Abstract
Background and Aims
Chronic respiratory diseases (CRDs) substantially contribute to morbidity and mortality globally and in Nepal. However, there is a paucity of evidence on the trend and the burden of CRDs in Nepal. This study reports the trend of the burden and contribution of major risk factors to CRDs in Nepal from 1990 to 2019.
Methods
This study is an observational study using publicly available data from Global Burden of Disease 2019 estimations for Nepal. The age‐standardized and age‐specific prevalence, incidence, mortality, disability‐adjusted life years (DALYs), and risk factors for CRDs in Nepal were extracted to measure the burden and its trend. The data are presented as percentages or as rates per 100,000 population.
Results
The age‐standardized incidence rate of CRDs in Nepal in 2019 was 913.6 per 100,000 (95% uncertainty interval [UI]: 828.7–1000.1), which was an increase of 7.7% from 848.6 per 100,000 (95% UI: 780.2–918.2) in 1990. However, the age‐standardized prevalence rate [4453/100,000 (4234.2–4671.8) in 1990; 4457.1/100,000 (4255.2–4666.8) in 2019] was almost stagnant. Most CRDs attributed to deaths and DALYs were due to chronic obstructive pulmonary disease.
Conclusions
Air pollution and smoking are the main risk factors for DALYs due to CRDs in Nepal. This surging burden of the incidence rate of CRDs in Nepal calls for more effective actions to curb the risk factors and diseases.
Keywords: chronic respiratory diseases, DALYs, incidence, mortality, Nepal, prevalence
1. INTRODUCTION
Chronic respiratory diseases (CRDs) are defined as the abnormalities of airways and lungs, primarily including chronic obstructive pulmonary disease (COPD), occupational lung diseases, and asthma. 1 They are significant contributors to the surging burden of noncommunicable diseases (NCDs) globally. 1 In 2017, 544.9 million people were estimated to be living with CRDs worldwide, a 39.8% increase compared to 1990. 2 The global prevalence of CRDs in 2017 was 7.1% (95% uncertainty interval [UI]: 6.6–7.7), and CRDs were the third most cause of mortality. 2 Globally, CRDs are attributed to above three million premature deaths annually.
Exposure to biomass fuel smoke, ambient air pollution, and smoking are the key risk factors of CRDs. 3 The burden of CRDs is disproportionately high in low‐ and middle‐income countries (LMICs), considering the ampler presence of risk factors, lack of knowledge and awareness of the disease, and its risk factors at the population level, which is further challenged by the lack of health system capacity to prevent and manage the rising burden of CRDs. 4 Most CRD‐related deaths occur in Asian countries, with approximately 75% of all cases. 2 Nine out of 10 COPD‐accounted deaths occur in LMICs like Nepal. 1
Nepal is going through an epidemiological transition with the increasing burden of NCDs like cardiovascular conditions, CRDs, diabetes, and cancers. 5 As of 2019, NCDs shares above 60% of disability‐adjusted life years (DALYs) in Nepal. 6 Despite this rising burden, the health system is still unprepared to prevent and manage NCDs. Nepal's multisectoral action plan for the prevention and control of NCDs (2021–2025) aims 25% reduction of premature mortality from NCDs, including CRDs by 2025. 7 In this context, evidence‐based and comprehensive information is advantageous for policymakers to make the best healthcare decisions for respiratory diseases.
A recent publication reviewed the prevalence of CRDs in Nepal, concluding limited data on the burden of CRDs in Nepal. 8 Similarly, recent studies report the prevalence and factors associated with COPD in Nepal. 9 , 10 However, a scientific and systematic understanding of the burden of CRDs accounting for the prevalence, incidence, mortality, DALYs, and their trend is yet to be available for Nepal. This study reports the trend of CRDs from 1990 to 2019 in terms of prevalence, incidence, mortality, DALYs, years of life lost (YLLs), and years lived with disabilities (YLDs). We also presented the contribution of major risk factors to CRDs DALYs in 2019.
2. METHODS
2.1. Study design
This is an observational study on the disease burden based on secondary data obtained from the Global Burden of Disease (GBD) study 2019 estimations for Nepal. 11
2.2. Data
This article uses publicly accessible data from the repository of the Institute of Health Metrics and Evaluation (IHME) based at the University of Washington, USA. 11 GBD study uses all available data sources, including national surveys and other epidemiological studies, to estimate the burden, measure the risk factors, and to quantify the health loss. A total of 402 citations, including survey data, surveillance data, and published/unpublished articles, were used as input sources for estimating the disease burden for Nepal comprising CRDs. 12 The GBD study protocol 13 and the visualization tool 14 are available online. Similarly, the methods applied in GBD 2019 are widely reported earlier. 15 , 16 The GBD study included COPD, asthma, pneumococcus, interstitial lung diseases (ILDs), and other chronic respiratory diseases as CRDs. 2 , 17 We downloaded the CRD prevalence, incidence, mortality rates, DALYs, YLLs, and YLDs data from Nepal by age and gender from 1990 to 2019 in excel format.
