Abstract
Introduction
In the spring of 2020, New York City was one of the first epicenters of the COVID outbreak. In this study, we evaluate the incidence and treatment of appendicitis in two New York City community hospitals during the COVID pandemic.
Methods
This retrospective study focused on the incidence and outcome of acute appendicitis in the adult population (>18 y old) during peak-COVID periods (March 16, 2020,-June 15, 2020) compared to pre-COVID and post-COVID periods. We compared the number of patients who underwent operative versus nonoperative management, patient demographics, length of stay (LOS), complications, and readmission rates within these time periods. Data are presented as mean ± standard deviation (analysis of variance).
Results
From January 1, 2020 to December 31, 2020, 393 patients presented with acute appendicitis and 321 (81.7%) were treated operatively, compared to 441 total and 366 treated operatively (83%) in 2019 (P = 0.88). During the COVID outbreak, fewer patients presented with appendicitis (mean 6.9 ± 1 pre-COVID case/week, 4.4 ± 2.4 peak-COVID cases/week and 7.6 ± 0.65 post-COVID cases/week, P = 0.018) with no significant difference in the pre-COVID and post-COVID period. There was no difference in LOS between the pre-, peak-, and post-COVID periods with a median of 1 for all the three, (interquartile range (IQR): 0.8-2, 0.6-2, 0.6-2, respectively, P = 0.43). Additionally, there was no difference in 30-day readmission rates (4.2%, 0%, 3.9%, P = 0.99) and postoperative complications (4.2%, 0%, 2.9%, P = 0.98).
Conclusions
During peak-COVID, there was a significant reduction in the number of patients who presented with acute appendicitis without a post rebound increase in presentation. Those who presented during peak-COVID were able to undergo operative management safely, without affecting LOS or postoperative complications.
Keywords: Appendectomy, Appendicitis, COVID-19, Operative management, Pandemic
Introduction
Acute appendicitis is one of the most common abdominal surgical conditions in the United States, with more than 300,000 appendectomies performed annually.1 Although nonoperative management with antibiotics can be an acceptable and effective treatment option for simple acute appendicitis,1 laparoscopic appendectomy is the gold standard in management.2 Other treatment modalities include percutaneous drainage of appendiceal abscess for patients with perforated appendicitis, but even then, interval appendectomy is often done after successful drainage and resolution of the acute inflammation.
The treatment algorithm for appendicitis changed with the rise of the novel 2019 coronavirus outbreak (COVID-19) caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). The World Health Organization announced COVID-19 a pandemic in March of 2020, and New York City was one of the first major epicenters for the virus across all the five boroughs.3 Hospitals began to ration resources and create protocols for treatment plans as the pandemic worsened.4, 5, 6, 7 The management for acute appendicitis varied worldwide as the virus continued to spread and little was known. Given the expeditious rate of global infection spread, some countries and cities elected to proceed with nonoperative management while others elected to favor operative management when possible.8, 9, 10, 11, 12, 13 Given unknowns about the virus and how it affected patients with comorbidities, there was concern that operating on these patients would increase morbidity related to COVID as well as potential viral transmission from producing pneumoperitoneum. There was also concern for preservation and allocation of staff and resources.
In this study, we look at our two hospitals in the diverse neighborhoods of Brooklyn and Queens, New York, and our practices for patients who were diagnosed with appendicitis during the COVID pandemic. We also evaluate for changes in rate of admissions for appendicitis as well as changes in management during the 2020 pandemic compared to 2019.
Methods
Patient population
Between March 16 and June 14, 2020, all elective surgical procedures in the NewYork Presbyterian (NYP) Brooklyn Methodist Hospital system were canceled to reallocate resources for patient safety and redistribute hospital staff. Only three operating rooms (ORs) out of eighteen were functioning during the peak as the others were converted temporarily into intensive care unit beds for COVID patients given capability for negative pressure ventilation. Similarly, all elective surgical procedures were restricted at NYP Queens Hospital between March 16, 2020, and June 14, 2020, with one OR out of twenty functioning for procedures.
