Abstract
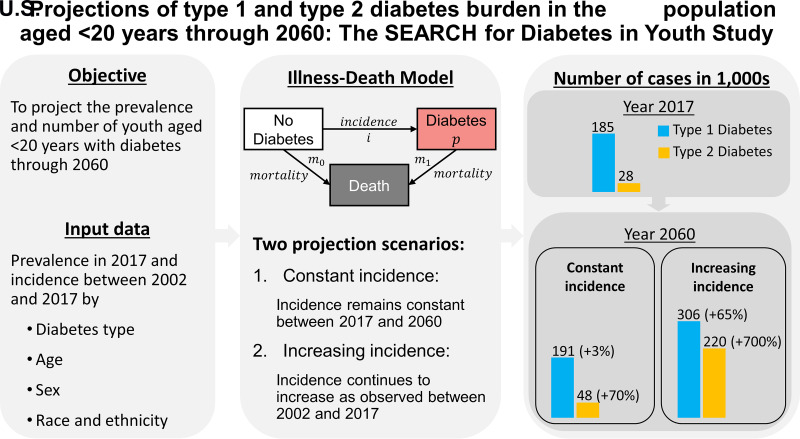
OBJECTIVE
To project the prevalence and number of youths with diabetes and trends in racial and ethnic disparities in the U.S. through 2060.
RESEARCH DESIGN AND METHODS
Based on a mathematical model and data from the SEARCH for Diabetes in Youth study for calendar years 2002–2017, we projected the future prevalence of type 1 and type 2 diabetes among youth aged <20 years while considering different scenarios of future trends in incidence.
RESULTS
The number of youths with diabetes will increase from 213,000 (95% CI 209,000; 218,000) (type 1 diabetes 185,000, type 2 diabetes 28,000) in 2017 to 239,000 (95% CI 209,000; 282,000) (type 1 diabetes 191,000, type 2 diabetes 48,000) in 2060 if the incidence remains constant as observed in 2017. Corresponding relative increases were 3% (95% CI −9%; 21%) for type 1 diabetes and 69% (95% CI 43%; 109%) for type 2 diabetes. Assuming that increasing trends in incidence observed between 2002 and 2017 continue, the projected number of youths with diabetes will be 526,000 (95% CI 335,000; 893,000) (type 1 diabetes 306,000, type 2 diabetes 220,000). Corresponding relative increases would be 65% (95% CI 12%; 158%) for type 1 diabetes and 673% (95% CI 362%; 1,341%) for type 2 diabetes. In both scenarios, substantial widening of racial and ethnic disparities in type 2 diabetes prevalence are expected, with the highest prevalence among non-Hispanic Black youth.
CONCLUSIONS
The number of youths with diabetes in the U.S. is likely to substantially increase in future decades, which emphasizes the need for prevention to attenuate this trend.
Graphical Abstract
Introduction
The incidence and prevalence of youth-onset diabetes have been on the rise in the U.S. in recent decades (1,2). Historically, youth-onset diabetes mainly referred to type 1 diabetes (3). However, one striking feature of more recent data is the rapid rise of type 2 diabetes among adolescents, with an annual percent change in incidence of 4.8% between 2002 and 2015 compared with 1.9% for type 1 diabetes (1). Whereas the reasons for increases in type 1 diabetes incidence are largely unknown, several explanations for the increase in type 2 diabetes incidence are likely. For instance, data from U.S. health surveys suggest that increasing prevalence of obesity in childhood and adolescence parallels trends in the incidence of type 2 diabetes (4,5). In addition, the increasing prevalence of type 2 diabetes in adulthood might be another important factor because exposure to diabetes in utero is associated with an increased risk of diabetes in offspring (3,6).
In addition to this increase in type 2 diabetes, recent trends in youth-onset diabetes also suggest a widening in racial and ethnic disparities in incidence and prevalence (1,2). Regarding health disparities, type 1 diabetes and type 2 diabetes are characterized by opposite patterns. Type 2 diabetes is more frequent among Hispanic/Latino, non-Hispanic Black/African American (NHB), Asian/Pacific Islander, and American Indian/Alaska Native youth compared with non-Hispanic White (NHW) youth, whereas in type 1 diabetes, this pattern is reversed (2,3). However, regarding type 1 diabetes, disparity patterns similar to type 2 diabetes are currently emerging, since increases in incidence and prevalence were faster in all racial and ethnic groups other than NHW youth (1,2).
The increasing trends in incidence raise concerns about the future burden of diabetes in youth regarding prevalence and the number of people affected. In particular, the rise of type 2 diabetes seems worrying because compared with youths and young adults with type 1 diabetes, those with type 2 diabetes have a worse cardiovascular risk profile and increased risk of complications and mortality (7–9). Furthermore, health disparities in type 2 diabetes prevalence might further increase in the future as a result of heterogeneous trends in incidence.
Hence, in this study, we aimed to project the future burden of diabetes in the U.S. youth through 2060 while accounting for age, sex, race and ethnicity, diabetes type–specific trends in incidence, and projected demographic changes. We built on the SEARCH for Diabetes in Youth (SEARCH) study, which allows for detailed analysis of trends in incidence by race and ethnicity, sex, and diabetes type between 2002 and 2017, and an estimate of diabetes prevalence by these same characteristics in 2017.
