Abstract
Background
The American Cancer Society, National Cancer Institute, Centers for Disease Control and Prevention, and North American Association of Central Cancer Registries provide annual information about cancer occurrence and trends in the United States. Part 1 of this annual report focuses on national cancer statistics. This study is part 2, which quantifies patient economic burden associated with cancer care.
Methods
We used complementary data sources, linked Surveillance, Epidemiology, and End Results-Medicare, and the Medical Expenditure Panel Survey to develop comprehensive estimates of patient economic burden, including out-of-pocket and patient time costs, associated with cancer care. The 2000-2013 Surveillance, Epidemiology, and End Results-Medicare data were used to estimate net patient out-of-pocket costs among adults aged 65 years and older for the initial, continuing, and end-of-life phases of care for all cancer sites combined and separately for the 21 most common cancer sites. The 2008-2017 Medical Expenditure Panel Survey data were used to calculate out-of-pocket costs and time costs associated with cancer among adults aged 18-64 years and 65 years and older.
Results
Across all cancer sites, annualized net out-of-pocket costs for medical services and prescriptions drugs covered through a pharmacy benefit among adults aged 65 years and older were highest in the initial ($2200 and $243, respectively) and end-of-life phases ($3823 and $448, respectively) and lowest in the continuing phase ($466 and $127, respectively), with substantial variation by cancer site. Out-of-pocket costs were generally higher for patients diagnosed with later-stage disease. Net annual time costs associated with cancer were $304.3 (95% confidence interval = $257.9 to $350.9) and $279.1 (95% confidence interval = $215.1 to $343.3) for adults aged 18-64 years and ≥65 years, respectively, with higher time costs among more recently diagnosed survivors. National patient economic burden, including out-of-pocket and time costs, associated with cancer care was projected to be $21.1 billion in 2019.
Conclusions
This comprehensive study found that the patient economic burden associated with cancer care is substantial in the United States at the national and patient levels.
Each year, the American Cancer Society, the National Cancer Institute, the Centers for Disease Control and Prevention, and the North American Association of Central Cancer Registries collaborate to provide updated information about cancer occurrence and trends by cancer site, sex, race and ethnicity , and age in the United States. Part 1 of this annual report focuses on national cancer statistics and highlights trends in stage-specific survival for melanoma of the skin (1). This study is part 2 of the report and addresses patient economic burden associated with cancer in the United States.
Historically, cancer has been one of the most expensive medical conditions to treat (2), and spending has increased in recent years (3) due in part to advances in cancer treatment, including targeted therapies, immunotherapies, advanced imaging, and supportive care; longer treatment durations; and more treatment combinations. Many people who have received a cancer diagnosis (cancer survivors) receive medical care directly related to their cancer during the initial period after diagnosis and for some, recurrence or new primaries, and at the end-of-life (EOL) (4-6). Many receive additional medical care as a result of late and lasting effects of disease and its treatment (4–6). Cancer survivors and their families increasingly face high out-of-pocket costs for their care (3,7,8), including patient cost-sharing through higher deductibles, copayments, and coinsurance (9–11). In the absence of charity care, families without health insurance or with limited coverage may be responsible for the entire cost of care (12,13). Medical financial hardship is increasingly common, with many cancer survivors reporting difficulty paying medical bills, high levels of financial distress, and delaying care or forgoing care altogether because of cost (14).
In addition to out-of-pocket expenses, cancer survivors also spend time traveling to and from care and waiting for and receiving care, which represents time not spent pursuing other activities, including work and leisure (15–18). This time spent receiving medical care (“patient time cost”) is referred to as an opportunity cost by health economists. Prior research has shown that patient time costs can be substantial (15–17) and can result in additional economic burdens for cancer survivors. Academic health economists have long recommended including these time costs in cost-effectiveness analyses of medical interventions (19,20). Estimates of patient out-of-pocket and time costs may also be useful for both providers and patients as part of informed decision-making.
Prior research estimating out-of-pocket costs in cancer survivors was limited by lack of detail on cancer site and stage at diagnosis (21,22). Similarly, most prior research estimating patient time costs has been limited by a lack of information for adults aged 18-64 years, who are not age-eligible for Medicare coverage (15,16). In this study, we build on and extend prior research estimating health care costs associated with cancer by phase of care using the Surveillance, Epidemiology, and End Results (SEER) registry data linked with Medicare enrollment and claims data (SEER-Medicare) to provide detailed estimates of out-of-pocket costs (4,6,23,24) by cancer site and stage for adults aged ≥65 years, and the Medical Expenditure Panel Survey (MEPS) data to provide out-of-pocket (21) and patient time costs (17) stratified by age group (18-64 years and ≥65 years), with all insurance coverage types. These data sources are complementary, and, to the extent possible, we take advantage of the populations included and level of clinical detail to provide comprehensive information about patient economic burden associated with cancer.
Methods
Data Sources
SEER-Medicare. The SEER data include age at cancer diagnosis, cancer site, stage at diagnosis, and date of diagnosis for patients living in SEER geographic areas diagnosed with incident cancers; patients were followed for vital status and cause of death (25). Medicare is the federal health insurance program that covers approximately 95% of adults aged 65 years and older and some younger adults with certain disabilities or medical conditions (eg, end-stage renal disease) (26). Medicare enrollment data contain demographic characteristics and monthly indicators for enrollment in fee-for-service Parts A (inpatient stays), B (physician and outpatient services), and D (prescription drugs covered through a pharmacy benefit) (27). The Medicare Part D pharmacy benefit for prescription drug coverage was introduced in 2006 (28), and approximately 60% of Medicare beneficiaries had Part D coverage during the study period (4). Medicare claims data include payments and dates of service. The linked SEER-Medicare database also includes a 5% random sample of all Medicare beneficiaries residing in the SEER areas (26). Medicare beneficiaries in the 5% random sample without a cancer diagnosis serve as controls for calculation of medical care costs associated with a cancer diagnosis. The SEER-Medicare data in years 2000-2013 were used in this study to identify cancer patients and survivors; vital status was measured through December 31, 2013. The observation period for estimating spending was 2007-2013.
Medical Expenditure Panel Survey. The MEPS is an annual nationally representative household survey of health care access, use, and expenditures in the US civilian noninstitutionalized population (29). Adults of all ages and types of health insurance coverage, including the uninsured, are surveyed by the MEPS. In-person interviews are supplemented with additional information about types of health-care services and payments by source, including out-of-pocket payments, from a sample of medical care providers, including physicians, hospitals, and pharmacies, for household survey respondents. The MEPS provides annual information about hospital inpatient stays, emergency room visits, medical provider and outpatient visits, and prescription drugs. The 2008-2017 MEPS data were used in this study and had a combined average annual response rate ranging from 44% to 59% (29).
Estimating Annualized Net Patient Responsibility and Out-of-Pocket Costs With SEER-Medicare Data
We estimated patient responsibility (the amount not paid by Medicare but by patients and other payers) and out-of-pocket costs associated with cancer for both Medicare Parts A and B and Part D from the SEER-Medicare data, respectively. We identified adults diagnosed with any cancer, between 2000 and 2012 from SEER, building on a prior study of all medical care costs associated with cancer (4). Survivors were required to have at least 1 month of observation between 2007 and 2013 in which they were aged 65 years and older and enrolled in fee-for-service Medicare with both Part A and Part B coverage; only those who also had Part D coverage were included in analyses of prescription drugs covered through a pharmacy benefit. Information was reported for the 21 most common cancer sites as well as all cancer sites combined. We used SEER historic staging to classify solid tumors into localized-, regional-, or distant-stage disease at diagnosis.
Phase of Care Definitions for Cancer Survivors and Controls. We used a phase-of-care approach to assign months of observation between 2007 and 2013 after cancer diagnosis into 3 clinically relevant phases, consistent with previous studies (4,6,24). Phases include the initial phase, defined as the first 12 months after each diagnosis; the EOL phase, defined as the 12 months before death among survivors who died; and the continuing phase, the months between the initial and the EOL phases (4–6). Patients contributed months of observation to phases of care based on the date of their diagnosis and date of death, if they died before December 31, 2013, relative to the study observation period of 2007-2013. Not all patients contributed months of observation to all phases of care. Patients diagnosed before 2006 did not contribute to the initial phase, and patients who survived through 2013 did not contribute to the EOL phase. We further divided the EOL phase into months of observation contributed by survivors who died from cancer (EOL-cancer death) or from other causes (EOL-noncancer death) based on information from the death certificate from SEER. For cancer patients who survived less than 24 months after their cancer diagnosis, months were first assigned to the EOL phase and any remaining months were then assigned to the initial phase. Patients who survived 12 months or less following diagnosis only contributed to the EOL phase.
Months of observation for controls were assigned to 2 phases: the EOL phase defined as the 12 months before death among controls who died and the continuing phase that included all other months. Once the months of observation for cases and controls were allocated to the respective phases, they were then stratified by calendar year.
Months of observation for cancer survivors and controls were matched in a 1:1 ratio by phase of care (described below), calendar year, registry, sex, age (to the nearest year), race, and Medicare Part D enrollment and entitlement status (described below). If more than 1 control was eligible for matching to a specific case, the control was randomly selected. Because not all Medicare beneficiaries have Part D prescription drug coverage, Medicare Part D enrollment and entitlement status were categorized as not enrolled in Part D, Part D low-income subsidy (LIS), and Part D non-LIS. Approximately 28% of Medicare Part D beneficiaries in this sample receive LIS (4), which helps beneficiaries with low income and limited assets by limiting their out-of-pocket payments for generic and branded prescription drugs (30). Months of observation for controls in the continuing phase were matched to those for cases in the initial, continuing, and EOL-cancer death phases, because it is assumed that health-care use and costs for controls approximate the noncancer use and costs for the cases. Months of observation for controls in the EOL phase were matched to those for cases in the EOL-noncancer death phase, consistent with prior studies.
