Abstract
Introduction
Sexual health is an important aspect of quality of life, yet both healthcare professionals and patients might hesitate to bring up the topic during appointments. Our study investigated obstetrician‐gynecologists' (OB/GYNs') self‐reported competences in discussing and treating sexual problems, as well as the barriers to bringing up the subject. An additional aim was to evaluate the need for continuing education in sexual medicine.
Material and methods
A web‐based questionnaire was sent to the members of The Finnish Society of Obstetrics and Gynecology (n = 1212). The survey was completed by 328 respondents (275 specialists and 53 OB/GYN residents). Their background information (gender, age, education, occupational status, daily number of patients, and daily number of patients with sexual health issues) was assessed. The questionnaire included four fields: (A) self‐reported competence in discussing and treating patients with sexual problems (three questions), (B) the barriers to bringing up sexual problems with patients (nine questions), (C) the source of education in sexual medicine (two questions), and (D) the need for education in sexual medicine (two questions).
Results
Most of the OB/GYNs self‐reported their competence to be good in discussing sexual problems, but poor in treating patients' sexual problems. The male OB/GYNs reported better competence than did the females. Several barriers were identified—most frequently, “shortness of the appointment time” (76%), “lack of knowledge about sexual medicine” (75%), and “lack of experience with sexual medicine” (74%). Older OB/GYNs and male OB/GYNs reported fewer barriers. The majority of the respondents considered their previous education in sexual medicine to be insufficient, especially in medical school (95%), but also in residency (83%), and they reported a need for additional education.
Conclusions
Our study indicated several barriers that hindered OB/GYNs from assessing sexual problems during appointments. Although OB/GYNs reported a good competence in discussing sexual problems, they reported a poor competence in treating them. Their previous education in sexual medicine was rated as insufficient, and continuing education was desired. The information provided by our study can be used for improving and organizing education in sexual medicine, which is crucial for diminishing the barriers to discussing and treating sexual problems.
Keywords: barriers, competence, education, gender, obstetrician‐gynecologist, sexual medicine
Obstetrician‐gynecologists self‐reported a good competence in discussing, but a poor competence in treating sexual problems. The majority considered their current state of education in sexual medicine insufficient.
Abbreviations
- aOR
adjusted odds ratio
- CI
confidence interval
- CME
continuing medical education
- OB/GYN
obstetrician‐gynecologist
Key message.
Obstetrician‐gynecologists self‐reported a good competence in discussing, but a poor competence in treating sexual problems. Several barriers emerged, a lack of time being the most frequently identified. The majority considered their current state of education in sexual medicine insufficient.
1. INTRODUCTION
Good sexual health is considered to be one of the cornerstones of good quality of life. 1 , 2 For women, obstetrician‐gynecologists (OB/GYNs) hold an important role in the assessment of sexual health issues. Sexual concerns are frequent; nevertheless, women may not bring up the topic themselves during appointments, instead often expecting the healthcare professionals to initiate the conversation. 1 , 3 According to a Latvian study, 4 80% of the women reported that they would like to be asked about sexual health issues during their gynecological visits, but only one‐third of them had that experience. In a Norwegian study, 87% of women stated that they would accept, of which 35% would like that the gynecologist ask about sexual function during an appointment. 5 Shame and other psychoemotional barriers were considered to be the main obstacles preventing women from starting the conversation. 4 In a Swedish study, the majority of young women having a gynecological examination reported that they had never been asked about sexual health issues (76%–99%, depending on the specific question). 6 A British survey showed that 37% of the women in (uro)gynecology clinics had a sexual complaint, but only 17% volunteered this information, and the rest only admitted it when questioned. 7
The American College of Obstetricians and Gynecologists has recommends that OB/GYNs should initiate a clinical discussion of sexual function during routine care visits. 8 Likewise, the European Board and College of Obstetrics and Gynecology states that women should have the opportunity to address sexual health problems alongside matters related to contraception and general sexual health. 9 However, for clinicians, several barriers may hinder them in bringing up the issue, the most frequently identified being the limited time in appointments and a lack of education. 10 , 11 Additionally, embarrassment 12 and the absence of effective treatment options 11 , 12 have been found to be obstacles to discussing sexual health issues. Mixed results have been reported in the studies focusing on the association between OB/GYNs' gender and age with regard to bringing up sexual health issues as a part of their routine clinical work. 11 , 13 , 14 , 15 In some studies, female 13 , 14 and younger 13 physicians were found to be more likely to ask about sexual activity compared to male and older physicians, respectively. However, in other studies, no differences concerning the OB/GYNs' gender 15 or age 14 , 15 have been found. According to a meta‐analysis conducted in the United States, male OB/GYNs typically provide higher self‐ratings than do female OB/GYNs in a number of areas (training, knowledge, performance, confidence, and competence or ability). 16 In that meta‐analysis, altogether 97 articles assessed gender differences, of which 11 articles evaluated self‐ratings. Similar findings of higher self‐reported ratings among male physicians compared to female physicians have also been reported in other specialties. 17 , 18
Many barriers to discussing sexual health have also been reported from the perspective of the patients. According to a Swedish study, of women with prolonged or severe dyspareunia, only 28% had consulted a physician. 19 In another study carried out in five Anglophone countries, only 32% of men and women with sexual problems had sought medical care. 20 The barriers to seeking medical care included the lack of bothersomeness, 20 embarrassment, 20 doubt about the possibility of a cure, 21 faith in the spontaneous remission of the problem, 21 and the fear of stigma. 21 In addition, many patients did not think they had a medical problem. 20 , 21
Our study investigated OB/GYNs' self‐reported competence in discussing and treating sexual problems during appointments in Finland. The barriers related to bringing up the issue were also assessed. We hypothesized that OB/GYNs face a range of barriers that prevent them from bringing up sexual health issues, even though they treat problems closely related to patients' sexual function. The information provided by our study can be used for planning and organizing future education in sexual medicine.
