Abstract
Study Objectives:
Polysomnograms (PSGs) collect a plethora of physiologic signals across the night. However, few of these PSG data are incorporated into standard reports, and hence, ultimately, under-utilized in clinical decision making. Recently, there has been substantial interest regarding novel alternative PSG metrics that may help to predict obstructive sleep apnea (OSA)–related outcomes better than standard PSG metrics such as the apnea-hypopnea index. We systematically review the recent literature for studies that examined the use of alternative PSG metrics in the context of OSA and their association with health outcomes.
Methods:
We systematically searched EMBASE, MEDLINE, and the Cochrane Database of Systematic Reviews for studies published between 2000 and 2022 for those that reported alternative metrics derived from PSG in adults and related them to OSA-related outcomes.
Results:
Of the 186 initial studies identified by the original search, data from 31 studies were ultimately included in the final analysis. Numerous metrics were identified that were significantly related to a broad range of outcomes. We categorized the outcomes into 2 main subgroups: (1) cardiovascular/metabolic outcomes and mortality and (2) cognitive function– and vigilance-related outcomes. Four general categories of alternative metrics were identified based on signals analyzed: autonomic/hemodynamic metrics, electroencephalographic metrics, oximetric metrics, and respiratory event–related metrics.
Conclusions:
We have summarized the current landscape of literature for alternative PSG metrics relating to risk prediction in OSA. Although promising, further prospective observational studies are needed to verify findings from other cohorts, and to assess the clinical utility of these metrics.
Citation:
Hajipour M, Baumann B, Azarbarzin A, et al. Association of alternative polysomnographic features with patient outcomes in obstructive sleep apnea: a systematic review. J Clin Sleep Med. 2023;19(2):225–242.
Keywords: alternative metrics, sleep apnea, apnea-hypopnea index, outcomes, polysomnogram
BRIEF SUMMARY
Current Knowledge/Study Rationale: There is a need to identify which patients with obstructive sleep apnea (OSA) are at greater risk of adverse outcomes. Novel alternative metrics derived from the polysomnogram (PSG) may help to risk-stratify patients and provide a more nuanced description of their disease.
Study Impact: In this systematic review, we have summarized the current landscape for alternative PSG metrics relating to risk prediction in OSA. We identified many alternative metrics that could be promising; these included autonomic/hemodynamic metrics, electroencephalogram-related metrics, oximetry metrics, and respiratory event–related metrics.
INTRODUCTION
Obstructive sleep apnea (OSA) is a common respiratory disease that affects approximately 1 billion adults worldwide.1 OSA is associated with multiple adverse outcomes, including daytime sleepiness, reduced quality of life, motor vehicle crashes, occupational injuries, hypertension, cancer, cardiovascular disease (CVD), arrhythmias, kidney disease, cognitive dysfunction (dementia), and all-cause mortality.2
When OSA is suspected, patients often undergo a polysomnogram (PSG), an overnight sleep study in which a plethora of raw physiologic data are continuously collected including electroencephalography (EEG), electrocardiogram (ECG), oxygen saturation using photoplethysmography, airflow, snoring, chin/limb electromyography (EMG), eye movements, and chest wall/abdominal movements. These PSGs are scored visually by technicians to ascertain sleep stages and respiratory events. Since the 1990s, key metrics of OSA severity derived from the PSG include the apnea-hypopnea index (AHI) and simple indices of arterial desaturation such as the oxygen desaturation index (ODI) and percentage of time spent below an oxygen saturation threshold (eg, 88% or 90%).3
However, current PSG metrics, such as AHI, are not strongly associated with OSA-related adverse outcomes including symptoms, objective daytime function, and long-term health complications. There has thus been substantial interest in alternative PSG metrics to better quantify the severity of OSA and predict the presence or incidence of adverse OSA-related outcomes.4 These types of metrics may thus provide the opportunity to risk-stratify patients for more aggressive therapy for OSA and other risk factors, contributing to a precision care approach. These metrics may help to select individuals who would be at increased risk of adverse outcomes (eg, cardiovascular [CV] events) who might then be preferentially recruited into randomized controlled trials.
The objective of this study was to systematically review the recent literature for studies that examined the use of alternative PSG metrics in the context of OSA and their association with health outcomes. In this context, an alternative metric was defined as one not typically reported in clinical PSG reports.