Patients who presented to the emergency department at NYP Brooklyn Methodist Hospital and NYP Queens Hospital between January 1, 2019 and December 2020 under the International Classification of Diseases codes relating to appendicitis were included within our study. Patients in the pediatric population (<18 y old) were excluded. During the OR shutdown, the pediatric units in both of this study's hospitals were redesigned to serve as intensive care units for COVID patients. Pediatric patients who required additional care or overnight stay were transferred to our institution's main pediatric hospital. Additional exclusion criteria included patients with chronic appendicitis, patients who presented for interval appendectomy for previous episode(s) of appendicitis, and those who underwent additional concurrent procedures or complications intraoperatively that warranted additional procedures.
Patients who underwent operative management for appendicitis were included for comparison of hospital course review. Operative management was defined as either laparoscopic or open appendectomies, or operative drainage. Nonoperative management included antibiotic treatment or minimally invasive drainage.
Data collection
Electronic medical records were extracted and retrospectively reviewed. Patient identification was removed prior to data analysis and institutional review board approval was obtained for retrospective review between both hospitals for the study prior to proceeding with data collection and analysis. Consent was waived given minimal risk to patients and patient information was de-identified. Overall comparison of incidence of appendicitis and rate of surgical versus conservative or nonoperative management was made between 2019 and 2020. Within 2020, incidence rates of appendicitis were divided into time intervals relative to the COVID pandemic peak when OR cases were limited to emergencies: January 1 to March 15, 2020 (preperiod), March 16 to June 14, 2020 (peak period), and June 15 to December 31, 2020 (post period).
Variables analyzed for patients with appendicitis in 2020 included sex, age, race, ethnicity, American Society of Anesthesiologists (ASA) classification, body mass index (BMI), and symptom duration length prior to admission. The primary outcome of the study focused on postoperative outcomes which were compared between the peak-COVID and the pre-COVID and post-COVID periods; these outcomes included hospital length of stay (LOS), readmission rates, and complication rates within 30 d postoperatively. Postoperative complications included deep venous thrombosis, urinary tract infection, pulmonary embolism, abscess formation, or surgical site infection. The surgical site infection was defined as superficial infections including cellulitis whereas abscesses pertained to deep infections.
Statistical analysis
Analysis was performed using the analysis of variance for univariate analysis. Chi-square test and Fisher's exact test were used for categorical data analysis, with a P-value <0.05 considered to be statistically significant. Continuous variables were noted to be skewed. The Kruskal–Wallis test was used to analyze age, LOS, BMI, and duration of symptoms. Statistics were performed on SAS OnDemand for Academics.
Results
2019 and 2020 incidence comparison
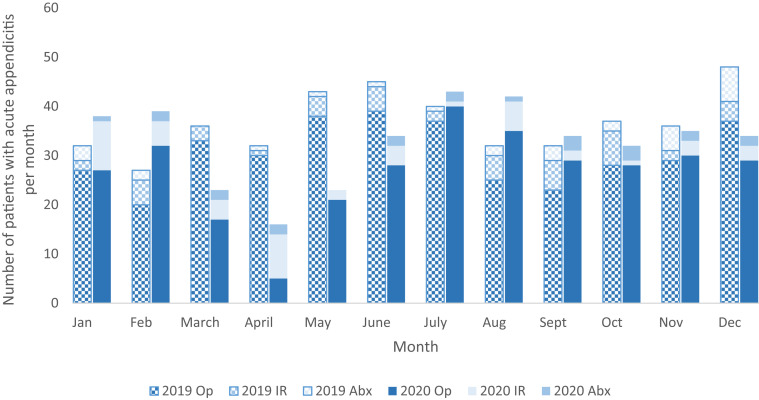
From January 1, 2020 to 12/31/2020, 393 patients presented with acute appendicitis and 321 (81.7%) were treated operatively, compared to 441 total and 366 treated operatively (83%) in 2019 (P = 0.88). In 2020, 12.7% (n = 50) of patients who presented with appendicitis underwent percutaneous drainage, whereas 5.6% (n = 22) had nonoperative management with antibiotics only. In 2019, 10.4% (n = 46) of the patients underwent interventional radiology (IR) drainage, and 6.3% (n = 28) were treated nonoperatively with antibiotics, in which there was no significant difference (P = 0.36). During the pre-COVID period in 2020, there was an average of 28 patients per month managed operatively compared to 2 with IR drainage and 7 with antibiotics. During the peak, there was an average of 18 patients per month managed operatively compared to 2 with IR drainage and 5 with antibiotics. Finally during the post, there was an average of 30 patients per month managed operatively compared to two per month with IR drainage and three per month with antibiotics (Fig. 1 ). Two patients who had undergone open appendectomy were initially from laparoscopic converted to open.