2. MATERIAL AND METHODS
This study was a part of the Finnish Sexual Medicine Education (SexMEdu) study investigating the level of education in sexual medicine in Finland. The participants were among the members of The Finnish Society of Obstetrics and Gynecology, which consists mainly of OB/GYN specialists and residents. The Society had 1212 members in 2019, including both working and retired OB/GYNs. The vast majority of OB/GYNs specialists and residents belong to The Finnish Society of Obstetrics and Gynecology, as it offers annual national educational meetings throughout the year and serves as a networking platform. OB/GYN residents often join the Society already at the beginning of their training. In Finland, there were 680 specialists in OB/GYN in 2019, of which 87% were female. 22 The Finnish Society of Obstetrics and Gynecology permitted us to send a questionnaire to members using its register of contact details. We did not have access to the actual register; instead, the Society forwarded our request to its members. A web‐based questionnaire and two reminders were sent between January 2019 and February 2020. Furthermore, an additional email was sent to chief physicians of OB/GYN in hospitals in order to improve the response rate. In the preface, it was stated that the questionnaire was directed only at OB/GYN specialists and residents. Background information included gender (female/male/other), age, education (specialist/resident), occupational status (hospital/private sector/researcher/clinical teacher/primary health/retired/other [maternal leave/leave of absence/sick leave/not currently working]/student; every responder could have several occupations), number of patients treated per day (1–10/≥11), and number of patients dealt with sexual health issues per day (0/1–5/≥6).
The questionnaire was a modification of the Portuguese SEXOS study questionnaire. 17 Permission to use the questionnaire was received from the Portuguese researchers. Translation to Finnish was carried out from the English version of the SEXOS questionnaire. This part of the study included the following four fields: (A) Self‐reported competence in discussing and treating patients with sexual problems (three separate questions), (B) Barriers to bringing up sexual problems during OB/GYNs' appointments (nine separate items), (C) Source of education in sexual medicine (two separate questions), and (D) Need for education in sexual medicine (two separate questions).
The questions are presented in Table 1. The web‐based questionnaire was programed not to proceed in case of a missing answer, ensuring that every participant submitted a complete questionnaire. The possible duplicate questionnaires were omitted (the same gender, age, the university and the year of graduation of medical degree and the university and the year of graduation of OB/GYN specialist).
TABLE 1.
Study questionnaire
| (A) The self‐reported competence in discussing and treating patients with sexual problems | |
| 1. How do you classify your competence in discussing sexual health problems with your patients? | |
| “Good”/“Quite good”/ “Quite poor”/ “Poor” | |
| 2. How do you classify your competence in treating your patients' sexual problems? | |
| “Good”/“Quite good”/“Quite poor”/“Poor” | |
| 3. How easy is it for you to discuss sexual health issues if your patient addresses the subject? | |
| “Not a problem”/“A minor problem”/“A moderate problem”/“A major problem”/“Cannot say” | |
| (B) The barriers to bringing up sexual problems during OB/GYNs' appointments | |
| Each item rated on a 5‐point scale of | |
| 1 = “Not at all”, 2 = “…,” 3 = “…,” 4 = “Very much”, and 5 = “Cannot say” | |
| Bringing up sexual problems with patients hinders: | |
| |
| |
| |
| |
| |
| |
| |
| |
| |
| (C) The source of education in sexual medicine | |
| 1. From which sources have you gained your knowledge about sexual medicine that you use in your patient work? (you can choose more than one option) | |
| “Medical books”/“Medical journals”/“Continuing education”/ “Congresses”/ “Consultation of guideline”/ “Education given in medical school”/ “Consultations and discussions with colleagues”/ “Education given in residency”/ “Sexuality counselor (authorized) training”/ “Sexuality therapist (authorized) training”/ “Clinical sexologist (authorized) training”/ “Other therapy training”/ “Sexuality educator (authorized) training”/ “Other, what:_____________” | |
| 2. How sufficient do you classify your prior education as a source of education when considering your sexual medicine competence? | |
| Each item rated on a 5‐point scale of | |
| 1 = “Insufficient”, 2 = “…,”3 = “…,” 4 = “Sufficient,” and 5 = “Not taken” | |
| (a) Medical school | |
| (b) Residency | |
| (c) Continuing medical education | |
| (D) The need for education in sexual medicine | |
| 1. Do you feel a need for continuing education in sexual medicine? | |
| “Yes”/ “No” | |
| 2. If you answered “yes” in which form would you prefer receiving continuing education? | |
| “Lectures”/“Workshops”/“Simulations”/ “Online learning platforms”/“Something else, what:____________” |
2.1. Statistical analyses
Data is presented with frequencies (percentages). In the analyses, each question in fields A and B was dichotomized (A: questions 1 and 2 were “poor” or “quite poor” vs “good” or “quite good” and question 3 was “a major problem” or “a moderate problem” vs “not a problem” or “a minor problem”; B: “very much” or “much” vs “not at all” or “some”). The “cannot say” responses in field B and in question 3 in field A were omitted from the analyses. Question 2 in field C was dichotomized as “insufficient” or “quite insufficient” vs “sufficient” or “quite sufficient.” Question 1 in field C and question 2 in field D were multiple‐choice questions with several options.
In the four fields of interests, (A–D), multivariable binary logistic regression was carried out with adjustment for the OB/GYNs' gender (female/male), age (28–39/40–49/50–74 years), daily number of patients treated (1–10/≥11) and daily number of patients who dealt with sexual health issues (0/1–5/≥6). In each field, each question was examined separately in the analyses. The results are presented using adjusted odds ratios (aORs) with 95% confidence intervals (CIs). p‐values of less than 0.05 were considered statistically significant. Statistical analyses were performed using the SAS System for Windows, version 9.4 (SAS Institute Inc.).
