Abstract
OBJECTIVE
To examine the relationship between intake of vegetables/potatoes and incident type 2 diabetes (T2D) and explore whether the relationship between vegetable intake and incident T2D is mediated by baseline BMI.
RESEARCH DESIGN AND METHODS
Cross-sectional associations between exposure (baseline intake of total vegetables, vegetable subgroups, and potatoes) and baseline BMI were assessed by multivariable-adjusted linear regression models. Associations between exposure and incident T2D were examined by multivariable-adjusted Cox proportional hazards models. Mediation by BMI was quantified through exploration of natural direct and indirect effects.
RESULTS
Among 54,793 participants in the Danish Diet, Cancer and Health cohort, 7,695 cases of T2D were recorded during a median follow-up of 16.3 years. Participants in the highest total vegetable intake quintile (median 319 g/day) had a 0.35 kg/m2 (95% CI −0.46, −0.24) lower BMI and a 21% (95% CI 16, 26%) lower risk of incident T2D after multivariable adjustment compared with those in the lowest quintile (median 67 g/day). Baseline BMI mediated ∼21% of the association between vegetable intake and incident T2D. Participants in the highest compared with the lowest (median 256 vs. 52 g/day) potato intake quintile had a 9% (95% CI 2, 16%) higher risk of T2D after multivariable adjustment, with no association found after accounting for underlying dietary pattern. Of the vegetable subclasses, higher intake of green leafy and cruciferous vegetables was associated with a statistically significantly lower risk of T2D.
CONCLUSIONS
The findings provide evidence that a higher vegetable, but not potato, intake might help mitigate T2D risk, partly by reducing BMI.
Introduction
The prevalence of diabetes, a leading cause of global morbidity, mortality, and health care system burden (1), has risen over recent decades (2). The estimated prevalence of diabetes among individuals age 20–79 years was 537 million in 2021 and is expected to rise to 643 million by 2030 (3). An increase in the consumption of ultraprocessed foods (4) and a simultaneous decrease in the consumption of fruits and vegetables (5,6) may be among the reasons for the global increase in type 2 diabetes (T2D) incidence (1,7).
A 2021 review emphasized the importance of plant-based foods and the increment of vegetables in the diet in reducing the risk of T2D (7). This is supported by findings from a large European study based on selected biomarkers of fruits and vegetables (α-carotene, β-carotene, lutein), which suggest a higher intake of vegetables may be inversely associated with T2D (8). In contrast, two recent (2019 and 2021) meta-analyses (9,10) described only nonsignificant or weak inverse associations between higher intake of total vegetables and green leafy vegetables (GLVs) with incident T2D. The prospective studies included in these meta-analyses were heterogeneous because of methodological differences in the derivation of the estimates. This variation in methodological approach may have influenced the derived estimates.
Although findings from these meta-analyses did not suggest that vegetables and vegetable subgroups play an important role in the prevention of T2D, a statistically significant positive association between total potato intake and incident T2D was reported (9,10). Of the 18 studies included in the meta-analyses, one included potatoes in the total vegetable category (11), whereas four studies (12–15) affirmed the exclusion of potatoes. The remaining 13 studies did not describe whether potatoes were included or excluded from total vegetable intake (9,10). Given the reported positive association with T2D, inclusion of potato intake in the estimation of total vegetable intake may mask true inverse associations between other vegetables and T2D. Furthermore, all studies except two (11,13) adjusted for BMI when observing the association between vegetable intake and T2D (13,16). Because BMI likely lies on the causal pathway, adjusting for it might remove, in part, the association present between vegetable intake and incident diabetes. In addition, some of the studies failed to describe or account for underlying dietary pattern. These flaws in exposure definition, discrepancies in statistical adjustment for lifestyle/dietary variables, and inconsistencies in outcome assessment methods and sample selection may explain the lack of association reported in many studies. Therefore, using the large prospective Danish Diet, Cancer and Health (DCH) study, the objectives of our study were threefold: 1) to examine the relationship between intake of vegetables (total and subgroups) and incident T2D, 2) to examine separately the association between intake of potatoes and incident T2D, and 3) to understand whether the relationship between vegetable intake and incident T2D is mediated by baseline BMI.
Research Design and Methods
Study Participants
The study population was composed of the cohort from the DCH study, which recruited 57,053 participants age 50–64 years from the Copenhagen and Aarhus regions of Denmark from 1993 to 1997 (17). This study was initiated to examine the relationship between food and dietary components and incidence of cancer and other chronic diseases. Participants in the study were invited using the Civil Registration System of Denmark, which assigns a unique ID to all Danish inhabitants. Using these unique IDs, data from the study participants were linked to the National Diabetes Register to facilitate the identification of incident cases of diabetes (18). This registry was complete on 1 January 1995, so we set our baseline to this date for those recruited before 1995. After excluding participants with prevalent diabetes or missing data (detailed in Supplementary Methods), 54,793 participants remained for analysis in the current study (Supplementary Fig. 1).
Vegetable Intake Assessment
Participants completed a detailed 192-item food frequency questionnaire (FFQ) at baseline. The frequency of intake reported by participants was adjusted through additional global questions specifying total intake of each food group (meat, fruit, vegetables/salads, and so on). A minutely designed recipe and portion size for each food and beverage item was used to estimate the daily intake of each food and nutrient using FoodCalc software (19). Exposures of interest in the current study were total vegetables (excluding potatoes), subgroups of vegetables, total potatoes, and potatoes based on different preparation methods (boiled, roasted, or mashed potatoes and potato fries/chips), expressed as grams per day. Individual vegetable intake was quantified from the responses to the FFQ on intake of a specific vegetable and intake of mixed dishes with standard recipes. Vegetable juices (carrot and tomato) were included in both total vegetable and vegetable subgroups. Individual vegetable intake was then categorized into the following subgroups: GLVs, cruciferous vegetables, yellow/orange/red vegetables, allium vegetables, other vegetables, and legumes, as per the recommended dietary guidelines (20,21). All vegetables, with and without the inclusion of potatoes, were summed to estimate 1) total vegetable intake and 2) total vegetable plus potato intake.
Assessment and Definition of Diabetes
A participant was considered as having diabetes based on the criteria of the National Diabetes Register, which was complete from 1995 (18). Based on the combined criteria of the National Diabetes Register (detailed in Supplementary Methods), the overall positive predictive value was 89% and the sensitivity was 86% for diabetes diagnosis defined by presence in the register (18). Studies have shown that T2D incidence is higher among those age >45 years (22), whereas T1D development is rare among adults (23). Therefore, incident diabetes cases in this study are hereafter referred to as T2D because participants were age >50 years at baseline.
Statistical Analysis
Baseline characteristics of cohort participants were summarized overall as well as according to total vegetable (excluding potatoes) intake. Two types of analyses were performed: a cross-sectional analysis and a time-to-event analysis. Firstly, a cross-sectional analysis was performed to examine the relationship between total vegetable (excluding potatoes) intake and baseline BMI; the exposure vegetable intake was fitted as quintiles, whereas BMI was fitted as a continuous response variable to obtain estimates for each quintile, considering the lowest quintile as a reference. Estimation of P values for a linear trend was achieved by the Wald test, assigning a median value for each quintile of vegetable intake and treating it as a continuous predictor. Secondly, for the time-to-event analysis, Cox proportional hazards models were used to investigate the associations of baseline intake of total vegetables (excluding potatoes), subgroups of vegetables, total potatoes, and potatoes based on different preparation methods with incident T2D.
In total, 54,793 participants underwent follow-up from baseline until either date of T2D diagnosis, death, or end of follow-up (31 December 2012), whichever came first. Baseline was first baseline visit date or 1 January 1995, whichever came last, because the National Diabetes Register was incomplete until 1995. For this analysis, continuous exposure variables were fitted as restricted cubic splines (where the median intake in the lowest quintile was considered the reference) to allow for a nonlinear relationship with the outcome variable, incident T2D. The resulting hazard ratios (HRs) (95% CIs) were graphed on the y-axis, with vegetable intake (cut at three SDs from the mean for visual simplicity) on the x-axis. HRs and 95% CIs in tables are presented for the median intake in each quintile. The χ2 test comparing nested models was used to test for nonlinearity. Log-log plots of the survival function were assessed for parallel appearance to test the assumptions of the Cox proportional hazards model, with no violations observed.
