Abstract
Objective:
Depression is a public health crisis, and scalable, affordable interventions are needed. Although many psychosocial interventions are effective, there is little research investigating their sustained, long-term influence on well-being. The purpose of this study was to examine whether a prenatal mindfulness intervention with demonstrated benefit for women’s depressive symptoms during the early postpartum period would exert effects through 8 years.
Method:
The sample of 162 lower-income women was racially and ethnically diverse. Women were assigned to receive an 8-week mindfulness-based intervention during pregnancy (MIND) or treatment as usual (TAU). Repeated assessments of depressive symptoms were collected using the PHQ-9 at baseline, post-intervention, and following childbirth (1-, 2-, 3–4, 5-, 6-, and 8 years from baseline). The most recent assessment of depressive symptoms was collected during the COVID-19 pandemic.
Results:
MIND and TAU women were equivalent on sociodemographic factors and depressive symptoms at baseline. Depressive symptoms at all follow-up assessments through 8 years were significantly lower among women in MIND compared to TAU. The odds of moderate or higher depressive symptoms were greater among TAU compared to MIND women at all timepoints except the 6-year assessment. By year 8, 12% of women in MIND reported moderate or more severe depressive symptoms compared to 25% of women in TAU.
Conclusions:
Results suggest the effects of a group-based psychosocial intervention during pregnancy may endure for years, well beyond the initial perinatal period. Investing in prevention and intervention efforts for mental health during pregnancy may have sustained benefits for the well-being of women.
Prenatal depression affects 12–27% of pregnant individuals (Mahaffey & Lobel, 2018). It is one of the strongest predictors of persistent depression (Guintivano et al., 2018), which is a major source of economic and social burden (Luca et al., 2020). Beyond the exceptional burden that depression places on women, its effects may extend to the entire family. Maternal depression has been associated with a broad range of deficits to offspring social, emotional, and cognitive functioning that may last well after initial exposure during the perinatal period (Goodman, 2020; Stein et al., 2014). Thus, detecting and intervening to prevent or treat depression during pregnancy is critical for reducing negative outcomes for women and their children.
In response to clinical guidelines and recommendations, it is now recommended that all pregnant and postpartum people are screened for depression and referred for follow-up care if appropriate (American College of Obstetricians and Gynecologists, 2018; Siu & and the US Preventive Services Task Force (USPSTF), 2016). Screening is an important component of care to support maternal mental health during the perinatal period but is insufficient; even when positive screens are identified, there is a dearth of available services and effective, scalable interventions. A U.S. Preventive Services Task Force Evidence Report concluded that psychological (e.g., cognitive behavioral therapy) or supportive (e.g., peer mentoring) interventions may be effective in preventing perinatal depression, however the majority of the reviewed treatment studies recruited non-Hispanic White women and none followed women for more than one year postpartum (O’Connor et al., 2019). More research is needed to identify the long-term effectiveness of prevention and early intervention efforts and additional evidence among racially/ethnically diverse and socioeconomically disadvantaged populations is especially critical (Stein et al., 2014).
Mindfulness-based interventions are widely used in clinical and non-clinical populations; a recent study of 44 meta-analyses of randomized controlled trials concluded that they hold “substantial transdiagnostic potential” across a wide range of outcomes, including depression (Goldberg et al., 2022, p. 126). For pregnant individuals, mindfulness-based interventions may be particularly appealing due to their brief duration and non-pharmacological approach (Vieten & Astin, 2008), and appear to be effective in the reduction or prevention of prenatal depression, at least in the short-term (Lucena et al., 2020). A systematic review of prenatal mindfulness-based interventions observed treatment-related reductions in depressive symptoms, although such results were less robust in randomized controlled trials compared to non-controlled trials and only followed women through 6 months postpartum (Shi & MacBeth, 2017).
In an initial study of an ethnically and racially diverse sample of low-income pregnant women, our team reported significantly lower depressive symptoms during the 3rd trimester of pregnancy and at six months postpartum among those who received a mindfulness-based intervention during pregnancy compared to treatment as usual (Epel et al., 2019). Although this evidence of short-term positive effects is compelling, understanding how long such effects are sustained is important to determine the social and economic value of intervention efforts and to understand if certain postnatal periods are vulnerable to attenuating treatment effects. In the present study, we examine the effects of the mindfulness intervention on women’s depressive symptoms from baseline through 8 years, a distal time period that is rarely collected in clinical trials. The timing of the final follow-up assessment (during COVID-19) provided an opportunity to detect whether intervention effects were sustained in the context of increased environmental stressors, potentially buffering the mental health impact of the pandemic.
Method
Participants
Women (N = 215) were recruited during pregnancy to participate in an 8-week mindfulness-based group intervention (MIND) focused on stress, depression, healthy eating, and gestational weight gain or treatment as usual (TAU) (ClinicalTrials.Gov identifier: NCT01307683). The following inclusion criteria were assessed by self-report: 1) English-speaking, 2) 18–45 years of age, 3) pre-pregnancy body mass index between 25 and 40 kg/m2, and 4) household income less than 500% of the federal poverty level. Women were excluded if they: 1) were non-English speaking, 2) had serious substance abuse or mental health problems that investigators felt would serve as a barrier for participation in the group intervention, 3) had medical conditions that might affect gestational weight gain (including diabetes, HIV, hypertension, and eating disorders), 4) had polycystic ovarian syndrome treated with metformin, 5) maintained a regular meditation practice (defined as 20 minutes or more at least twice a week), 6) had recent weight loss (more than 5% of one’s body weight within the prior six months), 7) used corticosteroids chronically, or 8) had previous gastric bypass surgery. In the original study, women were recruited on the basis of income and BMI, not depression, however 27% of the sample met criteria for moderate or more severe depressive symptoms (as indicated by the PHQ-9) at baseline (see Table 1) and the intervention was designed to prevent excessive weight gain in overweight and obese women by reducing stress, improving stress-related health behaviors, and promoting well-being. Thus, we characterize this intervention as a mixed prevention/primary intervention.
Table 1.