2.2. Ethics statement
The study protocol was approved by the Ethics Committee of Turku University (44/2017) on September 11, 2017. The Finnish Sexual Medicine Education (SexMEdu) study respected the Helsinki Declaration in terms of the anonymity of the participants and obtaining of informed consent. Replying to the questionnaire implied consent, which was made clear to the respondents within the questionnaire.
3. RESULTS
The survey was completed by 328 respondents, resulting in a response rate of 27%. Of these, 275 were OB/GYN specialists and 53 were residents. Eight respondents reported not working as clinicians, leading to their exclusion. In addition, there were 21 possible duplicates, which were omitted. Thus, 299 questionnaires were eligible for the analysis (Figure 1). Basic characteristics of the respondents are shown in Table 2. The mean age of the respondents was 47.1 years (SD 11.0, range 28–74 years). The mean age of the female respondents was 46.5 years (SD 10.5, range 28–74 years) and the male respondents 55 years (SD 14.0: range 30–74 years). Of all, 214 OB/GYNs reported working in a hospital, and of these, 44% also reported working in the private the sector, 19% as researchers, 7% as clinical teachers and 3% in primary health care. Moreover, 58 (19%) OB/GYNs reported to work in the private sector only. Furthermore, 12 retired OB/GYNs reported working in the private sector after having had a career working in a hospital, which is also allowed in Finland.
FIGURE 1.
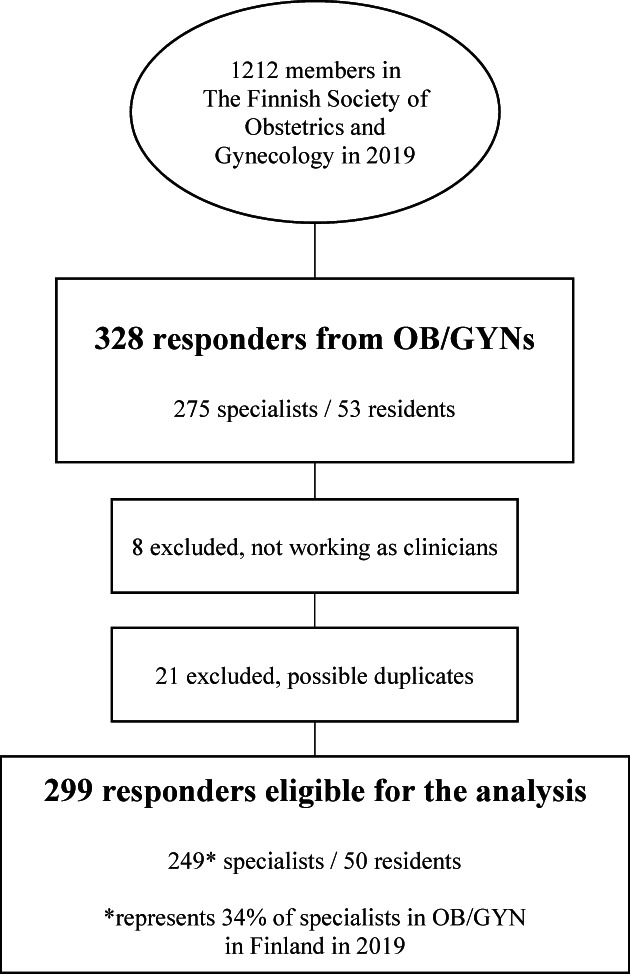
Flowchart of the study.
TABLE 2.
Basic characteristics (n = 299)
| % (n) | |
|---|---|
| Gender | |
| Female | 93 (278) |
| Male | 7 (21) |
| Other | 0 (0) |
| Age (years) | |
| 28–39 | 27 (82) |
| 40–49 | 36 (107) |
| 50–74 | 37 (110) |
| Education | |
| Specialist in OB/GYN | 83 (249) |
| Resident in OB/GYN | 17 (50) |
| Occupational status a | |
| Working in a hospital | 72 (214) |
| Working in the private sector | 56 (166) |
| Working as a researcher | 14 (41) |
| Working as a clinical teacher | 5 (16) |
| Working in primary health care | 5 (14) |
| Patients treated per day | |
| 1–10 | 39 (116) |
| ≥11 | 61 (183) |
| Patients dealt with sexual health issues per day | |
| 0 | 14 (41) |
| 1–5 | 74 (221) |
| ≥6 | 12 (37) |
More than one occupational option could be chosen. Also includes OB/GYNs who reported to be retired, students, on maternal leave or sick leave.
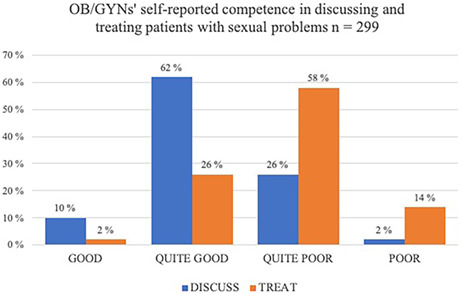
The results of self‐reported competence in discussing and treating patients with sexual problems are shown in Table 3. Most of the OB/GYNs (72%, n = 215/299) reported that their general competence in discussing sexual problems with their patients was good or quite good. However, an identical percentage (72%, n = 216/299) reported that their competence in treating patients' sexual problems was poor or quite poor. Compared to the male OB/GYNs, the female OB/GYNs were more likely to report a poor or quite poor competence treating (female 75%, n = 209/278 vs male 33%, n = 7/21) their patients' sexual problems. Additionally, there was a statistical tendency (aOR 4.41, CI: 0.95–20.36, p = 0.058) that the female OB/GYN were more likely to report a poor or quite poor competence in discussing sexual problems with their patients (female 29%, n = 82/278 vs male 10%, n = 2/21). As for age groups, the OB/GYNs in the age group of 40–49 years were less likely to report poor or quite poor competence to discuss compared to the age group of 28–39 years. No differences according to the number of patients treated daily were found. Furthermore, the more often the OB/GYNs dealt with sexual health issues with patients daily, the less they reported a poor or quite poor competence in discussing (0 patients per day dealt with sexual health issues: 43%, n = 18/41 vs 1–5 patients per day: 27%, n = 61/221 vs ≥6 patients per day: 14%, n = 5/37) and treating (0 patients per day dealt with sexual health issues: 89%, n = 36/41 vs 1–5 patients per day: 76%, n = 183/221 vs ≥6 patients per day: 32%, n = 12/37) their patients' sexual problems. If the patient brought up sexual health issues herself, almost all (98%, n = 294/299) of the OB/GYNs reported having no or only minor problems with discussing the subject, with no differences related to gender, age, or daily number of patients (no “cannot say” responses).