The following modeling strategy was used for the time-to-event analysis: model 1a adjusted for sex and age; model 1b adjusted for sex, age, smoking status, alcohol consumption, education level, physical activity level, and use of hormone replacement therapy (HRT); model 2 adjusted for the covariates in model 1b plus BMI; and model 3 adjusted for the covariates in model 1b plus intake of whole grains, refined grains, red meat, processed meat, poultry, dairy, fish, vegetable oil, animal fats, sugar and confectionery, soft drinks, fruit, coffee, and tea and intake of all other exposures except the exposure of interest (covariate assessment detailed in Supplementary Methods). We used an all-components model approach (i.e., adjustment for food groups specified in model 3, excluding the exposure food group), because it provides unbiased estimates compared with other methods of energy adjustment (24) and accounts for underlying dietary pattern. Covariates were selected a priori based on prior evidence of their relationship with both vegetable intake and T2D, and continuous covariates were modeled with restricted cubic splines. To examine potential effect modification by sex and BMI, multiplicative interaction terms were added to model 1b and assessed using the χ2 test comparing nested models. Furthermore, analyses were stratified by sex, and the HRs are presented. We investigated whether the association between vegetable intake (quintiles) and incident T2D was mediated by baseline BMI (continuous) when 1) the exposure was significantly inversely associated with both BMI and incident T2D and 2) the association between the exposure and incident T2D was attenuated when BMI was included as a covariate in the model. The mediation proportion was quantified using natural direct and indirect effects (25), where the natural direct effect estimated whether a substantial association would be observed if vegetable intake had no impact on BMI and the natural indirect effect estimated if vegetable intake only had an impact on T2D through its impact on BMI. For the estimation, Cox proportional hazards models within the Medflex package of R software (26) were used with bootstrapping (1,000 iterations) to compute 95% CIs.
Logistic regression models were fitted to obtain the predicted 15-year risk of T2D stratified by sex for each subgroup (BMI <30 and ≥30 kg/m2). For the risk estimate, a binary outcome of incident T2D (≤15 years) was used as a response variable; the estimate was for an average participant of the cohort, age 56 years, nonsmoking, nonuser of HRT, with a physical activity total metabolic equivalent score of 56, an alcohol intake of 13 g/day, and 8–10 years of completed education.
Furthermore, a sensitivity analysis was performed using only confirmed cases by excluding T2D cases with least sensitivity/positive predictive value (n = 1,861; 24% of cases) (detailed in Supplementary Methods). In addition, some supplementary analyses were performed to evaluate the influence of the Nordic diet index, exposure definition, and adjustment strategy for potential dietary confounders (detailed in Supplementary Methods).
The analyses were carried out in STATA/IC 16.1 (StataCorp LLC) and R statistics (R Core Team; 2021). All P values are two tailed, and the statistical significance level was set to 0.05.
Data and Resource Availability
Data described in the manuscript, codebook, and analytic code will be made available upon request pending application and approval by the DCH Steering Committee at the Danish Cancer Society.
Results
Among the 54,793 participants included in this study, 7,695 (4,243 men and 3,452 women) cases of incident T2D were recorded from the National Diabetes Register during 814,771 person-years of follow-up. The median (interquartile range [IQR]) length of follow-up was 16.3 (15.6–17.1) years.
Table 1 lists the baseline characteristics of the study participants across quintiles of total vegetable (excluding potato) intake (g/day). In the entire population, the median (IQR) intake of total vegetables was 166 (107–237) g/day. Compared with those in the lowest vegetable intake quintile, participants in the highest quintile were more likely to be female, be physically active, have a lower BMI, and have a higher education attainment and were less likely to be a current smoker. Additionally, participants in quintile 5 (Q5) of total vegetable intake had a healthier underlying dietary pattern; they consumed fewer soft drinks, less processed meat, and less animal fat and ate more whole grains, fruit, vegetable oils, fish, poultry, and dairy products compared with participants in Q1 (Supplementary Fig. 2). Likewise, participants in Q1 of potato (excluding fries/chips) intake had a comparatively healthier diet than participants in Q5 of potato intake.
Table 1.
Baseline characteristics of the DCH cohort
| Total population (N = 54,793) | Total vegetable intake quintile* | |||||
|---|---|---|---|---|---|---|
| Q1 (n = 10,959) | Q2 (n = 10,958) | Q3 (n = 10,959) | Q4 (n = 10,958) | Q5 (n = 10,959) | ||
| Total vegetable intake, g/day | 166 (107, 237) | 67 (50, 81) | 119 (107, 131) | 166 (154, 177) | 220 (204, 237) | 319 (284, 376) |
| Male sex | 25,955 (47.4) | 5,888 (53.7) | 5,650 (51.6) | 5,220 (47.6) | 5,009 (45.7) | 4,188 (38.2) |
| Age, years | 56 (52, 60) | 57 (53, 61) | 56 (52, 60) | 55 (52, 60) | 55 (52, 59) | 55 (52, 59) |
| BMI, kg/m2 | 25.5 (23.2, 28.1) | 25.9 (23.5, 28.8) | 25.7 (23.5, 28.4) | 25.5 (23.3, 28.0) | 25.3 (23.1, 27.8) | 25.1 (22.9, 27.7) |
| MET score | 56.5 (37.0, 85.0) | 49.5 (30.5, 77.8) | 54.0 (35.0, 81.5) | 56.0 (37.5, 82.5) | 59.5 (40.0, 86.8) | 64.2 (43.0, 93.9) |
| Smoking status | ||||||
| Never | 19,273 (35.2) | 3,066 (28.0) | 3,661 (33.4) | 3,987 (36.4) | 4,272 (39.0) | 4,287 (39.1) |
| Former | 15,745 (28.7) | 2,580 (23.5) | 2,969 (27.1) | 3,190 (29.1) | 3,357 (30.6) | 3,649 (33.3) |
| Current | 19,775 (36.1) | 5,313 (48.5) | 4,328 (39.5) | 3,782 (34.5) | 3,329 (30.4) | 3,023 (27.6) |
