Abstract
Objectives
By better understanding the long-term effects of COVID-19 and assessing rehabilitation placement among the patients in our study, we hope to determine the predictors of rehabilitation needs in individuals suffering from the long-term sequelae of COVID-19.
Methods
A retrospective chart review was performed of adult patients with a positive COVID-19 polymerase chain reaction test among multiple hospitals in a regional health system. The main outcomes measured were discharge disposition, total length of hospital stay, and overall all-cause mortality and readmission rates within 30 and 90 days of discharge.
Results
Of the 2502 patients included in the study, we found that 65.2% were discharged to home, while the remaining patients were discharged to home healthcare (33.6%), skilled nursing facilities (31.7%), or long-term acute rehabilitation centers (11.6%). The overall all-cause mortality rate at 30 and 90 days were 2.7% and 4.4%, respectively. The overall all-cause 30-day and 90-day readmission rates were 7.0% and 7.6%, respectively.
Conclusion
Younger age and shorter hospitalization stays were the most important predictors of home discharge. Discharge to home was also significantly associated with lower all-cause mortality rates at 30 and 90 days after discharge.
Keywords: COVID-19, Rehabilitation, Discharge disposition, Mortality, Age, Length of stay
Introduction
As of July 2022, SARS-CoV-2, the virus responsible for the COVID-19 pandemic, has infected over 560 million people and caused over 6.3 million deaths worldwide [1]. In the United States, the pandemic resulted in over 88 million cases and close to 1 million deaths [1]. Since the start of the pandemic, substantial resources have been poured into understanding the risk factors for mortality in high-risk patients infected by COVID-19. Individual reports from various hospitals worldwide have indicated that many COVID-19 survivors have required rehabilitation to manage long-term symptoms from their infections. One hospital in Paris indicated that up to 51% of their patients hospitalized with COVID-19 experienced long-term sequelae from their infection, including persistent shortness of breath, fatigue, cognitive issues, joint pain, and an overall decline in quality-of-life weeks to months after their initial infection [2], [3], [4]. In 2021, the Centers for Disease Control and Prevention (CDC) released guidelines on how to identify and manage long COVID, indicating its prevalence among COVID-19 survivors and the imminent need to address these long-term symptoms [5].
As the long-term sequelae of COVID-19 are becoming better characterized, it is imperative that we turn our attention to rehabilitation after infection resolution to provide these patients with the best likelihood of a complete recovery. This study aims to track the after discharge rehabilitation needs of patients hospitalized with COVID-19 in our hospital system to assess the disability burden of long COVID symptoms. We will specifically compare rehabilitation needs and placement of our patients hospitalized with COVID-19 and assess risk factors such as age, ethnicity, length of hospitalization, and intensive care unit placement. By better understanding the disability burden of long COVID and tracking rehabilitation placement among the patients in our hospital system, we hope to eventually determine the predictors of rehabilitation needs in individuals suffering from the long-term sequelae of COVID-19.
Statistical analysis
Descriptive statistics for demographic and clinical variables are presented for the overall patient cohort and stratified by whether the patient was discharged home. Depending on data distribution, continuous variables are presented as mean and SD or median and interquartile range and compared using independent-sample t-test or Mann–Whitney test, respectively. Categorical variables are presented as percentages and compared via the chi-square test.
Unadjusted and adjusted logistic regression models were estimated to identify factors associated with being discharged home. Variables in the adjusted model included age, length of stay, biological sex, race/ethnicity, body mass index, smoking status, need for invasive mechanical ventilation, dialysis requirement, and intensive care unit admission. The Kaplan–Meier method and Cox proportional-hazards models were estimated to evaluate differences in time to after discharge death and readmission, for which patients were censored at 30 or 90 days after discharge. For readmission analyses, death served as a competing risk; reported hazard ratios are cause-specific. The proportionality of hazards assumption was assessed for categorical variables using log-negative-log survival curves and using scaled Schoenfeld residuals for continuous variables. For all outcomes, the functional form of continuous variables was evaluated using restricted cubic splines with knot points at the 5th, 35th, 65th, and 95th percentiles; non-linear effects were retained based on model comparison via the likelihood ratio test. All analyses were conducted using SAS v. 9.4 with two-sided P-value <0.05 used to indicate statistical significance.