2.3. Statistical analysis
Bayesian metaregression tool DisMod‐MR 2.1 was applied to estimate the prevalence, incidence, and other epidemiological data of CRDs. 13 Various national surveys and scientific articles were included in the analysis. Prevalence was multiplied by disability weight to calculate YLDs. The GBD study normative standard life expectancy at each age was applied to estimate YLLs due to premature deaths. Similarly, YLLs and YLDs were summed to calculate DALYs. Mortality due to CRDs was estimated by using cause‐of‐death ensemble modeling. Risk exposure distribution was calculated by applying different research methods, such as randomized controlled trials, cohorts, or case–control studies. Descriptive analysis was done using tables and graphs for comparison of patterns and trends in deaths, incidence, prevalence, DALYs, YLDs, and YLLs due to CRDs in Nepal.
The study is exempted from ethical review and approval as it mobilizes publicly available deidentified data from the GBD study exempt.
3. RESULTS
3.1. Incidence and prevalence
The age‐standardized incidence rate (ASIR) of CRDs in Nepal in 2019 was 913.6 per 100,000 populations (95% UI: 828.7–1000.1), which was an increase of 7.7% from 848.6 per 100,000 populations (95% UI: 780.2–918.2) in 1990 (Table 1). The ASIR for CRDs increased from the year 1990 to 2000; however, it decreased from 2000 to 2010. A subsequent increase was seen again from 2010 to 2019. A similar pattern was seen in the ASIR of females, whereas no significant change in the trend was seen in males from 1990 to 2000. The ASIR of CRDs in females was greater than in males throughout all the years. However, the mortality was similar in both groups, as shown in Figure 1.
Table 1.
Change in incidence and prevalence of chronic respiratory diseases in Nepal, 1990–2019.
| Diseases | Age‐standardized incidence per 100,000 (95% UI) | Age‐standardized prevalence per 100,000 (95% UI) | ||||
|---|---|---|---|---|---|---|
| 1990 | 2019 | % Change | 1990 | 2019 | % Change | |
| All chronic respiratory diseases | 848.6 (780.2–918.2) | 913.6 (828.7–1000.1) | 7.7 | 4453 (4234.2–4671.8) | 4457.1 (4255.2–4666.8) | 0.1 |
| COPD | 293.8 (277.6–307.5) | 298.1 (286–310) | 1.4 | 3622.3 (3250.4–3622.3) | 3651.0 (3476.4–3824.2) | 0.8 |
| Asthma | 204.9 (179.6–233.8) | 175.5 (150.2–204.5) | −14.3 | 1254.0 (1117.3–1405.5) | 1072.5 (932.4–1072.5) | −14.4 |
| Interstitial lung disease | 349.5 (291.2–411.5) | 439.6 (358.4–518.8) | 25.7 | 47.7 (42.4–53) | 63.6 (57.0–70.5) | 33.3 |
| Pneumoconiosis | 0.5 (0.4–0.6) | 0.5 (0.4–0.6) | _ | 3.4 (2.8–4.2) | 4.2 (3.5–4.2) | 23.5 |
Abbreviations: COPD, chronic obstructive pulmonary disease; UI, uncertainty interval.
Figure 1.
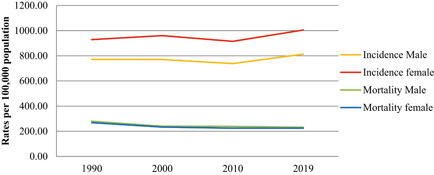
Trend in chronic respiratory disease mortality and incidence rates by gender (age‐standardized 1990–2019).
The age‐standardized prevalence rate (ASPR) of CRDs has remained almost the same (4453 per 100,000 populations in 1990 vs. 4457.1 per 100,000 populations in 2019) over the 29 years (Table 1). The ASPR was 24% higher among females (4904.9; 95% UI: 4658.7–5136.4) compared to males (3955.9; 95% UI: 3747.9–4170.1) in 2019. COPD remained the most prevalent disease‐specific CRD, with a prevalence rate of 3651 per 100,000 populations (95% UI: 3476.4–3824.2) in 2019. Prevalence was greater in females compared to males for each CRD, except for pneumoconiosis. The ASPR of ILD and pneumoconiosis increased by 33.3% and 23.5%, respectively, between 1990 and 2019. At the same time, the ASPR of asthma declined by 14.4%, and the prevalence rate of COPD remained almost stagnant.
The age‐specific prevalence of CRDs increased gradually, showing a sharp rise from 40 years onwards. The overall prevalence was higher among females than males (Figure 2A). COPD followed a similar trend (Figure 2B). However, the age‐specific prevalence of asthma slightly increased between the 5 and 9 years age group and later sharply increased from 25 years of age (Figure 2C).
Figure 2.
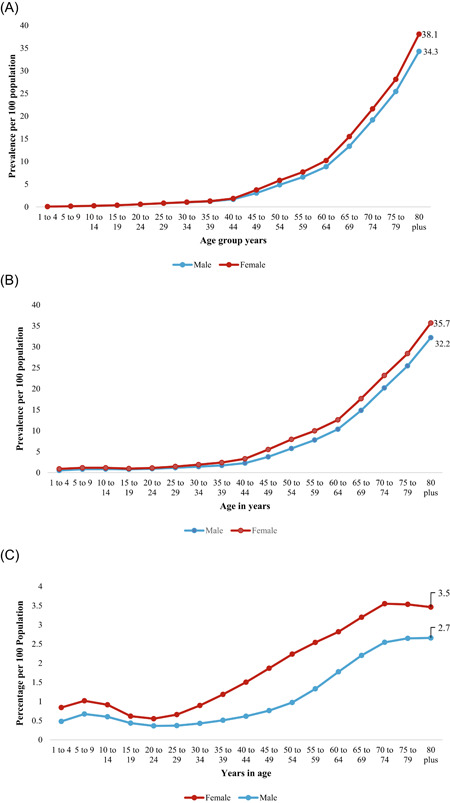
(A) Age‐ and sex‐specific prevalence of chronic respiratory disease in Nepal, 2019. (B) Age‐ and sex‐specific prevalence of chronic obstructive pulmonary disease in Nepal, 2019. (C) Age‐ and sex‐specific prevalence of asthma disease in Nepal, 2019.
