Abstract
Objectives
Epilepsy treatment decision making is complex and understanding what informs caregiver decision making about treatment for childhood epilepsy is crucial to better support caregivers and their children. We synthesised evidence on caregivers’ perspectives and experiences of treatments for childhood epilepsy.
Design
Systematic review of qualitative studies using a best-fit framework and Grading of Recommendations Assessment, Development and Evaluation Confidence in the Evidence from Reviews of Qualitative Research (GRADE-CERQual) approach.
Data sources
Searched Embase, PubMed, CINAHL, PsycINFO, SocINDEX and Web of Science from 1 January 1999 to 19 August 2021.
Eligibility criteria
We included qualitative studies examining caregiver’s perspectives on antiseizure medication, diet or surgical treatments for childhood epilepsy. We excluded studies not reported in English.
Data extraction and synthesis
We extracted qualitative evidence into 1 of 14 domains defined by the Theoretical Domains Framework (TDF). One reviewer extracted study data and methodological characteristics, and two reviewers extracted qualitative findings. The team verified all extractions. We identified themes within TDF domains and synthesised summary statements of these themes. We assessed our confidence in our summary statements using GRADE-CERQual.
Results
We identified five studies (in six reports) of good methodological quality focused on parent perceptions of neurosurgery; we found limited indirect evidence on parents’ perceptions of medications or diet. We identified themes within 6 of the 14 TDF domains relevant to treatment decisions: knowledge, emotion; social/professional role and identity; social influence; beliefs about consequences; and environmental context and resources.
Conclusions
Parents of children with epilepsy navigate a complex process to decide whether to have their child undergo surgery. Educational resources, peer support and patient navigators may help support parents through this process. More qualitative studies are needed on non-surgical treatments for epilepsy and among caregivers from different cultural and socioeconomic backgrounds to fully understand the diversity of perspectives that informs treatment decision making.
Keywords: QUALITATIVE RESEARCH, Epilepsy, NEUROSURGERY, Paediatric neurology
STRENGTHS AND LIMITATIONS OF THIS STUDY
This synthesis followed contemporary standards for the conduct of qualitative synthesis, which includes using a best-fit framework approach to categorise and synthesise findings based on the Theoretical Domains Framework.
Risks to rigour of included studies were assessed using the Critical Appraisal Skills Programme tool for qualitative studies.
Confidence in the conclusions drawn from this synthesis was rated using the Grading of Recommendations Assessment, Development and Evaluation Confidence in the Evidence from Reviews of Qualitative Research.
As with all qualitative synthesis, selecting which data to extract and how to code it is ultimately a subjective process.
This synthesis was limited to studies that examined parents’ perceptions, experiences and decision making about pursuing surgery to treat their child’s epilepsy.
Introduction
Epilepsy is a common neurological disorder in children, affecting about 1% of children in the USA.1 While there are different types of childhood epilepsy, each type involves recurring seizures caused by abnormal electrical activity in the brain. Epilepsy is categorised by seizure type (eg, focal, generalised or unknown), epilepsy type (eg, focal, generalised, unknown) and syndrome type (eg, childhood absence epilepsy, Dravet syndrome).2–4 No matter the type, epilepsy is a chaotic and unpredictable condition for both the affected children and their caregivers.5
Treatment and ongoing management approaches depend on the type of the epilepsy and prior treatment response. Treatment options for childhood epilepsy include antiseizure medications (ASMs), ketogenic diets or surgery. Although many children with new-onset epilepsy achieve seizure freedom with ASMs,6 these drugs are associated with numerous adverse effects (eg, tiredness, nausea, headache, difficulty concentrating, depression and suicidal ideation).7 Furthermore, about 20% of children continue to experience seizures despite drug treatment.8 The effectiveness of ketogenic diets (eg, Atkins diet) is supported by low quality evidence.9 However, these diets are also associated with adverse effects (eg, gastrointestinal symptoms, dyslipidaemia, decreased growth and kidney stones), and require considerable caregiver effort to maintain. Surgical interventions may isolate and remove the underlying neurological cause of seizures, but carry risks of bleeding, infection, hydrocephalus and new neurological deficits.
Epilepsy treatment decision making is thus complex and needs to consider each child’s unique form of epilepsy, evidence of each treatment’s potential benefits and harms, previous or ongoing experiences with treatment(s) and family’s values and preferences. Although studies of treatment effectiveness rarely explore how families navigate these complex considerations or how these considerations may evolve over time, qualitative studies can offer context on caregiver experiences and decision making. Syntheses of these qualitative studies can help shape caregiver and healthcare provider interactions and inform shared decision-making tools and processes. The purpose of this review is to summarise the qualitative research regarding caregivers’ perspectives and experiences of treatments for childhood epilepsy.
Methods
We conducted a qualitative evidence synthesis in accordance with standards for qualitative evidence syntheses.10–12
Data sources and searches
We searched EMBASE, PubMed (in process), CINAHL, PsycINFO, SocINDEX and Web of Science for studies published from 1 January 1999 to 19 August 2021, using terms related to epilepsy, treatments and caregiver perspectives (online supplemental appendix A). The search was limited to English-language. We also ran forward and backward citation searches (ie, snowball searching) on included studies to ensure relevant studies were not missed.
bmjopen-2022-066872supp001.pdf (328.1KB, pdf)
Study selection
We included qualitative studies that sought to understand caregiver’s perspectives on ASMs, diet or surgical treatments for childhood epilepsy. Studies needed to use qualitative methods for both data collection (eg, focus group, individual interviews or open-ended survey questions) and data analysis (eg, thematic analysis). We excluded studies that focused only on non-caregiver perceptions (eg, patient or healthcare provider) or that focused only on caregiver stress or caregiver expectations of treatment. We did not restrict by study country or care setting.