| Education, years | ||||||
| ≤7 | 17,955 (32.8) | 5,152 (47.0) | 3,994 (36.4) | 3,405 (31.1) | 2,835 (25.9) | 2,569 (23.4) |
| 8–10 | 25,300 (46.2) | 4,695 (42.8) | 5,206 (47.5) | 5,292 (48.3) | 5,251 (47.9) | 4,856 (44.3) |
| >10 | 11,538 (21.0) | 1,112 (10.1) | 1,758 (16.0) | 2,262 (20.6) | 2,872 (26.2) | 3,534 (32.2) |
| Hypertension | 8,601 (15.7) | 1,750 (16.0) | 1,711 (15.6) | 1,742 (15.9) | 1,702 (15.5) | 1,696 (15.5) |
| Hypercholesterolemia | 3,939 (7.2) | 765 (7.0) | 808 (7.4) | 797 (7.3) | 780 (7.1) | 789 (7.2) |
| Medication use | ||||||
| NSAIDs including aspirin | 17,753 (32.6) | 3,412 (31.4) | 3,455 (31.7) | 3,509 (32.2) | 3,648 (33.5) | 3,729 (34.2) |
| Antihypertensives | 6,444 (11.8) | 1,329 (12.1) | 1,304 (11.9) | 1,307 (11.9) | 1,236 (11.3) | 1,268 (11.6) |
| Statins | 989 (1.8) | 184 (1.7) | 200 (1.8) | 190 (1.7) | 210 (1.9) | 205 (1.9) |
| HRT use (women only) | ||||||
| Never | 15,653 (54.3) | 2,775 (54.7) | 2,881 (54.3) | 3,071 (53.5) | 3,255 (54.7) | 3,671 (54.2) |
| Current | 8,690 (30.1) | 1,478 (29.1) | 1,580 (29.8) | 1,758 (30.6) | 1,820 (30.6) | 2,054 (30.3) |
| Former | 4,466 (15.5) | 810 (16.0) | 840 (15.8) | 910 (15.9) | 867 (14.6) | 1,039 (15.4) |
| Unknown | 29 (0.1) | 8 (0.2) | 7 (0.1) | 0 (0.0) | 7 (0.1) | 7 (0.1) |
| Menopause (women only) | ||||||
| Postmenopausal | 16,934 (58.7) | 3,211 (63.3) | 3,211 (60.5) | 3,380 (58.9) | 3,341 (56.2) | 3,791 (56.0) |
| Premenopausal | 4,721 (16.4) | 626 (12.4) | 828 (15.6) | 928 (16.2) | 1,115 (18.7) | 1,224 (18.1) |
| Unknown | 7,183 (24.9) | 1,234 (24.3) | 1,269 (23.9) | 1,431 (24.9) | 1,493 (25.1) | 1,756 (25.9) |
| Dietary characteristics | ||||||
| Energy, kcal/day | 2,270 (1,877, 2,717) | 2,041 (1,667, 2,461) | 2,189 (1,809, 2,612) | 2,256 (1,894, 2,690) | 2,367 (1,989, 2,811) | 2,493 (2,088, 2,971) |
| Intake, g/day | ||||||
| Whole grains | 127 (86, 175) | 112 (67, 159) | 119 (81, 167) | 131 (90, 174) | 139 (102, 186) | 152 (109, 199) |
| Refined grains | 46 (29, 73) | 44 (26, 85) | 46 (29, 73) | 45 (29, 69) | 47 (31, 71) | 48 (32, 70) |
| Red meat | 78 (56, 107) | 72 (53, 96) | 79 (58, 106) | 81 (60, 109) | 82 (59, 112) | 78 (54, 113) |
| Processed meat | 25 (14, 40) | 28 (17, 45) | 27 (16, 42) | 25 (15, 39) | 23 (13, 37) | 20 (11, 35) |
| Total dairy | 296 (156, 561) | 261 (116, 549) | 280 (144, 554) | 293 (157, 545) | 314 (178, 567) | 339 (202, 594) |
| Total fish | 38 (25, 55) | 29 (19, 43) | 35 (24, 50) | 39 (27, 55) | 42 (29, 59) | 47 (32, 68) |
| Poultry | 18 (10, 27) | 12 (7, 19) | 16 (10, 25) | 19 (12, 28) | 21 (13, 32) | 24 (14, 37) |
| Vegetable oils | 5 (1, 9) | 1 (1, 2) | 2 (1, 6) | 5 (2, 8) | 6 (2, 11) | 9 (5, 13) |
| Animal fats | 10 (1, 21) | 13 (3, 23) | 11 (3, 22) | 11 (2, 21) | 10 (1, 21) | 7 (1, 19) |
| Sugar and confectionery | 47 (27, 78) | 43 (23, 75) | 46 (27, 76) | 47 (28, 78) | 48 (29, 79) | 49 (28, 81) |
| Soft drinks | 8 (1, 29) | 17 (2, 31) | 16 (3, 30) | 8 (2, 29) | 7 (1, 29) | 6 (1, 18) |
| Coffee | 900 (500, 1,300) | 900 (500, 1,300) | 900 (500, 1,300) | 900 (500, 1,300) | 900 (500, 1,300) | 500 (500, 900) |
| Tea | 86 (3, 500) | 16 (0, 200) | 29 (3, 500) | 86 (7, 500) | 157 (16, 500) | 200 (16, 500) |
| Fruit | 170 (93, 280) | 104 (45, 185) | 143 (78, 233) | 171 (102, 270) | 196 (122, 301) | 252 (156, 386) |
| Alcohol | 13 (6, 31) | 12 (3, 31) | 13 (6, 31) | 14 (7, 31) | 14 (7, 31) | 13 (6, 30) |
Values are given as median (IQR) or n (%).
HRT, hormone replacement therapy; MET, metabolic equivalent; NSAID, nonsteroidal anti-inflammatory drug.
Total vegetable intake, excluding potatoes.
The vegetable-eating pattern of this population was characterized by a high intake of potatoes, followed by yellow/orange/red vegetables; legumes were the least consumed (Supplementary Fig. 3). The median (IQR) intake of the three most consumed vegetables in this population was as follows: potatoes, 125 (80–182); tomatoes, 37 (23–55); and carrots, 21 (10–49) g/day (Supplementary Fig. 4). Boiled potatoes were the most commonly consumed form of potatoes in this population. The median (IQR) and percentage intake of the different potato forms (excluding fries/chips) were as follows: boiled potatoes, 96 (54–125) and 68; mashed potatoes, 12 (6–16) and 12; roasted potatoes, 12 (3–16) and 10; and other forms of potatoes or potatoes from mixed dishes, 10 (4–18) g/day and 10%. Potato fries/chips were the least consumed form in this population (2 [1–5] g/day).
Association Between Vegetable Intake and Incident T2D
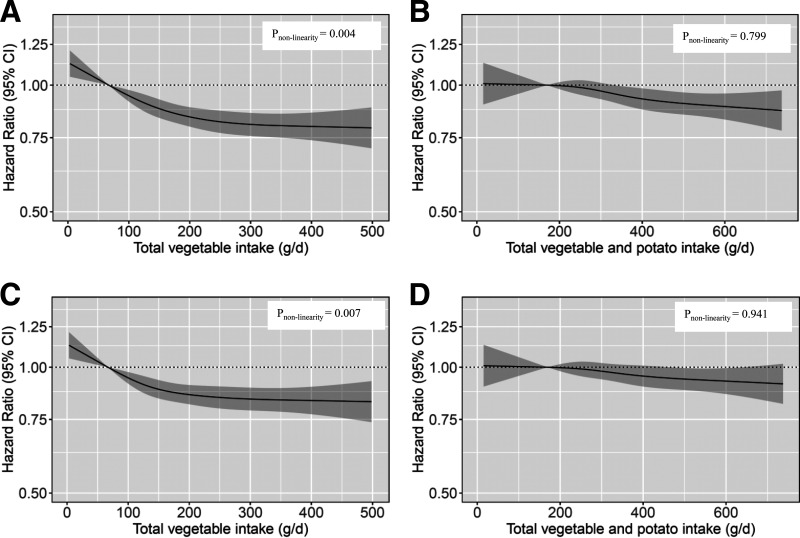
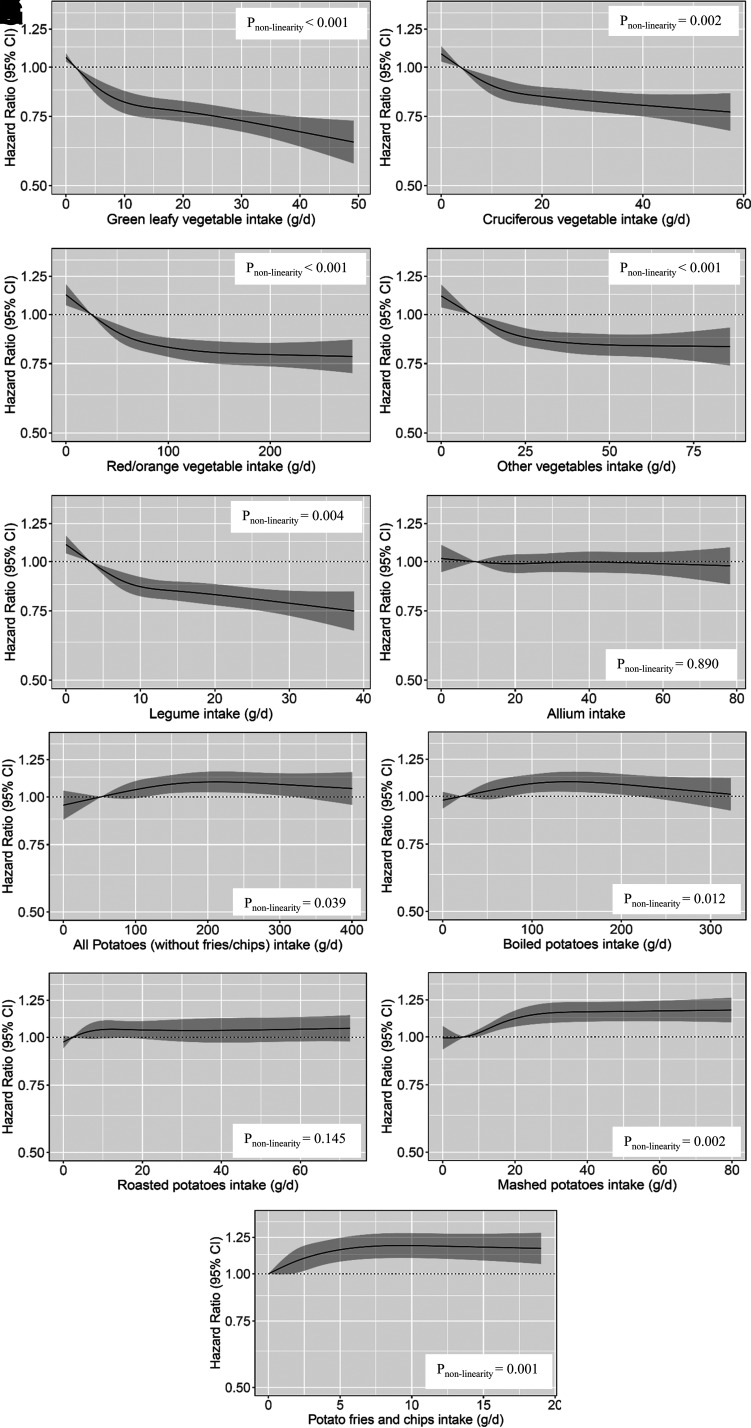
The association between total vegetable intake and incident T2D was inverse and nonlinear (P < 0.001 for nonlinearity) (Fig. 1); the steepness of the association was greater for lower levels of vegetable intake (<150 g/day), after which the gradient declined, and the association reached a plateau. After multivariable adjustment (model 1b), participants in the highest total vegetable intake quintile had a 21% lower risk of T2D (HRQ5vs.Q1 0.79; 95% CI 0.74, 0.84) compared with participants in the lowest quintile (Table 2). When BMI was included as an adjustment covariate, the risk of T2D was 18% lower for participants in the highest versus lowest quintile of vegetable intake (Fig. 1 and Table 2). As can be seen in Fig. 1, when potatoes were included in the estimate of total vegetable intake, participants in the highest quintile had an 11% lower risk of T2D compared with those in the lowest quintile (HRQ5vs.Q1 0.89; 95% CI 0.84, 0.95) (Table 2). For all subgroups of vegetables, except allium vegetables, participants in Q5 had a lower risk of incident T2D when compared with participants in Q1 (Fig. 2 and Table 2) after adjusting for demographic and lifestyle confounders (model 1b). On the contrary, the association remained inverse and significant only for GLVs and cruciferous vegetables after adjustment for potential dietary confounders (model 3).