Sample demographics overall and by intervention group
| Characteristic | Overall, N = 1621 | TAU, N = 73 | MIND, N = 89 | p-value2 |
|---|---|---|---|---|
|
| ||||
| Maternal age (years), Mean (±SD) | 28.0 (±5.8) | 28.1 (±6.2) | 28.0 (±5.4) | 0.92 |
| Gestational weeks at enrollment, Mean (±SD) | 17.1 (±4.2) | 19.9 (±4.1) | 14.8 (±2.7) | <0.001 |
| Maternal pre-pregnancy BMI, Mean (±SD) | 31.0 (±5.0) | 31.6 (±5.5) | 30.5 (±4.4) | 0.17 |
| Multiparous, n (%) | 88 (54) | 38 (52) | 50 (56) | 0.71 |
| Household income ($), Median [IQR] | 19,000 [9,300, 32,000] | 19,000 [10,000, 33,500] | 19,100 [8,370, 31,250] | 0.83 |
| Family poverty, Median [IQR] | 104 [55, 197] | 104 [52, 194] | 104 [56, 202] | 0.91 |
| Maternal partnership status, n (%) | >0.99 | |||
| Married, in committed relationship or engaged | 109 (68) | 49 (68) | 60 (67) | |
| Single, separated, or divorced | 52 (32) | 23 (32) | 29 (33) | |
| Maternal race/ethnicity, n (%) | 0.63 | |||
| White | 24 (15) | 11 (15) | 13 (15) | |
| Black | 63 (39) | 32 (44) | 31 (35) | |
| Asian | 4 (2.5) | 1 (14) | 3 (3.4) | |
| Pacific Islander | 1 (0.6) | 1 (14) | 0 (0) | |
| Multiracial/Other Race | 20 (12.0) | 7 (9.6) | 13 (15.0) | |
| Latino | 50 (31) | 21 (29) | 29 (33) | |
| Maternal depression (PHQ-9): baseline, Mean (±SD) | 7.1 (±4.9) | 6.9 (±4.9) | 7.3 (±5.0) | 0.63 |
| Moderate depression (baseline PHQ total >= 10), n (%) | 43 (27%) | 19 (26%) | 24 (28%) | 0.97 |
| Trial duration: post-intervention - baseline, Median [IQR] (in years) | 0.17 [0.15, 0.19] | 0.17 [0.16, 0.19] | 0.17 [0.15, 0.20] | 0.38 |
| Duration: baseline to follow-up ~1 year, Median [IQR] (in years) | 0.98 [0.92, 1.03] | 0.92 [0.88, 0.99] | 1.01 [0.96, 1.04] | <0.001 |
| Duration: baseline to follow-up ~2 years, Median [IQR] (in years) | 2.02 [1.94, 2.08] | 1.96 [1.90, 2.04] | 2.04 [2.00, 2.09] | 0.043 |
| Duration: baseline to follow-up ~3–4 years, Median [IQR] (in years) | 3.60 [3.50, 3.68] | 3.54 [3.44, 3.71] | 3.62 [3.54, 3.68] | 0.13 |
| Duration: baseline to follow-up ~5 years, Median [IQR] (in years) | 4.84 [4.59, 5.20] | 4.63 [4.51, 4.78] | 5.12 [4.77, 5.26] | <0.001 |
| Duration: baseline to follow-up ~6 years, Median [IQR] (in years) | 6.23 [5.87, 6.62] | 5.99 [5.66, 6.26] | 6.42 [6.06, 6.73] | <0.001 |
| Duration: baseline to follow-up ~ 8 years, Median [IQR] (in years) | 7.92 [7.48, 8.20] | 7.57 [7.27, 8.02] | 8.04 [7.82, 8.22] | <0.001 |
TAU = treatment as usual; MIND = mindfulness-based intervention
Mean (±SD); n (%); Median [IQR]
Welch Two Sample t-test; Pearson’s Chi-squared test; Fisher’s exact test
Upon culmination of their involvement in the original study, all women were invited to participate in a subsequent observational postnatal study for ongoing follow-up of maternal mental health and offspring development (Bush et al., 2017). The women who elected to participate in the subsequent study (N = 162; N = 89 MIND, N = 73 TAU) did not differ from the original sample on demographics or key study variables (Supplementary Table 1). Similarly, there we no differences in retention by intervention condition (Supplementary Table 2). Women in the present sample were 28 years old on average (SD = 5.8) and diverse with respect to race and ethnicity, including 39% Black, 15% White, 2.5% Asian, 0.6% Pacific Islander, and 12% Mixed race/Other race, and 31% identified as Hispanic. Most women were married or partnered (68%) and women reported a median family income of $19,000 (Range = $0-$98,000). See Table 1 for sample demographics overall and by intervention group. All procedures were approved by the Institutional Review Boards at the University of California San Francisco, California Pacific Medical Center, University of California Berkeley, and Contra Costa Regional Medical Center.
Procedures
Recruitment.
Sequential cohorts of women were recruited into the intervention to form groups of 8 to 12 women who were expected to deliver their offspring within the same two-month window. Gestational age at enrollment was an important consideration as the intervention was delivered in a group format, optimally to groups of women who were at a similar stage of pregnancy and who could complete the post-intervention assessment during pregnancy, prior to childbirth. As a result, women needed to be between 12 and 19 weeks gestation for assignment to the intervention group, which led to some difficulty recruiting enough eligible women in the same stage of pregnancy to form adequently-sized and randomly assigned intervention groups. It would have been problematic to the study design to only use half the number of recruited individuals for the treatment group, as the desired group size was 10 women. Thus, women who otherwise met study inclusion criteria but were slightly outside the gestational window (i.e., 20 to 23 weeks) were not assigned to the intervention, but were eligible to be part of the TAU group. Due to this recruitment strategy, women in the TAU group had slightly later gestational ages at enrollment (approximately 20 weeks) than the MIND group (approximately 15 weeks), but the groups did not differ on sociodemographic characteristics or depressive symptoms (see Table 1), providing well-matched groups for comparison. Please see Epel et al., 2019 for additional details of the recruitment strategy. Informed consent was obtained from all participants included in the study.
Study design.
