Abstract
Background:
High prevalence of very light cigarette smoking and use of alternative tobacco products (ATPs; i.e., electronic nicotine delivery systems [ENDS], cigars, and hookah) among young adult college students are causes for concern. The purpose of this study is to examine transitions in cigarette smoking (never vs. non-current vs. very light vs. heavier) among college students across 2.5 years and determine if use of ATPs is related to these transitions.
Methods:
This study used six waves of data across 2.5 years from Project M-PACT. Participants who were 18-25 years of age at baseline were included in this study (n = 4,806). Cigarette smoking state was categorized as never smoking, non-current smoking [0 cigarettes smoked per day (cpd) in past month], very light smoking (<=5 cpd in past month), and heavier smoking (> 5 in past month). Multi-state Markov models were used to examine temporal transitions in the four smoking states and examine the association of time-varying current ATP use with transitions in smoking states.
Results:
The probabilities of remaining in a smoking state decreased over time. The time-varying current ATP use was significantly related to increased odds of transitioning from never smoking to non-current smoking, from never smoking to very light smoking, and from non-current to very light smoking.
Conclusions:
Findings highlight the need to prevent ATP use among college students and in turn inhibit initiation and escalation of cigarette smoking.
Introduction
Tobacco use during young adulthood is dynamic and can fluctuate in both frequency and intensity of use (Hair et al., 2017; Henwood et al., 2018). Although most young adults do not smoke cigarettes, they may transition into different smoking states over time (Caldeira et al., 2012; Kasza et al., 2018; Robertson et al., 2016), such as from never smoking to very light smoking (initiation), or very light smoking to heavy smoking (escalation), or very light smoking to former smoking (desisting or quitting). However, limited studies examine transitions in cigarette smoking and evidence regarding the probability of transitions during young adulthood is mixed. For example, some longitudinal studies have shown that low stable cigarette consumption is the most common smoking trajectory during young adulthood, and a substantial percentage of light and intermittent smokers maintain a low smoking level across a couple of years (Caldeira et al., 2012; Klein et al., 2013). Other studies indicate that only a very small portion of young adult smokers maintain stable low cigarette consumption patterns over time (Hukkinen et al., 2009; White et al., 2009). Moreover, the prevalence of non-cigarette alternative tobacco product (ATP) use is particularly high among young adults (Cornelius et al., 2022), particularly college students, but the role of ATP use on transitions of cigarette smoking during young adulthood and the college years is underexplored. This study aimed to extend existing research by investigating transitions in cigarette smoking across a 2.5-year period among young adult college students and determining the role of ATP use in these transitions.
Young adulthood is associated with an increased risk of using multiple tobacco products, which is more prevalent during this developmental period than single product use (Loukas et al., 2016). Use of ATPs, such as electronic nicotine delivery systems [ENDS], cigars, hookah, and smokeless tobacco, are appealing to young adults and college students, in part because some of these products are marketed as safer alternatives to cigarettes (Pokhrel et al., 2015). However, young adult tobacco users tend to use ATPs to socialize with others, enjoy their flavors, or soothe negative emotions rather than to quit or reduce cigarette smoking (Doran & Brikmanis, 2016; Kostygina et al., 2016). Evidence indicates that the use of ATPs, especially use of multiple products increases nicotine intake and the risk of nicotine dependence, which may contribute to cigarette smoking several years into the future (Martinez et al., 2020; Niaura et al., 2020; Richardson et al., 2014). Although prior research indicates that individual ATP use is independently associated with elevated risk for future cigarette initiation, current smoking, or progression to heavier smoking (Delnevo et al., 2016; Glasser et al., 2019; Loukas et al., 2022; Soneji et al., 2015; Wolfson et al., 2015), there is limited research on the role of multiple product use on college students’ longitudinal transitions in cigarette smoking, such as from initial experimentation with cigarettes to very light smoking, to the development of heavier smoking, and/or to cessation.
Young adulthood is a critical developmental period for establishing smoking behavior. Recent data indicate that young adults have a significantly higher risk for cigarette onset than any other age group (Perry et al., 2018). Data from the National Survey of Drug Use and Health also show that among cigarette smokers those who initiated any cigarette smoking or became regular smokers during young adulthood increased substantially from 2002 to 2018 (Barrington-Trimis et al., 2020). Moreover, although the rates of cigarette initiation declined from 2009 to 2015 for some young adults (Cantrell et al., 2018), the prevalence of non-daily smoking and daily light smoking from 2005 to 2015 has increased (Jamal et al., 2016). Very light smoking, defined as no more than 5 cigarettes per day (cpd) in the past 30 days, is the predominant form of tobacco use among young adult smokers, particularly college students (Li et al., 2018).
Although college students are less likely to smoke heavily than their non-college-attending peers, they are more likely to maintain light or intermittent smoking patterns over time (Klein et al., 2013; White et al., 2009). For example, Caldeira et al. (2012) found that although most college student participants (n = 1,253) were stable non-smokers over a 4-year period, about 20% either maintained very light smoking or increased their smoking frequency, and only 3.2% decreased their smoking frequency during the college years. These findings are troubling given that smoking, even at very light levels, is associated with nicotine dependence and adverse health outcomes such as cardiovascular and pulmonary diseases and internalizing problems (i.e., depression and anxiety) (Bjartveit & Tverdal, 2005; Selya et al., 2016). Very light smoking has also been associated with increased risk for use of ATPs (Li et al., 2018). Yet, we know relatively little about the role of ATP use in longitudinal transitions into and out of very light smoking in the contemporary tobacco landscape.