Figure 1.
A–D: HRs based on cubic splines for the association between quintile of total vegetable intake (g/day) with (B and D) and without (A and C) potatoes, excluding BMI (model 1b) (A and B) and including BMI (model 2) (C and D) as a covariate with incident diabetes among participants in the DCH study (N = 54,793). HRs are based on a Cox proportional hazards model adjusted for sex, age, physical activity, smoking status, alcohol status, education level, and hormone replacement therapy and compare the amount of vegetable intake with the median intake in Q1. The χ2 test was used to obtain P values for nonlinearity comparing the nested models.
Table 2.
HRs of incident diabetes by quintile of vegetable and potato intake
| Quintile | |||||
|---|---|---|---|---|---|
| Q1 (n = 10,959) | Q2 (n = 10,958) | Q3 (n = 10,959) | Q4 (n = 10,958) | Q5 (n = 10,959) | |
| Vegetable intake | |||||
| Total vegetables | |||||
| N of events | 1,928 | 1,674 | 1,468 | 1,363 | 1,262 |
| Intake, g/day | 67 (0–94) | 119 (94–142) | 166 (142–190) | 220 (190–257) | 319 (257–1,739) |
| Model 1a | Ref | 0.84 (0.81, 0.88) | 0.75 (0.72, 0.79) | 0.69 (0.66, 0.73) | 0.65 (0.61, 0.69) |
| Model 1b | Ref | 0.91 (0.87, 0.95) | 0.86 (0.82, 0.91) | 0.82 (0.78, 0.87) | 0.79 (0.74, 0.84) |
| Model 2 | Ref | 0.91 (0.87, 0.96) | 0.87 (0.83, 0.92) | 0.85 (0.80, 0.90) | 0.82 (0.77, 0.88) |
| Model 3 | Ref | 0.90 (0.86, 0.95) | 0.85 (0.80, 0.90) | 0.82 (0.76, 0.88) | 0.78 (0.72, 0.85) |
| Total vegetables and potatoes | |||||
| N of events | 1,656 | 1,595 | 1,486 | 1,525 | 1,433 |
| Intake, g/day | 170 (0–212) | 246 (212–276) | 307 (276–339) | 377 (339–425) | 498 (425–2,119) |
| Model 1a | Ref | 0.93 (0.89, 0.97) | 0.88 (0.84, 0.92) | 0.85 (0.80, 0.89) | 0.81 (0.76, 0.86) |
| Model 1b | Ref | 0.99 (0.95, 1.03) | 0.96 (0.92, 1.01) | 0.93 (0.88, 0.99) | 0.89 (0.84, 0.95) |
| Model 2 | Ref | 0.99 (0.95, 1.03) | 0.97 (0.93, 1.02) | 0.95 (0.90, 1.01) | 0.93 (0.87, 0.98) |
| Model 3 | Ref | 0.97 (0.93, 1.02) | 0.95 (0.90, 1.00) | 0.92 (0.87, 0.98) | 0.89 (0.83, 0.95) |
| GLVs | |||||
| N of events | 1,997 | 1,642 | 1,501 | 1,337 | 1,218 |
| Intake, g/day | 2 (0–3) | 5 (3–6) | 9 (6–14) | 19 (14–22) | 29 (22–157) |
| Model 1a | Ref | 0.84 (0.80, 0.87) | 0.71 (0.67, 0.76) | 0.65 (0.61, 0.68) | 0.60 (0.57, 0.64) |
| Model 1b | Ref | 0.91 (0.87, 0.94) | 0.83 (0.78, 0.88) | 0.78 (0.73, 0.82) | 0.74 (0.69, 0.78) |
| Model 2 | Ref | 0.92 (0.88, 0.96) | 0.86 (0.81, 0.92) | 0.84 (0.79, 0.89) | 0.81 (0.76, 0.87) |
| Model 3 | Ref | 0.96 (0.91, 1.01) | 0.92 (0.84, 1.00) | 0.88 (0.80, 0.97) | 0.84 (0.76, 0.94) |
| Cruciferous vegetables | |||||
| N of events | 1,867 | 1,611 | 1,498 | 1,446 | 1,273 |
| Intake, g/day | 4 (0–6) | 8 (6–11) | 15 (11–18) | 22 (18–26) | 34 (26–186) |
| Model 1a | Ref | 0.86 (0.83, 0.90) | 0.76 (0.72, 0.80) | 0.73 (0.69, 0.77) | 0.69 (0.65, 0.74) |
| Model 1b | Ref | 0.92 (0.88, 0.96) | 0.86 (0.81, 0.91) | 0.84 (0.79, 0.89) | 0.81 (0.76, 0.86) |
| Model 2 | Ref | 0.93 (0.89, 0.97) | 0.88 (0.83, 0.93) | 0.87 (0.82, 0.92) | 0.85 (0.80, 0.90) |
| Model 3 | Ref | 0.96 (0.91, 1.01) | 0.93 (0.86, 1.01) | 0.92 (0.85, 1.00) | 0.91 (0.83, 0.99) |
| Yellow/orange/red vegetables | |||||
| N of events | 1,921 | 1,632 | 1,493 | 1,379 | 1,270 |
| Intake, g/day | 25 (0–36) | 47 (36–57) | 68 (57–81) | 98 (81–120) | 159 (120–1,377) |
| Model 1a | Ref | 0.84 (0.81, 0.88) | 0.76 (0.72, 0.80) | 0.71 (0.67, 0.75) | 0.67 (0.63, 0.72) |
| Model 1b | Ref | 0.91 (0.88, 0.95) | 0.86 (0.82, 0.91) | 0.83 (0.78, 0.87) | 0.80 (0.75, 0.85) |
| Model 2 | Ref | 0.92 (0.88, 0.96) | 0.87 (0.83, 0.92) | 0.85 (0.81, 0.90) | 0.83 (0.78, 0.89) |
| Model 3 | Ref | 0.97 (0.92, 1.03) | 0.95 (0.89, 1.03) | 0.94 (0.87, 1.02) | 0.92 (0.84, 1.01) |
| Allium vegetables | |||||
| N of events | 1,681 | 1,543 | 1,523 | 1,524 | 1,424 |
| Intake, g/day | 9 (0–13) | 15 (13–19) | 23 (19–28) | 32 (28–39) | 51 (39–184) |
| Model 1a | Ref | 0.94 (0.90, 0.98) | 0.90 (0.85, 0.95) | 0.89 (0.84, 0.94) | 0.88 (0.83, 0.93) |
| Model 1b | Ref | 0.99 (0.95, 1.03) | 0.99 (0.94, 1.05) | 1.00 (0.94, 1.05) | 0.99 (0.93, 1.06) |
| Model 2 | Ref | 0.98 (0.94, 1.02) | 0.96 (0.91, 1.02) | 0.96 (0.91, 1.01) | 0.94 (0.88, 1.00) |
| Model 3 | Ref | 1.02 (0.97, 1.08) | 1.05 (0.98, 1.13) | 1.08 (1.01, 1.16) | 1.11 (1.02, 1.20) |
| Other vegetables | |||||
| N of events | 1,825 | 1,635 | 1,497 | 1,387 | 1,351 |
| Intake, g/day | 9 (0–12) | 15 (12–19) | 22 (19–26) | 31 (26–38) | 48 (38–176) |
| Model 1a | Ref | 0.86 (0.83, 0.90) | 0.77 (0.73, 0.81) | 0.72 (0.69, 0.77) | 0.69 (0.65, 0.73) |
