Abstract
Purpose of Review
The goal of this narrative review is to educate clinicians regarding the foundational concepts, efficacy, and future directions of therapeutic vaccines for human papillomavirus (HPV)–mediated cancers.
Recent Findings
Therapeutic HPV vaccines deliver tumor antigens to stimulate an immune response to eliminate tumor cells. Vaccine antigen delivery platforms are diverse and include DNA, RNA, peptides, proteins, viral vectors, microbial vectors, and antigen-presenting cells. Randomized, controlled trials have demonstrated that therapeutic HPV vaccines are efficacious in patients with cervical intraepithelial neoplasia. In patients with HPV-mediated malignancies, evidence of efficacy is limited. However, numerous ongoing studies evaluating updated therapeutic HPV vaccines in combination with immune checkpoint inhibition and other therapies exhibit significant promise.
Summary
Therapeutic vaccines for HPV-mediated malignancies retain a strong biological rationale, despite their limited efficacy to date. Investigators anticipate they will be most effectively used in combination with other regimens, such as immune checkpoint inhibition.
Keywords: Human papillomavirus, Cancer, Therapeutic vaccine
Introduction
Human papillomavirus (HPV)–mediated cancers are common, and result in substantial morbidity and mortality. HPV causes 690,000 cancers of the cervix, oropharynx, anus, vulva, vagina, and penis annually, accounting for 5% of all cancers worldwide [1, 2]. Globally, cervical cancer is the most prevalent, and also the most fatal, HPV-mediated cancer [3]. Over 310,000 patients die of this disease each year [3]. In the USA, HPV-mediated oropharyngeal cancer (HPV + OPC) is the most common HPV-mediated cancer. Here, more than one-third of HPV + OPC patients have stage II–IV disease with 4-year overall survival (OS) rates ranging from 20 to 77% [4].
Treatment of HPV-mediated cancers is also toxic. In the USA, 85% of HPV + OPC patients require multimodal therapy involving primary surgery ± radiation ± chemotherapy or primary radiation ± chemotherapy[4]. Many develop subsequent xerostomia and dysphagia [5], and a minority experience long-term gastrostomy-tube dependence, osteoradionecrosis, and even treatment-related death [6–8].
Therefore, novel treatment options are required for patients with HPV-mediated malignancies. In the HPV + OPC population, deintensification trials to reduce patient morbidity continue to apply bi- and tri-modality treatment strategies, albeit at reduced doses [9–11]. Targeted biologic therapies, such as cetuximab, have exhibited limited efficacy in HPV-mediated cancers to date [12, 13]. Primary head and neck cancer (HNC) patients who received definitive treatment intensification with immune checkpoint inhibition did not experience improved oncologic outcomes [14]. In patients with recurrent or metastatic cervical cancer and HNC, immune checkpoint inhibitors (ICIs) only modestly prolonged overall or progression-free survival and only confer durable responses in a minority of patients [15–17].
Therapeutic vaccination is an experimental therapy for patients with HPV-mediated malignancies, and has the potential to help close this gap in care. Although early results have been underwhelming [18], promising trials pairing vaccines with novel adjuvants, other vaccines, ICIs, or other therapies are currently underway.
This narrative review focuses exclusively on therapeutic vaccines that leverage HPV-specific antigens, rather than HPV-agnostic therapeutic vaccines. This study has two primary objectives. First, we aimed to “prime” clinicians regarding foundational concepts in therapeutic cancer vaccination. Second, we aimed to recapitulate the evidence regarding the clinical efficacy of therapeutic vaccination in patients with HPV-mediated (pre)malignancies. As the target readers are clinicians, preclinical trials and trials evaluating immune response data alone are not discussed.
Foundational Concepts of Therapeutic Cancer Vaccines
Definition
In the context of cancer, therapeutic vaccination is a type of immunotherapy that delivers tumor antigens to the immune system to stimulate an immune response to eliminate tumor cells.
Within the broad category of cancer immunotherapy, therapeutic vaccination is distinguished by the nature in which it produces an immune response—via tumor antigen. This type of immunotherapy is distinct from others, including the following:
Oncolytic virus therapy (e.g., talimogene laherparepvec [T-vec]),
Targeted biologic therapy (e.g., cetuximab: IgG1 epidermal growth factor receptor [EGFR] monoclonal antibody),
ICIs (e.g., monoclonal antibodies to PD-1, PD-L1, and CTLA-4),
Cytokine therapies (e.g., interleukin-2 [IL-2], interferon-α [IFN-α]), and
Adoptive cell transfer (e.g., T cell receptor [TCR]–engineered T cell therapy) [19, 20].
The definition of therapeutic vaccination is further clarified by discussing its similarities and differences with other selected immunotherapies. Neither T-vec, bacillus Calmette-Guérin (BCG), nor adoptive cell transfer (ACT) therapy directly uses tumor antigen to induce an immune response. Talimogene laherparepvec is a recombinant, oncolytic herpes simplex virus [HSV]-1 encoding GM-CSF approved for local intratumoral treatment of unresectable, recurrent, metastatic melanoma [21, 22]. The therapy indirectly releases tumor antigens through viral-mediated tumor oncolysis. BCG is an attenuated, live strain of Mycobacterium bovis that is approved for treatment and prophylaxis of urinary bladder carcinoma in situ (CIS) and recurrent early-stage papillary tumors after transurethral resection [23]. The BCG live cancer vaccine stimulates the release of chemokines and cytokines, which activate an unspecified adaptive immune response [23]. Although controversial, we argue this is not a therapeutic cancer vaccine, as traditionally defined, because the vaccine does not include known, tumor-specific antigens.
In adoptive cell transfer (ACT) therapy, immune effector cells are activated independent of antigen delivery. Examples of ACT therapy include tumor-infiltrating lymphocyte (TIL)–based ACT therapy, and TCR-engineered T cell therapy, of which chimeric antigen receptor (CAR) T cell therapy is a type [19, 20]. CAR T cell therapy involves leukapheresis, genetically engineering autologous T cells to express CARs ex vivo, expansion, and reinfusion into patients. CARs bypass the MHC system and engraft T cells with predefined specificity towards a target antigen, facilitating improved affinity for, and elimination of, tumor cells [19, 24]. ACT therapy targeting HPV-16 E7 is promising. In a first-in-human, phase I trial in 12 patients with metastatic HPV16 + cancers after failed systemic treatment, the overall response rate was 50% [25].
Key Components and Considerations
Successful therapeutic vaccines consist of effective tumor antigens, antigen delivery platforms, adjuvant, and delivery vehicles [26]. We address the former three topics in this review. Many other features of these vaccines must be considered, and these are briefly discussed below.
Tumor Antigens
There are two primary categories of tumor antigens: tumor-associated antigens (TAAs) and tumor-specific antigens (TSAs) [27]. TAAs are self-antigens that are abnormally expressed by the tumor [27]. Since they are not entirely tumor-specific, TAAs are subject to tolerance mechanisms which must be overcome to elicit an immune response [27]. Hence, vaccines targeting TAAs also risk induction of autoimmunity. Cancer testis antigen is a quintessential TAA. It is overexpressed in a wide range of tumors, yet among “self” cells, it is only expressed by male germ cells [28]. These cells do not express major histocompatibility complex (MHC) class I molecules and therefore cannot present antigen to T cells [28]. TSAs, on the other hand, are entirely specific to the tumor and not subject to immune tolerance. Oncoviral antigens and neoantigens (generated by mutations in tumor DNA) are examples of TSAs [27, 29].
Antigen Delivery Platforms
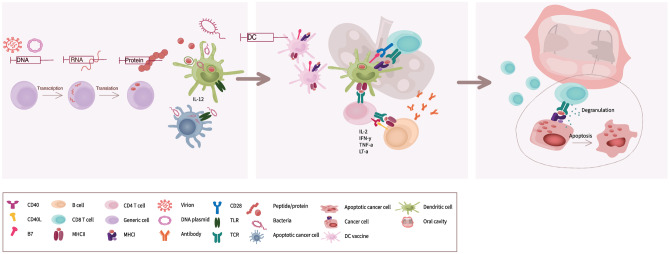
There are three broad categories of antigen delivery platforms: molecular, microbial, and cellular. Molecular antigen delivery platforms include small nucleic acids (e.g., DNA, RNA), and peptides or proteins (Fig. 1). Microbial vectors include viruses and, less commonly, bacterial vectors. In addition to expressing tumor antigen(s), microbial vectors themselves are often immunogenic (Fig. 1), thereby leveraging both adaptive and innate immunity. In some cases, microbial vectors are oncolytic.
Fig. 1.
The intended immune response to therapeutic vaccination for HPV-mediated malignancies. The primary goal of therapeutic vaccination for cancers of HPV etiology is to initiate a cytotoxic T cell response against HPV antigens expressed on tumor cells. DC-based vaccines introduce licensed DCs that have undergone licensing and been loaded with antigen ex vivo (center panel). Peptide- or protein-based vaccines introduce peptide/protein in a form for uptake by endogenous DCs, such as a virus-like particles or liposomal carriers (left panel). DNA- and RNA-based vaccines introduce nucleic acids which are then transcribed and translated by recipient cells to produce HPV peptides or proteins (left panel). The nucleic acids can be delivered via DNA plasmids, virus-like particles, viral vectors, or bacterial vectors. The targeted cell type and mechanism of cellular entry vary with the specific vaccine formulation and route of administration. For example, DNA plasmids may be injected intramuscularly, and electroporation can be used to enhance cellular uptake. Viral vectors can enter cells by viral infection pathways. All of these will be taken up by phagocytic cells, but bacterial vectors typically target phagocytes as the cell type in which the antigenic proteins will be produced. Left panel: Antigenic peptides or proteins or DNA/RNA encoding antigenic peptides/proteins are introduced in a formulation and via a route of administration designed to activate the innate immune system and trigger DC licensing. Licensed DCs will upregulate MHCI expression, present antigenic peptides, upregulate costimulatory molecules (B7), and migrate to secondary lymphoid organs, carrying antigen with them. Center panel: In the secondary lymphoid tissues, DCs may interact with CD4 + T helper cells, resulting in a further increase in costimulatory molecule expression. CD4 + T helper cells may also provide T cell help to B cells, enhancing B cell effector functions. Licensed DCs will interact with naïve CD8 + T cells; those with appropriate T cell receptor specificity will be activated. Activated CD8 + T cells will proliferate, acquire their effector function of cytotoxicity, exit the secondary lymphoid tissues, and migrate to sites of inflammation, including tumors. Right panel: Cytotoxic T cells will infiltrate the tumor and kill tumor cells expressing their cognate antigen by releasing cytotoxic molecules that induce apoptosis
Cellular vaccines use whole cells and involve the delivery of tumor antigens to activate an immune response. These primarily consist of two categories: whole tumor cell vaccines and antigen-presenting cell (APC)–based vaccines [27]. In the whole tumor cell vaccine approach, inactive, autologous, or allogeneic tumor cells are co-administered with adjuvant [30]. Given the approach’s limited success in phase III trials, enthusiasm for whole tumor cell vaccination has waned [27, 30].
