coordinate work across federal departments and agencies to positively change the social and environmental conditions that are enabling the type 2 diabetes epidemic. The NCCC further recommends that the ONDP be established at a level above the Department of Health and Human Services and that it be provided with resources to facilitate its effectiveness and accountability.
The ONDP should include, but not be limited to, departments and agencies outlined in the NCCC Report to Congress, including the USDA, the Department of Transportation, the Department of Education, the Department of Justice, the DoD, the Department of Labor, the Department of the Treasury, the Federal Trade Commission, the Federal Communications Commission, the Department of Housing and Urban Development, the Federal Bureau of Prisons, the Environmental Protection Agency, the Bureau of Indian Education, the Bureau of Indian Affairs, the VA, and the Department of Health and Human Services, among others.
ONDP’s responsibilities should include 1) overseeing the implementation and monitoring of the NCCC’s recommendations; 2) ensuring action, collaboration, and coordination among federal agencies with respect to trans-agency approaches to delaying, preventing, and controlling diabetes; 3) making recommendations to the executive and legislative branches regarding actions they can take to delay, prevent, and better treat type 2 diabetes; 4) advancing a health-in-all-policies agenda with respect to diabetes; and 5) providing resources and employing health impact assessments for relevant policies across non–health-related departments and agencies.
The Department of Health and Human Services should also establish an entity within the Office of the Secretary of the Department of Health and Human Services to 1) coordinate work across the Department of Health and Human Services to better prevent and treat diabetes; and 2) serve in the ONDP to foster broad, trans-agency collaborative work between federal agencies to positively impact the social and environmental contexts that are driving the type 2 diabetes epidemic.
Additional, specific, agency-level recommendations related to population-wide policies and programs are detailed in the article by Schillinger et al. (62).
Focus Area 2: Ensure Access to Health Care
Background
Access to health care refers to the degree to which individuals and groups can obtain needed services from the health care system. In the U.S., health insurance coverage impacts both individuals’ ability to access health care and their health outcomes. In people at risk for or with diabetes, health insurance and access to health care are critical to reducing the incidence of diabetes, ensuring the early detection of diabetes, reducing the adverse health effects of diabetes, and prolonging life (63,64).
In the U.S., health insurance is pluralistic. Historically, its foundation was employer-based coverage for working families. Most working-age adults obtained health insurance coverage for themselves and their dependents as a benefit of employment. After 1965, Medicaid and State Children’s Health Insurance Programs covered the poor, and Medicare covered virtually all Americans 65 years of age and older and younger people who were medically disabled. This patchwork system left substantial numbers of Americans uninsured including employed workers whose employers did not provide health insurance coverage, the near poor who worked but earned too much to be eligible for Medicaid, and the poor who did not meet Medicaid coverage requirements. Many, but not all, of these gaps in access to health insurance were addressed by the Affordable Care Act (ACA).
The ACA had its intended impact on expanding health insurance coverage among people with diabetes. From 2009 to 2016, 770,000 U.S. adults 18–64 years of age with diabetes gained health insurance (65). Insurance coverage improved for nearly all demographic subgroups with diabetes, including men, women, non-Hispanic White people, non-Hispanic Black people, Hispanic people, those who were married, those with less than and more than a high school education, and those with family incomes less than $35,000. Coverage increased among people treated with diabetes medications and among those with diabetes complications (65). Insurance coverage for adults 26–64 years of age with diagnosed diabetes increased from 85% to 95% and from 75% to 92% for those with undiagnosed diabetes. Among those with diabetes and low incomes, insurance coverage increased from 67% to 94% (66). For those 65 years of age and older, coverage remained stable at 99.5%, indicating the ongoing success of the Medicare program (65). Analyses of health insurance coverage in the general population 8 years after the ACA confirmed that fewer Americans were uninsured and that coverage gaps in health insurance were shorter (67). Nevertheless, in 2019, 31 million people, or 9.5% of the U.S. population, remained uninsured (68).
Both poor diabetes control and poor blood pressure control are more frequent among uninsured people than among insured people with diabetes (69). Compared with insured people, uninsured people with diabetes are more than twice as likely to have HbA1c >9%, indicating poor glucose control. Improvements in health outcomes, including survival and reductions in health disparities, have also been demonstrated for older adults with diabetes as a result of entering the Medicare program (64).