| Model 1b | Ref | 0.93 (0.89, 0.97) | 0.88 (0.83, 0.92) | 0.85 (0.80, 0.90) | 0.83 (0.78, 0.89) |
| Model 2 | Ref | 0.92 (0.88, 0.96) | 0.88 (0.84, 0.93) | 0.88 (0.83, 0.93) | 0.86 (0.81, 0.92) |
| Model 3 | Ref | 0.94 (0.88, 0.99) | 0.92 (0.84, 1.00) | 0.94 (0.85, 1.03) | 0.97 (0.86, 1.10) |
| Legumes | |||||
| N of events | 1880 | 1621 | 1456 | 1408 | 1330 |
| Intake, g/d | 3 (0 − 5) | 7 (5 − 9) | 11 (9 − 13) | 16 (13 − 19) | 24 (19 − 119) |
| Model 1a | Ref | 0.84 (0.80, 0.88) | 0.75 (0.71, 0.79) | 0.72 (0.68, 0.76) | 0.69 (0.65, 0.73) |
| Model 1b | Ref | 0.91 (0.87, 0.95) | 0.86 (0.81, 0.90) | 0.84 (0.79, 0.89) | 0.81 (0.76, 0.86) |
| Model 2 | Ref | 0.91 (0.87, 0.95) | 0.87 (0.82, 0.92) | 0.87 (0.82, 0.92) | 0.84 (0.79, 0.90) |
| Model 3 | Ref | 0.99 (0.93, 1.06) | 0.99 (0.90, 1.09) | 0.99 (0.90, 1.10) | 0.97 (0.87, 1.09) |
| Potato intake | |||||
| All potatoes (except fries/chips) | |||||
| N of events | 1,385/10,959 | 1,404/10,958 | 1,511/10,959 | 1,611/10,959 | 1,784/10,958 |
| Intake, g/day | 52 (0–73) | 87 (73–110) | 125 (110–142) | 163 (142–203) | 256 (203–1,332) |
| Model 1a | Ref | 1.00 (0.96, 1.05) | 1.04 (0.99, 1.10) | 1.10 (1.04, 1.16) | 1.15 (1.08, 1.22) |
| Model 1b | Ref | 1.03 (0.99, 1.08) | 1.07 (1.01, 1.13) | 1.09 (1.03, 1.15) | 1.09 (1.02, 1.16) |
| Model 2 | Ref | 1.03 (0.98, 1.08) | 1.07 (1.01, 1.13) | 1.11 (1.05, 1.17) | 1.12 (1.05, 1.19) |
| Model 3 | Ref | 1.01 (0.96, 1.06) | 1.03 (0.97, 1.09) | 1.05 (0.99, 1.11) | 1.04 (0.98, 1.12) |
| Boiled potatoes | |||||
| N of events | 1,653/12,662 | 1,614/12,628 | 1,144/8,489 | 1,623/10,685 | 1,661/10,329 |
| Intake, g/d | 21 (0–39) | 54 (46–54) | 96 (57–96) | 125 (98–139) | 225 (171–1,000) |
| Model 1a | Ref | 1.00 (0.95, 1.06) | 1.07 (1.02, 1.13) | 1.12 (1.05, 1.18) | 1.13 (1.06, 1.21) |
| Model 1b | Ref | 1.04 (0.98, 1.09) | 1.08 (1.02, 1.14) | 1.10 (1.03, 1.16) | 1.06 (1.00, 1.14) |
| Model 2 | Ref | 1.04 (0.98, 1.09) | 1.10 (1.04, 1.16) | 1.12 (1.05, 1.19) | 1.10 (1.03, 1.17) |
| Model 3 | Ref | 1.01 (0.96, 1.07) | 1.05 (0.99, 1.11) | 1.06 (1.00, 1.13) | 1.03 (0.96, 1.10) |
| Mashed potatoes | |||||
| N of events | 1,903/15,945 | 1,339/8,974 | 1,119/9,120 | 2,093/13,376 | 1,241/7,378 |
| Intake, g/day | 6 (0–6) | 8 (8–8) | 12 (12–12) | 16 (16–30) | 39 (39–369) |
| Model 1a | Ref | 1.01 (1.00, 1.02) | 1.05 (1.02, 1.08) | 1.09 (1.05, 1.13) | 1.19 (1.12, 1.26) |
| Model 1b | Ref | 1.01 (1.00, 1.02) | 1.04 (1.02, 1.07) | 1.08 (1.04, 1.12) | 1.16 (1.09, 1.23) |
| Model 2 | Ref | 1.00 (0.99, 1.02) | 1.03 (1.00, 1.06) | 1.06 (1.02, 1.10) | 1.13 (1.06, 1.20) |
| Model 3 | Ref | 1.00 (0.99, 1.02) | 1.02 (0.99, 1.04) | 1.03 (0.99, 1.07) | 1.07 (1.00, 1.14) |
| Roasted potatoes | |||||
| N of events | 1,912/14,642 | 1,709/12,118 | 922/7,624 | 1,870/12,319 | 1,282/8,090 |
| Intake, g/day | 2 (0–3) | 5 (5–6) | 12 (12–12) | 16 (16–21) | 27 (27–190) |
| Model 1a | Ref | 1.02 (0.99, 1.05) | 1.05 (0.99, 1.11) | 1.05 (1.00, 1.10) | 1.06 (0.99, 1.13) |
| Model 1b | Ref | 1.03 (1.00, 1.06) | 1.06 (1.00, 1.12) | 1.06 (1.01, 1.11) | 1.05 (0.99, 1.12) |
| Model 2 | Ref | 1.03 (1.00, 1.06) | 1.06 (1.00, 1.12) | 1.06 (1.00, 1.11) | 1.05 (0.98, 1.12) |
| Model 3 | Ref | 1.00 (0.97, 1.03) | 0.99 (0.93, 1.04) | 0.98 (0.93, 1.03) | 0.97 (0.90, 1.03) |
| Potato fries/chips | |||||
| N of events | 1,432/11,168 | 1,586/12,276 | 1,603/10,493 | 1,443/10,209 | 1,631/10,647 |
| Intake, g/day | 0 (0–1) | 2 (1–2) | 2 (2–3) | 4 (3–7) | 8 (7–84) |
| Model 1a | Ref | 1.08 (1.01, 1.17) | 1.09 (1.01, 1.18) | 1.12 (1.04, 1.21) | 1.14 (1.06, 1.23) |
| Model 1b | Ref | 1.11 (1.03, 1.19) | 1.12 (1.04, 1.21) | 1.17 (1.09, 1.26) | 1.20 (1.12, 1.30) |
| Model 2 | Ref | 1.05 (0.97, 1.13) | 1.05 (0.98, 1.14) | 1.08 (1.00, 1.16) | 1.10 (1.02, 1.19) |
| Model 3 | Ref | 1.07 (1.00, 1.16) | 1.08 (1.00, 1.17) | 1.08 (1.00, 1.17) | 1.08 (0.99, 1.18) |
Values are given as n, n/N, median (IQR), or HR (95% CI). HRs for the association between quintile of vegetable and potato intake (g/day) and incident diabetes among participants of DCH study (N = 54,793) derived from restricted cubic splines based on Cox proportional hazards model. Model 1a adjusted for sex and age; model 1b adjusted for sex, age, physical activity, smoking status, alcohol status, education level, and hormone replacement therapy; model 2 adjusted for covariates in model 1b plus BMI; and model 3 adjusted for covariates in model 1b plus intake (g/day) of whole grains, refined grains, red meat, processed meat, poultry, fish, dairy, vegetable oil, animal fats, sugar and confectionery, soft drinks, fruit, tea, and coffee and intake of other exposures, except the exposure of interest.