One reviewer screened titles and abstracts of citations retrieved from searches for eligibility. Two independent reviewers screened the full text of potentially relevant citations in PICO Portal (https://picoportal.org/). Disagreements were resolved through discussion of the full team.
Data extraction and quality assessment
For each study, we extracted details on the study design and methodological features, population characteristics and qualitative analysis findings.
One reviewer assessed risks to rigour using the Critical Appraisal Skills Programme (CASP) tool for qualitative studies, which appraises research aims, congruence between research aims and methodological approach, quality of sampling and data collection, appropriateness of application of methods, richness and conceptual depth of findings, appropriateness of interrogation of findings and researcher reflexivity.13 All team members reviewed the CASP assessments to ensure consistency of ratings across studies.
Two team members independently extracted and coded the qualitative findings of the included studies in MaxQDA 2020 (Berlin, Germany), an online platform designed to support qualitative data management, extraction and analysis. The extracted data included direct quotes from the participants (first order statements) and summary statements written by the study authors (second order statements). Extracted data were imported into spreadsheets to facilitate data cleaning, confirmation of themes and synthesis.
To categorise the extracted data, we used the Theoretical Domains Framework (TDF),14 15 which was developed to assist in identifying the cognitive, affective, social and environmental factors that may influence an individuals’ performance of a health behaviour. The health behaviour of interest for this review was the decision to pursue an epileptic treatment. The 14 domains include: knowledge; skills; social/professional role and identity; belief about capabilities; optimism; beliefs about consequences; reinforcement; intention; goals; memory, attention and decision processes; environmental context and resources; social influences; emotion and behavioural regulation (online supplemental appendix B). A third reviewer confirmed TDF domain codes, and the team discussed the coding to ensure accuracy and consistency both within and across TDF domains. One reviewer did a final confirmation of extracted text and coding to ensure no data were missed and that there was consistency across domains.
Data synthesis and analysis
We adopted a best-fit framework approach to guide our qualitative synthesis. In this approach, data are coded according to TDF domains. One reviewer then summarised key themes within each TDF domain. Themes were discussed and debated among the team until consensus was achieved. We used the finalised themes to develop summary statements and assessed our confidence in these statements using Grading of Recommendations Assessment, Development and Evaluation Confidence in the Evidence from Reviews of Qualitative Research (GRADE-CERQual).16–18 We rated our confidence in the summary statements as either high, moderate, low or very low based on our assessment of the four GRADE-CERQual domains: methodological limitations, relevance, coherence and adequacy of the data (online supplemental appendix C for definition of domains). ‘High confidence’ refers to a finding that is highly likely to be a reasonable representation of the phenomenon of interest, whereas ‘very low confidence’ refers to a review finding in which it was unclear if the finding was a reasonable representation.
Patient and public involvement
None.
Results
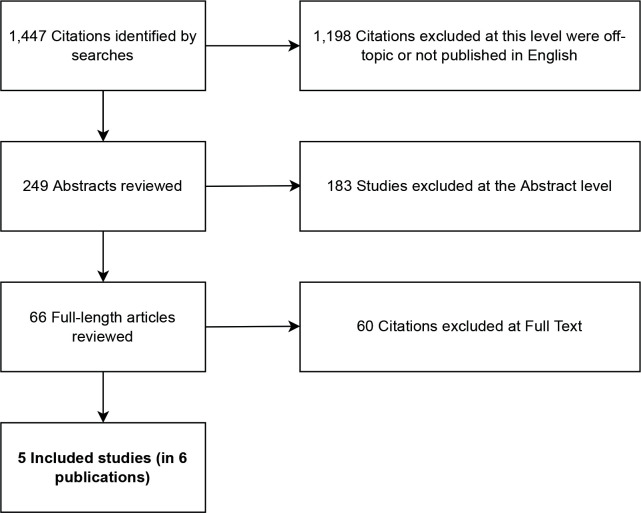
The literature search yielded 1447 citations from searches (see Preferred Reporting Items for Systematic Reviews and Meta-Analyses flow diagram, figure 1). We found 66 citations to retrieve for full-text screening of which five studies (in six publications) were included in the final sample.19–24 Table 1 presents characteristics of included studies.
Figure 1.
PRISMA flow diagram of studies identified. PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
Table 1.
Characteristics of included studies
| Study, year, country | Population | No of parents | Time from surgery to data collection | Study aim | Data collection methods | Data analysis methods |
| Baca*, 2015; Pieters, 2016, USA19 | Parents of children who had previously undergone resective epilepsy surgery | 37 (individual parents) 31 mothers; 6 other |
NR | Baca, 2015: To identify the nature and range of parent-perceived barriers to timely receipt of paediatric epilepsy surgery. Pieters, 2016: (A) To describe thoroughly the parental experiences and perceptions of this slow and arduous period prior to the presurgical referral and evaluation to a comprehensive paediatric epilepsy centre. (B) To delineate the range of parent identified factors, or facilitators, that helped move families forward along their journey to surgery |
Semi-structured interviews lasting on average 29 min (range 10–60 min) | Thematic analysis |
| Heath, 2016, UK21 | Parents of children who had undergone paediatric epilepsy surgery Also interviewed healthcare professionals caring for children with epilepsy |
9 (individual parents) 8 mothers; 1 father 10 healthcare professionals |
NR | To explore how parents and health professionals make decisions regarding paediatric epilepsy surgery to identify: (A) factors that influence the process of decision making regarding paediatric epilepsy surgery from the perspective of parents and professionals and (B) the support needs of those considering surgery as a treatment option for a child with medically intractable epilepsy |
Semistructured interviews lasting about 1 hour, and non-participant observations | Thematic analysis |
| O'Brien, 2020, UK22 | Parents and their children who had gone through resective epilepsy surgery | 9 parents (1 couple; 7 individual parents) 8 mothers; 1 father |
6 months to 3 years | To explore children’s and parents’ perspectives on the journey prior to and following surgical treatment, with a focus on the emotional experiences of children and their parents throughout the surgery journey | Semi-structured interviews lasting 25–75 min | Thematic analysis |
| Ozanne, 2016, Sweden23 | Parents of children who had previously undergone resective epilepsy surgery | 24 parents 13 mothers; 11 fathers |
5–10 years | To explore parental experiences before and after hemispherotomy as reported at a long-term follow-up and the parents' views on received information and support | Interviews (length of time not reported) | Content analysis |
| Sylven, 2020, Sweden24 | Parents of children who were undergoing resective epilepsy surgery (and 2 years post-surgery) | 107 (parental responses to both surveys) | 2 years | (A) To understand parental hopes and worries before their child underwent epilepsy surgery and (B) To understand parental satisfaction 2 years after their child had undergone epilepsy surgery | Surveys (open-ended questions) | Thematic analysis |
*Baca and Pieters included the same patient population but reported on different aspects of parent perspectives.