TABLE 3.
Self‐reported competence in discussing and treating patients with sexual problems (n = 299)
| Discussing with patients | Treating patients | |||
|---|---|---|---|---|
| Poor or quite poor | Poor or quite poor | |||
| 28% (n = 84) | 72% (n = 216) | |||
| aOR | 95% CI | aOR | 95% CI | |
| Gender | p = 0.058 | p < 0.0001 | ||
| Male | ref | ref | ||
| Female | 4.41 | 0.95–20.36 | 11.01 | 3.76–32.73 |
| Age | p = 0.034 | p = 0.403 | ||
| 28–39 | ref | ref | ||
| 40–49 | 0.41 | 0.21–0.81 | 0.63 | 0.30–1.34 |
| 50–74 | 0.72 | 0.39–1.35 | 0.62 | 0.29–1.33 |
| Patients treated per day | p = 0.454 | p = 0.631 | ||
| ≥11 | ref | ref | ||
| 1–10 | 0.81 | 0.47–1.40 | 0.86 | 0.48–1.57 |
| Patients dealt with sexual health issues per day | p = 0.014 | p < 0.0001 | ||
| ≥6 | ref | ref | ||
| 1–5 | 2.56 | 0.94–7.01 | 7.93 | 3.61–17.42 |
| 0 | 5.55 | 1.70–18.08 | 27.76 | 7.28–105.82 |
Note: p‐values are over the group values. aOR higher than 1 indicates worse self‐reported competence in the comparison group compared to the reference group (two categories: poor or quite poor vs good or quite good) in discussing or treating patients. aOR less than 1 indicates better self‐reported competence in the comparison group compared to the reference group (two categories: poor or quite poor vs good or quite good) in discussing or treating patients. The multivariable binary logistic regression was carried out with adjustment of OB/GYNs' gender (female/male), age (28–39/40–49/50–74 years), the number of patients treated per day (1–10/≥11) and the number of patients dealt with sexual health issues per day (0/1–5/≥6).
Abbreviations: aOR, adjusted odds ratio; CI, confidence interval; multivariable logistic regression.
The frequencies of the various barriers to bringing up sexual problems are presented in Table 4. In the entire cohort, the four most important barriers were “shortness of the appointment time”, “lack of knowledge about sexual medicine”, “lack of experience with sexual medicine”, and “sexual problem not being a priority at the appointment”. More female OB/GYNs than male OB/GYNs reported that “shortness of the appointment time”, “lack of knowledge about sexual medicine”, “lack of experience”, and “lack of effective treatment” were barriers much or very much of the time when bringing up sexual problems. Compared to the OB/GYNs in the youngest age group, fewer OB/GYNs in both of the older age groups reported barriers much or very much of the time concerning “shortness of the appointment time”, “lack of knowledge about sexual medicine”, “lack of experience with sexual medicine”, and “fear of failing to respond to patients’ sexual problems”.
TABLE 4.
Barriers to bringing up sexual problems with patients (n = 299)
| Shortness of the appointment time | Sexual problem not being a priority in the appointment | Personal attitudes and beliefs | Personal discomfort when addressing sexual problems | Lack of knowledge about sexual medicine | Lack of experience with sexual medicine | Lack of effective treatment | Fear of failing to respond to patients' sexual problems | Disability of the patient | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Much or very much 76% (n = 227/298) | Much or very much 62% (n = 185/286) | Much or very much 10% (n = 29/292) | Much or very much 10% (n = 30/298) | Much or very much 75% (n = 225/296) | Much or very much 74% (n = 220/297) | Much or very much 55% (n = 165/280) | Much or very much 46% (n = 139/296) | Much or very much 8% (n = 25/280) | ||||||||||
| Entire group | aOR | 95% CI | aOR | 95% CI | aOR | 95% CI | aOR | 95% CI | aOR | 95% CI | aOR | 95% CI | aOR | 95% CI | aOR | 95% CI | aOR | 95% CI |
| Gender | p = 0.0004 | p = 0.328 | p = 0.173 | p = 0.329 | p = 0.003 | p = 0.012 | p = 0.002 | p = 0.077 | p = 0.537 | |||||||||
| Male | ref | ref | ref | ref | ref | ref | ref | ref | ref | |||||||||
| Female | 7.76 | 2.50–24.10 | 1.63 | 0.61–4.36 | 0.42 | 0.12–1.47 | 2.83 | 0.35–22.79 | 4.72 | 1.70–13.12 | 3.77 | 1.35–10.56 | 5.55 | 1.91–16.15 | 2.58 | 0.90–7.35 | 1.94 | 0.24–15.95 |
| Age | p < 0.0001 | p = 0.104 | p = 0.213 | p = 0.863 | p = 0.011 | p = 0.001 | p = 0.663 | p = 0.0004 | p = 0.159 | |||||||||
| 28–39 | ref | ref | ref | ref | ref | ref | ref | ref | ref | |||||||||
| 40–49 | 0.08 | 0.03–0.23 | 0.64 | 0.33–1.26 | 1.16 | 0.38–3.52 | 1.15 | 0.42–3.14 | 0.30 | 0.13–0.72 | 0.19 | 0.08–0.48 | 1.14 | 0.61–2.13 | 0.29 | 0.15–0.54 | 0.38 | 0.13–1.09 |
