Abstract
Objectives
Mechanical alignment (MA)‐total knee arthroplasty (TKA) has been challenged due to the excessive soft tissue release and the evidence of the clinical outcomes of computer assisted navigation is still limited. The aim of this ambispective cohort study was to: (i) investigate whether computer assisted navigation is capable to achieve restricted kinematic alignment (rKA)‐TKA; and (ii) compare the short‐term outcomes between rKA‐TKA and MA‐TKA.
Methods
We retrospectively included 41 patients diagnosed with osteoarthritis who received MA‐TKA between April 2019 and January 2021 and 43 patients diagnosed with osteoarthritis who received rKA‐TKA were included in the prospective cohort from January 2021 to September 2021. Demographical, peri‐operative, and radiological data were collected and compared. Unpaired two‐sample t‐test for continuous variables and χ2 test for categorical variables were used to compare various measurements in two groups. The patient‐reported outcome measures at baseline, 10 days (T1), and 6 months (T6) after surgery were statistically analyzed by generalized estimating equation (GEE) models.
Results
Fourty‐one patients (45 knees) and 43 patients (48 knees) were included in the MA and the rKA group respectively. Three constitutional knee phenotypes (II, I, IV) were the commonest in our population. Navigation improved the surgical accuracy (1.5° vs 3.5°, p < 0.001) and precision (interquartile range 4.0 vs 2.0, p < 0.001) in the rKA group than the MA group. The changes in Knee Injury and Osteoarthritis Outcome Score 12 (KOOS12), EuroQol five‐dimension questionnaire (EQ5D) from baseline to T1 and T6 for patients with on‐target rKA were larger than on‐target MA counterparts (26.053 vs 18.607, P < 0.001(KOOS12, T1), 0.457 vs 0.367 p < 0.001(EQ5D, T1); 51.017 vs 46.896, P = 0.023(KOOS12, T6), 0.606 vs 0.565, P = 0.01(EQ5D, T6)). Patients with on‐target rKA had better Forgotten Joint Score (FJS) at T1 (54.126 vs 40.965, P = 0.002) compared with on‐target MA counterparts.
Conclusions
Computer assisted navigation achieved the level of accuracy required by rKA‐TKA. rKA‐TKA offered significantly better short‐term outcomes than MA‐TKA.
Keywords: Alignment, Navigation, Patient report outcome measures, Total knee arthroplasty
Computer assisted navigation achieved the rKA‐TKA.
Introduction
As the global population ages, more and more people are suffering from osteoarthritis and it was estimated the aging of the population would result in about 1.9 million individuals with total knee arthroplasty (TKA) by 2030. 1 However, it has been reported that up to 20% of patients are not satisfied with their new joints, and this may be due to significant kinematic changes. 2 , 3 , 4 Thus, conventional mechanical alignment (MA) which pursues the completely neutral alignment of the knee has been challenged due to its standardized procedure without consideration of individual anatomy and excessive soft tissue release. 5 To solve this dilemma, kinematic alignment (KA) was developed to restore constitutional limb anatomy. The philosophy of KA is to make the implant thickness equal to the exact amount of removed bone or cartilage to restore the diverse pre‐arthritic knee joint orientation in the population. 6 The KA is thought to be available in primary osteoarthritis without severe deformity. 7 However, the safe range for kinematically positioned total knee components remains to be determined. 8 Besides, an osteoarthritic knee may be different from its pre‐arthritic status. Therefore, the restricted kinematic alignment (rKA) is developed as a compromise for MA and KA. 9 It brings back the extreme anatomies toward acceptable ranges and it has been highlighted in publications that rKA introduces significantly less change to normal anatomy compared with MA, and thereafter has a favorable effect on normal biomechanics, leading to a more balanced flexion and extension places in medial and lateral compartments. 10 , 11 A limited amount of publications demonstrated that rKA is associated with better patient‐reported outcome measures (PROMs), 12 , 13 and the short‐term PROMs of rKA‐TKA remain to be investigated.
The traditional manual method cannot fulfill the requirement of rKA‐TKA implementation as it requires higher accuracy for individualized alignment. The development of new techniques including patient specific instrumentation (PSI), navigation, and robotic surgery improved the surgical precision of TKA, 14 which may be applicable in rKA‐TKA. However, errors still existed in executing surgical plans with the use of new techniques. 15 , 16 Therefore, when implementing rKA‐TKA with new techniques such as navigation, it is crucial to assess and consider the errors in intraoperative execution. Additionally, the combination of individualized rKA planning and navigation assisted execution remains poorly investigated. The evidence of whether this approach would improve the clinical outcome is limited.
The aim of this clinical observation‐driven ambispective cohort study was to: (i) investigate whether computer assisted navigation is capable to achieve rKA‐TKA; and (ii) compare the short‐term PROMs between patients who receive rKA‐TKA and patients who were treated MA‐TKA. We hypothesize that computer assisted navigation is a reliable and effective approach to performing rKA‐TKA, and rKA‐TKA offered significantly better short‐term outcomes than MA‐TKA.
Methods
Study Design and Participants
An ambispective cohort study was conducted after being approved by the Institutional Review Board (IRB No. JS‐2775). Retrospectively, between April 2019 and January 2021, consecutive patients listed at our clinic who exclusively underwent primary mechanical aligned TKA (MA‐TKA) were screened. Cases were considered eligible for inclusion if: (i) were diagnosed with osteoarthritis; (ii) were scheduled for cruciate‐retained (CR), primary, unilateral or bilateral TKA; (iii) were between 18 and 80 years old; and (iv) were capable of accomplishing minimum 6 months follow‐up. Patients were excluded if they: (i) had a severe joint deformity (varus or valgus over 20°) or unstable knee; (ii) had peripheral nervous system disease, rheumatological diseases, or dementia; and (ii) had a history of open knee surgery. Fourty‐one patients with 45 knees who underwent MA were included. In the prospective cohort, 43 patients with 48 knees were consecutively included with the same inclusion and exclusion criteria from January 2021 to September 2021. These patients received restricted kinematic aligned TKA (rKA‐TKA). All procedures of MA and rKA group were performed by one experienced arthroplasty surgeon and his team at a single institution. Perioperative management and standardized physical therapy were conducted by the same team.