Participants were asked to complete depression measures at baseline (pre-intervention), during their third trimester (post-intervention), and following childbirth (1, 2, 3–4, 5, and 6 years from baseline). The most recent assessment (8 years from baseline) was collected during a more acute phase of the COVID-19 pandemic by emailing all participants on a single date irrespective of the timing of their baseline assessment; surveys were completed between May and November 2020, and the majority of data from this pandemic timepoint (91%) were received by August 2020. Women were provided $25 per time point for completing baseline and post-intervention assessments. Participants in the intervention were additionally compensated $25 for attending each session to help cover their time, transportation, and childcare costs. During the postnatal follow-up study assessments, the compensation schedule was as follows: $60 each timepoint at 1 year, 2 years, 3–4 years, 5 years; $60 (if in person) or $25 (if remote) at 6 years; and $50 at 8 years. Study staff who scheduled and conducted follow-up visits were not aware of group assignment.
Mindfulness-based intervention (MIND).
The Mindful Moms Training intervention was developed from three existing, empirically-based interventions: The Mindful Motherhood Training (Vieten & Astin, 2008), Supporting Health by Integrating Nutition and Exercise (Daubenmier et al., 2016), and Mindfulness-Based Eating Awareness Training (Kristeller & Wolever, 2010). The intervention consisted of 8 weekly two-hour group sessions, two “booster” telephone sessions, and one postpartum group session with mothers and their infants. Sessions drew upon other mindfulness-based interventions, including mindfulness-based stress reduction (MBSR) and mindfulness-based cognitive therapy (MBCT), and began with mindful movement, followed by didactic presentations that focused upon stress reduction and acceptance-based coping, mindful eating, and nutrition. Women were encouraged to practice the skills outside of the group sessions with weekly homework activities. The intervention was delivered by well-trained instructors of diverse racial and ethnic backgrounds. Please see Veiten et al. (2018) for more information on the development and content of the intervention.
Treatment as usual (TAU).
TAU included any standard prenatal care and any mental health care that individuals sought on their own (and did not include any specific intervention). Therefore, women assigned to MIND and women assigned to TAU received medical care as usual. The only difference between the conditions was that the treatment group received the MIND intervention in addition to their usual care.
Any women who exhibited elevated symptom depressive severity scores were provided with a list of local mental health resources. Group assignment was masked from study principal investigators, retention and follow-up visit staff, and data analysts in both the original and postnatal follow-up studies.
Maternal depression.
Women self-reported their depressive symptoms using the PHQ-9 (Kroenke et al., 2001). At each timepoint, women completed the depression assessment on their own. Whenever possible, assessments were completed using a secure, online survey platform. If this was not possible (i.e., no smartphone, tablet, or internet access), women filled out hard copy versions of the assessment and returned them to study staff in person or by mail.
Data Analytic Plan
We began by conducting two linear mixed effects models. The first model tested the main effects of treatment and the second model tested treatment*time interactions on continuous depressive symptoms over time. Logistic regression then examined the effect of treatment on the odds of exhibiting moderate or higher depressive symptoms (PHQ-9 ≥10 as defined by Kroenke et al., 2001). Only one factor differed between MIND and TAU at enrollment: gestational weeks (women in MIND had slightly earlier gestational ages due to our enrollment strategy). In addition, duration between baseline and follow-up assessments calculated as years from baseline differed at some time points (e.g., women in MIND typically completed assessments after slightly longer durations from baseline than women in TAU). Please see Table 1 for more information. Thus, these two factors were included as covariates in the model. Models were fit using lme4 and glmmTMB in R and included fixed effects for treatment group and timepoint and a random intercept for participant.
Results
Overall, the study had excellent retention, particularly when considering the long duration of follow-up and the challenges of collecting data during the pandemic. Rates of retention across groups were: post-intervention (86%), 1 year (87%), 2 years (88%), 3–4 years (73%), 5 years (73%), 6 years (80%), and 8 years (68%). Retention rates among women assigned to MIND versus those assigned to TAU were similar, respectively: post-intervention (82%; 92%), 1 year (85%; 89%), 2 years (92%; 84%), 3–4 years (78%; 68%), 5 years (78%; 68%), 6 years (80%; 81%), 8 years (66%; 70%). Overall, at least six repeated measures of depressive symptoms were available for 77% of women. Little’s test of missingness was nonsignificant, indicating data are missing completely at random (MCAR; p = 0.12).
Table 2 reports the unadjusted depression means and standard deviations, and the percent of the sample with moderate or higher depressive symptoms overall and by condition. Post-baseline between-group effect sizes (Cohen’s d) ranged from 0.24 to 0.49 over time. Results of the linear mixed models adjusting for gestational age and and the duration between baseline and follow-up assessments are reported in Table 3. Depressive symptoms declined from baseline through 8 years for the sample regardless of intervention assignment (model 1), but such declines were generally larger in magnitude among women assigned to MIND relative to TAU (model 2).
Table 2.
Descriptive statistics on depressive symptom severity by time point
| Characteristic | Overall, N = 1621 | TAU, N = 731 | MIND, N = 891 | Cohen’s d |
|---|---|---|---|---|
|
| ||||
| Maternal depression (PHQ-9) | ||||
| Baseline | 7.1 (±4.9) | 6.9 (±4.9) | 7.3 (±5.0) | .08 |
| Post-intervention | 5.4 (±4.4) | 6.5 (±4.8) | 4.4 (±3.7) | .49 |
| 1-year follow-up | 4.5 (±4.0) | 5.1 (±4.0) | 4.1 (±4.0) | .25 |
| 2-year follow-up | 5.2 (±4.9) | 5.9 (±5.6) | 4.7 (±4.3) | .24 |
| 3–4-year follow-up | 4.4 (±4.5) | 5.0 (±5.o) | 4.0 (±4.0) | .25 |
| 5-year follow-up | 4.3 (±4.0) | 5.0 (±4.2) | 3.9 (±3.9) | .28 |
| 6-year follow-up | 3.4 (±4.9) | 4.4 (±5.7) | 2.5 (±3.9) | .39 |
| 7–8-year follow-up | 5.7 (±4.9) | 6.6 (±5.0) | 4.9 (±4.7) | .35 |
|
| ||||
| N and % with moderate depression (PHQ-9 total score >= 10) | ||||
|
| ||||
| Baseline | 43 (27%) | 19 (26%) | 24 (28%) | |
| Post-intervention | 28 (20%) | 18 (27%) | 10 (14%) | |
| 1-year follow-up | 19 (13%) | 11 (17%) | 8 (11%) | |
| 2-year follow-up | 24 (17%) | 15 (25%) | 9 (11%) | |
| 3–4-year follow-up | 15 (13%) | 10 (20%) | 5 (7.2%) | |
| 5-year follow-up | 15 (13%) | 11 (22%) | 4 (5.8%) | |
| 6-year follow-up | 16 (12%) | 9 (15%) | 7 (9.9%) | |
| 8-year follow-up | 20 (18%) | 13 (25%) | 7 (12%) | |
Mean (±SD); n (%)
Welch Two Sample t-test; TAU = treatment as usual; MIND = mindfulness-based intervention
Table 3.