| 50–74 | 0.18 | 0.06–0.56 | 0.48 | 0.25–0.94 | 2.22 | 0.79–6.25 | 1.31 | 0.49–3.46 | 0.28 | 0.12–0.67 | 0.22 | 0.09–0.54 | 1.34 | 0.71–2.51 | 0.43 | 0.23–0.79 | 0.51 | 0.19–1.36 |
| patients treated per day | p = 0.468 | p = 0.590 | p = 0.431 | p = 0.369 | p = 0.290 | p = 0.213 | p = 0.759 | p = 0.687 | p = 0.312 | |||||||||
| ≥11 | ref | ref | ref | ref | ref | ref | ref | ref | ref | |||||||||
| 1–10 | 0.79 | 0.42–1.50 | 1.16 | 0.68–1.98 | 0.72 | 0.31–1.65 | 1.43 | 0.66–3.08 | 0.72 | 0.40–1.32 | 0.69 | 0.38–1.24 | 1.08 | 0.65–1.82 | 0.90 | 0.55–1.49 | 0.62 | 0.25–1.56 |
| Patients dealt with sexual health issues per day | p = 0.0002 | p = 0.0004 | p = 0.231 | p = 0.140 | p = 0.0001 | p < 0.0001 | p = 0.196 | p = 0.016 | p = 0.545 | |||||||||
| ≥6 | ref | ref | ref | ref | ref | ref | ref | ref | ref | |||||||||
| 1–5 | 5.48 | 2.41–12.44 | 4.39 | 2.04–9.44 | 1.12 | 0.31–4.10 | 3.80 | 0.49–29.47 | 4.55 | 2.10–9.84 | 4.97 | 2.26–10.94 | 1.85 | 0.89–3.85 | 2.49 | 1.12–5.57 | 0.95 | 0.26–3.56 |
| 0 | 5.95 | 1.76–20.10 | 5.80 | 2.06–16.35 | 2.60 | 0.57–11.75 | 7.55 | 0.85–67.24 | 10.30 | 2.92–36.32 | 9.34 | 2.78–31.40 | 2.3 | 0.84–6.30 | 4.52 | 1.60–12.73 | 1.76 | 0.36–8.85 |
Note: The “cannot say” responses were omitted from the analyses. In each question the number of analyzed responses/total number of questionnaires are shown in the upper column. p‐values are over the group values. aOR higher than 1 indicates that the specific barrier is more likely to be reported as “much or very much” a barrier by the comparison group compared to the reference group. aOR lower than 1 indicates that the specific barrier is less likely to be reported as “much or very much” a barrier by the comparison group compared to the reference group. The multivariable binary logistic regression was carried out with adjustment of OB/GYNs' gender (female/male), age (28–39/40–49/50–74 years), the number of patients treated per day (1–10/≥11) and the number of patients dealt with sexual health issues per day (0/1–5/≥6).
Abbreviations: aOR, adjusted odds ratio; CI, confidence interval; multivariable logistic regression.
No differences emerged according to the number of patients treated daily. Furthermore, the OB/GYNs dealt with sexual health issues with patients less frequently were more likely to report that “shortness of the appointment time”, “sexual problem not being a priority at the appointment”, “lack of knowledge”, “lack of experience”, and “fear of failing to respond to patients” problems were barriers.
The participants' sources of education in sexual medicine are presented in Figure 2. The most important source was medical journals (68%, n = 202/299), followed by consulting/discussing with colleagues (56%, n = 168/299), continuing medical education (CME) (50%, n = 149/299), and medical books (45%, n = 134/299). Most of the OB/GYNs (95%, n = 283/299), reported that the education in sexual medicine they received during medical school was insufficient, and 83% (n = 248/299) considered the education in sexual medicine they received during their residency to be insufficient. CME was rated better, yet 43% (n = 129/299) still considered it insufficient. Nearly one third of the OB/GYNs (27%, n = 81/299) reported not participating in CME related to sexual medicine at all.
FIGURE 2.
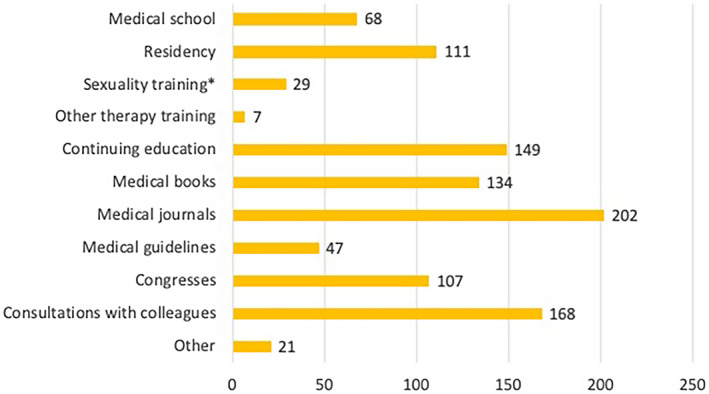
Self‐reported sources of education in sexual medicine, n = 299 (more than one option could be chosen). *Sexuality educator/counselor/therapist, clinical sexologist training (authorized).
A vast majority of the OB/GYNs (92%, n = 276/299), reported a need for CME in sexual medicine. Here, there was a difference between the age groups: compared to the OB/GYNs in the 28–39 age group, those in the 40–49 age group were more likely to report a need for CME (aOR 15.34, 95% CI: 1.92–122.59, p = 0.010). Compared to the OB/GYNs dealt with sexual health issues with 1–5 patients daily, those OB/GYNs dealt with 0 patients daily were more likely to report a need for CME (aOR 3.34, 95% CI: 1.09–10.26, p = 0.036). No other differences emerged related to gender or daily number of patients. Those reporting a need for CME preferred to receive this education through lectures (91%, n = 249/275) and online learning platforms (58%, n = 160/275), followed by workshops (26%, n = 71/275) and simulations (16%, n = 44/275).