APC-based vaccination represents the final step in (processed) antigen delivery to immune effector cells, and includes dendritic cell (DC)– and peripheral blood mononuclear cell (PBMC)–based vaccines. A common DC-based vaccine approach involves pulsing autologous DCs ex vivo with cell lysates or tumor antigens and reintroducing the licensed DCs into the patient (Fig. 1). Peripheral blood mononuclear cell (PBMC)–based vaccines are less commonly described, albeit prevalent, APC-based vaccines [31–33]. Some PBMC-based vaccines are mistakenly considered to be DC-based vaccines [31–33]. PBMCs are harvested by leukapheresis and consist of lymphocytes (i.e., T cells, B cells, natural killer cells) and monocytes, which differentiate into macrophages and dendritic cells. This approach leverages the antigen-presenting capacity of a broader spectrum of APCs, including B cells and other monocytes. It bypasses the process of DC isolation, which requires differentiation and maturation from monocytes in PBMCs [34]. Hence, proponents argue it is a simpler, less expensive approach compared to DC-based vaccines [31, 35].
Adjuvant
Therapeutic vaccines often co-administer adjuvant with tumor antigen(s) in order to enhance the “magnitude, breadth, and durability” of the immune response to the antigen(s) [36]. Adjuvants also guide the type(s) of innate, humoral, and cell-mediated immune response to be elicited [37]. For therapeutic cancer vaccines, the ideal adjuvant overcomes the tumor’s immunosuppressive microenvironment and elicits an effective, tumor-specific, CD8 + cytotoxic T cell response.
Adjuvant classification systems are heterogeneous, in part because the mechanisms of their immunogenicity are not fully understood [38]. One system classifies adjuvants on a continuum according to their depot/delivery and immunostimulatory capabilities [39]. Many newer adjuvants possess both traits. A broad definition of the term “adjuvant” is applied in this review and includes components of vaccines that are genetically engineered to express cytokines, chemokines, and costimulatory molecules.
In their landmark study, Singh and Hagan assign adjuvants to the following categories: mineral salts (e.g., aluminum salts), immunostimulators (e.g., cytokines, bacterial products such as lipopolysaccharide [LPS]), lipid particles (e.g., emulsions), microparticulates, and mucosal adjuvants [38]. Aluminum salts and water–oil emulsions are among the most commonly used vaccine adjuvants [36, 39]. The former preferentially induce humoral- over cell-mediated immunity and are used in the bivalent, quadrivalent, and nonavalent prophylactic HPV vaccines. Montanide ISA-51 is a combination of a water–oil emulsion and the surfactant mannide monooleate, and has been incorporated into several therapeutic HPV vaccines [39].
Coffman et al. emphasize the importance of adjuvant selection to shape the type of immune response desired [37]. They classify adjuvants into empirically derived adjuvants (e.g., aluminum salts, Freund’s adjuvant) and adjuvants targeting pattern recognition receptors (PRRs; e.g., toll-like receptor 3 [TLR3] ligands) [37]. Regardless of classification, each adjuvant directs a unique humoral-, cell-mediated, or mixed humoral- and cell-mediated immune response. For example, polyinosinic-polycytidylic acid (poly-IC) activates TLR3 and melanoma differentiation–associated protein 5 (MDA5), which collectively stimulate an antibody, Th1, and CD8 + T cell immune response [37]. In order to further optimize vaccine efficacy, Coffman et al. recommend combining empirically derived adjuvants and PRR ligands to appropriately guide a desired immune response [37].
Other Therapeutic Vaccine Considerations
Investigators and clinicians must consider many other factors in selecting a candidate therapeutic cancer vaccine. The route of therapeutic vaccine administration, dose, and dosing regimen schedule must be optimized [29]. Most vaccines apply a homologous prime-boost approach, where administration of a prime dose is followed by additional boost doses of the same vaccine, usually over a matter of weeks. The time to manufacture the vaccine is also a factor. This is shorter for small nucleic acid–based vaccines and longer for viral vectored and personalized vaccines [29].
Precedent for Therapeutic Cancer Vaccines
Although enthusiasm for therapeutic cancer vaccines is robust, particularly in combination with other therapies, there is limited precedent for the practice. The Federal Drug Administration (FDA) has only approved one therapeutic cancer vaccine, sipuleucel-T. Sipuleucel-T is an autologous PBMC-based vaccine (enriched for a DC fraction) approved for use in asymptomatic or minimally symptomatic metastatic, castration-resistant prostate cancer patients. PBMCs are pulsed ex vivo with the recombinant protein granulocyte–macrophage colony-stimulating factor (GM-CSF) fused to prostatic-acid phosphatase (PAP, which is expressed by prostate cancer cells). In a landmark phase III trial, sipuleucel-T significantly, albeit modestly, improved patient overall survival compared to placebo (median: 4.1 months, 25.8 months versus 21.7 months) [40].
Foundational Concepts in Therapeutic Vaccination for HPV-Mediated Cancers
HPV Epidemiology
HPV16 and HPV18 are the most common causes of HPV-mediated cancers. Among the over 200 known types of HPV, 13 in the Alphapapillomavirus genus are high-risk, or oncogenic [41, 42]. These include HPV types 16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, and 66 [41]. Several other types have been defined as “possibly” carcinogenic [43]. Cervical cancer accounts for 87% of the 610,000 HPV-mediated cancers worldwide and 57% and 18% of cervical cancers are attributable to HPV16 and HPV18, respectively [44]. HPV16 causes 82% of HPV-associated head and neck squamous cell carcinomas [45]. In the USA, HPV16 and HPV18 account for 86% of HPV-mediated OPCs [46].
High-Risk HPV Life Cycle and Pathogenesis
A cursory understanding of the HPV life cycle and pathogenesis provides a basis for understanding the (onco)viral antigen targets of HPV vaccines. A microwound in the epithelium exposing the basal lamina is thought to be a necessary precursor to HPV infection [47]. Virus particles consisting of viral DNA and two capsid proteins (L1, L2) access the basal lamina [47]. Basal epithelial cells internalize the virus, and the viral genome is transferred to the cell nucleus. These infected basal epithelial cells constitute a perpetual reservoir of HPV infection [47]. They divide and generate HPV-infected daughter cells which then migrate towards the cell surface.
The viral life cycle tracks with stages of epithelial cell migration. “Early” in its life cycle, the viral genome expresses six early, or “E,” proteins. E1, E2, E4, E5, E6, and E7 facilitate genome maintenance, cell proliferation, and genome amplification in the lower and middle epithelial layers [47]. In high-risk HPV types, E6 and E7 are oncoproteins which play a major role in determining the disease phenotype [47]. “Late” in its life cycle, the viral genome expresses two late, or “L,” proteins. L1 and L2 constitute the major and minor capsid proteins, respectively. Along with E4, they facilitate virus assembly and release in the upper epithelial layers [47].
Tumor-Specific Antigens: Prophylactic and Therapeutic HPV Vaccine Targets
L1 is the target of current prophylactic HPV vaccines and L1 and L2 serve as potential targets of next-generation vaccines [48]. L1 major capsid proteins self-assemble into highly immunogenic, inert, L1 virus-like particles (VLPs) that resemble the conformation of authentic virions [49–51]. For example, the nonavalent vaccine Gardasil consists of VLPs made of L1 from HPV types 6, 11, 18, 31, 33, 45, 52, and 58, along with the adjuvant, amorphous aluminum hydroxyphosphate sulfate (AAHS). These vaccines generate a robust, durable, neutralizing IgG antibody response and are extremely effective at protecting patients against new HPV infections and corollary development of HPV-mediated cancers [51–53]. According to high-quality phase III trial data, they are not effective against prevalent infections and do not accelerate their clearance [54]. This is presumably because L1 proteins are not expressed early in the viral life cycle; hence, the reservoir of infected basal epithelial cells remains unaffected by the vaccine-induced immune response.
To date, therapeutic vaccines for HPV-mediated tumors have largely targeted E6- and/or E7-based antigens of the HPV16 and/or HPV18 genotypes. The modest efficacy of these vaccines has prompted investigators to consider targeting additional tumor antigens (e.g., E1, E2), and other high-risk HPV genotypes. For example, researchers are investigating the efficacy of a viral vector vaccine expressing conserved regions from all six early proteins from five high-risk genotypes [55].
Foundational Concepts in Therapeutic Cancer Vaccine Immunology
Effective therapeutic cancer vaccines leverage both innate and adaptive immunity. Innate immunity is a rapid, antigen-independent, and nonspecific response to a foreign substance that lacks immunologic memory. A key feature of innate immunity is its ability to recognize conserved features of pathogens using host pattern recognition receptors (PRRs). As described above, TLR ligands are a type of vaccine adjuvant that bind PRRs, activate innate immunity, and polarize the adaptive immune response towards cellular or humoral immunity.
Adaptive immunity is an adaptable, antigen-specific response to a foreign substance (e.g., cancer) that involves immunological memory and is mediated by T and B cells. Adaptive immunity is comprised of cell-mediated immunity and humoral immunity. Therapeutic cancer vaccines primarily aim to kill cancer cells by stimulating cellular immunity. This involves antigen-mediated activation of cytotoxic T cells (CTLs), natural killer (NK) cells, macrophages, and release of cytokines and chemokines. The activated CTLs and NK cells then have the capacity to directly kill tumor cells.
Humoral immunity is an antibody-mediated immune response and plays a secondary role in therapeutic cancer vaccination. Tumor antigen is an antibody generator. Antibodies may bind to tumor antigen and (partially) inactivate tumor cells by blocking their ability to bind host cell receptors, promote tumor cell ingestion and destruction by phagocytes, and activate the complement cascade.
In Fig. 1, we describe the immune response to the spectrum of therapeutic HPV-mediated cancer vaccines.
Therapeutic HPV-Mediated Cancer Vaccine Trial Results: from Past to Present
Overview
To identify relevant manuscripts and clinical trials, we searched clinicaltrials.gov and pubmed.gov, and performed a bibliographic review in November 2021. A systematic, comprehensive literature review was not undertaken for this study; therefore, certain vaccines may not have received due representation.
We describe representative, early vaccines in Appendix Table 3. Next, we review evidence of vaccine efficacy in populations with pre-malignant and malignant disease, respectively (Appendix Table 4; Table 1). Finally, we discuss recently completed, or ongoing, therapeutic vaccine trials evaluating common and uncommon vaccines, respectively (Table 2; Appendix Table 5). Considering the intended reader, we only discuss trials with clinical results. Throughout the below content, we highlight at least one vaccine from each major antigen delivery system category.
Table 3.