Coronal Plane Alignment of Knee Classification
The full‐length weight‐bearing phase of lower limbs was obtained from all patients. The hip‐knee‐ankle (HKA) angle, lateral distal femoral angle (LDFA), and medial proximal tibial angle (MPTA) of each participant were measured by two experienced researchers separately. According to the coronal plane alignment of knee (CPAK) classification introduced by MacDessi et al. 17 we identified “the arithmetic HKA” (aHKA) using the algorithm: aHKA = LDFA – MPTA. A positive aHKA indicates varus and a negative aHKA indicates valgus constitutional alignment. We also determined joint line obliquity (JLO) using the algorithm: JLO = LDFA + MPTA. Combining aHKA and JLO, patients were divided into nine groups. Boundaries were determined according to the standard deviation of aHKA (SD = 6) and JLO (SD = 3) of our samples.
Preoperative Plans and Surgical Procedure
Surgical planning was scheduled based on HKA, LDFA, and MPTA. All patients received a cruciate‐retaining total knee prosthesis (Legion; Smith & Nephew, Memphis, TN, USA), and a tourniquet was applied during the operation. In the MA group, HKA was set to a neutral (0°) alignment. The femoral component was set to 3° externally rotated to the posterior condylar axis. In the rKA group, surgery was planned following the “restricted KA protocol” introduced by Vendittoli et al.. 11 The goal is to restore the constitutional alignment of the knee within a safe zone. In the coronal plane, the safe zone of both MPTA/LDFA was within ±5° of neutral while the safe zone of HKA was within ±3°. If the preoperative planned LDFA/MPTA resections would lead to an HKA outside the safe zone of ±3° of neutral, then LDFA and/or MPTA were adjusted to restrict HKA within the boundaries of the safe zone. A computer assisted navigation system was applied to conduct rKA TKA (Brainlab Knee3; Smith & Nephew, Memphis, TN, USA). Specifically, after incision and exposure to the knee joint, the tibial and femoral array was placed and visibility was checked. Anatomical landmarks of the femur and tibia were registered. The leg was brought to full extension/flexion with varus/valgus stress to test stability, and based on the stability information at this stage, an intraoperative plan of target alignment was derived. The navigation plane tool was attached to the cutting block, and bone resection was performed. The femur was first resected, followed by the tibia resection. The resected surface was verified to judge if the deviation from the desired position could be accepted or needed a reassessment of the cut. After performing the resection and verification, the spacer block was placed to assess leg alignment, stability, and medial/lateral gaps during rotation. Trial components were inserted to perform final verification, followed by prosthesis placement (Fig. 1).
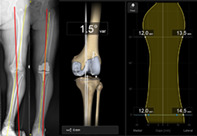
Fig. 1.
Intraoperative operation of computer assisted navigation. (A) The tibial and femoral array was placed at desired location. (B) The leg was brought into maximum flexion, applying varus and valgus stress to test stability before surgical plan was made. (C) Surgical planning layout. (D) Cutting blocks with navigation plane tool was applied during bone resection. (E) Trial components were inserted and leg alignment, stability and medial/lateral gaps during rotation was finally assessed
Data Collection and Postoperative Outcomes
Demographical information, hemoglobin, and hematocrit before surgery, 1 and 3 days after surgery were collected from the hospital information system. A radiological assessment of postoperative alignment was undertaken 3 days after surgery. The results of coronal plane HKA, LDFA, and MPTA were averaged after two different experienced researchers independently measured the same image, and the Pearson correlation coefficients were used to measure the consistency of inter‐observer comparisons. The primary endpoint of the cohort study was the completion of a 6‐month postoperative follow‐up. Patient‐reported outcome measures (PROMs) at baseline (T0) and time point of 10 days (T1) and 6 months (T6) after the operation was recorded by one trained fellow. The PROMs included: (i) the Knee Injury and Osteoarthritis Outcome Score 12 (KOOS12), the aggregated mean score of subscales: pain, function (activities of daily living and sport/recreation), and quality of life; (ii) the EuroQol five‐dimension questionnaire (EQ5D), representing overall health status. The relevant coefficients and norms of EQ5D for the Chinese population were applied to the model; 18 and (iii) Forgotten Joint Score (FJS), indicating patients' awareness of their replaced knees in daily life. The validity and reliability of all three PROMs have been thoroughly studied, 19 and all three PROMs have been shown to meet the requirements for psychometric validation and can be recommended to use as measures of TKA outcome.
Statistical Analysis
Summary statistics for demographic characteristics and clinical measures for subjects in the MA group and the rKA group were presented as mean (standard deviation, 95% confidence interval [CI]) for continuous variables and frequency (percentage) for categorical variables. Two‐sample tests (unpaired two‐sample t‐test for continuous variables and χ2 test for categorical variables) were used to compare various measurements in two groups.
To incorporate the repeated measure study design, we used the generalized estimating equations (GEE) approach to assess the effect of alignment on the post‐operation measure for each of the PROMs (change in KOOS12 from baseline, change in EQ5D from baseline, and FJS) while adjusting for demographic characteristics and clinical measures that might have influenced the outcome of interest. All the covariates were standardized before the model was fitted. It was also assumed that there was statistical significance when P < 0.05. Analyses were performed in SAS 9.4 (SAS Institute, Cary, NC, USA) and GraphPad Prism 9.0 (GraphPad Software, San Diego, CA, USA).
Given the sample size (n MA = 45, n rKA = 48) in this study, it was possible to detect an effect size (minimal detectable difference in units of standard deviation) of 0.6 for 80% statistical power at the significance level of 0.05.
Results
Demographic
For the mechanical alignment (MA) group, a total of 41 (45 knees) patients met the inclusion criteria, and a total of 43 (48 knees) patients were included in the restricted kinematic alignment (rKA) group. Among these patients, there were 32 (78.0%) females and 37 (86.0%) females in the MA group and the rKA group, respectively. The mean age of the MA group and the rKA group was 67.4 (95% CI 65.5–69.4) years and 69.3 (95% CI 67.3–71.2) years respectively. The BMI (in kg/m2) of the rKA group (mean = 27.2, 95% CI 26.2–28.2) is larger than the MA group (mean = 25.2, 95% CI 24.3–26.2) with a significant difference (P = 0.005). We measured the preoperative lower limb alignments (in degrees) of both groups of patients. There was no significant difference in HKA, LDFA, and MPTA angles between patients in the two groups before the operation (Table 1). The Pearson correlation coefficients, which measure the inter‐observer consistency in measuring preoperative HKA, LDFA, and MPTA, are computed as 0.997, 0.961, and 0.950, respectively.
TABLE 1.
