Abstract
A foundational component of digital health involves collecting and leveraging electronic health data to improve health and wellbeing. One of the central technologies for collecting these data are electronic health records (EHRs). In this commentary, the authors explore intersection between digital health and data-driven reflective practice that is described, including an overview of the role of EHRs underpinning technology innovation in healthcare. Subsequently, they argue that EHRs are a rich but under-utilised source of information on the performance of health professionals and healthcare teams that could be harnessed to support reflective practice and behaviour change. EHRs currently act as systems of data collection, not systems of data engagement and reflection by end users such as health professionals and healthcare organisations. Further consideration should be given to supporting reflective practice by health professionals in the design of EHRs and other clinical information systems.
Keywords: Digital health, Electronic health records, Health informatics, User experience design
Introduction
Electronic health records (EHRs) are repositories of patient health information, created by health professionals to capture data related to specific clinical encounters [1]. This type of information has great potential to enable health professionals to understand the quality of their performance and to support reflective practice and learning. Reflective practice is the process of revising habits, routines, and experiences to understand complex problems and learn from past behaviours [2, 3]. It is a process that can be engaged in by both individuals and groups of people [2]. In the context of the health workforce, reflective practice has been identified as an essential process for health professionals to maintain up to date knowledge and skills [4, 5].
To date, the potential of EHRs to support this has not been fully reached. The design of most modern EHR systems does little to encourage or enable health professional learning. Addressing this issue is important now because there has been a growing movement to make health information systems such as EHRs more interoperable [6]. Increased interoperability will enable a readily available flow of data that can be used for reflective practice by health professionals [6]. Furthermore, EHR development is currently undergoing an unprecedented era of innovation [7–9]. This is resulting in disruption to enterprise vendors by more agile next-generation EHRs that can respond to diverse needs of end users [10]. Innovation in EHR development runs parallel to similar technological innovations occurring in the education space such as the use of virtual and augmented reality [11] and bots [12] to transform learning. Finally, there are currently a range of changes in the policy landscape regarding how health professionals engage in learning activities; these emphasise the need for health professionals to use electronic data to understand their outcomes as a component of their mandated training activities and revalidation [13, 14]. In this commentary, we contextualise the intersection between digital health and data-driven reflective practice. Furthermore, we argue that EHRs are a rich source of information on the performance of health professionals and healthcare teams that could be harnessed to support reflection and learning.
Digital health is a diverse field that has been defined and redefined many times, but can be described as the use of electronic health data and digital technology to inform medical practice and improve health [15]. It includes consumer technologies such as apps and devices, communication technologies such as telehealth, and informatics technologies for capturing and harnessing electronic data [16]. Digital health also brings together multidisciplinary experts [17] to explore how technology can strengthen and transform healthcare. As a field, digital health includes individuals with expertise in human computer interaction, who seek to better understand the design of health technologies [18, 19], implementation scientists exploring how to implement and de-implement technologies [20], empirical researchers evaluating whether health technology improves health outcomes [21], and many other diverse stakeholders.
Electronic Health Data
A foundational component of digital health involves collecting and leveraging electronic health data to improve health and wellbeing. EHRs are core technologies for collecting these data. EHRs are information systems used by healthcare organisations around the world to capture data on patient care. In the context of digital health, the literature has explored EHR technology from many perspectives such as:
Investigating the knowledge and skills the health workforce require to utilise EHRs and the data within them [16, 22];
Understanding how organisations can efficiently implement EHRs [23] and their use as signifiers of digital maturity [24];
Evaluating the use of EHRs to undertake research that is integrated with routine clinical care [25];
Investigating the effectiveness of the use of EHRs as tools for improving quality of care [26, 27] and predicting health trajectories [28];
Exploring the potential of EHRs to support virtual care and other new healthcare models [29] and many applications beyond these.
The potential of EHR data for supporting tailored interventions to improve the processes and outcomes of care is gaining recognition by a range of disciplines in the health sector including medicine, nursing and allied health [30]. To date, the value of EHR data to support reflective practice via individual and team learning has been largely unrealised. This is surprising for a number of reasons. Firstly, and potentially most importantly, health professionals want to use EHR data for reflective practice and learning [30]. Secondly, many health professionals dedicate considerable work time in a range of learning activities [31]. Thirdly, reflection and workplace learning are recognised mechanisms to ensure health professionals stay up to date with emerging clinical evidence and best practice guidelines [32]. Finally, patients are increasingly advocating for increased involvement in collaborative clinical decision through data collection mechanisms such as patient reported measures and EHR gateways [33].
