Abstract
Introduction
Clozapine and olanzapine are some of the most effective antipsychotics, but both are associated with weight gain and relevant metabolic disturbances, including pre-diabetes and diabetes. Non-pharmacological/behavioural interventions have had limited effects counteracting these adverse effects. Semaglutide, a glucagon-like peptide 1 receptor agonist, is approved for the treatment of type 2 diabetes and obesity. We will investigate the long-term effects of add-on treatment with semaglutide once a week versus placebo once a week on the metabolic status in pre-diabetic (glycated haemoglobin A1c (HbA1c) 35–47 mmol/mol (5.4%–6.4%) and diabetic (HbA1c 48–57 mmol/mol (6.5%–7.4%)) patients diagnosed with a schizophrenia spectrum disorder who initiated clozapine or olanzapine treatment within the last 60 months.
Methods and analysis
This is a 26-week, double-blinded, randomised, placebo-controlled trial. Altogether, 104 patients diagnosed with a schizophrenia spectrum disorder, aged 18–65 years, with pre-diabetes or diabetes will be randomised to injections of 1.0 mg semaglutide once a week or placebo for 26 weeks. The primary endpoint is change from baseline in HbA1c. Secondary endpoints include changes in body weight, hip and waist circumference and plasma levels of insulin, glucagon, glucose, and C-peptide, insulin sensitivity, beta cell function, hepatic function, fibrosis-4 score, lipid profile, incretin hormones, bone markers, body composition, bone density, proteomic analyses and oxidative stress markers. Together with alcohol, tobacco and drug use, potential effects on the reward value of a sweet–fat stimulus, psychopathology, level of activity and quality of life will also be assessed.
Ethics and dissemination
This study is approved by the Danish Medicines Agency and the regional scientific ethics committee of the Capital Region of Denmark (committee C, #H-20019008) and will be carried out in accordance with International Council for Harmonisation Good Clinical Practice guidelines and the Helsinki Declaration. The results will be disseminated through peer-review publications and conference presentations.
Trial registration number
Keywords: DIABETES & ENDOCRINOLOGY, PSYCHIATRY, Adult psychiatry, Schizophrenia & psychotic disorders, MENTAL HEALTH
Strengths and limitations of this study.
A 26-week, double-blinded, randomised, parallel-group, placebo-controlled, good clinical practice-monitored, multicentre trial has been chosen in accordance with the trial objectives.
This study will evaluate the effects of add-on therapy of early glucagon-like peptide 1 (GLP-1) receptor agonist (semaglutide) intervention to dysglycaemic clozapine-treated or olanzapine-treated patients diagnosed with a schizophrenia spectrum disorder.
The viability of GLP-1 injection treatment will be determined by an assessment of the patients’ adherence to self-administration once a week.
Lack of rescue medication may cause more patients to be excluded from the placebo arm compared with the active arm during the trial period.
The 26-week trial period could limit exploring the full potential of the treatment.
Introduction
Background and rationale
Schizophrenia is a mental disorder with a heterogeneous genetic and neurobiological aetiology, affecting approximately 1% of the general population.1 Patients with schizophrenia have a shorter life expectancy of 10–15 years compared with the general population.2–6 This excess mortality is largely explained by a high prevalence of obesity, metabolic disturbances, type 2 diabetes and cardiovascular diseases.4 7–11
Researchers have suggested that glucose homeostasis is altered in patients with schizophrenia from illness onset, indicating that this group of patients may be at increased risk of developing impaired glucose homeostasis and type 2 diabetes.12–14 This risk could be further aggravated as a consequence of a high prevalence of a sedentary lifestyle, low physical activity, dietary risk, smoking and reduced access to adequate healthcare in patients with schizophrenia.15–19 Antipsychotic medications play a central role in the treatment of schizophrenia, but, unfortunately, several antipsychotics are also associated with body weight increase and the development of metabolic disturbances including pre-diabetes and type 2 diabetes.20–22 The two antipsychotics olanzapine and clozapine are quite efficacious,23 but regrettably, olanzapine and clozapine confer the highest risk of inducing weight gain and metabolic disturbances, including pre-diabetes compared with other psychotropic medications.8 20 23–25 The weight gain after clozapine initiation is on average 5 kg within the first 12 weeks of treatment.20 26 27 Clozapine is associated with long-term weight gain even though the risk of weight gain appears to be highest in the initial treatment period.28 29 The manifestation of type 2 diabetes in this group of patients follows a similar trend, with around 10% of those receiving clozapine developing the condition within the first year of treatment, approximately 35% within the first 10 years, and nearly 45% within the first 21 years of treatment.30 31
Body weight loss and improvements in metabolic disturbances can be achieved by switching to more weight-neutral antipsychotic medication.32 33 However, both olanzapine and clozapine are potent treatments for schizophrenia, with clozapine as the recommended choice for treatment-resistant schizophrenia.34–37 Due to the efficacy of the compound in otherwise partial or fully treatment-resistant patients, switching to another antipsychotic is often not possible without worsening psychotic symptoms.38 Despite the adverse effects, long-term antipsychotic treatment is associated with decreased all-cause mortality compared with non-use of antipsychotic drugs,11 39 40 and clozapine is associated with the lowest all-cause mortality compared with other antipsychotic drugs.11 39 This may be the outcome of improved control of psychiatric symptoms due to antipsychotic use, which promotes secondary prevention as a healthier lifestyle and more frequent use of care services for physical illness.39 41
Previously, limited effects have been demonstrated for counteracting antipsychotic-induced body weight gain and metabolic disturbances with non-pharmacological/behavioural interventions42–51 and adjunct pharmacological treatments.51–60 Several meta-analyses conclude evidence in favour of topiramate and metformin as adjunct pharmacological treatment51–53 61 while individual lifestyle counselling is found to be the most effective non-pharmacological intervention for weight reduction.51
Growing evidence suggests a potential benefit of adjunct pharmacological treatment with glucagon-like peptide 1 (GLP-1) glucagon-like peptide 1 receptor agonists (GLP-1RAs).62 GLP-1 is an incretin hormone secreted from the L cells in the intestinal mucosa in response to nutrients.63 GLP-1 stimulates insulin secretion and inhibits glucagon secretion, thereby lowering plasma glucose levels.63 Both effects are strictly glucose-dependent (more pronounced at higher levels of plasma glucose), and the effects cease as the level of plasma glucose reaches values below 4–5 mmol/L. Thus, the GLP-1RA keeps plasma glucose concentrations at lower levels without increasing the risk of hypoglycaemia.63 Additional effects include decreased gastric emptying, increased satiety, and decreased appetite and food intake leading to body weight loss63 with reduction of fat mass, android fat, trunk fat and lean body mass.64 65 Furthermore, recent data suggest that GLP-1RAs have beneficial effects on bone structure,66–68 and large-scale cardiovascular outcome trials have shown beneficial effects of GLP-1RAs on major adverse cardiovascular events in patients with type 2 diabetes at high risk of CVD.69–71 Currently, several studies have been conducted to investigate if these beneficial findings could be extended to the psychiatric population receiving antipsychotic medications.62 72–75 Our group previously reported that subcutaneous treatment for 16 weeks with the GLP-1RA liraglutide as adjunctive treatment to clozapine or olanzapine in patients with schizophrenia-spectrum disorder with pre-diabetes improved glycated haemoglobin A1c (HbA1c) with approximately 0.2% (2.3 mmol/mol) glucose tolerance, and several other cardiometabolic disturbances and induced a 5.3 kg body weight loss compared with placebo.76 Recent meta-analyses have reported that GLP-1RAs are effective and tolerable for managing antipsychotic-associated body weight gain,77 especially for clozapine/olanzapine-treated patients.62 However, studies involving a large number of participants and longer treatment duration are needed in order to replicate the results.78 79 Future research should focus on GLP-1RAs with an extended half-life as they allow subcutaneous administration once a week as opposed to short-acting GLP-1RAs like liraglutide, which requires daily subcutaneous administration. Furthermore, results have indicated that this newer group of GLP-1RAs is more effective.80
We will perform a clinical study with semaglutide (Ozempic), a GLP-1RA with an extended half-life of approximately 1 week, which permits once weekly subcutaneous administration. Ozempic 1.0 mg once a week was approved for the treatment of type 2 diabetes by the US Food and Drug Administration (FDA) in 2017 and the European Medicines Agency (EMA) in 2018. This trial will include a large number of participants, a long treatment duration and a novel GLP-1RA with a more potent efficacy, and an extended half-life expected to increase clinical outcomes.