Results
A total of 2719 patients met inclusion criteria, of whom 217 (8.0%) died during their hospital stay and were therefore excluded from subsequent analysis. Of the 2502 patients discharged alive, 1632 (65.2%) were discharged home. Discharge locations of the 870 patients not discharged to home are provided in Table 1 , with approximately three-fourths of these patients being discharged to home with healthcare provided (33.6%), a skilled nursing facility (SNF, 31.7%), or a long-term care facility (11.6%).
Table 1.
Discharge disposition.
| Overall (N = 2719) | Discharge Location |
||
|---|---|---|---|
| Not Home (n = 870) | Home (n = 1632) | ||
| Died in hospital | 217 (8.0) | - | - |
| Home or self care | 1,632 (60.0) | - | 100 |
| Home-health care | 292 (10.7) | 33.6 | - |
| Skilled nursing facility | 276 (10.2) | 31.7 | - |
| Long-term care | 101 (3.7) | 11.6 | - |
| Rehab facility | 73 (2.7) | 8.4 | - |
| Acute care hospital | 52 (1.9) | 6.0 | - |
| Swing bed | 28 (1.0) | 3.2 | - |
| Hospice/facility | 17 (0.6) | 2.0 | - |
| Hospice/home | 14 (0.5) | 1.6 | - |
| Left against medical Advice | 6 (0.2) | 0.7 | - |
| Custodial Care Facility | 5 (0.2) | 0.6 | - |
| Nursing Facility | 4 (0.2) | 0.5 | - |
| Psychiatric Hospital | 2 (0.1) | 0.2 | - |
Note. Data are presented as count (percent) or percent.
Demographic and clinical characteristics are presented in Table 2 . Unadjusted and adjusted odds of being discharged to home are presented in Table 3 . After adjustment, lower odds of being discharged home were observed in older patients, those with longer lengths of hospital stay, females, patients of non-Hispanic ethnicity, and patients requiring invasive mechanical ventilation.
Table 2.
Demographic and clinical characteristics.
| Overall (N = 2502) |
Not Home (n = 870) | Home (n = 1632) | P | ||
|---|---|---|---|---|---|
| Missing | Statistic | Statistic | Statistic | ||
| Age | 0 | 64.7 ± 16.5 | 74.0 ± 13.4 | 56.8 ± 15.8 | <.001 |
| Biological sex | |||||
| Female | 0 | 46.8 | 51.5 | 44.4 | <.001 |
| Male | 53.2 | 48.5 | 55.6 | ||
| Race | |||||
| White | 186 | 85.1 | 87.6 | 83.8 | <.001 |
| African American | 9.3 | 9.8 | 9.1 | ||
| Asian | 2.4 | 1.2 | 3.0 | ||
| Other | 3.2 | 1.4 | 4.2 | ||
| Hispanic or Latino | |||||
| No | 92 | 86.5 | 93.8 | 82.7 | <.001 |
| Yes | 13.5 | 6.2 | 17.3 | ||
| Body mass index | 27 | 32.3 ± 8.8 | 31.0 ± 8.9 | 32.9 ± 8.6 | <.001 |
| Not obese | 46.8 | 54.6 | 42.6 | <.001 | |
| Obese | 53.2 | 45.4 | 57.4 | ||
| Smoking status | |||||
| Never | 0 | 66.1 | 60.8 | 68.9 | <.001 |
| Current/former | 33.9 | 39.2 | 31.1 | ||
| English speaking | |||||
| No | 2 | 11.1 | 6.2 | 13.7 | <.001 |
| Yes | 88.9 | 93.8 | 86.3 | ||
| Insurance status | |||||
| Uninsured | 8 | 3.3 | 1.0 | 4.5 | <.001 |
| Insured | 96.7 | 99.0 | 95.5 | ||
| Academic medical center | |||||
| No | 0 | 76.9 | 78.1 | 76.2 | 0.304 |
| Yes | 23.1 | 21.9 | 23.8 | ||
| Intensive care unit | |||||
| No | 0 | 80.4 | 78.6 | 81.3 | 0.107 |
| Yes | 19.6 | 21.4 | 18.7 | ||
| Length of stay | 0 | 6 [3-9] | 9 [5-18] | 5 [3-7] | <.001 |
| Hospital length of stay | 0 | 5 [3-9] | 9 [5-18] | 5 [3-7] | <.001 |
| Supplemental oxygen | 0 | 35.7 | 33.5 | 36.8 | 0.093 |
| Dialysis | 0 | 2.0 | 2.8 | 1.5 | 0.035 |
| Mechanical ventilation | |||||
| Non-invasive | 0 | 11.2 | 19.8 | 6.6 | <.001 |
| Invasive | 5.6 | 11.3 | 2.5 | <.001 | |
Note. Data are presented as count, mean ± SD, or percent.