Selected early landmark therapeutic vaccine trials for HPV-mediated premalignancies and malignancies
| Antigen delivery system category, vaccine, and PMID identifier | Year | Journal | No. of citations* | Phase | N | Eligibility/enrolled | Adjuvant | Clinical and other notable outcomes |
|---|---|---|---|---|---|---|---|---|
| Small nucleic acids GX-188E ([DNA plasmid encoding HPV16 and 18 E6/E7 fusion protein] + FLT3L [Fms-like tyrosine kinase-3 ligand]) | ||||||||
| 25354725 [59] | 2014 | Nat Commun | 92 | I | 9 | CIN3 | IL-12# | 7/9 with complete lesion regression and viral clearance within 36 weeks of follow-up |
| Viral vector TA-HPV (tissue-antigen-HPV: recombinant vaccinia virus expressing HPV16/18 + E6/7 proteins) | ||||||||
| 8684105 [56•] | 1996 | Lancet | 111 | I/II | 8 | Invasive CC | - | 2/8 disease-free at 15 and 21 months, respectively |
| Bacterial vector ADXS11-001 (ADXS-HPV; axalimogene filolisbac [AXAL]; Lm-LLO-E7; live attenuated Listeria monocytogenes encoding HPV 16 E7 and tLLO) | ||||||||
| 19389451 [60] | 2009 | Vaccine | 145 | I | 15 | A/R CC | tLLO# | Flu-like syndrome in 100% patients, grade 3 AEs in 40% of patients; no grade 4/5 AEs; 1/15 with partial response |
| Peptides ISA101 (HPV16 E6/E7-SLPs [nine E6 SLPs, four E7 SLPs) | ||||||||
| 19890126 [58•] | 2009 | N Engl J Med | 406 | II | 22 | HPV16 + VIN3 | Montanide® ISA-51 | Objective clinical response in 79% of patients (n = 15/19) including complete response in 47% (n = 9/19) at 12 months |
| Protein(s) TA-CIN (tissue-antigen CIN; HPV16 L2/E6/E7 fusion protein) | ||||||||
| 20234368 [57] | 2010 | Br J Cancer | 98 | II | 19 | VIN2/3 | Imiquimod 5% cream | Complete regression of VIN in 58% (n = 11/19) patients at 20-weeks |
*Citation number per pubmed.gov, as of 09/4/2022
Table 4.
Results of selected randomized, double-blind, placebo-controlled trials evaluating therapeutic vaccines for HPV-mediated premalignancies
| Antigen delivery system category, vaccine, and PMID identifier | Phase | Sample size, distribution, outcome analysis | Dose, type (site), schedule (wks) | Eligibility/enrolled | Adjuvant | Primary and/or secondary clinical (or other) outcomes |
|---|---|---|---|---|---|---|
| Small nucleic acids | ||||||
| VGX-3100 [DNA plasmid encoding HPV16 and 18 E6/E7 genes] with electroporation | ||||||
| 26386540 [61••] | IIb |
VGX-3100: ITT: 125; PP: 107 Placebo: ITT: 42; PP: 36 |
6 mgs; 0, 4, 12; IM + EP | HPV16/18 + CIN2/3 | EP | Regression to CIN1 or normal pathology at 36 weeks: VGX-3100: 49.5%; placebo: 30.6%, p = 0.034; Concomitant histopathological regression and viral clearance: VGX-3100: 40.2%, placebo: 14.3%, p = 0.003 |
| ZYC101a (DNA plasmid encapsulated in biodegradable poly microparticles encoding segments of HPV16/18 E6/E7 proteins) | ||||||
| 14754702 [62] | II |
100 mcg: ITT: 53, mITT: 37 200 mcg: ITT: 58, mITT: 49 Placebo: ITT: 50; mITT: 41 |
100- and 200 mcgs; IM (lateral quadriceps); 0, 3, 6 | HPV + CIN2/3, no treatment for cervical dysplasia in the last year, ≤ 2 cervical quadrants involved | - | Histopathologic resolution/regression to ≤ CIN1 based on surgical excisional conization at 6 months: ZYC101a group: 43%, placebo: 27%, p = 0.12; (women < 25 years-old: ZYC101a group: 70%, placebo: 23%, p = 0.007) |
| Viral vector TG4001 (Tipapkinogen Sovacivec [TS]; attenuated, recombinant MVA [modified vaccinia virus Ankara] coding for IL-2, HPV16 E6/E7) | ||||||
| 30955915 [63] | II |
TS: ITT: 136; mITT: 129 (55 HPV16 monoinfection) Placebo: ITT: 70; mITT: 63 (27 HPV16 monoinfection) |
NR; SQ (thigh); 0, 1, 2 | CIN2/3, single or multiple HR-HPV infections; no prior ablative/excisional therapy | MVA, IL-2# | Complete histologic resolution at 6 months in patients with HPV16 monoinfection: TS: 18% (95% CI: 8–28%), placebo: 4% (95% CI: 0–11%); complete histologic resolution at 6 months in patients with any hr-HPV: TS: 24%, placebo: 10%, p < 0.05; regression to ≤ CIN1 at 6 months with any hr-HPV: TS: 36%, placebo: 21%, p < 0.05; viral DNA clearance superior with TS compared to placebo (p < 0.01) |
| Peptide HPV16 L1E7 CVLP (CVLP [chimeric virus-like particle]; truncated HPV16 L1 protein fused to truncated HPV16 E7 protein) | ||||||
| 17721997 [64] | NR |
CVLP: 75 mcg: ITT: 14; mITT: 12 CVLP: 250 mcg: ITT: 12; mITT: 11 Placebo: ITT: 13; mITT: 12 |
75- and 250 mcgs; SQ (upper arm); 0, 2, 6, 12 | HPV16 monoinfected CIN2/3; no prior therapy | - | Histopathologic regression to ≤ CIN1 at 24 weeks: CVLP: 39%, placebo: 24%, not significantly different; HPV16 DNA infection clearance at 24 weeks: CVLP: 12%, placebo: 0%, not significantly different |
CIN cervical intraepithelial neoplasia, NR not reported
Table 1.
Selected therapeutic vaccines for HPV-mediated malignancies with published, trial-based data
| Antigen delivery system category, vaccine, and PMID identifier | Phase | N | Eligibility/enrolled | Adjuvant | Other therapies | Primary and secondary clinical and other outcomes |
|---|---|---|---|---|---|---|
| Small nucleic acids | ||||||
| GX-188E ([DNA plasmid encoding HPV16 and 18 E6/E7 fusion protein] + FLT3L [Fms-like tyrosine kinase-3 ligand]) | ||||||
| 33271094 [65] | II | 36 | A/R, inoperable HPV16/HPV18 + CC | EP, FLT3L | Concurrent pembrolizumab | At 24 weeks, ORR: 42% (95% CI: 23–63); CRR: 15%, PRR: 27%; median follow-up 6.2 months (IQR: 3.5–8.1 months) |
| MEDI0457/INO-3112 (VGX-3100 [DNA plasmid encoding HPV16 and 18 E6/E7 genes] with electroporation + INO-9012 [DNA plasmid encoding IL-12]) | ||||||
| 32151670 [68] | I | 10 | Persistent/recurrent cervical cancer after CRT | EP, IL-12 | - | Any treatment-related AEs were grade 1; 8/10 patients with detectable cellular or humoral immune responses against HPV antigens |
| Bacterial vector | ||||||
| ADXS11-001 (ADXS-HPV; axalimogene filolisbac [AXAL]; Lm-LLO-E7; live attenuated Listeria monocytogenes encoding HPV 16 E7 and tLLO) | ||||||
| 29538258 [66] | II | 109 | Recurrent/refractory cervical cancer following prior chemotherapy and/or radiotherapy | tLLO | ADXS11-001 alone or with cisplatin | Median OS: ADXS11-001: 8.3 months; 95% CI, 5.9–10.5 months; ADXS11-001 + cisplatin: 8.8 months; 95% CI, 7.4–13.3 months. Best ORR: ADXS11-001 alone: 17%; ADXS11-001 + cisplatin: 15% |
| 29722659 [72] | I | 10 | Untreated, invasive, anal canal SCC | tLLO | ADXS11-001 administered as neoadjuvant and adjuvant therapy with concurrent chemoradiation | CRR: 100% among 9 patients completing treatment; rate of grade 3 AEs associated with ADXS11-01: 22% |
| 32341753 [67] | II | 36 | R/M anorectal SCC not amenable to curative surgery | tLLO | - | ORR: 3.4%; rate of stable disease: 20.7%; 6-month PFS: 15.5%; median PFS: 2.0 months; OS: 12.6 months; rate of grade 3 AEs: 28%; rate of grade 4 AEs: 3% |
| 32641240 [69] | II | 50 | Metastatic CC s/p curative treatment + ≥ 1-line(s) of systemic chemotherapy and/or biologic therapy | tLLO | - | Any AEs: 98%; rate of grade 3 AEs: 38%; grade 4 AEs: 4% (lung infection/sepsis; hypotension/cytokine release); OS at 12-months: 38%; median OS 6.1 months (95% CI: 4.3–12.1 months); medians PFS 2.8 months; 2% PRR, 10% stable disease |
| Peptides | ||||||
| ISA101 (HPV16 E6/E7-SLPs [nine E6 SLPs, four E7 SLPs) | ||||||
| 23557172 [74] | II | 20 | Incurable R/M HPV16 + gynecologic cancers (16 CCs, 2 VaCs, 2 ACs) | Montanide® ISA-51 | - | ORR: 0%; median OS: 12.6 months; immune response identified in 11/13 patients |
| 30267032 [70] | II | 24 | Incurable HPV16 + cancers (22 OPCs, 1 CC, 1 AC) | - | Concurrent nivolumab | ORR: 33% (90% CI: 19–50%); CRR: 8%, PRR: 25%; median duration of response: 10.3 months; median PFS: 2.7 months; median OS: 17.5 months |
| 35193933 [73] | “ | “ | (Longer-term data of the above trial) | “ | “ | ORR: 29%; median OS of 15.3 months and 2-year OS rate of 33%. Higher expression of immune, inflammatory, and interferon-signaling pathway genes were correlated with clinical response |
| P16-37–63 (p16INK4a 27-amino acid peptide fragment) | ||||||
| 26949913 [71] | I/IIa | 26 | A/R HPV + cancers (17 CCs, 7 OPCs, 1 VuC, 1 AC) | Montanide® ISA-51 VG | - | Patients experienced grade I AEs only (CTCAE); immune response identified in 17/20 patients; ORR: 0% median follow-up 5.6 months; median PFS 3.5 months, median OS 11.9 months |
| GL-0810 (HPV16 E7 peptides linked to a “penetrin” peptide sequence facilitating translocation to the ER + GA [Trojan peptide-based vaccine]) | ||||||
| 25537079 [75] | I | 9 | R/M HPV16 + HNSCC | Montanide® ISA-51 VG + GM-CSF | Grade 1 toxicity: 7/9; grade 2 toxicity: 3/9; T cell and antibody response in 4/9 patients [4/5 who received all 4 vaccinations; ORR: 0%; PFS: 80 days; OS: 196 days | |
| Autologous cell-based | ||||||
| BVAC-C (autologous B cells and monocytes transfected with recombinant HPV16/18 E6 and E7 genes) | ||||||
| 31948126 [76] | I | 11 | R/M HPV16/18 cervical cancer | α-Galactosyl ceramide | - | ORR: 11% (95% CI: 0–32%); 56% achieved stable disease (95% CI: 23–88%); median OS: 12 months |
A advanced, AE adverse event, CC cervical cancer, CI confidence interval, CR complete response, CTCAE Common Terminology Criteria for Adverse Events, ER endoplasmic reticulum, GA Golgi apparatus, GM-CSF granulocyte–macrophage colony-stimulating factor, HNSCC head and neck squamous cell carcinoma, IQR interquartile range, ORR overall response rate OS overall survival, PRR partial response rate, R/M recurrent/metastatic, SCC squamous cell carcinoma
Table 2.