Hypothesis
We hypothesise that add-on therapy with semaglutide once a week in dysglycaemic patients diagnosed with a schizophrenia spectrum disorder who initiated treatment with clozapine or olanzapine within 60 months, will improve overall glycaemic control and mitigate the antipsychotic-induced metabolic disturbances.
Objective and endpoints
This study was designed to evaluate the effects of 1.0 mg semaglutide once a week on the metabolic state in dysglycaemic patients diagnosed with a schizophrenia spectrum disorder, who initiated treatment with clozapine or olanzapine up to 60 months prior to inclusion. The primary endpoint is the change from baseline in HbA1c. For secondary endpoints, see box 1.
Box 1. Endpoints.
Primary endpoint
Glycated haemoglobin A1c.
Secondary endpoints
Body weight, hip and waist circumference.
Vitals signs (blood pressure and pulse).
Peptide hormones (insulin, C-peptide and glucagon).
Insulin sensitivity and beta cell function (evaluated by homeostatic model assessment).
Lipid profile (low-density lipoprotein, high-density lipoprotein, triglycerides and cholesterol).
Hepatic function and fibrosis-4 score (thrombocytes, alanine aminotransferase, aspartate aminotransferase, alkaline phosphatase and bilirubin).
Incretin hormones (glucagon-like peptide 1, glucagon-like peptide 2 and glucose-dependent insulinotropic polypeptide).
Bone markers (vitamin D, calcium, phosphate, magnesium, parathyroid hormone, procollagen type 1 N-terminal propeptide, C-terminal telopeptide of type 1 collagen and osteocalcin).
Body composition and bone density (dual-energy X-ray absorption scan).
Psychopathology (Positive and Negative Syndrome Scale–Six Items, Clinical Global Impression Severity Scale), psychosocial disability (Cognitive Test and the Global Assessment of Psychosocial Disability Scale) and quality of life (Schizophrenia Quality of Life Scale).
Reward value of sweet–fat stimulus (clicker test).
Activity measurements (wearable activity device).
Alcohol, drug and tobacco use (Alcohol Use Disorders Identification Test, Drug Use Disorders Identification Test and Fagerström Test for Nicotine Dependence).
Proteomic analyses and measurement of oxidative stress.
Methods and analysis
Trial design, setting and timeline
This trial is a 26week investigator-initiated, double-blinded, randomised, two-arm, parallel group, multicentre, good clinical practice (GCP)-monitored, and placebo-controlled study. All clinical visits will be conducted by investigators at Psychiatric Centre Copenhagen (PCK), Denmark; Psychiatric Centre Nordsjaelland (PCN), Denmark; and Aarhus University Hospital–Psychiatry (AUHP), Aarhus, Denmark, with PCK as the coordinating centre. It is the responsibility of the sponsor–investigator to inform sites of the terms and conditions of the protocol. All investigators will be trained in the study requirements, standardised clinical measurements and requirements for laboratory specimen collection including urine samples, counselling for adherence, and the eliciting of information from study participants in a uniform reproducible manner. Patient recruitment was initiated in September 2021. The number of patients to be included is 104. It is expected that PCK, PCN and AUHP will include 74, 10 and 20 patients, respectively. Initial and final visits will be performed at PCK and AUHP only. The study is expected to be completed in 2024.
Study population
Pre-diabetic and diabetic patients diagnosed with a schizophrenia spectrum disorder according to the criteria of the International Classification of Diseases, 10th Revision, WHO or the Diagnostic and Statistical Manual of Mental Disorders (Fifth Edition, the American Psychiatric Association) who initiated treatment with clozapine or olanzapine within the last 60 months and who can comply with the requirements for participation in the study (box 2) will be included.
Box 2. Eligibility criteria.
Inclusion criteria
Informed oral and written consent.
Diagnosed with a schizophrenia spectrum disorder according to the criteria of International Classification of Diseases, 10th Revision, or the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition.
Age 18–65 years (both included)
Body mass index of ≥25 kg/m2.
Diagnosed with pre-diabetes or type 2 diabetes, with the following plasma levels: pre-diabetes: HbA1c 35–47 mmol/mol (5.4%–6.4%) or type 2 diabetes: HbA1c 48–57 mmol/mol (6.5%–7.4%).
Exclusion criteria
Acute worsening of psychosis based on a clinical evaluation (score of 6 or 7 on the Clinical Global Impression Severity Scale).
Coercive measures.
Women of childbearing potential who are pregnant, breastfeeding or have the intention of becoming pregnant.
Women who are not willing to use an adequate contraceptive during the full length of the study.
Patients treated with corticosteroids or other hormone therapy (except oestrogens).
Any active substance abuse or dependence (except for nicotine).
Impaired hepatic function (plasma liver transaminases >2 times upper normal limit).
Impaired renal function (serum creatinine>150 µmol/L).
Impaired pancreatic function (acute or chronic pancreatitis and/or plasma amylase >2 times upper normal limit).
Cardiac problems defined as decompensated heart failure (New York Heart Association class III/IV), unstable angina pectoris and/or myocardial infarction within the last 12 months.
Hypertension with systolic blood pressure of >180 mm Hg or diastolic blood pressure of >100 mm Hg.
Any condition that the investigator feels would interfere with trial participation.
Receiving any experimental or premarketing drug within the last 3 months.
Use of diabetes medication or weight-lowering pharmacotherapy within the last 3 months.
Known type 1 diabetes.
Suicidal behaviour as judged by the investigator and based on clinical evaluation.
Plasma HbA1c of >57 mmol/mol (7.4%) (tested twice), in which case the patient will be excluded from the study.
Any known contraindication towards the treatment with semaglutide.
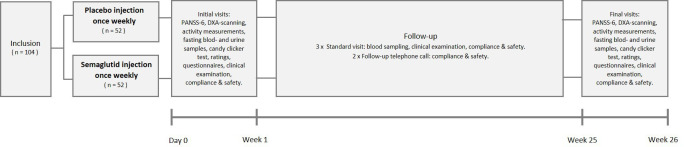
The planned number of patients to be screened, that is, documented informed consent, is 125 (expected screen failure rate: up to 20%). The number of patients to be included, randomised and started on semaglutid or placebo is 104. The number of patients expected to complete the trial is 52, with 26 in each arm (figure 1). The patients will be recruited via one of the psychiatric centres in the Capital Region of Copenhagen involved in the study; PCK, Psychiatric Centre Glostrup, Psychiatric Centre Ballerup (PCB), and Psychiatric Centre Amager (PCA), PCN or from AUHP, Central Denmark Region. The expected number of dropouts is difficult to estimate. In a recent study in patients diagnosed with a schizophrenia spectrum disorder and in stable treatment with clozapine or olanzapine receiving daily subcutaneous injections of the GLP-1RA liraglutide or placebo over a 16 week trial period, we had a drop-out rate of approximately 7%.76 We expect the study withdrawal to be higher in the present, longer-lasting study in patients that have more recently, that is, within 60 months, initiated treatment with clozapine or olanzapine. Consequently, we expect a drop-out rate of up to 50% in our study population over the 26-week trial period. If the drop-out rate should turn out to be higher than 50%, more patients will be included to reach the goal of 52 patients completing the study. In that case, a change in sample size will be documented in a substantial protocol amendment.