Estimation of Annualized Net Patient Responsibility and Out-of-Pocket Costs. Medicare Part A and Part B claims data contain information about Medicare payments and patient responsibility, a total amount that includes out-of-pocket costs (ie, deductibles, fixed copayments, coinsurance rates as a percentage of service costs) as well as payments from other insurers (31). Patient responsibility was calculated for each month of observation from amounts listed in the claims based on date of service. Mean monthly net patient responsibility associated with cancer was calculated as the difference between cases and controls. The individual components of patient responsibility are not reported separately by payment source (ie, patient, other insurer), and as a result, patient out-of-pocket costs cannot be estimated directly from Medicare Part A and Part B claims data. We used information from the MEPS (described below) to estimate out-of-pocket costs from patient responsibility amounts for Medicare Part A and Part B medical services. First, we estimated the components of annual patient responsibility among Medicare beneficiaries with a cancer history by payer type (ie, other insurer, patients) from the MEPS. Then we calculated the percentage of patient out-of-pocket costs relative to patient responsibility amount (28.9%) from the MEPS and applied this percentage to patient responsibility amounts for Medicare Part A and Part B medical services to estimate the patient out-of-pocket costs.
Unlike Medicare Part A and Part B claims data, Medicare Part D claims data contain information on patient out-of-pocket payments, including copayments, coinsurance rates as a percentage of prescription drug cost, and deductibles (24). Patient out-of-pocket cost was calculated for each month of observation from amounts listed in the Part D claims based on date of service.
Statistical Analyses. The mean monthly patient out-of-pocket cost associated with cancer was estimated as the difference between the mean monthly cost between cases and controls matched on phase of care, calendar year, registry, sex, age, race, and Medicare Part D enrollment and entitlement status. All costs are reported as annualized mean costs and inflated to 2019 US dollars using the Consumer Price Index for medical care. Estimates of means, standard errors, and medians were calculated for net patient responsibility and out-of-pocket costs for Medicare Part A and B claims and Medicare Part D claims, respectively, by phase of care, cancer site, and stage at diagnosis.
Estimating Patient Out-of-Pocket and Time Costs With MEPS Data
We estimated out-of-pocket and time costs among cancer survivors and adults without a cancer history (as the comparison group) from the MEPS data stratified by age group (18-64 years and ≥65 years). Cancer survivors were identified from a question asking if a doctor or other health professional had ever told the person they had cancer or a malignancy of any kind. Respondents were asked about their age(s) at each cancer diagnosis, and the time since first cancer diagnosis was calculated as the difference between age at first diagnosis and age at the survey interview and categorized as less than 2 years, 2-5 years, 6-10 years, and longer than 10 years, or unknown. Other characteristics included sex, race and ethnicity, marital status, educational attainment, health insurance coverage, and MEPS priority conditions (arthritis, asthma, diabetes, emphysema, heart disease [angina, coronary heart disease, heart attack, other heart condition or disease], high cholesterol, hypertension, and stroke), which were classified by the total number of conditions.
Annual Out-of-Pocket Spending Statistical Analyses. Annual out-of-pocket medical spending measured in the MEPS included patient out-of-pocket payments for hospital inpatient stays, emergency room visits, provider and outpatient visits, prescription drugs, and other medical services not covered by health insurance. Net out-of-pocket spending associated with cancer was calculated as the difference between cancer survivors and adults without a cancer history by age group. All spending was adjusted to 2019 US dollars. To preserve sample weights and nationally representativeness of our estimates, we did not match adults without a cancer history to cancer survivors. Instead we used multivariable 2-part models to estimate out-of-pocket costs adjusted for characteristics that vary between adults with and without a cancer history, including age, sex, educational attainment, and number of comorbid conditions. In the 2-part model, the first part is a logistic model for the probability of having any spending, followed by a generalized linear model with a gamma distribution and a log link among individuals with any spending. This approach is commonly used with health-care spending data because of the many individuals with zero spending and the skewness of the distribution among individuals with any spending (21,22,32,33). P less than .05 was considered statistically significant, and all tests of statistical significance were 2-sided. All estimates were weighted to account for the MEPS complex survey design and survey nonresponse.
Annual Patient Time Costs. Patient time costs include round-trip travel to care, waiting for care, and receiving care and were estimated by calculating annual medical service frequencies, applying service-specific time estimates, summarizing annual patient time, and multiplying by the hourly value of patient time, as has been done elsewhere (15–17). Medical service categories were identified from the MEPS visit files and consolidated files (29) and included overnight hospitalizations, emergency room visits, ambulatory surgery, provider office-based or hospital outpatient visits, chemotherapy, and radiation therapy. The MEPS stopped collecting information separately about chemotherapy and radiation therapy in 2013; estimates of service frequencies for chemotherapy and radiation therapy are based on data from 2008-2012 only. Annual service frequency was calculated for each service category. The annual hospital length of stay was a summary of inpatient days from all hospitalizations for the year.
Estimates of patient time associated with round-trip travel to care, waiting for care, and receiving care were calculated separately for each service category using national data sources from previously published studies (15–17). For example, the average time spent with a physician during an office visit in these earlier studies was calculated from the National Ambulatory Medical Care Survey. Patient time for emergency room visits was calculated as the difference between arrival time and discharge time from the National Hospital Ambulatory Medical Care Survey Emergency Department Patient Record. Patient time in the hospital (in days) was measured as the difference between admission and discharge dates and multiplied by 16 hours, an estimate of waking hours that could alternatively be spent pursuing usual activities, including work and leisure. Round-trip travel time to usual source of medical care was estimated from responses to a question from the MEPS about how long it takes to get to the usual medical provider and was added to all service time estimates. Waiting time was added to office-based or hospital outpatient visits, chemotherapy, and radiation therapy estimates. Time estimates for emergency room visits, hospitalizations, and ambulatory surgeries were based on the difference between admission and discharge time, so waiting time was not added to these estimates separately. All patient time estimates were estimated separately by metropolitan statistical area and nonmetropolitan statistical area status to reflect any differences in urban and rural travel, wait time, or practice patterns. As in previous studies (15–17), we used the median US wage ($19.14/h in 2019) to value patient time in our primary analyses of all services as well as for service-specific estimates. Another approach for valuing patient time based on age- and sex-specific wages, also known as the “human capital” approach (17,18), differentially values time for people not in the workforce or who have lower-paying jobs than for people with higher-paid work. In this study, we chose to value patient time equally with the median wage to avoid these inequities.
Annual Patient Time Cost Statistical Analyses. Estimates of annual service frequencies, patient time, and patient time costs for cancer survivors and adults without a cancer history used separate multivariable analyses to control for age, sex, educational attainment, and the number of comorbid conditions. We present adjusted predicted marginals from the multivariable regression analyses, which directly standardize the outcome of each group to the covariate distribution of the overall population (34). These standardized results can be compared like percentages. Net patient time cost associated with cancer was calculated as the difference in time costs between cancer survivors and adults without a cancer history by age group. P less than .05 was considered statistically significant, and all tests of statistical significance were 2-sided. All estimates were weighted to account for the MEPS complex survey design and survey nonresponse.
Estimating Net Patient Economic Burden Associated With Cancer Care in the United States in 2019
We combined previously published projections of cancer prevalence by phase of care in 2019 for all cancer sites overall and for 15 selected cancer sites (4) by age group (<65 years and ≥65 years) with annualized net estimates of out-of-pocket costs for medical services and prescription drugs covered through a pharmacy benefit by phase of care from SEER-Medicare to create national estimates of out-of-pocket spending in 2019. To reflect the greater net out-of-pocket spending associated with cancer in the younger age group, we used annual spending amounts for medical services and prescription drugs by age group (<65 years and ≥65 years) from the MEPS to adjust the SEER-Medicare estimates in the initial and last year of life-cancer death phases. This general approach has been used previously in estimating and projecting national spending associated with cancer based on SEER-Medicare data. Annual net patient time cost estimates from the MEPS by age group were also combined with the prevalence projections in 2019 to estimate national patient time costs. The sum of out-of-pocket and time costs reflects the national net patient economic burden associated with cancer care in 2019.
Results
Patient Responsibility and Net Out-of-Pocket Cost Estimates From SEER-Medicare Data
During 2007-2013, more than 800 000 newly diagnosed patients with cancer aged 65 years and older contributed to the initial phase of care, approximately 1 317 000 to the continuing phase, and approximately 437 000 to the EOL phase for medical services (Medicare Part A and Part B) (Table 1). The number of newly diagnosed patients with cancer and controls contributing to each phase of care by cancer site for prescription drugs covered through a pharmacy benefit was smaller (Supplementary Table 1, available online), because not all Medicare beneficiaries elected to enroll in Part D for prescription drug coverage.
Table 1.