Selected therapeutic vaccines for HPV-mediated premalignancies and malignancies under active or completed trial-based investigation, without published results
| Antigen delivery system category and vaccine | Phase | N | Eligibility | Adjuvant | Other therapies | (Projected) trial end date |
|---|---|---|---|---|---|---|
| Small nucleic acids | ||||||
| MEDI0457/INO-3112 (VGX-3100 [DNA plasmid encoding HPV16 and 18 E6/E7 genes] with electroporation + INO-9012 [DNA plasmid encoding IL-12]) | ||||||
| NCT03439085 | II | 77 | R/M HPV16/18 + cancers | EP, IL-12# | Concurrent durvalumab | Dec 2022 |
| NCT02172911 | I/II | 10 | Primary CC s/p CRT; R/M CC | EP, IL-12# | Curative intent: INO-3112 as adjuvant; R/M: INO-3112 alone | Sept 2017 |
| NCT03162224 | I/IIa | 35 | R/M HPV + HNC | EP, IL-12# | Concurrent durvalumab | March 2021 |
| NCT02163057 | I/IIa | 22 | HPV + HNC | EP, IL-12# | INO-3112 followed by surgery vs CRT | January 2017 |
| NCT03185013 | III | 201 | HPV 16/18 + CIN2/3 | EP | VGX-3100 only | April 2021 |
| NCT03721978 | III | 203 | HPV 16/18 + CIN2/3 | EP | VGX-3100 only | Sept 2022 |
| NCT03603808 | II | 80 | HIV + patients with anal HPV16/18 + HSIL | EP | VGX-3100 only | Aug 2022 |
| NCT00685412 | I | 18 | CIN II/III patients after surgery/ablation | EP | VGX-3100 only | March 2011 |
| NCT03180684 | II | 36 | VIN 2/3 | EP | Imiquimod | December 2020 |
| GX-188E ([DNA plasmid encoding HPV16 and 18 E6/E7 fusion protein] + FLT3L [Fms-like tyrosine kinase-3 ligand]) | ||||||
| NCT03444376 | Ib/II | 60 | Advanced, unresectable HPV16/18 + CC | EP, FLT3L# | Concurrent pembrolizumab | Dec 2023 |
| NCT02596243 | III | 134 | HPV 16/18 + CIN 2/3 | EP, FLT3L# | - | Aug 2018 |
| NCT02139267 | II | 72 | HPV16/18 + CIN 3 | EP, FLT3L# | - | March 2016 |
| VB10.16 (DNA plasmid encoding recombinant protein consisting of 3 modules: inactivated HPV16 E6/E7 protein, human chemokine MIP-1α, linked via dimerization module derived from human IgG3) | ||||||
| NCT04405349 | IIa | 50 | R/M HPV16 + CC ineligible for other therapies | MIP-1α# | Concurrent atezolizumab | Jan 2023 |
| NCT02529930 | I/II | 34 | HPV16 + cervical HSIL (CIN 2/3) | MIP-1α# | - | Jan 2019 |
| pNGVL4aCRTE6E7L2/ pNGVL4aCRTE6E7(detox) (DNA plasmid encoding calreticulin, HPV16 E6/E7/L2 proteins) | ||||||
| NCT04131413 | I | 48 | HIV + HPV16 + CIN2/3 | - | - | December 2024 |
| NCT00988559 | I | 132 | HPV16 + CIN 2/3 | - | ± Imiquimod | July 2016 |
| BNT113 (mRNA encoding HPV16 E6 and E7 proteins encapsulated within liposomes) | ||||||
| NCT04131413 | II | 285 | Unresectable, R/M HPV16 +, PD-L1 + HNSCC | Liposomes | Pembrolizumab alone versus pembrolizumab with BNT113 | May 2025 |
| NCT03418480 | I/II | 44 | Previously treated HPV16 + HNSCC; advanced HPV16 + mediated cervical, head and neck, anal, or penile cancer | Liposomes | Oct 2024 | |
| Viral vector (see combination vaccine category: TA-HPV, Ad-E6E7, MG1-E6E7) | ||||||
| Bacterial vector | ||||||
| ADXS11-001 (ADXS-HPV; axalimogene filolisbac [AXAL]; Lm-LLO-E7; live attenuated Listeria monocytogenes encoding HPV 16 E7 and tLLO) | ||||||
| NCT02002182 | II | 15 | Resectable HPV + OPC | tLLO# | ADXS11-001 followed by primary surgery | Aug 2023 |
| NCT02399813 | II | 51 | Persistent/recurrent anorectal SCC s/p at least one treatment regimen | tLLO# | - | May 2019 |
| NCT02853604 | III | 450 | High-risk locally advanced CC after CRT | tLLO# | ADXS11-001 as adjuvant after definitive CRT | October 2024 |
| Peptides | ||||||
| ISA101/101b (HPV16 E6/E7-SLPs [both ISA101 and 101b have nine E6 SLPs; ISA101 has four E7 SLPs while ISA101b has three E7 SLPs]) | ||||||
| NCT02128126 | I/II | 93 | A/R CC | ± IFNα-IIb | ISA101/101b + neoadjuvant carboplatin + paclitaxel ± bevacizumab | Aug 2018 |
| NCT04646005 | II | 105 | R/M HPV16 + CC | - | ISA101b + concurrent cemiplimab | Oct 2024 |
| NCT03258008 | II | 27 | Incurable HPV16 + OPC | - | ISA101b + concurrent utomilumab | June 2022 |
| NCT04369937 | II | 50 | Primary iIntermediate risk HPV + OPC | - | ISA101b concurrent pembrolizumab + IMRT + cisplatin | June 2024 |
| NCT04398524 | II | 86 | R/M HPV16 + OPC w/ progression on ICIs | - | ISA101b concurrent cemiplimab | Nov 2024 |
| NCT01923116 | I/II | 40 | HIV + men with HPV16 +, grade 2–3 AIN; CD4 count > 350/ul; local treatment-resistant | ± IFN-α | - | Dec 2017 |
| PDS0101 (nanoparticle-based cationic lipid R-DOTAP encapsulates six HPV16 + E6/E7 peptides; R-DOTAP elicits a cellular immune response) | ||||||
| NCT04580771 | II | 35 | Primary, LA CC | R-DOTAP# | CRT + concurrent and adjuvant PDS0101 | March 2024 |
| NCT02065973 | I | 12 | Hr-HPV + CIN 1 | R-DOTAP# | - | Dec 2015 |
| PepCan (4 peptides covering HPV16 E6) | ||||||
| NCT03821272 | I/II | 20 | HNSCC | Candida | - | December 2025 |
| NCT02481414 | II | 125 | HPV16 + cervical HSIL (CIN 2/3) | Candida | - | June 2022 |
| Autologous cell-based | ||||||
| SQZ-PBMC-HPV (peripheral blood mononuclear cells manufactured with immunogenic HPV16 epitopes) | ||||||
| NCT04084951 | I | 200 | HLA-A*02 + patients with LA/R/M HPV16 + cancers | Concurrent atezolizumab OR ipilimumab OR nivolumab OR nivolumab + ipilimumab | November 2022 | |
| NCT04892043 | I | 72 | HLA-A*02 + patients with LA/R/M HPV16 + cancers | - | Alone OR with concurrent: nivolumab OR ipilimumab OR nivolumab + ipilimumab | April 2024 |
| BVAC-C (B cells and monocytes transfected with E6/E7 gene of HPV) | ||||||
| NCT02866006 | I/II | 32 | Multiple metastatic progressive or recurrent HPV16/18 + CC | - | ± Concurrent topotecan | December 2022 |
| NCT04800978 | II | 37 | HPV16/18 + CC failure after first-line platinum-based chemotherapy | Concurrent durvalumab | August 2024 | |
| Heterologous prime-boost | ||||||
|
PVX-2 pBI-1 (small nucleic acid, prime vaccine: DNA plasmid encoding both signal peptide pNGVL4a-Sig [a detox form of HPV16 E7] AND HSP70) + TA-CIN (boost, protein vaccine) | ||||||
| NCT03911076 | II RCT | 122 | HPV16 + ASC-US, ASC-H, LSIL of cervix | - | Randomized to PVX-2 versus placebo | Jan 2024 |
|
pBI-1 (prime vaccine) + TA-HPV (tissue-antigen-HPV, boost, viral vector vaccine: recombinant vaccinia virus expressing HPV16/18 + E6/7 proteins) | ||||||
| NCT00788164 | I | 75 | HPV16 + CIN3 | ± imiquimod | pBI-1 + TA HPV OR imiquimod OR pBI-1 + TA HPV + imiquimod | Dec 2022 |
|
TheraT® vectors HB-201 attenuated arenavirus LCMV encoding inactivated HPV16 E6/E7 fusion protein + HB-202 attenuated arenavirus encoding inactivated HPV16 E6/E7 fusion protein (administered with neoadjuvant chemotherapy prior to surgery) | ||||||
| NCT05108870 | I/II | 98 | HPV + OPSCC | - | HB-201/HB-202 and carboplatin and paclitaxel ± surgery vs RT vs CRT | January 2026 |
| NCT04180215 | I/II | 100 | R/M HPV + cancers | - | - | June 2022 |
Trials in patients with HPV-mediated premalignancies part of, or encoded for, in the vaccine. ASC-US atypical squamous cells of undetermined significance, ASC-H atypical squamous cells – cannot exclude high-grade squamous intraepithelial lesion, CC cervical cancer, CIN cervical intraepithelial neoplasia, CRT chemoradiation therapy, HLA human leukocyte antigens, HPV human papillomavirus, Hr high risk, HSP heat shock protein, ICI immune checkpoint inhibitor, LA locally advanced, LSIL low-grade squamous intraepithelial lesion, OPC oropharyngeal cancer, R-DOTAP R-enantiomer of 1,2-dioleoyl-3-trimethylammonium-propane chloride, R/M recurrent/metastatic, SLPs synthetic long peptides, tLLO truncated Listeriolysin O
Table 5.
