Abstract
The mammalian brain has an endogenous central circadian clock that regulates central and peripheral cellular activities. At the molecular level, this day-night cycle induces the expression of upstream and downstream transcription factors that influence the immune system and the severity of viral infections over time. In addition, there are also circadian effects on host tolerance pathways. This stimulates adaptation to normal changes in environmental conditions and requirements (including light and food). These rhythms influence the pharmacokinetics and efficacy of therapeutic drugs and vaccines. The importance of circadian systems in regulating viral infections and the host response to viruses is currently of great importance for clinical management. With the knowledge gained from the COVID-19 pandemic, it is important to address any outbreak of viral infection that could become endemic and to quickly focus research on any knowledge gaps. For example, responses to booster vaccination COVID-19 may have different time-dependent patterns during circadian cycles. There may be a link between reactivation of latently infected viruses and regulation of circadian rhythms. In addition, mammals may show different seasonal antiviral responses in winter and summer. This article discusses the importance of the host circadian clock during monkeypox infection and immune system interactions.
Keywords: Monkeypox, Circadian clocks, Rhythms, Chronobiology, Virus, Infection, Medication, Vaccination, Clinical treatment
Introduction
Monkeypox virus (mpox) is a viral zoonosis (transmitted to humans from animals—rope tree squirrels, Gambian pouched rats, dormice, non-human primates). Several neurological manifestations, such as headache, fatigue, malaise, myalgia, altered consciousness, agitation, nausea, anorexia, and vomiting, have been reported in patients with mpox (Shafaati and Zandi 2022). The dynamics are uncertain of the mpox outbreak in 2022, which spread from endemic countries in Africa to other regions of the world. However, although we know little about its host range, evidence suggests that changes in virus ecology itself are probably responsible for the unexpected emergence of mpox in the human population [including men who have sex with men (MSM)] (Patrono et al. 2020). In addition, “epigenetics” and “circadian clocks,” two relatively recent models, are novel for mpox, and additional is needed. Current evidence indicates that the circadian clock controls and regulates innate and adaptive immunity, virus replication and spread, and the severity of viral infections. A better understanding of the circadian clock’s effects on mpox infection can help improve clinical management of the 2022 outbreak and clarify the epidemiology and clinical manifestations of zoonotic pathogens. Circadian rhythms play an important role in regulating daily physiological activities, particularly the immune response, which has a large impact on human health. Mpox infection can occur via respiratory, mucosal, or skin contact. It has been demonstrated in both natural and experimental infections that these exposure pathways influence how diseases manifest and their severity, with dermal exposure producing more severe disease including exanthema (Reynolds et al. 2006; Saijo et al. 2009; Zhuang et al. 2017). Thus, clinical signs may be influenced by how virus infection occurs (Shafaati and Zandi 2022; Choudhary et al. 2022).
Circadian clock and viral infections
Because any disruption of the host’s circadian rhythm results in increased pathogen proliferation and spread, thus having a significant impact on the severity of acute infection. Humans are more susceptible to infection at certain times of the day due to the daily rhythmic circadian cycle (Man et al. 2016). Edgar et al. showed that the time of virus infection has a positive correlation with the severity of herpes and influenza A virus infections (Edgar et al. 2016). In viral infections, the infection-biological clock is a new concept that reveals the complex relationships between circadian timing, host immunity, and virus-host interactions (Table 1). Table 1 describes that many viruses interact with circadian clock components (BMAL-1, CLOCK, REV-ERB, etc.), upsetting its order through a variety of processes for their own replication requirements. Research is needed in this new field with regard to re-emerging and emerging viral infections with unknown spread dynamics. Moreover, this will assist treatment and lead to improvements in public health policies (Ko and Takahashi 2006).
Table 1.