The first EHRs were developed in the 1970s [34], but the technology was not widely adopted until the late 1990s. The World Health Organization’s 2016 global survey of eHealth found that more than 50% (n = 23) of upper- and middle-income countries, 35% (n = 10) of lower-middle income countries and 10% (n = 3) of low-income countries have adopted national electronic records [35]. These data indicate there is an emerging trend in adopting EHRs in upper- and middle-income countries. EHRs are championed as a digital health solution that can offer wide reaching benefits at the clinical, organisational and societal level [36]. Improvements that EHRs can offer at the clinical level include minimisation of medical errors and improvements in care coordination [37].
The potential of EHRs for quality improvement [38], clinical research [39], professional development and practice improvement by health professionals [40] has already been recognised in the literature. Key barriers to using EHRs for these purposes include the perception that EHRs increase the workload of health professionals, particularly when the information systems are initially introduced [41]. Coupled with this, the usability and interoperability of EHRs have been recognised as a significant barrier to their adoption by the health workforce [42].
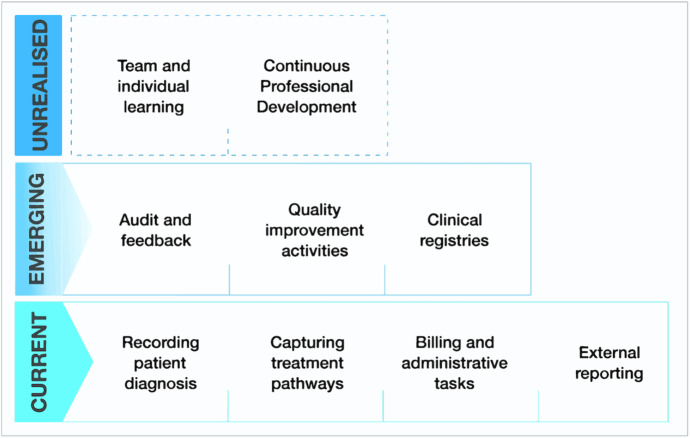
Although there is now a growing interest in open-source EHRs, healthcare organisations still largely adopt costly proprietary information systems developed by enterprise vendors [1, 38]. The design of modern EHRs is still heavily informed by their legacy as billing and administrative information systems, which includes a general repository for patient data [37] and coding of patient data for administrative and billing purposes (Fig. 1) [1].
Fig. 1.
Characterisation of the main uses of EHR data in healthcare organisations, with current uses at the bottom, emerging trends in use in the middle, and, at the top, potential uses that are yet to be realised
There is a considerable variation in the functionality of modern EHRs at different organisations around the world. At a minimum, most EHRs provide three key medical functions: (1) presenting the most-up-to date information on a patient, (2) storing supporting documentation about a patient (such as test results and imaging) and (3) enabling health professionals to input data about a patient’s diagnosis and treatment [1]. For the most part, modern EHRs act as systems of data collection, not systems of data engagement and reflective practice by end users such as health professionals and healthcare organisations.
Harnessing Electronic Health Records for Reflective Practice
Critiques of EHR design have highlighted flaws that hinder their use for professional development and reflection. Of particular note is the criticism that the design of many EHRs creates undesirable cognitive burdens. These burdens include information overload, problems of situational awareness due to fragmented presentation of data and increasing cognitive demands through actions such as having to click through multiple screens to navigate systems [43]. Furthermore, EHR design does not account for the nature of collaborative clinical work and can therefore be particularly poor at supporting team-cognition [43]. These design problems may be exacerbated by weaknesses in user testing to evaluate technology interfaces. Such testing often fails to go beyond studies with individual health professionals. Yet these technologies are frequently used by healthcare teams; teams typically have different usability needs from individual practitioners. A recent review of EHR design identified the following common usability issues: naturalness, consistency, preventing errors, minimising cognitive load, efficient interaction, forgiveness and feedback, effective use of language, effective information presentation and customisation/flexibility [44]. Guidelines for addressing cognitive load seem particularly important for supporting reflective practice. Specifically, these include the guidelines for (a) the design of the EHR interfaces include minimising users’ mental workload; (b) identifying the consequences of the users’ actions, so they can prevent future errors or make informed decisions about their practice; and (c) allowing users to customise information content delivered to them [44].
