Abstract
Background:
There is a growing body of evidence linking residential exposure to transportation noise with several nonauditory health outcomes. However, auditory outcomes, such as tinnitus, are virtually unexplored.
Objectives:
We aimed to investigate the association between residential transportation noise and risk of incident tinnitus.
Methods:
We conducted a nationwide cohort study including all residents in Denmark age , of whom 40,692 were diagnosed with tinnitus. We modeled road traffic and railway noise at the most () and least () exposed façades of all Danish addresses from 1990 until 2017. For all participants, we calculated 1-, 5-, and 10-y time-weighted mean noise exposure and retrieved detailed information on individual- and area-level socioeconomic covariates. We conducted analyses using Cox proportional hazards models.
Results:
We found positive associations between exposure to road traffic noise and risk of tinnitus, with hazard ratios of 1.06 [95% confidence interval (CI): 1.04, 1.08] and 1.02 (95% CI: 1.01, 1.03) per 10-dB increase in 10-y and , respectively. Highest risk estimates were found for women, people without a hearing loss, people with high education and income, and people who had never been in a blue-collar job. The association with road followed a positive, monotonic exposure–response relationship. We found no association between railway noise and tinnitus.
Discussion:
To our knowledge, this is the first study to show that residential exposure to road traffic noise may increase risk of tinnitus, suggesting noise may negatively affect the auditory system. If confirmed, this finding adds to the growing evidence of road traffic noise as a harmful pollutant with a substantial health burden. https://doi.org/10.1289/EHP11248
Introduction
Transportation noise is increasingly recognized as harmful to human health, being a growing source of concern among the general population. In Europe, more than people are exposed to transportation noise above the Environmental Noise Directive threshold of 55 dB.1 Noise is defined as unwanted sound, being often unpleasant and/or disruptive to the listener. Transportation noise exposure is believed to be detrimental to human health through stress reactions with activation of the hypothalamic–pituitary–adrenal axis, followed by increased levels of stress hormones.2,3 In addition, nighttime noise exposure can impact sleep quality and duration, which are crucial for physiological and mental restoration.2,3
In an extensive review of health effects of transportation noise, the World Health Organization (WHO) concluded that there is high-quality evidence for an association between road traffic noise and ischemic heart diseases.4 Since the WHO review, several observational studies have provided evidence suggesting that road traffic noise is also a risk factor for diabetes, stroke, and cardiovascular mortality.5–11 Despite emerging knowledge, the extent of health impacts from transportation noise is still not clear; e.g., the WHO stated in 2018 that there was a lack of studies investigating transportation noise and hearing-related outcomes, such as tinnitus, even though these are considered critical outcomes for the development of guidelines regarding health effects of noise.4
Tinnitus is a very common disorder characterized by the perception of sound in the ears or head in the absence of an external sound source.12 Epidemiological studies worldwide have reported the tinnitus prevalence to range between 5% and 43%.13 However, there is no standard criterion for tinnitus diagnosis, and the heterogeneity of the disease in terms of severity and impact is substantial.13 Although many people can habituate to it, others are severely affected by the disorder even after seeking medical treatment.12,14
Hearing loss and other otological conditions affecting the middle ear are main risk factors for tinnitus. However, although cochlear damage is often the origin of tinnitus, the central nervous system is believed to play an important role in the onset and persistence of the disorder.12,15 Tinnitus is considered a stressor per se, leading to increased physiological arousal and psychological distress.14,16 Nevertheless, several studies also suggest a reverse mechanism, where stressful situations and sleep disturbances precede tinnitus occurrence and contribute to the transition from mild to severe symptoms.14,15,17 As stress and sleep disturbance are proposed key mechanisms behind the harmful effects of noise,2–4 we hypothesize that transportation noise can affect onset and severity of tinnitus. However, to the extent of our knowledge, no longitudinal studies have investigated the effect of residential transportation noise on tinnitus or other auditory outcomes.
This nationwide cohort study aimed to investigate the association between residential road traffic and railway noise exposure, measured both at the least and the most exposed façades, and risk of incident tinnitus. The study was based on individual-level information on hearing-related diagnoses, address history, and socioeconomic factors.
Methods
Study Design and Participants
We performed a nationwide cohort study, including all residents age living in Denmark between 1 January 2000 and 31 December 2017, and born after 1920. All Danish residents were followed across health and administrative registers using the Danish unique personal identification number.18 We identified all Danish addresses in the Building and Housing Register,19 and, by linking them with the Civil Registration System,20 we retrieved address history for all study participants from 10 y before enrollment until censoring.
The study was conducted in accordance with principles of the Declaration of Helsinki and approved by the local authorities (record number: 2018-DCRC-0055). Because the study was entirely based on data from the Danish national registers, it did not require patients’ consent and approval from ethical committees.
Outcome
We followed all cohort members up for an incident diagnosis of tinnitus by linking their personal identification numbers to the Danish National Patient Register (DNPR).21 Tinnitus was defined as a primary (i.e., main cause of the visit) or secondary (i.e., coexisting) diagnosis for outpatient records according to the International Classification of Diseases (ICD) 8 code 781.31 or ICD10 code H93.1. Cohort members with a diagnosis of tinnitus before baseline were excluded.
Noise Exposure Assessment
We calculated road traffic and railway noise at the center of all façades of all residential buildings in Denmark, using precise geocoded data for location and floor (corresponding to the address height) of each address.22 We further selected the lowest and highest noise level for each address, which corresponded to noise at the least and most exposed façade, respectively. Noise levels were calculated as the equivalent continuous A-weighted sound pressure level () for day, evening, and night and represented as . An A-weighted scale aims to mimic human hearing responses by emphasizing the main frequencies perceived by the human ear when sound pressure levels are calculated. All noise values below 35 dB were set to 35 dB, because transportation noise levels below this threshold are likely not perceived, due to other noise sources. Road traffic noise was modeled for the years 1995, 2000, 2005, 2010, and 2015 using the Nordic prediction method.23 Input variables included annual average daily traffic, vehicle distribution, road type, and travel speed.24 Railway noise was modeled for the years 1997 and 2012 for all addresses within of a rail line, using the Nord2000 models.25 Input variables included annual average daily train lengths, travel speed, and train types. Both models considered screening from terrains, noise barriers, berms, and buildings, as well as ground absorption and noise reflections. We used linear interpolation to quantify exposure in intermediary years.