Table 3.
Unadjusted and adjusted odds ratio for being discharged to home.
| Unadjusted |
Adjusted |
||||
|---|---|---|---|---|---|
| OR (95% CI) | P | aOR (95% CI) | F-value | P | |
| Age (per 10 years older) | 0.51 (0.47-0.54) | <.001 | 0.47 (0.42-0.51) | 232.6 | <.001 |
| Hospital length of stay | 0.87 (0.85-0.88) | <.001 | 0.87 (0.85-0.89) | 178.8 | <.001 |
| Female vs Male | 0.75 (0.64-0.89) | <.001 | 0.65 (0.52-0.81) | 14.5 | <.001 |
| Hispanic vs Not Hispanic | 3.15 (2.31-4.29) | <.001 | 2.52 (1.50-4.25) | 12.1 | <.001 |
| Invasive Mechanical Ventilation | 0.20 (0.14-0.30) | <.001 | 0.36 (0.19-0.66) | 10.9 | 0.001 |
| Race | |||||
| White | 0.31 (0.16-0.59) | <.001 | 0.69 (0.30-1.59) | 3.0 | 0.386 |
| Black | 0.30 (0.15-0.60) | <.001 | 0.46 (0.18-1.12) | 0.088 | |
| Asian | 0.79 (0.31-2.01) | 0.614 | 1.56 (0.46-5.30) | 0.472 | |
| Other | Reference | Reference | |||
| New Dialysis | 0.55 (0.31-0.97) | 0.038 | 0.55 (0.26-1.14) | 2.6 | 0.106 |
| Body mass index | 1.03 (1.02-1.04) | <.001 | 0.99 (0.98-1.01) | 2.2 | 0.135 |
| Current/former smoker | 0.70 (0.59-0.83) | <.001 | 0.87 (0.70-1.09) | 1.5 | 0.226 |
| ICU vs No ICU | 0.85 (0.69-1.04) | 0.107 | 0.93 (0.70-1.23) | 0.3 | 0.609 |
aOR, adjusted OR; CI, confidence interval; ICU, intensive care unit; OR, odds ratio.