NR, not reported.
All studies examined parents’ perceptions, experiences and decision making leading to surgery. All studies were conducted after the children had undergone surgery, with one study also surveying parents ‘just prior’ to surgery.24 Three studies reported data on parents’ perceptions and experiences with medications and diet, but only in the context of selecting surgery (eg, parents considering surgery due to the undesirable side effects or uncontrolled epilepsy with prior treatments).19 21 24 In total, the views of 186 parents are represented in the 5 studies (the majority of whom were mothers, n=115). The time from children’s surgery to data collection ranged from 6 months to 10 years among the three studies reporting on timing. Four studies collected parent perspectives through semistructured interviews conducted in-person or over the telephone (length ranging from 10 to 75 min),19–23 and one study captured parent perceptions through open-ended survey questions.24
All studies were assessed to have minor risk to rigour (online supplemental appendix D) due to the retrospective nature of recruitment and the lack of consideration (or reporting) of the relationship between researchers and participants. Otherwise, studies were considered appropriate in their use of qualitative design, methods of data collection and analysis. The retrospective nature of the included studies raises concerns about recall bias, as surgical outcomes may have affected retrospective perceptions, and selection bias since studies only included parents of children who were referred to surgery and proceeded with surgery (and possibly experienced some level of success with surgery). All but one study23 did not report whether interviewers were part of the child’s care team, which may have influenced responses. Ozanne et al reported that the researchers that interviewed parents and analysed the data were not part of the epilepsy surgery team.23
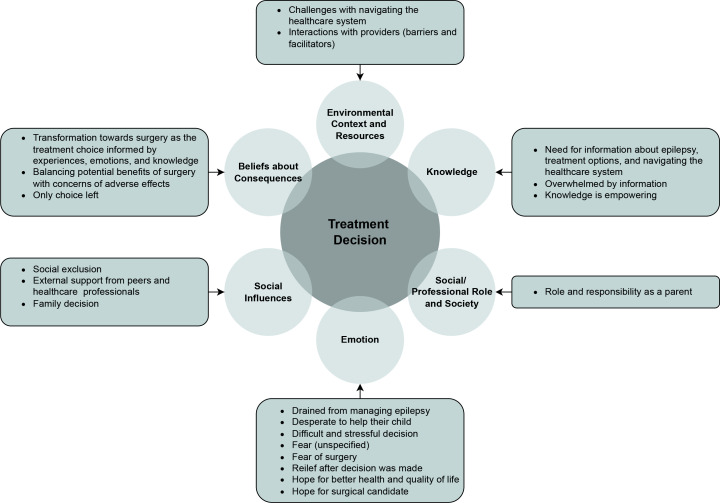
We identified and coded data for 6 of the 14 TDF domains: knowledge; emotion; social/professional role and identity; social influence; beliefs about consequences; and environmental context and resources (figure 2). We did not find evidence from extracted qualitative data for the remaining eight TDF domains. Online supplemental appendix E provides the extracted text from studies linked to their synthesised themes.
Figure 2.
The six theoretical domains identified in this review that impacted treatment decision making and the main themes representing those domains.
The GRADE-CERQual table (table 2) summarises findings and conclusions for each TDF domain. We had no or minor concerns with the coherence of the findings (ie, the synthesised findings reflect the complexity and variation of the data) or their relevance (ie, the extent to which synthesised findings are applicable to the context specified in the review question). We had minor or moderate concerns with the adequacy (ie, the degree of richness and quantity of the data supporting the synthesised finding) of the findings related to knowledge and environmental context and resources, respectively. Below, we report the summary statement (and associated GRADE-CERQual level of confidence) under each identified TDF domain and summarise the key themes that contributed to the statements.
Table 2.