Interference of viruses with the cellular circadian clock (Benegiamo et al. 2013; Mukherji et al. 2019; Chang et al. 2018; Matsuzawa et al. 2018; Shafaati et al. 2022)
| Circadian cycle agents | |||||
|---|---|---|---|---|---|
| BMAL-1 | CLOCK | REV-ERB | CRY1 and 2 | PER1 and 2 | Unknown |
| Modifying the host lipid pathway (dengue virus) | Overexpression of HBx protein (HBV) | Limits for infection rate (dengue virus) | Overexpression of HBx protein (HBV) | Overexpression of HBx protein (HBV) | Infection impairs of circadian rhythm (simian immunodeficiency virus) |
| Overexpression of HBx protein (HBV) | Remodeling of viral chromatin with interplay CLOCK: BMAL/IPC0 (herpesvirus) | Limits for infection rate (HCV) | mRNA levels are lower in HCC tissue (HBV) | mRNA levels are lower in HCC tissue (HBV) | Infection impairs of circadian rhythm (mpox) |
| Modifying the host lipid pathway (HCV) | Entry receptor expression is regulated by CLOCK (herpesvirus) | Control of infection by timing dependent host tolerance and immune activation (influenza virus) | Downregulation of in HCV patients | Downregulation of in HCV patients | |
| In HCV infection, miR-10 suppresses ROR to reduce Bmal1 expression | Control of infection by timing dependent host tolerance and immune activation (Influenza virus) | Tat reduces the circadian rhythm (HIV) | Control of infection by timing dependent host tolerance and immune activation (influenza virus) | ||
| Infection rates rise when BMAL1 levels are low (herpesvirus) | Tat reduces the circadian rhythm (HIV) | Decreases HIV promoter activity | Tat reduces the circadian rhythm (HIV) | ||
| Remodeling of viral chromatin with interplay CLOCK: BMAL/IPC0 (herpesvirus) | Limits for infection rate (Zika virus) | ||||
| Influenza virus-induced Bmal1 expression | |||||
| Control of infection by timing dependent host tolerance and immune activation (influenza virus) | |||||
| Reduces viral reproduction (RSV) | – | – | – | – | – |
| Reduces viral reproduction (parainfluenza virus type 3) | |||||
| Tat reduces the circadian rhythm (HIV) | |||||
| Modifying the host lipid pathway (Zika virus) | |||||
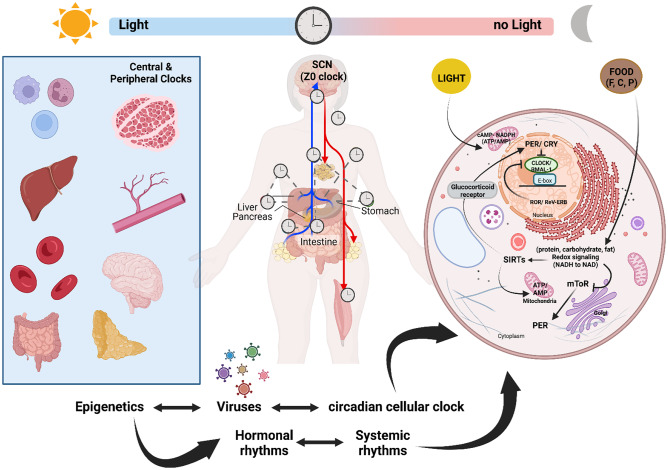
A host is obligatory for viral replication, propagation, and spread. Circadian rhythms can control a variety of viral diseases, including SARS-CoV-2, herpes, flavivirus, vesicular stomatitis virus, and influenza A infections (Soltani et al. 2021). Disruption of the circadian clock promotes the virus’s proliferation and spread, which is further explained in Fig. 1. Numerous immunological markers change during the day to predict environmental changes and lower the risk of infection. For various innate immune system functions, the cellular clock—where CLOCK, BMAL1, and REV-ERB regulate crucial processes including developing pattern recognition receptors (PRRs) involved in nucleic acid sensing, during viral infections. Understanding these processes is essential in defeating pathological virus infections (Silver et al. 2018).
Fig. 1.