Characteristics of patients at surgery in MA group and rKA group
| Characteristics | MA group | rKA group | Test statistic b | P value c |
|---|---|---|---|---|
| Sample size | 41 | 43 | ||
| Operation side a | 0.225 | 0.635 d | ||
| L | 20 (44.4%) | 19 (39.6%) | ||
| R | 25 (55.6%) | 29 (60.4%) | ||
| Gender a | 0.915 | 0.339 d | ||
| M | 9 (22.0%) | 6 (14.0%) | ||
| F | 32 (78.0%) | 37 (86.0%) | ||
| Age (years) | 67.4 (6.2; 65.5, 69.4) | 69.3 (6.4; 67.3, 71.2) | 1.312 | 0.193 |
| Height (m) | 1.6 (0.06; 1.59, 1.63) | 1.6 (0.07; 1.59, 1.63) | 0.215 | 0.830 |
| Weight (kg) | 65.6 (8.7; 62.9, 68.4) | 70.4 (9.0; 67.6, 73.2) | 2.484 | 0.015 |
| BMI (kg/m2) | 25.2 (3.0; 24.3, 26.2) | 27.2 (3.2; 26.2, 28.2) | 2.901 | 0.005 |
| Preoperative alignment (°) | ||||
| HKA | 7.8 (8.0; 5.3, 10.2) | 8.3 (6.6; 6.4, 10.2) | 0.360 | 0.720 |
| LDFA | 89.7 (5.5; 88.1, 91.4) | 90.1 (3.3; 89.1, 91.0) | 0.389 | 0.698 |
| MPTA | 85.0 (3.1; 84.1, 85.9) | 85.0 (2.8; 84.0, 85.6) | 0.289 | 0.773 |
Note: Values are presented as mean (standard deviation; 95% CI) unless indicated otherwise
t value for t‐test and χ 2 value for χ 2 test
Unpaired t‐test, except;
Frequency (percentage); and
χ 2 test.
Constitutional Alignment before Surgery
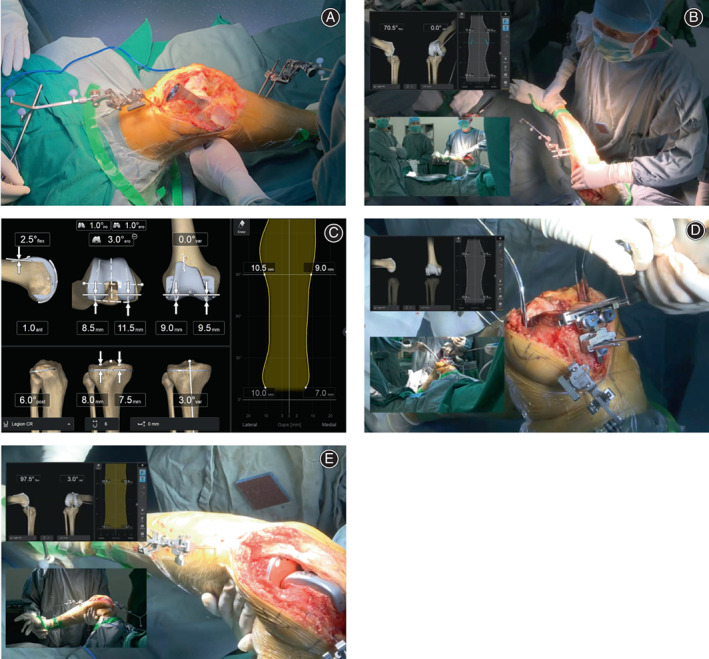
The constitutional lower limb alignments of patients before receiving knee replacement were diverse. By comparing the distribution of CPAK phenotypes between two groups of individuals, we found that the frequencies of each type were similar. The commonest CPAK types were type II (16 (35.6%) cases in the MA group and 17 (35.4%) cases in the rKA group), followed by type I, type IV, and Type V (Fig. 2A,B). Merged CPAK demonstrated the same diverse distribution pattern (Fig. 2C).
Fig. 2.
Plots of Coronal Plane Alignment of Knee (CPAK) of both MA group and rKA group. Plots of arithmetic hip‐knee‐ankle angle (aHKA) against joint line obliquity (JLO) show the preoperative CPAK types of patients in (A) MA group and (B) rKA group. (C) Combination of two groups was plotted. LDFA, lateral distal femoral angle; MPTA, medial proximal tibial angle. JLO = LDFA + MPTA; aHKA = LDFA – MPTA, varus >0°, valgus <0°
Radiological Assessment of Surgery
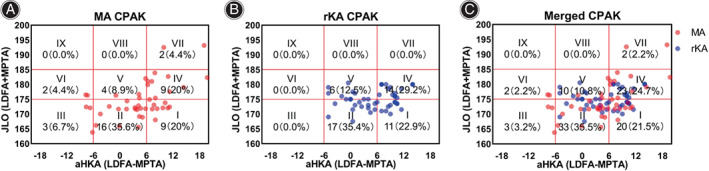
The distribution of postoperative HKA was more concentrated in the range of ±3° of neutral in the rKA group (Fig. 3A,B). Detailed radiological evaluation was summarized (Table 2). After the operation, the mean HKA (in degrees) of the rKA group (0.8, 95% CI 0.0–1.6) was smaller than that of the MA group (2.0, 95% CI 0.8–3.2), although this difference was not significant (P = 0.105). We defined cases in which the difference between target HKA (0° for MA, patient‐specific angles for rKA) and measured HKA was smaller than 1SD (≤1.5°) as on‐target cases, and for those with a difference greater than 2SD (>3°) were off‐target cases. In the MA group, 21 cases (46.7%) fell into the safe zone of ±3° of neutral, and 12 cases (26.7%) achieved on‐target MA, meanwhile, 24 cases (53.3%) were off target. In the rKA group, 41 cases (85.4%) fell into the range of ±3° of neutral. Thirty‐four cases (70.8%) were on‐target and six cases (12.5%) were off‐target. In the rKA group, operations were performed applying computer assisted navigation system. The verified accuracy (in degrees) was calculated according to the navigation system after the prosthesis was fitted. The verified accuracy of the rKA operation was 0.5 (95% CI 0.4–0.7). Actual accuracy (in degrees) was also calculated based on the image after surgery. The actual accuracy of the MA group (3.5, 95% CI 2.7–4.3) was significantly (P < 0.001) worse than that of the rKA group (1.5, 95% CI 1.1–1.9). The precision of the rKA group (interquartile range 4.0) was significantly (P < 0.001) better than that of the MA group (interquartile range 2.0) (Table 2). The Pearson correlation coefficients were used to measure the inter‐observer consistency in measuring postoperative HKA, LDFA, and MPTA, which were computed as 0.993, 0.982, and 0.963, respectively.