3.2. Mortality
Between 1990 and 2019, the death rates due to CRDs decreased for both males and females, and the decline was slightly more among females. In 2019, the age‐standardized death rate attributed to CRDs was 224.4 per 100,000 people (95% UI: 154.1–274.2) for females, whereas it was 238.9 per 100,000 people (95% UI: 171.6–282.5) for males (Table 2).
Table 2.
Rate of total deaths due to chronic respiratory diseases by gender in Nepal (age‐standardized, 1990–2019).
| Disease | Years | Female (95% UI)/100,000 | Male (95% UI)/100,000 | Both (95% UI)/100,000 |
|---|---|---|---|---|
| All CRDs | 1990 | 268.5 (189.3–344.8) | 280.1 (198.4–337.6) | 273 (213.1–326.1) |
| 2000 | 233.7 (171.1–271) | 240.2 (180.1–271.1) | 236.1 (185.4–266.4) | |
| 2010 | 224.7 (163.1–256.9) | 232 (175.6–264.3) | 227.7 (181.5–258.8) | |
| 2019 | 224.4 (154.1–274.2) | 238.9 (171.6–282.5) | 231.2 (175.7–270.3) | |
| COPD | 1990 | 184.1 (109.6–251) | 217.8 (145.2–271.1) | 199.7 (136.2–244.9) |
| 2000 | 166.6 (116.3–208.3) | 193 (138.4–226.5) | 178.9 (133.9–206.3) | |
| 2010 | 164.6 (116.1–203) | 190.1 (146.4–222) | 176.5 (139.4–202.6) | |
| 2019 | 168.4 (109.1–212.9) | 198.5 (143.9–238.3) | 182.4 (135.7–214.6) | |
| Asthma | 1990 | 75.7 (35.7–130.5) | 50.9 (24–106) | 63.2 (35.8–101.1) |
| 2000 | 57.5 (29–100.7) | 36.5 (19.4–72.7) | 47.1 (28.1–79.6) | |
| 2010 | 49.1 (24.9–83.9) | 30.3 (17.5–57) | 39.9 (23.7–68.7) | |
| 2019 | 43.8 (24.5–66) | 27.8 (15.9–45.2) | 36.3 (22.4–52.1) | |
| Interstitial | 1990 | 6.9 (3.3–11.3) | 7.9 (2.5–14.4) | 7.4 (4.1–11.4) |
| 2000 | 7.9 (4.1–11.6) | 7.7 (2.7–12.9) | 7.8 (4.6–11.3) | |
| 2010 | 9.3 (4.9–13.5) | 8.6 (3.5–14.5) | 9 (5.4–12.7) | |
| 2019 | 10.4 (5.8–15.9) | 9.6 (4.3–16.5) | 10 (5.8–14.4) | |
| Pneumoconiosis | 1990 | 0.1 (0–0.2) | 1.3 (0.2–2.3) | 0.7 (0.1–1.2) |
| 2000 | 0.1 (0–0.1) | 1 (0.1–1.7) | 0.5 (0.1–0.9) | |
| 2010 | 0.1 (0–0.1) | 0.9 (0.1–1.5) | 0.5 (0.1–0.8) | |
| 2019 | 0.1 (0–0.2) | 0.9 (0.2–1.5) | 0.5 (0.1–0.8) | |
| Other CRDs | 1990 | 1.6 (0.7–3.1) | 2 (0.5–3.5) | 1.8 (0.8–3.2) |
| 2000 | 1.5 (0.8–2.3) | 1.8 (0.5–2.9) | 1.6 (0.9–2.4) | |
| 2010 | 1.5 (0.8–2.3) | 1.8 (0.6–2.9) | 1.7 (0.9–2.4) | |
| 2019 | 1.5 (0.8–2.4) | 1.9 (0.7–3.1) | 1.7 (0.9–2.5) |
Abbreviations: COPD, chronic obstructive pulmonary disease; CRD, chronic respiratory disease; UI, uncertainty interval.
Death rate (4765.6; 95% UI: 3594.832–5695.7) and percentage of total deaths (32.1; 95% UI: 25.1–37.1) from CRDs was highest among 80‐plus years as compared to other age groups (Table 3).
Table 3.