Figure 1.
Study flowvhart. The number of patients to be randomised and assigned to one of two treatment arms, on 1.0 mg semaglutide or matching placebo once a weel is 104, with an expected drop-out rate of up to 50% for the 26-week trial period. DXA, dual-energy X-ray absorption; PANSS-6, Positive and Negative Syndrome Scale–Six Items.
Recruitment, inclusion and randomisation
To expand the knowledge about the project, we will contact psychiatrists and other employees working at the participating psychiatric departments with project information and ask them to have our recruitment folder and poster in their waiting room or at their noticeboard. Furthermore, a short notice with information about the study will appear in the medical journal system when a doctor prescribes either olanzapine or clozapine to a patient at one of the participating psychiatric centres. The participating psychiatric centres will provide the following data (from the medical record system) regarding patients diagnosed with a schizophrenia spectrum disorder who initiated treatment with clozapine or olanzapine within 60 months: name, social security number, contact information, diagnosis, HbA1c, body mass index (BMI), medication record, name of the primary psychiatrist and psychiatric department. Patients meeting inclusion criteria will be informed about the possibility of participating in this study after permission to be contacted has been obtained from the treating psychiatrist. Before any trial-related procedures are performed, patients will be thoroughly informed about the study and sign an informed consent form (online supplemental material 1). All patients will receive oral and written information about the trial, including the most common adverse events, and the procedures involved in the study. Patients will have the opportunity to ask questions and have up to 48 hours to consider participation. A pretreatment evaluation will be conducted to screen patients according to the inclusion and exclusion criteria (box 2). When a patient is included in the study, the patients will be block-randomised into two groups. The randomisation will be stratified by age (two levels) and sex (two levels). The supplier of semaglutide pens (Novo Nordisk A/S) will provide a subject randomisation list (SRL) for randomisation purposes. The SRL will come in two versions: one blinded version for the appointed blinded investigators responsible for randomisation and one unblinded version for the unblinded staff who handle the trial product. Novo Nordisk A/S will be responsible for labelling and blinding the semaglutide and placebo pens. A total dispensing unit number list (TDL) will be provided by Novo Nordisk A/S for the purpose of selecting dispensing units/pens containing the assigned treatment. The unblinded SRL and the TDL are only accessed and handled by appointed unblinded staff and will be uploaded in a separate randomisation module of the Research Electronic Data Capture (REDCap) program with no access for blinded staff. Via REDCap it will be possible for the blinded staff to automatically assign enrolled patients to the respective intervention via the blinded SRL. Unblinded staff will handle the dispensing of project medicine with double data entry to ensure integrity. Unblinded staff will not participate in any other parts of the trial.
bmjopen-2022-068652supp002.pdf (62.8KB, pdf)
Treatment protocol
The total trial duration is 26 weeks for each patient (table 1). The patients will receive blinded treatment in one of the two study arms: injection with 1.0 mg semaglutide or placebo once a week. Every 4 weeks, each patient will attend regular visits throughout the trial or be assessed by phone to evaluate adverse effects, and adherence to trial medication, and participate in testing with standard blood sampling (box 3) and a clinical examination (table 1).
Table 1.
Treatment procedures
| Screening | Inclusion (day 0) | Week 1 | Week 4 | Week 8 | Week 12 | Week 16 | Week 20 | Week 25 | Week 26 | |
| Introduction, informed consent, screening | X | |||||||||
| Height | X | X | X | |||||||
| Hip and waist circumference | X | X | X | X | X | |||||
| Body weight | X | X | X | X | X | X | ||||
| Blood pressure and heart rate | X | X | X | X | X | X | ||||
| Clinical evaluation of suicide risk | X | X | X | X | X | X | ||||
| Standard blood sampling and safety markers | X | X | X | X | ||||||
| Fasting blood and urine samples | X | X | ||||||||
| The Schizophrenia Quality of Life Scale | X | X | ||||||||
| Clinical Global Impression Severity | X | X | ||||||||
| Global Assessment of Psychosocial Disability | X | X | ||||||||
| Alcohol Use Disorders Identification Test | X | X | ||||||||
| Drug Use Disorders Identification Test | X | X | ||||||||
| Fagerström Test for Nicotine Dependence | X | X | ||||||||
| Clicker test | X | X | ||||||||
| Positive and Negative Syndrome Scale | X | X | ||||||||
| DXA scanning | X | X | ||||||||
| Activity device distributed | X | X | ||||||||
| Activity device collected | X | X | ||||||||
| Drug dispensing/returned | X | X | X | X | X | X | ||||
| Adherence/practice study treatment self-administration | X | X | X | X | X | X | X | X | X | |
| Adverse event assessment | X | X | X | X | X | X | X | X | X | |
| Follow-up by phone call | X | X |
DXA scan will be performed at baseline and at the termination of study participation. Activity measurements will be collected continuously during the first (week 1) and last week of participation (week 26) by using a wearable activity device91–93 (table 1). At baseline and the last visit, potential effects on the reward value of a sweet–fat stimulus will be examined using a progressive ratio task ‘clicker test’,94 a Positive and Negative Syndrome Scale–Six Items interview95 will be performed, and fasting blood and urine samples will be collected (box 3).
DXA, dual-energy X-ray absorption.
Box 3. Blood and urine analyses.
Standard blood sampling
Glycated haemoglobin A1c, glucose, insulin, C-peptide, thrombocytes, alanine aminotransferase, aspartate aminotransferase, alkaline phosphatase and bilirubin.
Fasting blood sampling
Glucagon-like peptide 1, glucagon-like peptide 2, glucose-dependent insulinotropic polypeptide, glucagon, vitamin D, calcium, phosphate, magnesium, parathyroid hormone, procollagen type 1 N-terminal propeptide, C-terminal telopeptide of type 1 collagen, osteocalcin, low-density liprotein, high-density lipoprotein, triglycerides, cholesterol, amylase, creatinine, sodium, potassium, semaglutide and proteomic analyses.
Fasting urine sampling
DNA and RNA oxidative stress biomarkers.
In addition, all patients will be evaluated on the following rating scales and questionnaires: Schizophrenia Quality of Life Scale,81 Clinical Global Impression Severity Scale (CGI-S),82 Alcohol Use Disorders Identification Test,83 Drug Use Disorders Identification Test,84 Fagerström Test for Nicotine Dependence85 and the Global Assessment of Psychosocial Disability86 scale. Women not willing to use an adequate contraceptive during the full length of the study will be excluded. Women with childbearing potential will have a pregnancy test (ie, beta-human chorionic gonadotropin) performed before inclusion or if any suspicion of pregnancy arises during the study. If a patient gives informed consent to participate in future ancillary studies, extra material (serum/plasma/urine) will be stored in a biobank for possible future further analyses at the inclusion and final visit. In this case, new approval by the regional health research ethics committee is required. Due to the time frame of the project, patients’ study-related travel expenses will be covered. Investigators will ensure that patients are covered by insurance via the hospital during study participation.