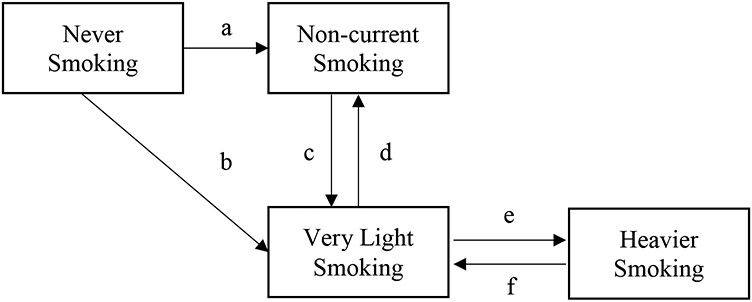
The purpose of the present study was to examine longitudinal transitions in cigarette smoking among college students across a 2.5-year period and determine the role of current ATP use in these transitions. We used Multistate Markov modelling to assess transitions in four states: never smoking (have never used cigarettes even one or two puffs), non-current/past 30-day smoking (have used cigarettes but not used in the past 30 days), very light smoking (≤ 5 cpd in the past 30 days), and heavier smoking (> 5 cpd), and to assess the effect of ATP use on seven transitions (see Figure 1). We addressed two research questions: 1) How do smoking states change across a 2.5-year period? 2) How does ATP use influence transitions in smoking states? We expected that most college students would be stable non-smokers (including never smokers and non-current smokers), but there would be transitions among smoking states, such as from non-current smoking to very light smoking and vice versa. Moreover, we expected that ATP use would elevate the risk for transitioning from non-smoking to smoking (either very light or heavier smoking) and decrease the probability of desisting or quitting smoking.
Figure 1.
Structure of allowed transitions for the multi-state Markov model.
Methods
Participants
Participants (n = 4,806) were 18-25 year old college students participating in the first six semi-annual waves of the Marketing and Promotions Across Colleges in Texas project (Project M-PACT), a rapid response, web-based project assessing tobacco use behaviors (Loukas et al., 2016). The average age of the participants was 20.1 years (SD = 1.83), with 62.1% between 18 and 20 years of age when recruited. More than half (64%) the participants were female; and 35.2% were non-Hispanic white, 31.1% were Hispanic/Latino, 8.0% were African-American/Black, 18.0% were Asian, and 7.6% reported another race/ethnicity or two or more races/ethnicities. Most (93.3%) of the participants were enrolled in a four-year college at recruitment compared with a two-year college.
Procedures
We recruited participants from 24 colleges in the five counties surrounding four target cities in Texas (Austin, Dallas/Fort Worth, Houston, and San Antonio). Eligible participants were required to be 18-29 years of age and full- or part-time degree- or certificate-seeking undergraduate students attending a participating four-year college or a vocational/technical program at a two-year college. Of the 13,714 eligible students, 5,482 (40%) provided consent and completed the baseline (Wave 1) survey between Nov 2014 and Feb 2015. We collected five additional waves every six months until spring 2017 (Wave 6). At each wave, we compensated participants with an e-gift card (raised from $10 at Wave 1-2 to $20 at Wave 3-6) and entered them into a drawing to win one of twenty $50 e-gift cards. Retention rates across the five follow-up waves ranged from 78% (Wave 5) to 81% (Wave 4). Additional procedural details and inclusion criteria of Project M-PACT have been reported elsewhere (Authors, 2016). The university leading the project provided human subjects approval for the study protocol and all participants provided consent.
For the purposes of this study, we only included students who were 18-25 years of age at baseline because this age range is typically considered to capture young adulthood (Elders et al., 1994) and because transitions in smoking and initiation are unlikely to occur after the age of 26 (Hair et al., 2017). In addition, the analysis only included students who provided valid answers to the smoking state questions at baseline and at least one follow-up survey. These criteria resulted in a sample of 4,806 participants. We conducted separate logistic regression analyses to assess if participants included in the present study differed from those excluded (n = 676) on the socio-demographic covariates (sex, age group, college type, and race/ethnicity) and on Wave 1 current tobacco use. The 676 excluded participants were significantly more likely to be non-Hispanic White (Odds Ratio [OR] = 1.50, 95% confidence interval [CI]: 1.26 – 1.74) and to be attending a 2-year college (OR = 2.31, 95% CI: 1.80 – 2.94). Moreover, excluded participants had higher odds of being tobacco users than those who were included in analyses (Odds Ratio = 1.95, 95% CI: 1.66 - 2.30).
Measures
Smoking States
We used three questions to assess smoking states. One question assessed lifetime/ever cigarette smoking. Two other questions, one regarding frequency of cigarette use and the other regarding cigarette quantity per day in the past 30 days, assessed current smoking: a) “on how many of the past 30 days did you smoke cigarettes?” and b) “on the days you smoked, how many cigarettes did you usually smoke each day?”. Based on prior research (Husten, 2009; Pierce et al., 2009), the total monthly number of cigarettes smoked was obtained by multiplying current frequency and current quantity; the average cpd was computed as total monthly cigarettes divided by 30. We created four categories of smoking states using responses from the three previous questions (ever use, frequency of use, quantity of use): 1 = never smoking (have never used cigarettes even one or two puffs), 2 = non-current smoking (ever used cigarettes, but smoked 0 cpd in the past 30 days), 3 = very light smoking (≤ 5 cpd in the past 30 days) and 4 = heavier smoking (> 5 cpd in the past 30 days).