Fig. 3.
Distribution of HKA angle before/after surgery in MA group and rKA group. The distribution of pre‐ and post‐operational HKA angle of patients in (A) MA group and in (B) rKA group is plotted. Horizontal axis stands for HKA angle with varus >0° and valgus <0°; Vertical axis stands for number of cases with corresponding angle. The safe zone from −3° to 3° is marked as gray area.
TABLE 2.
Comparison of alignments, surgical accuracy and precision of MA and rKA group
| Postoperative alignment (°) | MA group (n = 45) | rKA group (n = 48) | Test statistic a | P value b |
| HKA | 2.0 (4.0; 0.8, 3.2) | 0.8 (2.7; 0.0, 1.6) | 1.638 | 0.105 |
| LDFA | 91.5 (3.3; 90.5, 92.5) | 90.5 (1.8; 90.0, 91.0) | 1.777 | 0.079 |
| MPTA | 89.4 (2.5; 88.7, 90.2) | 89.7 (1.9; 89.1, 90.2) | 0.456 | 0.650 |
| Safe zone c | 21 (46.7%) | 41 (85.4%) | 15.69 | <0.001 d |
| On‐target c | 12 (26.7%) | 34 (70.8%) | 18.12 | <0.001 d |
| Off‐target c | 24 (53.3%) | 6 (12.5%) | 17.72 | <0.001 d |
| Verified Accuracy (°) | – | 0.5 (0.5; 0.4, 0.7) | – | |
| Actual Accuracy (°) | 3.5 (2.8; 2.7, 4.3) | 1.5 (1.4; 1.1, 1.9) | 4.301 | <0.001 |
| Precision e | 4.0 | 2.0 | 3.541 | <0.001 f |
Note: Safe zone: HKA within ± 3° of neutral;On‐target: the difference between specific target value and measurement is within 1.5°; Off‐target: the difference between specific target value and measurement is larger than 3°; Verified Accuracy = |HKAverification—HKAplan|; Actual Accuracy = |HKAfinal—HKAplan|; Precision was calculated as interquartile range of HKAfinal – HKAplan; Values are presented as mean (standard deviation; 95% CI) unless indicated otherwise
t value for t‐test, χ 2 value for χ 2 test, and Z value for Westenberg test
Unpaired t‐test
Frequency (percentage)
χ 2 test
Calculated value; and
Westenberg test for interquartile range equality.
Perioperative Record and Complications
Both operation time and tourniquet time were shorter in the MA group compared to the rKA group. In terms of blood loss, there was no significant difference in both hemoglobin and hematocrit between the two groups of patients from the day before the operation to 3 days after the operation. For those patients in the MA group, the length of hospitalization was significantly longer than that of patients in the rKA group. During the 6‐months follow‐up, complications, including aseptic loosening, joint instability, periprosthetic infection, and surgical site infection, were not observed in both groups (Table 3).
TABLE 3.
Perioperative records of patients in MA group and rKA group
| MA group | rKA group | Test statistic b | P value c | |
|---|---|---|---|---|
| Operation time (min) | 104.3 (17.9; 98.8, 109.8) | 121.7 (15.4; 117.0, 126.4) | 4.862 | <0.001 |
| Tourniquet time (min) | 64.5 (10.0; 61.5, 67.6) | 83.9 (10.2; 80.9, 86.9) | 9.202 | <0.001 |
| Length of Stay (day) | 9.8 (4.6; 8.3, 11.2) | 7.5 (1.5; 7.0, 7.9) | 3.195 | 0.002 |
| Hemoglobin (g/L) | ||||
| Day 0 | 136.7 (13.7; 132.5, 140.9) | 136.9 (11.2; 133.6, 140.2) | 0.099 | 0.921 |
| Day 1 | 124.8 (18.3; 119.2, 130.3) | 126.4 (10.5; 123.3, 129.5) | 0.514 | 0.609 |
| Day 3 | 118.1 (13.6; 113.9, 122.3) | 117.1 (9.2; 114.4, 199.8) | 0.412 | 0.682 |
| Hematocrit (%) | ||||
| Day 0 | 40.0 (7.3; 25.7, 54.3) | 39.5 (7.1; 25.6, 53.4) | 0.455 | 0.961 d |
| Day 1 | 36.2 (7.2; 22.1, 50.3) | 37.1 (7.0; 23.4, 50.8) | 0.861 | 0.928 d |
| Day 3 | 35.0 (7.1; 21.1, 48.9) | 34.8 (6.9; 21.3, 48.3) | 0.289 | 0.984 d |
| Complications a | 0 | 0 | – | |
Note: Operation time: total operation time of TKA recorded in surgical system; Tourniquet time: The length of time when tourniquet was applying; Day 0: the day before surgery; Day 1: the day after surgery; Day 3: three days after surgery; Complications: cases with aseptic loosening, joint instability, periprosthetic infection and surgical site infection. Values are presented as mean (standard deviation; 95% CI) unless indicated otherwise
Frequency
t value for t‐test and χ 2 value for χ 2 test
Unpaired t‐test
Z test for two proportions.
Short‐term Outcomes
We presented the results from the GEE models that examined the effects of alignment and other demographic characteristics and clinical measures on each of the PROMs (Table 4) as well as each estimated PROMs for subjects with on‐target rKA and on‐target MA at 10 days (T1) and 6 months (T6) after the operation (Table 5). We found that, after adjusting for potential effects of age, sex, BMI, operation and tourniquet time, length of stay, change in HKA, whether the case was on target, baseline KOOS12, and baseline EQ5D, there was a statistically significant difference in each of the PROMs between subjects with on‐target rKA and those with on‐target MA at T1. The estimated change in KOOS12 from baseline to T1 for subjects with on‐target rKA was 26.053 (95% CI 23.658–28.448) and that for subjects with on‐target MA was 18.607 (95% CI 15.691–21.523), resulting in a statistically significant difference (P < 0.001) in the change in KOOS12; the same trends were also observed in EQ5D. The estimated FJS at T1 for subjects with on‐target rKA was also higher than that for subjects with on‐target MA. Similar observations can also be made for T6.
TABLE 4.