GRADE-CERQual summary of findings statements and ratings
| Summary of review findings | Studies contributing | Methodological limitations (CASP ratings) | Coherence | Adequacy* | Relevance | CERQual assessment | Explanation of CERQual assessment |
| Knowledge: Caregivers value information about epilepsy, its treatment options, and navigating the healthcare system to access timely and effective treatment for their child. Despite feeling overwhelmed by the complexity and sometimes contradictory information, caregivers value learning this new language so they can become better advocates for their child | Baca/Pieters Heath O'Brien Ozanne |
Minor concerns: Nature of relationship between researchers and participants not reported; retrospective recruitment.† | No or very minor concerns: Findings reflect the complexity and variation of data |
Minor concerns: Included studies limited to surgery as treatment decision. We did not identify studies meeting inclusion criteria that addressed other treatments, such as diet or medications. Each study addressed knowledge acquisition and reported on it in some depth. |
No or very minor concerns | Moderate confidence | Four studies with similar findings; minor concerns related to methods and limited treatment scope (surgery). |
| Social/professional role and identity: parents feel a sense of duty and need to do the right thing in selecting a treatment for their child. | Heath | Minor concerns: Nature of relationship between researchers and participants not reported; retrospective recruitment.† | No or very minor concerns: Findings reflect the complexity and variation of data |
Minor concern: Included studies limited to surgery as treatment decision. | No or very minor concerns | Moderate confidence | One study; minor concerns related to methods and limited treatment scope (surgery). |
| Emotion: parents experience the journey of navigating their child’s epilepsy and ultimately selecting surgical treatment as an emotionally fraught one with emotions ranging from exhaustion, desperation and fear to relief and hope. | Baca/Pieters Heath O'Brien Ozanne Sylvén |
Minor concerns: Nature of relationship between researchers and participants not reported; retrospective recruitment.† | No or very minor concerns: Findings reflect the complexity and variation of data | No or very minor concerns: All four studies contributed to the rich depth of the varied emotions from fear of the illness to fear of the surgery to the mental toll that took on families and hope and relief that surgery may offer | No or very minor concerns | Moderate confidence | Five studies with similar findings; minor concerns related to methods and limited treatment scope (surgery). |
| Social influences: surgery is a family decision that requires outside support from other parents ‘experiencing the same thing’ and from a healthcare professional acting as ‘champions’. | Pieters Heath O'Brien |
Minor concerns: Nature of relationship between researchers and participants not reported; retrospective recruitment.† |
No or very minor concerns: Findings reflect the complexity and variation of data | No or very minor concerns | No or very minor concerns | Moderate confidence | Three studies with similar findings; minor concerns related to methods and limited treatment scope (surgery). |
| Beliefs about consequences: caregivers undergo a transformation from seeing surgery as a last resort to the only option for their child to have a chance at a better life. Surgery became a viable option as parents realised that their child’s current treatment was not working or it had unacceptable side effects, and some saw the side effects of surgery as less daunting than the disease. | Baca/Pieters Heath O'Brien Ozanne Sylvén |
Minor concerns: Nature of relationship between researchers and participants not reported; retrospective recruitment.† | No or very minor concerns: Findings reflect the complexity and variation of data |
No or very minor concerns | No or very minor concerns | Moderate confidence | Five studies with similar findings; minor concerns related to methods and limited treatment scope (surgery). |
| Environmental context and resources: parents expressed challenges in navigating the healthcare system and interacting with professionals to find the ‘right doctor’ or care team for their child. Parents value having their concerns heard and being engaged in the decision-making process. | Baca/Pieters Heath Ozanne |
Minor concerns: Nature of relationship between researchers and participants not reported; retrospective recruitment.† | No or very minor concerns: Findings reflect the complexity and variation of data | Moderate concerns: The three studies are limited to surgery and to USA, Sweden and the UK. Healthcare barriers seemed particularly salient to U.S. respondents (including insurance barriers) | No or very minor concerns | Low confidence | Three studies with similar findings; moderate concerns related to methods, limited scope (surgery), and context-specific healthcare experiences of participants |
*We only downgraded for adequacy due to studies being limited to surgery when the summarised theme was based on parent’s general feelings about epilepsy and could thus potentially apply to parent decisions regarding other treatment choices.
†Retrospective recruitment raises concerns about selection bias.
CASP, Critical Appraisal Skills Programme; GRADE-CERQual, Grading of Recommendations Assessment, Development and Evaluation Confidence in the Evidence from Reviews of Qualitative Research.
Tdf domain 1: knowledge
Summary statement
Evidence from four studies indicated that caregivers value information about epilepsy, its treatment options and navigating the healthcare system to access timely and effective treatment for their child. Despite feeling overwhelmed by the complexity and sometimes contradictory information, caregivers value learning this new language so they can become better advocates for their child (Moderate confidence).19–23
Once parents recognised ‘something [was] wrong’ with the health of their child, they sought information from multiple sources ‘to understand seizures and epilepsy and become better advocates for their child’.19 Parents wanted information about medications,19 surgery19 21 and what types of doctors were needed to care for their child.20 They also noted needing to learn about how to navigate the health system including multiple specialties, hospitals and insurance procedures.19
Parents often perceived the information they received from professionals as inadequate to make informed decisions.21 They described seeking lay language information from multiple sources, including additional professionals, the internet, books, family, friends and other parents.19 23 Parents expressed discomfort in the ‘lack of understandable information’ and ‘information imbalance’ between themselves and their child’s providers and sought to become ‘epilepsy experts in order to be effective advocates for their children.’20 After increasing their knowledge, parents felt more empowered to ask questions and participate more actively in the decision making.19 21 Parents thus described active learning to ensure productive information exchanges with providers (including using clinical terms) to support a positive shared-decision making process.20
TDF domain 2: social role and identity
Summary statement
Evidence from one study indicated that caregivers feel a sense of duty and need to do the right thing in selecting a treatment for their child (Moderate confidence).21
Parents reported a ‘sense of duty’ to be ‘strong’ and ‘brave’. They also reported feeling pressure to ‘do the right thing’ by their child; that is, choosing the treatment option that would give their child the best chance of ‘reaching their full potential’.21
TDF domain 3: emotion
Summary statement
Five studies provided evidence to suggest that caregivers experience the journey of navigating their child’s epilepsy and ultimately selecting surgical treatment as an emotionally fraught one with emotions ranging from exhaustion, desperation, fear to relief and hope (Moderate confidence).19–23
Parents expressed feeling drained and stressed from always being ‘on call’,19 worrying about a seizure,19 22 or mood and behavioural difficulties.22 Parents recalled feeling frustrated19 20 and desperate to ‘find a treatment option that would work’.20 For example, one mother was frustrated that her child’s provider continued to perform medication trials to manage seizures and not discuss surgery as an option,19 while another mother was desperate to get her son to another doctor but needed to wait for referrals because of insurance.