Other selected therapeutic vaccines for HPV-mediated premalignancies and malignancies under active or completed trial-based investigation, without published results
| Antigen delivery system category and vaccine | Clinicaltrials.gov identifier |
|---|---|
| Small nucleic acids | |
| ISA201 (two HPV16 E6 SLPs) + (Amplivant® [TLR2-L]) | NCT02821494 |
| HARE-40 (HPV anti-CD40 RNA vaccine) | NCT03418480 |
| Viral vector | |
| PRGN-2009 (gorilla adenovirus encoding HPV16/18 E6/E7 proteins) ± M7824 | NCT04432597 |
| Vvax001 (attenuated Semliki Forest Virus [SFV] encoding E6/E7 proteins) | NCT03141463 |
| Peptides | |
| P16-37–63 (p16INK4a 27-amino acid peptide fragment) + Montanide® ISA-51 VG | NCT02526316 |
| DPX-E7 (synthetic HPV16 E7 peptide consisting of amino acids 11–19) | NCT02865135 |
| Protein | |
| TA-CIN (tissue-antigen CIN; HPV16 L2/E6/E7 fusion protein) | NCT02405221 |
| TVGV-1 (HPV16 E7 bacterial exotoxin fusion protein) + GPI-0100 | NCT02576561 |
| ProCervix (two recombinant adenylate cyclase proteins, CyaA-HPV 16E7 and CyaA-HPV 18E7) + Aldara (5% imiquimod) | NCT01957878 |
| Autologous cell-based | |
| DCs loaded with HPV16/18 E6/E7, injected into adjacent lymph node × 6 | NCT03870113 |
| Peripheral blood mononuclear cells (PBMC) (antigen-presenting cells) treated in vitro with sargramostim (GM-CSF) pulsed with HPV16 E6 or E7, administered IV | NCT00019110 |
| Heterologous prime-boost | |
|
Ad-E6E7 (prime, viral vector vaccine: recombinant adenovirus encoding mutant, inactive HPV E6/E7 proteins) + MG1-E6E7 (boost, viral vector vaccine: recombinant, attenuated oncolytic rhabdovirus Maraba encoding HPV E6/E7 proteins; virus preferentially invades tumor cells, induces E6/E7 expression, lyses tumor cells, and invades adjacent tumor cells) |
NCT03618953 |
|
VTP-200 ChAdOx1-HPV recombinant, attenuated, chimpanzee adenovirus encoding conserved elements of HPV16/18/31/52/58 E1/E2/E4/E6/E7 proteins + MVA-HPV (boost) modified, attenuated vaccinia virus Ankara strain (MVA) encoding conserved elements of HPV16/18/31/52/58 E1/E2/E4/E6/E7 |
NCT04607850 |
Normal font: Trial in patients with HPV-mediated malignancies. Italicized font: Trial in patients with HPV-mediated premalignancies. CRT human calreticulin, a heat shock protein, LCMV lymphocytic choriomeningitis virus, M7824 (bintrafusp alfa) bifunctional fusion protein anti-PD-L1 human monoclonal antibody bound to extracellular domain of human TGF-β-receptor II, LLR2-L toll-like receptor 2 ligand
Early Landmark Trials
Appendix Table 3 highlights early trials evaluating representative therapeutic vaccines for HPV-mediated precancers and cancers [56•, 57, 58•, 59, 60]. There are several notable findings. To our knowledge, tissue-antigen HPV (TA-HPV) was the first therapeutic vaccine tested in humans to treat HPV-mediated disease [56• ]. In this viral vector vaccine, recombinant vaccinia virus was engineered to express HPV16 E6 and E7 proteins, along with HPV18 E6 and E7 proteins, and administered to cervical cancer patients [56• ]. Second, while outcomes of therapeutic vaccination were underwhelming for patients with invasive cancer (including TA-HPV) [56•, 60], outcomes were more favorable for patients with precancer [57, 58•, 59]. For example, the preliminary success of the first ISA101 trial in patients with HPV16 + vulvar intraepithelial neoplasia (VIN)-3 is underscored by its high-impact publication [58• ]. ISA101 is a peptide-based vaccine comprised of nine HPV16 E6 synthetic long-chain peptides (SLPs) and four HPV16 E7 SLPs [58• ]. Third, this is an emerging discipline. The outcomes of most early, therapeutic HPV vaccine trials were published within the last 15 years.
Randomized, Double-Blind, Placebo-Controlled Trials in Cervical Intraepithelial Neoplasia Patients
Several trials have evaluated therapeutic HPV vaccines in patients with cervical and anal intraepithelial neoplasia patients. However, only a handful are of high quality (see Appendix Table 4) [61••, 62–64]. Most of these randomized (blinded), controlled trials demonstrate that therapeutic HPV vaccination either trends towards efficacy or is effective in patients with cervical intraepithelial neoplasia (CIN) [61••, 62–64]. Notably, only the small nucleic acid vaccine VGX-3100 was significantly more effective than placebo according to its primary study outcome. Significantly more vaccinated patients (49.5%) than control patients (30.6%; p= 0.034) exhibited histopathological regression from CIN 2–3 disease to CIN 1 or normal pathology at 36 weeks [61••]. VGX-3100 is a DNA plasmid encoding HPV16 E6 and E7 genes, as well as HPV18 E6 and E7 genes. VGX-3100 is co-administered intramuscularly with electroporation [61••]. During electroporation, an electrical current transiently disrupts cell membrane integrity, facilitating DNA uptake in host cells [61••].
Phase I–II Trials in Patients with HPV-Mediated Malignancies
Conversely, clear evidence of therapeutic vaccine efficacy in patients with advanced, recurrent, or metastatic HPV-mediated malignancies is limited (Table 1) [65–76]. These trials exhibit a few significant findings. First, therapeutic vaccination alone was often unsuccessful. For example, all three peptide-based vaccines exhibited an overall response rate of 0% [71, 74, 75].
Second, in the rare circumstances when vaccine efficacy was identified, the degree of efficacy was limited [66, 67, 69, 76]. In a phase I trial of nine evaluable patients with recurrent or persistent cervical cancer treated with BVAC-C, an APC-based vaccine, the overall response rate was 11%, and 56% exhibited stable disease for 4.2–11 months [76]. Preparation and administration of BVAC-C requires apheris, PBMC collection, and isolation of B cells and monocytes. These cells are transduced with recombinant HPV16 E6 and E7 genes, as well as HPV18 E6 and E7 genes, using an adenovirus vector. The cells are incubated with α-galactosyl ceramide, a natural killer T cell ligand. These recombinant, autologous APCs are then harvested, prepared, and administered back to patients via intravenous injection.
ADXS11-001 alone also exhibited limited efficacy in patients [66, 67, 69]. Axalimogene filolisbac (ADXS-HPV) is a live, attenuated, recombinant, therapeutic vaccine that uses Listeria monocytogenes (Lm) as a bacterial vector. Native Listeria monocytogenes is an intracellular bacterium that uses listeriolysin O (LLO) and phospholipase C to escape phagosomes and enter the host cell cytoplasm. ADXS-HPV secretes an adjuvant-antigen fusion protein consisting of a truncated LLO fragment fused to a full-length HPV16 E7 peptide (tLLO-HPV16 E7). In a trial of 50 recurrent, metastatic cervical cancer patients who failed first-line systemic therapy, only 6% of patients exhibited a response to vaccination [69]. One patient with diffuse, metabolically avid retroperitoneal adenopathy exhibited a durable, complete response lasting 34 months at last follow-up [69]. However, this limited success was partially offset by concerns regarding treatment toxicity [69]. In the trial, 38% of patients experienced a grade 3 adverse event and 4% experienced a grade 4 adverse event [69].
Third, although a proportion of patients in combination trials responded to therapy, the degree to which efficacy is attributable to therapeutic vaccination is unknown [65, 70]. In the ISA101 + nivolumab [70] and GX-188E + pembrolizumab [65] trials, complete response rates ranged from 8 to 15% and overall response rates ranged from 33 to 42%, respectively [65, 70]. However, these outcomes substantially overlap with those of trials evaluating ICIs alone in similar populations [17], suggesting that vaccination may have conferred little to no benefit.
Ongoing, Recently Completed, or Recently Closed Therapeutic Vaccine Trials Without Published Results for HPV-Mediated (Pre)Malignancies
Since the primary barriers to vaccine efficacy in HPV-mediated malignancies are unknown, investigators have employed a shotgun approach to evaluate myriad, diverse, next-generation vaccines. In Table 2 and Appendix Table 5, we describe ongoing, recently completed, or recently closed vaccine trials for HPV-mediated malignancies and premalignancies. The results of these trials have not yet been published. Table 2 describes vaccines undergoing testing in multiple trials or phase II trials. Appendix Table 5 lists vaccines undergoing testing in single, smaller trials. Below, we synthesize and highlight several noteworthy findings from these collective trials.
The Challenge of Therapeutic HPV Vaccine Development
Among the many new trials featured in Table 2, many older trials with projected end dates from 2011 to 2019 have still not published their results. Trial investigators may not have prioritized dissemination of their findings due to negative or null results.
ADXS-HPV vaccine trial progress underscores the challenge of therapeutic vaccine development. To our knowledge, this therapeutic vaccine has been the only vaccine to undergo phase III trial investigation (AIM2CERV) in patients with HPV-mediated malignancies. Despite this, FDA-mediated concerns about treatment toxicity, as well as product chemistry, manufacturing, and controls, have recently dominated discussions about this vaccine [77–80]. Advaxis, the company that produces ADXS-HPV, has abruptly discontinued at least two ADXS-HPV trials. They specified that these decisions stemmed from financial concerns, not safety concerns or concerns about trial results [81]. Although the company continues to champion this product [82], we are not aware of any open ADXS-HPV trials that are actively recruiting patients.
Enthusiasm for New Adjuvants
The current wave of new trials has exhibited a common interest in testing new adjuvants. Some established vaccines have undergone adjuvant upgrades. MEDI0457 consists of VGX-3100 paired with INO-9012, a DNA plasmid encoding IL-12, which directs a cell-mediated immune response [68]. ISA201 consists of two HPV16 E6 SLPs paired with Amplivant®, a synthetic toll-like receptor-2 (TLR2) ligand [83, 84]. TLR2 ligand enhances SLP presentation to antigen-presenting cells (APCs), SLP processing, and APC activation [83, 84].
Other, less established vaccines are also testing novel adjuvants. The peptide-based vaccine PDS0101 uses the cationic lipid enantiomer R-1,2-dioleoyl-3-trimethylammonium-propane (R-DOTAP) to encapsulate and deliver its HPV16 E6 and E7 peptides. According to preclinical studies, R-DOTAP also activates TLR7 and TLR9, stimulating type 1 interferon production and a potent CD8 T cell response [85].
Use of Combination Therapy for HPV-Mediated Malignancies
Considering the limited efficacy of therapeutic vaccination alone for HPV-mediated malignancies to date, many new vaccine trials have paired vaccination with an ICI. For example, the phase II, AHEAD-MERIT trial aims to evaluate pembrolizumab monotherapy versus pembrolizumab with BNT113, an mRNA-based vaccine, as first-line therapy in 285 patients with unresectable recurrent or metastatic HPV16 +, PD-1-positive, head and neck squamous cell carcinoma [86]. BNT113 consists of mRNA encoding HPV16 E6 and E7 oncoproteins encapsulated within liposomes [86].
An ongoing phase II trial is evaluating PDS0101 in combination with M9241 (an immunocytokine) and bintrafusp alfa (a bifunctional fusion protein composed of the transforming growth factor β (TGF-β) receptor and an ICI) for patients with HPV16 + head and neck, cervical, anal, and vaginal cancers. Among 18 patients, the overall response rate was 55.6% and among six ICI-naïve patients, the ORR was 83.3% [87••].