Circadian oscillations of physiological infection. Most of brain central cells (glial cells and the neurons) and all the body’s peripheral tissues include molecular clocks. The brain’s pacemaker neurons in the SCN (supra-optic chiasmatic nucleus—a central clock) set clocks to the natural cycle of light and night. Almost all cell types have molecular clocks that control gene transcription in association with tissue-specific elements. Potential therapies include those that modify the activity of the central clock (such as light and melatonin, which both influence the sleep–wake cycle), as well as those that target peripheral targets such nucleotide levels, cryptochrome (CRY) stability, and nuclear receptor function [Abbreviation: P: proteins, C: carbohydrates, F: fatty acid, Circadian proteins: (BMAL1, CLOCK, PER, and CRY), SIRTs: sirtuin 1 is conserved mammalian nicotinamide adenine dinucleotide (NAD +) dependent histone deacetylase, which is encoded by the SIRT1 gene, SCN: the suprachiasmatic nucleus, often known as the SCN, is a collection of nerve cells (neurons) that functions as the body’s main clock. Direct input from the eyes is sent to the SCN, located in the hypothalamus part of the brain]
That virus infections, as mentioned, including COVID-19 are influenced by the circadian clock (Ray and Reddy 2020; Zandi et al. 2022; Zandi 2022). That the circadian clock effects on viruses may be a general phenomenon, supports the notion that mpox pathophysiology is likely under the control of the clock as well, even though there is as yet no direct evidence. This highlights the importance of researching mpox infection in relation to the circadian clock (Mazzoccoli et al. 2020).
Host cells are necessary for the replication, survival, and spread of viruses. The biological clock, which controls the circadian rhythmicity of immunological and cellular processes, shapes the host’s response to viral infections and patterns of host–pathogen interaction. Viral infections, like other infectious diseases, have an impact on the circadian clock circuitry of the infected host, which then interacts with the host’s molecular components. This shows that timing is important in this intricate interplay and raises the possibility that adopting chrono-modulated antiviral treatment strategies may be advantageous (Mazzoccoli et al. 2020). It has been demonstrated that the circadian clock affects viral infection by changing the host pathways necessary for viral replication. Viruses, unlike bacteria, do not have their own circadian rhythms, but they can affect and be influenced by the circadian rhythms of their hosts when they infect a cell. Viral infection may also alter circadian gene expression. According to previous studies of other viral infections (Ray and Reddy 2020; Ray et al. 2020; Mazzoccoli et al. 2020; Borrmann et al. 2021), the severity of mpox infection may depend on the time of exposure to the infectious agent in the day-night cycle. It has been demonstrated that simian immunodeficiency virus (SIV) infection impairs several components of circadian timing in monkeys, with significant ramifications for physiological processes, including temperature control and gross motor activity. These pathological changes are not connected to those found in the acute febrile response followed by viral infection. However, the animals show substantial circadian irregularities and hypothalamus microglia infiltration and macrophage development, implying similar physiological and psychological changes in HIV-infected people (Huitron-Resendiz et al. 2007).
Viral infections can be acute, like those caused by the influenza virus, or chronic, like those caused by the hepatitis B virus (HBV). It displays a coordination between the host immune response and viral escape mechanisms in both conditions. Given that viral replication depends on cellular pathways and since more than 80% of protein-coding genes in diverse tissues in humans exhibit daily rhythmic expression, it is not surprising that host clock components have been documented to either directly or indirectly influence virus replication (Borrmann et al. 2021). The significance of natural killer T cells, natural killer cells, and inflammatory monocytes in the daily dependence of influenza infection was shown by Sengupta et al. (2019). Nguyen et al. (2013) revealed that BMAL1 controls inflammatory monocytes’ diurnal rhythm. According to Majumdar et al. (2017), BMAL1 deficiency increases susceptibility to the respiratory syncytial virus (RSV) and PIV3 (human parainfluenza virus type 3) infection. Other respiratory viruses are also circadian dependent. In the context of pulmonary inflammation, REV-ERB can inhibit inflammatory responses including chemokine production (Caratti et al. 2018). Interleukin-6 (IL-6) production and the endotoxin response in macrophages were both boosted by genetic disruption of REV-ERB (Gibbs et al. 2012). These results demonstrate how the circadian clock controls the immune response, which has an impact on virus replication.
There is currently a lack of useful information on this topic for mpox, but given that the circadian rhythm is connected to the course of viral replication and the course of host tolerance, much needs to be accomplished for the outbreak of mpox in 2022. This also affected the unanticipated and surprising transmission routes in the mpox 2022 outbreak. By using monkeypox-specific cell lines and animal models (every 12 h and checking between the resting and active phases), the severity of the infection can be evaluated and correlated with the time of the viral infection and to what extent the mpox replication and its neutralization by the immune system require diverse circadian cycles. In addition, comparing common reservoirs of mpox in wild animals with the clock-dependent group will help to explain how mpox replication and progression may be grounded on circadian cycles (Shafaati and Zandi 2023).