Deaths from chronic respiratory diseases in Nepal by age groups and gender in 2019.
| Age groups (years) | Death per 100,000 (95% UI) | Percentage of total deaths (95% UI) | ||||
|---|---|---|---|---|---|---|
| Female | Male | Both | Female | Male | Both | |
| 1–4 | 0.6 (0.2–1.4) | 0.1 (0.0–0.5) | 0.3 (0.1–0.7) | 0.6 (0.3–1.4) | 0.1 (0.0–0.5) | 0.3 (0.1–0.7) |
| 5–9 | 0.1 (0.0–0.3) | 0.04 (0.0–0.2) | 0.1 (0.0–0.2) | 0.2 (0.0–0.5) | 0.1 (0.0–0.4) | 0.1 (0.0–0.5) |
| 10–14 | 0.1 (0.0–0.5) | 0.2 (0.1–0.3) | 0.1 (0.1–0.4) | 0.4 (0.1–1.6) | 0.4 (0.2–0.6) | 0.4 (0.2–1.0) |
| 15–19 | 0.8 (0.4–1.7) | 0.4 (0.2–1.0) | 0.6 (0.3–1.4) | 1.3 (0.7–3.1) | 0.4 (0.2–1.0) | 0.7 (0.5–1.7) |
| 20–24 | 1.1 (0.6–2.4) | 1.5 (0.9–2.4) | 1.3 (0.8–2.2) | 1.5 (0.9–3.4) | 1.0 (0.6–1.5) | 1.2 (0.8–2.0) |
| 25–29 | 1.7 (0.8–3.7) | 2.2 (1.2–3.5) | 1.9 (1.1–3.2) | 1.9 (1.0–4.1) | 1.5 (0.9–2.3) | 1.7 (1.1–2.8) |
| 30–34 | 3.6 (1.7–7.2) | 1.7 (0.6–3.2) | 2.8 (1.4–5.2) | 3.0 (1.6–6.2) | 1.0 (0.4–1.8) | 2.0 (1.1–3.8) |
| 35–39 | 9.5 (5.3–14.7) | 1.8 (0.5–5.9) | 6.2 (3.4–10.2) | 5.5 (3.4–8.2) | 0.8 (0.2–2.6) | 3.2 (1.9–5.0) |
| 40–44 | 23.0 (13.8–34.0) | 9.8 (5.2–15.2) | 17.1 (10.7–24.5) | 8.8 (5.5–11.8) | 2.9 (1.6–4.3) | 5.8 (4.0–7.5) |
| 45–49 | 57.0 (32.5–83.6) | 39.8 (23.3–58.8) | 49.0 (32.1–67.7) | 14.1 (8.3–18.8) | 7.5 (4.6–10.2) | 10.6 (7.5–13.2) |
| 50–54 | 120.1 (65.3–175.6) | 101.4 (62.1–147.9) | 111.1 (73.0–152.6) | 19.4 (10.4–26.0) | 11.6 (7.5–15.1) | 15.0 (10.7–18.4) |
| 55–59 | 191.9 (115.4–278.1) | 212.5 (128.4–303.2) | 201.9 (137.5–276.0) | 20.7 (12.5–27.5) | 15.1 (9.9–19.9) | 17.4 (12.7–21.5) |
| 60–64 | 390.8 (240.9–548.7) | 459.8 (289.6–628.9) | 423.9 (295.7–552.0) | 26.7 (17.2–34.3) | 20.2 (14.0–25.7) | 22.8 (17.3–27.2) |
| 65–69 | 728.3 (459.5–979.5) | 809.1 (530.4–1079.3) | 766.3 (545.1–971.4) | 31.2 (20.3–39.7) | 23.0 (16.2–28.9) | 26.5 (20.1–31.2) |
| 70–74 | 1288.3 (859.0–1674.1) | 1422.2 (977.2–1831.9) | 1353.5 (1005.7–1673.9) | 32.7 (22.4–40.7) | 26.4 (19.6–32.5) | 29.2 (22.8–34.3) |
| 75–79 | 2144.6 (1379.8–2808.1) | 2310.9 (1577.1–2950.7) | 2225.5 (1606.7–2728.3) | 32.8 (21.6–41.8) | 28.4 (20.2–34.9) | 30.4 (23.0–36.2) |
| 80 plus | 4718.1 (3205.3–5908.8) | 4820.6 (3420.5–5804.8) | 4765.6 (3594.8–5695.8) | 33.5 (22.9–41.2) | 30.7 (22.8–35.9) | 32.1 (25.1–37.1) |
Abbreviation: UI, uncertainty interval.
3.3. DALYs
In 2019, the age‐standardized DALYs for CRDs was 4339.3 per 100,000 populations (95% UI: 3410.6–5078.8), representing a decrease of 22.5% since 1990 (5600.3, 95% UI: 4407–6661.4). YLLs contributed almost 88% of DALYs due to CRDs in 2019, which is slightly less than its 91% contribution in 1990 (Table 4).
Table 4.
Age‐standardized DALYs rates per 100,000 population.
| Age standardized DALYs rates per 100,000 population (95% UI) | |||
|---|---|---|---|
| 1990 | 2019 | % Change | |
| All chronic respiratory diseases | 5600.3 (4407–6661.4) | 4339.3 (3410.6–5078.8) | −22.5 |
| Asthma | 1429.5 (877.4–2060.3) | 740.9 (482.3–1040.9) | −48.2 |
| COPD | 3931 (2817.2–4759.3) | 3318.4 (2546.5–3889.6) | −15.6 |
| Interstitial lung diseases | 153.5 (86 –238) | 195.1 (119.6–274.6) | 27.2 |
| Pneumoconiosis | 16.1 (4 –27.4) | 10.3 (3.8–16.9) | −36 |
| Other chronic respiratory diseases | 70 (38.9–116.7) | 74.4 (53.5–96.9) | 6.3 |
Abbreviations: COPD, chronic obstructive pulmonary disease; DALY, disability‐adjusted life years; UI, uncertainty interval.