Patient withdrawal
Patients are free to withdraw from the trial at any time without providing reason(s) for withdrawal and without prejudice to further treatment. The reason for withdrawal may be withdrawal of consent, discontinuation of clozapine/olanzapine, failure to maintain a present level of adherence with the clinical trial medication, that is, missing more than three consecutive injections or more than 12 injections in total, adverse event(s), pregnancy discovered during the trial, significant worsening of mental health (defined as a Clinical Global Impression–Improvement score of 6 or 7) or an HbA1c higher than 57 mmol/mol (7.4%). No rescue medication will be offered in this study. Dropouts will be replaced until 52 patients have completed the treatment period. Data from dropouts will be included in the data processing. Patients withdrawing from the trial should be encouraged to undergo the same final evaluations as patients completing the trial. Completion or trial termination for any reason will be fully documented in the clinical record form pages. The supplier of pens will provide emergency sealed codes for ‘emergency breaking only’. In case of emergencies, it is possible for the investigators to reveal treatment based on study ID, that is, to collect information about the specific patient without breaking all randomisation codes.
Intervention and choice of comparator
Participants will be randomly assigned to semaglutide (semaglutide 1.34 mg/mL, 1.5 mL prefilled pen-injector) or placebo (no active drug) administered in the same way and volume. The trial medication is administered subcutaneously once a week in the entire treatment period; days 1–28: 0.25 mg semaglutide/placebo, days 29–56: 0.5 mg semaglutide/placebo and days 57–182: 1.0 mg semaglutide/placebo). Patients who, due to adverse events, do not tolerate uptitration to 1.0 mg semaglutide will remain on 0.5 mg once a week. Patients who, due to adverse events, cannot tolerate dose escalation to 0.5 mg semaglutide/placebo will be excluded from the study. The patients will be instructed in the subcutaneous injection technique, which can be performed at home. If the patient cannot self-inject, a contact person will assist. Adherence and adverse events will be noted during the entire treatment period. For each patient treated, the batch number of the pen must be documented, and the patients will be asked to return the pens after usage. Patients will be asked to complete a weekly injection diary. If the patient accepts, they will receive a reminder of injections days and scheduled study visits. The importance of following study guidelines for adherence to weekly injections will be emphasised to all patients, and there will be a brief discussion of reasons for possibly missed doses and simple strategies for enhancing adherence. At the termination of study, levels of plasma-semaglutide will be assessed for adherence.
Sample size
The study is an explanatory study and the required patient population size is based on significance level (α) of 5%, a power (1−β) of 90%, where β (10%) is the risk of accepting a hypothesis that is false. Based on data from a recent study in similar patients,76 we estimated that the minimum relevant difference (MIREDIF) of HbA1c (primary endpoint) after 26 weeks of intervention would be −0.26% with an SD of 0.28%. With the aforementioned power, significance level, MIREDIF and SD, the trial requires 26 patients in each of the two arms, that is, a total of 52 patients. Thus, with an expected dropout of 50%, a total of 104 patients will be randomised.
Data management and statistical analysis
All data will be collected in electronic case report forms in REDCap hosted in the Capital Region of Denmark. The database will be locked after the last participants’ end of study. The sponsor–investigator has the final decision to terminate the trial. All statistical analyses except the post hoc sensitivity analyses will be performed with treatment groups still blinded. Before dividing participants into two groups, the statistical analysis plan will be uploaded at clinicaltrials.gov and the dataset will be locked. Statistical analyses will be performed using R (http://www.R-project.org/), with alpha set at 0.05. Statistical tests will be two-sided, and the level of significance will be 5%. All efficacy and safety analyses will be performed using a modified intention-to-treat principle in which all randomised participants who received at least one dose of the trial compound and have at least one assessment after baseline will be included. For the primary endpoint, repeated mixed-model analysis of covariance will be used to analyse change in the level of HbA1c from week 0 to week 26 for the semaglutide once a week and the placebo groups. All changes in secondary endpoints from baseline to the end of the trial will be analysed using repeated mixed-model analyses for continuous outcomes and mixed-model logistic regression for categorical outcomes. For comparison between the two groups, the covariates of age, sex, illness duration, treatment group, baseline CGI-S score and BMI will be included in the analyses together with the baseline value of the relevant variable. Effect sizes (Cohen d) for lowering HbA1c levels and reducing body weight will be calculated by dividing the difference of the means in change from baseline to endpoint (treatment−placebo) by the pooled SD.
Public involvement and data availability
No members of the public or patients were involved in the research question, the design, the conduct of the research. Following publication, researchers who provide a methodological sound proposal can request access to the trial dataset.
Ethics and dissemination
We expect that the present study will generate important information about the long-term effects of continuous-acting GLP-1RA as an add-on therapy for dysglycaemic patients treated with clozapine and olanzapine. Patients are included in this study within the first 5 years of initiating clozapine or olanzapine treatment if they have developed pre-diabetes or diabetes. Clozapine-induced metabolic changes can be observed within the first years after initiation of treatment,30 which is why we are exploring an GLP-1RA as a choice for early treatment of antipsychotic-induced metabolic changes. This study is not considered as posing ethical problems. Semaglutide once a week is approved for the treatment of type 2 diabetes, obesity and overweight in the presence of weight-related comorbidity by EMA and by the FDA. The treatment in this study is associated with minimal discomfort for the participating patients. Procedures include blood sample collection, and a weekly injection of semaglutide in the subcutis of the abdomen, thigh, or upper arm. At the two DXA scans, participants will be exposed to modest radiation of app, 0.01 mSv, corresponding to two to three times the dosage of a dental X-ray.87 It is painless and no adverse effects are expected.
Investigators will be given access to the cleaned datasets. At the end of the trial, one or more manuscripts will be prepared for publication in international scientific journals. Data will be processed and merged into one or more scientific articles and published in accordance with the Consolidated Standards of Reporting Trials 2010 statement in international, peer-reviewed scientific journals and presented at national and international scientific meetings. We will seek to publish both positive and negative results. While it is the intention that the sponsor–investigator will be the last author, the published international guidelines for authorship (International Committee of Medical Journal Editors, 1997) will be adhered to.88
Protocol, study approval and registration
The Standard Protocol Items: Recommendations for Interventional Trials (SPIRIT) guidelines were used as guidance for writing the protocol.89 The protocol and amendments are approved by the Danish Medicines Agency (EudraCT: 2020-000102-28) and the Regional Scientific Ethics Committee of the Capital Region of Denmark (committee C, #H-20019008). See online supplemental appendix A for further details. All data will be handled according to the General Data Protection Regulation. A detailed plan for curation has been approved by The Capital Region of Denmark. The investigators will ensure that the study will be carried out according to International Council for Harmonisation Good Clinical Practice (ICH-GCP) guidelines and the Helsinki Declaration90 and with national laws and regulations for clinical research. The study and a data sharing plan has been registered at ClinicalTrials.gov. In the process of ensuring data completeness and accuracy, source data verification will be performed by the GCP unit of Copenhagen University. The participants will be informed in writing about the possibility of audits and/or inspections. The audit and/or inspection might be performed by the hospital institutional review board/ethics committee or regulatory authority.
bmjopen-2022-068652supp001.pdf (83.9KB, pdf)
The status of the study is active recruitment of patients according to the approved protocol version, 9.0, 02.12.22.
Supplementary Material
Acknowledgments
We thank the participating Psychiatric Centers: Copenhagen, Glostrup, Ballerup, Amager, Nordsjaelland, Slagelse and Aarhus University Hospital, Psychiatry, for their cooperation in planning and participating in the design of this study.
Footnotes
Twitter: @Filip_Knop
Contributors: AF-J and TV conceived the study. AF-J, TV, MRS, HS, FKK, JN, CUC, CE, AAD, OK-F, OM, MØN, AMS and MV initiated the study design and helped with implementation. AF-J is grant holder. MRS, TV and AF-J has drafted the manuscript. All authors contributed to the refinement of the study protocol and this manuscript.
