Abstract
Objective:
To analyze the outcomes of a cohort of children diagnosed with Mycoplasma pneumoniae encephalitis whose treatment regimens included intravenous immunoglobulin (IVIG).
Methods:
A retrospective study was performed at a single center between 2011 and 2016 of children diagnosed with Mycoplasma pneumoniae encephalitis whose acute treatment regimen included IVIG. Details of therapeutic interventions and the clinical course were retrieved from medical records via an institutionally approved protocol. The modified Rankin score was used to quantify outcomes.
Results:
Four children met inclusion criteria, 3 of whom had prodromal symptoms of infection lasting 5 to 7 days before onset of their neurologic symptoms. One patient presented with neurologic symptoms with no clinical prodrome. The initial treatment regimen included systemic corticosteroids, antibiotics, or both. IVIG was administered for a total dose of 2 g/kg divided over 2 to 4 days to all 4 children. All children showed clinical improvement after IVIG. The 3 children with prodromal symptoms showed immediate and dramatic clinical improvement after IVIG therapy.
Discussion:
The immediate response to immunomodulatory therapy in the patients with prodrome suggests that the neurologic syndrome may be caused at least in part by an autoimmune process. The child who did not respond to IVIG had no prodrome, and also had normal electroencephalographic (EEG) and brain magnetic resonance imaging (MRI) findings. These cases suggest that early administration of IVIG should be considered in patients suspected of having Mycoplasma encephalitis, particularly in those who have had prodromal symptoms.
Keywords: encephalopathy, acute disseminated encephalomyelitis, autoimmune, altered mental status
Encephalitis is the most frequent extrapulmonary manifestation of Mycoplasma pneumoniae infection in children, accounting for 5% to 10% of cases of childhood encephalitis. 1 -4 The pathophysiology is poorly understood. Potential disease mechanisms include direct infection of the central nervous system, neurotoxin-mediated injury, an aberrant host immune response to the original infection, and vasculitis or thromboembolic phenomena. 1,4,5 The multiplicity of possible mechanisms suggests that a range of therapeutic approaches should be considered. 6 Treatment of neurologic complications of M pneumoniae is controversial, and typically includes a combination of antibiotics, corticosteroids, and intravenous immunoglobulin (IVIG). 7
It is widely accepted that antibiotics play a key role in the management of any M pneumoniae infection or parainfectious syndrome. However, the role of immunosuppressive medications such as corticosteroids and immunomodulatory therapies such as IVIG has not been studied extensively. For IVIG, in particular, only single case reports of its use in the setting of M pneumoniae are available.
Methods
Patients and Study Design
The study was approved by the institutional review board at the University of Florida, and consisted of a single-center retrospective analysis of children with Mycoplasma pneumoniae encephalitis who were treated with IVIG. The primary objective was to assess the efficacy of IVIG treatment of Mycoplasma pneumoniae encephalitis. Secondary objectives were to assess the reasons for selecting IVIG and to evaluate the safety of this treatment in the setting of the specific disease. We performed a review of our electronic medical record using the search terms mycoplasma, encephalitis, steroid, and age 0-18 years from January 1, 2011, through December 31, 2016. Inclusion criteria were children (age <18 years) diagnosed with Mycoplasma pneumoniae encephalitis who received IVIG therapy. The diagnosis of Mycoplasma encephalitis was made by a consistent clinical neurologic syndrome, positive serum IgM or IgG titers for M pneumonia, and exclusion of other probable causes. Patients with underlying neuropsychiatric disorders and alternative diagnoses were excluded. We attempted to assemble a subgroup of control patients with Mycoplasma pneumoniae encephalitis who were treated with corticosteroids but not IVIG; however, all such patients were ultimately excluded from the analysis as a result of alternative diagnoses or prior neuropsychiatric disorders. Efficacy was determined by serial assessments of neurologic status and laboratory/imaging studies.