Research Design and Methods
Study Design and Data Sources
We used an illness-death model and data on prevalence and incidence of diabetes in youth from the SEARCH study to project the prevalence and number of youths with diabetes in the U.S. through 2060. SEARCH is a population-based multicenter study among youth in the U.S. aged <20 years. A detailed description of the study is available elsewhere (2,10,11). Briefly, data were collected from clinical centers in 6 regions, including Colorado (covering 14 counties), Ohio (covering 8 counties), California (Kaiser Permanente Southern California covering 7 counties), Washington State (covering 5 counties), South Carolina (covering 4 counties), and beneficiaries of the Indian Health Service in select parts of Arizona and New Mexico (data collection coordinated by the Colorado center). The SEARCH study centers ascertained clinically diagnosed prevalent and incident cases of diabetes. Completeness of case ascertainment within the regions was estimated to be >90% (1,11). For this study, we used data on diabetes prevalence in 2017 and diabetes incidence from 2002 to 2017. To project the future prevalence of diabetes in youths, these data were used as input data for a partial differential equation that governs the illness-death model (12). Institutional review boards for each site approved the study protocol of the SEARCH study.
Statistical Analysis
Estimating Prevalence in 2017
In line with a previous analysis (2), the numerator of diabetes prevalence in 2017 included all individuals with prevalent diabetes aged <20 years in 2017. To be eligible as a participant, youths needed to be residents of the SEARCH geographic sites, Indian Health Service beneficiaries, or enrollees in the study’s California health plan. Age, sex, date of diagnosis, and diabetes type were obtained from medical records. Race and ethnicity were investigated because of known disparities in diabetes prevalence (2). In the context of these health disparities, race and ethnicity are considered social constructs rather than biological constructs (13). Race and ethnicity were obtained from self-report, medical records, or geocoding based on participants’ residential address in the prevalent year when data were missing (∼3% of the total participants with prevalent diabetes) and categorized into the four groups: Hispanic/Latino, NHB, NHW, and non-Hispanic other race(NH other race). While the degree of accuracy of the geocoding to estimate missing race and ethnicity is not known, we assumed that the impact of potential inaccuracies on the race and ethnicity distribution of the total population is low because the proportion of missing data was very low. Corresponding denominators consisted of all residents of the SEARCH study geographic sites, Indian Health Service beneficiaries, or enrollees in the study’s California health plan. Age-specific diabetes prevalence in youth aged <20 years in 2017 was estimated for 1-year age-groups.
Estimating Incidence Between 2002 and 2017
Participants with incident diabetes (numerator) who were aged <20 years in the year of diagnosis were included for diabetes incidence estimation between 2002 and 2017. The corresponding annual population at risk (denominator) included the population aged <20 years who were residents of the geographic study areas, Indian Health Service beneficiaries, or enrollees in the study’s California health plan.
We used Poisson regression with the number of participants with incident diabetes as the dependent variable and the logarithm of the population size at risk as an offset variable to estimate diabetes incidence rates. Independent variables were age, race and ethnicity, sex, and calendar year. We also included interactions between race and ethnicity and age, as well as race and ethnicity and calendar year, to allow for race and ethnicity–specific age patterns and temporal trends in diabetes incidence. Age was modeled using natural cubic splines, with the number knots providing the best fit according to the Bayesian information criterion. Calendar year was modeled linearly to reflect the long-term temporal trend between 2002 and 2017. The models were fitted separately for type 1 and type 2 diabetes as well as for males and females. Predicted incidences from these regression models were used as input data for the projection model.
Projection Model
Illness-Death Model
We used an illness-death model for the projection of diabetes prevalence. In this model, the population was divided into the three states of no diabetes, diabetes, and death. Using a partial differential equation and SEARCH input data, the model was used to project the age-specific prevalence (14,15) (Supplementary Methods 1). Since excess mortality associated with diabetes in youth has a negligible impact on future prevalence, we assumed mortality rates to be equal between youth with and without diabetes (15) (Supplementary Methods 1). We projected the future age-specific prevalence by solving the partial differential equation using SEARCH input data for prevalence and incidence. To quantify racial and ethnic disparities, prevalence ratios were estimated by dividing the prevalence among each racial and ethnic group by the prevalence among NHW youth (reference group).
For the incidence rate, input values for all years through 2060 were needed. Hence, we considered two different scenarios regarding assumed future trends in the incidence rate described in detail below.
Constant Incidence Scenario
In the constant incidence scenario, we assumed that the incidence rate will not change between 2017 and 2060 and used the age-specific incidence rate of diabetes estimated using SEARCH data for 2017 for all years until 2060. Estimation of the incidence rate in 2017 for each age-sex-race and ethnicity combination was based on Poisson regression models as described above.
Increasing Incidence Scenario
In the increasing incidence scenario, we assumed that the trends in the incidence rate observed in SEARCH between 2002 and 2017 will continue unchanged until 2060. Hence, we extrapolated the log-linear trend until 2060 by predicting incidence from Poisson regression models for each year of the projection period and for each age-sex-race and ethnicity combination.