Funding: This work was supported by an unrestricted research grant from Novo Nordisk A/S (including trial medication) and by Mental Health Services, Capital Region of Denmark (PhD salary). The study is an independent investigator-initiated and university-initiated study. The funding source will not have any role during its execution, analyses, interpretation of the data or decision to submit results. If protocol changes are made that can affect the study objectives, Novo Nordisk A/S must be informed and allowed to consider their continued support of the study. Sponsor–investigator must provide Novo Nordisk A/S with a copy of a proposed publication or disclosure containing data or results before submission to enable Novo Nordisk to make a review for medical accuracy and confidentiality. The Novo Nordisk Foundation (NNF21OC0068402), The Lundbeck Foundation, The P. Carlsen Foundation (21003) and The Dagmar Marshalls Foundation supported the project with scholarship grants.
Competing interests: AFJ received an unrestricted research grant from Novo Nordisk A/S for the present clinical study. TV served on scientific advisory panels and/or speaker's bureaus for Amgen, AstraZeneca, Boehringer Ingelheim, Bristol-Myers Squibb, Eli Lilly, Gilead, GSK, Merck Sharp & Dohme, Mundipharma, Novo Nordisk, Sanofi and Sun Pharma. TV served as a consultant to and/or received research support from Amgen, AstraZeneca, Boehringer Ingelheim, Bristol-Myers Squibb, Eli Lilly, Gilead, GSK, Merck Sharp & Dohme, Mundipharma, Novo Nordisk, Sanofi and Sun Pharma. HS served on scientific advisory panels for Boehringer Ingelheim and Novo Nordisk. CUC has been a consultant and/or advisor to or has received honoraria from AbbVie, Acadia, Alkermes, Allergan, Angelini, Aristo, Boehringer-Ingelheim, Cardio Diagnostics, Cerevel, CNX Therapeutics, Compass Pathways, Darnitsa, Gedeon Richter, Hikma, Holmusk, IntraCellular Therapies, Janssen/J&J, Karuna, LB Pharma, Lundbeck, MedAvante-ProPhase, MedInCell, Merck, Mindpax, Mitsubishi Tanabe Pharma, Mylan, Neurocrine, Newron, Noven, Otsuka, Pharmabrain, PPD Biotech, Recordati, Relmada, Reviva, Rovi, Seqirus, SK Life Science, Sunovion, Sun Pharma, Supernus, Takeda, Teva and Viatris. He provided expert testimony for Janssen and Otsuka. He served on a Data Safety Monitoring Board for Lundbeck, Relmada, Reviva, Rovi, Supernus, and Teva. He has received grant support from Janssen and Takeda. He received royalties from UpToDate and is also a stock option holder of Cardio Diagnostics, Mindpax, LB Pharma and Quantic. OKF reports speaker fees for Lundbeck Pharma A/S and consultant work for WCG Clinical. FKK served on scientific advisory panels and/or been part of speaker’s bureaus for, served as a consultant to and/or received research support from Amgen, AstraZeneca, Boehringer Ingelheim, Eli Lilly, MSD/Merck, Mundipharma, Norgine, Novo Nordisk, Sanofi and Zealand Pharma. MV received consultancy fees from Lundbeck and Janssen-Cilag. AAD received a speaker honorarium from Otsuka Pharmaceutical. MRS has nothing to disclose. Novo Nordisk A/S commented on the study design but will not influence trial conduction, data analysis, interpretation or publication. All data are owned by the authors, who all have full data access.
Patient and public involvement: Patients and/or the public were not involved in the design, conduct, reporting or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Ethics statements
Patient consent for publication
Not applicable.
References
- 1.Kahn RS, Sommer IE, Murray RM, et al. Schizophrenia. Nat Rev Dis Primers 2015;1:15067. 10.1038/nrdp.2015.67 [DOI] [PubMed] [Google Scholar]
- 2.Lawrence D, Hancock KJ, Kisely S. The gap in life expectancy from preventable physical illness in psychiatric patients in Western Australia: retrospective analysis of population based registers. BMJ 2013;346:f2539. 10.1136/bmj.f2539 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Saha S, Chant D, McGrath J. A systematic review of mortality in schizophrenia: is the differential mortality gap worsening over time? Arch Gen Psychiatry 2007;64:1123–31. 10.1001/archpsyc.64.10.1123 [DOI] [PubMed] [Google Scholar]
- 4.Laursen TM, Munk-Olsen T, Vestergaard M. Life expectancy and cardiovascular mortality in persons with schizophrenia. Curr Opin Psychiatry 2012;25:83–8. 10.1097/YCO.0b013e32835035ca [DOI] [PubMed] [Google Scholar]
- 5.Plana-Ripoll O, Pedersen CB, Agerbo E, et al. A comprehensive analysis of mortality-related health metrics associated with mental disorders: a nationwide, register-based cohort study. Lancet 2019;394:1827–35. 10.1016/S0140-6736(19)32316-5 [DOI] [PubMed] [Google Scholar]
- 6.Walker ER, McGee RE, Druss BG. Mortality in mental disorders and global disease burden implications: a systematic review and meta-analysis. JAMA Psychiatry 2015;72:334–41. 10.1001/jamapsychiatry.2014.2502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hennekens CH, Hennekens AR, Hollar D, et al. Schizophrenia and increased risks of cardiovascular disease. Am Heart J 2005;150:1115–21. 10.1016/j.ahj.2005.02.007 [DOI] [PubMed] [Google Scholar]
- 8.Henderson DC, Vincenzi B, Andrea NV, et al. Pathophysiological mechanisms of increased cardiometabolic risk in people with schizophrenia and other severe mental illnesses. Lancet Psychiatry 2015;2:452–64. 10.1016/S2215-0366(15)00115-7 [DOI] [PubMed] [Google Scholar]
- 9.Larsen JR, Svensson CK, Vedtofte L, et al. High prevalence of prediabetes and metabolic abnormalities in overweight or obese schizophrenia patients treated with clozapine or olanzapine. CNS Spectr 2019;24:441–52. 10.1017/S1092852918001311 [DOI] [PubMed] [Google Scholar]
- 10.Hayes JF, Marston L, Walters K, et al. Mortality gap for people with bipolar disorder and schizophrenia: UK-based cohort study 2000-2014. Br J Psychiatry 2017;211:175–81. 10.1192/bjp.bp.117.202606 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Correll CU, Solmi M, Croatto G, et al. Mortality in people with schizophrenia: a systematic review and meta-analysis of relative risk and aggravating or attenuating factors. World Psychiatry 2022;21:248–71. 10.1002/wps.20994 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pillinger T, Beck K, Gobjila C, et al. Impaired glucose homeostasis in first-episode schizophrenia: a systematic review and meta-analysis. JAMA Psychiatry 2019;74:261–9. 10.1001/jamapsychiatry.2016.3803 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Perry BI, McIntosh G, Weich S, et al. The association between first-episode psychosis and abnormal glycaemic control: systematic review and meta-analysis. Lancet Psychiatry 2016;3:1049–58. 10.1016/S2215-0366(16)30262-0 [DOI] [PubMed] [Google Scholar]