Data Collection
The following data were collected: demographics, details of IVIG treatment, all other treatments targeting Mycoplasma pneumoniae or encephalitis, comorbidities, relevant laboratory test results, and results of imaging studies. Neurologic status on admission, at IVIG initiation, and on discharge were recorded. Details regarding any adverse events were also collected. All data were entered into the Redcap database and summarized. 8
Results
Of 14 patients who were ascertained, 4 met inclusion criteria and were ultimately included in the analysis. A summary of key clinical data, including M pneumoniae titers, is presented in Table 1.
Table 1.
Patients’ Clinical Characteristics and Treatment Response.
| Patient 1 | Patient 2 | Patient 3 | Patient 4 | |
|---|---|---|---|---|
| Age, y/sex | 14/F | 7/M | 5/M | 11/F |
| Presenting symptom and duration (days) | Confusion (1) | Confusion and gait changes (1) | Confusion and seizure (7) | Confusion (2) |
| Prodromal symptom and duration (days) | Yes (7) |
Yes (11) |
Yes (5) |
None |
| Brain MRI | Abnormal (Figure 1) |
Normal | Normal | Normal |
| EEG | Normal | Slow background | Slow background | Normal |
| ESR | 33 | 42 | 22 | 41 |
| Serum WBC count, 103/mm3 | 18.6 | 7.5 | 7.2 | 11.5 |
| CSF studies | ||||
| WBC | 0 | 4 | 6 | 1 |
| RBC | 1 | 0 | 2 | 0 |
| Protein | 17 | 21 | 17 | 17 |
| Glucose | 58 | 55 | 62 | 63 |
| CSF Mycoplasma PCR | Not done | Negative | Negative | Negative |
| Serum Mycoplasma IgM titer, reference <0.76 U/L | 0.17 | 4.34 | 2.05 | 0.87 |
| Serum Mycoplasma IgG titer, reference <0.09 U/L | 0.23 | 0.84 | 1.46 | 0.72 |
| Anti-NMDA antibodies | Negative | Negative | Not done | Negative |
| Aquaporin 4 antibodies | Not done | Not done | Not done | Positive |
| Antibiotics (hospital days) |
Zithromax (2-6) |
Zithromax (1-5) |
Zithromax (8-12) |
None |
| Steroid dose (hospital days) |
Solumedrol 1 g/d (2-4) |
None | None | Prednisolone, from day 9, tapered over 4 wk) |
| IVIG 2 g/kg (hospital days) |
Yes (8-9) |
Yes (6-7) |
Yes (12-13) |
Yes (5-8) |
| Response to IVIG | Immediate | Immediate | Immediate | Slow |
Abbreviations: Anti-NMDA, anti–N-methyl-d-aspartate; CSF, cerebrospinal fluid; ESR, erythrocyte sedimentation rate; F, female; IVIG, intravenous immunoglobulin; M, male; MRI, magnetic resonance imaging; PCR, polymerase chain reaction; RBC, red blood cell; WBC, white blood cell.
Case 1
A 14-year-old previously healthy girl presented with a 3-day history of altered mental status. She was described as not acting herself, displaying disorientation, and attempting to elope from home. She had a 3-day history of cough and congestion 1 week before the onset of neurologic symptoms. Neurologic examination was notable for poor concentration, mildly impaired memory, and slowed speech. Brain magnetic resonance imaging (MRI) demonstrated 2 hyperintense lesions in the right frontal lobes. The larger lesion was located in the subcortical white matter of the right anterior frontal lobe at the midconvexity level and measured 10.4 × 9.1 × 9.9 mm (Figure 1). These lesions were hyperintense on fluid-attenuated inversion recovery and T2 sequences. The working diagnosis was acute disseminated encephalomyelitis (ADEM). The original differential diagnosis also included initial presentation of multiple sclerosis, neuromyelitis optica, and other demyelinating central nervous system diseases. The child was treated with a 5-day course of pulse methylprednisolone (1 g/d). Her mycoplasma titer came back elevated on day 6 of admission. She received empiric treatment with a 5-day course of azithromycin based on her results. Despite these treatments, the patient did not show perceptible improvement in her neurologic status. The patient developed agitation that was treated with intravenous lorazepam as needed. On hospital day 10, a course of IVIG (1 g/kg/d) was initiated for 2 days. At the completion of the second dose of IVIG, she experienced significant neurologic improvement and was subsequently discharged at hospital day 13. At the 6-month follow-up visit, she had completely recovered with respect to her neurologic status (modified Rankin Scale score of 0).