Covariates
We retrieved information on a variety of covariates available on registers at Statistics Denmark, which were selected with basis on the current literature and a review of plausible mechanisms. These included yearly individual-level information on: a) civil status: married/cohabiting/registered partnership; widowed; divorced; single; b) highest attained education: mandatory; secondary, vocational, or other short further education after high school; medium or long-term higher education (Bachelor’s, Master’s, or PhD degree); c) occupational status: blue-collar (employment that requires low-level skills); low-level white-collar (managers with 0–4 employees or with employment that requires intermediate-level skills); high-level white-collar (managers/directors with employees or with employment that requires high-level skills); unemployed; retired; d) disposable income (in quintiles, based on the yearly distribution among Danish adults between 25 and 70 y of age and standardized by calendar year and sex-specific categories); and e) country of origin: Denmark; immigrant or descendent of individuals from other Western country (i.e., European Union country, Andorra, Australia, Canada, Iceland, Liechtenstein, Monaco, New Zealand, Norway, San Marino, Switzerland, United States, and Vatican City State); immigrant or descendent of individuals from a non-Western country (all other countries).
We also collected address-level data on population density and generated neighborhood (parish) socioeconomic status variables by aggregating national data for the 2,160 parishes of Denmark (i.e., the proportion of inhabitants in each parish with low income (lowest quartile), who were unemployed, with manual labor, with only basic education, with a criminal record, and who belonged to single-parent families).26 Given potential beneficial health effects when living close to green areas (e.g., stress reduction and restoration),27,28 we also considered “access to green areas” as a covariate in the present study. For each address, we calculated the proportion of forests, recreational areas, and open nature areas within a and radius buffer (hereinafter referred as high-quality green areas), based on land-use categories extracted from a nationwide land-use and land-cover map for Denmark.29
Last, we retrieved from the DNPR all participants who had been referred to hospital examinations and treatment for hearing loss, other hearing loss–related diseases, and outer and middle ear diseases during and before the study period. Hearing loss diagnosis was defined according to the following ICD10 codes: H80, H810, H833, H838, H839, H90, H91, H93 (excluding H931, H932, H933B), and DH94. Outer and middle ear diseases were defined by the following ICD10 codes: H60, H61, H62, H65, H66, H67, H68, H69, H70, H71, H72, H73, H74, and H75.
Statistical Analyses
Hazard ratios (HR) were estimated using Cox regression models with age as underlying time scale. Participants were enrolled on 1 January 2000 or when they turned 30 y of age, whichever came last, and censored at age of tinnitus diagnosis, death, migration, missing address, or end of follow-up (31 December 2017), whichever came first. We included road traffic and railway noise exposures as time-weighted means calculated for running 1-, 5-, and 10-y periods, taking into consideration the full address history for each study participant.
We calculated linear associations between road traffic and railway noise at the most () and least () exposed façades (per 10 dB) and incident tinnitus, using: a) a basic model, adjusted by age (underlying time scale), sex, and calendar year; and b) a fully adjusted model, including all covariates. All covariates, apart from sex and region of origin, were included in the model as a time-varying variables. Individual-level covariates were updated yearly, whereas area-level covariates were changed every time a person changed address. In a sensitivity analysis, we calculated adjusted HRs considering only primary diagnoses of tinnitus and excluding all persons with a previous diagnosis for outer and middle ear diseases.
Using the fully adjusted model and a total of nine exposure categories, we explored the joint effect of 10-y mean road traffic (, 55–60, and ) and (, 40–50, and ) in relation to tinnitus. The lowest exposure category was used as reference. Additionally, we investigated exposure–response associations between road traffic and railway noise and tinnitus, using 3 dB categories of 10-y mean and . Reference categories were for road traffic and for road traffic , railway , and railway . Reference categories were chosen based on the distribution of the exposure variables and to maintain consistency with previous studies.10,30
We evaluated possible modification of the association between 10-y mean road traffic and and risk of tinnitus by including interaction terms between the exposure variable and different covariates: sex, education, blue-collar occupation, income, high-quality green space in , previous hearing loss diagnosis recorded in the DNPR, and previous diagnosis of cardiovascular comorbidity (stroke, hypertension, and ischemic heart diseases).
The assumption of linearity of road traffic and railway noise in relation to tinnitus was tested by log likelihood ratio tests comparing models with and without a quadratic term. We observed no deviation from linearity ( and 0.58 for road traffic and , respectively). We used Pearson coefficients to inspect correlation between road traffic and railway and .
Analyses were performed in SAS (version 9.4; SAS Institute Inc.). All participants with incomplete address history and/or missing information on covariates were excluded from the analyses.
Results
The study base included Danish residents. Of those, we excluded 12,476 individuals with prevalent tinnitus, 496,241 with incomplete address history, and 71,387 with incomplete information on covariates. The study population consisted of 3,520,926 individuals with a mean follow-up of 14.1 y and 40,692 incident cases of tinnitus.