Current Alternative Tobacco Products (ATP) Use
Current (past 30-day) use of ATPs, including ENDS, cigars, hookah and smokeless tobacco, was assessed with one item for each product, adapted from the Youth Tobacco Survey (Starr et al., 2005) and the Population Assessment of Tobacco and Health (PATH) Survey (National Institutes of Health, 2015). The current ENDS use question asked: “During the past 30 days, have you used any ENDS product…?” For all other products (i.e., cigar products, hookah, and smokeless tobacco), the question asked: “During the past 30 days, how many did you use/smoke [product]”? Students who responded 1 or more days to any of these items were considered as current ATP users. The time-varying current ATP use (0 = did not use any ATP in the past 30 days at Wave 1, 1 = used at least one ATP in the past 30 days at Wave 1) was the main exposure variable.
Socio-demographic Covariates
Sex, age group, race/ethnicity and college type (two-year or four-year), all assessed at Wave 1, were included as covariates in the model fitting process. Age was analyzed as two groups, younger (18-20 years) versus older (21-25 years) and race/ethnicity, a dichotomous variable, was created to indicate whether a participant was non-Hispanic White or a racial/ethnic minority. The reference groups were being male, older, ethnic minority and two-year college student.
Data Analysis
Transitions into and out of the four smoking states (never smoking, non-current smoking, very light smoking, and heavier smoking) over the 2.5-year period and the role of ATP use in these transitions was assessed with Multi-state Markov models. Markov models represent a process in which individuals move through a series of states in continuous time (Kaplan, 2008). The model assumes that the measure of a categorical variable is reliable and that all parameters can be obtained directly from manifest categorical responses, and it allows transitions to occur at any time along observed time intervals (Kaplan, 2008; Mhoon et al., 2010). The model uses all valid data from participants with two or more observations to estimate the transition intensity matrix, which defines the possible transitions between states. Effect of time-varying current ATP use was examined on six transitions (see Figure 1): a) from never smoking to non-current smoking; b) from never smoking to very light smoking; c) from non-current smoking to very light smoking; d) from very light smoking to non-current smoking; e) from very light smoking to heavier smoking; and f) from heavier smoking to very light smoking. Transitions from any smoking state back to never smoking were not allowed, because once someone uses cigarettes, there is no way to transition back to never use. The direct transitions from never smoking to heavier smoking; from non-current smoking to heavier smoking; and from heavier smoking to non-current smoking were not examined because changes of these two types were extremely rare (< 1% of all transitions) and resulted in inestimable parameter estimates in models that included covariates (Jackson, 2011, 2018).
We used R 3.3 with package msm (Jackson, 2011, 2018) to conduct all analyses and the optimal model was determined with log-likelihood ratio goodness-of-fit tests. A model without covariates was first fit to the data, followed by separate models examining the effect of ATP use at Wave 1 with one socio-demographic covariates entered at a time (sex, age group, race/ethnicity, college type) (Mhoon et al., 2010). Transition probabilities were estimated to show the probability that a specified state of interest was in the same or a different state at a defined timepoint. In this study, the defined time had 6-month increments (i.e., 0.5-year, 1 year, 1.5, 2, and 2.5 years).
Results
At baseline, 54.2% of the 4,806 participants were in the never smoking state, 26.4% were in the non-current smoking state, 17.7% were in the very light smoking state, and 1.7% were in the heavier smoking state. More than 94% of very light smokers are non-daily smokers Moreover, 28.7% of participants were current ATP users at baseline, 17.2% were current ENDS users, 16.7% were current hookah users, 9.7% were current cigar users, and 3.0% were current smokeless tobacco users. The prevalence of ATP use was 10.8% among never smokers, 36.5% among non-current smokers, 67.8% among very light smokers and 71.3% among heaver smokers, at baseline. Participants were more likely to use ATPs if they were in a heavier smoking state (OR = 3.93, 95% CI = [3.60, 4.30]), i.e., the odds of use ATP increased by 3.93 for each progression to a new state.
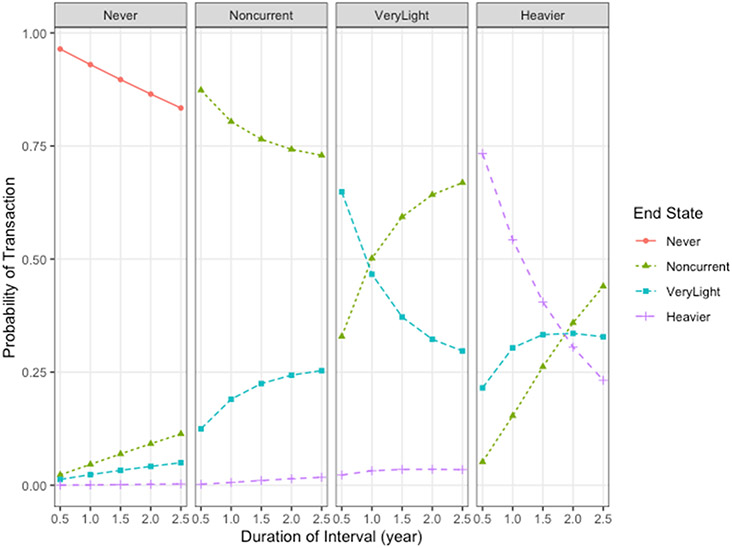
We first examined the transition probabilities of smoking states across a 2.5-year period using a Multi-state Markov model without covariates. As shown in Table 1 and Figure 1, the probabilities of remaining in one of the four smoking states decreased over time. However, never smoking and non-current smoking patterns were fairly stable. Across any 6-month period, the probability of remaining in the never smoking state was 96.4%, and the probability of remaining in the non-current smoking state was 87.3%. Even over the 2.5-year interval, the probability of remaining in the same state was 83.4% for the never smoking state and about 72.9% for the non-current smoking state. The probabilities of remaining in a smoking state decreased more for heavier smoking than for very light smoking. Across a 6-month interval, the probability of maintaining a very light smoking state was 64.9% and a heavier smoking state was 73.3%, but the probabilities of maintaining in the same state decreased to 29.7% for very light smoking, and 23.2% for heavier smoking, respectively, within a 2.5-year period.
