Abstract
Congenital syphilis (CS) is a rare entity and one of the most well-known congenital infections. A case of early CS presenting with fulminant sepsis is reported. A high index of suspicion is needed by the clinician to diagnose and treat this potentially life-threatening disease.
Keywords: Congenital syphilis, penicillin, sepsis
Introduction
Congenital syphilis (CS), caused by the transmission of Treponema pallidum (Tp) from mother to fetus via the placental route, is one of the most well-known congenital infections.[1] CS has been classified into early CS, late CS, and stigmata. Early CS is defined as a disease affecting children <2 years.[2] Diagnosis of early CS is difficult because more than half of the affected infants are asymptomatic, and the signs in symptomatic infants may be subtle and nonspecific.
“The eyes see, what the mind knows”
Hence, we report a case of early CS to emphasize that CS still occurs, and a high index of suspicion is needed by the clinician to diagnose and treat this potentially life-threatening disease.
Case Report
A preterm baby was born with thick meconium-stained liquor and required labor room resuscitation. The newborn was intubated and kept on a mechanical ventilator for severe respiratory distress. On systemic examination, the newborn had hepatosplenomegaly, hypotonia in all four limbs, and crepitations on auscultation. There were no cutaneous manifestations. Laboratory findings were suggestive of leukocytosis (TC-22000), thrombocytopenia (50,000), hyperkalemia, hyperbilirubinemia (maximum-19.4), and elevated liver enzymes (SGPT-130 IU/l SGOT-142 IU/l). Venereal disease research laboratory (VDRL) titer was 1:8, and C-reactive protein was 100. Cerebrospinal fluid examination showed random blood sugar – 19, protein – 110, VDRL titer was 1:32 – reactive, and TPHA – reactive. HIV antibody test, blood culture and sensitivity, and TORCH were negative. Chest X-ray shows widening of the right border of the heart and widened mediastinum [Figure 1]. X-ray of the bilateral lower limb was suggestive of periostitis changes [Figure 2]. Ophthalmologic examination showed retinopathy of prematurity with PLUS disease and interstitial keratitis. The mother was asymptomatic with VDRL titer 1:16. The newborn was given intramuscular benzathine penicillin along with intravenous ceftriaxone and inotropes. On the day of the life 3, the patient had active bleeding. INR was 2.9. The patient was re-intubated and given a unit FFP. Intravenous antibiotics were upgraded to meropenem and linezolid. However, the patient succumbed on 3rd day of life due to refractory shock.
Figure 1.
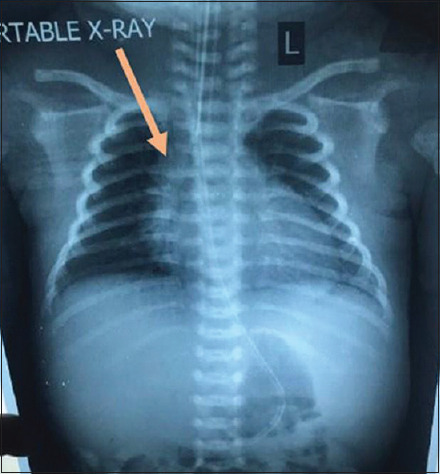
Chest X-ray showing widening of the right border of the heart and widened mediastinum (arrow)
Figure 2.

X-ray bilateral lower limb with hip showing periostitis changes (arrow)
Discussion
CS occurs when Tp crosses the placenta from the mother to the fetus during intrauterine life.
The incidence of CS is 11.6 cases per 100,000 live births in the US.[3] In India, it is 60 cases per 100,000 live births. Congenital infection may result in stillbirth, hydrops fetalis, or premature delivery. Diagnosis of early CS is difficult because more than half of the infants are asymptomatic and signs in symptomatic infants are subtle and nonspecific. If untreated, symptoms develop within weeks or months.[4] Cases may present with hepatosplenomegaly, thrombocytopenia, rhinitis, and condylomatous lesions over mucous membranes. Also, infants present with osteochondritis and periostitis of long bones of upper and lower limbs.[5] Interstitial keratitis, mostly seen in late CS, was also present in this case. The common neurological manifestations in early CS are postneonatal Erb's palsy, pseudo paralysis, and meningitis.
Characteristic mucocutaneous rash, presenting with erythematous maculopapular or bullous lesions, followed by desquamation involving hands and feet, is common in CS.[6]
It may present as vesiculobullous eruptions (sometimes called the syphilitic pemphigus) or erythema multiforme. Although acral dermatitis and vitamin or nutrient deficiency might mimic this disorder, skin rash of early CS is relatively recalcitrant to treatment, which might be the differential diagnostic point.