Baseline sociodemographic characteristics for people exposed to road traffic above and below 55 dB are presented in Table 1 and Table S1. The histograms for road traffic and railway and at baseline are shown in Figure S1 and Figure S2. Road traffic ranged from 35.0 to 90.1 dB, with median, mean, and interquartile ranges (IQR) of 57.6, 56.6, and 10.8 dB, respectively. For road traffic , the values ranged from 35.0 to 81.7 dB, with median of 45.2 dB, mean of 45.5 dB, and IQR of 8.3 dB. Railway among exposed persons ranged from 35.0 to 86.0 dB, with median of 54.5 dB, mean of 54.1 dB, and IQR of 11.8 dB; railway among exposed ranged from 35.0 to 81.5 dB, with median, mean, and IQR of 41.1, 44.8, and 8.5 dB, respectively. Road traffic and railway noise were correlated with each other, with Pearson correlation coefficients between road traffic and road traffic and railway and railway of 0.49, 0.28, and 0.22, respectively (Table S2).
Table 1.
Baseline characteristics of the study population (Denmark, 2000–2017) according to road traffic noise exposure at the most exposed façade.
| Baseline characteristics | Entire population () | road traffic noise () | road traffic noise () |
|---|---|---|---|
| Sex [% (men)] | 49.1 | 49.5 | 48.5 |
| Age () | |||
| Country of origin (%) | |||
| Denmark | 99.0 | 98.9 | 99.2 |
| Other Western country | 0.4 | 0.4 | 0.4 |
| Non-Western country | 0.6 | 0.7 | 0.4 |
| Civil status (%) | |||
| Married or cohabiting | 73.2 | 69.7 | 78.9 |
| Widow(er) | 4.6 | 4.1 | 5.5 |
| Divorced | 5.9 | 6.1 | 5.4 |
| Single | 16.3 | 20.1 | 10.2 |
| Individual income (%)a | |||
| Q1 | 20.3 | 20.8 | 19.4 |
| Q2 | 21.0 | 21.9 | 19.7 |
| Q3 | 21.0 | 21.9 | 19.6 |
| Q4 | 19.8 | 19.5 | 20.3 |
| Q5 | 17.9 | 15.9 | 21.0 |
| Occupational status (%) | |||
| Blue-collar | 40.0 | 40.9 | 38.5 |
| Low-level white-collar | 17.7 | 18.4 | 16.6 |
| High-level white-collar | 12.4 | 12.8 | 11.7 |
| Unemployed | 6.0 | 6.9 | 4.7 |
| Retired | 23.9 | 21.0 | 28.5 |
| Highest attained education (%) | |||
| Mandatory education | 32.8 | 30.9 | 36.0 |
| Secondary or vocational education | 47.4 | 47.7 | 46.8 |
| Medium or long education | 19.8 | 21.4 | 17.3 |
| High-quality green space | |||
| in radius | 19.6 | 18.5 | 21.3 |
| in radius | 24.3 | 22.6 | 26.9 |
| Area-level factors ()b | |||
| % of population with low income (1st quartile) | |||
| % unemployed in population | |||
| % of population in manual labor | |||
| % of population with only basic education | |||
| % population with criminal record | |||
| % single-parent families | |||
Note: Data were complete for all variables. The corresponding number of persons for each category is shown on Table S1. dB, decibel.
Individual income quintiles were standardized by calendar year and sex.
Based on the 2,160 parishes available in Denmark.
Road traffic noise was positively associated with tinnitus for all exposure windows, with substantially higher HRs for in comparison with . With the fully adjusted model, a 10-dB increase in 10-y mean and was associated with a 6% (; 95% CI: 1.04, 1.08) and 2% (; 95% CI: 1.01, 1.03) higher risk of tinnitus, respectively (Table 2). When only primary tinnitus diagnoses were considered, HRs per 10 dB were 1.07 and 1.06 for road and , respectively (Table S3). The HRs were nearly the same when individuals with a previous diagnosis for outer and middle ear diseases were excluded (Table S3). No association was found between railway noise and tinnitus (Table 2; Table S4; Figure S3).
Table 2.
Associations between 1-, 5-, and 10-y averaged residential exposure to road traffic and railway noise (linear, per 10 dB) at the most () and least () exposed façade and risk of incident tinnitus (40,692 cases, including both primary and secondary tinnitus diagnoses). Results were derived from cox proportional hazards models.
| Noise exposure per 10 dB | Basic modela HR (95% CI) | Fully adjusted modelb HR (95% CI) |
|---|---|---|
| Road traffic, | ||
| 1-y exposure | 1.02 (1.01, 1.03) | 1.01 (1.00, 1.02) |
| 5-y exposure | 1.03 (1.01, 1.04) | 1.02 (1.00, 1.03) |
| 10-y exposure | 1.03 (1.02, 1.04) | 1.02 (1.01, 1.03) |
| Road traffic, | ||
| 1-y exposure | 1.05 (1.04, 1.07) | 1.04 (1.03, 1.06) |
| 5-y exposure | 1.06 (1.04, 1.07) | 1.05 (1.03, 1.07) |
| 10-y exposure | 1.06 (1.05, 1.08) | 1.06 (1.04, 1.08) |
| Railway, | ||
| 1-y exposure | 1.03 (1.00, 1.06) | 1.01 (0.98, 1.04) |
| 5-y exposure | 1.03 (1.00, 1.06) | 1.00 (0.98, 1.03) |
| 10-y exposure | 1.02 (0.99, 1.04) | 0.99 (0.97, 1.02) |
| Railway, | ||
| 1-y exposure | 1.08 (1.04, 1.12) | 1.02 (0.98, 1.06) |
| 5-y exposure | 1.06 (1.02, 1.10) | 1.00 (0.96, 1.04) |
| 10-y exposure | 1.05 (1.02, 1.09) | 0.99 (0.96, 1.03) |
Note: CI, confidence interval; dB, decibel; HR, hazard ratio.
Adjusted for age (underlying time scale, sex, and calendar year).
Adjustment for age (underlying time scale), sex, calendar year, civil status, income, country of origin, occupational status, education, proportion of high-quality green areas within 150 and buffers, and a number of area-level socioeconomic variables: percentage of population with low income, with only basic education, who are unemployed, with manual labor, who are single-parent and with a criminal record, as well as mutual road traffic and railway noise adjustment. All covariates, apart from sex and region of origin, were included in the model as time-varying variables.