Table 1.
Transition probabilities across multiple time intervals.
| End State | |||||
|---|---|---|---|---|---|
| Time Interval | Start State | Never | Non-current | Very Light | Heavier |
| 0.5 year | Never | 0.964[0.961 to 0.968] | 0.023[0.02 to 0.026] | 0.013[0.011 to 0.015] | -- |
| 0.5 year | Non-current | -- | 0.873[0.865 to 0.881] | 0.125[0.117 to 0.133] | 0.002[0.002 to 0.003] |
| 0.5 year | Very Light | -- | 0.329[0.313 to 0.346] | 0.649[0.632 to 0.665] | 0.023[0.019 to 0.028] |
| 0.5 year | Heavier | -- | 0.052[0.042 to 0.062] | 0.215[0.182 to 0.253] | 0.733[0.686 to 0.774] |
| 1 year | Never | 0.93[0.923 to 0.936] | 0.046[0.041 to 0.052] | 0.023[0.02 to 0.027] | 0.001[0.001 to 0.001] |
| 1 year | Non-current | -- | 0.804[0.793 to 0.815] | 0.19[0.179 to 0.201] | 0.006[0.005 to 0.008] |
| 1 year | Very Light | -- | 0.502[0.483 to 0.521] | 0.466[0.447 to 0.484] | 0.032[0.026 to 0.039] |
| 1 year | Heavier | -- | 0.154[0.13 to 0.183] | 0.304[0.26 to 0.346] | 0.543[0.471 to 0.606] |
| 1.5 years | Never | 0.897[0.886 to 0.906] | 0.069[0.062 to 0.077] | 0.033[0.029 to 0.038] | 0.001[0.001 to 0.002] |
| 1.5 years | Non-current | -- | 0.765[0.752 to 0.779] | 0.225[0.212 to 0.238] | 0.01[0.008 to 0.013] |
| 1.5 years | Very Light | -- | 0.593[0.574 to 0.611] | 0.372[0.354 to 0.389] | 0.035[0.028 to 0.043] |
| 1.5 years | Heavier | -- | 0.262[0.224 to 0.299] | 0.333[0.295 to 0.367] | 0.405[0.337 to 0.478] |
| 2 years | Never | 0.865[0.852 to 0.875] | 0.092[0.083 to 0.101] | 0.042[0.037 to 0.047] | 0.002[0.002 to 0.003] |
| 2 years | Non-current | -- | 0.742[0.728 to 0.756] | 0.243[0.23 to 0.257] | 0.014[0.011 to 0.017] |
| 2 years | Very Light | -- | 0.642[0.624 to 0.66] | 0.323[0.306 to 0.339] | 0.035[0.028 to 0.043] |
| 2 years | Heavier | -- | 0.359[0.312 to 0.406] | 0.336[0.304 to 0.364] | 0.305[0.236 to 0.38] |
| 2.5 years | Never | 0.834[0.818 to 0.848] | 0.113[0.103 to 0.125] | 0.05[0.045 to 0.056] | 0.003[0.002 to 0.004] |
| 2.5 years | Non-current | -- | 0.729[0.714 to 0.745] | 0.253[0.239 to 0.268] | 0.017[0.014 to 0.021] |
| 2.5 years | Very Light | -- | 0.669[0.65 to 0.688] | 0.297[0.281 to 0.314] | 0.034[0.027 to 0.042] |
| 2.5 years | Heavier | -- | 0.440[0.391 to 0.49] | 0.328[0.305 to 0.35] | 0.232[0.168 to 0.298] |
The probabilities of switching between smoking states increased across time, but these transitions reflected both increasing and decreasing cigarette use (see Table 1). The probabilities of transitioning out of the never smoking state and heavier smoking to noncurrent smoking tended to increase across time (see Table 1). However, the increasing rate of transitions into and out of very light smoking diminished over time. For example, the probability of transitioning from non-current smoking to very light smoking increased from 12.5% across a 6-month interval to about 22.5% across a 1.5-year interval, then to 25.3% at the end of the 2.5-year interval. The probability of transitioning from heavier smoking to very light smoking increased from 21.5% across a 6-month interval to 30.4% across a 1-year interval, and then the probability of this transition remained near 30% over a period longer than 1 year. In addition, the probability of transitioning from very light smoking to noncurrent smoking increased markedly from 32.9% across a 6-month interval to 59.3% across a 1.5-year interval, then increased to 72.9% at the end of the 2.5-year interval. Compared with other transitions, the probability of transitioning from very light smoking to heavier smoking was relatively low (2% across 6 months and 3% over a longer period).
Next, we assessed model fit with each socio-demographic and time-varying current ATP use covariate in successive Markov models. The log-likelihood ratio goodness-of-fit tests revealed that the model including sex and current ATP use as covariates fit the data better than models with an individual covariate or with an alternative combination of covariates (p < 0.01) (see Supplementary Table 1). Results from the model with ATP use and sex (see Table 2) indicated that current ATP use associated with increased odds of making a transition from never smoking to non-current smoking, from never smoking to very light smoking, and from non-current smoking to very light smoking. ATP use was not associated with transitioning between very light smoking and heavier smoking and the odds of transitioning from very light smoking to non-current smoking. The examination of sex in the model indicated that most transitions between smoking states did not differ for males and females. However, compared to males, females were less likely to transition from non-current smoking to very light smoking (HR = 0.78, 95% CI: 0.67 – 0.90).