Figure 1.
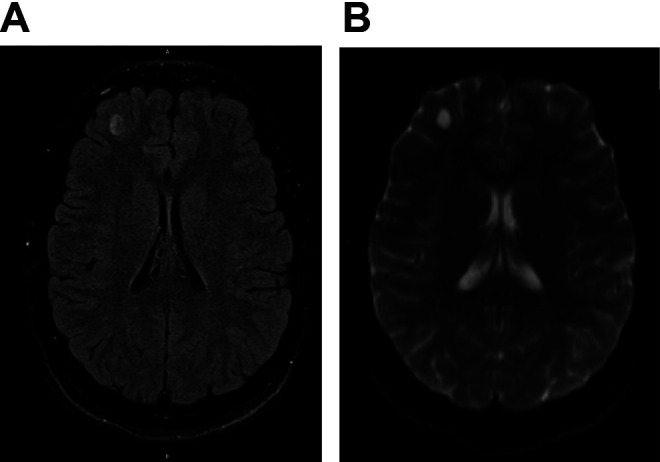
Brain magnetic resonance imaging (MRI) of case 1. (A) Fluid-attenuated inversion recovery MRI: nonrestricting, nonenhancing hyperintensities in the subcortical white matter of the right anterior frontal lobe. (B) T2 sequence: nonrestricting, nonenhancing hyperintensities in the subcortical white matter of the right anterior frontal lobe.
Case 2
A previously healthy 7-year-old boy presented with 1-day history of unsteady gait, diplopia, and confusion. This was preceded by 10 days’ history of intermittent fever, vomiting, headaches, and cough. Prior to admission, he was treated with amoxicillin, prednisolone, and albuterol for presumed pneumonia and asthma exacerbation. On admission, the patient was somnolent, but arousable to voice and followed one-step commands intermittently. He was unable to speak. Aside from his mental status, the other key neurologic examination findings were truncal, gait, and distal ataxia. He received a 5-day course of azithromycin for possible atypical bacterial infection. He also received intravenous ceftriaxone and intravenous acyclovir for possible bacterial and viral encephalitis. During his admission, he remained somnolent and ataxic. Further investigations demonstrated elevated serum mycoplasma IgM and IgG titers, accompanied by negative cerebrospinal fluid M pneumoniae polymerase chain reaction. Anti-NMDA receptor antibodies and other infectious studies were negative.
IVIG 1 g/kg was administered once daily on hospital days 5 and 6. By hospital day 6, the patient started to converse. On day 7, he was more awake, following commands and able to respond appropriately to questions. His gait started to improve as well and he continued to improve slowly. On hospital day 22, the patient was discharged with arrangement for outpatient rehabilitation due to moderate ataxia requiring assistance during ambulation with a Modified Rankin Scale score of 3. The patient was subsequently lost to follow-up.
Case 3
A 5-year-old previously healthy boy was admitted to the hospital after he presented with 5 days of fever and headache that culminated in a 1-day history of altered mental status (irritability and word finding difficulty), accompanied by seizures. On neurologic examination, he was noted to have fluctuating confusion with no focal motor or sensory deficits. He was treated with 2 days of empiric intravenous ceftriaxone and discharged home. At discharge, he was noted to be improving but he was not back to his baseline mental status.