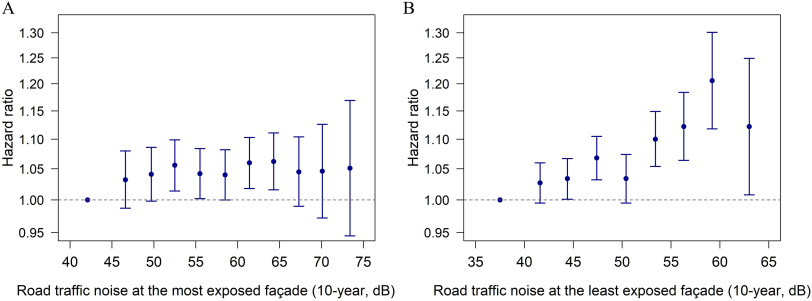
We found that the association between road and tinnitus followed a monotonic exposure–response relationship across the entire exposure range, whereas for an increase in risk was observed only in the low-exposure range, followed by a leveling off in risk at higher exposures (Figure 1; Table S4). Accordingly, when investigating combined exposure to road and , we observed higher HRs as exposure increased, whereas no clear tendencies were found across higher categories (Table 3).
Figure 1.
Associations between 10-y mean exposure to road traffic noise at the most (A) and least (B) exposed façades and risk of tinnitus using the fully adjusted model. The vertical bars show hazard ratios with 95% confidence interval at the median of the exposure categories compared with the reference category. Reference category was for and for . Risk estimates and number of cases for each exposure category are shown in Table S3.
Table 3.
Associations between categories combining residential exposure to road traffic at the most and least exposed façade and risk of incident tinnitus (40,692 cases, including both primary and secondary tinnitus diagnoses). Results were derived from cox proportional hazards models.
| Road traffic noise, | |||
|---|---|---|---|
| Road traffic noise, | 55–60 dB | ||
| Ref | 0.99 (0.94, 1.05) | 0.97 (0.92, 1.03) | |
| 40–50 dB | |||
| 1.03 (1.00, 1.07) | 1.02 (0.98, 1.06) | 1.05 (1.01, 1.09) | |
| 1.04 (0.98, 1.10) | 1.07 (1.03, 1.12) | 1.08 (1.03, 1.12) | |
Note: Results are given in hazard ratio (95% confidence interval) and were based on the fully adjusted model, i.e., adjusted for age (underlying time scale), railway noise, sex, calendar year, civil status, income, country of origin, occupational status, education, proportion of high-quality green areas within 150 and buffers, and a number of area-level socioeconomic variables: percentage of population with low income, with only basic education, who are unemployed, with manual labor, who are single-parent and with a criminal record. All covariates, apart from sex and region of origin, were included in the model as time-varying variables. dB, decibel; Ref, reference.
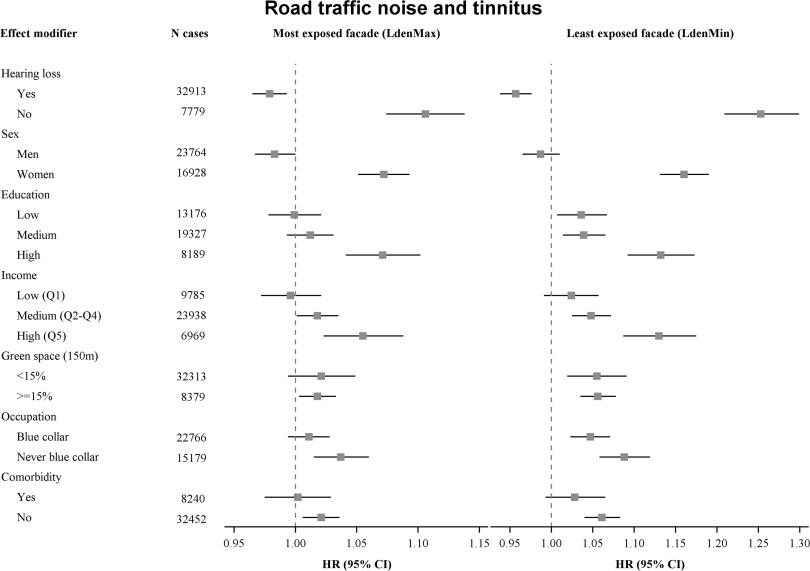
As shown in Figure 2, the positive associations between road traffic noise and tinnitus were present only among persons with no previous diagnosis of hearing loss. In contrast, we found negative associations among people with hearing loss. The association was only observed for women, and we found stronger associations among people with higher vs. lower education and income, among people who had never worked in a blue-collar occupation vs. those who had, and among people without vs. with cardiovascular comorbidity. We found no modification of the noise–tinnitus association in relation to surrounding green space (Figure 2 and Table S5).
Figure 2.
Effect modification analysis of associations between 10-y mean road traffic noise (continuous, per 10 dB, using the fully adjusted model) at the most and least exposed façade and risk of tinnitus by: hearing loss diagnosis, sex, education, income, green space (), occupation, and comorbidity. Risk estimates and number of cases in each modifier subgroup are shown in Table S5.
Discussion
In this large cohort study, we found residential exposure to road traffic noise to be associated with increased risk of tinnitus, especially noise at the least exposed façade (). Highest risk estimates were found for women and for people without a hearing loss, people with high education and income, and people who had never been in a blue-collar job. Associations between road and tinnitus followed a monotonic exposure–response relationship throughout the exposure range. Railway noise was not associated with increased risk of tinnitus.