Parameter estimates, 95% confidence intervals, and p‐values for GEE models that assessed the effect of alignment on PROMs after adjusting for demographic characteristics and clinical measures
| Effect | Change in KOOS12 from T0 | Change in EQ5D from T0 | FJS | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Estimate (95% CI) | Z value | P‐value | Estimate (95% CI) | Z value | P‐value | Estimate (95% CI) | Z value | P‐value | |
| Intercept time | 18.607 (15.691, 21.523) | 12.51 | <0.001 | 0.367 (0.334, 0.400) | 21.56 | <0.001 | 40.965 (33.752, 48.178) | 11.13 | <0.001 |
| T6 | 28.288 (25.373, 31.203) | 19.02 | <0.001 | 0.196 (0.172, 0.220) | 16.13 | <0.001 | 18.615 (15.816, 21.414) | 13.03 | <0.001 |
| Alignment | |||||||||
| rKA | 7.446 (3.706, 11.186) | 3.90 | <0.001 | 0.090 (0.049, 0.131) | 4.27 | <0.001 | 13.161 (4.717, 21.605) | 3.06 | 0.002 |
| Time × alignment | |||||||||
| T6 × rKA | −3.324 (−7.091, 0.443) | −1.73 | 0.084 | −0.049 (−0.082, −0.016) | −2.85 | 0.004 | −6.486 (−10.208, −2.764) | −3.42 | 0.001 |
| Age | −1.768 (−2.489, −1.047) | −4.80 | <0.001 | −0.012 (−0.022, −0.002) | −2.65 | 0.008 | −2.405 (−3.924, −0.886) | −3.10 | 0.002 |
| Sex | |||||||||
| Female | −1.283 (−3.129, 0.563) | −1.36 | 0.173 | −0.016 (−0.040, 0.008) | −1.38 | 0.168 | −0.715 (−5.192, 3.762) | −0.31 | 0.754 |
| BMI | 0.081 (−0.711, 0.873) | 0.20 | 0.842 | −0.004 (−0.012, 0.004) | −0.87 | 0.385 | 1.045 (−0.374, 2.464) | 1.44 | 0.149 |
| Operation time | −0.831 (−2.146, 0.484) | −1.24 | 0.216 | −0.010 (−0.022, 0.002) | −1.56 | 0.120 | 0.803 (−1.870, 3.476) | 0.59 | 0.556 |
| Tourniquet time | 0.225 (−1.123, 1.573) | 0.33 | 0.744 | 0.002 (−0.014, 0.018) | 0.27 | 0.791 | −0.649 (−4.122, 2.824) | −0.37 | 0.714 |
| Length of stay | −0.342 (−1.351, 0.667) | −0.66 | 0.507 | −0.005 (−0.017, 0.007) | −0.77 | 0.443 | 0.600 (−2.246, 3.446) | 0.41 | 0.679 |
| Change in HKA | 0.639 (−0.296, 1.574) | 1.34 | 0.181 | −0.001 (−0.011, 0.009) | −0.23 | 0.815 | −1.561 (−3.421, 0.299) | −1.64 | 0.100 |
| Target | |||||||||
| Not on‐target | 2.752 (0.108, 5.396) | 2.04 | 0.041 | 0.032 (0.007, 0.057) | 2.56 | 0.011 | 1.956 (−4.128, 8.040) | 0.63 | 0.529 |
| Target × alignment | |||||||||
| Not on‐target × rKA | −5.744 (−9.307, −2.181) | −3.16 | 0.002 | −0.052 (−0.089, −0.015) | −2.76 | 0.006 | −0.586 (−7.952, 6.780) | −0.16 | 0.876 |
| Baseline KOOS12 | −8.196 (−9.431, −6.961) | −13.00 | <0.001 | 0.005 (−0.007, 0.017) | 0.79 | 0.427 | 0.598 (−1.666, 2.862) | 0.52 | 0.605 |
| Baseline EQ5D | 0.876 (−0.245, 1.997) | 1.53 | 0.125 | −0.195 (−0.207, −0.183) | −32.44 | <0.001 | 1.418 (−0.961, 3.797) | 1.17 | 0.243 |
TABLE 5.
Estimated PROMs and 95% confidence intervals at T1 and T6 for subjects with on‐target rKA and on‐target MA based on GEE models that adjusted for demographic characteristics and clinical measures
| On‐target rKA | On‐target MA | Z Value | P‐value | |
|---|---|---|---|---|
| Estimated change in KOOS12 from baseline | ||||
| T1 | 26.053 (23.658, 28.448) | 18.607 (15.691, 21.523) | 3.90 | < 0.001 |
| T6 | 51.017 (48.567, 53.467) | 46.896 (44.187, 49.605) | 2.28 | 0.023 |
| Estimated change in EQ5D from baseline | ||||
| T1 | 0.457 (0.424, 0.490) | 0.367 (0.334, 0.400) | 4.27 | < 0.001 |
| T6 | 0.606 (0.581, 0.631) | 0.565 (0.538, 0.592) | 2.58 | 0.010 |
| Estimated FJS | ||||
| T1 | 54.126 (48.932, 59.320) | 40.965 (33.750, 48.180) | 3.06 | 0.002 |
| T6 | 66.256 (60.809, 71.703) | 59.581 (52.486, 66.676) | 1.64 | 0.102 |
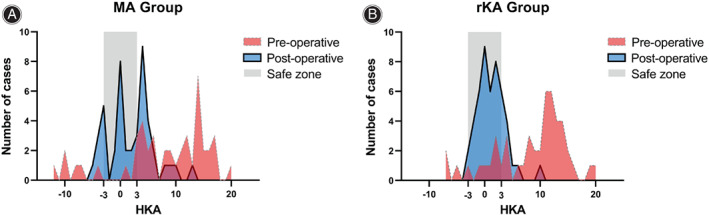
We also found some other demographic characteristics and clinical measures associated with the outcomes of interest. For example, when there was a one standard deviation increase in age (about 6 years), it was estimated that the change in KOOS12 after the operation would be 1.768 (95% CI 1.047–2.489, P < 0.001) lower, and the change in EQ5D and the FJS after the operation would also be lower. In addition, the baseline KOOS12 was found to have a statistically significant effect on the change in KOOS12 from baseline (estimate = −8.196, 95% CI ‐9.431 to −6.961, P < 0.001), and the baseline EQ5D was also found to have a statistically significant effect on the change in EQ5D from baseline. Note that, the covariates of target and target by alignment interaction were included in the model to account for potentially different effects between rKA and MA that are not on target compared to their on‐target counterparts. Interestingly, subjects with MA that is not on‐target were found to have 2.752 (95% CI 0.108–5.396, P = 0.041) higher increase in KOOS12 after operation, 0.032 (95% CI 0.007–0.057, P = 0.011) higher increase in EQ5D after operation, and 1.956 (95% CI −4.128 to 8.040, P = 0.529) higher FJS compared to those with on‐target MA. Some visualizations for the paths of KOOS12, EQ5D, and FJS were also presented (Fig. 4A–C).