When considering surgery as a potential treatment option, parents reported the decision process as ‘difficult’, ‘frightening’ and ‘stressful’.20 21 Parents feared surgery would lead to worse health outcomes for their child,21 24 change their child’s personality, or cause a loss of function (eg, partial or complete loss in speech or movement).24 Parents also feared the possibility of surgery making seizures worse (eg, increased frequency, duration). Thus, making the decision to have surgery ‘in vain’.24
However, for many parents, the decision to pursue surgery brought relief and feelings of hope. Parents in one study expressed gratitude once they finally decided to pursue surgery as they felt it was ‘demanding to not know if surgery would be possible’.23 Parents also reported feeling hope for improvements in their child’s health and well-being after they decided to choose surgery. Finally, after making the decision to pursue surgery (or learning it was a viable option), parents reported that they hoped for candidacy,19 21 and experienced relief when a date was set.21
TDF domain 4: social influence
Summary statement
Three studies provided evidence to suggest that surgery is a family decision that requires outside support from other caregivers ‘experiencing the same thing’ and from a healthcare professional acting as ‘champions’. (Moderate confidence) 20–22
Parents reported the value of connecting with other parents who were on a similar treatment journey (eg, had a child with epilepsy that was unresponsive to medication) and had experiences and expertise that they could draw on.20 21 Peer connections helped parents understand the surgical procedural from a ‘parental perspective’ and provided ‘emotional support’.21 Parents also reported the value of having a good team of epilepsy providers and a ‘champion’ (eg, doctor, nurse or social worker) to advocate for them and help them navigate purposefully through their journey.20 One mother described one such champion, a nurse coordinator, as a ‘life saver,’ who helped in getting referrals and pushed her to seek better care for her child.’20 Another mother described her child’s paediatrician as her champion because ‘he encouraged me and gave me…confidence.’20
Parents described seeing treatment decision making as a family choice and indicated the importance of involving partners, siblings, grandparents and the child (where developmentally appropriate). Parents found engaging the whole family in the decision-making process to be generally helpful, as the experience of the child’s epilepsy and potential consequences of treatment impacted the whole family.21 However, for some families, decision making regarding surgery gave rise to conflicts. For example, one mother described herself as more agreeable to surgery than the child’s father because, as the primary parent, she ‘witnessed’ the true extent of their child’s seizures.21
TDF domain 5: beliefs about consequences
Summary statement
Five studies provided evidence to suggest that parents undergo a transformation from seeing surgery as a last resort to the only option for their child to have a chance at a better life. Surgery became a viable option as parents realised that their child’s current treatment was not working or it had unacceptable side effects, and some saw the side effects of surgery as less daunting than the disease. 19–24
Parents of children who went on to have surgery reported going through a transformation in thinking of surgery as a ‘last resort’ to a ‘necessary and hopeful option’.19 This transformation in thinking evolved as parents acquired greater understanding about their child’s illness and prognosis, experience in treating their child with other treatments, acquired knowledge about the potential risks and benefits of surgery, and processed the diverse emotions associated with surgery.19 20
An important part of parents’ moving toward a decision about surgery was weighing what they perceived to be the benefits and harms of surgery.21 24 In terms of benefits, parents hoped surgery would lead to improved outcomes such as seizure reduction and the opportunity for a ‘normal life’ without the side effects of medications.21 24 Some parents were sceptical about the efficacy of surgery due to their experiences with medications and the ketogenic diet. According to parents, these treatments were associated with side effects, negatively affected their child’s quality of life, and provided only minimal improvement in seizure control.21 In terms of adverse effects, parents were concerned that surgery would lead to surgical complications or various postsurgical impairments, including a change in personality, loss of speech or motor function and behavioural problems.24 A small number of parents reported having no concerns before surgery.24
Beyond rational consideration of the benefits and risks of surgery, parents often reported coming to the decision to select surgery only after exhausting all other treatment options.21–23 Parents expressed feeling like ‘it was the only choice [they] could make’21 and their ‘only option’21 in improving their child’s outcomes or preventing their condition from getting worse. Parents understood there were potential complications associated with surgery, but ‘preferred to take a risk [in proceeding with surgery] rather than live in constant fear’23 or having a child that ‘was unconscious all the time’.22
TDF domain 6: environmental context and resources
Summary statement
Three studies provided evidence that parents face challenges in navigating the healthcare system and interacting with professionals to find the ‘right doctor’ or care team for their child. Parents value having their concerns heard and being engaged in the decision-making process (low confidence).19–21 23
Parents from one study in the USA19 20 and another in Sweden.23 reported experiencing significant barriers with navigating the healthcare system. In the USA,19 20 parents expressed frustration with the extensive time it took to find the right doctor after navigating various doctors from different specialties across multiple institutions. Prior to selecting surgery for their child, parents reported difficulties in finding the ‘right doctor’ with knowledge to ‘effectively identify the problem, and then make a clear plan of action.’ Parents attributed these difficulties to the lack of paediatric neurologists in their local area, inconsistencies in treatment recommendations, and rigid adherence to centre-specific treatment protocols.19 20 Once parents made a decision to pursue surgery, they reported battles with insurance companies to pay for surgery.19 20 Parents in the Sweden study reported similar frustrations with ‘the bureaucracy’ as they felt it took ‘a long time to get a correct diagnosis’ and ‘adequate support’. They thought that it would be helpful if the authorities understood that parents only asked for help when they had reached their limit, and then, urgent help was necessary.23
Parents listed several provider-specific interactions they found to be either enablers or barriers to their experience of identifying and selecting appropriate treatment for their child. With respect to enablers, parents valued when providers validated (and shared) their concerns, gave their time and fostered trust, and engaged parents in the treatment decision-making process. Barriers noted by parents included having their concerns doubted or ignored,19 23 receiving inadequate information or support (especially before the epilepsy was recognised to be drug-resistant),23 and feeling excluded from discussions about their child’s surgical candidacy.21 One study reported that parents perceived physician variability in knowledge about epilepsy and their lack of understanding about the pre-surgical referral process and appropriateness of surgery as barriers.19 Parents in one study reported how they felt more reassured when their child received care from a comprehensive team of professionals with diverse expertise.20 Parents from one study suggested providers give an ‘earlier and softer introduction of surgery as a possible treatment option.’21
See box 1 for example excerpts for TDF domains.