We are not aware of previous studies investigating associations between residential exposure to transportation noise and tinnitus. Several epidemiological studies, however, have looked at occupational and leisure noise in relation to tinnitus and consistently shown increased risk of tinnitus following repeated noise exposure.31,32 Noise levels of 85 dB over an 8-h period is typically considered the threshold of which noise can damage the auditory system, likely causing permanent hearing loss and tinnitus.31 Residential exposure to road traffic and railway noise is not likely to reach this level for such a long period of time (hours) and therefore not expected to cause permanent changes in the cochlea. However, transportation noise is a known environmental stressor.3 A recent scoping review concluded that stress increases the distress caused by and the loudness of tinnitus,33 and studies have indicated that stress may play a major role in the development, maintenance, and worsening of tinnitus, especially among people who have a strong negative emotional reaction toward the condition.14,33 In support, we found stronger noise–tinnitus associations when considering only primary diagnoses of tinnitus, which likely represent the more severe cases because these patients have been referred for additional treatment or counseling. One of the most discussed mechanistic models posits that high levels of arousal or stress sustain negative thoughts in relation to tinnitus, therefore reducing the ability of the individual to habituate to the symptoms.34 Also, increased levels of stress hormones may affect the limbic, reticular, and auditory systems, possibly causing or worsening the disorder.35 These are therefore potential underlying mechanisms behind the observed noise–tinnitus associations.
Most studies on transportation noise and health are based on noise estimations at the most exposed façade. However, assessing noise at the least exposed façade may be of significant relevance and a proxy for nighttime exposure, because buildings usually have a quiet side where people in noisy conditions would likely place a bedroom.36 In the present study, we observed higher risk estimates when noise was modeled for the least exposed façade in comparison with the most exposed façade, and we found a clear exposure–response relationship for . Having difficulties in initiating and maintaining sleep is one of the most frequent reports by tinnitus patients, often originating as a reaction to the annoyance experienced by tinnitus patients.32 However, studies have also shown sleeping difficulties to precede tinnitus distress, therefore aggravating tinnitus symptoms.37 The bidirectional relationship between tinnitus and sleeping problems may be explained by a common neurobiological mechanism related to hyperarousal of the sympathetic nervous system, which can be reinforced by a vicious cycle, where sleep disturbance would worsen tinnitus symptoms and more severe symptoms would contribute to impaired sleep.38 In agreement, tinnitus has been found to be louder and more distressing during the night and in the early morning.39 It is therefore possible that noise-induced stress arousals in the middle of the night, together with sleep interruptions, may increase tinnitus patients’ awareness of tinnitus and subsequent level of distress when they try to resume sleep. These people may consequently be more prone to seek medical help, enabling us to identify them in the Danish health registers.
Most tinnitus sufferers are also hearing impaired.12,40,41 In our study only 19% of the identified cases were not previously diagnosed with hearing loss. We observed a positive association between road traffic noise and tinnitus only among people without a hearing loss diagnosis. We found higher risk estimates when considering only primary diagnoses of tinnitus, which likely correspond to people without hearing loss, who would approach the ear, nose, throat (ENT) doctor solely due to their tinnitus symptoms when the symptoms become bothersome to them. In contrast, tinnitus for many hearing loss patients will likely be registered as a secondary diagnosis (in the hospital registry) when they attend a hearing clinic for investigation of their original hearing problem. When hearing loss is present, the cause of tinnitus and hearing loss is usually the same, unless stated otherwise.42,43 In addition, König et al. observed a clear relation between tinnitus intensity and the degree of hearing loss.44 We therefore speculate that the severity of tinnitus among individuals with hearing impairment would probably be much more related to their degree of hearing loss and therefore not be as affected by noise-induced stressful events in comparison with the individuals with other causal onsets of tinnitus. Furthermore, individuals with hearing impairment hear sounds with a reduced acuity and may be likely less disturbed by transportation noise.
Another interesting finding of our study was a negative association between road traffic noise and tinnitus among people who were previously diagnosed with hearing loss. A potential explanation is that external low-level noise may mask tinnitus sounds.41,45,46 This masking is possibly the case for individuals with mild to moderate hearing impairment who may still be able to hear the noise but with not such high intensity to cause stress reactions and/or wake them up, especially at night when no hearing aid is used.
We found the association between road traffic noise and tinnitus to be present only among women and to be higher among people with high income and education and among people who have never been in a blue-collar job, generally indicating socioeconomic status as an important effect modifier of tinnitus–noise associations. Women and people of higher socioeconomic position may be more likely to seek a doctor with their medical problems, and they may be more persistent in demanding examination and treatment.47,48 These characteristics would make them more likely to be captured as cases in the hospital register. Furthermore, these are groups that were likely less exposed to occupational noise during their life courses.49,50 These findings may also be explained by a much lower proportion of hearing loss diagnoses in these groups and the fact that we observed associations only among people without a hearing loss diagnosis, therefore drawing the risk estimates toward the null. In agreement, the effect modification analysis showed higher HRs among individuals without cardiovascular comorbidity, which generally consists of younger individuals who also are less likely to have a hearing loss. Additionally, previous research revealed higher degrees of tinnitus distress, tension, and perceived stress among female patients,51 which may also explain higher risk estimates among women in comparison with men.
We did not find railway noise to be associated with tinnitus. Railway noise is usually perceived as less annoying than road traffic noise,4,52 which could explain why this noise source is not sufficient to aggravate tinnitus symptoms. Besides, the Danish railway system consists mostly of passenger trains, which usually do not operate during the night, thus not causing sleep disturbances to the same extent as road traffic sources.