- 14.Steiner J, Berger M, Guest PC, et al. Assessment of insulin resistance among drug-naive patients with first-episode schizophrenia in the context of hormonal stress axis activation. JAMA Psychiatry 2017;74:968–70. 10.1001/jamapsychiatry.2017.1983 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vancampfort D, Firth J, Schuch FB, et al. Sedentary behavior and physical activity levels in people with schizophrenia, bipolar disorder and major depressive disorder: a global systematic review and meta-analysis. World Psychiatry 2017;16:308–15. 10.1002/wps.20458 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Firth J, Siddiqi N, Koyanagi A, et al. A blueprint for protecting physical health in people with mental illness the lancet psychiatry commission part 1: physical health disparities for people with mental illness. Lancet Psychiatry 2019;6:675–712. 10.1016/S2215-0366(19)30132-4 [DOI] [PubMed] [Google Scholar]
- 17.Thornicroft G. Physical health disparities and mental illness: the scandal of premature mortality. Br J Psychiatry 2011;199:441–2. 10.1192/bjp.bp.111.092718 [DOI] [PubMed] [Google Scholar]
- 18.McCreadie RG, Scottish Schizophrenia Lifestyle Group . Diet, smoking and cardiovascular risk in people with schizophrenia: descriptive study. Br J Psychiatry 2003;183:534–9. 10.1192/bjp.183.6.534 [DOI] [PubMed] [Google Scholar]
- 19.Mitchell AJ, Malone D, Doebbeling CC. Quality of medical care for people with and without comorbid mental illness and substance misuse: systematic review of comparative studies. Br J Psychiatry 2009;194:491–9. 10.1192/bjp.bp.107.045732 [DOI] [PubMed] [Google Scholar]
- 20.Allison DB, Mentore JL, Heo M, et al. Antipsychotic-Induced weight gain: a comprehensive research synthesis. Am J Psychiatry 1999;156:1686–96. 10.1176/ajp.156.11.1686 [DOI] [PubMed] [Google Scholar]
- 21.Correll CU, Lencz T, Malhotra AK. Antipsychotic drugs and obesity. Trends Mol Med 2011;17:97–107. 10.1016/j.molmed.2010.10.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pillinger T, McCutcheon RA, Vano L, et al. Comparative effects of 18 antipsychotics on metabolic function in patients with schizophrenia, predictors of metabolic dysregulation, and association with psychopathology: a systematic review and network meta-analysis. Lancet Psychiatry 2020;7:64–77. 10.1016/S2215-0366(19)30416-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Huhn M, Nikolakopoulou A, Schneider-Thoma J, et al. Comparative efficacy and tolerability of 32 oral antipsychotics for the acute treatment of adults with multi-episode schizophrenia: a systematic review and network meta-analysis. Lancet 2019;394:939–51. 10.1016/S0140-6736(19)31135-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.De Hert M, Detraux J, van Winkel R, et al. Metabolic and cardiovascular adverse effects associated with antipsychotic drugs. Nat Rev Endocrinol 2011;8:114–26. 10.1038/nrendo.2011.156 [DOI] [PubMed] [Google Scholar]
- 25.Masuda T, Misawa F, Takase M, et al. Association with hospitalization and all-cause discontinuation among patients with schizophrenia on clozapine vs other oral second-generation antipsychotics: a systematic review and meta-analysis of cohort studies. JAMA Psychiatry 2019;76:1052–62. 10.1001/jamapsychiatry.2019.1702 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Leadbetter R, Shutty M, Pavalonis D, et al. Clozapine-induced weight gain: prevalence and clinical relevance. Am J Psychiatry 1992;149:68–72. 10.1176/ajp.149.1.68 [DOI] [PubMed] [Google Scholar]
- 27.Bobo WV, Jayathilake K, Lee MA, et al. Changes in weight and body mass index during treatment with melperone, clozapine and typical neuroleptics. Psychiatry Res 2010;176:114–9. 10.1016/j.psychres.2009.03.026 [DOI] [PubMed] [Google Scholar]
- 28.Bai Y-M, Chen J-Y, Chen T-T, et al. Weight gain with clozapine: 8-year cohort naturalistic study among hospitalized chinese schizophrenia patients. Schizophr Res 2009;108:122–6. 10.1016/j.schres.2008.10.023 [DOI] [PubMed] [Google Scholar]
- 29.Pai N, Deng C, Vella S-L, et al. Are there different neural mechanisms responsible for three stages of weight gain development in anti-psychotic therapy: temporally based hypothesis. Asian J Psychiatr 2012;5:315–8. 10.1016/j.ajp.2012.05.005 [DOI] [PubMed] [Google Scholar]
- 30.Henderson DC, Cagliero E, Gray C, et al. Clozapine, diabetes mellitus, weight gain, and lipid abnormalities: a five-year naturalistic study. Am J Psychiatry 2000;157:975–81. 10.1176/appi.ajp.157.6.975 [DOI] [PubMed] [Google Scholar]
- 31.Nemani KL, Greene MC, Ulloa M, et al. Clozapine, diabetes mellitus, cardiovascular risk and mortality: results of a 21-year naturalistic study in patients with schizophrenia and schizoaffective disorder. Clin Schizophr Relat Psychoses 2019;12:168–76. 10.3371/CSRP.KNMG.111717 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mukundan A, Faulkner GEJ, Cohn T, et al. Antipsychotic switching for people with schizophrenia who have neuroleptic-induced weight or metabolic problems. Cochrane Database Syst Rev 2007;CD006629. 10.1002/14651858.CD006629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Siskind D, Gallagher E, Winckel K, et al. Does switching antipsychotics ameliorate weight gain in patients with severe mental illness? A systematic review and meta-analysis. Schizophr Bull 2021;47:948–58. 10.1093/schbul/sbaa191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kane J, Honigfeld G, Singer J, et al. Clozapine for the treatment-resistant schizophrenic. A double-blind comparison with chlorpromazine. Arch Gen Psychiatry 1988;45:789–96. 10.1001/archpsyc.1988.01800330013001 [DOI] [PubMed] [Google Scholar]
- 35.Correll CU, Agid O, Crespo-Facorro B, et al. A guideline and checklist for initiating and managing clozapine treatment in patients with treatment-resistant schizophrenia. CNS Drugs 2022;36:659–79. 10.1007/s40263-022-00932-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Howes OD, McCutcheon R, Agid O, et al. Treatment-resistant Schizophrenia: treatment response and resistance in psychosis (TRRIP) working group consensus guidelines on diagnosis and terminology. Am J Psychiatry 2017;174:216–29. 10.1176/APPI.AJP.2016.16050503 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kane JM, Agid O, Baldwin ML, et al. Clinical guidance on the identification and management of treatment-resistant schizophrenia. J Clin Psychiatry 2019;80:2783. 10.4088/JCP.18COM12123 [DOI] [PubMed] [Google Scholar]
- 38.Ostuzzi G, Vita G, Bertolini F, et al. Continuing, reducing, switching, or stopping antipsychotics in individuals with schizophrenia-spectrum disorders who are clinically stable: a systematic review and network meta-analysis. Lancet Psychiatry 2022;9:614–24. 10.1016/S2215-0366(22)00158-4 [DOI] [PubMed] [Google Scholar]
- 39.Taipale H, Tanskanen A, Mehtälä J, et al. 20-year follow-up study of physical morbidity and mortality in relationship to antipsychotic treatment in a nationwide cohort of 62,250 patients with schizophrenia (FIN20). World Psychiatry 2020;19:61–8. 10.1002/wps.20699 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Schneider-Thoma J, Efthimiou O, Huhn M, et al. Second-generation antipsychotic drugs and short-term mortality: a systematic review and meta-analysis of placebo-controlled randomised controlled trials. Lancet Psychiatry 2018;5:653–63. 10.1016/S2215-0366(18)30177-9 [DOI] [PubMed] [Google Scholar]