Despite gains in insurance, income-related disparities in health outcomes have widened over time, likely exacerbated by increasing income inequality in the U.S. (70). Compared with adults with higher incomes, U.S. adults with lower incomes report skipping 23% more doctor visits, tests, treatments, or prescription medicines because of cost (71). Nonadherence to medical care such as medications and other treatments due to cost has been reported in 20% to 40% of people with diabetes. For those with self-reported financial insecurity, the nonadherence rate is 60% (72).
The COVID-19 pandemic highlighted additional problems with access to health care in the U.S. During the early months of the pandemic, 21.9 million Americans lost their jobs or left the workforce and 5.4 million of them became uninsured. Although some people who lost their employer-sponsored health insurance were able to receive insurance through state-based exchanges, the federal government initially declined to open its marketplace exchanges to offer special enrollment periods and declined to account for income changes to provide subsidies. Federal exchanges for marketplace health plans must offer enrollment opportunities for individuals whose employment status changes and subsidies for those whose financial circumstances change.
The COVID-19 pandemic also highlighted problems with the Medicaid program (73). At the time of this publication, 12 states have elected not to expand Medicaid eligibility, creating a “coverage gap” for adults who have incomes above their states’ eligibility for Medicaid but below the level of income making them eligible for tax credits to purchase health insurance through the marketplace (74). In 2019, more than 2.2 million adults in the U.S. fell into the insurance coverage gap (74). Ninety-seven percent of them lived in the southern U.S.: 35% in Texas, 19% in Florida, 12% in Georgia, and 10% in North Carolina (74). Low-income individuals in the coverage gap were more likely to be Black (74,75).
Taken together, these findings highlight the importance of access to affordable health care for people at risk for or with diabetes. Great strides have been made under the ACA, but important gaps remain. To address those gaps, access to employer-sponsored health insurance coverage must be improved, the coverage and affordability of individual marketplace health insurance plans must be improved, and, while not a federal decision, Medicaid eligibility must be expanded in all 50 states.
Preventing and successfully treating diabetes is possible only if individuals have access to comprehensive, high-quality, and affordable health care. Access to health care is foundational to improving health outcomes for people with or at risk for diabetes and is essential to efforts to ensure health equity.
The NCCC recommends that federal policies and programs be designed to ensure that all people at risk for and with diabetes have access to comprehensive, high-quality, and affordable health care and that no one at risk for or with diabetes who needs health care will be denied it because of cost.
Focus Area 3. Promote Health Equity in Diabetes
Rationale
Although addressing social and environmental conditions through trans-agency collaboration and providing access to health care will help to prevent and control diabetes, attention must also be paid to the ways in which policies and programs can be leveraged to promote diabetes-related health equity. Currently, few federal policies and programs are designed to narrow inequities in health, and some inadvertently increase disparities. For example, the CMS policies governing the accreditation of Diabetes Self-Management Training (DSMT) programs may exacerbate health disparities for Medicare beneficiaries. Diabetes is primarily managed by affected individuals, their families, and caregivers, and DSMT can help each of them make better care decisions (76). Unfortunately, the administrative burden associated with establishing and maintaining DSMT programs and the low reimbursement rates create barriers to the availability and sustainability of DSMT programs and result in disparities based on race (i.e., lower uptake for non-White individuals), health status (e.g., lower uptake for those with comorbidities) (77), and residence (e.g., fewer accredited programs in rural communities). Indeed, 62% of rural counties lack any DSMT program (78).
On 20 January 2021, President Joe Biden issued an Executive Order on Advancing Racial Equity and Support for Underserved Communities Through the Federal Government (79). The NCCC supports this presidential action and recommends additional actions consistent with that executive order.
The NCCC recommends that achieving health equity be a component of all federal policies and programs that affect people at risk for or with diabetes. Specifically, the NCCC recommends the following:
Federal agencies consider and evaluate the impact on health disparities of all new, all revised, and selected existing policies and programs that affect diabetes prevention, diabetes, and the complications of diabetes.
Federal agencies ensure the collection and use of data to assess the impact of those policies and programs on health disparities and modify the policies and/or programs as needed to reduce health disparities.