It should be noted that “time of dosing and pharmacokinetic effectiveness” have an impact on circadian clocks (Sengupta et al. 2019). The dosage time affects most drugs with moderate (8 to 15 h) half-lives. The level of neutralizing antibodies that are induced after vaccination is regulated in part by the dosing time, which also controls the efficacy of viral vaccines (Ruben et al. 2019). Influenza virus strains A and B, for instance, respond better to morning vaccination than to evening vaccination (Long et al. 2016). To achieve the optimal clinical outcomes, circadian rhythm should not be neglected while formulating drugs, determining their dosage, and administering mpox vaccines. Mpox-host interactions affect essential physiological processes such as metabolic pathways, protein synthesis, macrophage activation, and apoptosis, which suppress inflammatory responses and disrupt interleukin and complement signaling (Lu and Zhang 2020; Weaver and Isaacs 2008).
Circadian clock and monkeypox virus infection
Because monkey and human poxviruses are so similar, monkeys were first used in smallpox experiments. The serial passage of monkeypox, variola, vaccinia, and chimpanzee poxviruses in baboons (Papio cynocephalus) has been the focus of numerous studies as well (Heberling et al. 1976). 53.4% of baboon genes, 8120 genes, undergo body-wide oscillations. Among these genes, there are daytime and nighttime variation groups (Soltani et al. 2021). Nighttime groups predominantly are enriched for cellular signaling and growth, whereas daytime groups of genes are predominantly enriched for metabolism.
The critical parts of the circadian network are CLOCK (along with its paralog NPAS2), its heterodimeric partner BMAL1 (ARNTL), and its downstream targets, PER1, PER2, CRY1, and CRY2 (Rijo-Ferreira and Takahashi 2019). To control circadian gene expression, the transcription factors CLOCK and BMAL combine to create heterodimers that bind to E-boxes, which are genomic regulatory regions. The repressors PER (period) and CRY (cryptochrome) are expressed as a result of this complex, and they dimerize to establish a negative feedback loop that inhibits CLOCK: BMAL1-mediated transcription (Sengupta et al. 2019). Different biological-physiological rhythms are produced because of core clock genes’ regulation. Although it is well established that a considerable portion (3–16%) of mRNA transcripts express themselves rhythmically, it is yet unknown how circadian cycles affects the transcriptomes in different cells (Hughes et al. 2009). Genes that interact with SARS-CoV-2 proteins are highly indicative of this rhythmicity. Notably for influenza and SARS-CoV-2, the inflammatory phase of viral infections is highly correlated with the circadian rhythm. Possible impacts on health care could result from viral infections linked to circadian cycles. The most circadian-regulated organs or cells may respond to infection in a time-dependent approach. These findings suggest that patients should refrain from actions that interfere with their circadian rhythms, such as insufficient sleep and excessive fatigue (Sengupta et al. 2019; Gachon et al. 2018). Melatonin may help anyone with certain circadian rhythm sleep disorders, whether they are adults or children.
Epigenetics, circadian clocks, and viral infection
DNA methylation, histone post-translational modifications (PTMs), and non-coding RNAs are the main mechanisms of epigenetic regulation. They all result in chromatin remodeling and changes in control of gene expression. Inputs to the cell, such as light or nutrients, allow the transcription of genes to turn on and off, eventually leading to signaling pathway activity clock-BMAL1-dependent clock-controlled gene activation is correlated with circadian modifications of histone PTM promoters (Shafaati et al. 2023). Chromatin remodelers are continuously recruited to the promoter region of clock-controlled genes, including sirtuin deacetylase 1 (SIRT1, a NAD+-dependent histone deacetylase) and histone deacetylase 3 (HDAC3). Clock transcription factor regulates activity of histone acetyltransferase. The clock-controlled genes’ rhythmic expression is canceled in its absence. The DNMT1, DNMT3a, and DNMT3b enzyme family methylates a cytosine residue in CpG dinucleotides, which is necessary for biological clock function (DNA methylation) (Sahar and Sassone-Corsi 2013) and is disrupted by viral infection. Approximately 3% of the world’s population is infected with hepatitis C virus (HCV), which infects the liver. Different genotypes of HCV have been demonstrated to interfere with molecular clock and epigenetic modifications (Jueliger et al. 2016). To control lipid metabolism, cell proliferation, and regeneration, SIRT1 regulates the circadian cycle of clock-controlled genes in the liver (Sato et al. 2017). It has been shown that HCV has a direct effect on the circadian clock system. Treatments for conditions linked to HCV infection may be more effective if circadian modulation of the HCV life cycle by host rhythmic oscillations were better understood (Ko and Takahashi 2006). The molecular clock and viral interaction with cellular processes are both influenced by genetic and epigenetic factors.