Linear mixed effects models of the main effects of treatment (Model 1) and treatment*time interactions (Model 2) on continuous depressive symptoms over time
| Model 1 | Model 2 | |
|---|---|---|
|
| ||
| Coefficient | estimate (se) | estimate (se) |
|
| ||
| MIND intervention | −2.24 ***(0.63) | −0.90 (0.82) |
| Post-intervention | −1.55 *** (0.41) | −0.34 (0.60) |
| Follow-up duration: ~1 year | −2.52 *** (0.41) | −1.98 *** (0.62) |
| Follow-up duration: ~2 years | −1.59 *** (0.41) | −0.65 (0.61) |
| Follow-up duration: ~3–4 years | −2.49 *** (0.43) | −1.79 *** (0.65) |
| Follow-up duration: ~5 years | −2.47 *** (0.43) | −1.68 ** (0.67) |
| Follow-up duration: ~6 years | −3.69 *** (0.42) | −2.83 *** (0.64) |
| Follow-up duration: ~8 years | −1.31 *** (0.44) | −0.35 (0.66) |
| MIND * Post-intervention | −2.31 *** (0.82) | |
| MIND * Follow-up duration: ~1 year | −1.02 (0.88) | |
| MIND * Follow-up duration: ~2 years | −1.72 ** (0.83) | |
| MIND * Follow-up duration: ~3–4 years | −1.32 (0.87) | |
| MIND * Follow-up duration: ~5 years | −1.45 (0.92) | |
| MIND * Follow-up duration: ~6 years | −1.60 * (0.90) | |
| MIND * Follow-up duration: ~8 years | −1.79 * (0.93) | |
| Intercept | 8.29 *** (0.50) | 7.58 *** (0.57) |
| N | 162 | 162 |
|
| ||
| Observations | 1060 | 1060 |
| Marginal R2 / Conditional R2 | 0.095 / 0.459 | 0.100 / 0.463 |
p<0.1
p<0.05
p<0.01
Notes. MIND = mindfulness-based intervention. Follow-up duration indicates the amount of time between the baseline and follow-up assessments. Models adjusted for gestational age at recruitment and duration between baseline and follow-up assessments.
Results of model 2 yielded the estimated marginal means that are depicted in Figure 1. Although baseline depressive symptoms did not differ by condition, all post-baseline pairwise comparisons of mean differences in depressive symptom between women in MIND compared to women in TAU were significant (mean differences ranged from −1.9 to −3.2, all ps < .05, Figure 1), including the pandemic timepoint. Logistic regression indicated that the odds of moderate or higher depressive symptoms were greater among TAU compared to MIND women at all timepoints with the exception of the 6-year assessment (ORs = 1.2 to 2.5, Figure 2).
Figure 1.
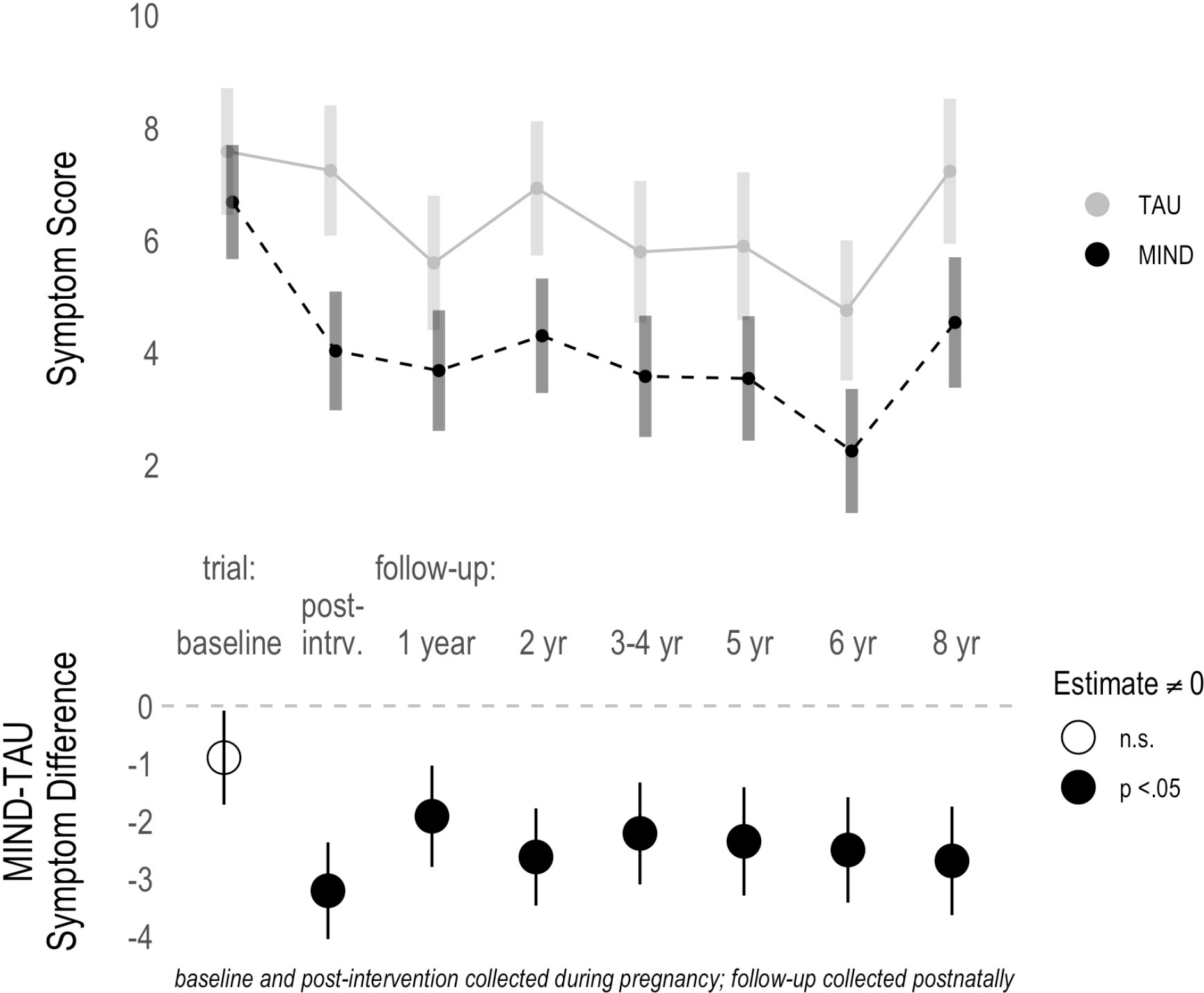
Average depressive symptom scores (upper panel) and depressive symptom difference scores (lower panel) between MIND and TAU from baseline through 8 years
TAU = treatment as usual; MIND = mindfulness-based intervention
Figure 2.