Table 2.
Hazard ratios [95% CI] depicting the effect of time-varying alternative tobacco product (ATP) use on overall transition intensities.
| End State | |||
|---|---|---|---|
| Start State | Non-current | Very Light | Heavier |
| Never | 4.80 [3.46-6.66] | 5.15 [3.34-7.94] | - |
| Non-current | - | 2.37 [2.05-2.75] | - |
| Very Light | 1.01 [0.89-1.16] | - | 1.20 [0.77-1.87] |
| Heavier | - | 1.10 [0.72-1.70] | - |
Discussion
The present study examined transitions in cigarette smoking and the association between ATP and these transitions in a sample of young adult college students. Consistent with prior research (Caldeira et al., 2012; Hair et al., 2017), most participants were never smokers at baseline, and never smoking was highly stable across time. However, among current/past 30-day cigarette users, very light smoking was more common than heavier smoking. Further findings indicated that although very light smoking was less stable than never smoking and non-current smoking among young adults, the probability of maintaining very light smoking after 2.5 years was slightly higher than maintaining heavier smoking. Moreover, findings confirmed that although transitions out of very light smoking after one year were prevalent, some college students maintained very light cigarette smoking over the 2.5-year period, and there were substantial transitions into very light smoking from non-current smoking and from heavier smoking. Finally, findings showed that ATP use increased the odds of transitioning from never and non-current smoking to very light smoking but did not impede transitioning from very light smoking to non-current smoking. Taken together, these findings indicate that smoking is dynamic during young adulthood and underscore the need for prevention and intervention efforts targeting college students focused on all types of tobacco products. Further, given that very light smoking is associated with adverse health outcomes, efforts should focus on preventing ATP use among young adults, which may reduce the risk of very light smoking.
Our findings indicate that although tobacco control efforts may have been successful in reducing the overall prevalence of cigarette smoking among young adults (Cantrell et al., 2018), they may not have been as effective in reducing smoking initiation and very light smoking behavior among young adults (Villanti et al., 2019). Consistent with expectations, we found that the probability of transitioning out of never smoking, to non-current smoking or to very light smoking, over the 2.5-year period was substantial. This finding corroborates research showing that many people start smoking during young adulthood (Barrington-Trimis et al., 2020). In fact, recent evidence indicates that the onset of cigarette smoking may now be even more common among young adults than adolescents and interventions to prevent cigarette initiation during young adulthood are needed (Barrington-Trimis et al., 2020; Perry et al., 2018).
We also found that very light smoking was more common among our participants than heavier smoking and there were relatively few transitions from very light to heavier smoking. These findings confirmed that very light smoking is a predominant pattern, particularly among young adults (Pierce et al., 2009; Substance Abuse Mental Health Services Administration, 2012). Although there are misperceptions regarding the health effects associated with this pattern of smoking (Amrock & Weitzman, 2015), evidence indicates that very light smoking increases the risk for nicotine exposure, nicotine dependence, and adverse health outcomes (Bjartveit & Tverdal, 2005; Selya et al., 2016). Given that very light smoking may lead to heavier smoking as young adults transition into adulthood (Robertson et al., 2016; White et al., 2009), tobacco control efforts that assist young adults in transitioning from very light smoking to non-current smoking are needed.
Further findings indicated that the probability of remaining in one of the four states decreased over time and the probabilities of transitioning between states increased across time. These findings underscored the dynamic nature of cigarette smoking during young adulthood. As expected and consistent with prior research (Caldeira et al., 2012; Hair et al., 2017), although smoking patterns remained stable across time, the probabilities of remaining in a smoking state decreased across time, with the decrease more pronounced for heavier smoking than for very light smoking.
Despite the dynamic nature of smoking during young adulthood, there is also evidence for solidification of certain smoking patterns. For example, our findings indicated that as time passed, the increasing rate of transitioning out of very light smoking diminished. These findings are consistent with research showing that although young adults transition across different smoking states, they tend to establish stable smoking patterns by the end of young adulthood (Hair et al., 2017; Rath et al., 2012). Hence tobacco prevention and intervention efforts need to be conducted earlier rather than later in young adulthood to prevent solidification, particularly of very light smoking.
Other findings indicated that ATP use elevated risk for cigarette initiation (from never smoking to non-current smoking or to very light smoking) and escalation (from non-current smoking to very light smoking) (Barrington-Trimis et al., 2016; Doran et al., 2015; Primack et al., 2018; Primack et al., 2015; Soneji et al., 2017; Soneji et al., 2015). These findings corroborate research showing that use of ATPs may elevate risk for concurrent and subsequent use of traditional cigarettes (Delnevo et al., 2016; Meier et al., 2015; Sutfin et al., 2012). Some ATPs, such as ENDS and hookah, have gained popularity rapidly among young adults in recent years (Gilreath et al., 2016; Schulenberg et al., 2020). Many young adults, especially very light smokers, use ATPs for coping, to improve affect, or for socialization purposes (Doran & Brikmanis, 2016), instead of use for cutting down on or quitting cigarettes (Doran & Brikmanis, 2016). Together, these strategies contribute to increased risk for nicotine dependence and the progression of cigarette smoking several years into the future (Doran et al., 2015). Consistent with previous studies, our results also showed that sex was not related to transitions in smoking states (Verplaetse et al., 2019; Yi et al., 2017), except that female young adults were less likely to transition from non-current smoking to very light smoking after controlling for ATP use.