A day after discharge, he was readmitted as a result of the occurrence of another seizure that had a focal semiology. A repeat electroencephalogram (EEG) showed generalized background slowing. Oxcarbazepine therapy was initiated. During this second hospital stay, he continued to exhibit fluctuating change in mental status with no EEG correlates. Repeat cerebrospinal fluid analysis was unremarkable. He was then found to have elevated mycoplasma IgM and IgG titers. On the fourth day of the second hospital admission, IVIG (1 g/kg × 2) and azithromycin therapies were started. After the first dose of IVIG, his mental status improved. On discharge (hospital day 6) he was alert, conversational with no focal neurologic deficit.
On follow-up outpatient evaluation, he was noted to be stable. About a month after discharge, he returned to school and has been reported to be functioning at his prior academic level (modified Rankin Scale score of 0). He was weaned off oxcarbazepine after 2 months.
Case 4
An 11-year-old girl presented with a 2-day history of confusion, nonsensical speech, and disorientation with no prodromal symptoms of infection. Her medical history was only notable for a single prior episode suspicious for seizure. On neurologic examination, she was disoriented to time and place with decreased concentration. No other focal neurologic findings were noted. Cerebrospinal fluid studies were unremarkable. She was found to have elevated mycoplasma IgM and IgG titers. Because of concern for possible autoimmune encephalopathy, she received IVIG 0.5/kg/d from hospital days 5 through 8. The patient’s neurologic status improved mildly, and she was discharged home on hospital day 8. She had residual difficulty with concentration but was able to carry out most of her activities of daily living (modified Rankin Scale score of 1). At the 6-month follow-up visit, she had made a complete neurologic recovery with a modified Rankin Scale score of 0.
Clinical Course
The 4 children all experienced improvement of their neurologic status after administration of IVIG. For the first 3 children, the neurologic improvement was temporally related to the administration of IVIG; the same 3 patients had prodromal symptoms of infection. Only 1 patient had an abnormal brain MRI with lesions that raised the possibility of acute disseminated encephalomyelitis but were not classic for this diagnosis. The only patient who did not respond promptly to IVIG therapy was also the only one without prodromal symptoms of infection. This patient had unremarkable EEG, brain MRI, and cerebrospinal fluid studies. Further testing later revealed positive aquaporin 4 antibodies in addition to the elevated Mycoplasma titers (see Table 1).
Discussion
Two distinct clinical patterns have been described for Mycoplasma pneumoniae encephalitis, the first associated with a prolonged prodrome (≥7 days) and the other associated with a shorter (<7 days) or absent prodrome before the onset of neurologic symptoms. Those with the prolonged prodrome had higher rates of respiratory symptoms, chest radiograph abnormalities, elevated IgM antibody titers in peripheral blood samples, and detection of M pneumoniae in the respiratory tract. An indirect pathogenetic mechanism appears more likely for those with a prolonged prodrome exhibiting robust respiratory inflammation as evidenced by higher rates of respiratory symptoms and chest radiograph abnormalities, the development of an IgM response in peripheral blood, and detection of the organism only in the respiratory tract. The association of a brief prodrome with detection of M pneumoniae in the cerebrospinal fluid, but not the respiratory tract, and the lack of an IgM response in peripheral blood suggests rapid spread to the central nervous system prior to significant organism replication in the respiratory tract. The lack of an IgM response in those with a brief prodrome is not likely a reflection of early sampling. These findings help support the hypothesis of 2 distinct neurologic disease forms, one of early onset associated with direct infection of the central nervous system and one of late onset mediated by indirect, likely immunologically mediated, mechanisms. 9
At present, immunomodulatory therapies for Mycoplasma pneumoniae encephalitis are used in addition to conventional antimicrobial therapy and a short course of corticosteroids. However, there are no controlled studies that examine the comparative efficacy of these therapies.