Box 1. Example excerpts for Theoretical Domains Framework domains.
Knowledge
[Parent]: ‘I googled it until I couldn’t google anymore, and I think that gave me a better understanding of what was going on.’21
A mother who stated, ‘I just think knowledge is power and it also brings some comfort to making a good decision,’ exemplified the sense of empowerment associated with gaining fluency in the language of epilepsy.19
Social/professional role and identity
Parents discussed feeling pressure from a need to ‘do the right thing’ by their child; that is, choosing the treatment option that would give their child the best chance of reaching their full potential.21
Emotion
Participant descriptions highlighted the significant impact that epilepsy had on on the child’s and family’s lives prior to epilepsy surgery. Worries about seizures and the associated risks led to constant fatigue for some: ‘you’re tired yourself before you even go out the door’.22
[Parent]: ‘At first I was horrified at the thought of this innocent—having her brain opened and operated on. It just seemed so barbaric’.20
Social influences
Most participants described finding it difficult to talk to others about epilepsy, with several reporting that they limited the information they shared, or withholding the diagnosis altogether. ‘Gosh, we didn’t tell anybody. We were ashamed.’22
[E]xchanging shared experiences with peers gave direction to decision-making because it helped with processing complex factual and emotional information.20
Beliefs about consequences
This transformation occurred as parents became increasingly aware of the severity of their child’s epilepsy and its impact on their child’s and their future life. Although surgery remained scary, epilepsy was or became scarier than surgery. As some parents feared that their child would die from epilepsy, surgery was no longer perceived as an elective treatment.19
They wanted that their child could do everything their friends could do like ‘play football, cycle, and swim independently’. Some parents mentioned that they wanted their child to be able to go back to school and have a ‘proper social life’ while some parents referenced the future hoping that the child would be better placed to get a job and driving license as a result of surgery.24
Parents felt that epilepsy surgery was a question of life or death, of chaos or control. It was terrifying to see the child so ill. The epilepsy was uncontrolled, and drugs gave side effects. Parents felt that there was no alternative to surgery. However, it was a difficult decision since they did not know the outcome.23
Environmental context and resources
Trust and safety characterised the relations to the paediatric neurologists and specialist nurses. It strengthened parents’ trust to see that the paediatric neurologist fought for the child and that the parents’ opinions counted in the decision process. Parents appreciated continuous contact.23
Looking back, one father voiced happiness that he listened to his parental instincts rather than the opinion of one doctor. He (doctor) said, ‘I don’t believe that she is a surgical candidate.’ As a parent, I listened and I wanted to think otherwise…. In hindsight, I’m glad I didn’t listen to him.’19
Discussion
Understanding caregiver perspectives about treatments for childhood epilepsy is important to ensure that parents are appropriately supported during their decision-making process. Our qualitative evidence synthesis of five studies, which had minimal risks to rigour, identified key findings across six domains: knowledge, emotions, social/professional role and identify, social influences, beliefs about consequences, environmental context and resources. However, the evidence was limited surgical treatment. Overall, these findings suggest that the decision to select surgery for childhood epilepsy involves parents going through a complex journey of acquiring extensive knowledge, working through intense emotions and perceived parental responsibilities, needing family and peer support, transforming beliefs about epilepsy and potential treatment options, and navigating various barriers and facilitators of the healthcare system.
These findings are supported by a similar review conducted by Samanta et al that sought to understand caregiver decision making around epilepsy surgery for children with drug-resistant epilepsy.25 In their synthesis of a similar body of evidence, these reviewers identified the following as key determinants: knowledge and information, communication and care coordination, caregivers’ emotional state and socioeconomic factors. While the findings of our review are similar to Samanta, our scope and methodology differ. We sought to explore caregiver decision making around all treatments for epilepsy, not just surgery. We also used rigorous methodological tools (eg, TDF and GRADE-CerQual). Use of these tools strengthens our findings by placing them within a framework that identifies facilitators and barriers, and by providing criteria to establish confidence in the certainty of these findings.