The use of high-quality Danish registers enabled us to identify many tinnitus cases and conduct a nationwide prospective study with a long follow-up time, which is a major strength of the study. Besides a very large study population, we had access to detailed and time-varying individual- and area-level sociodemographic and socioeconomic information, as well as precise address location and history for each study participant. Our analysis relied on validated exposure models to estimate noise from two transportation sources at both the most and least exposed façade, the latter better reflecting nighttime exposure.22,23
Diagnosing tinnitus imposes many challenges, because there is no objective test to confirm the occurrence of the disorder. Moreover, tinnitus intensity and severity are highly heterogeneous, with some people being much more affected by the condition than others.12 Because our study is based on register-based diagnoses, we believe our analyses are rather limited to more severe and bothersome tinnitus cases, because these patients would be more likely to seek medical help for their tinnitus (i.e., primary diagnosis) and/or complain about the condition even if tinnitus was not the primary cause of the visit (i.e., secondary diagnosis). Therefore, we expect our population to have a large number of people with an undiagnosed tinnitus, especially those who are not significantly bothered by the condition and possibly those of lower socioeconomic position. This outcome misclassification is believed to be nondifferential with regard to noise exposure and would thus in most situations drive the risk estimates toward the null.
Our study presents other limitations. The exposure assessment was limited to home addresses and did not consider individual preventive measures regarding, e.g., window quality and bedroom disposition, therefore hindering the estimation of indoor noise exposure, and other noise sources (e.g., from neighbors, community life, and construction sites). We also lacked detailed information on occupational noise exposure, such as type and exposure duration, which is a well-known risk factor for tinnitus and potentially a confounder on the exposure–disease pathway. Even though our models were adjusted for occupational status, we were not able to differentiate the available classes (i.e., blue-collar, low- and high-level white-collar, unemployed, and retired) into different job functions, or to capture the full picture of current and past exposure history. Similarly, although we used detailed socioeconomic information, measured by individual (e.g., disposable income and highest attained education) and address-level covariates, we cannot rule out potential residual confounding. Finally, our findings were limited to the Danish population, which represents specific characteristics related to ethnicity, genetics, and the presence and distribution of various noise sources. Therefore, our findings should be generalized with caution, and more studies are needed to test the consistency of our results in other study settings, including different population characteristics and geographical locations.
To the best extent of our knowledge, this is the first study investigating the association between residential exposure to transportation noise and risk of tinnitus. Our study, which covered an entire country, showed consistent associations between road traffic noise and tinnitus, especially when noise was measured at the least exposed façade. No association was found for railway noise. The hypothesized underlying mechanisms behind the observed associations include noise-induced stress reactions and disturbance of sleep, which would increase people’s awareness of tinnitus, likely exacerbating the condition. Further mechanistic studies, preferably including information on indoor exposure, are needed to confirm the noise–tinnitus pathways hereby proposed. Although causality remains uncertain, these findings suggest that transportation noise may also affect the auditory system. Last, this study adds to the evidence of road traffic noise as a harmful pollutant with a growing health burden.
Supplementary Material
Acknowledgments
This work was supported by the William Demant Foundation (grant number: 18-0964).
References
- 1.European Environment Agency. 2020. Environmental Noise in Europe – 2020. https://www.eea.europa.eu/publications/environmental-noise-in-europe/ [accessed 2 February 2022].
- 2.Babisch W. 2002. The noise/stress concept, risk assessment and research needs. Noise Health 4(16):1–11, PMID: . [PubMed] [Google Scholar]
- 3.Basner M, Babisch W, Davis A, Brink M, Clark C, Janssen S, et al. . 2014. Auditory and non-auditory effects of noise on health. Lancet 383(9925):1325–1332, PMID: , 10.1016/S0140-6736(13)61613-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization. 2018. Environmental Noise Guidelines for the European Region. Copenhagen, Denmark: WHO Regional Office for Europe. https://www.euro.who.int/__data/assets/pdf_file/0008/383921/noise-guidelines-eng.pdf [accessed 2 February 2022]. [Google Scholar]
- 5.Roswall N, Pyko A, Ögren M, Oudin A, Rosengren A, Lager A, et al. . 2021. Long-term exposure to transportation noise and risk of incident stroke: a pooled study of nine Scandinavian cohorts. Environ Health Perspect 129(10):1–10, PMID: , 10.1289/EHP8949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Vienneau D, Eze IC, Probst-Hensch N, Roosli M. 2019. Association between transportation noise and cardio-metabolic diseases: an update of the WHO meta-analysis. In: Proceedings of the 23rd International Congress on Acoustics Integrating 4th EAA Euroregion 2019. 9–13 September 2019. Aachen, Germany. 10.18154/RWTH-CONV-239440. http://publications.rwth-aachen.de/record/769851/files/769851.pdf [accessed 3 February 2022]. [DOI] [Google Scholar]