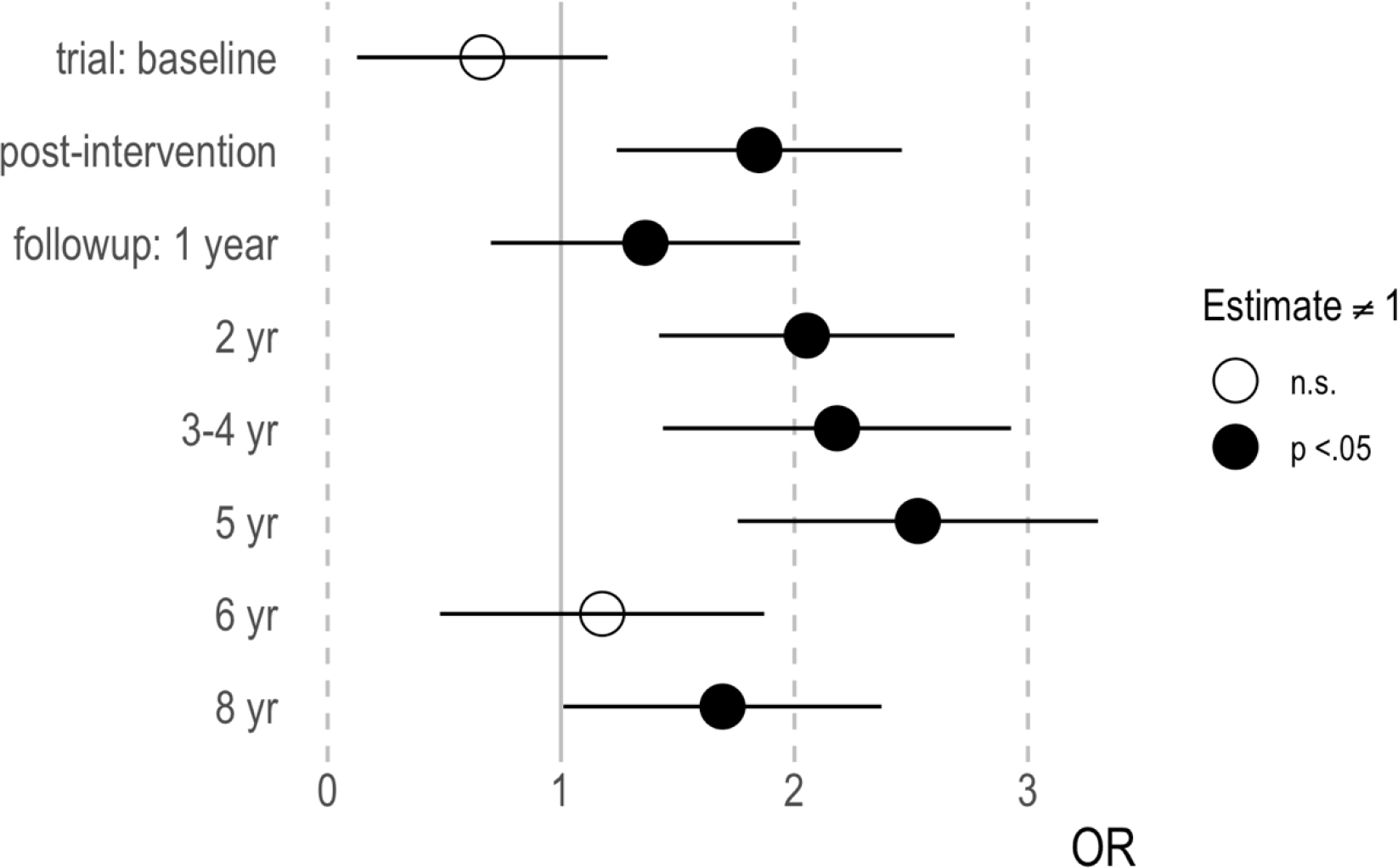
Greater odds of moderate or higher depression (PHQ-9 ≥10) among TAU compared to MIND over time
Discussion
A brief, evidence-based group mindfulness intervention during pregnancy had long-lasting, clinically meaningful effects on reducing maternal depressive symptoms. In a sample of low-income pregnant women who were racially and ethnically diverse, those who were assigned to mindfulness training reported significantly lower depressive symptoms at each annual or bi-annual assessment across an 8-year follow-up period compared to those in the control condition. Additionally, women who participated in the intervention were less likely to develop moderate or more severe symptoms across the 8-year period.