Fig. 1.
Number of patients who presented with acute appendicitis each month during 2019 and 2020 and form of management. Op = operative; IR = interventional radiology for percutaneous drainage; Abx = antibiotics only.
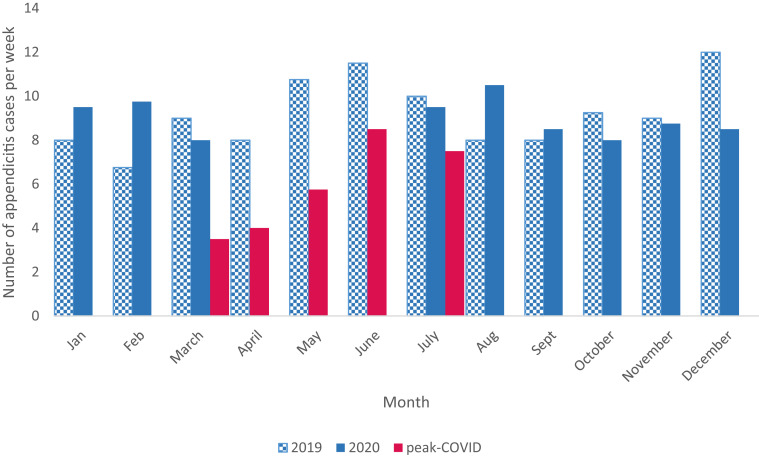
The average weekly rate of acute appendicitis during the pre-COVID, peak-COVID time and post-COVID time periods was 6.9 ± 1, 4.4 ± 2.4, and 7.6 ± 0.65, respectively (P = 0.018), with the median incidence rate being 6.8, 5.3, and 7.4 d (Fig. 2 ).
Fig. 2.
Weekly rate of appendicitis cases during 2019, 2020, and peak-COVID time period in 2020.
2020 comparison between pre-COVID, peak-COVID, and post-COVID shutdown
Patient demographics
The median age for patients during the pre-COVID, peak-COVID and post-COVID shutdown periods were 37, 33, and 38 y old (interquartile range [IQR] 29-47, 26-44, 29-50, respectively. There was no difference in sex for patients who underwent surgery during the three time periods; males encompassed 60.6%, 51.2%, and 48.8% of patients during the pre-COVID, peak-COVID and post-COVID while females were 38.4%, 48.8%, and 51.2%, respectively, (P = 0.23). There was also no difference in BMI, with median BMIs of 25.4, 25.8, and 26.3 for these time periods (IQR 22.2-28.7, 22.5-28.7, and 23-30, respectively, P = 0.16) (Table 1 ).
Table 1.
Comparison of patient demographic and preoperative factors.