- 7.Münzel T, Sørensen M, Daiber A. 2021. Transportation noise pollution and cardiovascular disease. Nat Rev Cardiol 18(9):619–636, PMID: , 10.1038/s41569-021-00532-5. [DOI] [PubMed] [Google Scholar]
- 8.Hegewald J, Schubert M, Lochmann M, Seidler A. 2021. The burden of disease due to road traffic noise in Hesse, Germany. Int J Environ Res Public Health 18(17):9337, PMID: , 10.3390/ijerph18179337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hao G, Zuo L, Weng X, Fei Q, Zhang Z, Chen L, et al. . 2022. Associations of road traffic noise with cardiovascular diseases and mortality: longitudinal results from UK Biobank and meta-analysis. Environ Res 212(pt A):113129, PMID: , 10.1016/j.envres.2022.113129. [DOI] [PubMed] [Google Scholar]
- 10.Thacher JD, Poulsen AH, Hvidtfeldt UA, Raaschou-Nielsen O, Brandt J, Geels C, et al. . 2021. Long-term exposure to transportation noise and risk for type 2 diabetes in a nationwide cohort study from Denmark. Environ Health Perspect 129(12):1–11, PMID: , 10.1289/EHP9146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Thacher JD, Hvidtfeldt UA, Poulsen AH, Raaschou-Nielsen O, Ketzel M, Brandt J, et al. . 2020. Long-term residential road traffic noise and mortality in a Danish cohort. Environ Res 187:109633–109638, 10.1016/j.envres.2020.109633. [DOI] [PubMed] [Google Scholar]
- 12.Baguley D, McFerran D, Hall D. 2013. Tinnitus. Lancet 382(9904):1600–1607, PMID: , 10.1016/S0140-6736(13)60142-7. [DOI] [PubMed] [Google Scholar]
- 13.McCormack A, Edmondson-Jones M, Somerset S, Hall D. 2016. A systematic review of the reporting of tinnitus prevalence and severity. Hear Res 337:70–79, PMID: , 10.1016/j.heares.2016.05.009. [DOI] [PubMed] [Google Scholar]
- 14.Betz LT, Mühlberger A, Langguth B, Schecklmann M. 2017. Stress reactivity in chronic tinnitus. Sci Rep 7:41521–41529, PMID: , 10.1038/srep41521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rauschecker JP, Leaver AM, Mühlau M. 2010. Tuning out the noise: limbic-auditory interactions in tinnitus. Neuron 66(6):819–826, PMID: , 10.1016/j.neuron.2010.04.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Heinecke K, Weise C, Schwarz K, Rief W. 2008. Physiological and psychological stress reactivity in chronic tinnitus. J Behav Med 31(3):179–188, PMID: , 10.1007/s10865-007-9145-0. [DOI] [PubMed] [Google Scholar]
- 17.Mazurek B, Boecking B, Brueggemann P. 2019. Association between stress and tinnitus – new aspects. Otol Neurotol 40(4):e467–e473, PMID: , 10.1097/MAO.0000000000002180. [DOI] [PubMed] [Google Scholar]
- 18.Schmidt M, Pedersen L, Sørensen HT. 2014. The Danish Civil Registration System as a tool in epidemiology. Eur J Epidemiol 29(8):541–549, PMID: , 10.1007/s10654-014-9930-3. [DOI] [PubMed] [Google Scholar]
- 19.Christensen G. 2011. The Building and Housing Register. Scand J Public Health 39(suppl 7):106–108, PMID: , 10.1177/1403494811399168. [DOI] [PubMed] [Google Scholar]
- 20.Pedersen CB. 2011. The Danish Civil Registration System. Scand J Public Health 39(suppl 7):22–25, PMID: , 10.1177/1403494810387965. [DOI] [PubMed] [Google Scholar]
- 21.Lynge E, Sandegaard JL, Rebolj M. 2011. The Danish National Patient Register. Scand J Public Health 39(suppl 7):30–33, PMID: , 10.1177/1403494811401482. [DOI] [PubMed] [Google Scholar]
- 22.Thacher JD, Poulsen AH, Raaschou-Nielsen O, Jensen A, Hillig K, Roswall N, et al. . 2020. High-resolution assessment of road traffic noise exposure in Denmark. Environ Res 182:109051–109059, PMID: , 10.1016/j.envres.2019.109051. [DOI] [PubMed] [Google Scholar]
- 23.Bendtsen H. 1999. The Nordic prediction method for road traffic noise. Sci Total Environ 235(1–3):331–338, 10.1016/S0048-9697(99)00216-8. [DOI] [Google Scholar]
- 24.Jensen SS, Plejdrup MS, Hillig K. 2019. GIS-Based National Road and Traffic Database 1960–2020. Aarhus, Denmark: Aarhus University, DCE – Danish Centre for Environment and Energy. https://dce2.au.dk/pub/TR151.pdf [accessed 8 February 2022].
- 25.Plovsing B, Kragh J. 2006. Nord2000. Comprehensive Outdoor Sound Propagation Model. Part 1: Propagation in an Atmosphere without Significant Refraction. Lyngby, Denmark: DELTA Danish Electronics, Light & Acoustics. http://www.magasbakony.hu/Val/Nord2000_homogeneous_atmosphere_Part_1.pdf [accessed 8 February 2022].
- 26.Hvidtfeldt UA, Sørensen M, Geels C, Ketzel M, Khan J, Tjønneland A, et al. . 2019. Long-term residential exposure to PM2.5, PM10, black carbon, NO2, and ozone and mortality in a Danish cohort. Environ Int 123:265–272, PMID: , 10.1016/j.envint.2018.12.010. [DOI] [PubMed] [Google Scholar]
- 27.D’Alessandro D, Buffoli M, Capasso L, Fara GM, Rebecchi A, Capolongo S, et al. . 2015. Green areas and public health: improving wellbeing and physical activity in the urban context. Epidemiol Prev 39(4 suppl 1):8–13, PMID: . [PubMed] [Google Scholar]
- 28.Nieuwenhuijsen MJ, Khreis H, Triguero-Mas M, Gascon M, Dadvand P. 2017. Fifty shades of green: pathway to healthy urban living. Epidemiology 28(1):63–71, PMID: , 10.1097/EDE.0000000000000549. [DOI] [PubMed] [Google Scholar]
- 29.Levin G, Jepsen MR, Blemmer MK. 2012. BASEMAP: Technical Documentation of a Model for Elaboration of a Land-Use and Land-Cover Map for Denmark. Aarhus, Denmark: Aarhus University, DCE – Danish Centre for Environment and Energy. https://www2.dmu.dk/Pub/TR11.pdf [accessed 10 February 2022].