The present study adds substantially to existing research, particularly because of the long duration of these observed results. Follow-up assessments in prior studies of prenatal mindfulness-based interventions typically conclude during the first postpartum year. For example, a study of mindfulness-based cognitive therapy delivered during pregnancy found greater reductions in depressive symptoms at post-intervention and 6-months postpartum relative to treatment as usual (Dimidjian et al., 2016). Although not a mindfulness-based intervention, CenteringPregnancy bears some similarity to the present study in its group-based delivery and coverage of topics related to mental health and lifestyle (relaxation, physical activity, and nutrition), and it has been found to predict a steeper decline in depressive symptoms from baseline to 1 year compared to individual prenatal care. (Felder et al., 2017). The timing of the present study is also notable. A growing body of empirical research has documented increases in maternal mental health problems during the COVID-19 pandemic (Racine et al., 2021). Accordingly, we observed that average rates of depression symptoms across all women increased during the pandemic, regardless of group assignment. However, the benefits of the intervention persisted during the pandemic in terms of significantly lower levels of depressive symptoms among women who participated in MIND, compared to those assigned to TAU, at 8 years following the intervention.
The social and demographic characteristics of the sample are important to acknowledge. Offering accessible, scalable, culturally-relevant mindfulness interventions that are congruent with the needs of lower-income, Black, Indigenous, and people of color is essential to health equity (Garfield & Watson-Singleton, 2021; Biggers et al., 2020; Nagy et al., 2022). Most pregnancy mindfulness interventions have been examined in White populations. Findings from the current study provide preliminary evidence for their benefit in racially and/or ethnically diverse, lower income birthing populations who may experience particularly heightened levels of stress due to social inequities. To expand the reach and effectiveness of mindfulness-based programs, intervention and implementation research must attend to a broad range of issues, including cultural sensitivity, cost, scheduling, distance from public transportation, session length, and need for childcare.
It is interesting to speculate why a mindfulness intervention that was delivered during pregnancy resulted in initial and sustained reductions in depressive symptoms. Mindfulness-based interventions generally have moderate to large effects in the prevention and reduction of depressive symptoms (Hofmann et al., 2010; Strauss et al., 2014). In the short-term, mindfulness techniques may exert their salubrious effects through improved emotion regulation (Dhillon et al., 2017). As depression has been conceptualized as a disorder with its etiological roots in emotion regulation deficits, improvements in regulatory skills may reduce or protect against the development of symptoms (D’Avanzato et al., 2013). In a recent meta-analysis, mindful attention, decentering, and acceptance mediated the effects of mindfulness-based therapies on anxiety and depression (Johannsen et al., 2022). A prior analysis of women who received MIND observed immediate post-intervention improvements in mindfulness-related skills (non-reactivity, non-judgement, acceptance) that were, in turn, associated with decreases in depressive symptoms in the short-term (Vieten et al., 2018). The mindful movement practices that were incorporated into each class may have also been beneficial to mood; growing evidence suggests mindfulness-informed yoga interventions during pregnancy may reduce depression (Gong et al., 2015; Muzik et al., 2012; Newham et al., 2014). Ongoing and consistent practice of these mindfulness skills, including mindful breathing, mindful eating and mindful movement, may have preserved intervention benefits over time, however the continued use of mindfulness practices was not assessed in the present study. It is unclear the extent to which ongoing mindfulness practice contributed to sustained group differences in depression.
It has also been suggested that mindfulness-based interventions delivered during the perinatal period enhance the pregnant individual’s capacity for coping adaptively with prenatal challenges and parenting stressors that emerge during the prenatal and early infancy period, with benefits that may extend to mothers and offspring (Duncan & Bardacke, 2010). Our recently published research indicates that the MIND was associated with differences in offspring physiological and behavioral reactivity and regulation; infants born to women in MIND had more salutary profiles of biobehavioral reactivity and regulation than did infants born to women TAU (Noroña-Zhou et al., 2022). It is possible that intervention-related improvements in children’s physiological and behavioral functioning made parenting easier for women, improving parenting self-efficacy and subsequent maternal depressive symptoms (Somers et al., 2021). The sample size in the current study is limited for testing these complex mediating pathways, which are an area ripe for future research.
Results of the study should be considered in light of several limitations. First, enrollment challenges prohibited the possibility of fully randomized groups and thus, the study design was quasi-experimental. However, the intervention and control groups differed at enrollment only on weeks of gestation, and later had slight variability in the duration between baseline and follow-up assessments. Importantly, the groups were matched on sociodemographic factors and equivalent in depressive symptoms at baseline. Second, the study was not designed to treat major depressive disorder and is limited by use of a self-report measure of depressive symptoms and did not assess clinical diagnoses of depression, but the PHQ-9 has been validated against structured clinical interviews in pregnant populations (Davis et al., 2013; Sidebottom et al., 2012). Third, results may not be generalizable beyond the type of sample collected here, however the inclusion of a racially and ethnically diverse sample of low-income women provides much-needed representation of communities not typically studied in this research (Waldron et al., 2018). Fourth, we did not collect information on mental healthcare received outside of the study. It is possible that women who received MIND sought out and received additional mental health care services (i.e., participation in the mindfulness intervention increased awareness or acceptance of other psychological support) and this contributed to the sustained reductions in depressive symptoms across time. However, even if this were the case, it would still be reasonable to attribute group-based differences in depression to participation in the mindfulness-based intervention, as engagement in additional supportive services would have been a result of the intervention. Finally, the relatively small sample size and lack of information about potential mediating variables precluded the ability to test mechanistic pathways through which the intervention contributed to sustained effects.
The economic burden of perinatal mood and anxiety disorders is substantial; it is estimated that such conditions cost an estimated $14 billion for mother-child dyads in the United States from conception through 5 years postpartum (Luca et al., 2020). The results of the present study suggest that a brief, low-cost mindfulness-based intervention delivered during pregnancy may foster skills that support women’s positive mental health during and well beyond the perinatal period. In light of the consequences of depression on women and its downstream negative sequelae for offpsing (Dadi et al., 2020), our findings suggest a modest investment during pregnancy may benefit two generations.