Number of cancer patients aged 65 years and older, with Medicare Fee-for-Service Part A and Part B, SEER-Medicare 2007-2013a
| Cancer site | Phase of care |
|||
|---|---|---|---|---|
| Initial | Continuing | End-of-life |
||
| Cancer | Other cause | |||
| Bladder | 52 490 | 74 913 | 15 180 | 19 633 |
| Brain | 2882 | 2490 | 7845 | 1705 |
| Breast | 126 034 | 250 192 | 22 527 | 35 908 |
| Cervix uteri | 2238 | 4224 | 1618 | 743 |
| Colorectal | 81 226 | 137 618 | 42 023 | 34 596 |
| Esophagus | 5275 | 5125 | 8449 | 1689 |
| Hodgkin lymphoma | 1450 | 2529 | 854 | 563 |
| Kidney | 26 754 | 40 003 | 10 817 | 8160 |
| Leukemia | 18 366 | 24 824 | 15 128 | 7389 |
| AML | 2226 | 1804 | 7416 | 1041 |
| CLL | 11 763 | 17 513 | 3805 | 4344 |
| CML | 2598 | 3181 | 1519 | 1225 |
| Liver | 5644 | 4968 | 9280 | 2295 |
| Lung | 73 836 | 70 089 | 124 277 | 24 747 |
| NSCLC | 68 128 | 66 400 | 106 775 | 23 007 |
| SCLC | 5708 | 3689 | 17 502 | 1740 |
| Melanoma | 64 428 | 97 579 | 7212 | 15 635 |
| Myeloma | 11 734 | 13 944 | 9650 | 3733 |
| Non-Hodgkin lymphoma | 34 448 | 52 908 | 18 048 | 11 367 |
| Oral cavity or pharynx | 15 858 | 23 432 | 8261 | 5277 |
| Ovary | 8088 | 11 807 | 10 241 | 1492 |
| Pancreas | 8804 | 5321 | 29 571 | 2458 |
| Prostate | 158 840 | 335 539 | 23 403 | 48 559 |
| Stomach | 9411 | 10 623 | 11 809 | 3333 |
| Thyroid | 10 684 | 19 255 | 1688 | 1714 |
| Uterus | 22 098 | 42 161 | 7561 | 5804 |
| All sites combined | 808 148 | 1 316 976 | 436 986 | 270 816 |
Includes patients diagnosed with in-situ and invasive cancers. AML = acute myeloid leukemia; CLL = chronic lymphocytic leukemia; CML = chronic myeloid leukemia; NSCLC = non-small cell lung cancer; SCLC = small cell lung cancer; SEER = Surveillance, Epidemiology, and End Results Program. The reference source for this table is Mariotto et al., 2020 (4).
Annualized Net Patient Out-of-Pocket Costs by Cancer Site and Phase of Care. Annualized net patient out-of-pocket costs by cancer site and phase of care were calculated from the net patient responsibility estimates reported in Supplementary Table 2 (available online). Averaged across all cancer sites, out-of-pocket costs associated with cancer for medical services were highest in the initial ($2200) and EOL ($3823) phases and lowest in the continuing phase ($466), following a “U” or “J” shaped curve (Table 2). By cancer site, out-of-pocket costs for medical services were highest in the initial and end-of life phases for acute myeloid leukemia ($6093 and $7039, respectively) and brain cancer ($5751 and $5901, respectively) and in the continuing phase for myeloma ($1532), pancreatic cancer ($1083), and acute myeloid leukemia ($1056).
Table 2.
Net annualized patient out-of-pocket costs associated with cancer by phase of care, SEER-Medicare 2007-2013a,b,c
| Cancer site | Medical services (Medicare parts A and B) |
Prescription drugs covered through pharmacy benefit (Medicare part D) |
Medical services and prescription drugs |
||||||
|---|---|---|---|---|---|---|---|---|---|
| Initial | Continuing | End-of-life cancer death | Initial | Continuing | End-of-life cancer death | Initial | Continuing | End-of-life cancer death | |
| Bladder | $1472 | $503 | $3195 | $154 | $119 | $201 | $1626 | $622 | $3396 |
| Brain | $5751 | $975 | $5901 | $522 | $247 | $479 | $6273 | $1222 | $6380 |
| Breast | $2206 | $384 | $2852 | $202 | $167 | $275 | $2408 | $551 | $3127 |
| Cervix uteri | $3038 | $349 | $3148 | −$6 | −$36 | $29 | $3032 | $313 | $3177 |
| Colorectal | $2641 | $482 | $3857 | $66 | $30 | $91 | $2706 | $512 | $3948 |
| Esophagus | $4196 | $664 | $4459 | $336 | $113 | $210 | $4532 | $777 | $4669 |
| Hodgkin lymphoma | $3802 | $617 | $4201 | $378 | $75 | $384 | $4180 | $693 | $4585 |
| Kidney | $1693 | $606 | $3388 | $309 | $222 | $938 | $2003 | $827 | $4326 |
| Leukemia | $1973 | $797 | $5176 | $642 | $413 | $582 | $2615 | $1210 | $5758 |
| AML | $6093 | $1056 | $7039 | $1267 | $335 | $639 | $7359 | $1392 | $7678 |
| CLL | $1318 | $790 | $3393 | $122 | $117 | $333 | $1440 | $907 | $3726 |
| CML | $1572 | $799 | $4342 | $2456 | $2341 | $946 | $4028 | $3141 | $5288 |
| Liver | $2746 | $970 | $2745 | $577 | $466 | $773 | $3323 | $1436 | $3517 |
| Lung | $3140 | $780 | $4003 | $460 | $309 | $546 | $3601 | $1089 | $4550 |
| NSCLC | $3050 | $776 | $3930 | $470 | $312 | $588 | $3519 | $1089 | $4518 |
| SCLC | $4461 | $861 | $4474 | $325 | $236 | $274 | $4786 | $1097 | $4748 |
| Melanoma | $662 | $340 | $2980 | $123 | $95 | $440 | $786 | $434 | $3420 |
| Myeloma | $3562 | $1532 | $4132 | $2576 | $1593 | $1818 | $6138 | $3125 | $5950 |
| Non-Hodgkin lymphoma | $3767 | $848 | $4940 | $219 | $88 | $297 | $3987 | $936 | $5237 |
| Oral cavity or pharynx | $3029 | $465 | $3978 | $161 | $36 | $186 | $3191 | $500 | $4164 |
| Ovary | $3166 | $902 | $3907 | $154 | $6 | $142 | $3320 | $908 | $4049 |
| Pancreas | $4280 | $1083 | $4158 | $819 | $519 | $871 | $5099 | $1602 | $5029 |
| Prostate | $1819 | $335 | $2830 | $95 | $48 | $533 | $1914 | $382 | $3363 |
| Stomach | $3116 | $534 | $4007 | $308 | $145 | $164 | $3424 | $678 | $4172 |
| Thyroid | $1354 | $415 | $3347 | $228 | $177 | $434 | $1582 | $592 | $3782 |
| Uterus | $1944 | $337 | $3187 | $40 | $15 | $146 | $1984 | $352 | $3333 |
| All sites combined | $2200 | $466 | $3823 | $243 | $127 | $448 | $2443 | $593 | $4271 |
Includes patients diagnosed with in-situ and invasive cancers. AML = acute myeloid leukemia; CLL = chronic lymphocytic leukemia; CML = chronic myeloid leukemia; NSCLC = non-small cell lung cancer; SCLC = small cell lung cancer; SEER = Surveillance, Epidemiology, and End Results Program.
Costs associated with cancer are estimated as the difference between cancer cases and matched controls. All estimates in 2019 US dollars.
Out-of-pocket costs estimated from patient responsibility for medical services (including infusion drugs) under Medicare Parts A/B claims. Out-of-pocket costs for oral prescription drugs estimated directly from Medicare Part D claims.
Out-of-pocket costs for prescription medications covered through a pharmacy benefit followed the same pattern overall by phase of care (initial = $243, EOL = $448, and continuing = $127), with some differences by cancer site (Table 2; Supplementary Table 3, available online). By cancer site, out-of-pocket costs were highest in the initial, continuing, and EOL phases for chronic myeloid leukemia (CML; $2456, $2341, and $946, respectively) and myeloma ($2576, $1593, and $1818, respectively). Notably, annualized out-of-pocket costs by phase of care for CML and myeloma were less consistent with a “U-shaped” curve by phase of care.
Annualized Net Patient Out-of-Pocket Costs by Cancer Site, Phase of Care, and Stage at Diagnosis. Across all cancer sites, annualized net patient out-of-pocket costs for medical services were lowest for patients originally diagnosed with localized disease compared with regional or distant disease (Table 3; patient responsibility estimates are found in Supplementary Table 4, available online). In the initial phase of care, annualized costs were $1694, $3194, and $3540 for cancers diagnosed with localized, regional, or distant disease, respectively; differences in out-of-pocket costs between localized and distant stage at diagnosis were greatest for bladder, colorectal, non-small cell lung cancer (NSCLC), oral cavity or pharynx, and stomach cancers.
Table 3.