Summary
We have presented the background and methods used by the NCCC to address its charge. We have also described three cross-cutting and foundational recommendations that are integral to the NCCC’s report: 1) improve collaboration across non–health-related and health-related federal departments and agencies to improve social and environmental conditions; 2) ensure health insurance and access to health care for all Americans at risk for and with diabetes; and 3) promote health equity across federal programs and policies that impact populations at risk for and with diabetes. Subsequent articles in this series will focus on specific recommendations that impact the general population to reduce the burden of diabetes, that target populations at higher risk for diabetes to prevent or delay the onset of diabetes, and that target populations with established diabetes to improve diabetes treatment and reduce complications. Enacting these recommendations will improve the extent to which federal policies and programs can be leveraged to more effectively prevent and control diabetes and its complications.
Article Information
Acknowledgments. The NCCC acknowledges Alicia A. Livinski and Nancy L. Terry, biomedical librarians from the National Institutes of Health Library, Division of Library Services, Office of Research Services, who performed the literature searches. The NCCC also thanks Yanni Wang (International Biomedical Communications) and Heather Stites (University of Michigan) for their editorial assistance.
Funding. The NCCC was supported through a Joint Funding Agreement among eight federal agencies: The Agency for Healthcare Research and Quality (AHRQ), the Centers for Disease Control and Prevention (CDC), the Centers for Medicare and Medicaid Services (CMS), the Food and Drug Administration (FDA), the Health Resources and Services Administration (HRSA), the Indian Health Service (IHS), the National Institutes of Health (NIH), and the Office of Minority Health (OMH). The Office of the Assistant Secretary for Health (OASH), the Office of Disease Prevention and Health Promotion (ODPHP), and the Office on Women’s Health (OWH) provided management staff and contractor support.
The funders had no role in the preparation, review, or approval of the manuscript or the decision to submit the manuscript for publication. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Health and Human Services or other departments and agencies of the federal government.
Duality of Interest. No potential conflicts of interest relevant to this article were reported.
Prior Presentation. Parts of this study were presented at the 82nd Scientific Sessions of the American Diabetes Association, New Orleans, LA, 3–7 June 2022.
Footnotes
This article contains supplementary material online at https://doi.org/10.2337/figshare.21494160.
C.P. was the Designated Federal Officer for the National Clinical Care Commission. All other authors were members of the National Clinical Care Commission.
Retired
This article is part of a special article collection available at https://diabetesjournals.org/collection/1586/The-Clinical-Care-Commission-Report-to-Congress.
References
- 1. Wang L, Li X, Wang Z, et al. Trends in prevalence of diabetes and control of risk factors in diabetes among US adults, 1999-2018. JAMA 2021;326:1–13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Centers for Disease Control and Prevention . National Diabetes Statistics Report. Accessed 12 October 2022. Available from https://www.cdc.gov/diabetes/data/statistics-report/index.html
- 3. Centers for Disease Control and Prevention . Prevalence of Both Diagnosed and Undiagnosed Diabetes, 2020. Accessed 19 August 2021. Available from https://www.cdc.gov/diabetes/data/statistics-report/diagnosed-undiagnosed-diabetes.html
- 4. Coughlin SS, Calle EE, Teras LR, Petrelli J, Thun MJ. Diabetes mellitus as a predictor of cancer mortality in a large cohort of US adults. Am J Epidemiol 2004;159:1160–1167 [DOI] [PubMed] [Google Scholar]