4. DISCUSSION
Our study is the first to survey the barriers to bringing up sexual problems in OB/GYNs' appointments in Finland, and, to the best of our knowledge also in Scandinavia. Although the OB/GYNs self‐reported a good level of competence in discussing sexual problems with their patients, they considered their competence in treating these problems to be poor. This finding was most evident among female OB/GYNs. The OB/GYNs indicated several barriers to bringing up sexual problems, among which “shortness of the appointment time” was the most important. Furthermore, “lack of knowledge about sexual medicine” and “lack of experience with sexual medicine” were highlighted. Interestingly, a minority reported facing barriers related to their “personal attitudes and beliefs”, their “personal discomfort”, or “disability of the patient”. Our findings bring to attention the need for continuing education in sexual medicine, which the OB/GYNs themselves also wished for. It was notable that the education in sexual medicine given in medical school and even in residency was considered to be insufficient.
In our study, the most frequently reported barrier to bringing up sexual problems with patients was “shortness of the appointment time”. Our results confirmed the results of previous studies among OB/GYNs and urogynecologists in various countries. 10 , 11 , 15 Similar barriers related to time have also been described in studies conducted in other specialties. 17 , 23 , 24 Furthermore, we found that female OB/GYNs, younger OB/GYNs, and OB/GYNs who reported dealing with sexual health issues less often were more likely to report this barrier. Sexual health issues can be complex and, thus, undoubtedly time‐consuming to address. Therefore, methods facilitating for instance sexual history taking, such as computer applications 25 and screening tools, 26 could be useable.
In addition, in our study, “lack of knowledge and experience with sexual medicine” and “fear of failing to respond to patients” sexual problems' were reported to be important barriers. Comparable findings have previously been reported among both OB/GYNs 10 , 11 , 15 and general practitioners. 23 , 24 All these barriers emphasize the need for high‐quality and sufficient education. Indeed, the majority of the OB/GYNs in our study regarded that their education in sexual medicine was insufficient and the vast majority expressed the need for continuing education. These findings are similar to those of previous studies conducted among OB/GYN residents 27 , 28 and medical students. 29 A crucial problem is that education in sexual medicine is fragmented and nonstandardized, and it also differs from country to country. Most medical programs dedicate only a few hours to sexual health content, the majority of which is focused on reproduction and disorders of anatomy rather than on practicing how to integrate sexual health into clinical anamnesis and conversations. 30 It could be worthwhile to introduce efficient models, such as “Permission, Limited Information, Specific Suggestions, and Intensive Therapy (PLISSIT)”, 31 and “Bring up, Explain, Tell, Time, Educate, Record” (BETTER)”, 32 which are counseling models to both assess and manage a patient's sexuality concerns.
According to our results, the male OB/GYNs self‐reported better competence in both discussing (tendency) and treating patients with sexual problems than the female OB/GYNs. In addition, the female OB/GYNs reported more barriers to bringing up sexual problems, especially those barriers concerning “lack of knowledge, experience, and effective treatment”. Our findings are in agreement with previous studies. 16 , 17 , 18 According to a meta‐analysis, the male OB/GYNs provided higher self‐ratings than the female OB/GYNs in a number of areas, such as training, knowledge, performance, confidence, and ability. 16 Furthermore, in a German study among urologists and urology residents, the male urologists self‐reported a higher level of confidence in taking care of patients with sexual‐related problems and self‐reported facing fewer barriers when addressing sexual health issues compared to female urologists. 17 Compared to female respondents, male respondents have also been found to self‐rate themselves as having a higher level of competence in fields other than medicine (eg computer skills, grammar, and mathematics). 16 Accordingly, these results may reflect the historical position of women in society compared to men, as the respondents may have unconsciously adopted these views. It is noteworthy that all these previous studies have evaluated self‐reported competence, not the actual competence. Thus, one important point would be to support the females' self‐confidence and self‐esteem. Another explanation might echo the fact that, during the past few years, the proportion of young female OB/GYN has grown in Finland, and only few young OB/GYNs are male; in our study, too, the male OB/GYNs were older and, therefore, probably more experienced, which could partly have affected our results concerning gender.
The older OB/GYNs were less likely to report barriers to bringing up the issue compared to the younger OB/GYNs. This is a novel finding, and an explanation for it could be that the OB/GYNs' experience, self‐confidence, and interest in the topic grow as their careers progress, lessening the barriers to addressing the topic with patients. The life experience of senior OB/GYNs may also make it easier for them to speak about sensitive topics. In some previous studies, female 13 , 14 and younger 13 physicians were found to be more likely to ask about sexual activity compared to male or older physicians. In these studies, however, the study aim differed from ours, as we studied the self‐rated competence and barriers, not the working methods.
Possible reasons why some OB/GYNs reported a poor level of competence in treating sexual problems include the ineffectiveness of the available treatments. Thus, in addition to improving education in sexual medicine for physicians, there is a general need for more research on women's sexual problems.
One of our study's merits was the questionnaire, which was previously used in different populations. 23 , 24 It contained a wide panel of questions and therefore provided feasible information about sexual medicine. In addition, the questionnaire was online, which permitted anonymous replies; thus, it was plausible that we received more honest answers compared to those obtained during personal interviews. The web‐based questionnaire was also a practical tool, allowing us to gather a large amount of information. Furthermore, the respondents could choose the place and time most convenient for them to fill out the survey. The questionnaire was designed not to progress if replies were missing, which guaranteed that the questionnaire was complete for every respondent.