Considerable research has been undertaken into understanding the factors that enable health professionals to maintain clinical knowledge and competency [45–48]. It has been established that many adult learners value training and education that feels both authentic and is aligned with their experiences in the real world. The literature suggests that personal learning aligned to the learners’ experience is more impactful. For health professionals, the role of adaption has been noted through the Master Adaptive Learner (MAL) Framework [49], which can be used to guide skills acquisition by health professionals, with an emphasis on learners being adaptive in order to develop new clinical skills. The capacity of health professionals to act as adaptive learners was severely tested during the COVID pandemic [50]. Data captured within EHRs has a potential to support this learning adaptation. This is because the data could characterise different aspects of professional practice and by personalising learning for individual practitioners.
The physician feedback model (PFM) [51] describes the processes that health professionals use to reflect on their practice based on feedback and how they translate this into behaviour change. Although not designed to describe feedback derived from an EHR, the model provides an effective framing mechanism for understanding the process of reviewing EHR data, reflecting on practice and acting on that reflection if required. The PFM has three components to describe feedback to health professionals: (1) reaction — health professionals’ acceptance of clinical-performance feedback; (2) action — the behaviours health professionals engaging in after receiving feedback; and (3) impact — how a health professional translates feedback into patient-management behaviour. Consideration of the components of the PFM could help inform the design of EHR systems to support reflective practice and also support understanding of how health professionals might use EHR data. For EHR system design, the reaction component of the model suggests that effective feedback systems should contain data from a respected source, incorporate content that is relevant and present feedback in a timely/personalised manner. The action component of the model explains that health professionals will take three categories of action in response to feedback: (i) retroactive acts — revisiting previously seen patient interactions to correct a problem; (ii) proactive acts — focusing on changing interactions with future patients; and (iii) defensive acts — trying to justify performance. The first two acts are more conducive to a health professional accepting feedback, so it would be important to facilitate such reactions when using EHR data to give performance feedback. The impact component of the model suggests there are multiple factors that might influence whether a health professional changes their clinical practice behaviour based on feedback including their core values, emotional response and environmental factors.
The current design of EHRs does little to support such workplace-based learning by health professionals; ideal design of EHRs that would support learning is unclear. There are several key recommendations that if adopted could improve the utility of EHRs to support practice reflection and learning. A first recommendation would be for vendors to prioritise development and implementation of EHRs that are also tools for documenting health professional learning [40] and not just for documenting patient care [37]. A second recommendation would be for EHR designers to be guided by the principles of the effective feedback, such as those described in the PFM, as outlined above [51]. Designing such an approach is likely complex as it may need to account for issues related to data quality and completeness that are currently a challenge for the healthcare sector [52]. A third recommendation is to explore the application of machine learning to the plethora of structured and unstructured data in EHRs to help develop smarter profiles of health professional clinical practice and map such data to create individual clinical practice models to support learning.
It is likely that EHR design may need to scaffold people in using the data and to personalise workplace learning to be delivered when and in a way the individual is most receptive to change. Such scaffolding has potential to help health professionals understand and enhance their learning, as well as track and assess their learning progression over time. Promising scaffolding approaches include comparing current and historical performance to track performance changes over time, comparing performance against peers using metrics according to stage of training/experience, and using EHR data to compare performance against a defined standard [53]. Redesigned EHRs may automatically accumulate evidence that continuing professional development requirements have been achieved, a proposal that has have already been noted in the literature [40]. Coupled with this, designers of EHRs that support learners may need to think beyond the specific information system, to the healthcare context they are implemented in.
Whilst EHR design has a long way to go if it is to support learning, there is an equally large gap in understanding when and how health professionals want technology to help them to reflect on their clinical practice. The processes health professionals use to reflect on feedback are described in the PFM [51]. What is not well understood is the role of technology in supporting or disrupting the processes described in models such as the PFM. The importance of considering adoption enablers and barriers of such systems is highlighted in the mixed adoption by health professionals of EHR alerts [54]. Such alerts are intended to prompt reflective practice at the point of decision making. Considering both the technological and human factors will be critical for the repurposing of EHRs to support reflective practice.