All projections of the age-specific prevalence were stratified by sex, race and ethnicity, and diabetes type. The number of youth with diabetes was estimated by multiplying the projected prevalence with the corresponding population size as projected by the U.S. Census Bureau for 2060 (16). Handling of different classifications regarding race and ethnicity in the population projections and SEARCH is described in Supplementary Methods 2. We estimated 95% CIs using Monte Carlo simulation (Supplementary Methods 3).
Sensitivity Analyses
As a sensitivity analysis, we modeled the impact of three hypothetical interventions that annually attenuate the increasing trend in incidence of type 1 and type 2 diabetes by 1%, 2%, and 3%, respectively, from the year 2018 onward. We chose these reductions arbitrarily because of the lack of evidence for effective prevention of diabetes in youth. All analyses were performed using R version 4.0.4 statistical software (R Foundation for Statistical Computing).
Results
Input Data
In 2017, among 3.6 million youth under surveillance, SEARCH identified 7,759 participants with prevalent type 1 diabetes and 1,230 with prevalent type 2 diabetes (2). Age-specific prevalence is shown in Supplementary Figs. 2 and 3.
Between 2002 and 2017, the mean annual number of incident cases identified in SEARCH was ∼1,100 (type 1 diabetes) and ∼300 (type 2 diabetes) among ∼5 million youth at risk each year. More detailed results about trends in incidence are subject to further investigations and are planned to be published in another article.
Projected Prevalence
The trends in projected prevalence and number of cases of diabetes were similar for males and females. Therefore, we report results for both sexes combined in the following sections.
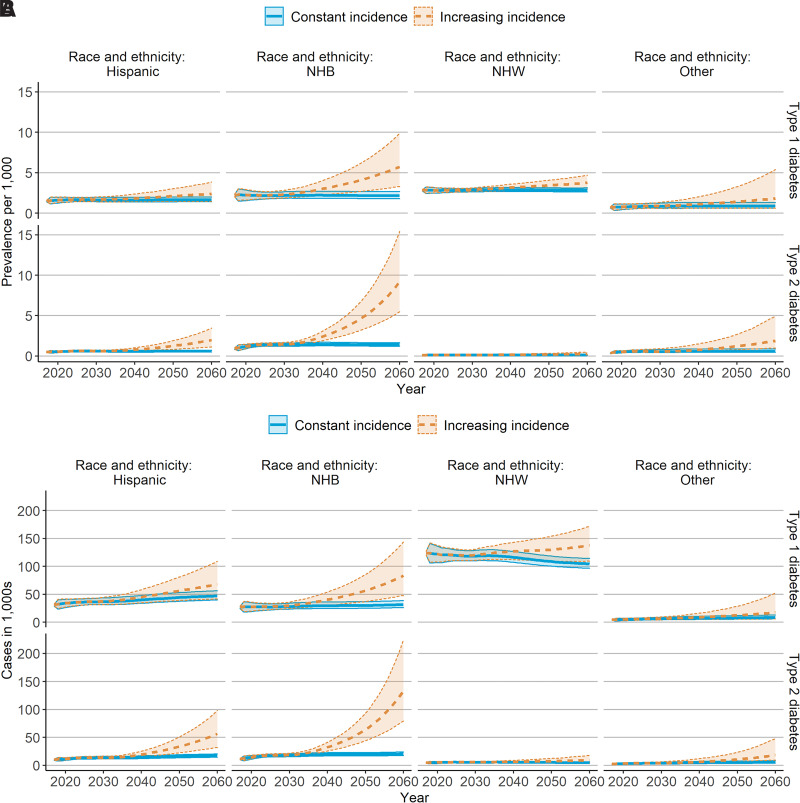
Figure 1A shows the projected prevalence under the constant incidence and increasing incidence scenarios between 2017 and 2060. For type 1 diabetes, the highest prevalence in 2017 was observed among NHW youth, followed by NHB, Hispanic/Latino, and NH other race youth. Under the constant incidence scenario, the prevalence was projected to remain stable until 2060, whereas under the increasing incidence scenario, the prevalence increased in all racial and ethnic groups. These increases were most pronounced among NHB youth.
Figure 1.
Projected prevalence of (A) and number of youths with (B) diabetes aged <20 years in the U.S., 2017–2060. In the constant incidence scenario, prevalence was projected under the assumption that the incidence rate did not change between 2017 and 2060. In the increasing incidence scenario, prevalence was projected under the assumption that trends in incidence observed between 2002 and 2017 continued until 2060. Shaded areas indicate 95% CIs.
For type 2 diabetes, the highest prevalence in 2017 was observed among NHB youth, followed by Hispanic/Latino, NH other race, and NHW youth. In contrast to type 1 diabetes, slight increases in prevalence were seen in the constant incidence scenario until 2025, particularly among NHB youth. From 2025 onward, the prevalence was projected to remain stable. In the increasing incidence scenario, the prevalence increased among all groups, particularly among NHB youth.