Fig. 4.

Visualization of short‐term clinical outcomes of patients in different timepoints. The (A) changes in estimated KOOS12 from baseline (T0), (B) changes in EQ5D from baseline (T0) and (C) estimated FJS at different timepoints are plotted. T0: before surgery; T1: 10 days after surgery; T6: 6 months after surgery. *P < 0.05, **P < 0.01, ***P < 0.001.
Discussion
In this study, we adopted a patient‐specific rKA strategy based on phenotypes analysis. We demonstrated that the computer assisted navigation provided adequate accuracy and precision in rKA‐TKA and rKA‐TKA had priority over MA‐TKA in short‐term clinical outcomes.
Rationale of Adopting rKA Strategy
The key to the success of TKA is to provide a stable and comfortable kinematic by achieving proper alignment and balanced mediolateral gaps and correcting joint deformities. 20 As the earliest and most widely used strategy, mechanical alignment (MA) fulfills the need to improve prosthetic survival at the early stage when the quality of the prosthesis remained poor. 21 However, more and more evidence indicates that MA‐TKA fails to restore preoperative kinematics. 22 Hence, with the full development of prosthetic materials, surgeons began to focus on the phenotypes of the knee of the population. Several studies have revealed the diversity of knee phenotypes, therefore the neutral lower limb alignment pursued by the traditional MA does not conform to the constitutional anatomy of individuals. 23 , 24 , 25 Among different classifications, we regard the CPAK classification proposed by MacDessi et al. 17 as a practical system since the nine classifications defined based on mathematical formulas have good clinical applicability. In our population, the preoperative CPAK distribution was similar to that of authors that phenotype I, II, and IV were three main types, rather than type V, of which preoperative alignment was as neutral as the alignment that the MA strategy pursued. Hence, this was convincing enough for us to choose a more individualized strategy. KA seemed to be an option for us because it restores the same anatomy as preoperative knees and does not alter original gaps and ligament laxity. 26 We retrospectively analyzed the lower limb alignments of the MA group and the mean preoperative HKA was 7.8°, which was out of the commonly accepted safe range of ±3°. This supported our choice to use the rKA strategy so that we could reduce soft tissue release and partially restore the constitutional kinematics without potentially sacrificing long‐term survival.
Navigation Is Capable for rKA‐TKA with Accuracy, Precision and Safety
To accurately implement rKA alignment, computer assisted navigation was applied to formulate the individualized alignment goal for each patient, based on the preoperative alignment. Based on the previous surgical experience of our center, there was an error of about 0.5° in the navigation system. This meant even if we strictly followed the guide during operation, there was still an average error of 0.5° from the planned value when performing alignment verification after the prosthesis was installed. The same phenomenon was observed in this study that the verified accuracy of navigation was 0.5°. Therefore, we recommend in order to improve the rKA‐TKA success rate with navigation, the planned HKA should not exceed ±2.5° to account for errors in navigation assisted surgery. This preoperative planning strategy was regarded as restricted rKA (rrKA). In the rKA group, the application of navigation improved the accuracy and precision compared to the conventional method in the MA group, which was widely reported by other publications. 27 , 28 , 29
We evaluated the radiological outcomes of two groups. Before surgery, the distribution of HKA in both groups was scattered and the varus of more than 3° was predominant. To determine whether the targeted alignment was achieved for each case, the difference between targeted HKA and postoperative HKA was calculated. The ratio of on‐target cases was higher in the rKA group compared to the MA group (P < 0.001), and the off‐target rate was lower (P < 0.001). This off‐target rate of navigation assisted TKA (rKA group, 12.5%) was similar to the results reported by Shah et al.. 16 In terms of keeping postoperative HKA within a ± 3° safe zone, the rKA group was also superior to the MA group (P < 0.001). To summarize, in the aspect of postoperative radiology assessment, computer assisted navigation is capable to achieve rKA‐TKA with high accuracy and precision.
We found that the operation time and tourniquet time significantly increased in the rKA group than in the MA group, and this was consistent with some other studies. 28 , 30 In a study based on a large sample size, Sekimura et al. claimed that the operation time of navigation TKA was longer than the traditional TKA at the beginning, and later developed to be shorter by 2018. 31 In our opinion, the increase in time was due to: (i) there were more steps in navigation TKA, for instance, planning, registration, verification, etc. which prolonged the operation time; and (ii) there was a learning curve when applying new techniques so that the time was able to be shortened in following cases. The reasons that surgeons cared about operation time were due to the increase in time associated with infection and more blood loss. We, therefore, investigated the blood loss by acquiring the value of hemoglobin and hematocrit from the day before the operation (day 0) to three days after (day 3). There was no significant blood loss between these two groups, and this was not consistent with studies indicating navigation could reduce the blood loss and transfusion rate. 32 , 33 , 34 In both groups, no TKA‐related complication was reported during the 6‐month follow‐up.
rKA‐TKA Can Improve Short‐term PROMs
In this ambispective study, we had been not able to apply navigation in the MA group, so the accuracy and precision of surgery were different in the two groups. Therefore, we used GEE models to adjust for this difference in accuracy and precision, along with some other demographic characteristics (i.e., age, sex, operation sides, etc.) and clinical measures that may have potential effects on PROMs. In addition, the correlation between the measurements taken on the two knees of the bilateral TKA cases can be significantly larger than the correlation between the measurements taken on two separate patients, and GEE models are also capable of adjusting for such correlation in the analysis. 35 , 36 One of the most important discoveries was that when surgery was precisely performed to achieve the target (i.e., MA or rKA) in both groups, those patients who received rKA‐TKA had a better short‐term performance than those with MA‐TKA. This made up for deficiencies in the design of this ambispective study, and this was also in line with the purpose pursued by the rKA strategy. In our opinion, this improved performance was due to the limited soft tissue release and correction of severe preoperative deformities, resulting in better knee kinematics. The higher KOOS12 and EQ5D represented less pain and discomfort, and higher FJS may suggest a higher willingness to exercise. We believed these improvements were critical for recovery, meaning that patients can start ROM and other functional exercises earlier, which would therefore reduce the incidence of postoperative deep vein thrombosis and allow patients to return to normal life earlier. 37 , 38 We also found that the outcomes of those with MA that were not on‐target were better than those with on‐target MA. This was because, in our MA group, the alignments of those not on‐target cases were inadvertently closer to the goal of rKA or KA. This might suggest the superiority of rKA over MA from another perspective. Greater BMI has been widely identified as a risk factor for osteoarthritis, but we did not observe this effect on our results of PROMs. It was not surprising that those more aged people had a poorer prognosis, and those who had worse preoperative knee conditions can benefit more from the surgery.