The present study has some limitations. First, although we used current conventions for categorizing current smokers, heavier smoking (using more than 5 cigarettes per day) is very rare among young adults and was also rare in our sample. Only 1.7% of students were heavier smokers at the start of the study and there were relatively few transitions from very light to heavier smoking. Second, we examined these transitions in smoking with a 6-month interval across a 2.5-year period, which covered only part of young adulthood. While the interval between waves is shorter than many longitudinal surveys, it may well miss some of the change that is occurring. To fully depict the dynamics of smoking patterns across young adulthood, it may be important to track transitions into and out of smoking states in a shorter interval across a longer period. Third, our survey measured self-reported smoking behavior the month prior to each study wave (i.e., one sixth of months between waves). It is possible that important variance in use was not captured by survey data and our model. For example, we did not account for the potential effects of systematic variations in college student schedules (such as weekends and holiday breaks). Furthermore, the study sample consisted of college/university students from Texas, thus findings may not be representative of other populations of young adults. Last, data used in this study were largely collected before JUUL and comparable devices entered the market, which could have mitigated the likelihood of ENDS in particular motivating transitions from never to active smoking states. Additional research with other samples is needed to replicate study findings.
The current study extends existing research by showing that cigarette smoking is dynamic during young adulthood and by demonstrating that ATP use elevates risk for transitioning into very light smoking and impedes desistance or quitting very light smoking. The dynamic nature of smoking provides opportunities for intervention efforts. In particular, there is a need to prevent the initiation of very light smoking among young adult college students and to intervene to reduce use. Interventions should target all types of tobacco products but should underscore the role of ATP use in initiating and maintaining cigarette use, even at very light levels.
Supplementary Material
Figure 2.
Transition probabilities across two and half years (with a six-month interval).
Note. Each panel represents a different starting smoking state, and the series represent the probability of being in each of the four smoking states at a certain time conditioned on that starting smoking state.
References
- Amrock SM, & Weitzman M (2015). Adolescents' perceptions of light and intermittent smoking in the United States. Pediatrics, 135(2), 246–254. 10.1542/peds.2014-2502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barrington-Trimis JL, Braymiller JL, Unger JB, McConnell R, Stokes A, Leventhal AM, Sargent JD, Samet JM, & Goodwin RD (2020). Trends in the age of cigarette smoking initiation among young adults in the US from 2002 to 2018. JAMA Netw Open, 3(10), e2019022. 10.1001/jamanetworkopen.2020.19022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barrington-Trimis JL, Urman R, Berhane K, Unger JB, Cruz TB, Pentz MA, Samet JM, Leventhal AM, & McConnell R (2016). E-cigarettes and future cigarette use. Pediatrics, 138(1), e20160379. 10.1542/peds.2016-0379 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bjartveit K, & Tverdal A (2005). Health consequences of smoking 1-4 cigarettes per day. Tob Control, 14(5), 315–320. 10.1136/tc.2005.011932 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caldeira KM, O'Grady KE, Garnier-Dykstra LM, Vincent KB, Pickworth WB, & Arria AM (2012). Cigarette smoking among college students: longitudinal trajectories and health outcomes. Nicotine Tob Res, 14(7), 777–785. 10.1093/ntr/nts131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cantrell J, Bennett M, Mowery P, Xiao H, Rath J, Hair E, & Vallone D (2018). Patterns in first and daily cigarette initiation among youth and young adults from 2002 to 2015. PLoS One, 13(8), e0200827. 10.1371/journal.pone.0200827 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cornelius ME, Loretan CG, Wang TW, Jamal A, & Homa DM (2022). Tobacco product use among adults - United States, 2020. MMWR: Morbidity and Mortality Weekly Report, 71(11), 397–405. 10.15585/mmwr.mm7111a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Delnevo CD, Villanti AC, Wackowski OA, Gundersen DA, & Giovenco DP (2016). The influence of menthol, e-cigarettes and other tobacco products on young adults’ self-reported changes in past year smoking. Tobacco Control, 25(5), 571–574. 10.1136/tobaccocontrol-2015-052325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doran N, & Brikmanis K (2016). Expectancies for and use of e-cigarettes and hookah among young adult non-daily smokers. Addictive Behaviors, 60, 154–159. 10.1016/j.addbeh.2016.04.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doran N, Godfrey KM, & Myers MG (2015). Hookah use predicts cigarette smoking progression among college smokers. Nicotine & Tobacco Research, 17(11), 1347–1353. 10.1093/ntr/ntu343 [DOI] [PubMed] [Google Scholar]