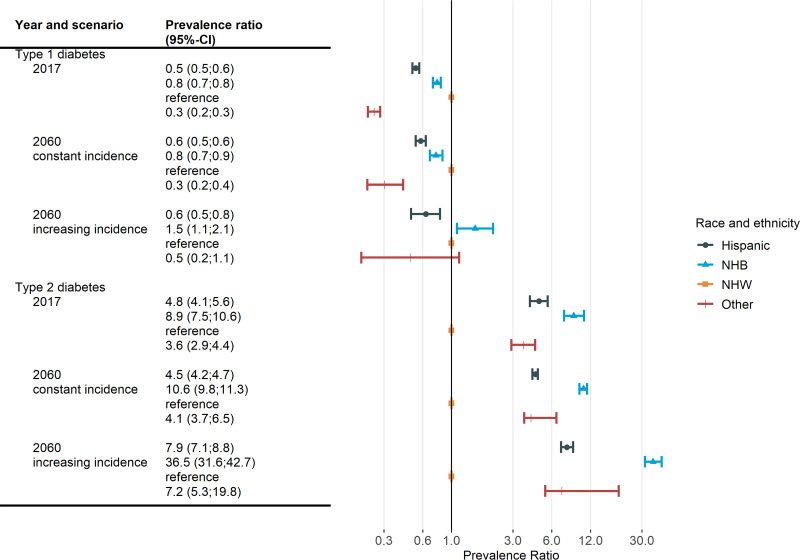
These projected trends in prevalence corresponded to a widening gap in racial and ethnic disparities for type 2 diabetes prevalence (Fig. 2). For instance, under the increasing incidence scenario, the prevalence ratio comparing NHB and NHW youth increased from 8.9 (95% CI 7.5; 10.6) in 2017 to 36.5 (95% CI 31.6; 42.7) in 2060. In contrast, racial and ethnic differences in type 1 diabetes prevalence showed a tendency to narrow in both projection scenarios (Fig. 2). However, this narrowing was not due to declining prevalence among NHW youth but increasing prevalence in all other racial and ethnic groups.
Figure 2.
Projected racial and ethnic disparities in diabetes prevalence among youth aged <20 years in the U.S., 2017–2060. In the constant incidence scenario, prevalence was projected under the assumption that the incidence rate did not change between 2017 and 2060. In the increasing incidence scenario, prevalence was projected under the assumption that trends in incidence observed between 2002 and 2017 continued until 2060.
Projected Number of Youth With Diabetes
The projected number of diabetes cases is partly determined by trends in population growth, which is projected to differ among populations by race and ethnicity (16). Hence, despite stable prevalence in the constant incidence scenario (Fig. 1A), the number of type 1 and type 2 diabetes cases is projected to increase among NHB, Hispanic/Latino, and NH other race youth due to projected population growth, whereas a decrease can be seen in type 1 diabetes among NHW youth due to a projected population decline (16) (Fig. 1B). In the increasing incidence scenario, the increases in the number of cases are considerably larger, and the decline among NHW youth is reversed. The largest increases in this scenario occurred among NHB youth.
We combined youths from all racial and ethnic groups to estimate the overall prevalence and number of cases of diabetes (Table 1). The overall number of youths with type 1 diabetes is projected to remain stable at ∼190,000 between 2017 and 2060 in the constant incidence scenario, and to increase to ∼306,000 in the increasing incidence scenario, corresponding to a relative increase of 65% (Table 2). The number of youths with type 2 diabetes is projected to increase from 28,000 to 48,000 in the constant incidence scenario and to 220,000 in the increasing incidence scenario (Table 1), corresponding to relative increases of ∼70% and 700%, respectively (Table 2). Results for short-term projections for the years 2030 and 2040 are provided in Supplementary Table 3. Combining both diabetes types resulted in case increases from 213,000 (95% CI 209,000; 218,000) in 2017 to 239,000 (95% CI 209,000; 282,000) in 2060 in the constant incidence scenario and 526,000 (95% CI 335,000; 893,000) in the increasing incidence scenario.
Table 1.