Conclusions
Addressing the suboptimal use of EHRs in supporting learning and reflective practice is important due to the disruption occurring in the health sector related to both the design of informatics technology and changes in policy about the use of routinely collected data to reflect on clinical practice [55]. Perhaps more importantly, this gap should be addressed urgently because EHR data has the potential to transform health professionals’ learning by strengthening processes that are known to improve clinical performance by health professionals and potentially reducing time spent on activities that do not change behaviour or improve care. EHRs that are designed to support professional learning have the potential to facilitate feedback of outcomes data to health professionals, so that they have access to objective information and patient narratives that can be used for self-evaluation of clinical performance [6]. Furthermore, EHR data has potential to link clinical outcomes with learning activities and guide health professionals towards training that is also likely to influence patients’ quality of care [56].
Given the considerable potential of EHRs that scaffold health professional learning, and the growth of open source and non-enterprise EHRs [57], why are there no examples of ones that do this? Is this a blind spot that today’s EHR vendors have thus far overlooked that will in future be remedied? Does the gap represent a complex design problem that no one has yet been able to address? What is the role of cost as a barrier to develop EHRs that truly support practitioner learning? It is likely that the solution lies in answering not one but all of these questions. Whilst the gap remains, there is a significant missed opportunity in the digital health sector: EHRs that support reflective practice and transform learning for health professionals.
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions.
Declarations
Competing Interests
Author AJ is undertaking a postdoctoral research fellowship that is fully funded through the Digital Health CRC (Cooperative Research Centre). Author TS is an Academic Lead for the Digital Health CRC. The DHCRC is established and supported under the Australian Government’s Cooperative Research Centres Program. Authors AJ, JK, ST, MP, RB, RC, DG, and TS report no conflicts of interest.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Change history
2/20/2023
Missing Open Access funding information has been added in the Funding Note.
References
- 1.Alpert JS. The electronic medical record in 2016: advantages and disadvantages. Digital Medicine. 2016;2(2):48. doi: 10.4103/2226-8561.189504. [DOI] [Google Scholar]
- 2.Amulya J (2004) What is reflective practice. Center for Reflective Community Practice, Massachusetts Institute of Technology, Cambridge, MA.[Online]
- 3.Schön DA. The reflective practitioner: how professionals think in action. New York, NY: Basic Books; 1983. [Google Scholar]
- 4.Mann K, Gordon J, MacLeod A. Reflection and reflective practice in health professions education: a systematic review. Adv Health Sci Educ. 2009;14(4):595–621. doi: 10.1007/s10459-007-9090-2. [DOI] [PubMed] [Google Scholar]
- 5.Jayatilleke N, Mackie A. Reflection as part of continuous professional development for public health professionals: a literature review. J Public Health. 2013;35(2):308–312. doi: 10.1093/pubmed/fds083. [DOI] [PubMed] [Google Scholar]
- 6.Cifra CL, Sittig DF, Singh H. Bridging the feedback gap: a sociotechnical approach to informing clinicians of patients’ subsequent clinical course and outcomes. BMJ Qual Saf. 2021;30(7):591–597. doi: 10.1136/bmjqs-2020-012464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Davenport TH, Hongsermeier T, Mc Cord KA. Using AI to improve electronic health records. Harv Bus Rev. 2018;12:1–6. [Google Scholar]
- 8.Kukafka R, Ancker JS, Chan C, Chelico J, Khan S, Mortoti S, Natarajan K, Presley K, Stephens K. Redesigning electronic health record systems to support public health. J Biomed Inform. 2007;40(4):398–409. doi: 10.1016/j.jbi.2007.07.001. [DOI] [PubMed] [Google Scholar]