Net annualized patient out-of-pocket costs for medical services and prescription drugs by phase of care and stage at diagnosis, SEER-Medicare 2007-2013a,b,c
| Service type and cancer site | Phase of care |
|||||
|---|---|---|---|---|---|---|
| Initial phase |
End-of-life cancer death |
|||||
| Localized | Regional | Distant | Localized | Regional | Distant | |
| Medical services (Medicare Parts A/B) | ||||||
| Bladder | $1244 | $2956 | $3952 | $2634 | $3564 | $4810 |
| Breast | $2053 | $3108 | $3711 | $2479 | $2893 | $3677 |
| Cervix uteri | $2221 | $3572 | $4100 | $2770 | $3102 | $3690 |
| Colorectal | $1755 | $3283 | $5953 | $3000 | $3616 | $4932 |
| Esophagus | $3379 | $5092 | $4878 | $3914 | $4467 | $5002 |
| Kidney | $1508 | $1993 | $3140 | $3007 | $3449 | $4006 |
| Liver | $2742 | $2829 | $3714 | $2647 | $2708 | $3631 |
| Lung | $2238 | $3406 | $4567 | $2840 | $3605 | $4756 |
| NSCLC | $2207 | $3313 | $4542 | $2816 | $3540 | $4755 |
| SCLC | $3514 | $4559 | $4745 | $3274 | $4068 | $4761 |
| Melanoma | $706 | $1636 | $2719 | $2498 | $2892 | $4575 |
| Oral cavity or pharynx | $1727 | $4044 | $4645 | $3178 | $4154 | $4476 |
| Ovary | $1891 | $3022 | $3565 | $2965 | $3098 | $4086 |
| Pancreas | $3133 | $4858 | $4646 | $3519 | $4256 | $4571 |
| Prostated | $1834 | $1826 | $2800 | $3047 | ||
| Stomach | $2358 | $4260 | $4731 | $3289 | $4010 | $4882 |
| Thyroid | $1149 | $1644 | $2520 | $3094 | $3491 | $3480 |
| Uterus | $1575 | $2769 | $3430 | $2858 | $3278 | $3706 |
| All sites combined | $1694 | $3194 | $3540 | $2868 | $3604 | $4526 |
| Prescription drugs covered through pharmacy benefit (Medicare part D) | ||||||
| Bladder | $154 | $146 | $195 | $248 | $143 | $226 |
| Breast | $214 | $251 | $280 | $302 | $279 | $271 |
| Cervix uteri | −$6 | −$28 | $92 | −$53 | $44 | $32 |
| Colorectal | $64 | $48 | $115 | $94 | $94 | $102 |
| Esophagus | $415 | $235 | $444 | $193 | $169 | $341 |
| Kidney | $224 | $302 | $1713 | $627 | $979 | $1326 |
| Liver | $490 | $754 | $1435 | $591 | $1008 | $1336 |
| Lung | $325 | $408 | $787 | $484 | $513 | $618 |
| NSCLC | $324 | $417 | $851 | $499 | $550 | $687 |
| SCLC | $360 | $305 | $346 | $206 | $251 | $290 |
| Melanoma | $125 | $236 | $434 | $445 | $350 | $438 |
| Oral cavity or pharynx | $99 | $197 | $198 | $350 | $136 | $211 |
| Ovary | −$5 | −$11 | $221 | $289 | $50 | $145 |
| Pancreas | $449 | $796 | $1308 | $521 | $897 | $1057 |
| Prostated | $85 | $290 | $507 | $640 | ||
| Stomach | $291 | $221 | $596 | $120 | $134 | $268 |
| Thyroid | $222 | $232 | $316 | $745 | $434 | $218 |
| Uterus | $24 | $55 | $87 | $140 | $126 | $195 |
| All sites combined | $180 | $224 | $833 | $342 | $373 | $613 |
Includes patients diagnosed with invasive cancers with information about stage at diagnosis; patients diagnosed with in-situ disease or missing information about stage were excluded from stage-specific analyses. NSCLC = non-small cell lung cancer; SCLC = small cell lung cancer; SEER = Surveillance, Epidemiology, and End Results Program.
Costs associated with cancer are estimated as the difference between cancer cases and matched controls. All estimates in 2019 US dollars.
Out-of-pocket costs estimated from patient responsibility for medical services (including infusion drugs) under Medicare Parts A/B claims. Out-of-pocket costs for oral prescription drugs estimated directly from Medicare Part D claims.
Prostate cancer stage reported as localized or regional during some years of study.
Annualized net patient out-of-pocket costs for medical services for all cancer sites combined were higher in the EOL phase of care than in the initial phase of care within stage at diagnosis: $2868 vs $1694, $3604 vs $3194, and $4526 vs $3540 for cancers diagnosed with localized, regional, or distant disease, respectively (Table 3). Differences in out-of-pocket costs between localized and distant stage at diagnosis in the EOL phase of care were greatest for bladder cancer, colorectal cancer, NSCLC, and melanoma. Out-of-pocket costs in the continuing phase were also generally higher among patients diagnosed with later stage disease (Supplementary Table 5, available online).
Annual Net Patient Out-of-Pocket and Time Costs From MEPS Data
Characteristics of cancer survivors and adults without a cancer history from the MEPS are shown in Table 4. Cancer survivors in both age groups (18-64 years and ≥65 years) were more likely to be older, non-Hispanic White, have at least some college education, and have more MEPS priority conditions than adults without a cancer history. The most common cancer diagnoses among survivors were breast and prostate cancers (data not shown). Most cancer survivors were diagnosed 6 or more years before the survey, with fewer cancer survivors diagnosed within 2 years before the survey.
Table 4.
Characteristics of cancer survivors and adults without a cancer history by age group, MEPS, 2008-2017
| Sociodemographic and health characteristics | Aged 18–64 y |
Aged ≥65 y |
||
|---|---|---|---|---|
| Cancer survivors, No. (weighted %) | No cancer history, No. (weighted %) | Cancer survivors, No. (weighted %) | No cancer history, No. (weighted %) | |
| Total | 8419 (100) | 190 283 (100) | 9066 (100) | 31 569 (100) |
| Age group, y | ||||
| 18-44 | 2194 (23.2) | 116 178 (59.5) | — | — |
| 45-49 | 985 (11.0) | 20 642 (10.6) | — | — |
| 50-54 | 1356 (16.6) | 20 526 (11.3) | — | — |
| 55-59 | 1752 (22.1) | 18 382 (10.1) | — | — |
| 60-64 | 2132 (27.1) | 14 555 (8.5) | — | — |
| 65-69 | — | — | 2295 (23.6) | 11 350 (35.1) |
| 70-74 | — | — | 2052 (23.0) | 7508 (24.1) |
| 75-79 | — | — | 1830 (19.8) | 5405 (17.1) |
| 80+ | — | — | 2889 (33.6) | 7306 (23.7) |
| Sex | ||||
| Male | 2631 (35.5) | 90 551 (49.9) | 4306 (47.6) | 13 299 (43.2) |
| Female | 5788 (64.5) | 99 732 (50.1) | 4760 (52.4) | 18 270 (56.8) |
| Race or ethnicity | ||||
| Non-Hispanic White | 5212 (79.3) | 75 417 (62.0) | 6612 (86.4) | 17 503 (75.2) |
| Non-Hispanic Black | 1277 (7.9) | 37 624 (12.5) | 1285 (6.4) | 5798 (9.4) |
| Hispanic | 1457 (8.6) | 57 600 (17.0) | 763 (4.2) | 5092 (8.7) |
| All other groups | 473 (4.2) | 19 642 (8.4) | 406 (3.0) | 3176 (6.7) |
| Marital status | ||||
| Married or partnered | 4616 (61.0) | 92 160 (51.7) | 4686 (54.7) | 16 170 (55.1) |
| Other | 3803 (39.0) | 98 121 (48.3) | 4380 (45.3) | 15 398 (44.9) |
| Educational attainment | ||||
| Less than high school graduate | 1349 (10.6) | 40 888 (14.4) | 1940 (15.6) | 8984 (20.0) |
| High school graduate | 2507 (27.5) | 57 126 (28.1) | 2949 (33.4) | 9626 (31.6) |
| Some college or more | 4563 (61.9) | 92 269 (57.5) | 4177 (51.0) | 12 959 (48.4) |
| No. of MEPS priority conditionsa | ||||
| 0 | 2165 (26.0) | 103 749 (53.2) | 519 (5.8) | 2831 (9.0) |
| 1 | 2015 (24.9) | 43 376 (23.8) | 1255 (14.3) | 5075 (16.3) |
| 2 | 1671 (20.6) | 22 181 (12.3) | 2002 (22.2) | 7247 (24.0) |
| 3+ | 2568 (28.5) | 20 977 (10.7) | 5290 (57.6) | 16 416 (50.6) |
| Health insurance coverage | ||||
| Age 18-64 y, any private | 5425 (73.7) | 114 871 (71.6) | — | — |
| Age 18-64 y, public only | 2079 (17.7) | 33 571 (12.4) | — | — |
| Age 18-64 y, uninsured | 915 (8.7) | 41 841 (16.0) | — | — |
| Age ≥65 y, Medicare + private | — | — | 4551 (56.2) | 13 830 (52.4) |
| Age ≥65 y, Medicare + public | — | — | 1195 (8.8) | 5688 (11.3) |
| Age ≥65 y, Medicare only | — | — | 3239 (35.0) | 11 381 (36.4) |
| Years since first cancer diagnosis | ||||
| Missing | 415 (4.4) | — | 980 (11.2) | — |
| <2 | 1088 (12.7) | — | 775 (8.4) | — |
| 2-5 | 2340 (27.4) | — | 1811 (19.5) | — |
| 5-10 | 1702 (19.7) | — | 1714 (19.0) | — |
| >10 | 2874 (35.7) | — | 3786 (41.8) | — |
Medical Expenditure Panel Survey (MEPS) priority conditions include arthritis, asthma, diabetes, emphysema, heart disease (angina, coronary heart disease, heart attack, other heart condition or disease), high cholesterol, hypertension, and stroke.
Net Annual Patient Out-of-Pocket Costs. Annual patient out-of-pocket spending for medical services and prescription drugs covered through a pharmacy benefit were higher for cancer survivors than for adults without a cancer history (Table 5). Net annual out-of-pocket costs (95% confidence interval [CI]) associated with cancer were higher among adults aged 18-64 years than adults aged 65 years and older for medical services ($232.7 [$173.2 to $292.3] vs $97.7 [$11.5 to $184.0]) and prescription drugs ($87.4 [$62.0 to $112.8] vs $67.0 [$31.4 to $102.7]), yielding ratios of 2.38 to 1 and 1.30 to 1, respectively. Overall, net annual out-of-pocket costs were higher in the younger ($327.4, 95% CI = $260.0 to $394.9) than in the older group ($173.4, 95% CI = $72.4 to $274.4).