In addition, symptoms of early CS include fever, failure to thrive, hepatosplenomegaly, lymphadenopathy, osteochondritis, pneumonitis, pseudo paralysis, and rhinitis. Rhinitis (“snuffles”) has been reported in as many as 73%of infants. It usually develops in the 2nd–3rd week of life and may be the earliest clinical sign. Mucocutaneous involvement is present in as many as 70% of infants. They may be apparent at birth or develop during the first few weeks of life.[6] However, in the present case, there were no cutaneous findings.
In terms of laboratory parameters, the present case had leukocytosis, Coombs-negative hemolytic anemia, thrombocytopenia, hypoproteinemia, hypoalbuminemia, hyperbilirubinemia, and elevated liver enzyme levels. Anemia has been found to be associated with early CS. There is no definite known cause of anemia, but it may be attributed to hemolysis, interference with hematopoiesis, hypersplenism, and nutritional deficiency. Thrombocytopenia, in association with hemolytic anemia, is commonly present early in the disease, often before the classical signs of syphilis develop. The cause of thrombocytopenia is postulated due to a decrease in platelet survival rather than a decrease in marrow production.
Jaundice is characterized by elevations of both conjugated and unconjugated bilirubin. Since these laboratory findings are difficult to identify upon physical examination, a high index of suspicion is necessary to make the right diagnosis early.[6] In our case, the patient had anemia, thrombocytopenia, jaundice, elevated liver enzymes, and elevated CSF protein which supported the diagnosis.
As per the standard treatment guidelines, infants fulfilling any one of the following criteria should receive treatment.
Whose RPR/VDRL titer is four-fold higher than that of the mother at delivery
Born to mothers with clinical evidence of syphilis.
Treatment for infants with the proven or highly probable disease should consist of either of the following:
Aqueous crystalline penicillin G 100,000–150,000 units/kg/day IV, administered as 50,000 units/kg/dose IV every 12 h during the first 7 days of life and every 8 h thereafter for a total of 10 days, or
Procaine penicillin G 50,000 units/kg/dose IM daily in a single dose for 10 days.
For infants who are at least 4 weeks of age or older, treatment is aqueous penicillin G 50,000 units/kg/dose every 6 hourly intravenously for 10–14 days because of the difficulty in excluding neurosyphilis in this age group.[6] Prevention of CS requires early diagnosis and appropriate treatment of syphilis-infected mothers. CS can invariably be prevented if treatment is completed at least 2 weeks before delivery. Follow-up should be done at 2nd, 4th, 6th, 12th, and 15th months post treatment.
Conclusion
Although syphilis is one of the age-old diseases, for which effective treatment has been available since the introduction of penicillin in the mid-20th century, the diagnosis of CS, which is now uncommon, should not be precluded.[6]
CS continues to be a public health concern, causing substantial morbidity and adverse outcomes. Rare associations and manifestations of CS need to be identified to prevent adverse outcomes.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Modi M, Sharma A, Marfatia YS, Naik E, Toney J. Late congenital syphilis with stigmata. Indian J Sex Transm Dis AIDS. 2008;29:32.. [Google Scholar]
- 2.Woods CR. Syphilis in children: Congenital and acquired. Semin Pediatr Infect Dis. 2005;16:245–57. doi: 10.1053/j.spid.2005.06.005. [DOI] [PubMed] [Google Scholar]
- 3.Workowski KA, Bolan GA Centers for Disease Control and Prevention. Sexually transmitted diseases treatment guidelines, 2015. MMWR Recomm Rep. 2015;64:1–137. [PMC free article] [PubMed] [Google Scholar]
- 4.American Academy of Pediatrics. Red Book. 26th. Elk Grove Village, IL: American Academy of Pediatrics; 2003. Report of the committee on infectious diseases; p. 595607. [Google Scholar]
- 5.Fan P, Fu M, Liao W, Luan Q, Hu X, Gao T, et al. Early congenital syphilis presented with exclusive bending pain of extremity: Case report. J Dermatol. 2007;34:214–6. doi: 10.1111/j.1346-8138.2007.00253.x. [DOI] [PubMed] [Google Scholar]
- 6.Shah KH, Jagati AG, Rathod SP, Chaudhary RG. Early congenital syphilis: Resurgence of an entity nearing elimination. Indian J PaediatrDermatol. 2019;20:154–6. [Google Scholar]