Total DALYs, YLLs, and YLDs were higher among males than females throughout the 29 years (1990–2019) (Figure 3).
Figure 3.

Chronic respiratory diseases related disability‐adjusted life years (DALYs), years of life lost (YLLs), and years lived with disabilities (YLDs) by age and sex in 2019.
DALYs attributed to CRDs, COPD, and asthma increased gradually in the 30‐plus age group (Figure 4).
Figure 4.

Age‐wise chronic respiratory diseases (CRDs), chronic obstructive pulmonary disease (COPD), and asthma disability‐adjusted life years (DALYs) by age in Nepal, 2019.
3.4. Risk factors attributable to CRDs
The leading risk factor attributable to DALYs lost due to CRDs are air pollution, smoking, and household air pollution. Occupational risk factors and smoking were the major contributors to DALYs lost to asthma (Figure 5).
Figure 5.
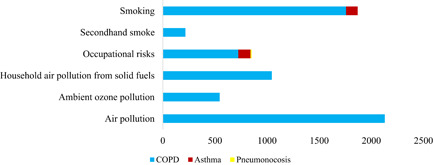
Chronic respiratory disease (CRD) risk factors contributing to disability‐adjusted life years for specific CRDs (age‐standardized, 2019). COPD, chronic obstructive pulmonary disease.
When comparing the incidence, prevalence, death rates, and DALYs data of CRDs from Nepal to the global and South Asian regions, the incidence rates in Nepal were lower than the global and South Asian figures. In contrast, the rate of mortality was significantly greater than the global, and South Asian countries' rates except that of Bangladesh and Pakistan. The prevalence of CRDs in Nepal was lesser than global and South Asian countries' estimates; however, CRDs that caused DALYs were higher than the global and South Asian countries' data. (Table 5).
Table 5.
Comparing chronic respiratory disease‐related incidence, prevalence, death, and DALYs between countries and regions in 2019.
| Age‐standardized rates per 100,000 populations | ||||
|---|---|---|---|---|
| Incidence | Deaths | Prevalence | DALYs | |
| Nepal | 913 (828.7–1000.1) | 231.2 (175.7–270.3) | 4457.1 (4179.0–4658.1) | 4339.2 (3410.6–5078.7) |
| Global | 1001.5 (882.9–1144.4) | 51.2 (45.9–55.5) | 5789.1 (5290.6–6418.1) | 1293.7 (1182.9–1403.5) |
| South Asia | 1090.3 (966.8–1219.1) | 118.7 (97.5–135.8) | 5366.2 (4957.7–5815.7) | 2559.2 (2206.9–2879.0) |
| Afghanistan | 1019 (901.4–1165.9) | 67.8 (51.9–81.3) | 6187.2 (5648.3–6825.7) | 1754.0 (1422.5–2077.0) |
| Bangladesh | 884.1 (789.8–973.6) | 62.0 (47.2–106.8) | 4202.5 (3974.7–4431.0) | 1499.6 (1228.5–2192.8) |
| Bhutan | 919.6 (827.7–1009.1) | 123.1 (94.1–164.6) | 4417.2 (4179.0–4658.1) | 2436.4 (1953.3–3190.0) |
| India | 1156.3 (1021.7–1298.1) | 125.1 (95.2–145.2) | 5654.8 (5180.0–6155.1) | 2678.8 (2208.0–3047.9) |
| Maldives | 1015.8 (884.3–1167.5) | 51.6 (42.4–61.4) | 5428.1 (4905.9–6056.3) | 1251.6 (1093.2–1428.3) |
| Pakistan | 716.9 (648.0–788.9) | 100.3 (83.0–122.7) | 4115.2 (3814.0–4461.8) | 2228.1 (1901.4–2641.9) |
Abbreviation: DALYs, disability‐adjusted life years.
4. DISCUSSION
Nepal experienced a 7.7% increase in incidence and stagnant prevalence of CRDs between 1990 and 2019. The incidence and prevalence of CRDs in Nepal were found to be lower than the global and South Asian rates, as shown in Table 5. However, CRD‐ attributed DALYs were more than the global and South Asian countries' estimates. 14 Similarly, the death rates were significantly higher in Nepal. The percentage of total deaths increased by more than 139% between 1990 (8.8%) to 2019 (21.1%), making CRDs the second leading cause of death in Nepal below cardiovascular diseases. Despite less prevalence and incidence, there was a high number of deaths. This might be due to higher exposure to risk factors, poor treatment, unavailability of medicines and treatment, and lack of early diagnosis and treatment. Nepal still does not have a cause‐of‐death surveillance system or other established and validated verbal autopsy forms at the national level to record deaths due to CRDs. Thus, estimations were calculated using statistical models and might be over or underestimated.