Figure 2.
A–K: HRs based on cubic splines for the association between quintile of vegetable/potato intake (g/day) with incident diabetes among participants in the DCH study (N = 54,793): GLV (A), cruciferous vegetable (B), red/orange vegetable (C), other vegetable (D), legume (E), allium (F), all potato (except fries/chips) (G), boiled potato (H), roasted potato (I), mashed potato (J), and potato fries/chips (K) intake. HRs are based on a Cox proportional hazards model adjusted for sex, age, physical activity, smoking status, alcohol status, education level, and hormone replacement therapy and compare the amount of vegetable/potato intake with the median intake in Q1. The χ2 test was used to obtain P values for nonlinearity comparing the nested models.
Conversely, total potato (excluding fries/chips) intake was nonlinearly positively associated with incident T2D (Fig. 2); a 9% higher risk of T2D was observed for participants in Q5 compared with those in Q1 (HRQ5vs.Q1 1.09; 95% CI 1.02, 1.16; model 1b) (Table 3). When considering different preparation methods, intake of potato fries/chips as well as boiled, roasted, and mashed potatoes was positively associated with incident T2D (Fig. 2). All were statistically significant, except for roasted potatoes. However, after accounting for underlying dietary pattern by adjustment for food groups, only mashed potatoes and potato fries/chips were statistically significant and positively associated with T2D. The association was positive but nonsignificant for total potatoes (excluding fries/chips) and boiled potatoes (model 3) (Table 2). A sensitivity analysis including only confirmed cases (Supplementary Table 1) strengthened the association of total vegetable (excluding potatoes) intake and T2D but diminished it for potato intake and T2D.
Table 3.
15-year predicted risk of diabetes
| BMI, kg/m2 | Total vegetable intake | ||
|---|---|---|---|
| Q1 risk (95% CI), % | Q5 risk (95% CI), % | Risk difference, % | |
| Men | |||
| >18.5 and <30 | 11.12 (10.30, 11.98) | 8.90 (8.17, 9.68) | 2.22 |
| ≥30 | 32.59 (30.60, 34.65) | 27.41 (25.46, 29.44) | 5.18 |
| Women | |||
| >18.5 and <30 | 8.24 (7.60, 8.93) | 6.55 (6.02, 7.13) | 1.69 |
| ≥30 | 25.78 (24.03, 27.60) | 21.33 (19.75, 23.01) | 4.45 |
The 15-year predicted risk (%) of diabetes is based on logistic regression model. Estimates are for a nonsmoking participant, age 56 years, who has completed 8–10 years of education, has a total daily metabolic equivalent score of 56, has an alcohol intake of 13 g/day, and is not taking hormone replacement therapy unless denoted by the stratification variable.
Mediation Analysis Between Vegetable Intake and BMI
The cross-sectional analysis between vegetables and BMI showed that their relationship was inverse and linear (P < 0.001 for trend) after multivariable adjustment (Supplementary Table 2). Participants in Q5 had a 0.35 (95% CI −0.46, −0.24) kg/m2 lower BMI than participants in Q1 of total vegetable intake (model 1b). This inverse relationship was present between all vegetable subgroups and BMI, except allium vegetables, where the relationship was positive and linear (P < 0.001 for trend).
The mediation analysis showed that BMI partially mediated the association between vegetable intake and T2D. After multivariable adjustment, 21% (95% CI 12, 29%) of the association between total vegetable intake and T2D was mediated through baseline BMI (model 1b) (Supplementary Table 3). Among the vegetable subgroups that showed inverse associations with both baseline BMI and incident T2D, the mediation explained by BMI was highest for the association between GLVs (mediation proportion 36%; 95% CI 28, 43%) and lowest for other vegetables (mediation proportion 14%; 95% CI 13, 34%) and incident T2D.
Association Between Vegetable Intake and Incident T2D Upon Stratification
The association between vegetable intake and T2D was present among both men (HRQ5vs.Q1 0.76; 95% CI 0.70, 0.83) and women (HRQ5vs.Q1 0.83; 95% CI 0.75, 0.91; P > 0.05 for interaction). For baseline BMI (P = 0.007 for interaction), on an absolute scale, the difference in the estimated risk of T2D was higher among participants with a BMI ≥30 (5.2% men; 4.5% women) (Table 3) than among participants with a BMI <30 kg/m2 (2.2% men; 1.7% women).
Upon stratification by healthy Nordic diet index categories, the associations remained inverse for vegetable intake and incident T2D across the categories (Supplementary Table 4). The exclusion of legumes from total vegetables slightly attenuated the association between vegetable intake and incident T2D, but the association remained inverse and significant. The conventional adjustment method of including total energy intake and the healthy Nordic diet index instead of all component models strengthened the associations between vegetable and potato intake and incident T2D (Supplementary Table 5). Further adjustment for fiber (g/day) and glycemic index attenuated the association between vegetable intake and incident T2D, but the association remained inverse and significant. However, further adjustment for fiber and glycemic index did not change the association between potato intake and incident T2D (Supplementary Table 5).
Conclusions
In this prospective study of 54,793 participants with 7,695 cases of incident T2D, we observed that a higher intake of total vegetables (excluding potatoes) was inversely associated with incident T2D. Upon adjustment for demographic and lifestyle confounders, participants in the highest versus lowest quintile of vegetable intake had a 21% lower risk of T2D; this association plateaued at a vegetable intake of 150–250 g/day. Higher intake of GLVs and cruciferous vegetables was inversely associated with T2D after accounting for underlying dietary pattern. On the contrary, total potato intake was not significantly associated with T2D after accounting for underlying dietary pattern. Furthermore, higher total vegetable intake and vegetable subgroup intake were inversely associated with baseline BMI, and baseline BMI partially mediated the inverse association of total vegetable and vegetable subgroup intake with incident T2D.
Prior observational studies reported discordant findings for the association between total vegetable intake and incident T2D. The most recent meta-analysis summarizing these studies only observed a significantly lower risk of T2D when vegetable intake was modeled as a cubic spline, with a 12–14% lower risk observed for vegetable intake between 200 and 400 g/day (9). This finding of a nonlinear association is somewhat similar to the results of our study, where the inverse association was steeper for lower intake, and no further decrease in risk was observed for total vegetable intake >250 g/day. Among the pooled prospective studies, only a large U.S.-based cohort (NIH-AARP [National Institutes of Health–AARP] cohort; N = 401,909) (27) and a cohort of Chinese women (Shanghai Women’s Study; N = 64,191) (28) reported a lower risk of T2D with higher total vegetable intake. Although the median vegetable intake in both the NIH-AARP study and Shanghai Women’s Study (median 256 and 236 g/day, respectively (9)) was higher compared with that in our study (median 166 g/day), both studies observed a plateau in the association at intake above the median, which is somewhat similar to our findings. These findings suggest that higher intake beyond a threshold may not provide added benefits for lowering the risk of T2D. This is important because a recent review showed that almost 90% of countries (119 of 136) have an average vegetable intake below the World Health Organization recommendation (≥240 g/day) (29), and the nonlinear nature of the association observed in our study suggests that individuals with a very low intake of vegetables at baseline will likely benefit the most by increasing their vegetable intake. In addition, we observed that individuals with a higher vegetable intake had a healthier underlying dietary pattern but that the association between vegetable intake and T2D was still inverse and significant after accounting for all other dietary components. In regard to vegetable subgroups, only the Shanghai Women’s Study (28) observed a lower risk of T2D for higher intake of different vegetable subgroups, namely GLVs, tomatoes, and cruciferous, yellow, allium, and other vegetables. Conversely, we observed a positive association for allium vegetables, which may be because intake of allium vegetables from meat dishes was high in our study, and higher meat consumption is associated with higher incidence of T2D (10). Contrarily, the 2021 meta-analysis observed no association between the vegetable subgroups and incident T2D, which could be due to fewer prospective studies reporting the association between vegetable subgroups and incident T2D (two to eight studies for vegetable subgroups vs. 17 studies for total vegetables) (9).