- 5. Shang L, Shao M, Guo Q, et al. Diabetes mellitus is associated with severe infection and mortality in patients with COVID-19: a systematic review and meta-analysis. Arch Med Res 2020;51:700–709 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. American Diabetes Association . Economic costs of diabetes in the U.S. in 2017. Diabetes Care 2018;41:917–928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Dieleman JL, Baral R, Birger M, et al. US spending on personal health care and public health, 1996-2013. JAMA 2016;316:2627–2646 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. National Commission on Diabetes . Report of the National Commission on Diabetes to the Congress of the United States: the long-range plan to combat diabetes. Vol. I, 1975. https://babel.hathitrust.org/cgi/pt?id=uc1.31210023083353&view=1up&seq=4&skin=2021
- 9. Nathan DM, Genuth S, Lachin J, et al.; Diabetes Control and Complications Trial Research Group . The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med 1993;329:977–986 [DOI] [PubMed] [Google Scholar]
- 10. Hill-Briggs F, Adler NE, Berkowitz SA, et al. Social determinants of health and diabetes: a scientific review. Diabetes Care 2020;44:258–279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Golden SH, Joseph JJ, Hill-Briggs F. Casting a health equity lens on endocrinology and diabetes. J Clin Endocrinol Metab 2021;106:e1909–e1916 [DOI] [PubMed] [Google Scholar]
- 12. Lewis ME, Volpert-Esmond HI, Deen JF, Modde E, Warne D. Stress and cardiometabolic disease risk for indigenous populations throughout the lifespan. Int J Environ Res Public Health 2021;18:1821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. NCQA/HEDIS . Comprehensive Diabetes Care (CDC). Accessed 24 June 2022. Available from https://www.ncqa.org/hedis/measures/comprehensive-diabetes-care/
- 14. Chen Y, Rolka D, Xie H, Saydah S. Imputed state-level prevalence of achieving goals to prevent complications of diabetes in adults with self-reported diabetes–United States, 2017-2018. MMWR Morb Mortal Wkly Rep 2020;69:1665–1670 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Ali MK, Bullard KM, Gregg EW, Del Rio C. A cascade of care for diabetes in the United States: visualizing the gaps. Ann Intern Med 2014;161:681–689 [DOI] [PubMed] [Google Scholar]
- 16. World Health Organization . Global health risks: mortality and burden of disease attributable to selected major risks. World Health Organization, 2009. Available from https://apps.who.int/iris/handle/10665/44203
- 17. Lin X, Xu Y, Pan X, et al. Global, regional, and national burden and trend of diabetes in 195 countries and territories: an analysis from 1990 to 2025. Sci Rep 2020;10:14790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Department of Health and Human Services . Establishment of the National Clinical Care Commission and solicitation of nominations for commission members. Federal Register, 2018. Available from https://www.federalregister.gov/documents/2018/04/26/2018-08797/establishment-of-the-national-clinical-care-commission-and-solicitation-of-nominations-for
- 19. Hill JO, Galloway JM, Goley A, et al. Scientific statement: socioecological determinants of prediabetes and type 2 diabetes. Diabetes Care 2013;36:2430–2439 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Baptista DR, Wiens A, Pontarolo R, Regis L, Reis WC, Correr CJ. The chronic care model for type 2 diabetes: a systematic review. Diabetol Metab Syndr 2016;8:7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. National Clinical Care Commission . Report to Congress on Leveraging Federal Programs to Prevent and Control Diabetes and Its Complications, 2021. Accessed 10 August 2022. Available from https://health.gov/about-odphp/committees-workgroups/national-clinical-care-commission/report-congress
- 22. Bailey ZD, Krieger N, Agénor M, Graves J, Linos N, Bassett MT. Structural racism and health inequities in the USA: evidence and interventions. Lancet 2017;389:1453–1463 [DOI] [PubMed] [Google Scholar]
- 23. Cunningham SA, Patel SA, Beckles GL, et al. County-level contextual factors associated with diabetes incidence in the United States. Ann Epidemiol 2018;28:20–25.e2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Mercado CI, McKeever Bullard K, Gregg EW, Ali MK, Saydah SH, Imperatore G. Differences in U.S. rural-urban trends in diabetes ABCS, 1999-2018. Diabetes Care 2021;44:1766–1773 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Stuebe AM, Schwarz EB. The risks and benefits of infant feeding practices for women and their children. J Perinatol 2010;30:155–162 [DOI] [PubMed] [Google Scholar]