- Elders MJ, Perry CL, Eriksen MP, & Giovino GA (1994). The report of the Surgeon General: preventing tobacco use among young people. Am J Public Health, 84(4), 543–547. 10.2105/ajph.84.4.543 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilreath TD, Leventhal A, Barrington-Trimis JL, Unger JB, Cruz TB, Berhane K, Huh J, Urman R, Wang K, Howland S, Pentz MA, Chou CP, & McConnell R (2016). Patterns of alternative tobacco product use: emergence of hookah and e-cigarettes as preferred products amongst youth. Journal of Adolescent Health, 58(2), 181–185. 10.1016/j.jadohealth.2015.10.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glasser A, Abudayyeh H, Cantrell J, & Niaura R (2019). Patterns of e-cigarette use among youth and young adults: review of the impact of e-cigarettes on cigarette smoking. Nicotine Tobacco & Research, 21(10), 1320–1330. 10.1093/ntr/nty103 [DOI] [PubMed] [Google Scholar]
- Hair E, Bennett M, Williams V, Johnson A, Rath J, Cantrell J, Villanti A, Enders C, & Vallone D (2017). Progression to established patterns of cigarette smoking among young adults. Drug Alcohol Depend, 177, 77–83. 10.1016/j.drugalcdep.2017.03.040 [DOI] [PubMed] [Google Scholar]
- Henwood BF, Lahey J, Rhoades H, Winetrobe H, & Wenzel SL (2018). Examining the health status of homeless adults entering permanent supportive housing. Journal of Public Health, 40(2), 415–418. 10.1093/pubmed/fdx069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hukkinen M, Kaprio J, Broms U, Koskenvuo M, & Korhonen T (2009). Characteristics and consistency of light smoking: long-term follow-up among Finnish adults. Nicotine & Tobacco Research, 11(7), 797–805. 10.1093/ntr/ntp065 [DOI] [PubMed] [Google Scholar]
- Husten CG (2009). How should we define light or intermittent smoking? Does it matter? Nicotine & Tobacco Research, 11(2), 111–121. 10.1093/ntr/ntp010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson C (2011). Multi-state models for panel data: the msm package for R. Journal of Statistical Software, 38(8), 1–29. 10.18637/jss.v038.i08 [DOI] [Google Scholar]
- Jackson C (2018). Package ‘msm’. [Google Scholar]
- Jamal A, King BA, Neff LJ, Whitmill J, Babb SD, & Graffunder CM (2016). Current cigarette smoking among adults - United States, 2005-2015. MMWR Morb Mortal Wkly Rep, 65(44), 1205–1211. 10.15585/mmwr.mm6544a2 [DOI] [PubMed] [Google Scholar]
- Kaplan D (2008). An overview of Markov chain methods for the study of stage-sequential developmental processes. Developmental Psychology, 44(2), 457–467. 10.1037/0012-1649.44.2.457 [DOI] [PubMed] [Google Scholar]
- Kasza KA, Borek N, Conway KP, Goniewicz ML, Stanton CA, Sharma E, Fong GT, Abrams DB, Coleman B, Schneller LM, Lambert EY, Pearson JL, Bansal-Travers M, Murphy I, Cheng YC, Donaldson EA, Feirman SP, Gravely S, Elton-Marshall T, Trinidad DR, Gundersen DA, Niaura RS, Cummings KM, Compton WM, & Hyland AJ (2018). Transitions in tobacco product use by U.S. adults between 2013(-)2014 and 2014(-)2015: findings from the PATH study wave 1 and wave 2. Int J Environ Res Public Health, 15(11), 1–14. 10.3390/ijerph15112515 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klein EG, Bernat DH, Lenk KM, & Forster JL (2013). Nondaily smoking patterns in young adulthood. Addictive Behaviors, 38(7), 2267–2272. 10.1016/j.addbeh.2013.03.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kostygina G, Glantz SA, & Ling PM (2016). Tobacco industry use of flavours to recruit new users of little cigars and cigarillos. Tob Control, 25(1), 66–74. 10.1136/tobaccocontrol-2014-051830 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li X, Loukas A, & Perry CL (2018). Very light smoking and alternative tobacco use among college students. Addictive Behaviors, 81, 22–25. 10.1016/j.addbeh.2018.01.038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loukas A, Chow S, Pasch KE, Li X, Hinds I, Josephine T, Marti CN, Harrell MB, Creamer MR, & Perry CL (2016). College students' polytobacco use, cigarette cessation, and dependence. American Journal of Health Behavior, 40(4), 514–522. 10.5993/AJHB.40.4.13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loukas A, Marti CN, & Harrell MB (2022). Electronic nicotine delivery systems use predicts transitions in cigarette smoking among young adults. Drug and Alcohol Dependence, 231, 109251. 10.1016/j.drugalcdep.2021.109251 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martinez U, Martinez-Loredo V, Simmons VN, Meltzer LR, Drobes DJ, Brandon KO, Palmer AM, Eissenberg T, Bullen CR, Harrell PT, & Brandon TH (2020). How does smoking and nicotine dependence change after onset of vaping? A retrospective analysis of dual users. Nicotine Tob Res, 22(5), 764–770. 10.1093/ntr/ntz043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meier EM, Tackett AP, Miller MB, Grant DM, & Wagener TL (2015). Which nicotine products are gateways to regular use? American Journal of Preventive Medicine, 48(1), S86–S93. 10.1016/j.amepre.2014.09.018 [DOI] [PubMed] [Google Scholar]
- Mhoon KB, Chan W, Del Junco DJ, & Vernon SW (2010). A continuous-time markov chain approach analyzing the stages of change construct from a health promotion intervention. JP journal of biostatistics, 4(3), 213–226. http://www.ncbi.nlm.nih.gov/pubmed/23504410 [PMC free article] [PubMed] [Google Scholar]
- National Institutes of Health. (2015). Population Assessment of Tobacco and Health. Retrieved August 31 from https://pathstudyinfo.nih.gov/UI/HomeMobile.aspx
- Niaura R, Rich I, Johnson AL, Villanti AC, Romberg AR, Hair EC, Vallone DM, & Abrams DB (2020). Young adult tobacco and e-cigarette use transitions: examining stability using multistate modeling. Nicotine Tob Res, 22(5), 647–654. 10.1093/ntr/ntz030 [DOI] [PubMed] [Google Scholar]