Supplementary Material
Public Health Significance:
This study highlights the potential for long-lasting benefits of a brief psychosocial, group-based intervention during pregnancy on women’s depressive symptoms for 8 years. In light of the economic and social burden of maternal depression and its potential impact on offspring, our findings suggest a modest investment during pregnancy may support well-being across two generations.
Funding:
This work was supported by the National Heart, Lung, and Blood Institute (U01 HL097973; R01 HL116511-02), National Institutes of Health (UCSF-CTSI UL1 TR000004), the Robert Wood Johnson Health and Society Scholars Program, the Lisa and John Pritzker Family Fund, and the Lisa Stone Pritzker Family Fund. Dr. Roubinov received funding from the National Institute of Mental Health (K23MH1137019).
Footnotes
Conflict of Interest Disclosures: None
Data transparency statement:
The data reported in this manuscript were collected as part of a larger data collection. Findings from the data collection have been reported in two separate manuscripts. Epel et al. (2019) reported on depressive symptoms at baseline, post-intervention, and 6-months postpartum only. Felder et al. (2018) conducted latent profile analysis of depressive symptoms at post-intervention, 6-months postpartum, and 18-months postpartum only. The current manuscript extends the prior published manuscripts by using linear mixed models to examine depressive symptoms at each timepoint from baseline through 8 years post-intervention (1-, 2-, 3–4, 5-, 6-, and 8 years from baseline).
References
- American College of Obstetricians and Gynecologists. (2018). ACOG Committee Opinion No. 757: Screening for perinatal depression. Obstet Gynecol, 132(5), e208–e212. [DOI] [PubMed] [Google Scholar]
- Bush NR, Jones-Mason K, Coccia M, Caron Z, Alkon A, Thomas M, Coleman-Phox K, Wadhwa PD, Laraia BA, Adler NE, & Epel ES (2017). Effects of pre- and postnatal maternal stress on infant temperament and autonomic nervous system reactivity and regulation in a diverse, low-income population. Development and Psychopathology, 29(5), 1553–1571. 10.1017/S0954579417001237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dadi AF, Miller ER, Bisetegn TA, & Mwanri L (2020). Global burden of antenatal depression and its association with adverse birth outcomes: An umbrella review. BMC Public Health, 20(1), 173. 10.1186/s12889-020-8293-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daubenmier J, Moran PJ, Kristeller J, Acree M, Bacchetti P, Kemeny ME, Dallman M, Lustig RH, Grunfeld C, Nixon DF, Milush JM, Goldman V, Laraia B, Laugero KD, Woodhouse L, Epel ES, & Hecht FM (2016). Effects of a mindfulness-based weight loss intervention in adults with obesity: A randomized clinical trial. Obesity, 24(4), 794–804. 10.1002/oby.21396 [DOI] [PMC free article] [PubMed] [Google Scholar]
- D’Avanzato C, Joormann J, Siemer M, & Gotlib IH (2013). Emotion regulation in depression and anxiety: Examining diagnostic specificity and stability of strategy use. Cognitive Therapy and Research, 37(5), 968–980. [Google Scholar]
- Davis K, Pearlstein T, Stuart S, O’Hara M, & Zlotnick C (2013). Analysis of brief screening tools for the detection of postpartum depression: Comparisons of the PRAMS 6-item instrument, PHQ-9, and structured interviews. Archives of Women’s Mental Health, 16(4), 271–277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dhillon A, Sparkes E, & Duarte RV (2017). Mindfulness-based interventions during pregnancy: A systematic review and meta-analysis. Mindfulness, 8(6), 1421–1437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dimidjian S, Goodman SH, Felder JN, Gallop R, Brown AP, & Beck A (2016). Staying well during pregnancy and the postpartum: A pilot randomized trial of mindfulness-based cognitive therapy for the prevention of depressive relapse/recurrence. Journal of Consulting and Clinical Psychology, 84(2), 134–145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duncan LG, & Bardacke N (2010). Mindfulness-based childbirth and parenting education: Promoting family mindfulness during the perinatal period. Journal of Child and Family Studies, 19(2), 190–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epel E, Laraia B, Coleman-Phox K, Leung C, Vieten C, Mellin L, Kristeller JL, Thomas M, Stotland N, Bush N, Lustig RH, Dallman M, Hecht FM, & Adler N (2019). Effects of a Mindfulness-Based Intervention on Distress, Weight Gain, and Glucose Control for Pregnant Low-Income Women: A Quasi-Experimental Trial Using the ORBIT Model. International Journal of Behavioral Medicine, 26(5), 461–473. 10.1007/s12529-019-09779-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Felder JN, Epel E, Lewis JB, Cunningham SD, Tobin JN, Rising SS, Thomas M, & Ickovics JR (2017). Depressive symptoms and gestational length among pregnant adolescents: Cluster randomized control trial of CenteringPregnancy® plus group prenatal care. Journal of Consulting and Clinical Psychology, 85(6), 574–584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldberg SB, Riordan KM, Sun S, & Davidson RJ (2022). The Empirical Status of Mindfulness-Based Interventions: A Systematic Review of 44 Meta-Analyses of Randomized Controlled Trials. Perspectives on Psychological Science, 17(1), 108–130. 10.1177/1745691620968771 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gong H, Ni C, Shen X, Wu T, & Jiang C (2015). Yoga for prenatal depression: A systematic review and meta-analysis. BMC Psychiatry, 15(1), 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodman SH (2020). Intergenerational Transmission of Depression. Annual Review of Clinical Psychology, 16, 213–238. [DOI] [PubMed] [Google Scholar]