- 41.Correll CU, Rubio JM, Kane JM. What is the risk-benefit ratio of long-term antipsychotic treatment in people with schizophrenia? World Psychiatry 2018;17:149–60. 10.1002/wps.20516 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Caemmerer J, Correll CU, Maayan L. Acute and maintenance effects of non-pharmacologic interventions for antipsychotic associated weight gain and metabolic abnormalities: a meta-analytic comparison of randomized controlled trials. Schizophr Res 2012;140:159–68. 10.1016/j.schres.2012.03.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Fink A, Cieslak S, Rosenbach F. Non-pharmacological interventions for the prevention of weight gain in schizophrenic patients treated with antipsychotic medication. Psychiatr Prax 2015;42:359–69. 10.1055/s-0035-1552670 [DOI] [PubMed] [Google Scholar]
- 44.Fernández-San-Martín MI, Martín-López LM, Masa-Font R, et al. The effectiveness of lifestyle interventions to reduce cardiovascular risk in patients with severe mental disorders: meta-analysis of intervention studies. Community Ment Health J 2014;50:81–95. 10.1007/s10597-013-9614-6 [DOI] [PubMed] [Google Scholar]
- 45.Bonfioli E, Berti L, Goss C, et al. Health promotion lifestyle interventions for weight management in psychosis: a systematic review and meta-analysis of randomised controlled trials. BMC Psychiatry 2012;12:78. 10.1186/1471-244X-12-78 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Daumit GL, Dickerson FB, Wang N-Y, et al. A behavioral weight-loss intervention in persons with serious mental illness. N Engl J Med 2013;368:1594–602. 10.1056/NEJMoa1214530 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Green CA, Yarborough BJH, Leo MC, et al. The STRIDE weight loss and lifestyle intervention for individuals taking antipsychotic medications: a randomized trial. Am J Psychiatry 2015;172:71–81. 10.1176/appi.ajp.2014.14020173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Speyer H, Christian Brix Nørgaard H, Birk M, et al. The change trial: no superiority of lifestyle coaching plus care coordination plus treatment as usual compared to treatment as usual alone in reducing risk of cardiovascular disease in adults with schizophrenia spectrum disorders and abdominal obesity. World Psychiatry 2016;15:155–65. 10.1002/wps.20318 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Bartels SJ. Clinically significant improved fitness and weight loss among overweight persons with serious mental illness. Physiol Behav 2017;176:139–48. 10.1016/j.physbeh.2017.03.040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Magni LR, Ferrari C, Rossi G, et al. Superwellness program: a cognitive-behavioral therapy-based group intervention to reduce weight gain in patients treated with antipsychotic drugs. Braz J Psychiatry 2017;39:244–51. 10.1590/1516-4446-2016-1993 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Vancampfort D, Firth J, Correll CU, et al. The impact of pharmacological and non-pharmacological interventions to improve physical health outcomes in people with schizophrenia: a meta-review of meta-analyses of randomized controlled trials. World Psychiatry 2019;18:53–66. 10.1002/wps.20614 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Fiedorowicz JG, Miller DD, Bishop JR, et al. Systematic review and meta-analysis of pharmacological interventions for weight gain from antipsychotics and mood stabilizers. Curr Psychiatry Rev 2012;8:25–36. 10.2174/157340012798994867 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Mizuno Y, Suzuki T, Nakagawa A, et al. Pharmacological strategies to counteract antipsychotic-induced weight gain and metabolic adverse effects in schizophrenia: a systematic review and meta-analysis. Schizophr Bull 2014;40:1385–403. 10.1093/schbul/sbu030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Choi YJ. Efficacy of adjunctive treatments added to olanzapine or clozapine for weight control in patients with schizophrenia: a systematic review and meta-analysis. ScientificWorldJournal 2015;2015:970730. 10.1155/2015/970730 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Zheng W, Li X-B, Tang Y-L, et al. Metformin for weight gain and metabolic abnormalities associated with antipsychotic treatment: meta-analysis of randomized placebo-controlled trials. J Clin Psychopharmacol 2015;35:499–509. 10.1097/JCP.0000000000000392 [DOI] [PubMed] [Google Scholar]
- 56.Praharaj SK, Jana AK, Goyal N, et al. Metformin for olanzapine-induced weight gain: a systematic review and meta-analysis. Br J Clin Pharmacol 2011;71:377–82. 10.1111/j.1365-2125.2010.03783.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ehret M, Goethe J, Lanosa M, et al. The effect of metformin on anthropometrics and insulin resistance in patients receiving atypical antipsychotic agents: a meta-analysis. J Clin Psychiatry 2010;71:1286–92. 10.4088/JCP.09m05274yel [DOI] [PubMed] [Google Scholar]
- 58.Liang H, Li H, Hu Y, et al. Effects of topiramate for atypical antipsychotic-induced body weight gain and metabolic adversities: a systematic review and meta-analysis. Zhonghua Yi Xue Za Zhi 2016;96:216–23. 10.3760/cma.j.issn.0376-2491.2016.03.014 [DOI] [PubMed] [Google Scholar]
- 59.Mahmood S, Booker I, Huang J, et al. Effect of topiramate on weight gain in patients receiving atypical antipsychotic agents. J Clin Psychopharmacol 2013;33:90–4. 10.1097/JCP.0b013e31827cb2b7 [DOI] [PubMed] [Google Scholar]
- 60.Zheng W, Xiang Y-T, Xiang Y-Q, et al. Efficacy and safety of adjunctive topiramate for schizophrenia: a meta-analysis of randomized controlled trials. Acta Psychiatr Scand 2016;134:385–98. 10.1111/acps.12631 [DOI] [PubMed] [Google Scholar]
- 61.Maayan L, Vakhrusheva J, Correll CU. Effectiveness of medications used to attenuate antipsychotic-related weight gain and metabolic abnormalities: a systematic review and meta-analysis. Neuropsychopharmacology 2010;35:1520–30. 10.1038/npp.2010.21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Siskind D, Hahn M, Correll CU, et al. Glucagon-like peptide-1 receptor agonists for antipsychotic-associated cardio-metabolic risk factors: a systematic review and individual participant data meta-analysis. Diabetes Obes Metab 2019;21:293–302. 10.1111/dom.13522 [DOI] [PubMed] [Google Scholar]
- 63.Holst JJ. The physiology of glucagon-like peptide 1. Physiol Rev 2007;87:1409–39. 10.1152/physrev.00034.2006 [DOI] [PubMed] [Google Scholar]
- 64.Rondanelli M, Perna S, Astrone P, et al. Twenty-four-week effects of liraglutide on body composition, adherence to appetite, and lipid profile in overweight and obese patients with type 2 diabetes mellitus. Patient Prefer Adherence 2016;10:407–13. 10.2147/PPA.S97383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Li C-J, Yu Q, Yu P, et al. Changes in liraglutide-induced body composition are related to modifications in plasma cardiac natriuretic peptides levels in obese type 2 diabetic patients. Cardiovasc Diabetol 2014;13:36. 10.1186/1475-2840-13-36 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Iepsen EW, Lundgren JR, Hartmann B, et al. GLP-1 receptor agonist treatment increases bone formation and prevents bone loss in weight-reduced obese women. J Clin Endocrinol Metab 2015;100:2909–17. 10.1210/jc.2015-1176 [DOI] [PubMed] [Google Scholar]