Projected prevalence and number of youth with diabetes in the U.S., 2060
| Year | ||||||
|---|---|---|---|---|---|---|
| 2060 | ||||||
| 2017 | Constant incidence* | Increasing incidence† | ||||
| Prevalence per 1,000 youths (95% CI) | Number of cases × 1,000 (95% CI) | Prevalence per 1,000 youths (95% CI) | Number of cases × 1,000 (95% CI) | Prevalence per 1,000 youths (95% CI) | Number of cases × 1,000 (95% CI) | |
| Type 1 diabetes | 2.2 (2.2; 2.3) | 185 (181; 189) | 2.1 (1.9; 2.5) | 191 (168; 222) | 3.4 (2.3; 5.3) | 306 (205; 476) |
| Hispanic/ Latino | 1.5 (1.4; 1.6) | 31 (29; 32) | 1.7 (1.4; 2.0) | 47 (40; 56) | 2.4 (1.5; 3.8) | 68 (42; 109) |
| NHB | 2.2 (2.0; 2.3) | 27 (25; 28) | 2.2 (1.8; 2.7) | 32 (26; 39) | 5.7 (3.3; 9.9) | 83 (48; 143) |
| NHW | 2.8 (2.7; 2.9) | 124 (120; 127) | 2.9 (2.6; 3.1) | 105 (97; 114) | 3.8 (3.0; 4.7) | 137 (109; 172) |
| NH other race | 0.7 (0.6; 0.8) | 4 (4; 5) | 0.9 (0.6; 1.3) | 8 (6; 13) | 1.8 (0.6; 5.4) | 18 (6; 52) |
| Type 2 diabetes | 0.3 (0.3; 0.4) | 28 (27; 30) | 0.5 (0.5; 0.7) | 48 (41; 58) | 2.5 (1.4; 4.6) | 220 (129; 410) |
| Hispanic/ Latino | 0.5 (0.5; 0.5) | 10 (9; 11) | 0.6 (0.5; 0.7) | 17 (15; 20) | 2.0 (1.1; 3.5) | 56 (32; 98) |
| NHB | 0.9 (0.8; 1.0) | 11 (10; 12) | 1.4 (1.2; 1.6) | 20 (18; 24) | 9.2 (5.5; 15.4) | 134 (80; 224) |
| NHW | 0.1 (0.1; 0.1) | 5 (4; 5) | 0.1 (0.1; 0.2) | 5 (4; 6) | 0.3 (0.1; 0.5) | 9 (5; 18) |
| NH other race | 0.4 (0.3; 0.4) | 2 (2; 3) | 0.6 (0.5; 0.9) | 5 (4; 8) | 1.9 (1.0; 4.9) | 18 (10; 48) |
*In the constant incidence scenario, prevalence was projected under the assumption that the incidence rate did not change between 2017 and 2060.
†In the increasing incidence scenario, prevalence was projected under the assumption that trends in incidence observed between 2002 and 2017 continued until 2060.
Table 2.
Projected percent change in prevalence and number of youths with diabetes in the U.S., 2017–2060
| Relative change from 2017 to 2060 | ||||
|---|---|---|---|---|
| Constant incidence* | Increasing incidence† | |||
| Percent change in prevalence (95% CI) | Percent change in number of cases (95% CI) | Percent change in prevalence (95% CI) | Percent change in number of cases (95% CI) | |
| Type 1 diabetes | −5 (−16; 11) | 3 (−9; 21) | 52 (3; 138) | 65 (12; 158) |
| Hispanic/Latino | 10 (−8; 33) | 54 (29; 85) | 59 (−2; 157) | 121 (37; 259) |
| NHB | −1 (−18; 22) | 18 (−3; 46) | 163 (51; 358) | 214 (80; 446) |
| NHW | 1 (−6; 11) | −15 (−22; −7) | 33 (6; 67) | 11 (−11; 39) |
| NH other race | 21 (−17; 86) | 100 (36; 207) | 155 (−14; 670) | 321 (43; 1,171) |
| Type 2 diabetes | 56 (31; 93) | 69 (43; 109) | 612 (325; 1,228) | 673 (362; 1,341) |
| Hispanic/Latino | 20 (0; 46) | 67 (40; 103) | 296 (132; 617) | 452 (223; 899) |
| NHB | 52 (27; 82) | 82 (51; 117) | 901 (484; 1,629) | 1093 (596; 1,960) |
| NHW | 28 (1; 68) | 7 (−16; 41) | 142 (24; 375) | 102 (3; 297) |
| NH other race | 49 (15; 137) | 146 (90; 292) | 406 (163; 1,220) | 735 (334; 2,078) |
*In the constant incidence scenario, prevalence was projected under the assumption that the incidence rate did not change between 2017 and 2060.
†In the increasing incidence scenario, prevalence was projected under the assumption that trends in incidence observed between 2002 and 2017 continued until 2060.
In sensitivity analyses, we modeled three hypothetical interventions that annually attenuate the increasing trend in incidence by 1%, 2%, and 3%. These analyses resulted in 396,000 (95% CI 255,000; 686,000), 294,000 (95% CI 187,000; 485,000), and 218,000 (95% CI 139,000; 366,000) cases (type 1 and type 2 diabetes) in 2060, respectively (see Supplementary Table 4 for results by diabetes type). These numbers correspond to 122,000 (95% CI −499,000; 197,000), 231,000 (95% CI −611,000; 52,000), and 308,000 (95% CI −528,000; −196,000) prevented prevalent cases, respectively.
Conclusions
Based on an illness-death model and data on prevalence and incidence of diabetes in youth in the U.S., we projected the prevalence and number of youth with diabetes through 2060. We accounted for differences in prevalence, incidence, and annual percent change in incidence by race and ethnicity, sex, and diabetes type, as well as projected demographic changes until 2060. We found that the number of youth with diabetes will increase 12% from 213,000 (type 1 diabetes 185,000, type 2 diabetes 28,000) in 2017 to 239,000 (type 1 diabetes 191,000, type 2 diabetes 48,000) in 2060, if the incidence remains as observed in 2017. Assuming that trends in incidence observed between 2002 and 2017 continue, the projected number of youth with diabetes will more than double to 526,000 (type 1 diabetes 306,000, type 2 diabetes 220,000). In both scenarios, we observed a substantial widening of disparities among race and ethnicity groups in type 2 diabetes prevalence. Increases in prevalence were least pronounced among NHW youth and most pronounced among NHB youth.