We enrolled participants from The Finnish Society of Obstetrics and Gynecology. Although our response rate was quite low, it fell within the range reported in previous studies among OB/GYNs (18%–65.6%) 10 , 11 , 13 , 14 , 15 and was higher than that reported in a study among urologists (16%). 17 During the last few decades, the general interest in taking part in surveys has declined. 33 It is also noteworthy that there is a large group of retired OB/GYNs among the members of the Society, who do not practice and thus did not obviously reply to the survey. In addition, also physicians in other specialties can be members of The Finnish Society of Obstetrics and Gynecology; however, the preface of the questionnaire indicated that the survey was intended only for OB/GYN specialists and residents. In 2019, at the time of our survey, there were 680 specialists in OB/GYN in Finland under 65 years old. 22 In our study, there were 231 specialists in OB/GYN under 65 years old; accordingly, the respondents to our survey represented one third (34%) of the specialists in OB/GYN in Finland in 2019. Furthermore, majority, 72%, of our respondents reported to work in a hospital, which was somewhat higher percentage than estimated in the report conducted by the Finnish Medical Association (https://www.erikoisalani.fi/tulokset/16?emp=rt‐1). The fact that we sent an additional email to chief physicians of OB/GYN in hospitals in order to improve the response rate, plausibly led to a higher proportion of the OB/GYNs who were working in a hospital to respond to our survey. Nevertheless, 44% of them reported to practice also in the private sector, which is in concordance with the estimation of the Finnish Medical Association. However, we are fully aware that, with a higher response rate, our results would have been more reliable and easier to interpret and expand to apply to OB/GYNs in general.
The information about nonresponders was not available for comparison as we did not have any access to the actual register of the Society. Therefore, our results could be distorted by the fact that the OB/GYNs who were more interested in sexual medicine were keener to complete our survey. However, by assessing the information related to the daily number of patients with sexual health issues and by sorting the data in the analyses accordingly, we could evaluate that effect. Furthermore, the information regarding the participants' former education was retrospective, going back several decades for some of the respondents. Females were more strongly represented among our respondents; however, the gender ratio correlated with that of the OB/GYNs in Finland. 22 Thus, the findings regarding gender differences should be confirmed using larger samples. Last, our study included only Finnish OB/GYNs; therefore, our results might not be directly applicable to OB/GYNs in other countries. However, our respondents likely formed a consistent study group, as Finland is a racially and culturally homogenous country.
5. CONCLUSION
The Finnish OB/GYNs who participated in this study self‐reported a good competence in discussing sexual problems with their patients, whereas their competence in treating these problems was self‐evaluated as being poor. Several barriers to bringing up sexual problems emerged, including a lack of time during appointments. Our study clearly showed the great need for continuing education in sexual medicine, as most of the OB/GYNs considered their education to be insufficient and expressed a need for more education. Implementing sexual medicine as one of the learning objectives in the curriculum of the OB/GYN specialist degree could diminish the identified barriers in future.
AUTHOR CONTRIBUTIONS
AA the principal investigator and writer of the paper. PP‐K and KK are the leaders and co‐writers of the study. JG and S‐MM are the co‐investigators and co‐writers of the paper. MR and TV are the statisticians of the study.
FUNDING INFORMATION
This study was financially supported by Satasairaala Central Hospital (EVO grant, Anna Aromaa) and Turku University Hospital Foundation (Anna Aromaa).
CONFLICT OF INTEREST
None.
Aromaa A, Kero K, Grönlund J, et al. Let's talk about sexuality – A web‐based survey of self‐reported competence in sexual problems among obstetrician‐gynecologists in Finland. Acta Obstet Gynecol Scand. 2023;102:190‐199. doi: 10.1111/aogs.14492
REFERENCES
- 1. Fairchild PS, Haefner JK, Berger MB. Talk about sex: sexual history‐taking preferences among Urogynecology patients and general gynecology controls. Female Pelvic Med Reconstr Surg. 2016;22:297‐302. [DOI] [PubMed] [Google Scholar]
- 2. Flynn KE, Lin L, Bruner DW, et al. Sexual satisfaction and the importance of sexual health to quality of life throughout the life course of U.S. Adults. J Sex Med. 2017;13:1642‐1650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Berman L, Berman J, Felder S, et al. Seeking help for sexual function complaints: what gynecologists need to know about the female patient's experience. Fertil Steril. 2003;79:572‐576. [DOI] [PubMed] [Google Scholar]
- 4. Briedite I, Ancane G, Ancans A, Erts R. Insufficient assessment of sexual dysfunction: a problem in gynecological practice. Medicina (Kaunas). 2013;49:315‐320. [PubMed] [Google Scholar]
- 5. Lonnée‐Hoffmann RAM, Christensen SS, Hagemann CT. How do women want their gynaecologist to address sexual function? A cross‐sectional survey among outpatients. Reprod Female Child Health. 2022;1:11‐17. [Google Scholar]
- 6. Wendt E, Hildingh C, Lidell E, Westerståhl A, Baigi A, Marklund B. Young women's sexual health and their views on dialogue with health professionals. Acta Obstet Gynecol Scand. 2007;86:590‐595. [DOI] [PubMed] [Google Scholar]
- 7. Roos AM, Sultan AH, Thakar R. Sexual problems in the gynecology clinic: are we making a mountain out of a molehill? Int Urogynecol J. 2012;23:145‐152. [DOI] [PubMed] [Google Scholar]