Conclusion
The host response to viral infections is determined by the biological circadian rhythm, which also regulates immune and cellular activity. This affects the patterns of host–pathogen interactions. Consequently, interference between the circadian clock and viral infection increases host susceptibility to emerging and re-emerging viral infections. Given the high endemic potential of mpox and other zoonotic viral infections, to improve clinical management and outcomes, it is important to determine whether infection is severe at specific times of the circadian cycle. In addition, the effects of environmental and genetic changes (epigenetic factors and ecosystem) should also be investigated.
Abbreviations
- mpox
Monkeypox
- MSM
Men who have sex with men
- HBV
Hepatitis B virus
- HCV
Hepatitis C virus
- HIV
Human immunodeficiency virus
- SIV
Simian immunodeficiency virus
- DNMTs
DNA methyltransferases
- HDAC-3
Histone deacetylase 3
Data availability
Not applicable.
Declarations
Ethics approval
Not applicable.
Informed consent
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Benegiamo G, Mazzoccoli G, Cappello F, Rappa F, Scibetta N, Oben J, et al. Mutual antagonism between circadian protein period 2 and hepatitis C virus replication in hepatocytes. PLoS ONE. 2013;8(4):e60527. doi: 10.1371/journal.pone.0060527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borrmann H, McKeating JA, Zhuang X. The circadian clock and viral infections. J Biol Rhythms. 2021;36(1):9–22. doi: 10.1177/0748730420967768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caratti G, Iqbal M, Hunter L, Kim D, Wang P, Vonslow RM, et al. REVERBa couples the circadian clock to hepatic glucocorticoid action. J Clin Investig. 2018;128(10):4454–4471. doi: 10.1172/JCI96138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang CC, Naranbhai V, Stern J, Roche M, Dantanarayana A, Ruian K, et al. Variation in cell associated unspliced HIV RNA on antiretroviral therapy is associated with the circadian regulator BMAL-1. AIDS (london, England) 2018;32(15):2119. doi: 10.1097/QAD.0000000000001937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choudhary O, Chopra H, Shafaati M, Dhawan M, Metwally A, Saied A et al (2022) Reverse zoonosis and its relevance to the monkeypox outbreak 2022. New microbes and new infections [DOI] [PMC free article] [PubMed]
- Edgar RS, Stangherlin A, Nagy AD, Nicoll MP, Efstathiou S, O’Neill JS, et al. Cell autonomous regulation of herpes and influenza virus infection by the circadian clock. Proc Natl Acad Sci. 2016;113(36):10085–10090. doi: 10.1073/pnas.1601895113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gachon F, Yeung J, Naef F. Cross-regulatory circuits linking inflammation, high-fat diet, and the circadian clock. Genes Dev. 2018;32(21–22):1359–1360. doi: 10.1101/gad.320911.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gibbs JE, Blaikley J, Beesley S, Matthews L, Simpson KD, Boyce SH, et al. The nuclear receptor REV-ERBα mediates circadian regulation of innate immunity through selective regulation of inflammatory cytokines. Proc Natl Acad Sci. 2012;109(2):582–587. doi: 10.1073/pnas.1106750109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heberling R, Kalter S, Rodriguez A. Poxvirus infection of the baboon (Papio cynocephalus) Bull World Health Organ. 1976;54(3):285. [PMC free article] [PubMed] [Google Scholar]