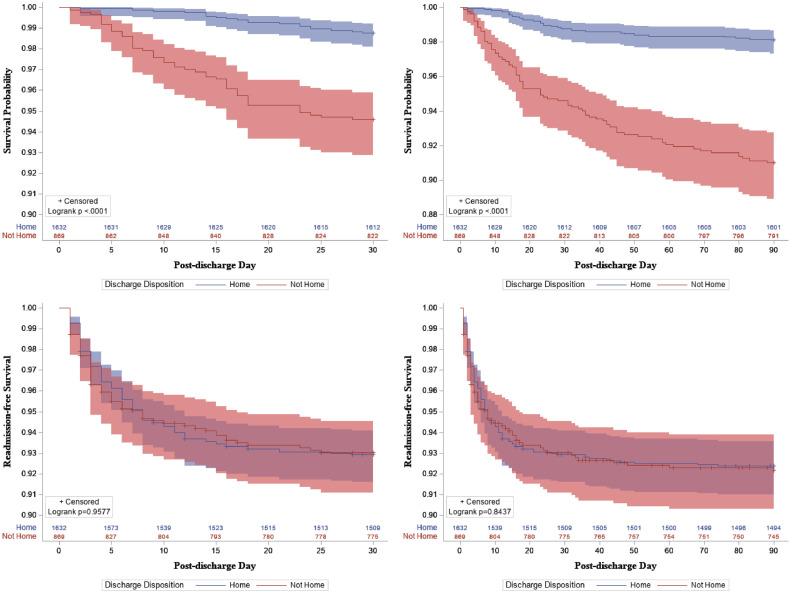
The overall all-cause mortality rate within 30 days of discharge was 2.7% (95% confidence interval [CI]: 2.2% to 3.4%) with a 90-day all-cause mortality rate of 4.4% (95% CI: 3.7% to 5.3%). Both the 30-day and 90-day mortality rates were statistically lower in patients discharged to home (30-day: 1.2% vs 5.5%, P <.001; 90-day: 1.9% vs 9.1%, P <.001). When considering time-to-death, patients discharged to home died later during the follow-up period (Fig. 1 ; both log-rank P <0.001) and had 61.9% and 60.2% lower risk of death during the 30-day and 90-day follow-up periods, respectively (Table 4 ).
Figure 1.
Kaplan–Meier curves for all-cause mortality (top row) and all-cause readmission (bottom row) for 30 days after discharge (left column) and 90 days after discharge (right column). Shaded areas represent 95% confidence intervals.
Table 4.
Risk of death during the 30-day and 90-day follow-up period.
| Unadjusted |
Adjusted |
|||
|---|---|---|---|---|
| HR (95% CI) | p | aHR (95% CI) | p | |
| All-cause Mortality | ||||
| 30-day | 0.22 (0.13-0.37) | <0.001 | 0.38 (0.20-0.72) | 0.003 |
| 90-day | 0.20 (0.13-0.31) | <0.001 | 0.40 (0.24-0.65) | <0.001 |
| All-cause Readmission | ||||
| 30-day | 1.01 (0.74-1.38) | 0.959 | 1.11 (0.76-1.63) | 0.596 |
| 90-day | 0.97 (0.72-1.31) | 0.843 | 1.20 (0.84-1.74) | 0.322 |
Note. HR below 1 indicate a lower risk of the outcome in patients discharged to home relative to patients not discharged to home. aHR were adjusted for age, biological sex, race, ethnicity, tobacco use, body mass index, whether the patient was in the intensive care unit, hospital length of stay, need for invasive mechanical ventilation, and new dialysis.
aHR, adjusted HR; CI, confidence interval; HR, hazard ratios.
Finally, the overall all-cause 30-day readmission rate was 7.0% (95% CI: 6.1% to 8.1%) and the all-cause 90-day readmission rate was 7.6% (95% CI: 6.7% to 8.7%). The 30-day and 90-day readmission rates were statistically similar between patients discharged to home or not (30-day: 7.1% vs 6.9%, P =.889; 90-day: 7.6% vs 7.7%, P =.926). Likewise, both time-to-readmission (Fig. 1) and risk of readmission (Table 4) were statistically similar for patients discharged to home or not during the 30-day and 90-day follow-up periods.