Strengths and Limitations
The strength of this study lies in the comprehensive data collection and rigorous statistical analysis, which provided a basis for clinical decision‐making in the application of navigation‐assisted rKA‐TKA. This study has some limitations: (i) we were not able to retrospectively include more patients in the MA group because of limited cases in our center: and the sample size was also not large enough for us to match patients between two groups in the study; (ii) navigation was only applied in the rKA group but not in the MA group. However, the GEE model is capable of taking into account the confounding effect of different surgical techniques 35 , 36 ; and (iii) we only followed the patients for 6 months, so this study was not able to provide further evidence for longer clinical outcomes.
Based on this study, we recommend applying navigation in rKA‐TKA to improve short‐term outcomes. In the future, larger sample size will be studied to establish knee phenotypes based on our population, and the prognosis of patients with different phenotypes will be investigated to provide a more detailed flow chart for preoperational planning to implement real individualized rKA‐TKA and improve the prognosis.
Conclusion
The study found that computer assisted navigation achieved the level of accuracy required to perform rKA‐TKA. Within the knee phenotypes demonstrated in this series, rKA‐TKA offered significantly better short‐term functional outcomes than MA‐TKA.
Author Contributions
All authors had full access to the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Ruichen Ma contributed in conceptualization, data curation, formal analysis, investigation, methodology, validation, visualization, writing original draft and editing. Xi Chen contributed in conceptualization, data curation, funding acquisition, methodology, supervision and draft review. Haolin Li contributed in formal analysis, methodology, draft review and editing. Yiou Wang, Songlin Li and Shanni Li contributed in investigation, methodology, draft review and editing. Wenwei Qian contributed in conceptualization, methodology, funding acquisition, supervision and draft review.
Conflict of Interest
The authors have no conflicts of interest relevant to this article.
Ethics Statement
This study involving human participants was reviewed and approved by the Institutional Review Board of Peking Union Medical College Hospital. The study was undertaken with the understanding and written informed content of each participant.
Authorship Declaration
All authors listed meet the authorship criteria according to the latest guidelines of the International Committee of Medical Journal Editors, and all authors are in agreement with the manuscript.
Acknowledgment
This work was supported by the Non‐profit Central Research Institute Fund of Chinese Academy of Medical Science. Grant number NWB20204183/A2020418300. The authors commit to making the relevant anonymized study data and analytical methods available on reasonable request.
Ruichen Ma and Xi Chen are share first authorship.
References
- 1. Singh JA, Yu S, Chen L, Cleveland JD. Rates of total joint replacement in the United States: future projections to 2020‐2040 using the National Inpatient Sample. J Rheumatol. 2019;46(9):1134–40. [DOI] [PubMed] [Google Scholar]
- 2. Collins M, Lavigne M, Girard J, Vendittoli PA. Joint perception after hip or knee replacement surgery. Orthop Traumatol Surg Res. 2012;98(3):275–80. [DOI] [PubMed] [Google Scholar]
- 3. McClelland JA, Webster KE, Feller JA. Gait analysis of patients following total knee replacement: a systematic review. Knee. 2007;14(4):253–63. [DOI] [PubMed] [Google Scholar]
- 4. Bourne RB, Chesworth BM, Davis AM, Mahomed NN, Charron KDJ. Patient satisfaction after total knee arthroplasty: who is satisfied and who is not? Clin Orthop Relat Res. 2010;468(1):57–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Bellemans J. Neutral mechanical alignment: a requirement for successful TKA: opposes. Orthopedics. 2011;34(9):e507–9. [DOI] [PubMed] [Google Scholar]
- 6. Nisar S, Palan J, Rivière C, Emerton M, Pandit H. Kinematic alignment in total knee arthroplasty. EFORT Open Rev. 2020;5(7):380–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Hirschmann MT, Becker R, Tandogan R, Vendittoli P‐A, Howell S. Alignment in TKA: what has been clear is not anymore! Knee Surg Sports Traumatol Arthrosc. 2019;27(7):2037–9. [DOI] [PubMed] [Google Scholar]
- 8. Rivière C, Iranpour F, Auvinet E, Howell S, Vendittoli PA, Cobb J, et al. Alignment options for total knee arthroplasty: a systematic review. Orthop Traumatol Surg Res. 2017;103(7):1047–56. [DOI] [PubMed] [Google Scholar]
- 9. Vendittoli P‐A, Martinov S, Blakeney WG. Restricted kinematic alignment, the fundamentals, and clinical applications. Front Surg. 2021;8:697020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Gu Y, Roth JD, Howell SM, Hull ML. How frequently do four methods for mechanically aligning a total knee arthroplasty cause collateral ligament imbalance and change alignment from normal in white patients? AAOS exhibit selection. J Bone Joint Surg Am. 2014. Jun 18;96(12):e101. [DOI] [PubMed] [Google Scholar]
- 11. Almaawi AM, Hutt JRB, Masse V, Lavigne M, Vendittoli P‐A. The impact of mechanical and restricted kinematic alignment on knee anatomy in total knee arthroplasty. J Arthroplasty. 2017;32(7):2133–40. [DOI] [PubMed] [Google Scholar]
- 12. Blakeney W, Clément J, Desmeules F, Hagemeister N, Rivière C, Vendittoli P‐A. Kinematic alignment in total knee arthroplasty better reproduces normal gait than mechanical alignment. Knee Surg Sports Traumatol Arthrosc. 2019;27(5):1410–7. [DOI] [PubMed] [Google Scholar]