Table 5.
Annual out-of-pocket costs, by cancer history and age group, MEPS, 2008-2017
| Service type | Out-of-pocket cost estimatea (95% CI) |
P b | ||
|---|---|---|---|---|
| Cancer survivors | No cancer history | Net difference | ||
| Aged 18-64 y | ||||
| Medical services | $743.0 ($682.3 to $803.8) | $510.3 ($496.7 to $523.9) | $232.7 ($173.2 to $292.3) | <.001 |
| Prescription medications | $280.8 ($256.6 to $305.0) | $193.4 ($187.2 to $199.7) | $87.4 ($62.0 to $112.8) | <.001 |
| Total out-of-pocket | $1031.0 ($962.6 to $1099.4) | $703.6 ($687.5 to $719.7) | $327.4 ($260.0 to $394.9) | <.001 |
| Aged ≥65 y | ||||
| Medical services | $1041.8 ($964.1 to $1119.4) | $944.0 ($893.5 to $994.5) | $97.7 ($11.5 to $184.0) | .03 |
| Prescription medications | $574.5 ($542.9 to $606.1) | $507.4 ($490.1 to $524.8) | $67.0 ($31.4 to $102.7) | <.001 |
| Total out-of-pocket | $1623.7 ($1534.1 to $1712.5) | $1450.3 ($1393.0 to $1507.0) | $173.4 ($72.4 to $274.4) | <.001 |
All estimates adjusted for age, sex, educational attainment, and number of comorbid conditions; and are reported in 2019 US dollars https://meps.ahrq.gov/about_meps/Price_Index.shtml. CI = confidence interval; MEPS = Medical Expenditure Panel Survey.
Wald’s F, 2-sided.
Net Annual Patient Time Costs. Cancer survivors in both age groups (18-64 years and ≥65 years) were more likely to have overnight hospitalizations, emergency room visits, ambulatory surgeries, provider office-based or hospital outpatient visits, chemotherapy, and radiation therapy than adults without a cancer history (Table 6; Supplementary Table 5, available online). Among adults with these services, cancer survivors in both age groups also had greater service frequency (Table 6; Supplementary Table 6, available online) and spent more time receiving care than their counterparts without a cancer history (Supplementary Table 7, available online). Net annual mean time costs associated with cancer (95% CI) were $304.3 ($257.9 to $350.9) for adults aged 18-64 years, and $279.1 ($215.1 to $343.3) for adults aged 65 years and older. In both age groups, hospitalizations and office visits were the services with the largest contribution to the overall time costs and accounted for the most of the net time costs.
Table 6.
Annual medical service use and patient time costs, by cancer history and age group, MEPS, 2008-2017a,b
| Age group and service type | Cancer survivors |
No cancer history |
Net time costs associated with cancer, estimate (95% CI) | ||||
|---|---|---|---|---|---|---|---|
| % with service | Mean service use (among adults with service) | Time costs | % with service | Mean service use (among adults with service) | Time costs | ||
| Aged 18-64 y | |||||||
| Service-specific estimates | |||||||
| Emergency room visits | 17.4 | 1.6 | $21.2 | 12.5 | 1.4 | $12.7 | $8.5 ($6.6 to $10.3) |
| Ambulatory surgery | 17.9 | 1.8 | $39.8 | 9.6 | 1.6 | $14.9 | $24.9 ($21.6 to $28.3) |
| Inpatient hospitalization | 9.8 | 7.4 | $244.0 | 5.9 | 5.5 | $88.0 | $156.0 ($128.3 to $212.9) |
| Chemotherapyc | 3.2 | 8.6 | $10.8 | 0.0 | 4.1 | $0.0 | $10.8 ($8.1 to $13.5) |
| Radiationc | 1.9 | 15.8 | $6.9 | 0.1 | 8.3 | $0.1 | $6.8 ($4.6 to $9.0) |
| Office visits | 80.6 | 9.6 | $220.5 | 69.3 | 7.2 | $135.1 | $85.4 ($74.1 to $96.8) |
| Total time cost | — | — | $566.6 | — | — | $262.3 | $304.3 ($257.9 to $350.9) |
| Aged ≥65 y | |||||||
| Service-specific estimates | |||||||
| Emergency room visits | 22.1 | 1.5 | $26.1 | 19.0 | 1.5 | $21.6 | $4.5 ($2.7 to $6.3) |
| Ambulatory surgery | 34.5 | 2.3 | $80.6 | 23.5 | 2.0 | $46.8 | $33.8 ($27.4 to $40.1) |
| Inpatient hospitalization | 20.0 | 8.7 | $425.0 | 15.3 | 8.3 | $314.9 | $110.1 ($64.5 to $176.5) |
| Chemotherapyc | 4.1 | 8.9 | $10.5 | 0.1 | 11.1 | $0.1 | $10.4 ($7.7 to $13.1) |
| Radiationc | 2.7 | 17.0 | $5.9 | 0.3 | 12.3 | $0.5 | $5.4 ($3.5 to $7.3) |
| Office visits | 95.2 | 14.9 | $400.5 | 91.1 | 11.4 | $291.5 | $109.0 ($90.7 to $127.4) |
| Total time cost | — | — | $982.6 | — | — | $703.5 | $279.1 ($215.1 to $343.3) |
All estimates adjusted for age, sex, educational attainment, and number of comorbid conditions. CI = confidence interval; MEPS = Medical Expenditure Panel Survey.
All time cost estimates in 2019 US dollars.
Information about use of chemotherapy and radiation therapy was restricted to years 2008-2012 when these data were collected separately in the MEPS.
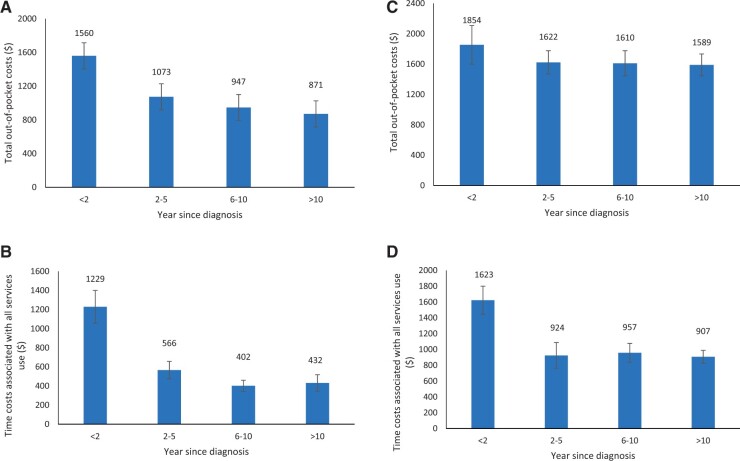
Out-of-pocket and patient time costs among cancer survivors from the MEPS stratified by time since diagnosis (ie, ≤2 years, 2-5 years, 6-10 years, >10 years) are shown in Figure 1. Among cancer survivors in both age groups, out-of-pocket costs and patient time costs were highest among those who were more recently diagnosed and were lowest among those diagnosed 6 years or more before the MEPS survey. In adults aged 18-64 years, mean annual out-of-pocket costs were $1560 among those diagnosed within 2 years; $1074, diagnosed 2-5 years; $947, diagnosed 6-10 years; and $871, diagnosed more than 10 years before the survey (Figure 1, A). Annual patient time costs followed a similar pattern, with highest costs among those diagnosed within 2 years ($1229), followed by 2-5 years ($566), 6-10 years ($402), and more than 10 years ($432) before the survey (Figure 1, B).
Figure 1.
Total annual patient out-of-pocket and time costs among cancer survivors, by age group and time since diagnosis. The figure shows the total annual costs among cancer survivors by age group and by years since cancer diagnosis in years in 4 panels: (A) annual patient out-of-pocket and (B) time costs are shown for survivors aged 18-64 years and (C) annual patient out-of-pocket and (D) time costs for survivors aged 65 years and older, respectively. Data are from the 2008-2017 Medical Expenditure Panel Survey. All estimates were adjusted for age, sex, educational attainment, and the number of comorbid conditions. All cost estimates are in 2019 US dollars. Error bars indicate 95% confidence intervals.
Among the group aged 65 years and older, the highest annual out-of-pocket costs were $1854 among those diagnosed within 2 years and approximately $1600 for all other time since diagnosis categories (Figure 1, C). Annual patient time costs in the older age group were highest ($1623) among those diagnosed within 2 years of the survey and more similar (approximately $930) in all other years (Figure 1, D).
Net National Patient Economic Burden Associated With Cancer Care in 2019
Net national economic burden associated with cancer care for 2019 for all cancers combined and by selected cancer sites are shown in Table 7. One-year and 5-year relative survival by cancer site and age group are shown in Supplementary Table 8 (available online), and the underlying prevalence projections by cancer site, age group, and phase of care are shown in Supplementary Table 9 (available online). Prevalence projections were then combined with net out-of-pocket costs for medical services and prescription drugs by site and phase of care from SEER-Medicare (Table 2), with adjustments for greater net out-of-pocket spending in the population younger than 65 years from the MEPS (2.38 and 1.30 for medical services and prescription drugs, respectively; Table 5) and time cost estimates by age group (Table 6). For example, in the initial phase of care for all cancer sites combined, net annualized out-of-pocket costs were $2200 and $243 for medical services and prescription drugs for patients aged 65 years and older, respectively, and time costs were $279. Corresponding adjustments to the net out-of-pocket cost estimates for greater spending in the younger population yielded $5240 and $316 for medical services and prescription drugs for patients younger than 65 years, respectively, and time cost estimates of $304.