- 9.Robichaux C, Tietze M, Stokes F, McBride S. Reconceptualizing the electronic health record for a new decade: a caring technology? Adv Nurs Sci. 2019;42(3):193–205. doi: 10.1097/ANS.0000000000000282. [DOI] [PubMed] [Google Scholar]
- 10.Glaser J (2020) Its time for a new kind of electronic health record. Harvard Business Review June 2020, 12
- 11.Kyaw BM, Saxena N, Posadzki P, Vseteckova J, Nikolaou CK, George PP, Divakar U, Masiello I, Kononowicz AA, Zary N. Virtual reality for health professions education: systematic review and meta-analysis by the digital health education collaboration. J Med Internet Res. 2019;21(1):e12959. doi: 10.2196/12959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Corral J (2021) Artificially intelligent chatbots for health professions education. In: Digital innovations in healthcare education and training. edn.: Elsevier; 127–135
- 13.Australia MBo (2017) Building a professional performance framework. 2017
- 14.Archer J, Bloor K, Bojke C, Boyd A, Bryce M, Ferguson J, Gutacker N, Hillier C, Luscombe K, Price T (2018) Evaluating the development of medical revalidation in England and its impact on organisational performance and medical practice: overview report. Evaluating the development of medical revalidation in England and its impact on organisational performance and medical practice: overview report 2018
- 15.Cristina P. A digital (r)evolution: introducing The Lancet Digital Health. Lancet Digit Health. 2019;1:1. doi: 10.1016/S2589-7500(19)30010-X. [DOI] [PubMed] [Google Scholar]
- 16.Shaw T, McGregor D, Brunner M, Keep M, Janssen A, Barnet S. What is eHealth (6)? Development of a conceptual model for eHealth: qualitative study with key informants. J Med Internet Res. 2017;19(10):e324. doi: 10.2196/jmir.8106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Health TLD. Reflecting on a future ready for digital health. The Lancet Digital Health. 2020;2(5):e209. doi: 10.1016/S2589-7500(20)30087-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Baysari MT, Zheng WY, Van Dort B, Reid-Anderson H, Gronski M, Kenny E. A late attempt to involve end users in the design of medication-related alerts: survey study. J Med Internet Res. 2020;22(3):e14855. doi: 10.2196/14855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Peute LW, Lichtner V, Baysari MT, Hägglund M, Homco J, Jansen-Kosterink S, Jauregui I, Kaipio J, Kuziemsky CE, Lehnbom EC. Challenges and best practices in ethical review of human and organizational factors studies in health technology: a synthesis of testimonies. Yearb Med Inform. 2020;29(01):058–070. doi: 10.1055/s-0040-1701979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Greenhalgh T, Wherton J, Papoutsi C, Lynch J, Hughes G, Hinder S, Fahy N, Procter R, Shaw S. Beyond adoption: a new framework for theorizing and evaluating nonadoption, abandonment, and challenges to the scale-up, spread, and sustainability of health and care technologies. J Med Internet Res. 2017;19(11):e367. doi: 10.2196/jmir.8775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chew DP, Hyun K, Morton E, Horsfall M, Hillis GS, Chow CK, Quinn S, D’Souza M, Yan AT, Gale CP. Objective risk assessment vs standard care for acute coronary syndromes: a randomized clinical trial. JAMA Cardiol. 2021;6(3):304–313. doi: 10.1001/jamacardio.2020.6314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pontefract S, Wilson K. Using electronic patient records: defining learning outcomes for undergraduate education. BMC Med Educ. 2019;19(1):1–8. doi: 10.1186/s12909-019-1466-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Boonstra A, Versluis A, Vos JF. Implementing electronic health records in hospitals: a systematic literature review. BMC Health Serv Res. 2014;14(1):1–24. doi: 10.1186/1472-6963-14-370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cresswell K, Sheikh A, Krasuska M, Heeney C, Franklin BD, Lane W, Mozaffar H, Mason K, Eason S, Hinder S. Reconceptualising the digital maturity of health systems. Lancet Digital Health. 2019;1(5):e200–e201. doi: 10.1016/S2589-7500(19)30083-4. [DOI] [PubMed] [Google Scholar]
