Abstract
Acute testicular pain with no arterial flow on Doppler ultrasonography is highly consistent with testicular torsion. In adults, there are rare etiologies of testicular infarction other than torsion, including infection, vasculitis, and trauma. We describe a 41-year-old man with type 2 diabetes complicated by severe vasculopathy and positive SARS-CoV-2 status presenting with acute right testicular pain. Surgical exploration and pathology were concerning for arteriosclerosis and vasculitis. These observations suggest that medically complex patients presenting with acute testicular pain in the setting of COVID-19 infection could be at risk for ischemia; causes of testicular pain beyond torsion should be considered.
Keywords: Testicular infarction, Diabetes, SARS-CoV-2, COVID-19, Vasculopathy
1. Introduction
Acute testicular pain may result from ischemia, inflammatory or infectious conditions, or trauma. Testicular torsion is a twisting of the spermatic cord and its contents leading to venous obstruction and subsequent compromise of the arterial blood supply to the testis. It is a surgical emergency prompting operative exploration to salvage the affected testis, and is the most common identifiable cause of testicular infarction. Other rarer causes include epididymo-orchitis, vasculitis, or trauma.
This case report considers an adult male patient with a history of complicated type 2 diabetes and newly positive SARS-CoV-2 status who presented with acute right testicular pain and was found to have testicular infarction with no evidence of torsion. We discuss multiple potential contributors to his unique presentation and discuss the body of relevant literature that remains limited at this time.
2. Case presentation
The patient is a 41-year-old man with a history of hypertension, type 2 diabetes complicated by end-stage renal disease on hemodialysis and peripheral arterial disease, and chronic left knee septic arthritis presenting to the emergency department (ED) with acute right testicular pain for 10 hours. His pain was diffuse, sharp, non-radiating, and progressive. He reported no history of trauma and denied fevers, chills, flank pain, abdominal pain, shortness of breath, chest pain, or cough. He was a lifetime non-smoker and sexually inactive.
In the ED, his vital signs were normal. Laboratory tests were notable for a serum white blood cell count (WBC) of 12.1 × 103/μL, glucose of 84 mg/dL, and a positive SARS-CoV-2 PCR test. He denied having COVID-19 before and was fully vaccinated. His most recent hemoglobin A1c was 4.9%. Physical exam revealed an uncircumcised phallus, mild right scrotal swelling, bilateral descended testes, and right testicular tenderness without a cremasteric reflex. Scrotal Doppler ultrasound (US) revealed a 4 × 2.5 × 3.4 cm right testis with no mass and no detectable arterial blood flow. Serpentine calcifications were noted bilaterally within the testes, interpreted as calcifications of intratesticular vessels. The contralateral left testis had normal arterial flow.
With concern for testicular torsion, the patient was taken emergently to the operating room for scrotal exploration. The right testis appeared diffusely edematous and ischemic, but the spermatic cord was not torsed. The seminiferous tubules were necrotic upon opening the tunica. The testicular artery felt significantly calcified, and no Doppler pulses were found in the spermatic cord or testis. Right orchiectomy was performed. The contralateral left testis was healthy and pexed using three-point fixation. The patient was discharged home.
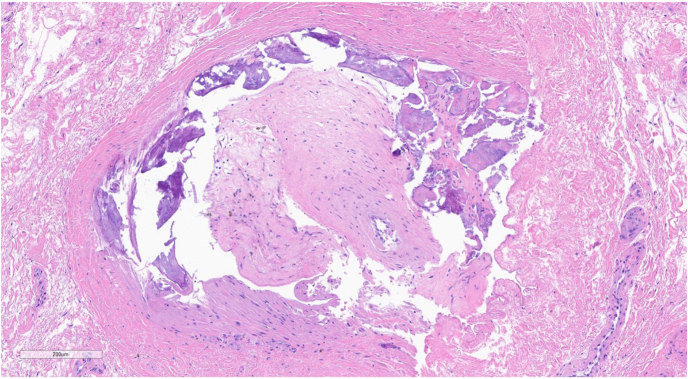
Subsequent pathology revealed acute and chronic ischemic changes including marked tubular fibrosis, interstitial fibrosis, new and old hemorrhage, and hypospermatogenesis (Fig. 1). Vessels within the spermatic cord showed intimal calcification and stenosis with central recanalization (Fig. 2).
Fig. 1.
Testis demonstrating peritubular and interstitial fibrosis, maturation arrest at primary spermatocyte, and old hemorrhage.
Fig. 2.
Spermatic cord artery demonstrating intimal fibrosis and calcification with partial recanalization of lumen.
On postoperative day (POD) 5, the patient was admitted for recurrent septic arthritis. His urologic exam on POD 8 was unremarkable, revealing a well-healing midline scrotal incision. On POD 12, the patient complained of worsening left testicular pain; exam revealed testicular tenderness and a positive cremasteric reflex. Serum WBC was 26.7 × 103/μL. Scrotal Doppler US indicated normal flow and vascularity of the left testis. He was started on levofloxacin for presumed left epididymo-orchitis, and he was discharged on POD 21 with resolved symptoms.