An immunologic basis for the form of Mycoplasma pneumoniae encephalitis associated with extended prodromal symptoms has been suggested. 9 The positive aquaporin 4 antibody in the nonresponder patient raises the intriguing possibility that the Mycoplasma pneumoniae triggered an autoimmune response. A single-center cohort study from Australia described patients diagnosed with Mycoplasma pneumoniae encephalitis who were also found to have elevated antibody titers to NMDA receptors and voltage-gated potassium channels. 10 The lack of direct evidence for M pneumoniae infection in cerebrospinal fluid by culture or polymerase chain reaction suggests a possible autoimmune process. 11 Prior reports of neurologic improvement after IVIG therapy for such patients with concurrent encephalitis and pneumonia associated with M pneumoniae infection are limited to single case reports. 6,11 More extensive studies are needed before IVIG can be definitely recommended in this setting. However, our cases suggest that early administration of IVIG should be considered in patients suspected of having Mycoplasma pneumonia encephalitis, particularly in those who have had prodromal symptoms of infection for about a week or longer and are not responsive to other therapies.
Footnotes
Author Contributions: MD conceptualized and designed study, designed and collected data, drafted manuscript. PK, JS, and RL reviewed study design, reviewed and analyzed data, revised manuscript. SB collected and interpreted radiographic data, revised manuscript. SG mentored Dr. Mebratu Daba, conceptualized study design, reviewed and interpreted data, drafted and revised manuscript.
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Redcap database funded through Clinical and Translational Science Institute (CTSI) grant support (NIH National Center for Advancing Translational Sciences [NCATS] grant UL1 TR000064).
ORCID iD: Suman Ghosh  https://orcid.org/0000-0003-1036-3887
https://orcid.org/0000-0003-1036-3887
Ethical Approval: The study was approved by the institutional review board at the University of Florida (IRB 201700565).
References
- 1. Tsiodras S, Kelesidis I, Kelesidis T, Stamboulis E, Giamarellou H. Central nervous system manifestations of Mycoplasma pneumoniae infections. J Infect. 2005;51(5):343–354. [DOI] [PubMed] [Google Scholar]
- 2. Kammer J, Ziesing S, Davila LA, et al. Neurological manifestations of Mycoplasma pneumoniae infection in hospitalized children and their long-term follow-up. Neuropediatrics. 2016;47(5):308–317. [DOI] [PubMed] [Google Scholar]
- 3. Bitnun A, Ford-Jones EL, Petric M, et al. Acute childhood encephalitis and Mycoplasma pneumoniae. Clin Infect Dis. 2001;32(12):1674–1684. [DOI] [PubMed] [Google Scholar]
- 4. Narita M. Classification of extrapulmonary manifestations due to Mycoplasma pneumoniae infection on the basis of possible pathogenesis. Front Microbiol. 2016;7:23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. He J, Liu M, Ye Z, et al. Insights into the pathogenesis of Mycoplasma pneumoniae (review). Mol Med Rep. 2016;14(5):4030–4036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Chambert-Loir C, Ouachee M, Collins K, Evrard P, Servais L. Immediate relief of Mycoplasma pneumoniae encephalitis symptoms after intravenous immunoglobulin. Pediatr Neurol. 2009;41(5):375–377. [DOI] [PubMed] [Google Scholar]
- 7. Yimenicioglu S, Yakut A, Ekici A, Bora Carman K, Cagrı Dinleyici E. Mycoplasma pneumoniae infection with neurologic complications. Iran J Pediatr. 2014;24(5):647–651. [PMC free article] [PubMed] [Google Scholar]
- 8. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Al-Zaidy SA, MacGregor D, Mahant S, Richardson SE, Bitnun A. Neurological complications of PCR-proven M. pneumoniae infections in children: prodromal illness duration may reflect pathogenetic mechanism. Clin Infect Dis. 2015;61(7):1092–1098. [DOI] [PubMed] [Google Scholar]
- 10. Pillai SC, Hacohen Y, Tantsis E, et al. Infectious and autoantibody-associated encephalitis: clinical features and long-term outcome. Pediatrics. 2015;135(4):e974–e984. [DOI] [PubMed] [Google Scholar]
- 11. Sakoulas G. Brainstem and striatal encephalitis complicating Mycoplasma pneumoniae pneumonia: possible benefit of intravenous immunoglobulin. Pediatr Infect Dis J. 2001;20(5):543–545. [DOI] [PubMed] [Google Scholar]