A similar analysis using SEARCH data published in 2012 also projected a substantial increase in the number of youths affected by diabetes in scenarios assuming constant and increasing incidence rates (17). However, the numerical results differ, particularly in the projected increases by diabetes type. As an example, assuming increasing incidence rates, Imperatore et al. (17) projected 672,000 (type 1 diabetes 587,000, type 2 diabetes 84,000) cases for 2050, whereas we estimated 526,000 (type 1 diabetes 306,000, type 2 diabetes 220,000) cases for 2060. Hence, our projections were lower for type 1 diabetes but considerably higher for type 2 diabetes. These differences are mostly due to our inclusion of empirically observed race and ethnicity–specific trends in incidence, whereas the data available for Imperatore et al. only allowed for applying trends in incidence to youth from all racial and ethnic groups equally. Comparison of these two studies highlights the additional benefit of accounting for type as well as for race and ethnicity–specific input data when projecting the future burden of diabetes in youth.
Implications for Public Health
Our results suggest a substantial increase in the number of youths with diabetes, indicating an increasing demand for diabetes specialists and care teams to care for children, adolescents, and emerging adults; medical devices; and programs aimed at optimizing glycemic control and preventing complications in future decades. The future burden of type 2 diabetes in youth may impose challenges on the treatment of type 2 diabetes. Since a growing number of people will spend much of their lives with type 2 diabetes and accumulate long disease duration, a potential exists for an increased risk of complications associated with diabetes duration. Hence, the trend toward longer diabetes duration due to increasing prevalence in youth and reductions in diabetes-related mortality among adults may result in increasingly diverse diabetes-related morbidity (e.g., because of increasing rates of diabetes-related cancers and disabilities) (18). One major challenge might be the rise in obesity among U.S. youth (4,5). During the severe acute respiratory syndrome coronavirus 2 pandemic, the rate of obesity increased among youth, which may contribute to the increased risk of type 2 diabetes (19).
From an intergenerational perspective, the projected growth in the prevalence of reproductive age women with diabetes seems particularly problematic, since exposure to maternal diabetes in utero is associated with an increased risk of obesity and type 2 diabetes in offspring (3,6,20). These future prospects raise the question of how to attenuate or reverse current trends in youth-onset diabetes. In a sensitivity analysis assuming an attenuation of increasing trends in incidence by 2% annually, we projected 126,000 type 2 diabetes cases compared with 220,000 cases without attenuation of incidence trends. Hence, it is hypothetically possible to considerably reduce the projected increased diabetes burden in youth. Unfortunately, evidence on prevention of type 2 diabetes in youth is scarce, and additional research would be needed to determine how a sustainable change in population-wide incidence of type 2 diabetes over the next few decades can be achieved. Besides interventions aimed at behavioral change on the individual level, social determinants of health, such as built environment, obesogenic food environments, and epigenetic factors, are increasingly gaining attention as manipulable causes of type 2 diabetes (3,20–22). Intervening in social determinants of health might also be a promising path to reduce racial and ethnic disparities in youth-onset type 2 diabetes (23). Regarding type 1 diabetes, faster increases in projected prevalence among all racial and ethnic groups other than NHW youth suggest changing disparity patterns. Further research on the causes of heterogeneous trends in type 1 diabetes incidence could help identify preventive measures.
To provide information about the main drivers of future dynamics of diabetes in youths, future modeling studies could incorporate risk factors such as obesity and family history of diabetes. For instance, our model can be extended to incorporate single risk factors or risk scores that account for several risk factors (24,25).
Strengths and Limitations
This study was based on population-based data from one source with standardized procedures and a unified study protocol over a period of 16 years. Given that diabetes in youths, type 2 diabetes in particular, is difficult to study because of small numbers, these data are a valuable resource. For instance, in a similar study from 2012 (17), data on trends in incidence were only available for type 1 diabetes among NHW and Hispanic/Latino youth (26). In contrast, we were able to inform the projection model with incidence trend data stratified by sex, diabetes type, and four racial and ethnic groups. Our projection model allowed us to combine these data on the dynamics of diabetes with demographic changes as projected by the U.S. Census Bureau (16).
Our study is also subject to some limitations. First, the SEARCH study only provides data on diagnosed diabetes. Hence, we could not account for undiagnosed diabetes. While this means that the true prevalence may be underestimated, the frequency of undiagnosed diabetes in the general population of youths appears to be quite low (27). This may hold true in particular for type 1 diabetes because of its severity and insulin requirement at disease onset. Undiagnosed type 2 diabetes might be more common in the adult population. However, in youths, pancreatic β-cell function appears to deteriorate more rapidly than in adults (28), suggesting that youth rapidly develop hyperglycemia and may require medical attention sooner than adults. Indeed, data from the National Health and Nutrition Examination Survey showed that in youth aged 10–19 years, undiagnosed diabetes is uncommon (29). Another limitation is the precision of the projected estimates. Although the SEARCH study comprises a large number of participants, wide CIs for some projected estimates were obtained, particularly in the increasing incidence scenario. Furthermore, although the SEARCH study is the largest population-based study of diabetes in youth in the U.S., it does not cover all geographic regions and may not be representative for all regions.