Table 7.
Net patient economic burden associated with cancer in the United States in 2019a
| Site | Patient out-of-pocket costs by phase of care (in millions)b |
Patient time cost (in millions) | Patient economic burden (in millions) | ||||
|---|---|---|---|---|---|---|---|
| Initial | Continuing | End-of-life cancer death | End-of-life other cause of death | Total out-of-pocket costs | |||
| Bladder | $160.3 | $440.9 | $62.4 | $39.1 | $702.6 | $235.4 | $938.0 |
| Breast | $955.4 | $1937.3 | $181.7 | $63.4 | $3137.8 | $1112.2 | $4250.0 |
| Cervix | $63.0 | $82.7 | $17.6 | $8.6 | $172.0 | $82.7 | $254.6 |
| Colorectal | $497.2 | $684.4 | $221.2 | $57.4 | $1460.3 | $440.6 | $1900.9 |
| Hodgkin lymphoma | $77.3 | $153.6 | $9.8 | $6.3 | $247.0 | $70.1 | $317.1 |
| Kidney | $143.9 | $410.3 | $75.7 | $24.2 | $654.1 | $164.3 | $818.3 |
| Leukemia | $145.2 | $469.6 | $118.2 | $25.7 | $758.7 | $131.8 | $890.5 |
| Lung | $401.4 | $416.2 | $490.0 | $45.4 | $1353.0 | $162.8 | $1515.8 |
| Melanoma | $103.2 | $540.1 | $43.1 | $24.2 | $710.6 | $394.1 | $1104.6 |
| Non-Hodgkin lymphoma | $390.2 | $611.5 | $147.7 | $38.1 | $1187.5 | $218.8 | $1406.3 |
| Oral cavity or pharynx | $171.3 | $161.8 | $78.9 | $18.1 | $430.0 | $109.8 | $539.9 |
| Ovary | $101.7 | $195.8 | $74.2 | $6.1 | $377.8 | $72.2 | $450.0 |
| Prostate | $805.2 | $1234.1 | $125.2 | $97.3 | $2261.8 | $1035.5 | $3297.3 |
| Thyroid | $138.3 | $499.7 | $11.8 | $12.6 | $662.4 | $265.5 | $927.8 |
| Corpus uterine | $171.0 | $256.8 | $47.8 | $17.6 | $493.2 | $231.2 | $724.5 |
| All sites combined | $4718.8 | $8878.2 | $2101.5 | $521.4 | $16219.9 | $4873.6 | $21093.6 |
National cancer prevalence estimates by age group, phase of care, and cancer site combined with annualized patient out-of-pocket costs from Surveillance, Epidemiology, and End Results Program-Medicare and annual patient time costs from the Medical Expenditure Panel Survey (MEPS).
Out-of-pocket costs estimated from patient responsibility for medical services (including infusion drugs) under Medicare Parts A/B claims. Out-of-pocket costs for oral prescription drugs estimated directly from Medicare Part D claims. Estimates from the MEPS in Table 5 were used to incorporate higher out-of-pocket spending in younger age group for medical services ($232.7 vs $97.7) and prescription drugs ($87.4 vs $67.0), yielding ratios of 2.38 and 1.30, respectively. All estimates are in 2019 US dollars.
For all cancers combined, patient out-of-pocket costs were projected to be $16.22 billion, with highest costs for breast ($3.14 billion), prostate ($2.26 billion), colorectal ($1.46 billion), and lung ($1.35 billion) cancers, reflecting the higher prevalence of these cancers (Supplementary Table 9, available online). Annual time costs in 2019 were projected to be $4.87 billion for all cancers combined, with breast ($1.11 billion) and prostate ($1.04 billion) cancers accounting for almost one-half of time costs. In 2019, the total patient economic burden associated with cancer care was projected to be $21.1 billion.
Discussion
This study provides comprehensive information about patient economic burden associated with cancer care in the United States, including estimates of out-of-pocket costs and patient time costs as part of the annual report to the nation on the status of cancer. We found that the net patient economic burden of cancer was $21.1 billion nationally for both out-of-pocket and time costs in 2019, which is approximately 12% of previously reported estimates of net national medical care spending associated with cancer [$183 billion in 2015 (4)] and approximately $2700 for patients aged 65 years and older, on average per person, in the first year after diagnosis alone. Average per person out-of-pocket spending and time cost associated with cancer in the first year after diagnosis is even greater for younger patients, approximately $5900. Cancer survivors may experience challenges with these expenses, because nearly 40% of American families report being unable to afford an unexpected expense of $400 (35). We estimated annual patient out-of-pocket costs for most cancers well above this amount, while cancer treatment costs continue to rise (3,7,36). Our findings can provide cost data for discussions about expected costs of treatment as part of informed decision making, as highlighted by the American Society of Clinical Oncology (37), the Institute of Medicine (38), and the President’s Cancer Panel (39) as an element of high-quality care.
We found substantial variation in the pattern and magnitude of net annualized patient out-of-pocket costs by cancer site from the SEER-Medicare data, reflecting differences in treatment intensity and duration and average survival. For example, our study shows that Medicare beneficiaries aged 65 years and older, newly diagnosed with CML, might expect more than $4000 in out-of-pocket costs associated with cancer in the first year following diagnosis and more than $3000 annually in the following years, due largely to ongoing maintenance therapy. Medicare beneficiaries with breast cancer might expect out-of-pocket costs associated with cancer closer to $2400 in the first year after diagnosis and approximately $550 annually afterwards. All cancer survivors would experience net annual time cost burdens of approximately $300.
Consistent with other studies of medical care costs associated with cancer by phase of care (4,6,24), our annualized estimates of out-of-pocket costs from SEER-Medicare are highest in the initial phase of care and at the EOL phase and lowest in the continuing phase, following a “U-shaped” or “J-shaped” curve for medical services and for prescription drugs for most cancer sites. Additionally, out-of-pocket costs within each phase of care were generally highest for patients originally diagnosed with distant disease, followed by regional and localized disease for all solid cancers, reflecting greater treatment intensity for more advanced disease. These estimates we report by phase of care and stage at diagnosis may be useful inputs for studies examining the cost-effectiveness of interventions to increase early detection or to improve other aspects of cancer care.
Patterns of costs by phase of care were consistent across cancer sites except for prescription drugs covered through a pharmacy benefit for CML. Increasing use of maintenance therapies for patients with CML, melanoma, and NSCLC (40,41) suggests that ongoing evaluation of longer-term patient out-of-pocket cost and trajectories may be informative. Additionally, growth in the number of effective oral prescription medications (40) that can be safely administered at home means that patients would likely spend less time traveling to care and receiving infusions. In some instances, however, patient cost-sharing for oral anticancer medications through a pharmacy benefit can be greater than for infusion medications received in a provider’s office and covered as a medical benefits (42). Many states have enacted “oral oncology parity” laws, which are intended to minimize this difference in patient out-of-pocket costs, yet these laws do not apply to Medicare, Medicaid, or self-funded private plans (34). Prior research has shown that greater cost-sharing can adversely affect treatment adherence to oral medications (43,44); ongoing evaluation will be important.
This study is the first, to our knowledge, to report nationally representative estimates from the MEPS for both net annual patient out-of-pocket and time costs associated with cancer—key components of patient economic burden. We found that nationally, time costs represent approximately 23% ($4.9 billion/$21.1 billion) of the patient economic burden, as shown in Table 7. Academic health economists have long recommended that patient time costs be included in cost-effectiveness analyses (19,20), but few studies have included them, in part, because these data are not routinely available. Exclusion of patient time costs from cost-effectiveness analyses can bias results to interventions that place a greater burden on patients and their families (45). Aspects of patient time, including traveling to and from care, may also serve as a barrier to care (46).
There are multiple approaches for valuing patient time. Because time spent seeking medical care represents a lost opportunity for usual activities, including both work and leisure, we chose a single median wage rate, valuing each person’s time equally, as has been done elsewhere (16,17). Other methods that value time differently for different populations may lead to inequities when evaluating the costs associated with health interventions, particularly for populations who are low income, retired, or otherwise economically marginalized (47).
Our approach for creating estimates of patient economic burden builds on and extends standard methods for estimating health-care costs with SEER-Medicare and MEPS data (15–17). Nonetheless, there are some limitations with this study. Some of the data used in this study are older and may not fully reflect more recent patterns of care. Detailed estimates by cancer site and stage at diagnosis from SEER-Medicare were limited to adults aged 65 years and older. Other studies have shown that within cancer site and stage at diagnosis, younger cancer patients tend to receive more intensive treatment than their older counterparts (48–50). Consistent with greater treatment intensity in younger patients, additional information on out-of-pockets costs from the MEPS in our study shows that net out-of-pocket costs associated with cancer are generally higher among adult cancer survivors aged 18-64 years than adults aged 65 years and older. Differences in net out-of-pocket costs associated with cancer by age group also reflect the near universal insurance coverage by the Medicare program among those aged 65 years and older, whereas nearly all uninsured adults are in the 18- to 64-year age group (51).
Informal caregivers frequently accompany cancer patients to medical care appointments and provide care in the home; research is increasingly documenting the burden of cancer diagnoses for family members and other unpaid caregivers (52,53). Neither the SEER-Medicare nor the MEPS data contain comprehensive information about family or caregiver economic burden associated with cancer (54). As a result, our time cost estimates likely understate the annual amount of time spent receiving cancer-related care from the perspective of persons outside the health-care system who provide support to cancer survivors. Further development of longitudinal data resources may inform research quantifying family or caregiver time costs as well as productivity losses due to caregiver time spent away from work.