- 13. Laforest G, Kostretzis L, Kiss M‐O, Vendittoli P‐A. Restricted kinematic alignment leads to uncompromised osseointegration of cementless total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2022;30(2):705–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Gao J, Dong S, Li JJ, Ge L, Xing D, Lin J. New technology‐based assistive techniques in total knee arthroplasty: a Bayesian network meta‐analysis and systematic review. Int J Med Robot. 2020;e2189. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 15. Amanatullah DF, Di Cesare PE, Meere PA, Pereira GC. Identification of the landmark registration safe zones during total knee arthroplasty using an imageless navigation system. J Arthroplasty. 2013;28(6):938–42. [DOI] [PubMed] [Google Scholar]
- 16. Shah SM, Sciberras NC, Allen DJ, Picard F. Technical and surgical causes of outliers after computer navigated total knee arthroplasty. J Orthop. 2020;18:171–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. MacDessi SJ, Griffiths‐Jones W, Harris IA, Bellemans J, Chen DB. Coronal plane alignment of the knee (CPAK) classification. Bone Joint J. 2021;103‐B(2):329–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Yang Z, Busschbach J, Liu G, Luo N. EQ‐5D‐5L norms for the urban Chinese population in China. Health Qual Life Outcomes. 2018;16(1):210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Wang Y, Yin M, Zhu S, Chen X, Zhou H, Qian W. Patient‐reported outcome measures used in patients undergoing total knee arthroplasty. Bone Joint Res. 2021;10(3):203–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Blakeney WG, Vendittoli P‐A. The future of TKA. In: Rivière C, Vendittoli P‐A, editors. Personalized hip and knee joint replacement. Cham: Springer; 2020. [PubMed] [Google Scholar]
- 21. Robinson RP. The early innovators of today's resurfacing condylar knees. J Arthroplasty. 2005;20(1 Sundefined1):2–26. [DOI] [PubMed] [Google Scholar]
- 22. Lee YS, Howell SM, Won Y‐Y, Lee O‐S, Lee SH, Vahedi H, et al. Kinematic alignment is a possible alternative to mechanical alignment in total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2017;25(11):3467–79. [DOI] [PubMed] [Google Scholar]
- 23. Moser LB, Hess S, de Villeneuve Bargemon J‐B, Faizan A, LiArno S, Amsler F, et al. Ethnical differences in knee phenotypes indicate the need for a more individualized approach in knee arthroplasty: a comparison of 80 Asian knees with 308 Caucasian knees. J Pers Med. 2022;12(1):121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Hirschmann MT, Moser LB, Amsler F, Behrend H, Leclerq V, Hess S. Functional knee phenotypes: a novel classification for phenotyping the coronal lower limb alignment based on the native alignment in young non‐osteoarthritic patients. Knee Surg Sports Traumatol Arthrosc. 2019;27(5):1394–402. [DOI] [PubMed] [Google Scholar]
- 25. Lin Y‐H, Chang F‐S, Chen K‐H, Huang K‐C, Su K‐C. Mismatch between femur and tibia coronal alignment in the knee joint: classification of five lower limb types according to femoral and tibial mechanical alignment. BMC Musculoskelet Disord. 2018;19(1):411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. MacDessi SJ, Griffiths‐Jones W, Chen DB, Griffiths‐Jones S, Wood JA, Diwan AD, et al. Restoring the constitutional alignment with a restrictive kinematic protocol improves quantitative soft‐tissue balance in total knee arthroplasty: a randomized controlled trial. Bone Joint J. 2020;102‐B(1):117–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Song E‐K, Seon J‐K, Park S‐J. Flexion‐extension gaps balanced using navigation assistance in TKA. Orthopedics. 2009;32(10 Suppl):26–30. [DOI] [PubMed] [Google Scholar]
- 28. Martin A, Wohlgenannt O, Prenn M, Oelsch C, von Strempel A. Imageless navigation for TKA increases implantation accuracy. Clin Orthop Relat Res. 2007;460:178–84. [DOI] [PubMed] [Google Scholar]
- 29. Hannan R, Free M, Arora V, Harle R, Harvie P. Accuracy of computer navigation in total knee arthroplasty: a prospective computed tomography‐based study. Med Eng Phys. 2020;79:52–9. [DOI] [PubMed] [Google Scholar]
- 30. Li Y, Tian H, Geng X. Effect of the surgical time and coronalmechanical alignment after total knee arthroplasty using computer navigation system, traditionalor 3D printing patient‐specific instruments. Zhonghua Yi Xue Za Zhi. 2018;98(27):2157–61. [DOI] [PubMed] [Google Scholar]
- 31. Sekimura TK, Upfill‐Brown A, Hsiue PP, Khoshbin A, Zeegen EN, Stavrakis AI. Trends in operative time and short‐term outcomes after conventional and navigated total knee arthroplasty. Arthroplasty Today. 2021;8:188–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. McConnell J, Dillon J, Kinninmonth A, Sarungi M, Picard F. Blood loss following total knee replacement is reduced when using computer‐assisted versus standard methods. Acta Orthop Belg. 2012;78(1):75–9. [PubMed] [Google Scholar]
- 33. Millar NL, Deakin AH, Millar LL, Kinnimonth AWG, Picard F. Blood loss following total knee replacement in the morbidly obese: effects of computer navigation. Knee. 2011;18(2):108–12. [DOI] [PubMed] [Google Scholar]
- 34. Schnurr C, Csécsei G, Eysel P, König DP. The effect of computer navigation on blood loss and transfusion rate in TKA. Orthopedics. 2010;33(7):474. [DOI] [PubMed] [Google Scholar]
- 35. Have TRT, Diggle PJ, Liang K‐Y, Zeger SL. Analysis of longitudinal data. J Am Stat Assoc. 1995;90(431):1123. [Google Scholar]
- 36. Liang K‐Y, Zeger SL. Longitudinal data analysis using generalized linear models. Biometrika. 1986;73(1):13–22. [Google Scholar]
- 37. Aresti N, Kassam J, Bartlett D, Kutty S. Primary care management of postoperative shoulder, hip, and knee arthroplasty. BMJ. 2017;359:j4431. [DOI] [PubMed] [Google Scholar]
- 38. Fleischman AN, Crizer MP, Tarabichi M, Smith S, Rothman RH, Lonner JH, et al. 2018 john N. insall award: recovery of knee flexion with unsupervised home exercise is not inferior to outpatient physical therapy after TKA: a randomized trial. Clin Orthop Relat Res. 2019;477(1):60–9. [DOI] [PMC free article] [PubMed] [Google Scholar]