In summary, the number of youths with diabetes is projected to increase substantially, emphasizing the importance of additional research on, and implementation of, primary and secondary preventive interventions. The projected trends indicate a substantial widening of the gap in health disparities in type 2 diabetes prevalence, with the highest estimates for NHB youth. If the current trends continue, U.S. health care systems could face an increasing demand of youth-onset diabetes health care services, resulting in increasing health care costs.
Article Information
Acknowledgments. The SEARCH study is indebted to the many youth and their families and health care providers, whose participation made this study possible.
Funding. SEARCH 3/4 was supported by the Kaiser Permanente Southern California’s Marilyn Owsley Clinical Research Center (funded by Kaiser Foundation Health Plan and supported in part by the Southern California Permanente Medical Group), the South Carolina Clinical and Translational Research Institute at the Medical University of South Carolina (National Institutes of Health [NIH]/National Center for Advancing Translational Sciences [NCATS] grants UL1 TR000062 and UL1 TR001450), Seattle Children’s Hospital and the University of Washington (NIH/NCATS grant UL1 TR00423), University of Colorado Pediatric Clinical and Translational Research Center (NIH/NCATS grant UL1 TR000154), the Barbara Davis Center at the University of Colorado at Denver (Diabetes Endocrinology Research Center NIH grant P30 DK57516), the University of Cincinnati (NIH/NCATS grants UL1 TR000077 and UL1 TR001425), and the Children with Medical Handicaps program managed by the Ohio Department of Health. SEARCH 4 is funded by the National Institute of Diabetes and Digestive and Kidney Diseases (grants 1R01 DK127208-01 and 1UC4 DK108173) and supported by the Centers for Disease Control and Prevention. The Population Based Registry of Diabetes in Youth Study is funded by the Centers for Disease Control and Prevention (grants 1U18 DP006131, U18 DP006133, U18 DP006134, U18 DP006136, U18 DP006138, U18 DP006139, and DP-15-002), and supported by the National Institute of Diabetes and Digestive and Kidney Diseases. SEARCH 1, 2, and 3 are funded by the Centers for Disease Control and Prevention (grants 00097, DP-05-069, and DP-10-001), and supported by the National Institute of Diabetes and Digestive and Kidney Diseases, Kaiser Permanente Southern California (grants U48/CCU919219, U01 DP000246, and U18 DP002714), University of Colorado Denver (grants U48/CCU819241-3, U01 DP000247, and U18 DP000247-06A1), Cincinnati Children’s Hospital Medical Center (grants U48/CCU519239, U01 DP000248, and 1U18 DP002709), University of North Carolina at Chapel Hill (grants U48/CCU419249, U01 DP000254, and U18 DP002708), Seattle Children’s Hospital (grants U58/CCU019235-4, U01 DP000244, and U18 DP002710-01), and Wake Forest University School of Medicine (U48/CCU919219, U01 DP000250, and 200-2010-35171).
This study includes data provided by the Ohio Department of Health, which should not be considered an endorsement of this study or its conclusions. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention or the National Institute of Diabetes and Digestive and Kidney Diseases.
Duality of Interest. No potential conflicts of interest relevant to this article were reported.
Author Contributions. T.T. drafted the manuscript. T.T., R.B., S.I., D.D., J.D., E.J.M.-D., J.M.L., C.P., L.D., A.D.L., S.H.S., R.B.D., A.H., and G.I. contributed to the acquisition, analysis, or interpretation of data and to the critical revision of the manuscript for important intellectual content. T.T., R.B., S.I., and A.H. contributed to the statistical analysis. R.B., A.H., and G.I. contributed to the concept and design. R.B. and G.I. supervised the study. T.T. and S.I. are the guarantors for this work and, as such, had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Prior Presentation. Parts of this study were presented in abstract form at the 81st Scientific Sessions of the American Diabetes Association, virtual, 25–29 June 2021.
Footnotes
This article contains supplementary material online at https://doi.org/10.2337/figshare.21514014.