Discussion
Our data demonstrated that 65.2% of hospitalized patients with COVID-19 are discharged to home, with younger age and shorter hospital length of stay being the most important predictors of home discharge. The remaining 40% were primarily discharged to home healthcare, SNFs, or long-term acute care rehabilitation hospitals. Discharge to these outpatient rehabilitation services is associated with patient factors, accessibility, and substandard inpatient quality assessments [6]. Generally, patients with persistent functional deficits, increased frailty, cognitive deficits, and/or lack of in-home support are considered for admission to outpatient rehabilitation centers, all of which are associated with increasing age and a longer, more complicated hospital stay [6], [7], [8]. Regarding COVID-19, older adults tend to suffer a more severe course of infection, and survivors are at higher risk of persistent functional deficits after infection resolution [9], [10]. It follows that these patients are also likely to require outpatient rehabilitation services and, thus, are less likely to be discharged home.
The results of our study are comparable to findings reported in recent literature. A study conducted by the CDC analyzed 126,137 electronic health records of patients with COVID-19 from the Premier Healthcare Database and reported that 60% of the patients were discharged to home or self care [11]. Furthermore, 15% of the patients were discharged to an SNF, and the remaining patients were discharged to either a home with assistance from an organization, hospice or other outpatient location. The study also reported that increased age, defined as 65 years and older, discharge to an SNF or home healthcare, and increased hospital length of stay are associated with increased risk of readmission, although they note that age and discharge to SNF have a more robust association with readmission risk compared to the length of stay. These findings further support our data and suggest that these factors are associated with a more complicated hospitalization course [11]. Additionally, a similar retrospective study reported functional status to be a strong determining factor for discharge disposition for patients with COVID-19 [12]. Key findings include patients with longer hospitalization, increased age, and comorbidities who were more likely to be discharged to an institution away from home.
Contrarily, a study involving 310 patients hospitalized with COVID-19 reported a high home discharge rate of 90.6% and, consequently, a lower SNF placement rate. However, the study's relatively younger population and patients’ preference to avoid SNF placement due to pandemic regulations were key contributors to a lowered SNF placement rate [13].
Our results further add to the existing literature regarding the long-term burden of COVID-19 infections. We found that patients discharged away from home were significantly associated with a higher mortality rate at both 30-day and 90-day intervals. As previously discussed, the patients expected to be discharged to rehabilitation centers have likely suffered a more severe course of the disease and thus are at an increased risk for mortality. Our data support recent analyses that showed increased age and SNF placement to be associated with increased mortality rates [14]. By understanding the predisposing risk factors for increased mortality following COVID-19 infection, discharge disposition decisions can be properly adjusted to plan for adequate resources necessary to care for those patients needing this type of specialized care with the goal of improving patient outcomes.
However, our study does have some limitations. Given the retrospective study design, there is a possibility of selection bias. Although this bias is common among retrospective cohort studies, understanding all limitations is helpful in determining the validity and clinical importance of our study. Furthermore, there also may be other variables necessary to be included in the adjusted analyses for which we did not account. However, determining every possible potential variable as they relate to outcome variables prior to data analysis is improbable; therefore, we selected the variables that we believed to be the most important based on prior literature and similar studies. Lastly, our mortality rates include only patients that expired in our health system and do not capture patient deaths that had occurred outside of the hospital setting. These deaths were not reported in the records and were not included in our results. This might have resulted in an underestimation of the mortality. Although mortality may be underreported, we believe this discrepancy to be minor and unlikely to change the analysis results, given the strength of the correlation both before and after adjustment.
Author contributions
SP, GTT, AR, ZC, MV, MT, RV, CD participated in the study design. RW, IN performed data collection and statistical analyses. SP, GTT, AR, ZC, RW helped draft the manuscript. RV, MT, MV, CD overviewed and supervised the project. All authors read and approved the final manuscript.
Declaration of competing interest
The authors have no conflicts of interest to declare
Acknowledgments
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Ethical approval
This study was approved by the Institutional Review Board at Creighton University (#2002233-01).
References
- 1.World Health Organization. WHO Coronavirus (COVID-19) Dashboard with Vaccination Data, https://covid19.who.int/; 2022 [accessed 18 July 2022].