3. Discussion
Acute unilateral testicular pain and absent cremasteric reflex is clinically diagnostic of torsion until proven otherwise and requires emergent surgical exploration. Though surgical intervention should not be delayed for imaging, Doppler US will show decreased or no flow to the affected testis. Our patient met these criteria and was surgically explored, and found to have a globally infarcted right testis but no torsion of the spermatic cord. While the differential diagnosis includes intermittent torsion, his medically complex history and pathological findings strongly suggest other etiologies of testicular infarction.
This patient has insulin-dependent diabetes complicated by severe vasculopathy. His history of peripheral arterial disease, sonographic and intraoperative evidence of arterial calcification, and histologic findings of intimal calcification and stenosis of cord vessels are consistent with diabetes-associated microangiopathy and advanced atherosclerosis.1 Underlying pathology from diabetes may increase the risk for testicular vascular compromise. At least one prior case report of segmental testicular infarction in a 55-year-old man has been reported as a result of diabetic microangiopathy.1 While that patient underwent a partial orchiectomy for focal infarction, his pathology also revealed necrotic seminiferous tubules and interstitial fibrosis.
Novel SARS-CoV-2 infection can impact multiple organ systems, causing direct vascular injury as well as arterial and venous thromboses of the kidneys, spleen, liver, gastrointestinal, and male reproductive systems.2,3 While the exact pathophysiological mechanism remains under investigation, researchers have posited immune dysregulation, systemic endothelial infection, and clotting pathway activation as possible causes of COVID-19 vasculitides or vasculitis-like disease.2 Although our patient did not manifest symptomatic COVID-19, his positive test raises suspicion of whether he was more prone to vascular compromise at the time of presentation.
A 26-year-old man presenting with acute unilateral testicular pain 2 days following recovery from mildly symptomatic SARS-CoV-2 infection has been reported.3 Although his first scrotal US showed mild hypoperfusion of the testis, a repeat US 3 days later showed no flow, and pathology from his orchiectomy specimen revealed massive infarction with segmental obliterative endotheliitis of cord vessels including the spermatic artery and notably, positive SARS-CoV-2 spike protein in endothelial cells. Others have investigated the role of the angiotensin-converting enzyme 2 (ACE2) receptor—normally found in pulmonary epithelium but also in other organs including the testes—in mediating SARS-CoV-2 cellular entry, and proposed viral binding to testicular ACE2 leading to tissue inflammation and vasculitis.4,5
Finally, our patient had his postoperative course complicated by epididymo-orchitis of his remaining left testis, which can lead to segmental testicular infarction in severe cases. Given his propensity for developing infections and underlying diabetic vasculopathy, he requires close follow-up of his remaining testis.
4. Conclusion
While testicular torsion is the most common identifiable cause of testicular infarction, other potential causes should be considered in medically complex patients, including infection, inflammation, and vasculopathy. Elucidating uncommon etiologies can have implications for postoperative management and patient counseling.
Funding statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of competing interest
The authors have no conflicts of interest or disclosures to declare.
Contributor Information
Tenny R. Zhang, Email: trz9004@nyp.org.
Samantha L. Thorogood, Email: slt7002@nyp.org.
Jeremy Miyauchi, Email: jem9349@med.cornell.edu.
Joseph Del Pizzo, Email: jod2009@med.cornell.edu.
Peter N. Schlegel, Email: pnschleg@med.cornell.edu.
References
- 1.El Atat R., Derouiche A., Kourda N., et al. Segmental infarction of the testis: an exceptional complication of diabetes microangiopathy. Int J Impot Res. 2007;19(6):615–616. doi: 10.1038/sj.ijir.3901608. [DOI] [PubMed] [Google Scholar]
- 2.McGonagle D., Bridgewood C., Ramanan A.V., et al. COVID-19 vasculitis and novel vasculitis mimics. Lancet Rheumatol. 2021;3(3):224–233. doi: 10.1016/S2665-9913(20)30420-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Parron D., Gartzia A., Iturregui A.M., et al. SARS-CoV-2-associated obliterative arteritis causing massive testicular infarction. Clin Pract. 2021;11(2):246–249. doi: 10.3390/clinpract11020037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.La Marca A., Busani S., Donno V., et al. Testicular pain as an unusual presentation of COVID-19: a brief review of SARS-CoV-2 and the testis. Reprod Biomed Online. 2020;41(5):903–906. doi: 10.1016/j.rbmo.2020.07.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Li M.Y., Li L., Zhang Y., et al. Expression of the SARS-CoV-2 cell receptor gene ACE2 in a wide variety of human tissues. Infect Dis Poverty. 2020;9(1):45. doi: 10.1186/s40249-020-00662-x. [DOI] [PMC free article] [PubMed] [Google Scholar]