LMICs like Nepal are experiencing an epidemiological transition. 18 The already compromised health systems of these less‐developed and resource‐limited countries are facing a triple burden of communicable diseases, NCDs, and road traffic accidents. 19 The significant contributors of CRDs such as COPD, asthma, and ILDs are smoking, air pollution, and occupational risks. During the past 15 years, the pollution load in the air increased by nearly 35%, mostly in urban cities like Kathmandu. 20 During this period, the country has experienced rapid urbanization, increased closed spaces, and increased vehicular emissions, contributing to increased outdoor pollution. 18 , 21 The air quality in Nepal is rapidly degrading, and fine particulate matter 2.5 (PM2.5) exposure was so high that Nepal ranked 178 among 180 countries in Environmental Performance Index 2022. 22 Likewise, Nepal Demographic and Health Survey (NDHS) in 2016 showed that 66% of Nepalese households usage solid biomass fuel for cooking as these are cheaper and widely available fuel source. 23 Also, the PM10 level under these conditions is three times higher than in clean fuels. 24 Alongside this, over half of the males and 8.4% of females consume tobacco, of which nearly half of those smoke cigarettes. 25 Similar figures were reported by Noncommunicable Disease Risk Factors: World Health Organization STEPwise approach to Surveillance (STEPS) survey in Nepal 2019, where the prevalence of daily tobacco smoking among males and females was 20.8% and 6.2%, respectively. 26 Although smoking in public places is banned by law in Nepal, it is still poorly implemented. 27 These ailments have contributed to the burden of CRDs in Nepal, and these data are reinforced by other studies. 28
In our analysis, both incidence and prevalence rates of CRDs were more in females than in males. Women are particularly affected by household smoke and indoor air pollution as they are more involved in cooking. 29 , 30 , 31 This can be supported by the fact that, in 2019, indoor air pollution from biomass fuel use, smoking, and outdoor air pollution was the major risk factors for CRDs. However, some recent publications have reported a more prevalence of COPD among males than their counterparts in Nepal. 9 , 10 , 32
Along with the epidemiological transition, Nepal is concurrently experiencing a demographic transition. Life expectancy has improved from 54.4 years in 1990 to 70.8 years in 2019. 33 Only 5.8% of the total population was of age 60 years and above in 1991, increasing to 8.1% in 2011. The growth rate of the elderly population in 2011 was 3.8%. 34 Evidence shows that with increasing age, the risk of COPD and related DALYs and deaths is also expected to increase. 35 However, GBD data show that there has only been a slight increase in incidence and almost uniform prevalence and death rates.
Data show an increased prevalence of CRDs, COPD, and asthma with increasing age for both males and females. Likewise, mortality rates also increased with increasing age. There was a two‐fold rise in deaths per 100,000 for every 5‐year increase in age, particularly from age 40. This can be attributable to greater exposure to risk factors such as smoking, air pollution, and physiological decline in lung function with aging. 9 The NDHS 2016 report also shows that smoking and tobacco use and smoking frequency increase with increasing age and is highest among the older age population for both males and females. 36
In the case of asthma, other environmental factors like pesticide use, cold weather, and air pollution are considered risk factors. 37 A slight increase in the prevalence of asthma in children in their first 5 years was observed. Studies show that conditions like passive smoking, high indoor air pollution, and biomass fuel used in cooking are major risk factors for the occurrence of bronchial asthma in children. 38 Children are highly exposed to indoor air pollution at an early age leading to degraded lung function and eventually causing disease of the lungs. 39 Similarly, studies show that lung infection at the early stages of life contributes to the development of COPD in later stages. 9 , 40 This aligns with our findings of a higher prevalence of chronic respiratory illness in older adults.
The data demonstrate an increase in age‐standardized incidence and prevalence of COPD and ILD. However, the same for asthma has decreased between 1990 and 2019. A recent systematic review reports that presumptive COPD patients might have been misclassified as having asthma or other diseases, thus affecting estimates. 8 However, recent advances in diagnostic methods and availability in LMICs like Nepal have allowed early COPD and ILD detection and distinction with asthma. 41 Thus, better diagnostic methods for other respiratory diseases and their availability might have contributed to the apparent decrease in asthma incidence and prevalence over other respiratory diseases.
Similarly, there may be a disproportionally distributed diagnostic ability between primary and secondary care institutions. Thus, diseases that may have a higher tendency to reach specialized care, where diagnostic ability and registration are possible (i.e., ILD), may seem to have grown disproportionally in incidence and prevalence as opposed to the more common diseases COPD and asthma, which more often are dealt with at the primary care level. There is also likely a high degree of underdiagnosis of CRDs, profoundly affecting patients with asthma.
The estimates are results from the modeling of the primary data. Few population‐based studies assessed the prevalence and incidence of CRDs in Nepal. 8 , 9 , 10 , 32 Where data are unavailable, the estimations were computed by out‐of‐sample predictive validity of the modeling efforts. 32 Even in available data, there might be required to be categorical identification of the desired and alternate methods of measurement for each outcome. So, these data have limitations during the prediction. Despite this limitation, this is the first of its kind attempt to present national‐level trends and distribution of the CRD burden in Nepal mobilizing the data obtained from the GBD study database, which uses standardized procedures to calculate metrics generating comparable data globally.
5. CONCLUSION
COPD and asthma are the most prevailing CRDs in Nepal. The CRDs in Nepal are mainly attributable to air pollution and smoking. Based on these findings, effective health education and awareness programs may be immediately required to combat air pollution, prevent smoking initiation, and promote smoking cessation. So, more strict measures in air pollution and smoking control and their effective implementation should be considered by concerned stakeholders.