- 26. Gunderson EP, Greenspan LC, Faith MS, Hurston SR; SWIFT Offspring Study Investigators . Breastfeeding and growth during infancy among offspring of mothers with gestational diabetes mellitus: a prospective cohort study. Pediatr Obes 2018;13:492–504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Schillinger D. Social determinants, health literacy, and disparities: intersections and controversies. Health Lit Res Pract 2021;5:e234–e243 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Institute of Medicine (US) Committee on Health Literacy . Health Literacy: A Prescription to End Confusion. Nielsen-Bohlman L, Panzer AM, Kindig DA, Eds. Washington, DC, National Academies Press, 2004. Available from https://www.ncbi.nlm.nih.gov/books/NBK216032/ [PubMed] [Google Scholar]
- 29. Schillinger D, Grumbach K, Piette J, et al. Association of health literacy with diabetes outcomes. JAMA 2002;288:475–482 [DOI] [PubMed] [Google Scholar]
- 30. Bailey SC, Brega AG, Crutchfield TM, et al. Update on health literacy and diabetes. Diabetes Educ 2014;40:581–604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Zoellner J, You W, Connell C, et al. Health literacy is associated with healthy eating index scores and sugar-sweetened beverage intake: findings from the rural Lower Mississippi Delta. J Am Diet Assoc 2011;111:1012–1020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Seligman HK, Berkowitz SA. Aligning programs and policies to support food security and public health goals in the United States. Annu Rev Public Health 2019;40:319–337 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Seligman HK, Schillinger D. Hunger and socioeconomic disparities in chronic disease. N Engl J Med 2010;363:6–9 [DOI] [PubMed] [Google Scholar]
- 34. Leung CW, Ding EL, Catalano PJ, Villamor E, Rimm EB, Willett WC. Dietary intake and dietary quality of low-income adults in the Supplemental Nutrition Assistance Program. Am J Clin Nutr 2012;96:977–988 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Gucciardi E, Vahabi M, Norris N, del Monte JP, Farnum C. The intersection between food insecurity and diabetes: a review. Curr Nutrition Rep 2014;3:324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Tabaei BP, Rundle AG, Wu WY, et al. Associations of residential socioeconomic, food, and built environments with glycemic control in persons with diabetes in New York City from 2007-2013. Am J Epidemiol 2018;187:736–745 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Billimek J, Sorkin DH. Food insecurity, processes of care, and self-reported medication underuse in patients with type 2 diabetes: results from the California Health Interview Survey. Health Serv Res 2012;47:2159–2168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Berkowitz SA, Seligman HK, Choudhry NK. Treat or eat: food insecurity, cost-related medication underuse, and unmet needs. Am J Med 2014;127:303–310.e3 [DOI] [PubMed] [Google Scholar]
- 39. Bagby SP, Martin D, Chung ST, Rajapakse N. From the outside in: biological mechanisms linking social and environmental exposures to chronic disease and to health disparities. Am J Public Health 2019;109(S1):S56–S63 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Amuda AT, Berkowitz SA. Diabetes and the built environment: evidence and policies. Curr Diab Rep 2019;19:35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Booth GL, Creatore MI, Moineddin R, et al. Unwalkable neighborhoods, poverty, and the risk of diabetes among recent immigrants to Canada compared with long-term residents. Diabetes Care 2013;36:302–308 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Sundquist K, Eriksson U, Mezuk B, Ohlsson H. Neighborhood walkability, deprivation and incidence of type 2 diabetes: a population-based study on 512,061 Swedish adults. Health Place 2015;31:24–30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Fazli GS, Moineddin R, Chu A, Bierman AS, Booth GL. Neighborhood walkability and pre-diabetes incidence in a multiethnic population. BMJ Open Diabetes Res Care 2020;8:e000908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Schootman M, Andresen EM, Wolinsky FD, et al. The effect of adverse housing and neighborhood conditions on the development of diabetes mellitus among middle-aged African Americans. Am J Epidemiol 2007;166:379–387 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Vijayaraghavan M, Jacobs EA, Seligman H, Fernandez A. The association between housing instability, food insecurity, and diabetes self-efficacy in low-income adults. J Health Care Poor Underserved 2011;22:1279–1291 [DOI] [PubMed] [Google Scholar]
