Polycystic ovarian syndrome (PCOS) is an endocrinal disorder with a prevalence ranging from 3.7% to 22.5% among the Indian population.[1] Although a medical condition, it clearly has psychosocial ramifications because of the stress and lifestyle factors associated with it.[2,3] Yet, there is limited research highlighting the lived experiences of stress recounted by these women. In general, qualitative studies foregrounding the voices of patients with PCOS are few. The case delineated here illustrates the advantage of doing in-depth interviews, wherein the range of multiple stressors faced by a woman with PCOS becomes evident. Finally, considering the stress experienced by women with PCOS, the case study emphasizes the need for a holistic intervention that moves beyond the biomedical treatment and also addresses the psychosocial factors in PCOS.
This paper reports on a case of a 24-year-old single woman, whom we will call Girishma, who was admitted to the Government Yoga and Naturopathy Hospital and College located inside Arignar Anna Government Hospital of Indian Medicine, Chennai. The clinic mainly provides services to patients with chronic conditions that require lifestyle modifications. The inpatient naturopathy treatment for PCOS patients usually involves following a special diet composed of raw fruits and vegetables along with yoga and natural therapies (like acupuncture, massage, and hydrotherapy). Girishma was taking inpatient treatment for reducing weight and regularizing menstrual cycles. She had been experiencing irregular cycles since the age of 16, and an ultrasound scan taken in 2014 indicated multiple cysts in the ovaries. She had been managing her PCOS by taking medicines for three years. Intermittently, she also opted for naturopathy treatment due to the distressing side effects (swelling and pain in the hands and legs, weight gain, and difficulty breathing) of allopathic medicines. It was during one of these treatment phases, in May 2019, that the first author interviewed her following clearance from the Institutional Ethics Committee of IIT Hyderabad.
Girishma is an engineering graduate, working as an IT professional. She originally hailed from Chennai but had been working in Kerala since December 2017. Her immediate family included her parents and a younger brother. Girishma’s father was the eldest son of his family with three younger siblings. Due to many family responsibilities from an early age, he had become financially drained and was not able to support his marital family as he got older. At the time of the interview, he was working as a welder and did not have a stable source of income. There was also additional stress as Girishma’s mother had been diagnosed with breast cancer at an advanced stage in 2015. Therefore, she was physically and mentally weak after cancer treatment. Girishma also had a younger brother pursuing his undergraduate degree in a private college in Chennai. From her point of view, her brother detached himself from everyone, thereby leaving the entire family burden onto Girishma. Since she did not receive financial support from her family members or relatives, she had to earn by giving tuitions in the evenings ever since her school days. Girishma felt that all this took a toll on her health.
Girishma spoke about health issues as constantly demanding her attention and interfering with her productivity. Her primary health complaints included wheezing, digestion problems, severe abdominal and body pain due to irregular periods, and weight gain. Due to her priorities of managing the family, work, finances, and mother’s health, she said she often neglected her health and skipped meals. Irregular meals, consuming oily foods and fast foods contributed to her weight gain and aggravated her PCOS symptoms.
Sometimes, due to body pain, I cannot even get up from the bed. I actually feel relieved while I get my periods pain because it means I will get my periods now. I know I will feel better after that.
Girishma felt that PCOS has resulted in a great deal of mental stress for her. Apart from her health complaints, she felt unhealthy and had difficulty in walking and breathing. As she said, “PCOS is like having a disease.” The feeling of “having PCOS” or being a patient of PCOS weighed on her. The idea of being “abnormal” due to irregular menses and lacking an essential bodily function which she imagined her peers did added to her worries. Further, Girishma was also disturbed by the side effects of medicines such as weakness and weight gain.
I feel that I am not like other girls who get their menses regularly. I feel it (PCOS) is like having a disease, and I have lots of health complaints because of it.
Apart from stress arising from her family situation, financial issues, and health complaints, Girishma was also concerned about her future marriage prospects, largely feeling pressured by her mother’s expectations. She said that her mother wanted her to get married soon but was worried that PCOS might affect her fertility. But Girishma was hesitant, considering the financial situation of her family and the additional responsibilities that marriage would bring. She felt that it would be better to focus on bringing her PCOS under control before marriage.
I don’t want others to say something (negative) after marriage. I don’t want to take that stress. Let’s say I have a problem in conceiving, then, immediately, everyone will start saying that ‘she has PCOS’. So, let me cure this before marriage itself.
Girishma’s case illustrates the multiple stressors that were impinging on her from different directions. There is evidence that stress has an adverse effect on PCOS, as it results in hormonal imbalance and decreases the chances of recovering from the condition.[4] Figure 1 depicts the stressors related to PCOS on one side and the stressors emanating from other factors of life on the other. Ultimately, all of these influence each other, exacerbating the Girishma’s overall stress levels.
Figure 1.
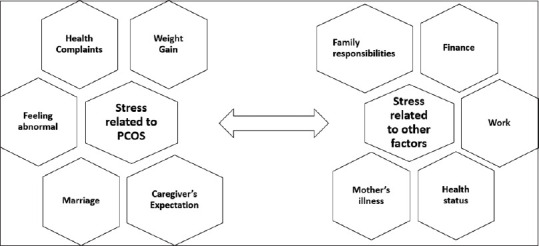
Stress related to PCOS and others factors influencing each other (Source: Original)
The case of Girishma helps us to understand that PCOS is not merely a medical condition but a lifestyle disorder in which several factors play a role. Therefore, only focusing on the physical symptoms and providing medication for the treatment of PCOS is not sufficient. It is also essential to reduce the stress levels of the patient through other supportive services. Through this case, we seek to emphasize the importance of qualitative research for understanding PCOS as a complex lifestyle disorder with multiple ramifications. Any approach to PCOS, therefore, needs to deal with it not only as a physical condition but also needs to reduce the patient’s burden and stress by working at multiple levels, including helping them make lifestyle changes.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgements
We would like to acknowledge the Government Yoga and Naturopathy Hospital and College, inside the campus of Arignar Anna Government Hospital of Indian Medicine, for giving us permission to carry out the study and all the informants for sharing their experiences with us. This research is part of the doctoral thesis of the first author, funding for which was received by the University Grants Commission.
REFERENCES
- 1.Ganie MA, Vasudevan V, Wani IA, Baba MS, Arif T. Epidemiology, pathogenesis, genetics &management of polycystic ovary syndrome in India. Indian J Med Res. 2019;150:333–44. doi: 10.4103/ijmr.IJMR_1937_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pathak G, Nichter M. Polycystic ovary syndrome in globalizing India:An ecosocial perspective on an emerging lifestyle disease. Soc Sci Med. 2015;146:21–8. doi: 10.1016/j.socscimed.2015.10.007. [DOI] [PubMed] [Google Scholar]
- 3.Manlove HA. “Polycystic ovary syndrome (PCOS) in urban India”. UNLV Theses, Dissertations, Professional Papers, and Capstones. 2011:936. http://dx.doi.org/10.34917/2269240. [Google Scholar]
- 4.Papalou O, Diamanti-Kandarakis E. The role of stress in PCOS. Expert Rev Endocrinol Metab. 2017;12:87–95. doi: 10.1080/17446651.2017.1266250. [DOI] [PubMed] [Google Scholar]