Detailed data by cancer site and phase of care for adults younger than 65 years are not available from SEER-Medicare, although consistent with our findings from the MEPS reported here, studies conducted in managed care settings suggest that costs of care related to cancer are generally higher among younger patients and survivors than in older populations (55–57). Because of limitations in the availability of comprehensive data for newly diagnosed cancer patients in the younger age group, we could not directly create phase of care–specific estimates for multiple cancer sites for patients and survivors younger than 65 years. Instead, we used estimates from the MEPS data, which are available for both age groups, to reflect higher out-of-pocket spending in cancer patients and survivors younger than 65 years.
Despite this adjustment, our phase of care and national estimates may understate out-of-pocket costs for adults younger than 65 years. Additionally, the detailed cost information in SEER-Medicare fee-for-service claims is not available for patients enrolled in Medicare Advantage (58), private managed care plans that represented approximately 30% of older Medicare beneficiaries during the study period (59). As encounter data for Medicare Advantage enrollees become available through SEER-Medicare, additional research examining any differences in treatment intensity is warranted. Medicare Part A and Part B claims contain information about patient responsibility, but patient out-of-pocket costs, a component of patient responsibility, are not reported separately in claims. We used information from the MEPS to calculate patient out-of-pocket costs as a percentage of patient responsibility and applied this percentage to patient responsibility amounts from SEER-Medicare. Out-of-pocket costs are available directly from Medicare Part D, however. Additionally, out of-pocket cost estimates from SEER-Medicare are for patients with insurance coverage and may not be generalizable to experiences of adults without health insurance coverage or who are underinsured.
Our estimates of out-of-pocket costs from SEER-Medicare are not treatment specific, and the expected costs of treatment may influence informed decision making, such as the choice of oral vs infusion therapies. The MEPS does not collect information about cancer stage at diagnosis, treatment(s), or other clinical characteristics. Exact cancer diagnosis date or date of death for adults who died is unavailable in MEPS, and as a result, we could evaluate total out-of-pocket and time costs only by year since diagnosis and not by phase of care. As a result, our MEPS out-of-pocket cost estimates are not directly comparable with SEER-Medicare out-of-pocket estimates by phase of care, although they can both be combined with cancer prevalence in a specific year to estimate annual costs. There were insufficient numbers of cancer survivors in the MEPS to estimate out-of-pocket and time costs separately for multiple cancer sites; instead, we report summary measures overall, for all cancer survivors. The majority of cancer survivors in the MEPS are reporting use and spending many years following their cancer diagnosis, and estimates may not fully reflect experiences of new diagnosed patients or those at the end of life when treatment intensity and out-of-pocket spending are higher. Thus, our out-of-pocket and patient time cost estimates from the MEPS likely understate these costs.
Despite these limitations, this article provides the most comprehensive estimates of patient economic burden associated with cancer, including out-of-pocket and time costs, in the United States published to date. We found that patient economic burden associated with cancer care is substantial, both nationally and for individual cancer survivors. Findings reported here can inform patient and provider understanding about expected costs of care.
Funding
No specific funding was provided for this research.
Notes
Role of the funder: Not applicable.
Disclosures: Authors declare no conflicts of interest.
Author contributions: All authors (KRY, AM, FT, JZ, FI, HS, RLS, JH, AJ, EMW) contributed to the conceptualization of the study and the writing and review of the manuscript. KRY wrote the original draft and KRY and AM made decisions about methodology with the SEER-Medicare data and KRY and JZ made decisions about methodology with the MEPS data.
Disclaimer: The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the American Cancer Society, Centers for Disease Control and Prevention, the National Cancer Institute, or the North American Association of Central Cancer Registries.
Data Availability
The linked SEER-Medicare data are available through request from the National Cancer Institute. The Medical Expenditure Panel Survey (MEPS) data are publicly available from the Agency for Healthcare Research and Quality website.
Supplementary Material
Contributor Information
K Robin Yabroff, Surveillance and Health Equity Science, American Cancer Society, Kennesaw, GA, USA.
Angela Mariotto, Division of Cancer Control and Population Sciences, National Cancer Institute, Rockville, MD, USA.
Florence Tangka, Division of Cancer Prevention and Control, National Center for Chronic Disease Prevention and Health Promotion, Centers for Disease Control and Prevention, Atlanta, GA, USA.
Jingxuan Zhao, Surveillance and Health Equity Science, American Cancer Society, Kennesaw, GA, USA.
Farhad Islami, Surveillance and Health Equity Science, American Cancer Society, Kennesaw, GA, USA.
Hyuna Sung, Surveillance and Health Equity Science, American Cancer Society, Kennesaw, GA, USA.
Recinda L Sherman, North American Association of Central Cancer Registries, Springfield, IL, USA.
S Jane Henley, Division of Cancer Prevention and Control, National Center for Chronic Disease Prevention and Health Promotion, Centers for Disease Control and Prevention, Atlanta, GA, USA.
Ahmedin Jemal, Surveillance and Health Equity Science, American Cancer Society, Kennesaw, GA, USA.
Elizabeth M Ward, North American Association of Central Cancer Registries, Springfield, IL, USA.
References
- 1. Islami F, Ward EM, Sung H, et al. Annual report to the nation on the status of cancer, Part 1: national cancer statistics [published online ahead of print July 8, 2021]. J Natl Cancer Inst. 2021;113(12):1648–1669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Soni A. Trends in the five most costly conditions among the U.S. civilian noninstitutionalized population, 2002 and 2012. Agency for Healthcare Research and Quality, Rockville, MD. Statistical Brief #470 Web site. Published April 2015. http://www.meps.ahrq.gov/mepsweb/data_files/publications/st470/stat470.shtml. Accessed April 7, 2021. [PubMed]
- 3. Shih YC, Smieliauskas F, Geynisman DM, Kelly RJ, Smith TJ. Trends in the cost and use of targeted cancer therapies for the privately insured nonelderly: 2001 to 2011. J Clin Oncol. 2015;33(19):2190–2196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Mariotto AB, Enewold L, Zhao J, Zeruto CA, Yabroff KR. Medical care costs associated with cancer survivorship in the United States. Cancer Epidemiol Biomarkers Prev. 2020;29(7):1304–1312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Mariotto AB, Yabroff KR, Shao Y, Feuer EJ, Brown ML. Projections of the cost of cancer care in the United States: 2010-2020. J Natl Cancer Inst. 2011;103(2):117–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Yabroff KR, Lamont EB, Mariotto A, et al. Cost of care for elderly cancer patients in the United States. J Natl Cancer Inst. 2008;100(9):630–641. [DOI] [PubMed] [Google Scholar]
- 7. Dusetzina SB, Huskamp HA, Keating NL. Specialty drug pricing and out-of-pocket spending on orally administered anticancer drugs in Medicare Part D, 2010 to 2019. JAMA. 2019;321(20):2025-–2027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Shih YT, Xu Y, Liu L, Smieliauskas F. Rising prices of targeted oral anticancer medications and associated financial burden on Medicare beneficiaries. J Clin Oncol. 2017;35(22):2482–2489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.2019 Employer health benefits survey: section 7: employee cost sharing. Kaiser Family Foundation website. https://www.kff.org/report-section/ehbs-2019-section-7-employee-cost-sharing. Published September 25, 2019. Accessed January 13, 2020.
- 10. Claxton GR, Long M, Damico A, Whitmore H. Kaiser Family Foundation 2018 employer health benefits survey. 2018. https://wwwkfforg/health-costs/report/2018-employer-health-benefits-survey/. Accessed April 7, 2021.
- 11. Rae MC, Cox C. Tracking the rise in premium contributions and cost-sharing for families with large employer coverage. https://wwwhealthsystemtrackerorg/brief/tracking-the-rise-in-premium-contributions-and-cost-sharing-for-families-with-large-employer-coverage/?_hsenc=p2ANqtz--vCGhhfJpJXBuK7q SOv6h0fmd0N6ggVbxRJENc fWGq6ioPAeOm202D0jlQ5kLESxSOi6N0dOkByCmxlAr2r0MHvH3DJw&_hsmi=75726948&utm_campaign=KFF-2019-Health-Costs&utm_source=hs_email&utm_medium=email&utm_content=75726948. Accessed April 7, 2021.
- 12.Health News from National Public Radio. When hospitals sue for unpaid bills, it can be ‘ruinous’ for patients. 2019. https://wwwnprorg/sections/health-shots/2019/06/25/735385283/hospitals-earn-little-from-suing-for-unpaid-bills-for-patients-it-can-be-ruinous. Accessed April 7, 2021.