- 46. Axon RN, Gebregziabher M, Dismuke CE, et al. Differential impact of homelessness on glycemic control in veterans with type 2 diabetes mellitus. J Gen Intern Med 2016;31:1331–1337 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. U.S. Department of Housing and Urban Development . 2020 Annual Homeless Assessment Report Part 1: Homelessness Increasing Even Prior to COVID-19 Pandemic. Washington, DC, U.S. Department of Housing and Urban Development, 2021. Available from https://www.hud.gov/press/press_releases_media_advisories/hud_no_21_041
- 48. Berkowitz SA, Kalkhoran S, Edwards ST, Essien UR, Baggett TP. Unstable housing and diabetes-related emergency department visits and hospitalization: a nationally representative study of safety-net clinic patients. Diabetes Care 2018;41:933–939 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Ludwig J, Sanbonmatsu L, Gennetian L, et al. Neighborhoods, obesity, and diabetes–a randomized social experiment. N Engl J Med 2011;365:1509–1519 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Bonini MG, Sargis RM. Environmental toxicant exposures and type 2 diabetes mellitus: two interrelated public health problems on the rise. Curr Opin Toxicol 2018;7:52–59 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Sargis RM, Simmons RA. Environmental neglect: endocrine disruptors as underappreciated but potentially modifiable diabetes risk factors. Diabetologia 2019;62:1811–1822 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Wang X, Karvonen-Gutierrez CA, Herman WH, Mukherjee B, Harlow SD, Park SK. Urinary metals and incident diabetes in midlife women: Study of Women’s Health Across the Nation (SWAN). BMJ Open Diabetes Res Care 2020;8:e001233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Bowe B, Xie Y, Li T, Yan Y, Xian H, Al-Aly Z. The 2016 global and national burden of diabetes mellitus attributable to PM2·5 air pollution. Lancet Planet Health 2018;2:e301–e312 [DOI] [PubMed] [Google Scholar]
- 54. Park SK, Wang X, Ding N, Karvonen-Gutierrez C, Herman WH, Mukherjee B, Harlow SD. Per- and polyfluoroalkyl substances (PFAS) and incident diabetes in midlife women: the Study of Women’s Health Across the Nation (SWAN). Diabetologia 2022;65:1157–1168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Tessum CW, Paolella DA, Chambliss SE, Apte JS, Hill JD, Marshall JD. PM2.5 polluters disproportionately and systemically affect people of color in the United States. Sci Adv 2021;7:eabf4491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Ruiz D, Becerra M, Jagai JS, Ard K, Sargis RM. Disparities in environmental exposures to endocrine-disrupting chemicals and diabetes risk in vulnerable populations. Diabetes Care 2018;41:193–205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Lê-Scherban F, Ballester L, Castro JC, et al. Identifying neighborhood characteristics associated with diabetes and hypertension control in an urban African-American population using geo-linked electronic health records. Prev Med Rep 2019;15:100953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Environmental Protection Agency . Navajo Nation: Cleaning Up Abandoned Uranium Mines. Washington, DC, Environmental Protection Agency [Google Scholar]
- 59. Rudolph L, Caplan J, Mitchell C, Ben-Moshe K, Dillon L. 2013. Health in All Policies: Improving Health Through Intersectoral Collaboration. NAM Perspectives. Discussion Paper, National Academy of Medicine, Washington, DC. Available from 10.31478/201309a. [DOI]
- 60. United States Code . Public Law 93-353. Available from https://www.govinfo.gov/content/pkg/STATUTE-88/pdf/STATUTE-88-Pg362.pdf
- 61. National Institute of Diabetes and Digestive and Kidney Diseases . Diabetes Mellitus Interagency Coordinating Committee (DMICC). Accessed 18 August 2021. Available from https://www.niddk.nih.gov/about-niddk/advisory-coordinating-committees/diabetes-mellitus-interagency-coordinating-committee-dmicc
- 62. Schillinger D, Bullock A, Powell C, et al. The National Clinical Care Commission report to Congress: leveraging federal policies and programs for population-level diabetes prevention and control: recommendations from the National Clinical Care Commission. Diabetes Care 2023;46:e24–e38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Institute of Medicine (US) Committee on Monitoring Access to Personal Health Care Services . Access to Health Care in America. Washington, DC, National Academies Press, 1993 [Google Scholar]