References
- 1. Divers J, Mayer-Davis EJ, Lawrence JM, et al. Trends in incidence of type 1 and type 2 diabetes among youths - selected counties and Indian reservations, United States, 2002-2015. MMWR Morb Mortal Wkly Rep 2020;69:161–165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Lawrence JM, Divers J, Isom S, et al.; SEARCH for Diabetes in Youth Study Group . Trends in prevalence of type 1 and type 2 diabetes in children and adolescents in the US, 2001-2017. JAMA 2021;326:717–727 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Dabelea D. Diabetes in youth-looking backwards to inform the future: Kelly West Award Lecture 2017. Diabetes Care 2018;41:233–240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Ogden CL, Carroll MD, Lawman HG, et al. Trends in obesity prevalence among children and adolescents in the United States, 1988-1994 through 2013-2014. JAMA 2016;315:2292–2299 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Fryar CD, Carroll MD, Afful J. Prevalence of overweight, obesity, and severe obesity among children and adolescents aged 2–19 years: United States, 1963–1965 through 2017–2018. NCHS Health E-Stats; 2020 [Google Scholar]
- 6. Dabelea D, Mayer-Davis EJ, Lamichhane AP, et al. Association of intrauterine exposure to maternal diabetes and obesity with type 2 diabetes in youth: the SEARCH case-control study. Diabetes Care 2008;31:1422–1426 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Dabelea D, Stafford JM, Mayer-Davis EJ, et al.; SEARCH for Diabetes in Youth Research Group . Association of type 1 diabetes vs type 2 diabetes diagnosed during childhood and adolescence with complications during teenage years and young adulthood. JAMA 2017;317:825–835 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Reynolds K, Saydah SH, Isom S, et al. Mortality in youth-onset type 1 and type 2 diabetes: the SEARCH for Diabetes in Youth study. J Diabetes Complications 2018;32:545–549 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Lawrence JM, Reynolds K, Saydah SH, et al.; SEARCH for Diabetes in Youth Study Group . Demographic correlates of short-term mortality among youth and young adults with youth-onset diabetes diagnosed from 2002 to 2015: the SEARCH for Diabetes in Youth study. Diabetes Care 2021;44:2691–2698 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. SEARCH Study Group . SEARCH for Diabetes in Youth: a multicenter study of the prevalence, incidence and classification of diabetes mellitus in youth. Control Clin Trials 2004;25:458–471 [DOI] [PubMed] [Google Scholar]
- 11. Hamman RF, Bell RA, Dabelea D, et al.; SEARCH for Diabetes in Youth Study Group . The SEARCH for Diabetes in Youth study: rationale, findings, and future directions. Diabetes Care 2014;37:3336–3344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Brinks R, Landwehr S. Age- and time-dependent model of the prevalence of non-communicable diseases and application to dementia in Germany. Theor Popul Biol 2014;92:62–68 [DOI] [PubMed] [Google Scholar]
- 13. Williams DR. Race and health: basic questions, emerging directions. Ann Epidemiol 1997;7:322–333 [DOI] [PubMed] [Google Scholar]
- 14. Tönnies T, Röckl S, Hoyer A, et al. Projected number of people with diagnosed type 2 diabetes in Germany in 2040. Diabet Med 2019;36:1217–1225 [DOI] [PubMed] [Google Scholar]
- 15. Tönnies T, Imperatore G, Hoyer A, et al. Estimating prevalence of type I and type II diabetes using incidence rates: the SEARCH for Diabetes in Youth study. Ann Epidemiol 2019;37:37–42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. U.S. Census Bureau . 2017 National Population Projections Datasets, 2018. Accessed 12 October 2021. Available from https://www.census.gov/data/datasets/2017/demo/popproj/2017-popproj.html
- 17. Imperatore G, Boyle JP, Thompson TJ, et al.; SEARCH for Diabetes in Youth Study Group . Projections of type 1 and type 2 diabetes burden in the U.S. population aged <20 years through 2050: dynamic modeling of incidence, mortality, and population growth. Diabetes Care 2012;35:2515–2520 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Gregg EW, Sattar N, Ali MK. The changing face of diabetes complications. Lancet Diabetes Endocrinol 2016;4:537–547 [DOI] [PubMed] [Google Scholar]
- 19. Lange SJ, Kompaniyets L, Freedman DS, et al.; DNP3 . Longitudinal trends in body mass index before and during the COVID-19 pandemic among persons aged 2-19 years - United States, 2018-2020. MMWR Morb Mortal Wkly Rep 2021;70:1278–1283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Rughani A, Friedman JE, Tryggestad JB. Type 2 diabetes in youth: the role of early life exposures. Curr Diab Rep 2020;20:45. [DOI] [PubMed] [Google Scholar]
- 21. Zimmet PZ. Diabetes and its drivers: the largest epidemic in human history? Clin Diabetes Endocrinol 2017;3:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Hill-Briggs F, Adler NE, Berkowitz SA, et al. Social determinants of health and diabetes: a scientific review. Diabetes Care 2020;44:258–279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Hartz J, Powell-Wiley TM. Locations! Location! Location? Elucidating the social determinants of cardiometabolic health among United States adolescents. J Adolesc Health 2018;63:519–520 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Hoyer A, Kaufmann S, Brinks R. Risk factors in the illness-death model: simulation study and the partial differential equation about incidence and prevalence. PLoS One 2019;14:e0226554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Tönnies T, Heidemann C, Paprott R, et al. Estimating the impact of tax policy interventions on the projected number and prevalence of adults with type 2 diabetes in Germany between 2020 and 2040. BMJ Open Diabetes Res Care 2021;9:e001813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Vehik K, Hamman RF, Lezotte D, et al. Increasing incidence of type 1 diabetes in 0- to 17-year-old Colorado youth. Diabetes Care 2007;30:503–509 [DOI] [PubMed] [Google Scholar]
- 27. Zeitler P. Update on nonautoimmune diabetes in children. J Clin Endocrinol Metab 2009;94:2215–2220 [DOI] [PubMed] [Google Scholar]
- 28. Nadeau KJ, Anderson BJ, Berg EG, et al. Youth-onset type 2 diabetes consensus report: current status, challenges, and priorities. Diabetes Care 2016;39:1635–1642 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Wallace AS, Wang D, Shin J-I, Selvin E. Screening and diagnosis of prediabetes and diabetes in US children and adolescents. Pediatrics 2020;146:e20200265. [DOI] [PMC free article] [PubMed] [Google Scholar]