- 13. Bruhn WE, Rutkow L, Wang P, et al. Prevalence and characteristics of Virginia hospitals suing patients and garnishing wages for unpaid medical bills. JAMA. 2019;322(7):691–692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Zheng Z, Jemal A, Han X, et al. Medical financial hardship among cancer survivors in the United States. Cancer. 2019;125(10):1737–1747. [DOI] [PubMed] [Google Scholar]
- 15. Yabroff KR, Warren JL, Knopf K, Davis WW, Brown ML. Estimating patient time costs associated with colorectal cancer care. Med Care. 2005;43(7):640–648. [DOI] [PubMed] [Google Scholar]
- 16. Yabroff KR, Davis WW, Lamont EB, et al. Patient time costs associated with cancer care. J Natl Cancer Inst. 2007;99(1):14–23. [DOI] [PubMed] [Google Scholar]
- 17. Yabroff KR, Guy GP Jr, Ekwueme DU, et al. Annual patient time costs associated with medical care among cancer survivors in the United States. Med Care. 2014;52(7):594–601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Kessler LG, Ramsey SD. The forest and the trees: the human costs of cancer. J Natl Cancer Inst. 2007;99(1):2–3. [DOI] [PubMed] [Google Scholar]
- 19. Weinstein MC, Siegel JE, Gold MR, Kamlet MS, Russell LB. Recommendations of the panel on cost-effectiveness in health and medicine. JAMA. 1996;276(15):1253–1258. [PubMed] [Google Scholar]
- 20. Sanders GD, Neumann PJ, Basu A, et al. Recommendations for conduct, methodological practices, and reporting of cost-effectiveness analyses: second panel on cost-effectiveness in health and medicine. JAMA. 2016;316(10):1093–1103. [DOI] [PubMed] [Google Scholar]
- 21. Guy GP Jr, Ekwueme DU, Yabroff KR, et al. Economic burden of cancer survivorship among adults in the United States. J Clin Oncol. 2013;31(30):3749–3757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Guy GP Jr, Yabroff KR, Ekwueme DU, Rim SH, Li R, Richardson LC. Economic burden of chronic conditions among survivors of cancer in the United States. J Clin Oncol. 2017;35(18):2053–2061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Yabroff KR, Lund J, Kepka D, Mariotto A. Economic burden of cancer in the United States: estimates, projections, and future research. Cancer Epidemiol Biomarkers Prev. 2011;20(10):2006–2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Mariotto AB, Warren JL, Zeruto C, et al. Cancer-attributable medical costs for colorectal cancer patients by phases of care: what is the effect of a prior cancer history? J Natl Cancer Inst Monogr. 2020;2020(55):22–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.National Cancer Institute. The Surveillance, Epidemiology, and End Results (SEER) Program. https://seercancergov/. Accessed February 28, 2021.
- 26. Enewold L, Parsons H, Zhao L, et al. Updated overview of the SEER-Medicare data: enhanced content and applications. J Natl Cancer Inst Monogr. 2020;2020(55):3–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Centers for Medicare and Medicaid Services. What's Medicare? https://wwwmedicaregov/what-medicare-covers/your-medicare-coverage-choices/whats-medicare. Accessed May 20, 2021.
- 28.Centers for Medicare and Medicaid Services. CMS' program history. https://wwwcmsgov/About-CMS/Agency-Information/History. Accessed May 20, 2021.
- 29.Agency for Healthcare Research and Quality. Medical expenditure panel survey. http://wwwmepsahrqgov/mepsweb/. Accessed February 27, 2021. [PubMed]
- 30.Centers for Medicare and Medicaid Services. Low income subsidy for Medicare prescription drug coverage. https://wwwcmsgov/Medicare/Prescription-Drug-Coverage/LimitedIncomeandResources. Accessed May 20, 2021.
- 31.National Cancer Institute. Patient out-of-pocket payments. https://healthcaredeliverycancergov/seermedicare/considerations/measureshtml#6. Accessed May 20, 2021.
- 32. Tangka FK, Trogdon JG, Richardson LC, Howard D, Sabatino SA, Finkelstein EA. Cancer treatment cost in the United States: has the burden shifted over time? Cancer. 2010;116(14):3477–3484. [DOI] [PubMed] [Google Scholar]
- 33. Zheng Z, Yabroff KR, Guy GP Jr, et al. Annual medical expenditure and productivity loss among colorectal, female breast, and prostate cancer survivors in the United States. J Natl Cancer Inst. 2016;108(5):djv382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Graubard BI, Korn EL. Predictive margins with survey data. Biometrics. 1999;55(2):652–659. [DOI] [PubMed] [Google Scholar]
- 35.The Federal Reserve System. Report on the economic well-being of U.S. households in 2018. https://wwwfederalreservegov/publications/2019-economic-well-being-of-us-households-in-2018-dealing-with-unexpected-expenseshtm. Accessed April 7, 2021.
- 36. Conti RM, Fein AJ, Bhatta SS. National trends in spending on and use of oral oncologics, first quarter 2006 through third quarter 2011. Health Aff (Millwood). 2014;33(10):1721–1727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Meropol NJ, Schrag D, Smith TJ, et al. ; American Society of Clinical Oncology. American Society of Clinical Oncology guidance statement: the cost of cancer care. J Clin Oncol. 2009;27(23):3868–3874. [DOI] [PubMed] [Google Scholar]
- 38.Institute of Medicine. Delivering Affordable Cancer Care in the 21st Century: Workshop Summary. Washington, DC: National Academies Press; 2013. [PubMed] [Google Scholar]
- 39.President's Cancer Panel. Promoting value, affordability, and innovation in cancer drug treatment. https://prescancerpanelcancergov/report/drugvalue/ExecutiveSummaryhtml. Accessed April 7, 2021.
- 40.The IQVIA Institute. Global trends in oncology. 2019. https://wwwiqviacom/insights/the-iqvia-institute/reports/global-oncology-trends-2019. Accessed April 7, 2021.
- 41.American Society of Clinical Oncology. Understanding maintenance therapy. https://wwwcancernet/navigating-cancer-care/how-cancer-treated/understanding-maintenance-therapy. Accessed April 7, 2021.
- 42. Dusetzina SB, Huskamp HA, Jazowski SA, et al. Oral oncology parity laws, medication use, and out-of-pocket spending for patients with blood cancers. J Natl Cancer Inst. 2020;112(10):1055–1062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Winn AN, Keating NL, Dusetzina SB. Factors associated with tyrosine kinase inhibitor initiation and adherence among Medicare beneficiaries with chronic myeloid leukemia. J Clin Oncol. 2016;34(36):4323–4328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Neugut AI, Zhong X, Wright JD, Accordino M, Yang J, Hershman DL. Nonadherence to medications for chronic conditions and nonadherence to adjuvant hormonal therapy in women with breast cancer. JAMA Oncol. 2016;2(10):1326–1332. [DOI] [PubMed] [Google Scholar]
- 45. Russell LB. Completing costs: patients' time. Med Care. 2009;47(7, suppl 1):S89–S93. [DOI] [PubMed] [Google Scholar]
- 46. Ambroggi M, Biasini C, Del Giovane C, Fornari F, Cavanna L. Distance as a barrier to cancer diagnosis and treatment: review of the literature. Oncologist. 2015;20(12):1378–1385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Tranmer JE, Guerriere DN, Ungar WJ, Coyte PC. Valuing patient and caregiver time: a review of the literature. Pharmacoeconomics. 2005;23(5):449–459. [DOI] [PubMed] [Google Scholar]
- 48. Doria-Rose VP, Harlan LC, Stevens J, Little RF. Treatment of de novo acute myeloid leukemia in the United States: a report from the Patterns of Care program. Leuk Lymphoma. 2014;55(11):2549–2555. [DOI] [PubMed] [Google Scholar]
- 49. Murphy CC, Harlan LC, Lund JL, Lynch CF, Geiger AM. Patterns of colorectal cancer care in the United States: 1990-2010. J Natl Cancer Inst. 2015;107(10):djv198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Kaniski F, Enewold L, Thomas A, Malik S, Stevens JL, Harlan LC. Temporal patterns of care and outcomes of non-small cell lung cancer patients in the United States diagnosed in 1996, 2005, and 2010. Lung Cancer. 2017;103:66–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Yabroff KR, Zhao J, Han X, Zheng Z. Prevalence and correlates of medical financial hardship in the USA. J Gen Intern Med. 2019;34(8):1494–1502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Yabroff KR, Kim Y. Time costs associated with informal caregiving for cancer survivors. Cancer. 2009;115(S18):4362–4373. [DOI] [PubMed] [Google Scholar]
- 53. de Moor JS, Dowling EC, Ekwueme DU, et al. Employment implications of informal cancer caregiving. J Cancer Surviv. 2017;11(1):48–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Lund JL, Yabroff KR, Ibuka Y, et al. Inventory of data sources for estimating health care costs in the United States. Med Care. 2009;47(7, suppl 1):S127–S142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Banegas MP, Yabroff KR, O'Keeffe-Rosetti MC, et al. Medical care costs associated with cancer in integrated delivery systems. J Natl Compr Canc Netw. 2018;16(4):402–410. [DOI] [PubMed] [Google Scholar]
- 56. Taplin SH, Barlow W, Urban N, et al. Stage, age, comorbidity, and direct costs of colon, prostate, and breast cancer care. J Natl Cancer Inst. 1995;87(6):417–426. [DOI] [PubMed] [Google Scholar]
- 57. Fireman BH, Quesenberry CP, Somkin CP, et al. Cost of care for cancer in a health maintenance organization. Health Care Financ Rev. 1997;18(4):51–76. [PMC free article] [PubMed] [Google Scholar]
- 58. Fishman PA, Hornbrook MC, Ritzwoller DP, O'Keeffe-Rosetti MC, Lafata JE, Salloum RG. The challenge of conducting comparative effectiveness research in cancer: the impact of a fragmented U.S. health-care system. J Natl Cancer Inst Monogr. 2013;2013(46):99–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Freed MD, Neuman TA. Dozen facts about Medicare advantage in 2020; 2021. https://wwwkfforg/medicare/issue-brief/a-dozen-facts-about-medicare-advantage-in-2020/. Accessed May 20, 2021.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The linked SEER-Medicare data are available through request from the National Cancer Institute. The Medical Expenditure Panel Survey (MEPS) data are publicly available from the Agency for Healthcare Research and Quality website.