- 64. Goldman DP, Cohen BG, Ho JY, McFadden DL, Ryan MS, Tysinger B. Improved survival for individuals with common chronic conditions in the Medicare population. Health Econ 2021;30(Suppl. 1):80–91 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Casagrande SS, McEwen LN, Herman WH. Changes in health insurance coverage under the Affordable Care Act: a national sample of U.S. adults with diabetes, 2009 and 2016. Diabetes Care 2018;41:956–962 [DOI] [PubMed] [Google Scholar]
- 66. Myerson R, Romley J, Chiou T, Peters AL, Goldman D. The Affordable Care Act and health insurance coverage among people with diagnosed and undiagnosed diabetes: data from the National Health and Nutrition Examination Survey. Diabetes Care 2019;42:e179–e180 [DOI] [PubMed] [Google Scholar]
- 67. Collins SR, Bhupal HK. Health insurance coverage eight years after the ACA. Issue Briefs. New York, NY, The Commonwealth Fund, 2021. Available from https://www.commonwealthfund.org/publications/issue-briefs/2019/feb/health-insurance-coverage-eight-years-after-aca
- 68. Cohen RA, Terlizzi EP, Martinez ME, Cha AE. Health insurance coverage: early release of estimates from the national health interview survey, January–June 2019. Atlanta, GA, Centers for Disease Control and Prevention. Available from https://www.cdc.gov/nchs/data/nhis/earlyrelease/insur202005-508.pdf
- 69. Zhang X, Bullard KM, Gregg EW, et al. Access to health care and control of ABCs of diabetes. Diabetes Care 2012;35:1566–1571 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Doty MM, Tikkanen RS, FitzGerald M, Fields K, Williams RD 2nd. Income-related inequality in affordability and access to primary care in eleven high-income countries. Health Aff (Millwood) 2021;40:113–120 [DOI] [PubMed] [Google Scholar]
- 71. Collins SR, Gunja MZ, Aboulafia GNUS. Health insurance coverage in 2020: a looming crisis in affordability. Issue Briefs. New York, NY, The Commonwealth Fund, 2020. Available from https://www.commonwealthfund.org/publications/issue-briefs/2020/aug/looming-crisis-health-coverage-2020-biennial
- 72. Patel MR, Piette JD, Resnicow K, Kowalski-Dobson T, Heisler M. Social determinants of health, cost-related nonadherence, and cost-reducing behaviors among adults with diabetes: findings from the national health interview survey. Med Care 2016;54:796–803 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Allen HL, Sommers BD. Medicaid and COVID-19: at the center of both health and economic crises. JAMA 2020;324:135–136 [DOI] [PubMed] [Google Scholar]
- 74. Garfield R, Orgera K, Damico A. The coverage gap: uninsured poor adults in states that do not expand Medicaid. San Francisco, CA, Kaiser Family Foundation, 2021. Accessed 8 August 2021. Available from https://www.kff.org/medicaid/issue-brief/the-coverage-gap-uninsured-poor-adults-in-states-that-do-not-expand-medicaid/
- 75. Medicaid . Medicaid Expansion Helps Address Health Disparities. Washington, DC, Centers for Medicare and Medicaid Services. Accessed 17 August 2021. Available from https://www.medicaid.gov/about-us/program-history/medicaid-50th-anniversary/entry/47671
- 76. Strawbridge LM, Lloyd JT, Meadow A, Riley GF, Howell BL. One-year outcomes of diabetes self-management training among Medicare beneficiaries newly diagnosed with diabetes. Med Care 2017;55:391–397 [DOI] [PubMed] [Google Scholar]
- 77. Strawbridge LM, Lloyd JT, Meadow A, Riley GF, Howell BL. Use of Medicare’s diabetes self-management training benefit. Health Educ Behav 2015;42:530–538 [DOI] [PubMed] [Google Scholar]
- 78. Rutledge SA, Masalovich S, Blacher RJ, Saunders MM. Diabetes self-management education programs in nonmetropolitan counties–United States, 2016. MMWR Surveill Summ 2017;66:1–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. White House . Executive Order on Advancing Racial Equity and Support for Underserved Communities Through the Federal Government. Washington, DC, The White House. Accessed 8 August 2021. Available from https://www.whitehouse.gov/briefing-room/presidential-actions/2021/01/20/executive-order-advancing-racial-equity-and-support-for-underserved-communities-through-the-federal-government/