- Hughes ME, DiTacchio L, Hayes KR, Vollmers C, Pulivarthy S, Baggs JE, et al. Harmonics of circadian gene transcription in mammals. PLoS Genet. 2009;5(4):e1000442. doi: 10.1371/journal.pgen.1000442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huitron-Resendiz S, Marcondes MCG, Flynn CT, Lanigan CM, Fox HS. Effects of simian immunodeficiency virus on the circadian rhythms of body temperature and gross locomotor activity. Proc Natl Acad Sci. 2007;104(38):15138–15143. doi: 10.1073/pnas.0707171104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jueliger S, Lyons J, Cannito S, Pata I, Pata P, Shkolnaya M, et al. Efficacy and epigenetic interactions of novel DNA hypomethylating agent guadecitabine (SGI-110) in preclinical models of hepatocellular carcinoma. Epigenetics. 2016;11(10):709–720. doi: 10.1080/15592294.2016.1214781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ko CH, Takahashi JS (2006) Molecular components of the mammalian circadian clock. Human molecular genetics 15(suppl_2):R271–R7 [DOI] [PubMed]
- Long JE, Drayson MT, Taylor AE, Toellner KM, Lord JM, Phillips AC. Morning vaccination enhances antibody response over afternoon vaccination: a cluster-randomised trial. Vaccine. 2016;34(24):2679–2685. doi: 10.1016/j.vaccine.2016.04.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu Y, Zhang L. DNA-sensing antiviral innate immunity in poxvirus infection. Front Immunol. 2020;11:1637. doi: 10.3389/fimmu.2020.01637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Majumdar T, Dhar J, Patel S, Kondratov R, Barik S. Circadian transcription factor BMAL1 regulates innate immunity against select RNA viruses. Innate Immun. 2017;23(2):147–154. doi: 10.1177/1753425916681075. [DOI] [PubMed] [Google Scholar]
- Man K, Loudon A, Chawla A. Immunity around the clock. Science. 2016;354(6315):999–1003. doi: 10.1126/science.aah4966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matsuzawa T, Nakamura Y, Ogawa Y, Ishimaru K, Goshima F, Shimada S, et al. Differential day-night outcome to HSV-2 cutaneous infection. J Invest Dermatol. 2018;138(1):233–236. doi: 10.1016/j.jid.2017.07.838. [DOI] [PubMed] [Google Scholar]
- Mazzoccoli G, Vinciguerra M, Carbone A, Relógio A. The circadian clock, the immune system, and viral infections: the intricate relationship between biological time and host-virus interaction. Pathogens. 2020;9(2):83. doi: 10.3390/pathogens9020083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mukherji A, Bailey SM, Staels B, Baumert TF. The circadian clock and liver function in health and disease. J Hepatol. 2019;71(1):200–211. doi: 10.1016/j.jhep.2019.03.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nguyen KD, Fentress SJ, Qiu Y, Yun K, Cox JS, Chawla A. Circadian gene Bmal1 regulates diurnal oscillations of Ly6Chi inflammatory monocytes. Science. 2013;341(6153):1483–1488. doi: 10.1126/science.1240636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrono LV, Pléh K, Samuni L, Ulrich M, Röthemeier C, Sachse A, et al. Monkeypox virus emergence in wild chimpanzees reveals distinct clinical outcomes and viral diversity. Nat Microbiol. 2020;5(7):955–965. doi: 10.1038/s41564-020-0706-0. [DOI] [PubMed] [Google Scholar]
- Ray S, Reddy AB. COVID-19 management in light of the circadian clock. Nat Rev Mol Cell Biol. 2020;21(9):494–495. doi: 10.1038/s41580-020-0275-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ray S, Valekunja UK, Stangherlin A, Howell SA, Snijders AP, Damodaran G, et al. Circadian rhythms in the absence of the clock gene Bmal1. Science. 2020;367(6479):800–806. doi: 10.1126/science.aaw7365. [DOI] [PubMed] [Google Scholar]
- Reynolds MG, Yorita KL, Kuehnert MJ, Davidson WB, Huhn GD, Holman RC, et al. Clinical manifestations of human monkeypox influenced by route of infection. J Infect Dis. 2006;194(6):773–780. doi: 10.1086/505880. [DOI] [PubMed] [Google Scholar]