Through the TDF framework, we identified decision domains that presented potential barriers to care that are amenable to action. For example, parents often felt that they did not have enough information to make decisions about surgery. They reported experiencing intense psychological distress and exhaustion during their decision-making process and felt these emotions acutely through their role as parents responsible for making a potentially life-altering decision for their child. Parents also reported valuing connections with peers who were going through (or had gone through) the same experience. Healthcare systems and providers may therefore consider providing parents with resources, such as patient navigators to help guide them through the healthcare system and better understand the care pathway. They can also help parents to access peer support and advocates26 27
The findings also identified gaps in the evidence base regarding parents’ perceptions and decision-making processes. Foremost, we did not identify any studies exploring parent decision making around non-surgical treatment options. Qualitative studies that prospectively explore caregiver decision making about these treatments are needed to determine if perspectives differ from those about surgery. We also did not identify evidence mapping to certain TDF domains that we expected to find evidence for, such as goals. Studies included in this review were vague and inconsistent in reporting parent’s goals or their desired outcomes of treatment. Some studies noted that parents wanted what ‘was best’ for their child or they would be happy with a reduction in seizure frequency. Survey data collected from parents considering surgery found the primary goal was seizure freedom (98%), followed by reduced medication (90%), and improved cognition (82%).28 We also did not identify evidence for the domain of memory, attention and decision process. Thus, we could not determine if parents become more skilled and confident in their decision making over time through experience and acquired knowledge.
Similarly, we found limited evidence for the domain of environmental context and resources. Further evidence is needed to understand how culture and equity play a role in parents’ perceptions about treatment and their capacity to access care for their child. For example, parents reported important barriers in knowledge, access to professionals to diagnose and treat their child, and challenges with accessing and paying for surgery. The extent to which these factors would be the similar among families from different cultural or socioeconomic backgrounds or from countries with varying economic, educational and social resources needs further exploration.
Strengths and limitations
This review followed contemporary standards for the conduct of qualitative synthesis, which includes the use of a best-fit framework approach, a theory-informed framework to guide our synthesis and extraction, and use of the CASP and GRADE-CerQual tool to assess the rigour and confidence of our findings. The use of the TDF is a particular strength of this review as it lends itself to both actionable interventions (eg, mapping intervention strategies to key domains identified) and future research (eg, further examination of domains not identified in the evidence such as ‘memory, attention and decision processes’). However, as with all qualitative research, selecting which data to extract and how to code it is ultimately a subjective process. We attempted to limit subjectivity within our group by coding in duplicate and having regular meetings to ensure consistency across and within domains.
One primary limitation is that the data in all studies included in this were collected retrospectively. Parents were asked for their perceptions after their child had undergone surgery. This may have resulted in selection bias, as studies recruited parents of children referred to and proceeded with surgery. Thus, findings may not be fully reflective of the wider population of parents who are making decisions regarding surgery. The perceptions of parents who declined surgery were not captured. The retrospective nature of the data collection may have also resulted in recall bias. The time from children’s surgery to data collection ranged from 6 months to 10 years. Parents may have forgotten important aspects of their journey to surgery or filled in gaps of memory due to experiences with the child’s outcome. As described by one study, parent responses were ‘memories processed through emotions and coloured from further experiences, which were then developed into opinions and personal views.’23
Conclusion
Parents of children with epilepsy navigate a complex process to decide whether to have their child undergo surgery. Educational resources, peer support and patient navigators may help support parents through this process. More qualitative studies are needed to fully understand the diversity of experiences of parents across various points in the decision-making pathway and among different healthcare contexts. Qualitative studies are needed that address parents’ perceptions and experiences with selecting non-surgical epilepsy treatment options such as diet and medications.
Supplementary Material
Acknowledgments
We would like to give a special thank you to Jane Noyes, MSc, DPhil for her mentorship, review and support in the completion of this manuscript. We would also like to acknowledge Laura Koepfler, MLS of ECRI for her contribution in designing and running the literature searches.
Footnotes
Contributors: SU served as project lead and participated as a team member in identifying studies for inclusion, extracting and coding data, synthesising findings, developing and grading summary statements, and drafting of initial report and manuscript; KK participated as team member in all aspects of data extraction, coding, synthesis, developing and grading summary statements, validating all findings and revising initial drafts of manuscript; RW participated in all aspects of data extraction, coding, synthesis, developing summary statements, and reviewing manuscript; GA coordinated and revised search strategies and participated in all aspects of data extraction, coding, synthesis and review of manuscript; KAR participated in all aspects of data extraction, coding, synthesis, developing summary statements, and reviewing manuscript; MV participated in all aspects of data extraction, coding, synthesis, developing summary statements and reviewing manuscript. All contributors accept full responsibility for the finished work and conduct of the study and had full access to the data and controlled the decision to publish.
Funding: This work was funded by the Agency for Healthcare Research and Quality through the following contracts: RTI-University of North Carolina EPC (290-2015-00011-I), Brown University EPC (290-2015-00002-I), ECRI Institute-Penn Medicine EPC (290-2015-00005-I), Johns Hopkins University EPC (290-2015-00006-I). No award or grant number.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
No data are available.
Ethics statements
Patient consent for publication
Not applicable.