AUTHOR CONTRIBUTIONS
Tara Ballav Adhikari: Conceptualization; data curation; formal analysis; funding acquisition; investigation; methodology; project administration; resources; software; validation; visualization; writing – original draft; writing – review and editing. Kiran Paudel: Conceptualization; data curation; formal analysis; investigation; methodology; project administration; resources; software; visualization; writing – original draft; writing – review and editing. Rajan Paudel: Investigation; methodology; writing – original draft; writing – review and editing. Sandesh Bhusal: Data curation; investigation; methodology; writing – original draft; writing – review and editing. Anupa Rijal: Methodology; visualization; writing – original draft; writing – review and editing. Marieann Högman: Supervision; visualization; writing – original draft; writing – review and editing. Dinesh Neupane: Supervision; writing – original draft; writing – review and editing. Torben Sigsgaard: Supervision; writing – original draft; writing – review and editing. Per Kallestrup: Supervision; visualization; writing – original draft; writing – review and editing. All authors have read and approved the final version of the manuscript.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflict of interest.
TRANSPARENCY STATEMENT
The corresponding author Kiran Paudel affirms that this manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
ACKNOWLEDGMENTS
The authors are grateful to the Institute of Health Metrics Evaluation (IHME), Global Burden of Disease Study 2019 team for making the data available.
Adhikari TB, Paudel K, Paudel R, et al. Burden and risk factors of chronic respiratory diseases in Nepal, 1990–2019: an analysis of the global burden of diseases study. Health Sci Rep. 2023;6:e1091. 10.1002/hsr2.1091
DATA AVAILABILITY STATEMENT
The study is based on publicly available data from the Global Burden of Disease Study 2019. The data can be downloaded from http://ghdx.healthdata.org/gbd-results-tool. K. P. or T. B. A. had full access to all of the data in this study and takes complete responsibility for the integrity of the data and the accuracy of the data analysis.
REFERENCES
- 1. World Health Organization (WHO) .Chronic respiratory diseases. WHO; 2021. https://www.who.int/health-topics/chronic-respiratory-diseases#tab=tab_1 [Google Scholar]
- 2. Soriano JB, Kendrick PJ, Paulson KR, et al. Prevalence and attributable health burden of chronic respiratory diseases, 1990–2017: a systematic analysis for the global burden of disease study 2017. Lancet Respir Med. 2020;8(6):585‐596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Bousquet J, Khaltaev N, eds. Global Surveillance, Prevention and Control of Chronic Respiratory Diseases: A Comprehensive Approach. World Health Organization; 2007. [Google Scholar]
- 4. Zeng LH HM, Syed SK, Saadullah M, et al. Revamping of chronic respiratory diseases in low‐ and middle‐income countries. Front Public Health. 2023;9:757089. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 5. Mishra SR, Sthresha N, Gyawali B, Shrestha A. Nepal's increasing burden of non communicable diseases and injuries, global burden of disease study 1990‐2017. JACC. 2020;75(11) (suppl_1):3478. [Google Scholar]
- 6. Nepal Health Research Council (NHRC), MoHP, IHME, and MEOR. Nepal Burden of Disease 2019: A Country Report Based on the 2019 Global Burden of Disease Study. NHRC; 2021. [Google Scholar]
- 7. Sharma SR, Page R, Matheson A, Lambrick D, Faulkner J, Mishra SR. Non‐communicable disease prevention in Nepal: systemic challenges and future directions. Glob Health Promot. 2019;26(3):94‐97. [DOI] [PubMed] [Google Scholar]
- 8. Ekezie W, Jenkins AR, Hall IP, et al. The burden of chronic respiratory diseases in adults in Nepal: a systematic review. Chron Respir Dis. 2021;18:147997312199457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Adhikari TB, et al. Prevalence of chronic obstructive pulmonary disease and its associated factors in Nepal: findings from a community‐based household survey. Int J Chronic Obstruct Pulm Dis. 2020;15:2319‐2331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Karki KB, Poudyal A, Shrestha N, et al. Factors associated with chronic obstructive pulmonary diseases in Nepal: evidence from a nationally representative population‐based study. Int J Chronic Obstruct Pulm Dis. 2021;16:1109‐1118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Institute for Health Metrics and Evaluation (IHME) and University of Washington . Global burden of disease study results. IHME and University of Washington. http://ghdx.healthdata.org/gbd-results-tool?params=gbd-api-2019-permalink/4d5dc09405e10db67d4c2d4620178dd1. [Google Scholar]
- 12. Institute for Health Metrics and Evaluation (IHME). Global Burden of Disease Study 2019 (GBD 2019) Data Input Sources Tool. IHME; 2019. http://ghdx.healthdata.org/gbd-2019/data-input-sources?components=9&locations=164 [Google Scholar]
- 13. Institute for Health Metrics and Evaluation (IHME) and University of Washington. Protocol for the Global Burden of Diseases, Injuries, and Risk Factors Study (GBD). IHME and University of Washington; 2020. http://www.healthdata.org/gbd/about/protocol [Google Scholar]
- 14. Institute for Health Metrics and Evaluation (IHME) and University of Washington. GBD Compare|Viz Hub. IHME and University of Washington; 2021. https://vizhub.healthdata.org/gbd-compare/ [Google Scholar]