- 67.Zhang YS, Weng WY, Xie BC, et al. Glucagon-like peptide-1 receptor agonists and fracture risk: a network meta-analysis of randomized clinical trials. Osteoporos Int 2018;29:2639–44. 10.1007/s00198-018-4649-8 [DOI] [PubMed] [Google Scholar]
- 68.Maagensen H, Larsen JR, Jørgensen NR, et al. Liraglutide does not change bone turnover in clozapine-and olanzapine-treated schizophrenia overweight patients with prediabetes-randomized controlled trial. Psychiatry Res 2021;296:113670. 10.1016/j.psychres.2020.113670 [DOI] [PubMed] [Google Scholar]
- 69.Lau J, Bloch P, Schäffer L, et al. Discovery of the once-weekly glucagon-like peptide-1 (GLP-1) analogue semaglutide. J Med Chem 2015;58:7370–80. 10.1021/acs.jmedchem.5b00726 [DOI] [PubMed] [Google Scholar]
- 70.Marso SP, Bain SC, Consoli A, et al. Semaglutide and cardiovascular outcomes in patients with type 2 diabetes. N Engl J Med 2016;375:1834–44. 10.1056/NEJMoa1607141 [DOI] [PubMed] [Google Scholar]
- 71.Marso SP, Daniels GH, Brown-Frandsen K, et al. Liraglutide and cardiovascular outcomes in type 2 diabetes. N Engl J Med 2016;375:311–22. 10.1056/NEJMoa1603827 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Ishøy PL, Knop FK, Broberg BV, et al. Effect of GLP-1 receptor agonist treatment on body weight in obese antipsychotic-treated patients with schizophrenia: a randomized, placebo-controlled trial. Diabetes Obes Metab 2017;19:162–71. 10.1111/dom.12795 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Whicher CA, Price HC, Phiri P, et al. The use of liraglutide 3.0 Mg daily in the management of overweight and obesity in people with schizophrenia, schizoaffective disorder and first episode psychosis: results of a pilot randomized, double-blind, placebo-controlled trial. Diabetes Obes Metab 2021;23:1262–71. 10.1111/dom.14334 [DOI] [PubMed] [Google Scholar]
- 74.Lee SE, Lee NY, Kim SH, et al. Effect of liraglutide 3.0mg treatment on weight reduction in obese antipsychotic-treated patients. Psychiatry Res 2021;299:113830. 10.1016/j.psychres.2021.113830 [DOI] [PubMed] [Google Scholar]
- 75.Perlis LT, Lamberti JS, Miedlich SU. Glucagon-like peptide analogs are superior for diabetes and weight control in patients on antipsychotic medications: a retrospective cohort study. Prim Care Companion CNS Disord 2020;22:27304. 10.4088/PCC.19m02504 [DOI] [PubMed] [Google Scholar]
- 76.Larsen JR, Vedtofte L, Jakobsen MSL, et al. Effect of liraglutide treatment on prediabetes and overweight or obesity in clozapine- or olanzapine-treated patients with schizophrenia spectrum disorder: a randomized clinical trial. JAMA Psychiatry 2017;74:719–28. 10.1001/jamapsychiatry.2017.1220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Wang Y, Wang D, Cheng J, et al. Efficacy and tolerability of pharmacological interventions on metabolic disturbance induced by atypical antipsychotics in adults: a systematic review and network meta-analysis. J Psychopharmacol 2021;35:1111–9. 10.1177/02698811211035391 [DOI] [PubMed] [Google Scholar]
- 78.Lee K, Abraham S, Cleaver R. A systematic review of licensed weight-loss medications in treating antipsychotic-induced weight gain and obesity in schizophrenia and psychosis. Gen Hosp Psychiatry 2022;78:58–67. 10.1016/j.genhosppsych.2022.07.006 [DOI] [PubMed] [Google Scholar]
- 79.de Boer N, Cahn W. Antipsychotic-Induced weight gain: is the weight over? New guidelines needed. Acta Psychiatr Scand 2022;146:185–9. 10.1111/acps.13485 [DOI] [PubMed] [Google Scholar]
- 80.O’Neil PM, Birkenfeld AL, McGowan B, et al. Efficacy and safety of semaglutide compared with liraglutide and placebo for weight loss in patients with obesity: a randomised, double-blind, placebo and active controlled, dose-ranging, phase 2 trial. Lancet 2018;392:637–49. 10.1016/S0140-6736(18)31773-2 [DOI] [PubMed] [Google Scholar]
- 81.Heinrichs DW, Hanlon TE, Carpenter WT. The quality of life scale: an instrument for rating the schizophrenic deficit syndrome. Schizophr Bull 1984;10:388–98. 10.1093/schbul/10.3.388 [DOI] [PubMed] [Google Scholar]
- 82.Busner J, Targum SD. The clinical global impressions scale: applying a research tool in clinical practice. Psychiatry (Edgmont) 2022;4:28–37. [PMC free article] [PubMed] [Google Scholar]
- 83.Saunders JB, Aasland OG, Babor TF, et al. Development of the alcohol use disorders identification test (audit): who Collaborative project on early detection of persons with harmful alcohol consumption -- II. Addiction 1993;88:791–804. 10.1111/j.1360-0443.1993.tb02093.x [DOI] [PubMed] [Google Scholar]
- 84.Berman AH, Bergman H, Palmstierna T, et al. Evaluation of the drug use disorders identification test (DUDIT) in criminal justice and detoxification settings and in a Swedish population sample. Eur Addict Res 2005;11:22–31. 10.1159/000081413 [DOI] [PubMed] [Google Scholar]
- 85.Heatherton TF, Kozlowski LT, Frecker RC, et al. The fagerström test for nicotine dependence: a revision of the fagerström tolerance questionnaire. Br J Addict 1991;86:1119–27. 10.1111/j.1360-0443.1991.tb01879.x [DOI] [PubMed] [Google Scholar]
- 86.World Health Organisation . Multiaxial classification of child and adolescent psychiatric disorders. Cambridge Univ Press, 1996. [Google Scholar]
- 87.Damilakis J, Adams JE, Guglielmi G, et al. Radiation exposure in X-ray-based imaging techniques used in osteoporosis. Eur Radiol 2010;20:2707–14. 10.1007/s00330-010-1845-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Uniform requirements for manuscripts submitted to biomedical journals. JAMA 1997;277:927. 10.1001/jama.1997.03540350077040 [DOI] [PubMed] [Google Scholar]
- 89.Chan A-W, Tetzlaff JM, Gøtzsche PC, et al. SPIRIT 2013 explanation and elaboration: guidance for protocols of clinical trials. BMJ 2013;346:e7586. 10.1136/bmj.e7586 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.World Medical Association . World medical association declaration of helsinki. JAMA 2013;310:2191. 10.1001/jama.2013.281053 [DOI] [PubMed] [Google Scholar]
- 91.SENS motion: Discrete wearable activity sensor for healthcare and research. 2022. Available: www.sens.dk
- 92.Ghaffari A, Rahbek O, Lauritsen REK, et al. Criterion validity of linear accelerations measured with low-sampling-frequency accelerometers during overground walking in elderly patients with knee osteoarthritis. Sensors (Basel) 2022;22:5289. 10.3390/s22145289 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Pedersen BS, Kristensen MT, Josefsen CO, et al. Validation of two activity monitors in slow and fast walking hospitalized patients. Rehabil Res Pract 2022;2022:9230081. 10.1155/2022/9230081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Miras AD, Jackson RN, Jackson SN, et al. Gastric bypass surgery for obesity decreases the reward value of a sweet-fat stimulus as assessed in a progressive ratio task. Am J Clin Nutr 2012;96:467–73. 10.3945/ajcn.112.036921 [DOI] [PubMed] [Google Scholar]
- 95.Østergaard SD, Lemming OM, Mors O, et al. PANSS-6: a brief rating scale for the measurement of severity in schizophrenia. Acta Psychiatr Scand 2016;133:436–44. 10.1111/acps.12526 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2022-068652supp002.pdf (62.8KB, pdf)
bmjopen-2022-068652supp001.pdf (83.9KB, pdf)