A handful of trials for primary cancer patients have applied traditional, first-line therapy with therapeutic vaccination as neoadjuvant, concurrent, and/or adjuvant treatment.
Heterologous Prime-Boost Vaccines
In the heterologous prime-boost approach, the prime and booster vaccines are unique (Tables 4 and 5) [88]. The TheraT® viral vectors HB-201 and HB-202 represent an important example of this approach. HB-201 consists of attenuated, recombinant lymphocytic choriomeningitis (LCMV) encoding an inactivated HPV16 E6 and E7 fusion protein. HB-202 consists of recombinant Pichinde virus (PICV) encoding the same protein [89]. LCMV and PICV are two different RNA-based arenavirus species within the family Arenaviridae and genus Mammarenavirus. Early phase I results in patients with recurrent/metastatic HPV16 + cancers have been promising [87••]. Immunogenicity may be greater in patients receiving alternating therapy compared to monotherapy (HB-201 alone) [90].
Other Future Directions
Personalized Therapeutic Vaccines
Considering the limited efficacy of therapeutic vaccines that use HPV-specific antigens, personalized, therapeutic vaccines may warrant further investigation. The basis for personalized therapeutic vaccination is that mutations in tumor cell DNA result in the production of novel epitopes of self-antigens (i.e., neoantigens), which can be identified by next-generation sequencing. Neoantigens that are anticipated to elicit an immune response are selected and the vaccine is produced. The weaknesses of this approach include the high cost, time-intensive nature, and challenge of selecting neoantigens that can be presented by antigen-presenting cells in vivo.
GEN-009, a representative neoantigen-based vaccine, was recently evaluated in a phase I/IIa trial in patients with solid tumors, including head and neck squamous cell carcinoma. Early safety, immune response, and efficacy data were encouraging [91].
Need for Novel, Multimodal Therapeutic Approaches
Given the complexity of cancer biology, maximally optimized, therapeutic HPV vaccines are unlikely to cure HPV-mediated malignancies on their own. In their landmark article, “Hallmarks of Cancer: Next Generation,” Hanahan and Weinberg described the eight hallmark, biological capabilities of cancer [92]. Only one involves “avoiding immune destruction.” [92] The other seven hallmarks include sustaining proliferative signaling, evading growth suppressors, resisting cell death, enabling replicative immortality, inducing angiogenesis, activating invasion and metastasis, and deregulating cellular energetics [92]. Genome instability and mutation, as well as tumor-promoting inflammation, are two key enabling characteristics of these hallmarks [92].
Novel, multimodal oncologic approaches that more comprehensively address these diverse hallmarks of cancer will be necessary. Investigators have established biological rationales for pairing immune checkpoint inhibition with virtually all other oncologic therapies, including, but not limited to, therapeutic vaccination [87••, 93, 94], other immunotherapies (e.g., oncolytic virus therapy) [93, 95], cytotoxic chemotherapy [96], and radiotherapy [97]. Evaluation of novel approaches involving three or more therapies, including therapeutic HPV vaccination and immune checkpoint inhibition, appears indicated [87••].
Additionally, most combination trials are evaluating therapeutic HPV vaccines in the locoregionally advanced, recurrent, or metastatic setting. However, there is also a strong biological rationale for therapeutic HPV vaccination, with or without ICIs, in the primary, neoadjuvant setting, followed by standard first-line therapy [98–100].
Conclusion
Despite their limited efficacy to date, therapeutic vaccines for HPV-mediated malignancies retain a strong biological rationale, along with substantial clinical promise. Myriad ongoing trials evaluating diverse antigen delivery systems, adjuvant, prime-boost approaches, and combination therapies are sure to advance the discipline. Combination regimens incorporating therapeutic HPV vaccination, immune checkpoint inhibition, and other therapies (e.g., novel adjuvant[s]) may most effectively harness the power of this therapy.
Appendix
Funding
Eugene P. Frenkel, M.D., Clinical Scholars Program.
Declarations
Conflict of Interest
The authors declare no competing interests.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Footnotes
This article is part of the Topical collection on HEAD AND NECK: Human Papilloma Virus Associated Head and Neck Squamous Cell Carcinoma
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
- 1.Senkomago V, Henley SJ, Thomas CC, Mix JM, Markowitz LE, Saraiya M. Human papillomavirus-attributable cancers - United States, 2012–2016. MMWR Morb Mortal Wkly Rep. 2019;68(33):724–728. doi: 10.15585/mmwr.mm6833a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.de Martel C, Georges D, Bray F, Ferlay J, Clifford GM. Global burden of cancer attributable to infections in 2018: a worldwide incidence analysis. Lancet Glob Health. 2020;8(2):e180–e190. doi: 10.1016/S2214-109X(19)30488-7. [DOI] [PubMed] [Google Scholar]
- 3.Arbyn M, Weiderpass E, Bruni L, et al. Estimates of incidence and mortality of cervical cancer in 2018: a worldwide analysis. Lancet Glob Health. 2020;8(2):e191–e203. doi: 10.1016/S2214-109X(19)30482-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cramer JD, Hicks KE, Rademaker AW, Patel UA, Samant S. Validation of the eighth edition American Joint Committee on Cancer staging system for human papillomavirus-associated oropharyngeal cancer. Head Neck. 2018;40(3):457–466. [DOI] [PubMed]
- 5.Høxbroe Michaelsen S, Grønhøj C, Høxbroe Michaelsen J, Friborg J, von Buchwald C. Quality of life in survivors of oropharyngeal cancer: a systematic review and meta-analysis of 1366 patients. Eur J Cancer. 2017;78:91–102. doi: 10.1016/j.ejca.2017.03.006. [DOI] [PubMed] [Google Scholar]
- 6.Caparrotti F, Huang SH, Lu L, et al. Osteoradionecrosis of the mandible in patients with oropharyngeal carcinoma treated with intensity-modulated radiotherapy. Cancer. 2017;123(19):3691–3700. doi: 10.1002/cncr.30803. [DOI] [PubMed] [Google Scholar]
- 7.de Almeida JR, Byrd JK, Wu R, et al. A systematic review of transoral robotic surgery and radiotherapy for early oropharynx cancer: a systematic review. Laryngoscope. 2014;124(9):2096–2102. doi: 10.1002/lary.24712. [DOI] [PubMed] [Google Scholar]
- 8.Machtay M, Moughan J, Trotti A, et al. Factors associated with severe late toxicity after concurrent chemoradiation for locally advanced head and neck cancer: an RTOG analysis. J Clin Oncol. 2008;26(21):3582–3589. doi: 10.1200/JCO.2007.14.8841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chera BS, Amdur RJ, Green R, et al. Phase II trial of de-intensified chemoradiotherapy for human papillomavirus-associated oropharyngeal squamous cell carcinoma. J Clin Oncol. 2019;37(29):2661–2669. doi: 10.1200/JCO.19.01007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ferris RL, Flamand Y, Weinstein GS, et al. Phase II randomized trial of transoral surgery and low-dose intensity modulated radiation therapy in resectable p16+ locally advanced oropharynx cancer: an ECOG-ACRIN Cancer Research Group Trial (E3311). J Clin Oncol. 2021:Jco2101752. [DOI] [PMC free article] [PubMed]
- 11.Ma DJ, Price KA, Moore EJ, et al. Phase II evaluation of aggressive dose de-escalation for adjuvant chemoradiotherapy in human papillomavirus-associated oropharynx squamous cell carcinoma. J Clin Oncol. 2019;37(22):1909–1918. doi: 10.1200/JCO.19.00463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gillison ML, Trotti AM, Harris J, et al. Radiotherapy plus cetuximab or cisplatin in human papillomavirus-positive oropharyngeal cancer (NRG Oncology RTOG 1016): a randomised, multicentre, non-inferiority trial. Lancet. 2019;393(10166):40–50. doi: 10.1016/S0140-6736(18)32779-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pignata S, Scambia G, Lorusso D, et al. The MITO CERV-2 trial: a randomized phase II study of cetuximab plus carboplatin and paclitaxel, in advanced or recurrent cervical cancer. Gynecol Oncol. 2019;153(3):535–540. doi: 10.1016/j.ygyno.2019.03.260. [DOI] [PubMed] [Google Scholar]
- 14.Lee NY, Ferris RL, Psyrri A, et al. Avelumab plus standard-of-care chemoradiotherapy versus chemoradiotherapy alone in patients with locally advanced squamous cell carcinoma of the head and neck: a randomised, double-blind, placebo-controlled, multicentre, phase 3 trial. Lancet Oncol. 2021;22(4):450–462. doi: 10.1016/S1470-2045(20)30737-3. [DOI] [PubMed] [Google Scholar]
- 15.Colombo N, Dubot C, Lorusso D, et al. Pembrolizumab for persistent, recurrent, or metastatic cervical cancer. N Engl J Med. 2021;385(20):1856–1867. doi: 10.1056/NEJMoa2112435. [DOI] [PubMed] [Google Scholar]
- 16.Burtness B, Harrington KJ, Greil R, et al. Pembrolizumab alone or with chemotherapy versus cetuximab with chemotherapy for recurrent or metastatic squamous cell carcinoma of the head and neck (KEYNOTE-048): a randomised, open-label, phase 3 study. Lancet. 2019;394(10212):1915–1928. doi: 10.1016/S0140-6736(19)32591-7. [DOI] [PubMed] [Google Scholar]
- 17.Ferris RL, Blumenschein G, Jr, Fayette J, et al. Nivolumab for recurrent squamous-cell carcinoma of the head and neck. N Engl J Med. 2016;375(19):1856–1867. doi: 10.1056/NEJMoa1602252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Schneider K, Grønhøj C, Hahn CH, von Buchwald C. Therapeutic human papillomavirus vaccines in head and neck cancer: a systematic review of current clinical trials. Vaccine. 2018;36(45):6594–6605. doi: 10.1016/j.vaccine.2018.09.027. [DOI] [PubMed] [Google Scholar]
- 19.Waldman AD, Fritz JM, Lenardo MJ. A guide to cancer immunotherapy: from T cell basic science to clinical practice. Nat Rev Immunol. 2020;20(11):651–668. doi: 10.1038/s41577-020-0306-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zhang Y, Zhang Z. The history and advances in cancer immunotherapy: understanding the characteristics of tumor-infiltrating immune cells and their therapeutic implications. Cell Mol Immunol. 2020;17(8):807–821. doi: 10.1038/s41423-020-0488-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Andtbacka RH, Kaufman HL, Collichio F, et al. Talimogene laherparepvec improves durable response rate in patients with advanced melanoma. J Clin Oncol. 2015;33(25):2780–2788. doi: 10.1200/JCO.2014.58.3377. [DOI] [PubMed] [Google Scholar]