- 15. Vos T, Lim SS, Abbafati C, et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the global burden of disease study 2019. Lancet. 2020;396(10258):1204‐1222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Yang X, Zhang T, Zhang Y, Chen H, Sang S. Global burden of COPD attributable to ambient PM2.5 in 204 countries and territories, 1990 to 2019: a systematic analysis for the global burden of disease study 2019. Sci Total Environ. 2021;796:148819. [DOI] [PubMed] [Google Scholar]
- 17. Salvi S, Kumar GA, Dhaliwal RS, et al. The burden of chronic respiratory diseases and their heterogeneity across the states of India: the global burden of disease study 1990–2016. Lancet Glob Health. 2018;6(12):e1363‐e1374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Mishra SR, Neupane D, Bhandari PM, Khanal V, Kallestrup P. Burgeoning burden of non‐communicable diseases in Nepal: a scoping review. Global Health. 2015;11:32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Haileamlak A. Editorial: the triple challenges of low and middle‐income countries. Ethiop J Health Sci. 2018;28(1):1‐2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Mahapatra PS, Puppala SP, Adhikary B, et al. Air quality trends of the Kathmandu Valley: a satellite, observation and modeling perspective. Atmos Environ. 2019;201:334‐347. [Google Scholar]
- 21. Neupane D and Kallestrup P. Non‐communicable diseases in Nepal: challenges and opportunities. J Nepal Health Res Counc. 2013;11(24):225‐228. [PubMed] [Google Scholar]
- 22. Wendling ZA, Emerson JW, de Sherbinin A, Esty DC. Environmental Performance Index 2020. Yale Center for Environmental Law & Policy; 2020. [Google Scholar]
- 23. Ghimire S, Mishra SR, Sharma A, Siweya A, Shrestha N, Adhikari B. Geographic and socio‐economic variation in markers of indoor air pollution in Nepal: evidence from nationally‐representative data. BMC Public Health. 2019;19(1):195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Shrestha IL, Shrestha SL. Indoor air pollution from biomass fuels and respiratory health of the exposed population in Nepalese households. Int J Occup Environ Health. 2005;11(2):150‐160. [DOI] [PubMed] [Google Scholar]
- 25. Khanal V, Adhikari M, Karki S. Social determinants of tobacco consumption among Nepalese men: findings from Nepal Demographic and Health Survey 2011. Harm Reduct J. 2013;10(1):40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Dhimal M, Bista B, Bhattarai S, et al. Report of Non Communidable Disease Risk Factors: STEPS Survey Nepal 2019. Nepal Health Research Council. [PubMed] [Google Scholar]
- 27. Khanal GN, Khatri RB. Burden, prevention and control of tobacco consumption in Nepal: a narrative review of existing evidence. Int Health. 2020;13(2):110‐121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Hu G, Zhou Y, Tian J, et al. Risk of COPD from exposure to biomass smoke. Chest. 2010;138(1):20‐31. [DOI] [PubMed] [Google Scholar]
- 29. Bates MN, Pokhrel AK, Chandyo RK, et al. Kitchen PM2.5 concentrations and child acute lower respiratory infection in Bhaktapur, Nepal: the importance of fuel type. Environ Res. 2018;161:546‐553. [DOI] [PubMed] [Google Scholar]
- 30. Ranabhat CL, Kim CB, Kim CS, Jha N, Deepak KC, Connel FA. Consequence of indoor air pollution in rural area of Nepal: a simplified measurement approach. Front Public Health. 2015;3:5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Pandey MR. Prevalence of chronic bronchitis in a rural community of the Hill Region of Nepal. Thorax. 1984;39(5):331‐336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Adhikari TB, Neupane D, Kallestrup P. Burden of COPD in Nepal. Int J Chronic Obstruct Pulm Dis. 2018;13:583‐589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. The World Bank Group. Life Expectancy at Birth, Total (Years)—Nepal. The World Bank Group; 2020. [Google Scholar]
- 34. Government of Nepal, N.P.C.S., Central Bureau of Statistics. Population Monograph of Nepal. Government of Nepal; 2014. [Google Scholar]
- 35. MacNee W. Is chronic obstructive pulmonary disease an accelerated aging disease? Ann Am Thorac Soc. 2016;13(suppl 5):S429‐S437. [DOI] [PubMed] [Google Scholar]
- 36. Shrestha N, Mehata S, Pradhan PMS, Joshi D, Mishra SR. A nationally representative study on socio‐demographic and geographic correlates, and trends in tobacco use in Nepal. Sci Rep. 2019;9(1):2682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Paudel U, Pant KP. Beyond smoking: environmental determinants of asthma prevalence in Western Nepal. J Health Pollut. 2020;10(25):20031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Pokharel PK, Kabra SK, Kapoor SK, Pandey RM. Risk factors associated with bronchial asthma in school going children of rural Haryana. Indian J Pediatr. 2001;68(2):103‐106. [DOI] [PubMed] [Google Scholar]
- 39. Devakumar D, Semple S, Osrin D, et al. Biomass fuel use and the exposure of children to particulate air pollution in southern Nepal. Environ Int. 2014;66(100):79‐87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Duan P, Wang Y, Lin R, et al. Impact of early life exposures on COPD in adulthood: a systematic review and meta‐analysis. Respirology. 2021;26:1131‐1151. [DOI] [PubMed] [Google Scholar]
- 41. Dixon LC, Ward DJ, Smith J, Holmes S, Mahadeva R. New and emerging technologies for the diagnosis and monitoring of chronic obstructive pulmonary disease: a horizon scanning review. Chron Respir Dis. 2016;13(4):321‐336. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The study is based on publicly available data from the Global Burden of Disease Study 2019. The data can be downloaded from http://ghdx.healthdata.org/gbd-results-tool. K. P. or T. B. A. had full access to all of the data in this study and takes complete responsibility for the integrity of the data and the accuracy of the data analysis.