- 2.Carfì A, Bernabei R, Landi F, Gemelli Against COVID-19 Post-Acute Care Study Group Persistent symptoms in patients after acute COVID-19. JAMA. 2020;324:603–605. doi: 10.1001/jama.2020.12603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Naidu SB, Shah AJ, Saigal A, Smith C, Brill SE, Goldring J, et al. The high mental health burden of “Long COVID” and its association with on-going physical and respiratory symptoms in all adults discharged from hospital. Eur Respir J. 2021;57 doi: 10.1183/13993003.04364-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Writing Committee for the COMEBAC Study Group. Morin L, Savale L, Pham T, Colle R, Figueiredo S, Harrois A, Gasnier M, Lecoq AL, Meyrignac O, Noel N, Baudry E, Bellin MF, Beurnier A, Choucha W, Corruble E, Dortet L, Hardy-Leger I, Radiguer F, Sportouch S, Verny C, Wyplosz B, Zaidan M, Becquemont L, Montani D, Monnet X. Four-month clinical status of a cohort of patients after hospitalization for COVID-19. JAMA. 2021;325:1525–1534. doi: 10.1001/JAMA.2021.3331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention. Long COVID or post-COVID conditions, https://www.cdc.gov/coronavirus/2019-ncov/long-term-effects/index.html; 2022 [accessed 18 July 2022].
- 6.Allen LA, Hernandez AF, Peterson ED, Curtis LH, Dai D, Masoudi FA, et al. Discharge to a skilled nursing facility and subsequent clinical outcomes among older patients hospitalized for heart failure. Circ Heart Fail. 2011;4:293–300. doi: 10.1161/CIRCHEARTFAILURE.110.959171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hägg S, Jylhävä J, Wang Y, Xu H, Metzner C, Annetorp M, et al. Age, frailty, and comorbidity as prognostic factors for short-term outcomes in patients with coronavirus disease 2019 in geriatric care. J Am Med Dir Assoc. 2020;21:1555–1559. doi: 10.1016/j.jamda.2020.08.014. e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Premara Blue Cross. Skilled nursing facility (SNF): admission, continued stay and transition of care guideline, https://www.premera.com/medicalpolicies-individual/11.01.510.pdf; 2022 [accessed 18 July 2022].
- 9.Tenforde MW, Kim SS, Lindsell CJ, Billig Rose E, Shapiro NI, Files DC, et al. Symptom duration and risk factors for delayed return to usual health among outpatients with COVID-19 in a multistate health care systems network — United States, March–June 2020. MMWR Morb Mortal Wkly Rep. 2020;69:993–998. doi: 10.15585/MMWR.MM6930E1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vehar S, Boushra M, Ntiamoah P, Biehl M. Post-acute sequelae of SARS-CoV-2 infection: caring for the ‘long-haulers.’. Cleve Clin J Med. 2021;88:267–272. doi: 10.3949/CCJM.88A.21010. [DOI] [PubMed] [Google Scholar]
- 11.Lavery AM, Preston LE, Ko JY, Chevinsky JR, DeSisto CL, Pennington AF, et al. Characteristics of hospitalized COVID-19 patients discharged and experiencing same-hospital readmission — United States, March–August 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1695–1699. doi: 10.15585/MMWR.MM6945E2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Roberts P, Wertheimer J, Park E, Nuño M, Riggs R. Identification of functional limitations and discharge destination in patients with COVID-19. Arch Phys Med Rehabil. 2021;102:351–358. doi: 10.1016/J.APMR.2020.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Loerinc LB, Scheel AM, Evans ST, Shabto JM, O'Keefe GA, O'Keefe JB. Discharge characteristics and care transitions of hospitalized patients with COVID-19. Healthcare. 2021;9 doi: 10.1016/J.HJDSI.2020.100512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sule AA, Rabaan AA, Tirupathi R. Mortality risk stratification helps identify patients with COVID-19 at risk of adverse outcomes. Am J Manag Care. 2021;27:309–310. doi: 10.37765/AJMC.2021.88721. [DOI] [PubMed] [Google Scholar]