- 25.Mc Cord KA, Hemkens LG. Using electronic health records for clinical trials: where do we stand and where can we go? CMAJ. 2019;191(5):E128–E133. doi: 10.1503/cmaj.180841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Claire Simon K, Hentati A, Rubin S, Franada T, Maurer D, Hillman L, Tideman S, Szela M, Meyers S, Frigerio R. Successful utilization of the EMR in a multiple sclerosis clinic to support quality improvement and research initiatives at the point of care. Mult Scler J Exp Transl Clin. 2018;4(4):2055217318813736. doi: 10.1177/2055217318813736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Berman L, Duffy B, Brenn BR, Vinocur C. MyPOD: an EMR-based tool that facilitates quality improvement and maintenance of certification. J Med Syst. 2017;41(3):39. doi: 10.1007/s10916-017-0686-7. [DOI] [PubMed] [Google Scholar]
- 28.Bora A, Balasubramanian S, Babenko B, Virmani S, Venugopalan S, Mitani A, de Oliveira MG, Cuadros J, Ruamviboonsuk P, Corrado GS. Predicting the risk of developing diabetic retinopathy using deep learning. Lancet Digital Health. 2021;3(1):e10–e19. doi: 10.1016/S2589-7500(20)30250-8. [DOI] [PubMed] [Google Scholar]
- 29.Jones MS, Goley AL, Alexander BE, Keller SB, Caldwell MM, Buse JB. Inpatient transition to virtual care during COVID-19 pandemic. Diabetes Technol Ther. 2020;22(6):444–448. doi: 10.1089/dia.2020.0206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Shaw T, Janssen A, Crampton R, O’Leary F, Hoyle P, Jones A, Shetty A, Gunja N, Ritchie AG, Spallek H. Attitudes of health professionals to using routinely collected clinical data for performance feedback and personalised professional development. Med J Aust. 2019;210:S17–S21. doi: 10.5694/mja2.50022. [DOI] [PubMed] [Google Scholar]
- 31.Chaiyachati KH, Shea JA, Asch DA, Liu M, Bellini LM, Dine CJ, Sternberg AL, Gitelman Y, Yeager AM, Asch JM. Assessment of inpatient time allocation among first-year internal medicine residents using time-motion observations. JAMA Intern Med. 2019;179(6):760–767. doi: 10.1001/jamainternmed.2019.0095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Car LT, Soong A, Kyaw BM, Chua KL, Low-Beer N, Majeed A. Health professions digital education on clinical practice guidelines: a systematic review by Digital Health Education collaboration. BMC Med. 2019;17(1):1–16. doi: 10.1186/s12916-019-1370-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kuo AM-S, Thavalathil B, Elwyn G, Nemeth Z, Dang S. The promise of electronic health records to promote shared decision making: a narrative review and a look ahead. Med Decision Making. 2018;38(8):1040–1045. doi: 10.1177/0272989X18796223. [DOI] [PubMed] [Google Scholar]
- 34.Berner ES, Detmer DE, Simborg D. Will the wave finally break? A brief view of the adoption of electronic medical records in the United States. J Am Med Inform Assoc. 2005;12(1):3–7. doi: 10.1197/jamia.M1664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Organization WH (2017) Global diffusion of eHealth: making universal health coverage achievable: report of the third global survey on eHealth: World Health Organization; 2017
- 36.Menachemi N, Collum TH. Benefits and drawbacks of electronic health record systems. Risk Manage Healthcare Policy. 2011;4:47. doi: 10.2147/RMHP.S12985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Schofield P, Shaw T, Pascoe M. Toward comprehensive patient-centric care by integrating digital health technology with direct clinical contact in Australia. J Med Internet Res. 2019;21(6):e12382. doi: 10.2196/12382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Jones SS, Rudin RS, Perry T, Shekelle PG. Health information technology: an updated systematic review with a focus on meaningful use. Ann Intern Med. 2014;160(1):48–54. doi: 10.7326/M13-1531. [DOI] [PubMed] [Google Scholar]
- 39.Walsh SH. The clinician’s perspective on electronic health records and how they can affect patient care. BMJ. 2004;328(7449):1184–1187. doi: 10.1136/bmj.328.7449.1184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Grad RM, Pluye P, Shulha M, Tang DL, Tu K, Goodman K, Meuser J. EBM, CME and the EMR. BMJ Evidence-Based Med. 2014;19(1):1–3. doi: 10.1136/eb-2013-101231. [DOI] [PubMed] [Google Scholar]