In our study, total potato intake seemed to be associated with the higher risk of T2D. However, participants with higher potato intake also had a higher consumption of foods linked to a higher risk of T2D, such as refined grains, red and processed meat, and soft drinks (10). This association with potatoes was attenuated after accounting for underlying dietary pattern. When considering different preparation methods for potatoes in our study, the association between boiled potatoes and T2D was attenuated, whereas associations remained significant for mashed potatoes and potato fries/chips, even after accounting for underlying dietary pattern. A study of three U.S.-based cohorts reported weak positive associations between boiled/baked/mashed potato intake and T2D, but adjustment for the underlying diet of participants in this U.S. study was based on either dietary score or fewer food groups (30) when compared with our study. The all-components model used in our study provides an unbiased estimate of the effect of the exposures on outcome, regardless of confounding by common dietary causes (24). This U.S.-based study had substantial influence in the 2019 and 2021 meta-analyses (9,10), leading to a significant direct association between total potato intake and incident T2D, which could be misleading. Our findings on all potatoes (excluding fried/chips) are in agreement with those of a recent U.S.-based Framingham Offspring study (31), which observed no association of potatoes with incident T2D. However, their findings on the null association of fried potatoes with incident T2D are uncommon and require replication in other studies. Although potatoes have a high glycemic index and have been suggested to increase body weight when consumed in excess (32), preparation methods of potatoes and meal context (how and with which other foods the potatoes are consumed) affect total calorie intake, glycemic load, energy density (calories consumed per gram of food), trans fats, acrylamide formation, and association with health outcomes. Additionally, an intervention study observed that the glycemic/insulinemic response to mashed potatoes was influenced by other foods consumed in concert, such as salad, protein, and fat content of the meal, indicating that meal context affects biological response (33). Comparatively, boiled potatoes eaten without added fats provide fewer calories and may be a healthier option to maintain a healthy weight than mashed potatoes (which are often eaten with added butter) or potato fries/chips (which are high in unhealthy fats), because being overweight or obese is a risk factor for T2D. Furthermore, potatoes are rich in nutrients (34), and substituting refined grains such as white bread/rice with plain boiled potatoes might be a healthier choice; however, additional studies are required to evaluate the substitution effect. In fact, a 4-week single-blind randomized clinical crossover trial suggested better diet quality and no difference in cardiometabolic health upon replacement of refined grains with steamed/baked potatoes (35). Our findings suggest that potato intake may have a null effect, whereas vegetables seem to protect against T2D.
The biological mechanism for the inverse association between vegetable consumption and T2D is not yet completely understood. However, findings from preclinical studies suggest that an increase in vegetable intake might help reduce body weight, plasma glucose, and insulin resistance, thereby regulating glucose-insulin homeostasis and preventing diabetes (36,37). Prior preclinical and prospective studies stated that the beneficial effects of vegetables might be due to the various bioactive components present in vegetables, such as vitamin E (37), sulforaphane (36), α-carotene, β-carotene, and vitamin C (8). A recent study from eight European countries suggested that, rather than a single nutrient or phytochemical, several bioactives in vegetables work together to create a synergistic effect and help lower T2D risk (8). Although it is well established that inflammatory markers play crucial roles in the pathogenesis of T2D (38), a 2021 European study showed that higher vegetable intake was associated with better inflammatory profiles and that this was mediated through the gut microbiome (39). Vegetables are also a rich source of fiber, providing little to no energy, which helps to reduce overall energy consumption and thereby prevent weight gain (40). However, our findings on further adjustment for fiber and glycemic index should be interpreted with caution. Dietary fiber is a component of food groups such as vegetables, fruit, and whole grains, and a high degree of multicollinearity exists among fiber/other nutrients and food groups, making the study findings difficult to interpret. We further observed that BMI could be a potential mediator, and our finding is in agreement with those of a prior prospective study (13), which suggested that BMI likely lies on the causal pathway of the association between vegetable intake and T2D.
Our study has several unique strengths. They include a large sample size; a prospective study design with 18 years of follow-up; accumulation of sufficient cases using a credible diabetes register, providing enough power to observe the association; minimal loss to follow-up; a homogenous population; detailed data on vegetable intake; and availability of relevant lifestyle and potential dietary confounders, reducing the source of bias and confounding. Furthermore, we show that inverse associations between vegetable intake and diabetes are present across the categories of the healthy Nordic diet index, suggesting that the associations are not simply driven by a healthier/unhealthier underlying dietary pattern. On the other hand, the limitations of the study need to be considered while interpreting the results. Firstly, vegetable intake was assessed by self-reported FFQ, and any errors in the estimation of vegetable intake would likely bias our associations toward null. Secondly, the exposure was estimated at baseline only, and participants might have changed their diet during the long follow-up period, which would introduce estimation error that would likely bias the observed associations toward null. In addition, BMI was measured only at baseline, and changes in BMI could not be accounted for, which introduces uncertainty into the temporality of the cross-sectional and mediation analyses. Thirdly, the National Diabetes Register does not distinguish between T1D and T2D; however, given the age range of the cohort (50–64 years at baseline), a vast majority of the incident cases were assumed to be T2D. Furthermore, given the prospective nature of the cohort, conclusions regarding the causal link between vegetable intake and T2D cannot be made. Lastly, the observed inverse association between vegetables and T2D could be in part due to some participants’ better socioeconomic setting, healthier lifestyle, and comparatively healthier dietary pattern, for which we could not account. Although we adjusted for all potential dietary confounders, residual confounding cannot be ruled out.
In conclusion, a higher intake of total vegetables, GLVs, and cruciferous vegetables was statistically significantly associated with a lower risk of incident T2D, whereas a higher intake of mashed potatoes and potato fries/chips was statistically significantly associated with a higher risk of incident T2D, even after accounting for underlying dietary pattern. BMI partially mediated the association between vegetable intake and incident T2D; therefore, prior cohort studies including BMI as a covariate likely undermined the association between vegetable intake and T2D. Because total potato intake was not associated and vegetable intake was inversely associated with T2D, the inclusion of potato intake within the total vegetable category in studies may mask the association between vegetable intake and T2D. In addition, both preparation method and meal context are important when evaluating the association between potatoes and T2D. Accounting for underlying dietary pattern is crucial when observing the relationship between dietary exposures and risk of disease incidence. The findings support current dietary recommendations encouraging the increased consumption of vegetables other than potatoes to reduce overweight and obesity and subsequent T2D risk.
Article Information
Acknowledgments. The authors thank Peter Fjeldstad Hendriksen, Danish Cancer Society Research Center, for data management.
Funding. The DCH study was funded by the Danish Cancer Society, Copenhagen, Denmark. P.P. is funded by the Edith Cowan University Higher Degree by Research Scholarship, Perth, Australia. The salary of L.C.B. is supported by a National Health and Medical Research Council of Australia Emerging Leadership Investigator Grant (1172987) and a National Heart Foundation of Australia Postdoctoral Research Fellowship (102498). The salary of C.P.B. is supported by the Royal Perth Hospital Research Foundation Lawrie Beilin Career Advancement Fellowship (CAF 127/2020). The salary of J.M.H. is supported by a National Health and Medical Research Council of Australia Senior Research Fellowship (APP1116937).
Duality of Interest. No potential conflicts of interest relevant to this article were reported.
Author Contributions. P.P. designed the study and analysis plan, analyzed the data, and wrote the original manuscript. C.K. and A.O. supported the planning of some analyses. A.T. conducted the original cohort study. K.M. provided statistical support. L.C.B., C.P.B., and J.M.H. contributed to the study design. NPB conceived of the study concept, designed the study, and supervised the study. All authors read, critically reviewed, and approved the final version of the manuscript for publication. P.P. and N.P.B. are the guarantors of this work and, as such, had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Footnotes
This article contains supplementary material online at https://doi.org/10.2337/figshare.21445401.