- 22.Kaufman HL, Kim DW, DeRaffele G, Mitcham J, Coffin RS, Kim-Schulze S. Local and distant immunity induced by intralesional vaccination with an oncolytic herpes virus encoding GM-CSF in patients with stage IIIc and IV melanoma. Ann Surg Oncol. 2010;17(3):718–730. doi: 10.1245/s10434-009-0809-6. [DOI] [PubMed] [Google Scholar]
- 23.Lobo N, Brooks NA, Zlotta AR, et al. 100 years of Bacillus Calmette-Guérin immunotherapy: from cattle to COVID-19. Nat Rev Urol. 2021;18(10):611–622. doi: 10.1038/s41585-021-00481-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.June CH, Sadelain M. Chimeric antigen receptor therapy. N Engl J Med. 2018;379(1):64–73. doi: 10.1056/NEJMra1706169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nagarsheth NB, Norberg SM, Sinkoe AL, et al. TCR-engineered T cells targeting E7 for patients with metastatic HPV-associated epithelial cancers. Nat Med. 2021;27(3):419–425. doi: 10.1038/s41591-020-01225-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hu Z, Ott PA, Wu CJ. Towards personalized, tumour-specific, therapeutic vaccines for cancer. Nat Rev Immunol. 2018;18(3):168–182. doi: 10.1038/nri.2017.131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hollingsworth RE, Jansen K. Turning the corner on therapeutic cancer vaccines. NPJ Vaccines. 2019;4:7. doi: 10.1038/s41541-019-0103-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gjerstorff MF, Andersen MH, Ditzel HJ. Oncogenic cancer/testis antigens: prime candidates for immunotherapy. Oncotarget. 2015;6(18):15772–15787. doi: 10.18632/oncotarget.4694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Blass E, Ott PA. Advances in the development of personalized neoantigen-based therapeutic cancer vaccines. Nat Rev Clin Oncol. 2021;18(4):215–229. doi: 10.1038/s41571-020-00460-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Le DT, Pardoll DM, Jaffee EM. Cellular vaccine approaches. Cancer J. 2010;16(4):304–310. doi: 10.1097/PPO.0b013e3181eb33d7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dehghan-Manshadi M, Nikpoor AR, Hadinedoushan H, et al. Preventive cancer vaccination with P5 HER-2/neo-derived peptide-pulsed peripheral blood mononuclear cells in a mouse model of breast cancer. Biochem Cell Biol. 2021;99(4):435–446. doi: 10.1139/bcb-2020-0559. [DOI] [PubMed] [Google Scholar]
- 32.Peterson AC, Harlin H, Gajewski TF. Immunization with Melan-A peptide-pulsed peripheral blood mononuclear cells plus recombinant human interleukin-12 induces clinical activity and T-cell responses in advanced melanoma. J Clin Oncol. 2003;21(12):2342–2348. doi: 10.1200/JCO.2003.12.144. [DOI] [PubMed] [Google Scholar]
- 33.Szeto GL, Van Egeren D, Worku H, et al. Microfluidic squeezing for intracellular antigen loading in polyclonal B-cells as cellular vaccines. Sci Rep. 2015;5:10276. doi: 10.1038/srep10276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Perez CR, De Palma M. Engineering dendritic cell vaccines to improve cancer immunotherapy. Nat Commun. 2019;10(1):5408. doi: 10.1038/s41467-019-13368-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gajewski TF, Fallarino F, Ashikari A, Sherman M. Immunization of HLA-A2+ melanoma patients with MAGE-3 or MelanA peptide-pulsed autologous peripheral blood mononuclear cells plus recombinant human interleukin 12. Clin Cancer Res. 2001;7(3 Suppl):895s–901s. [PubMed] [Google Scholar]
- 36.Pulendran B, P SA, O’Hagan DT. Emerging concepts in the science of vaccine adjuvants. Nat Rev Drug Discov. 2021;20(6):454–475. [DOI] [PMC free article] [PubMed]
- 37.Coffman RL, Sher A, Seder RA. Vaccine adjuvants: putting innate immunity to work. Immunity. 2010;33(4):492–503. doi: 10.1016/j.immuni.2010.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Singh M, O’Hagan D. Advances in vaccine adjuvants. Nat Biotechnol. 1999;17(11):1075–1081. doi: 10.1038/15058. [DOI] [PubMed] [Google Scholar]
- 39.Guy B. The perfect mix: recent progress in adjuvant research. Nat Rev Microbiol. 2007;5(7):505–517. doi: 10.1038/nrmicro1681. [DOI] [PubMed] [Google Scholar]
- 40.Nabhan C. Sipuleucel-T immunotherapy for castration-resistant prostate cancer. N Engl J Med. 2010;363(20):1966–1967; author reply 1968. [DOI] [PubMed]
- 41.Human papillomaviruses. IARC Monogr Eval Carcinog Risks Hum. 2007;90:1–636. [PMC free article] [PubMed]
- 42.Roden RBS, Stern PL. Opportunities and challenges for human papillomavirus vaccination in cancer. Nat Rev Cancer. 2018;18(4):240–254. doi: 10.1038/nrc.2018.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Geraets D, Alemany L, Guimera N, et al. Detection of rare and possibly carcinogenic human papillomavirus genotypes as single infections in invasive cervical cancer. J Pathol. 2012;228(4):534–543. doi: 10.1002/path.4065. [DOI] [PubMed] [Google Scholar]
- 44.Forman D, de Martel C, Lacey CJ, et al. Global burden of human papillomavirus and related diseases. Vaccine. 2012;30(Suppl 5):F12–23. doi: 10.1016/j.vaccine.2012.07.055. [DOI] [PubMed] [Google Scholar]
- 45.Ndiaye C, Mena M, Alemany L, et al. HPV DNA, E6/E7 mRNA, and p16INK4a detection in head and neck cancers: a systematic review and meta-analysis. Lancet Oncol. 2014;15(12):1319–1331. doi: 10.1016/S1470-2045(14)70471-1. [DOI] [PubMed] [Google Scholar]
- 46.Viens LJ, Henley SJ, Watson M, et al. Human papillomavirus-associated cancers - United States, 2008–2012. MMWR Morb Mortal Wkly Rep. 2016;65(26):661–666. doi: 10.15585/mmwr.mm6526a1. [DOI] [PubMed] [Google Scholar]
- 47.Doorbar J, Quint W, Banks L, et al. The biology and life-cycle of human papillomaviruses. Vaccine. 2012;30(Suppl 5):F55–70. doi: 10.1016/j.vaccine.2012.06.083. [DOI] [PubMed] [Google Scholar]
- 48.Schiller JT, Müller M. Next generation prophylactic human papillomavirus vaccines. Lancet Oncol. 2015;16(5):e217–225. doi: 10.1016/S1470-2045(14)71179-9. [DOI] [PubMed] [Google Scholar]
- 49.Chen XS, Garcea RL, Goldberg I, Casini G, Harrison SC. Structure of small virus-like particles assembled from the L1 protein of human papillomavirus 16. Mol Cell. 2000;5(3):557–567. doi: 10.1016/S1097-2765(00)80449-9. [DOI] [PubMed] [Google Scholar]
- 50.Kirnbauer R, Booy F, Cheng N, Lowy DR, Schiller JT. Papillomavirus L1 major capsid protein self-assembles into virus-like particles that are highly immunogenic. Proc Natl Acad Sci U S A. 1992;89(24):12180–12184. doi: 10.1073/pnas.89.24.12180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Mariani L, Venuti A. HPV vaccine: an overview of immune response, clinical protection, and new approaches for the future. J Transl Med. 2010;8:105. doi: 10.1186/1479-5876-8-105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Herrero R, González P, Markowitz LE. Present status of human papillomavirus vaccine development and implementation. Lancet Oncol. 2015;16(5):e206–216. doi: 10.1016/S1470-2045(14)70481-4. [DOI] [PubMed] [Google Scholar]
- 53.Arbyn M, Xu L, Simoens C, Martin-Hirsch PP. Prophylactic vaccination against human papillomaviruses to prevent cervical cancer and its precursors. Cochrane Database Syst Rev. 2018;5(5):Cd009069. [DOI] [PMC free article] [PubMed]
- 54.Hildesheim A, Herrero R, Wacholder S, et al. Effect of human papillomavirus 16/18 L1 viruslike particle vaccine among young women with preexisting infection: a randomized trial. JAMA. 2007;298(7):743–753. doi: 10.1001/jama.298.7.743. [DOI] [PubMed] [Google Scholar]
- 55.Hancock G, Blight J, Lopez-Camacho C, et al. A multi-genotype therapeutic human papillomavirus vaccine elicits potent T cell responses to conserved regions of early proteins. Sci Rep. 2019;9(1):18713. doi: 10.1038/s41598-019-55014-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.• Borysiewicz LK, Fiander A, Nimako M, et al. A recombinant vaccinia virus encoding human papillomavirus types 16 and 18, E6 and E7 proteins as immunotherapy for cervical cancer. Lancet. 1996;347(9014):1523–1527. To our knowledge, this is the first peer-reviewed study describing the use of a therapeutic HPV vaccine in humans. [DOI] [PubMed]
- 57.Daayana S, Elkord E, Winters U, et al. Phase II trial of imiquimod and HPV therapeutic vaccination in patients with vulval intraepithelial neoplasia. Br J Cancer. 2010;102(7):1129–1136. doi: 10.1038/sj.bjc.6605611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.• Kenter GG, Welters MJ, Valentijn AR, et al. Vaccination against HPV-16 oncoproteins for vulvar intraepithelial neoplasia. N Engl J Med. 2009;361(19):1838–1847. This is the first landmark study demonstrating the potential promise of therapeutic HPV vaccines for premalignancies. [DOI] [PubMed]
- 59.Kim TJ, Jin HT, Hur SY, et al. Clearance of persistent HPV infection and cervical lesion by therapeutic DNA vaccine in CIN3 patients. Nat Commun. 2014;5:5317. doi: 10.1038/ncomms6317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Maciag PC, Radulovic S, Rothman J. The first clinical use of a live-attenuated Listeria monocytogenes vaccine: a phase I safety study of Lm-LLO-E7 in patients with advanced carcinoma of the cervix. Vaccine. 2009;27(30):3975–3983. doi: 10.1016/j.vaccine.2009.04.041. [DOI] [PubMed] [Google Scholar]
- 61.•• Trimble CL, Morrow MP, Kraynyak KA, et al. Safety, efficacy, and immunogenicity of VGX-3100, a therapeutic synthetic DNA vaccine targeting human papillomavirus 16 and 18 E6 and E7 proteins for cervical intraepithelial neoplasia 2/3: a randomised, double-blind, placebo-controlled phase 2b trial. Lancet. 2015;386(10008):2078–2088. This was the first trial among patients with premalignancies where a therapeutic HPV vaccine was efficacious according to its primary, predefined endpoint. [DOI] [PMC free article] [PubMed]
- 62.Garcia F, Petry KU, Muderspach L, et al. ZYC101a for treatment of high-grade cervical intraepithelial neoplasia: a randomized controlled trial. Obstet Gynecol. 2004;103(2):317–326. doi: 10.1097/01.AOG.0000110246.93627.17. [DOI] [PubMed] [Google Scholar]