| Patient factor | Time period |
P-value | ||
|---|---|---|---|---|
| Pre-COVID (n = 71) | Peak-COVID (n = 43) | Post-COVID (n = 207) | ||
| Age in y (median, IQR) | 37 (29-47) | 33 (26-44) | 38 (29-50) | 0.37 |
| Sex (%) | ||||
| Male | 43 (60.6%) | 21 (51.2%) | 101 (48.8%) | 0.23 |
| Female | 28 (39.4%) | 21 (48.8%) | 106 (51.2%) | |
| Race (%) | ||||
| Caucasian | 31 (43.7%) | 14 (32.6%) | 79 (38.2%) | 0.2 |
| African-American | 7 (9.9%) | 4 (9.3%) | 27 (13%) | |
| Asian | 9 (12.7%) | 13 (2%) | 36 (17.4%) | |
| Other | 0 (0%) | 0 (0%) | 0 (0%) | |
| Unknown | 24 (33.8%) | 12 (27.9%) | 65 (31.4%) | |
| Ethnicity (%) | ||||
| Non-Hispanic | 42 (59.2%) | 22 (51.2%) | 107 (51.7%) | 0.31 |
| Hispanic | 16 (22.5%) | 10 (23.3%) | 66 (31.9%) | |
| Unknown | 11 (15.5%) | 11 (25.6%) | 33 (15.9%) | |
| ASA class (%) | ||||
| I | 31 (43.7%) | 19 (44.2%) | 55 (26.6%) | 0.0015 |
| II | 33 (46.5%) | 18 (41.9%) | 119 (57.5%) | |
| III | 2 (2.8%) | 1 (2.3%) | 25 (12%) | |
| IV | 1 (1.4%) | 0 (0%) | 0 (0%) | |
| V | 0 (0%) | 0 (0%) | 0 (0%) | |
| BMI (median, IQR) | 25.4 (22.2-28.7) | 25.8 (22.5-28.7) | 26.3 (23.0-30.0) | 0.16 |
ASA = American Society of Anesthesiologists; BMI = body mass index; IQR = Interquartile range; SD = standard deviation.
(Table 1) The majority ASA class for pre-COVID, peak-COVID, and post-COVID periods were ASA II (46.5%), ASA I (44.2%), and ASA II (57.5%), respectively, (P = 0.0015). The median and mode for the pre-COVID and peak-COVID periods were ASA I, whereas the median and mode for the post period was ASA II. In regards to race and ethnicity, there was no significant difference (P = 0.2), and of patients with reported ethnicity, there was also no significant difference (P = 0.3). Median symptom duration for each time period was 1 d (IQR 1-2, P = 0.45) (Table 1). The majority of patients underwent laparoscopic approach regardless of time period in relation to the pandemic peak. Two patients in post-COVID that had open appendectomies were laparoscopic converted to open, representing 9% of all open appendectomies in this time frame.
There were a total of ten patients who presented during the peak- and post-COVID periods who were COVID positive. Two of these patients were operated on during the peak-COVID period. The remaining eight patients were treated post-COVID; one was treated nonoperatively with antibiotics and the other seven were treated surgically (six laparoscopically and one open). Only one patient in the post-COVID time had readmission for abscess.
Postoperative outcomes
There was no significant change in LOS with the median number of days for LOS being 1 d for all three time periods (IQR 0.8-2, 0.6-2, 0.6-2 for pre-, peak-, and post-COVID respectively) (Table 2 ).
Table 2.
Comparison of patient outcomes postoperatively.
| Operative outcome | Time period |
P-value | ||
|---|---|---|---|---|
| Pre (n = 71) | Peak (n = 43) | Post (n = 207) | ||
| Method of surgery | ||||
| Laparoscopic | 66 (93%) | 40 (93%) | 184 (88.9%) | 0.49 |
| Open | 5 (7%) | 3 (7%) | 23 (11.1%) | |
| Symptom duration in days (median, IQR) | 1 (1-2) | 1 (1-2) | 1 (1-2) | 0.43 |
| LOS in days (median, IQR) | 1 (0.8-2) | 1 (0.6-2) | 1 (0.6-2) | 0.63 |
| Readmissions (%) | 3 (4.2%) | 0 (0%) | 8 (3.9%) | 0.99 |
| Postoperative complications (%) | 3 (4.2%) | 0 (0%) | 6 (2.9%) | 0.98 |
| PE | 0 (0%) | 0 (0%) | 0 (0%) | |
| UTI | 0 (0%) | 0 (0%) | 0 (0%) | |
| DVT | 0 (0%) | 0 (0%) | 0 (0%) | |
| Abscess | 1 (1.4%) | 0 (0%) | 6 (2.9%) | |
| SSI | 2 (2.8%) | 0 (0%) | 0 (0%) | |
DVT = deep venous thrombosis; LOS = length of stay; PE = pulmonary embolism; Readmissions = 30 d readmissions; SD = standard deviation; SSI = surgical site infection; UTI = urinary tract infection.