- Perry CL, Pérez A, Bluestein M, Garza N, Obinwa U, Jackson C, Clendennen SL, Loukas A, & Harrell MB (2018). Youth or young adults: which group is at highest risk for tobacco use onset? Journal of Adolescent Health, 63(4), 412–420. 10.1016/j.jadohealth.2018.04.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pierce JP, White MM, & Messer K (2009). Changing age-specific patterns of cigarette consumption in the United States, 1992-2002: association with smoke-free homes and state-level tobacco control activity. Nicotine Tob Res, 11(2), 171–177. 10.1093/ntr/ntp014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pokhrel P, Fagan P, Kehl L, & Herzog TA (2015). Receptivity to e-cigarette marketing, harm perceptions, and e-cigarette use. Am J Health Behav, 39(1), 121–131. 10.5993/AJHB.39.1.13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Primack BA, Shensa A, Sidani JE, Hoffman BL, Soneji S, Sargent JD, Hoffman RM, & Fine MJ (2018). Initiation of traditional cigarette smoking after electronic cigarette use among tobacco-naive US young adults. Am J Med, 131(4), 443.e441–443.e449. 10.1016/j.amjmed.2017.11.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Primack BA, Soneji S, Stoolmiller M, Fine MJ, & Sargent JD (2015). Progression to traditional cigarette smoking after electronic cigarette use among US adolescents and young adults. JAMA Pediatrics, 169(11), 1018–1023. 10.1001/jamapediatrics.2015.1742 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rath JM, Villanti AC, Abrams DB, & Vallone DM (2012). Patterns of tobacco use and dual use in us young adults: the missing link between youth prevention and adult cessation. Journal of Environmental and Public Health, 2012, 1–9. 10.1155/2012/679134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richardson A, Williams V, Rath J, Villanti AC, & Vallone D (2014). The next generation of users: prevalence and longitudinal patterns of tobacco use among US young adults. American Journal of Public Health, 104(8), 1429–1436. 10.2105/AJPH.2013.301802 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robertson L, Iosua E, McGee R, & Hancox RJ (2016). Nondaily, low-rate daily, and high-rate daily smoking in young adults: a 17-year follow-up. Nicotine & Tobacco Research, 18(5), 943–949. 10.1093/ntr/ntv167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schulenberg J, Johnston L, O'Malley P, Bachman J, Miech R, & Patrick M (2020). Monitoring the Future national survey results on drug use, 1975-2019: Volume II, college students and adults ages 19-60. http://monitoringthefuture.org/pubs.html#monographs [Google Scholar]
- Selya AS, Dierker L, Rose JS, Hedeker D, & Mermelstein RJ (2016). Early-emerging nicotine dependence has lasting and time-varying effects on adolescent smoking behavior. Prev Sci, 17(6), 743–750. 10.1007/s11121-016-0673-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soneji S, Barrington-Trimis JL, Wills TA, Leventhal AM, Unger JB, Gibson LA, Yang J, Primack BA, Andrews JA, Miech RA, Spindle TR, Dick DM, Eissenberg T, Hornik RC, Dang R, & Sargent JD (2017). Association between initial use of e-cigarettes and subsequent cigarette smoking among adolescents and young adults: a systematic review and meta-analysis. JAMA Pediatrics, 171(8), 788–797. 10.1001/jamapediatrics.2017.1488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soneji S, Sargent JD, Tanski SE, & Primack BA (2015). Associations between initial water pipe tobacco smoking and snus use and subsequent cigarette smoking: results from a longitudinal study of US adolescents and young adults. JAMA Pediatrics, 169(2), 129–136. 10.1001/jamapediatrics.2014.2697 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Starr G, Rogers T, Schooley M, Porter S, Wiesen E, & Jamison N (2005). Key outcome indicators for evaluating comprehensive tobacco control programs. CDC. [Google Scholar]
- Substance Abuse Mental Health Services Administration. (2012). The NSDUH report: trends in cigarette use among adolescents and young adults. http://archive.samhsa.gov/data/2k12/NSDUH047/SR047CigaretteTrends2012.htm
- Sutfin EL, McCoy TP, Berg CJ, Champion H, Helme DW, O'Brien MC, & Wolfson M (2012). Tobacco use by college students: a comparison of daily and nondaily smokers. American Journal of Health Behavior, 36(2), 218–229. 10.5993/AJHB.36.2.7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verplaetse TL, Moore KE, Pittman BP, Roberts W, Oberleitner LM, Peltier MKR, Hacker R, Cosgrove KP, & McKee SA (2019). Intersection of e-cigarette use and gender on transitions in cigarette smoking status: findings across waves 1 and 2 of the Population Assessment of Tobacco and Health Study. Nicotine Tob Res, 21(10), 1423–1428. 10.1093/ntr/nty187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Villanti AC, Niaura RS, Abrams DB, & Mermelstein R (2019). Preventing smoking progression in young adults: the concept of prevescalation. Prev Sci, 20(3), 377–384. 10.1007/s11121-018-0880-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- White HR, Bray BC, Fleming CB, & Catalano RF (2009). Transitions into and out of light and intermittent smoking during emerging adulthood. Nicotine & Tobacco Research, 11(2), 211–219. 10.1093/ntr/ntn017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolfson M, Suerken CK, Egan KL, Sutfin EL, Reboussin BA, Wagoner KG, & Spangler J (2015). The role of smokeless tobacco use in smoking persistence among male college students. The American Journal of Drug and Alcohol Abuse, 41(6), 541–546. 10.3109/00952990.2015.1078345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yi Z, Mayorga ME, Hassmiller Lich K, & Pearson JL (2017). Changes in cigarette smoking initiation, cessation, and relapse among U.S. adults: a comparison of two longitudinal samples. Tobacco Induced Diseases, 15(1), 1–11. 10.1186/s12971-017-0121-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.