- Rijo-Ferreira F, Takahashi JS. Genomics of circadian rhythms in health and disease. Genome Medicine. 2019;11(1):1–16. doi: 10.1186/s13073-019-0704-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruben MD, Smith DF, FitzGerald GA, Hogenesch JB. Dosing time matters. Science. 2019;365(6453):547–549. doi: 10.1126/science.aax7621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saijo M, Ami Y, Suzaki Y, Nagata N, Iwata N, Hasegawa H, et al. Virulence and pathophysiology of the Congo Basin and West African strains of monkeypox virus in non-human primates. J Gen Virol. 2009;90(9):2266–2271. doi: 10.1099/vir.0.010207-0. [DOI] [PubMed] [Google Scholar]
- Sengupta S, Tang SY, Devine JC, Anderson ST, Nayak S, Zhang SL, et al. Circadian control of lung inflammation in influenza infection. Nat Commun. 2019;10(1):1–13. doi: 10.1038/s41467-019-11400-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shafaati M, Zandi M (2022) State-of-the-art on monkeypox virus: an emerging zoonotic disease. Infection 1–6 [DOI] [PubMed]
- Shafaati M, Zandi M. Monkeypox virus neurological manifestations in comparison to other orthopoxviruses. Travel Med Infect Dis. 2022;1(49):102414. doi: 10.1016/j.tmaid.2022.102414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shafaati M, Zandi M, Choudhary OP (2022) Monkeypox virus crosstalk with HIV; where do we stand now? Int J Surg (London, England) 105:106897–106897 [DOI] [PMC free article] [PubMed]
- Shafaati M, Zandi M. Human monkeypox (hMPXV) re-emergence: host immunity status and current vaccines landscape. J Med Virol. 2023;95(1):e28251. doi: 10.1002/jmv.28251. [DOI] [PubMed] [Google Scholar]
- Shafaati M, Zandi M, Choudhary OP. Impact of epigenetic mechanisms in re-emerging viruses. Travel Med Infect Dis. 2023;52:102535. doi: 10.1016/j.tmaid.2022.102535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sahar S, Sassone-Corsi P (2013) The epigenetic language of circadian clocks. Circadian clocks 29–44 [DOI] [PubMed]
- Sato S, Solanas G, Peixoto FO, Bee L, Symeonidi A, Schmidt MS et al (2017) Circadian reprogramming in the liver identifies metabolic pathways of aging. Cell 170(4):664–77. e11 [DOI] [PMC free article] [PubMed]
- Silver AC, Buckley SM, Hughes ME, Hastings AK, Nitabach MN, Fikrig E. Daily oscillations in expression and responsiveness of Toll-like receptors in splenic immune cells. Heliyon. 2018;4(3):e00579. doi: 10.1016/j.heliyon.2018.e00579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soltani S, Faramarzi S, Zandi M, Shahbahrami R, Jafarpour A, Rezayat SA, et al. Bacterial coinfection among coronavirus disease 2019 patient groups: an updated systematic review and meta-analysis. New Microbes and New Infections. 2021;43:100910. doi: 10.1016/j.nmni.2021.100910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weaver JR, Isaacs SN. Monkeypox virus and insights into its immunomodulatory proteins. Immunol Rev. 2008;225(1):96–113. doi: 10.1111/j.1600-065X.2008.00691.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zandi M (2022) ORF9c and ORF10 as accessory proteins of SARS-CoV-2 in immune evasion. Nat Rev Immunol 22(5):331–131 [DOI] [PMC free article] [PubMed]
- Zandi M, Shokri S, Mahmoudvand S, Hosseinzadeh Adli A, Mohammadi R, Haddadi A. Interplay between cellular metabolism and DNA viruses. J Med Virol. 2022;94(11):5163–5173. doi: 10.1002/jmv.28018. [DOI] [PubMed] [Google Scholar]
- Zhuang X, Rambhatla SB, Lai AG, McKeating JA. Interplay between circadian clock and viral infection. J Mol Med. 2017;95(12):1283–1289. doi: 10.1007/s00109-017-1592-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.