- 8. American College of Obstetricians and Gynecologists' Committee on Practice Bulletins‐Gynecology . Female sexual dysfunction: ACOG practice bulletin clinical management guidelines for obstetrician‐gynecologists, number 213. Obstet Gynecol. 2019;134:e1‐e18. [DOI] [PubMed] [Google Scholar]
- 9. European Board and College of Obstetrics and Gynaecology . Contraception and sexual health‐standard 7. Standards of Care for Women's Health in Europe‐Gynaecology Services 2014. European Board and College of Obstetrics and Gynaecology; 2014. Accessed June 7, 2022. https://eeca.unfpa.org/sites/default/files/pub‐pdf/Standards%20of%20Care%20for%20Gynaecology%20Services.pdf [Google Scholar]
- 10. McCool ME, Apfelbacher C, Brandstetter S, Mottl M, Loss J. Diagnosing and treating female sexual dysfunction: a survey of the perspectives of obstetricians and gynaecologists. Sex Health. 2016;13:234‐240. [DOI] [PubMed] [Google Scholar]
- 11. Pauls RN, Kleeman SD, Segal JL, Silva WA, Goldenhar LM, Karram MM. Practice patterns of physician members of the American Urogynecologic Society regarding female sexual dysfunction: results of a national survey. Int Urogynecol J. 2005;16:460‐467. [DOI] [PubMed] [Google Scholar]
- 12. Bachmann G. Female sexuality and sexual dysfunction: are we stuck on the learning curve? J Sex Med. 2006;3:639‐645. [DOI] [PubMed] [Google Scholar]
- 13. Sobecki JN, Curlin FA, Rasinski KA, Lindau ST. What we Don't talk about when we Don't talk about sex: results of a National Survey of U.S. obstetrician/gynecologists. J Sex Med. 2012;9:1285‐1294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Wimberly YH, Hogben M, Moore‐Ruffin J, Moore SE, Fry‐Johnson Y. Sexual history‐taking among primary care physicians. J Natl Med Assoc. 2006;98:1924‐1929. [PMC free article] [PubMed] [Google Scholar]
- 15. Roos AM, Thakar R, Sultan AH, Scheer I. Female sexual dysfunction: are urogynecologists ready for it? Int Urogynecol J. 2009;20:89‐101. [DOI] [PubMed] [Google Scholar]
- 16. Farrow VA, Anderson B, Chescheir NC, Schulkin J. Sex differences among obstetrician‐gynecologists: a review of survey studies. Obstet Gynecol Surv. 2013;68:235‐253. [DOI] [PubMed] [Google Scholar]
- 17. Schloegl I, Köhn FM, Dinkel A, et al. Education in sexual medicine ‐ a nationwide study among German urologists/andrologists and urology residents. Andrologia. 2017;49:1‐11. [DOI] [PubMed] [Google Scholar]
- 18. Ariffin F, Chin KL, Ng C, Miskan M, Lee VK, Isa MR. Are medical students confident in taking a sexual history? An assessment on attitude and skills from an upper middle income country. BMC Res Notes. 2015;8:1‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Danielsson I, Sjöberg I, Stenlund H, Wikman M. Prevalence and incidence of prolonged and severe dyspareunia in women: results from a population study. Scand J Public Health. 2003;31:113‐118. [DOI] [PubMed] [Google Scholar]
- 20. Nicolosi A, Laumann EO, Glasser DB, Brock G, King R, Gingell C. Sexual activity, sexual disorders and associated help‐seeking behavior among mature adults in five Anglophone countries from the global survey of sexual attitudes and behaviors (GSSAB). J Sex Marital Ther. 2006;32:331‐342. [DOI] [PubMed] [Google Scholar]
- 21. Donaldson RL, Meana M. Early dyspareunia experience in young women: confusion, consequences, and help‐seeking barriers. J Sex Med. 2011;8:814‐823. [DOI] [PubMed] [Google Scholar]
- 22. The Finnish Medical Association, Valvira, National Supervisory Authority for Welfare and Health . Physicians in Finland: Statistics on physicians in 2019. Accessed January 18, 2022. https://www.laakariliitto.fi/site/assets/files/5256/sll_taskutilasto_en_220620.pdf
- 23. Alarcão V, Ribeiro S, Miranda FL, et al. General practitioners' knowledge, attitudes, beliefs, and practices in the management of sexual dysfunction‐results of the Portuguese SEXOS study. J Sex Med. 2012;9:2508‐2515. [DOI] [PubMed] [Google Scholar]
- 24. Manninen SM, Kero K, Perkonoja K, Vahlberg T, Polo‐Kantola P. General practitioners' self‐reported competence in the management of sexual health issues‐a web‐based questionnaire study from Finland. Scand J Prim Health Care. 2021;39:279‐287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Ross MW, Newstrom N, Coleman E. Teaching sexual history taking in health care using online technology: a PLISSIT‐plus zoom approach during the coronavirus disease 2019 shutdown. Sex Med. 2021;9:100290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Romero Otero J, García Gómez B, Medina Polo J, et al. The brief sexual symptom checklist as a screening tool for sex‐related problems in the primary care setting: focus on erectile dysfunction. Urol Int. 2018;101:98‐105. [DOI] [PubMed] [Google Scholar]
- 27. Kristufkova A, Pinto Da Costa M, Mintziori G, Vásquez JL, Aabakke AJM, Fode M. Sexual health during postgraduate training ‐ European survey across medical specialties. Sex Med. 2018;6:255‐262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Vieira TCSB, de Souza E, da Silva I, Torloni MR, Ribeiro MC, Nakamura MU. Dealing with female sexuality: training, attitude, and practice of obstetrics and gynecology residents from a developing country. J Sex Med. 2015;12:1154‐1157. [DOI] [PubMed] [Google Scholar]
- 29. Komlenac N, Siller H, Hochleitner M. Medical students indicate the need for increased sexuality education at an Austrian medical university. Sex Med. 2019;7:318‐325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Shindel AW, Baazeem A, Eardley I, Coleman E. Sexual health in undergraduate medical education: existing and future needs and platforms. J Sex Med. 2016;13:1013‐1026. [DOI] [PubMed] [Google Scholar]
- 31. Tuncer M, Oskay ÜY. Sexual counseling with the PLISSIT model: a systematic review. J Sex Marital Ther. 2022;48:309‐318. [DOI] [PubMed] [Google Scholar]
- 32. Quinn C, Happell B. Getting BETTER: breaking the ice and warming to the inclusion of sexuality in mental health nursing care. Int J Ment Health Nurs. 2012;21:154‐162. [DOI] [PubMed] [Google Scholar]
- 33. Tourangeau R. Survey research and societal change. Annu Rev Psychol. 2004;55:775‐801. [DOI] [PubMed] [Google Scholar]