- Guintivano J, Manuck T, & Meltzer-Brody S (2018). Predictors of Postpartum Depression: A comprehensive review of the last decade of evidence. Clinical Obstetrics and Gynecology, 61(3), 591–603. 10.1097/GRF.0000000000000368 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hofmann SG, Sawyer AT, Witt AA, & Oh D (2010). The effect of mindfulness-based therapy on anxiety and depression: A meta-analytic review. Journal of Consulting and Clinical Psychology, 78(2), 169–183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johannsen M, Nissen ER, Lundorff M, & O’Toole MS (2022). Mediators of acceptance and mindfulness-based therapies for anxiety and depression: A systematic review and meta-analysis. Clinical Psychology Review, 94, 102156. [DOI] [PubMed] [Google Scholar]
- Kristeller JL, & Wolever RQ (2010). Mindfulness-Based Eating Awareness Training for Treating Binge Eating Disorder: The Conceptual Foundation. Eating Disorders, 19(1), 49–61. 10.1080/10640266.2011.533605 [DOI] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, & Williams JBW (2001). The PHQ-9. Journal of General Internal Medicine, 16(9), 606–613. 10.1046/j.1525-1497.2001.016009606.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luca DL, Margiotta C, Staatz C, Garlow E, Christensen A, & Zivin K (2020). Financial toll of untreated perinatal mood and anxiety disorders among 2017 births in the United States. American Journal of Public Health, 110(6), 888–896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lucena L, Frange C, Pinto ACA, Andersen ML, Tufik S, & Hachul H (2020). Mindfulness interventions during pregnancy: A narrative review. Journal of Integrative Medicine, 18(6), 470–477. 10.1016/j.joim.2020.07.007 [DOI] [PubMed] [Google Scholar]
- Mahaffey BL, & Lobel M (2018). Mental heath and emotional distress during pregnancy. In The new handbook of health psychology. Taylor & Francis/Routledge. [Google Scholar]
- Muzik M, Hamilton SE, Rosenblum KL, Waxler E, & Hadi Z (2012). Mindfulness yoga during pregnancy for psychiatrically at-risk women: Preliminary results from a pilot feasibility study. Complementary Therapies in Clinical Practice, 18(4), 235–240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newham JJ, Wittkowski A, Hurley J, Aplin JD, & Westwood M (2014). Effects of antenatal yoga on maternal anxiety and depression: A randomized controlled trial. Depression and Anxiety, 31(8), 631–640. [DOI] [PubMed] [Google Scholar]
- Noroña-Zhou AN, Coccia M, Epel E, Vieten C, Adler NE, Laraia B, Jones-Mason K, Alkon A, & Bush NR (2022). The Effects of a Prenatal Mindfulness Intervention on Infant Autonomic and Behavioral Reactivity and Regulation. Psychosomatic Medicine, 84(5), 525–535. 10.1097/PSY.0000000000001066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Connor E, Senger CA, Henninger ML, Coppola E, & Gaynes BN (2019). Interventions to prevent perinatal depression: Evidence report and systematic review for the US Preventive Services Task Force. Jama, 321(6), 588–601. [DOI] [PubMed] [Google Scholar]
- Racine N, Hetherington E, McArthur BA, McDonald S, Edwards S, Tough S, & Madigan S (2021). Maternal depressive and anxiety symptoms before and during the COVID-19 pandemic in Canada: A longitudinal analysis. The Lancet Psychiatry, 8(5), 405–415. 10.1016/S2215-0366(21)00074-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi Z, & MacBeth A (2017). The effectiveness of mindfulness-based interventions on maternal perinatal mental health outcomes: A systematic review. Mindfulness, 8(4), 823–847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sidebottom AC, Harrison PA, Godecker A, & Kim H (2012). Validation of the Patient Health Questionnaire (PHQ)-9 for prenatal depression screening. Archives of Women’s Mental Health, 15(5), 367–374. [DOI] [PubMed] [Google Scholar]
- Siu AL & and the US Preventive Services Task Force (USPSTF). (2016). Screening for Depression in Adults: US Preventive Services Task Force Recommendation Statement. JAMA, 315(4), 380–387. 10.1001/jama.2015.18392 [DOI] [PubMed] [Google Scholar]
- Somers JA, Curci SG, & Luecken LJ (2021). Infant vagal tone and maternal depressive symptoms: A bottom-up perspective. Journal of Clinical Child & Adolescent Psychology, 50(1), 105–117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stein A, Pearson RM, Goodman SH, Rapa E, Rahman A, McCallum M, Howard LM, & Pariante CM (2014). Effects of perinatal mental disorders on the fetus and child. The Lancet, 384(9956), 1800–1819. 10.1016/S0140-6736(14)61277-0 [DOI] [PubMed] [Google Scholar]
- Strauss C, Cavanagh K, Oliver A, & Pettman D (2014). Mindfulness-based interventions for people diagnosed with a current episode of an anxiety or depressive disorder: A meta-analysis of randomised controlled trials. PLOS One, 9(4), e96110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vieten C, & Astin J (2008). Effects of a mindfulness-based intervention during pregnancy on prenatal stress and mood: Results of a pilot study. Archives of Women’s Mental Health, 11(1), 67–74. [DOI] [PubMed] [Google Scholar]
- Vieten C, Laraia BA, Kristeller J, Adler N, Coleman-Phox K, Bush NR, Wahbeh H, Duncan LG, & Epel E (2018). The mindful moms training: Development of a mindfulness-based intervention to reduce stress and overeating during pregnancy. BMC Pregnancy and Childbirth, 18(1), 201. 10.1186/s12884-018-1757-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waldron EM, Hong S, Moskowitz JT, & Burnett-Zeigler I (2018). A systematic review of the demographic characteristics of participants in US-based randomized controlled trials of mindfulness-based interventions. Mindfulness, 9(6), 1671–1692. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data reported in this manuscript were collected as part of a larger data collection. Findings from the data collection have been reported in two separate manuscripts. Epel et al. (2019) reported on depressive symptoms at baseline, post-intervention, and 6-months postpartum only. Felder et al. (2018) conducted latent profile analysis of depressive symptoms at post-intervention, 6-months postpartum, and 18-months postpartum only. The current manuscript extends the prior published manuscripts by using linear mixed models to examine depressive symptoms at each timepoint from baseline through 8 years post-intervention (1-, 2-, 3–4, 5-, 6-, and 8 years from baseline).