- 41.Janssen A, Donnelly C, Elder E, Pathmanathan N, Shaw T. Electronic medical record implementation in tertiary care: factors influencing adoption of an electronic medical record in a cancer centre. BMC Health Serv Res. 2021;21(1):1–9. doi: 10.1186/s12913-020-06015-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Fennelly O, Cunningham C, Grogan L, Cronin H, O’Shea C, Roche M, Lawlor F, O’Hare N (2020) Successfully implementing a national electronic health record: a rapid umbrella review. International Journal of Medical Informatics 2020:104281 [DOI] [PMC free article] [PubMed]
- 43.Beasley JW, Holden RJ, Sullivan F (2011) Electronic health records: research into design and implementation. In.: British Journal of General Practice; 2011 [DOI] [PMC free article] [PubMed]
- 44.Zahabi M, Kaber DB, Swangnetr M. Usability and safety in electronic medical records interface design: a review of recent literature and guideline formulation. Hum Factors. 2015;57(5):805–834. doi: 10.1177/0018720815576827. [DOI] [PubMed] [Google Scholar]
- 45.Lauer AK, Lauer DA (2017) The good doctor: more than medical knowledge & surgical skill. Annals of eye science 2017, 2 [DOI] [PMC free article] [PubMed]
- 46.Galvin E, Wiese A, Dahly D, O’Farrell J, Cotter J, Bennett D. Maintenance of professional competence in Ireland: a national survey of doctors’ attitudes and experiences. BMJ Open. 2020;10(12):e042183. doi: 10.1136/bmjopen-2020-042183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wiese A, Galvin E, O’Farrell J, Cotter J, Bennett D. Doctors’ maintenance of professional competence: a qualitative study informed by the theory of planned behaviour. BMC Health Serv Res. 2021;21(1):1–10. doi: 10.1186/s12913-021-06438-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Gunawan J, Aungsuroch Y, Fisher ML, Marzilli C, Liu Y. Factors related to the clinical competence of registered nurses: systematic review and meta-analysis. J Nurs Scholarsh. 2020;52(6):623–633. doi: 10.1111/jnu.12594. [DOI] [PubMed] [Google Scholar]
- 49.Cutrer WB, Miller B, Pusic MV, Mejicano G, Mangrulkar RS, Gruppen LD, Hawkins RE, Skochelak SE, Moore DE., Jr Fostering the development of master adaptive learners: a conceptual model to guide skill acquisition in medical education. Acad Med. 2017;92(1):70–75. doi: 10.1097/ACM.0000000000001323. [DOI] [PubMed] [Google Scholar]
- 50.Goldhamer MEJ, Pusic MV, Co JPT, Weinstein DF. Can covid catalyze an educational transformation? Competency-based advancement in a crisis. N Engl J Med. 2020;383(11):1003–1005. doi: 10.1056/NEJMp2018570. [DOI] [PubMed] [Google Scholar]
- 51.Payne VL, Hysong SJ. Model depicting aspects of audit and feedback that impact physicians’ acceptance of clinical performance feedback. BMC Health Serv Res. 2016;16(1):1–12. doi: 10.1186/s12913-016-1486-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Singer A, Yakubovich S, Kroeker AL, Dufault B, Duarte R, Katz A. Data quality of electronic medical records in Manitoba: do problem lists accurately reflect chronic disease billing diagnoses? J Am Med Inform Assoc. 2016;23(6):1107–1112. doi: 10.1093/jamia/ocw013. [DOI] [PubMed] [Google Scholar]
- 53.Sebok-Syer SS, Goldszmidt M, Watling CJ, Chahine S, Venance SL, Lingard L. Using electronic health record data to assess residents’ clinical performance in the workplace: the good, the bad, and the unthinkable. Acad Med. 2019;94(6):853–860. doi: 10.1097/ACM.0000000000002672. [DOI] [PubMed] [Google Scholar]
- 54.Ancker JS, Edwards A, Nosal S, Hauser D, Mauer E, Kaushal R. Effects of workload, work complexity, and repeated alerts on alert fatigue in a clinical decision support system. BMC Med Inform Decis Mak. 2017;17(1):1–9. doi: 10.1186/s12911-017-0430-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ellaway RH, Topps D, Pusic M. Data, big and small: emerging challenges to medical education scholarship. Acad Med. 2019;94(1):31–36. doi: 10.1097/ACM.0000000000002465. [DOI] [PubMed] [Google Scholar]
- 56.Fidopiastis CM, Venta KE, Baker EG, Stanney KM. A step toward identifying sources of medical errors: modeling standards of care deviations for different disease states. Military Med. 2018;183(suppl_1):105–110. doi: 10.1093/milmed/usx203. [DOI] [PubMed] [Google Scholar]
- 57.Kiah MLM, Haiqi A, Zaidan B, Zaidan A. Open source EMR software: profiling, insights and hands-on analysis. Comput Methods Programs Biomed. 2014;117(2):360–382. doi: 10.1016/j.cmpb.2014.07.002. [DOI] [PubMed] [Google Scholar]