Overall complication rates were 4.2% (n = 3), 0% (n = 0), and 2.9% (n = 6) in the pre-, peak-, and post-COVID periods (P = 0.98). Readmission rates were 4.2% (n = 3), 0% (n = 0), and 3.9% (n = 6), respectively (P = 0.99) (Table 2).
Discussion
Laparoscopic surgery, which began gaining widespread use approximately 50 y ago, is now the standard of care for many conditions requiring emergency general surgery including appendicitis. However, the COVID-19 pandemic presented a significant challenge to public health in New York City health systems not seen in over a century and impacted the routine use of laparoscopic surgery. In addition to disaster preparedness protocols which led to surgical resource reallocation and staff redeployment, surgical management of appendicitis may have also been limited by unmeasurable changes such as differences in patient attitude toward hospitalization and concerns for staff safety due to laparoscopic plume contributed to the increasing adoption of nonoperative management.14 Although nonoperative management has been a topic of recent interest, the pandemic may have helped accelerate the use of nonoperative management for appendicitis. Our hospitals, like others in New York City and across the nation, halted elective surgeries and limited OR availability due to ad hoc local and national guidelines regarding COVID.15 Although our hospitals had a significant reduction in operative case volume during the peak of the pandemic, the percentage of general surgery cases compared to other specialties during this time did not decrease.16 Despite the decrease in patients with appendicitis that went to the OR during the COVID lockdown period, in our cohort, the proportion of operative appendicitis remained the same. This suggests that during the COVID lockdown period, there was a decrease in presentation of appendicitis rather than decrease in operative management.
There were no significant differences noted in patient demographics, including age, sex, BMI, or symptom duration. On admission, some patients opted not to disclose race or ethnicity, limiting the analysis. Interestingly, there was a significant difference between the three time periods in ASA classification. Without significant differences in other preoperative characteristics such as age, gender, BMI, it is possible that the difference in ASA class reflects a behavioral change in patients who have an option to present to the hospital. However, without a difference in severity of appendicitis on presentation in our data, factors outside of behavior may contribute to this pattern.
There was no significant difference in postoperative complications, LOS, or readmission rates for patients who underwent operative management for appendicitis between the three time periods. Although outpatient appointments in NYC during the peak of the pandemic were limited to virtual visits and telephone calls due to restrictions,17 the number of postoperative complication or readmission rates was potentially blunted by routine patient education regarding signs and symptoms requiring prompt medical attention. While there was a concern for worsened outcomes during the shutdown time period due to delayed presentation, decreased OR staff, and decreased recent surgical volume, our dataset does not show an increase in postoperative adverse events for patients with operative appendicitis during the time frame of the pandemic shutdown.
Although some studies have advocated for nonoperative management during the conditions of the pandemic,10 , 11 it may not be necessary to delay operative management on these patients. There is mixed literature on the severity of appendicitis on presentation during the quarantine and shutdowns.11, 12, 13 In our patient population, we could not detect a difference in the acuity or severity of appendicitis on presentation. There is not enough data to confirm the safety of operating on patients who test positive for COVID-19, as only a small subset of our patient population who presented with acute appendicitis had concurrent COVID infection. We are also unable to compare rates with pre-COVID patients as testing was not available at that time.
Acute appendicitis was found to have decreased incidence in other areas and countries as well during the pandemic, including Europe and other parts of the United States.18 , 19 Although there are some reports that COVID-19 may present as appendicitis,20 it is difficult to determine whether these patients incidentally also had appendicitis or if these symptoms and findings were truly related to the virus. Further studies are necessary to understand what specific factors played a role in the decrease in incidence of appendicitis during the peak-COVID time frame.