References
- 1.Russ SA, Larson K, Halfon N. A national profile of childhood epilepsy and seizure disorder. Pediatrics 2012;129:256–64. 10.1542/peds.2010-1371 [DOI] [PubMed] [Google Scholar]
- 2.Sarmast ST, Abdullahi AM, Jahan N. Current classification of seizures and epilepsies: scope, limitations and recommendations for future action. Cureus 2020;12:e10549. 10.7759/cureus.10549 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Symonds JD, Elliott KS, Shetty J, et al. Early childhood epilepsies: epidemiology, classification, aetiology, and socio-economic determinants. Brain 2021;144:2879–91. 10.1093/brain/awab162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Scheffer IE, Berkovic S, Capovilla G, et al. ILAE classification of the epilepsies: position paper of the ILAE commission for classification and terminology. Epilepsia 2017;58:512–21. 10.1111/epi.13709 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rodenburg R, Meijer AM, Deković M, et al. Family factors and psychopathology in children with epilepsy: a literature review. Epilepsy Behav 2005;6:488–503. 10.1016/j.yebeh.2005.03.006 [DOI] [PubMed] [Google Scholar]
- 6.Rosati A, De Masi S, Guerrini R. Antiepileptic drug treatment in children with epilepsy. CNS Drugs 2015;29:847–63. 10.1007/s40263-015-0281-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mutanana N, Tsvere M, Chiweshe MK. General side effects and challenges associated with anti-epilepsy medication: a review of related literature. Afr J Prim Health Care Fam Med 2020;12:e1–5.:2162. 10.4102/phcfm.v12i1.2162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wirrell EC. Predicting pharmacoresistance in pediatric epilepsy. Epilepsia 2013;54 Suppl 2:19–22. 10.1111/epi.12179 [DOI] [PubMed] [Google Scholar]
- 9.Martin-McGill KJ, Jackson CF, Bresnahan R, et al. Ketogenic diets for drug-resistant epilepsy. Cochrane Database Syst Rev 2018;11:CD001903. 10.1002/14651858.CD001903.pub4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Noyes J BA, Cargo M, Flemming K, et al. Chapter 21: qualitative evidence. In: Li T, Page MJ, Welch VA, et al., eds. Cochrane Handbook for Systematic Reviews of Interventions version 63. Cochrane, 2019. [Google Scholar]
- 11.Porritt K, Gomersall J, Lockwood C. JBI’s systematic reviews: study selection and critical appraisal. Am J Nurs 2014;114:47–52. 10.1097/01.NAJ.0000450430.97383.64 [DOI] [PubMed] [Google Scholar]
- 12.Wong G, Greenhalgh T, Westhorp G, et al. RAMESES publication standards: meta-narrative reviews. BMC Med 2013;11:20. 10.1186/1741-7015-11-20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Programme CAS . CASP qualitative studies checklist. 2022.
- 14.Michie S, Johnston M, Abraham C, et al. Making psychological theory useful for implementing evidence based practice: a consensus approach. Qual Saf Health Care 2005;14:26–33. 10.1136/qshc.2004.011155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cane J, O’Connor D, Michie S. Validation of the theoretical domains framework for use in behaviour change and implementation research. Implement Sci 2012;7:37. 10.1186/1748-5908-7-37 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Glenton C, Carlsen B, Lewin S, et al. Applying GRADE-cerqual to qualitative evidence synthesis findings-paper 5: how to assess adequacy of data. Implement Sci 2018;13(Suppl 1):14. 10.1186/s13012-017-0692-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Colvin CJ, Garside R, Wainwright M, et al. Applying GRADE-cerqual to qualitative evidence synthesis findings-paper 4: how to assess coherence. Implement Sci 2018;13(Suppl 1):13. 10.1186/s13012-017-0691-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lewin S, Bohren M, Rashidian A, et al. Applying GRADE-cerqual to qualitative evidence synthesis findings-paper 2: how to make an overall cerqual assessment of confidence and create a summary of qualitative findings table. Implement Sci 2018;13(Suppl 1):10. 10.1186/s13012-017-0689-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Baca CB, Pieters HC, Iwaki TJ, et al. “ a journey around the world ”: parent narratives of the journey to pediatric resective epilepsy surgery and beyond. Epilepsia 2015;56:822–32. 10.1111/epi.12988 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pieters HC, Iwaki T, Vickrey BG, et al. “ it was five years of hell ”: parental experiences of navigating and processing the slow and arduous time to pediatric resective epilepsy surgery. Epilepsy Behav 2016;62:276–84.:S1525-5050(16)30263-3. 10.1016/j.yebeh.2016.07.019 [DOI] [PubMed] [Google Scholar]
- 21.Heath G, Abdin S, Begum R, et al. Putting children forward for epilepsy surgery: a qualitative study of UK parents’ and health professionals’ decision-making experiences. Epilepsy Behav 2016;61:185–91. 10.1016/j.yebeh.2016.05.037 [DOI] [PubMed] [Google Scholar]
- 22.O’Brien J, Gray V, Woolfall K. Child and parent experiences of childhood epilepsy surgery and adjustment to life following surgery: a qualitative study. Seizure 2020;83:83–8. 10.1016/j.seizure.2020.10.006 [DOI] [PubMed] [Google Scholar]
- 23.Ozanne A, Verdinelli C, Olsson I, et al. Parental experiences before and long-term after their children’s hemispherotomy - a population-based qualitative study. Epilepsy Behav 2016;60:11–6. 10.1016/j.yebeh.2016.04.025 [DOI] [PubMed] [Google Scholar]
- 24.Sylvén I, Olsson I, Hallböök T, et al. “In the best case seizure-free” - parental hopes and worries before and satisfaction after their child’s epilepsy surgery. Epilepsy Behav 2020;110:107153. 10.1016/j.yebeh.2020.107153 [DOI] [PubMed] [Google Scholar]
- 25.Samanta D, Hoyt ML, Perry MS. Parental experience and decision-making for epilepsy surgery: a systematic review of qualitative and quantitative studies. Epilepsy Behav 2021;123:108263. 10.1016/j.yebeh.2021.108263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Michie S, van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci 2011;6:42. 10.1186/1748-5908-6-42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gainforth HL, Sheals K, Atkins L, et al. Developing interventions to change recycling behaviors: a case study of applying behavioral science. Applied Environmental Education & Communication 2016;15:325–39. 10.1080/1533015X.2016.1241166 [DOI] [Google Scholar]
- 28.Bach Q, Thomale UW, Müller S. Parents’ and children’s decision-making and experiences in pediatric epilepsy surgery. Epilepsy Behav 2020;107:107078. 10.1016/j.yebeh.2020.107078 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2022-066872supp001.pdf (328.1KB, pdf)
Data Availability Statement
No data are available.