- 30.Sørensen M, Poulsen AH, Hvidtfeldt UA, Münzel T, Thacher JD, Ketzel M, et al. . 2021. Transportation noise and risk of stroke: a nationwide prospective cohort study covering Denmark. Int J Epidemiol 50(4):1147–1156, PMID: , 10.1093/ije/dyab024. [DOI] [PubMed] [Google Scholar]
- 31.Themann CL, Masterson EA. 2019. Occupational noise exposure: a review of its effects, epidemiology, and impact with recommendations for reducing its burden. J Acoust Soc Am 146(5):3879–3905, PMID: , 10.1121/1.5134465. [DOI] [PubMed] [Google Scholar]
- 32.Bhatt JM, Lin HW, Bhattacharyya N. 2016. Tinnitus epidemiology: prevalence, severity, exposures, and treatment in the United States. JAMA Otolaryngol Head Neck Surg 142(10):959–965, PMID: , 10.1001/jamaoto.2016.1700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Elarbed A, Fackrell K, Baguley DM, Hoare DJ. 2021. Tinnitus and stress in adults: a scoping review. Int J Audiol 60(3):171–182, PMID: , 10.1080/14992027.2020.1827306. [DOI] [PubMed] [Google Scholar]
- 34.McKenna L, Handscomb L, Hoare DJ, Hall DA. 2014. A scientific cognitive-behavioral model of tinnitus: novel conceptualizations of tinnitus distress. Front Neurol 5:196–15, PMID: , 10.3389/fneur.2014.00196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Al-Mana D, Ceranic B, Djahanbakhch O, Luxon LM. 2008. Hormones and the auditory system: a review of physiology and pathophysiology. Neuroscience 153(4):881–900, PMID: , 10.1016/j.neuroscience.2008.02.077. [DOI] [PubMed] [Google Scholar]
- 36.Bodin T, Björk J, Ardö J, Albin M. 2015. Annoyance, sleep and concentration problems due to combined traffic noise and the benefit of quiet side. Int J Environ Res Public Health 12(2):1612–1628, PMID: , 10.3390/ijerph120201612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Langenbach M, Olderog M, Michel O, Albus C, Köhle K. 2005. Psychosocial and personality predictors of tinnitus-related distress. Gen Hosp Psychiatry 27(1):73–77, PMID: , 10.1016/j.genhosppsych.2004.08.008. [DOI] [PubMed] [Google Scholar]
- 38.Wallhäusser-Franke E, Schredl M, Delb W. 2013. Tinnitus and insomnia: is hyperarousal the common denominator? Sleep Med Rev 17(1):65–74, PMID: , 10.1016/j.smrv.2012.04.003. [DOI] [PubMed] [Google Scholar]
- 39.Probst T, Pryss RC, Langguth B, Rauschecker JP, Schobel J, Reichert M, et al. . 2017. Does tinnitus depend on time-of-day? An ecological momentary assessment study with the “TrackYourTinnitus” application. Front Aging Neurosci 9:253–259, PMID: , 10.3389/fnagi.2017.00253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sindhusake D, Golding M, Newall P, Rubin G, Jakobsen K, Mitchell P. 2003. Risk Factors for tinnitus in a population of older adults: the blue mountains hearing study. Ear Hear 24(6):501–507, PMID: , 10.1097/01.AUD.0000100204.08771.3D. [DOI] [PubMed] [Google Scholar]
- 41.Eggermont JJ, Roberts LE. 2004. The neuroscience of tinnitus. Trends Neurosci 27(11):676–682, PMID: , 10.1016/j.tins.2004.08.010. [DOI] [PubMed] [Google Scholar]
- 42.Coles RRA. 1995. Classification of causes, mechanisms of patient disturbance, and associated counseling. In: Mechanisms of Tinnitus. Vernon JA, Moller AR, eds. Needham Heights, MA: Allyn & Bacon, 11–19. [Google Scholar]
- 43.Shapiro SB, Noij KS, Naples JG, Samy RN. 2021. Hearing loss and tinnitus. Med Clin North Am 105(5):799–811, PMID: , 10.1016/j.mcna.2021.05.003. [DOI] [PubMed] [Google Scholar]
- 44.König O, Schaette R, Kempter R, Gross M. 2006. Course of hearing loss and occurrence of tinnitus. Hear Res 221(1–2):59–64, PMID: , 10.1016/j.heares.2006.07.007. [DOI] [PubMed] [Google Scholar]
- 45.Vernon JA, Meikle MB. 2003. Tinnitus: clinical measurement. Otolaryngol Clin North Am 36(2):293–305, vi, PMID: , 10.1016/s0030-6665(02)00162-7. [DOI] [PubMed] [Google Scholar]
- 46.Hobson J, Chisholm EJ, el Refaie A. 2012. Sound therapy (masking) in the management of tinnitus in adults. Cochrane Database Syst Rev 11(11):CD006371–22, PMID: , 10.1002/14651858.CD006371.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bertakis KD, Azari R, Helms LJ, Callahan EJ, Robbins JA. 2000. Gender differences in the utilization of health care services. J Fam Pract 49(2):147–152, PMID: . [PubMed] [Google Scholar]
- 48.Wiltshire JC, Roberts V, Brown R, Sarto GE. 2009. The effects of socioeconomic status on participation in care among middle-aged and older adults. J Aging Health 21(2):314–335, PMID: , 10.1177/0898264308329000. [DOI] [PubMed] [Google Scholar]
- 49.Michaud DS, Marro L, McNamee JP. 2021. Self-reported occupational noise exposure and cardiovascular disease in Canada: results from the Canadian Health Measures Survey. J Acoust Soc Am 150(2):990–1000, PMID: , 10.1121/10.0005588. [DOI] [PubMed] [Google Scholar]
- 50.Suadicani P, Hein HO, Gyntelberg F. 2012. Occupational noise exposure, social class, and risk of ischemic heart disease and all-cause mortality – a 16-year follow-up in the Copenhagen Male Study. Scand J Work Environ Health 38(1):19–26, PMID: , 10.5271/sjweh.3200. [DOI] [PubMed] [Google Scholar]
- 51.Niemann U, Boecking B, Brueggemann P, Mazurek B, Spiliopoulou M. 2020. Gender-specific differences in patients with chronic tinnitus—baseline characteristics and treatment effects. Front Neurosci 14:1–11, PMID: , 10.3389/fnins.2020.00487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Miedema HME, Vos H. 1998. Exposure-response relationships for transportation noise. J Acoust Soc Am 104(6):3432–3445, PMID: , 10.1121/1.423927. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.