A causal link between the viral infections and appendicitis remains a tantalizing hypothesis; however, due to the low incidence of COVID-19 within our cohort, we cannot evaluate for an association between COVID-19 infection and appendicitis from our data. Interestingly, our data did not show evidence of a rebound in incidence of acute appendicitis after the shutdown, as the number of patients who presented during the preperiods and post periods were relatively similar. It is possible that patients with appendicitis traveled to hospitals in other locations because of traveling bans, but there was a decrease in acute appendicitis in other geographic areas as well during the pandemic.17 , 18 In addition, there was a decrease in overall surgical urgent cases which reflects a decrease in the admission rates of patients with surgical disease.16 In New York and other major cities, there was an overall decrease in emergency department visits,21 suggesting that there were broader changes in hospital use among patients during the peak-COVID time period.
Limitations
This study has inherent limitations as a retrospective study at two institutions from a single city. In addition, given the increased use of telehealth during the shutdown period, patients who may have otherwise presented to the hospital may have opted for telehealth visits at home. Our data also does not capture attrition rates and patients lost to follow-up, which may result in underreported postoperative outcomes. Although there are some studies that have shown that appendectomies were safe during the pandemic,9 further investigation is needed to better evaluate the safety and efficacy of operative management for appendicitis during the peak of the virus. With the advent of the COVID-19 vaccines, future steps would be to investigate long-term trends in the natural history of appendicitis, treatment patterns, and post-treatment course in relation to COVID-19. We did not investigate length of surgery and time to surgery as time to surgery would be difficult to compare between the peak and post time periods due to mandatory preoperative COVID testing. During these time frames, processing times for COVID swabs continued to evolve, thus affecting time to surgery. Despite this, LOS did not change significantly, signifying that there were no major changes in outcomes for appendectomies. We also did not include insurance status as part of our study. This would be a critical value to include in future research in comparing demographics of patients and how socioeconomic status may or may not be associated with the pandemic.
In summary, we found that appendectomies were safe for patients during the peak of the first wave of COVID-19 and lockdown. Surgeons should not hesitate to operate on patients with appendicitis whom they deem to be safe candidates as long as there is adequate staffing and resources available. However, surgeons should continue to be diligent in appropriately risk stratifying and optimizing patients preoperatively and consider each patient on an individual basis before proceeding with surgery.
Author Contributions
Olivia Cheng, Roseanna Lee, and James Hu contributed to study conception and design. Olivia Cheng, James Hu, Roseanna Lee, Julie Hong, Nakia Sarad, and Chun-Cheng Chen contributed to acquisition of data. Olivia Cheng contributed to analysis and interpretation of data. Olivia Cheng, James Hu, and Julie Hong contributed to drafting of manuscript. Roseanna Lee, Michael Zenilman, Bashar Fahoum, and Chun-Cheng Chen contributed to critical revision of manuscript.
Disclosure
None declared.
Funding
None to report.
References
- 1.Salminen P., Paajanen H., Rautio T., et al. Antibiotic therapy vs appendectomy for treatment of uncomplicated acute appendicitis: the APPAC randomized clinical trial. JAMA. 2015;313:2340–2348. doi: 10.1001/jama.2015.6154. [DOI] [PubMed] [Google Scholar]
- 2.Fitzmaurice G.J., McWilliams B., Hurreiz H., Epanomeritakis E. Antibiotics versus appendectomy in the management of acute appendicitis: a review of the current evidence. Can J Surg. 2011;54:307–314. doi: 10.1503/cjs.006610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wadhera R.K., Wadhera P., Gaba P., et al. Variation in COVID-19 hospitalizations and deaths across New York city boroughs. JAMA. 2020;323:2192–2195. doi: 10.1001/jama.2020.7197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Emanuel E.J., Persad G., Upshur R., et al. Fair allocation of scarce medical resources in the time of covid-19. N Engl J Med. 2020;382:2049–2055. doi: 10.1056/NEJMsb2005114. [DOI] [PubMed] [Google Scholar]