- 63.Harper DM, Nieminen P, Donders G, et al. The efficacy and safety of Tipapkinogen Sovacivec therapeutic HPV vaccine in cervical intraepithelial neoplasia grades 2 and 3: randomized controlled phase II trial with 2.5 years of follow-up. Gynecol Oncol. 2019;153(3):521–529. [DOI] [PubMed]
- 64.Kaufmann AM, Nieland JD, Jochmus I, et al. Vaccination trial with HPV16 L1E7 chimeric virus-like particles in women suffering from high grade cervical intraepithelial neoplasia (CIN 2/3) Int J Cancer. 2007;121(12):2794–2800. doi: 10.1002/ijc.23022. [DOI] [PubMed] [Google Scholar]
- 65.Youn JW, Hur SY, Woo JW, et al. Pembrolizumab plus GX-188E therapeutic DNA vaccine in patients with HPV-16-positive or HPV-18-positive advanced cervical cancer: interim results of a single-arm, phase 2 trial. Lancet Oncol. 2020;21(12):1653–1660. doi: 10.1016/S1470-2045(20)30486-1. [DOI] [PubMed] [Google Scholar]
- 66.Basu P, Mehta A, Jain M, et al. A randomized phase 2 study of ADXS11-001 Listeria monocytogenes-listeriolysin O immunotherapy with or without cisplatin in treatment of advanced cervical cancer. Int J Gynecol Cancer. 2018;28(4):764–772. doi: 10.1097/IGC.0000000000001235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Eng C, Fakih M, Amin M, et al. A phase II study of axalimogene filolisbac for patients with previously treated, unresectable, persistent/recurrent loco-regional or metastatic anal cancer. Oncotarget. 2020;11(15):1334–1343. doi: 10.18632/oncotarget.27536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Hasan Y, Furtado L, Tergas A, et al. A phase 1 trial assessing the safety and tolerability of a therapeutic DNA vaccination against HPV16 and HPV18 E6/E7 oncogenes after chemoradiation for cervical cancer. Int J Radiat Oncol Biol Phys. 2020;107(3):487–498. doi: 10.1016/j.ijrobp.2020.02.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Huh WK, Brady WE, Fracasso PM, et al. Phase II study of axalimogene filolisbac (ADXS-HPV) for platinum-refractory cervical carcinoma: an NRG oncology/gynecologic oncology group study. Gynecol Oncol. 2020;158(3):562–569. doi: 10.1016/j.ygyno.2020.06.493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Massarelli E, William W, Johnson F, et al. Combining immune checkpoint blockade and tumor-specific vaccine for patients with incurable human papillomavirus 16-related cancer: a phase 2 clinical trial. JAMA Oncol. 2019;5(1):67–73. doi: 10.1001/jamaoncol.2018.4051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Reuschenbach M, Pauligk C, Karbach J, et al. A phase 1/2a study to test the safety and immunogenicity of a p16(INK4a) peptide vaccine in patients with advanced human papillomavirus-associated cancers. Cancer. 2016;122(9):1425–1433. doi: 10.1002/cncr.29925. [DOI] [PubMed] [Google Scholar]
- 72.Safran H, Leonard KL, Perez K, et al. Tolerability of ADXS11-001 Lm-LLO Listeria-based immunotherapy with mitomycin, fluorouracil, and radiation for anal cancer. Int J Radiat Oncol Biol Phys. 2018;100(5):1175–1178. doi: 10.1016/j.ijrobp.2018.01.004. [DOI] [PubMed] [Google Scholar]
- 73.Sousa LG, Rajapakshe K, Rodriguez Canales J, et al. ISA101 and nivolumab for HPV-16(+) cancer: updated clinical efficacy and immune correlates of response. J Immunother Cancer. 2022;10(2). [DOI] [PMC free article] [PubMed]
- 74.van Poelgeest MI, Welters MJ, van Esch EM, et al. HPV16 synthetic long peptide (HPV16-SLP) vaccination therapy of patients with advanced or recurrent HPV16-induced gynecological carcinoma, a phase II trial. J Transl Med. 2013;11:88. doi: 10.1186/1479-5876-11-88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Zandberg DP, Rollins S, Goloubeva O, et al. A phase I dose escalation trial of MAGE-A3- and HPV16-specific peptide immunomodulatory vaccines in patients with recurrent/metastatic (RM) squamous cell carcinoma of the head and neck (SCCHN) Cancer Immunol Immunother. 2015;64(3):367–379. doi: 10.1007/s00262-014-1640-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Choi CH, Choi HJ, Lee JW, et al. Phase I study of a B cell-based and monocyte-based immunotherapeutic vaccine, BVAC-C in human papillomavirus type 16- or 18-positive recurrent cervical cancer. J Clin Med. 2020;9(1). [DOI] [PMC free article] [PubMed]
- 77.Advaxis I. A phase 1/2 study in patients with HPV16+ recurrent/metastatic head and neck squamous cell carcinoma and other cancers. In. November 27, 2019 ed. Clinicaltrials.gov: U.S. National Library of Medicine. 2019.
- 78.Advaxis announces FDA lifts clinical hold on phase 1/2 combination study of axalimogene filolisbac with durvalumab. Berkshire Hathaway. https://www.businesswire.com/news/home/20180713005040/en/Advaxis-Announces-FDA-Lifts-Clinical-Hold-on-Phase-12-Combination-Study-of-Axalimogene-Filolisbac-with-Durvalumab. Published 2018. Accessed August 28, 2022.
- 79.FDA lifts partial clinical hold on phase 3 AIM2CERV study of axalimogene filolisbac. Berkshire Hathaway. https://www.businesswire.com/news/home/20190515005119/en/FDA-Lifts-Partial-Clinical-Hold-on-Phase-3-AIM2CERV-Study-of-Axalimogene-Filolisbac. Published 2019. Accessed August 28, 2022.
- 80.Advaxis I. Study of ADXS11-001 in subjects with high risk locally advanced cervical cancer (AIM2CERV). In. August 3, 2016 ed. Clinicaltrials.gov: U.S. National Library of Medicine. 2016.
- 81.Advaxis announces increasing focus on neoantigen-directed immunotherapies and closing of its phase 3 AIM2CERV study. Berkshire Hathaway. https://www.businesswire.com/news/home/20190627005184/en/Advaxis-Announces-Increasing-Focus-on-Neoantigen-Directed-Immunotherapies-and-Closing-of-Its-Phase-3-AIM2CERV-Study. Published 2019. Accessed August 28, 2022.
- 82.HPV-associated cancers. Advaxis, Inc. https://www.advaxis.com/hpv-associated-cancers. Accessed August 28, 2022.
- 83.Zom GG, Welters MJ, Loof NM, et al. TLR2 ligand-synthetic long peptide conjugates effectively stimulate tumor-draining lymph node T cells of cervical cancer patients. Oncotarget. 2016;7(41):67087–67100. doi: 10.18632/oncotarget.11512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Zom GG, Willems M, Khan S, et al. Novel TLR2-binding adjuvant induces enhanced T cell responses and tumor eradication. J Immunother Cancer. 2018;6(1):146. doi: 10.1186/s40425-018-0455-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Gandhapudi SK, Ward M, Bush JPC, Bedu-Addo F, Conn G, Woodward JG. Antigen priming with enantiospecific cationic lipid nanoparticles induces potent antitumor CTL responses through novel induction of a type I IFN response. J Immunol. 2019;202(12):3524–3536. doi: 10.4049/jimmunol.1801634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.SE B. A clinical trial investigating the safety, tolerability, and therapeutic effects of BNT113 in combination with pembrolizumab versus pembrolizumab alone for patients with a form of head and neck cancer positive for human papilloma virus 16 and expressing the protein PD-L1 (AHEAD-MERIT). In. September 1, 2020 ed. Clinicaltrials.gov: U.S. National Library of Medicine; 2020.
- 87.•• Combo approaches for HPV16+ cancers. Cancer Discov. 2021;11(8):1865–1866. Highlighting the potential of combination therapy, this manuscript describes very favorable preliminary response rates for HPV16+ cancer patients receiving a therapeutic vaccine (PDDS0101), an immunocytokine (M9241), and an immune checkpoint inhibitor fused to transforming growth factor β (TGF-β) receptor (bintrafusp alpha). [DOI] [PubMed]
- 88.Lu S. Heterologous prime-boost vaccination. Curr Opin Immunol. 2009;21(3):346–351. doi: 10.1016/j.coi.2009.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Summary notification information format for the release of genetically modified organisms other than higher plants in accordance with Article 11 of Directive 2001/18/EC: Product HB-201, HB-202 Hookipa Pharma.
- 90.Edwards D, Schwendinger M, Katchar K, et al. Abstract 3284: HB-201 and HB-202, an arenavirus-based immunotherapy, induces tumor T cell infiltration in patients with HNSCC and other HPV16+ tumors. Cancer Research. 2022;82(12_Supplement):3284–3284.
- 91.Gillison ML, Awad MM, Twardowski P, et al. Long term results from a phase 1 trial of GEN-009, a personalized neoantigen vaccine, combined with PD-1 inhibition in advanced solid tumors. J Clin Oncol. 2021;39(15_suppl):2613–2613.
- 92.Hanahan D, Weinberg RA. Hallmarks of cancer: the next generation. Cell. 2011;144(5):646–674. doi: 10.1016/j.cell.2011.02.013. [DOI] [PubMed] [Google Scholar]
- 93.Ott PA, Hodi FS, Kaufman HL, Wigginton JM, Wolchok JD. Combination immunotherapy: a road map. J Immunother Cancer. 2017;5:16. doi: 10.1186/s40425-017-0218-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Strauss J, Floudas CS, Sater HA, et al. Phase II evaluation of the triple combination of PDS0101, M9241, and bintrafusp alfa in patients with HPV 16 positive malignancies. J Clin Oncol. 2021;39(15_suppl):2501–2501.
- 95.Chen CY, Hutzen B, Wedekind MF, Cripe TP. Oncolytic virus and PD-1/PD-L1 blockade combination therapy. Oncolytic Virother. 2018;7:65–77. doi: 10.2147/OV.S145532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Bailly C, Thuru X, Quesnel B. Combined cytotoxic chemotherapy and immunotherapy of cancer: modern times. NAR Cancer. 2020;2(1):zcaa002. [DOI] [PMC free article] [PubMed]
- 97.Zhang Z, Liu X, Chen D, Yu J. Radiotherapy combined with immunotherapy: the dawn of cancer treatment. Signal Transduct Target Ther. 2022;7(1):258. doi: 10.1038/s41392-022-01102-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Grinshtein N, Bridle B, Wan Y, Bramson JL. Neoadjuvant vaccination provides superior protection against tumor relapse following surgery compared with adjuvant vaccination. Cancer Res. 2009;69(9):3979–3985. doi: 10.1158/0008-5472.CAN-08-3385. [DOI] [PubMed] [Google Scholar]
- 99.Ogino H, Taylor JW, Nejo T, et al. Randomized trial of neoadjuvant vaccination with tumor-cell lysate induces T cell response in low-grade gliomas. J Clin Invest. 2022;132(3). [DOI] [PMC free article] [PubMed]
- 100.Zhang L, Zhou X, Sha H, Xie L, Liu B. Recent progress on therapeutic vaccines for breast cancer. Front Oncol. 2022;12:905832. doi: 10.3389/fonc.2022.905832. [DOI] [PMC free article] [PubMed] [Google Scholar]