References
- 1. Zhou B, Lu Y, Hajifathalian K, et al.; NCD Risk Factor Collaboration (NCD-RisC) . Worldwide trends in diabetes since 1980: a pooled analysis of 751 population-based studies with 4.4 million participants. Lancet 2016;387:1513–1530 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Ogurtsova K, da Rocha Fernandes JD, Huang Y, et al. IDF Diabetes Atlas: global estimates for the prevalence of diabetes for 2015 and 2040. Diabetes Res Clin Pract 2017;128:40–50 [DOI] [PubMed] [Google Scholar]
- 3. International Diabetes Federation . IDF Diabetes Atlas, 10th edition, 2021. Accessed 25 March 2022. Available from https://diabetesatlas.org
- 4. Moodie R, Stuckler D, Monteiro C, et al.; Lancet NCD Action Group . Profits and pandemics: prevention of harmful effects of tobacco, alcohol, and ultra-processed food and drink industries. Lancet 2013;381:670–679 [DOI] [PubMed] [Google Scholar]
- 5. Produce for Better Health Foundation . State of the Plate: America’s Fruit & Vegetable Consumption Trends: 2020 Executive Summary. Accessed 25 March 2022. Available from https://fruitsandveggies.org/stateoftheplate2020
- 6. Sachdeva S, Sachdev TR, Sachdeva R. Increasing fruit and vegetable consumption: challenges and opportunities. Indian J Community Med 2013;38:192–197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Jardine MA, Kahleova H, Levin SM, Ali Z, Trapp CB, Barnard ND. Perspective: Plant-based eating pattern for type 2 diabetes prevention and treatment: efficacy, mechanisms, and practical considerations. Adv Nutr 2021;12:2045–2055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Zheng J-S, Sharp SJ, Imamura F, et al. Association of plasma biomarkers of fruit and vegetable intake with incident type 2 diabetes: EPIC-InterAct case-cohort study in eight European countries. BMJ 2020;370:m2194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Halvorsen RE, Elvestad M, Molin M, Aune D. Fruit and vegetable consumption and the risk of type 2 diabetes: a systematic review and dose-response meta-analysis of prospective studies. BMJ Nutr Prev Health 2021;4:519–531 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Neuenschwander M, Ballon A, Weber KS, et al. Role of diet in type 2 diabetes incidence: umbrella review of meta-analyses of prospective observational studies. BMJ 2019;366:l2368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Rayner J, D’Arcy E, Ross LJ, Hodge A, Schoenaker DAJM. Carbohydrate restriction in midlife is associated with higher risk of type 2 diabetes among Australian women: a cohort study. Nutr Metab Cardiovasc Dis 2020;30:400–409 [DOI] [PubMed] [Google Scholar]
- 12. Ahmed A, Lager A, Fredlund P, Elinder LS. Consumption of fruit and vegetables and the risk of type 2 diabetes: a 4-year longitudinal study among Swedish adults. J Nutr Sci 2020;9:e14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Hodge AM, English DR, O’Dea K, Giles GG. Glycemic index and dietary fiber and the risk of type 2 diabetes. Diabetes Care 2004;27:2701–2706 [DOI] [PubMed] [Google Scholar]
- 14. Mursu J, Virtanen JK, Tuomainen TP, Nurmi T, Voutilainen S. Intake of fruit, berries, and vegetables and risk of type 2 diabetes in Finnish men: the Kuopio Ischaemic Heart Disease Risk Factor Study. Am J Clin Nutr 2014;99:328–333 [DOI] [PubMed] [Google Scholar]
- 15. Bazzano LA, Li TY, Joshipura KJ, Hu FB. Intake of fruit, vegetables, and fruit juices and risk of diabetes in women. Diabetes Care 2008;31:1311–1317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Liu S, Serdula M, Janket S-J, et al. A prospective study of fruit and vegetable intake and the risk of type 2 diabetes in women. Diabetes Care 2004;27:2993–2996 [DOI] [PubMed] [Google Scholar]
- 17. Tjønneland A, Olsen A, Boll K, et al. Study design, exposure variables, and socioeconomic determinants of participation in Diet, Cancer and Health: a population-based prospective cohort study of 57,053 men and women in Denmark. Scand J Public Health 2007;35:432–441 [DOI] [PubMed] [Google Scholar]
- 18. Carstensen B, Kristensen JK, Marcussen MM, Borch-Johnsen K. The National Diabetes Register. Scand J Public Health 2011;39(Suppl.):58–61 [DOI] [PubMed] [Google Scholar]
- 19. Lauritzen J. Foodcalc 1.3. computer program 1998. Accessed 31 January 2022. Available from https://www.ibt.ku.dk/jesper/foodcalc/default.html
- 20. National Health and Medical Research Council . Australian Dietary Guidelines. Accessed 29 November 2021. Available from https://www.nhmrc.gov.au/adg
- 21. U.S. Department of Agriculture, U.S. Department of Health and Human Services . Dietary Guidelines for Americans, 2020–2025, 9th edition. Accessed 29 November 2021. Available from https://www.dietaryguidelines.gov
- 22. Expert Committee on the Diagnosis and Classification of Diabetes Mellitus . Report of the expert committee on the diagnosis and classification of diabetes mellitus. Diabetes Care 2003;26(Suppl. 1):S5–S20 [DOI] [PubMed] [Google Scholar]
- 23. Xu G, Liu B, Sun Y, et al. Prevalence of diagnosed type 1 and type 2 diabetes among US adults in 2016 and 2017: population based study. BMJ 2018;362:k1497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Tomova GD, Arnold KF, Gilthorpe MS, Tennant PWG. Adjustment for energy intake in nutritional research: a causal inference perspective. Am J Clin Nutr 2022;115:189–198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Lange T, Rasmussen M, Thygesen LC. Assessing natural direct and indirect effects through multiple pathways. Am J Epidemiol 2014;179:513–518 [DOI] [PubMed] [Google Scholar]
- 26. Steen J, Loeys T, Moerkerke B, Vansteelandt S. Medflex: an R package for flexible mediation analysis using natural effect models. J Stat Softw 2017;76:1–4636568334 [Google Scholar]
- 27. Mamluk L, O’Doherty MG, Orfanos P, et al. Fruit and vegetable intake and risk of incident of type 2 diabetes: results from the consortium on health and ageing network of cohorts in Europe and the United States (CHANCES). Eur J Clin Nutr 2017;71:83–91 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Villegas R, Shu XO, Gao Y-T, et al. Vegetable but not fruit consumption reduces the risk of type 2 diabetes in Chinese women. J Nutr 2008;138:574–580 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Kalmpourtzidou A, Eilander A, Talsma EF. Global vegetable intake and supply compared to recommendations: a systematic review. Nutrients 2020;12:1558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Muraki I, Rimm EB, Willett WC, Manson JE, Hu FB, Sun Q. Potato consumption and risk of type 2 diabetes: results from three prospective cohort studies. Diabetes Care 2016;39:376–384 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Yiannakou I, Pickering RT, Yuan M, Singer MR, Moore LL. Potato consumption is not associated with cardiometabolic health outcomes in Framingham Offspring Study adults. J Nutr Sci 2022;11:e73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Beals KA. Potatoes, nutrition and health. Am J Potato Res 2019;96:102–110 [Google Scholar]
- 33. Hätönen KA, Virtamo J, Eriksson JG, Sinkko HK, Sundvall JE, Valsta LM. Protein and fat modify the glycaemic and insulinaemic responses to a mashed potato-based meal. Br J Nutr 2011;106:248–253 [DOI] [PubMed] [Google Scholar]
- 34. Zaheer K, Akhtar MH. Potato production, usage, and nutrition—a review. Crit Rev Food Sci Nutr 2016;56:711–721 [DOI] [PubMed] [Google Scholar]
- 35. Johnston EA, Petersen KS, Kris-Etherton PM. Daily intake of non-fried potato does not affect markers of glycaemia and is associated with better diet quality compared with refined grains: a randomised, crossover study in healthy adults. Br J Nutr 2020;123:1032–1042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Suresh S, Waly MI, Rahman MS, et al. Broccoli (Brassica oleracea) reduces oxidative damage to pancreatic tissue and combats hyperglycaemia in diabetic rats. Prev Nutr Food Sci 2017;22:277–284 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Veeramani C, Alsaif MA, Al-Numair KS. Lavatera critica controls systemic insulin resistance by ameliorating adipose tissue inflammation and oxidative stress using bioactive compounds identified by GC-MS. Biomed Pharmacother 2018;106:183–191 [DOI] [PubMed] [Google Scholar]
- 38. Wang X, Bao W, Liu J, et al. Inflammatory markers and risk of type 2 diabetes: a systematic review and meta-analysis. Diabetes Care 2013;36:166–175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Menni C, Louca P, Berry SE, et al. High intake of vegetables is linked to lower white blood cell profile and the effect is mediated by the gut microbiome. BMC Med 2021;19:37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Mozaffarian D, Hao T, Rimm EB, Willett WC, Hu FB. Changes in diet and lifestyle and long-term weight gain in women and men. N Engl J Med 2011;364:2392–2404 [DOI] [PMC free article] [PubMed] [Google Scholar]