- 5.Mattingly A.S., Rose L., Eddington H.S., et al. Trends in US surgical procedures and health care system response to policies curtailing elective surgical operations during the COVID-19 pandemic. JAMA Netw Open. 2021;4:e2138038. doi: 10.1001/jamanetworkopen.2021.38038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Prakash L., Dhar S.A., Mushtaq M. COVID-19 in the operating room: a review of evolving safety protocols. Patient Saf Surg. 2020;14:30. doi: 10.1186/s13037-020-00254-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Al-Jabir A., Kerwan A., Nicola M., et al. Impact of the Coronavirus (COVID-19) pandemic on surgical practice - Part 1. Int J Surg. 2020;79:168–179. doi: 10.1016/j.ijsu.2020.05.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kelly M.E., Murphy E., Bolger J.C., Cahill R.A. COVID-19 and the treatment of acute appendicitis in Ireland: a new era or short-term pivot? Colorectal Dis. 2020;22:648–649. doi: 10.1111/codi.15141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Salgaonkar H., Aladeojebi A., Murcott D., Nnaji M., Tsiamis A., Cheruvu C.V. Emergency appendicectomy during COVID-19 pandemic - a single UK centre experience. Pol Przegl Chir. 2021;93:33–39. doi: 10.5604/01.3001.0014.8090. [DOI] [PubMed] [Google Scholar]
- 10.Scott C., Lambert A. Managing appendicitis during the COVID-19 pandemic in the UK. Br J Surg. 2020;107:e271. doi: 10.1002/bjs.11752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pringle H.C.M., Donigiewicz U., Bennett M.R., et al. Appendicitis during the COVID-19 pandemic: lessons learnt from a district general hospital. BMC Surg. 2021;21:242. doi: 10.1186/s12893-021-01231-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Finkelstein P., Picado O., Muddasani K., et al. A retrospective analysis of the trends in acute appendicitis during the COVID-19 pandemic. J Laparoendosc Adv Surg Tech. 2021;31:243–246. doi: 10.1089/lap.2020.0749. [DOI] [PubMed] [Google Scholar]
- 13.Scheijmans J.C.G., Borgstein A.B.J., Puylaert C.A.J., et al. Impact of the COVID-19 pandemic on incidence and severity of acute appendicitis: a comparison between 2019 and 2020. BMC Emerg Med. 2021;21:61. doi: 10.1186/s12873-021-00454-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Klein M.J., Frangos S.G., Krowsoski L., et al. Acute care surgeons’ response to the COVID-19 pandemic: observations and strategies from the epicenter of the American crisis. Ann Surg. 2020;272:e66–e71. doi: 10.1097/SLA.0000000000004028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Knisely A., Zhou Z.N., Wu J., et al. Perioperative morbidity and mortality of patients with covid-19 who undergo urgent and emergent surgical procedures. Ann Surg. 2021;273:34–40. doi: 10.1097/SLA.0000000000004420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.McClelland P.H., Cheng O., Hu J., et al. Operative shutdown and recovery: restructuring surgical operations during the SARS-CoV-2 pandemic. J Surg Res. 2021;268:181–189. doi: 10.1016/j.jss.2021.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Koziatek C.A., Rubin A., Lakdawala V., et al. Assessing the impact of a rapidly scaled virtual urgent care in New York city during the COVID-19 pandemic. J Emerg Med. 2020;59:610–618. doi: 10.1016/j.jemermed.2020.06.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rosenthal M.G., Fakhry S.M., Morse J.L., et al. Where did all the appendicitis go? Impact of the COVID-19 pandemic on volume, management, and outcomes of acute appendicitis in a Nationwide, multicenter analysis. Ann Surg Open. 2021;2:e048. doi: 10.1097/AS9.0000000000000048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tankel J., Keinan A., Blich O., et al. The decreasing incidence of acute appendicitis during COVID-19: a retrospective multi-centre study. World J Surg. 2020;44:2458–2463. doi: 10.1007/s00268-020-05599-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Malbul K., Katwal S., Maharjan S., Shrestha S., Dhital R., Rajbhandari A.P. Appendicitis as a presentation of COVID-19: a case report. Ann Med Surg (Lond) 2021;69:102719. doi: 10.1016/j.amsu.2021.102719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jeffery M.M., D’Onofrio G., Paek H., et al. Trends in emergency department visits and hospital admissions in health care systems in 5 states in the first months of the covid-19 pandemic in the us. JAMA Intern Med. 2020;180:1328–1333. doi: 10.1001/jamainternmed.2020.3288. [DOI] [PMC free article] [PubMed] [Google Scholar]