METHODS
This study was performed in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.5
Eligibility criteria
Inclusion criteria
Studies were included in this review if they (1) referenced an alternative metric elicited from PSG (either attended level 1 or unattended level 2), (2) reported an outcome that was patient-centered (eg, symptoms, mortality, CV outcomes), and (3) were published in the English language as full papers (ie, not as abstracts).
Exclusion criteria
Studies were excluded if they (1) referenced metrics that are typically reported from PSG (eg, AHI, rapid eye movement [REM]/non-REM [NREM] AHI, ODI, lowest oxygen saturation, arousal index, standard sleep architecture), (2) did not derive data from full PSG studies (eg, used level 3 studies or oximetry), (3) focused on pediatric patients, (4) focused on narrow populations (eg, spinal cord injuries, pregnant women, underlying lung disease), and (5) only compared the metric(s) to AHI without patient-specific outcomes. We also excluded studies that focused on advanced OSA physiologic endotyping (eg, arousal threshold, loop gain) as these are currently challenging to measure from PSG and were felt to be beyond the scope of this review.6,7 Moreover, we excluded studies that assessed the role of therapy (continuous positive airway pressure [CPAP]) on health outcomes.
Search strategy and selection criteria
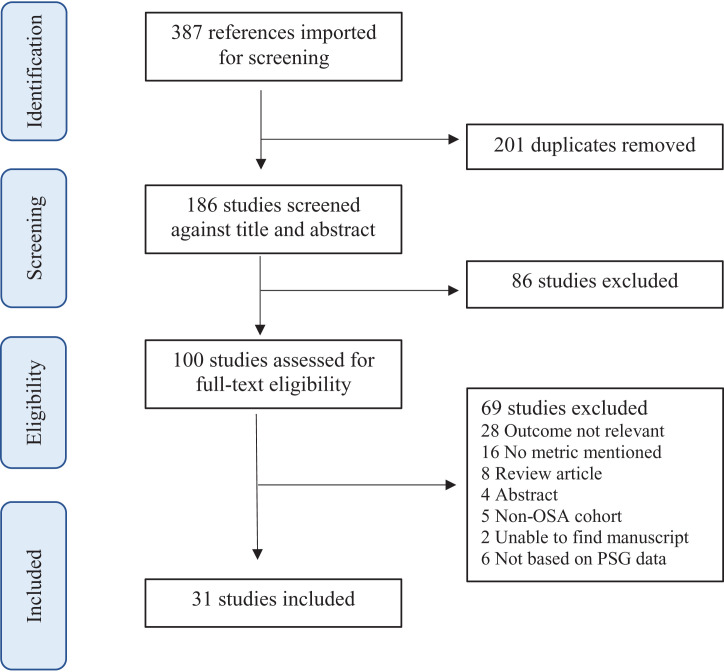
We systematically searched EMBASE, MEDLINE, and the Cochrane Database of Systematic Reviews from January 1, 2000, to April 1, 2022, using a broad search strategy and included keywords such as “obstructive sleep apnea” AND “polysomnogram” with alternative metrics. Details of the search strategy are presented in Table S1 (181.8KB, pdf) in the supplemental material. We limited the search to the above dates to reflect modern OSA diagnostic practices. Potentially relevant articles were accessed for full-text review. Citations from eligible articles were also searched to identify other potentially relevant studies. A flow chart of identified studies is presented in Figure 1.
Figure 1. PRISMA flow chart of identified studies, excluded and included.
PRISMA = Preferred Reporting Items for Systematic Reviews and Meta-Analyses
Three authors (M.H., B.B., and N.T.A.) conducted the literature search and extracted the data. The search strategy and items for data extraction were predefined and agreed upon by the authors. Variables that were extracted from each study included the following: year of publication, country of study, data sources, the metric used, mean AHI, mean body mass index (BMI), sex breakdown, mean age, study endpoints, sample size, and major results.
RESULTS
Study selection
A total of 387 articles were identified. After duplicates were removed, 186 papers remained. Of the 186 unique studies identified in our search, 100 qualified for full-text review, of which 31 were included in the final data extraction (see Figure 1). The extracted data from these 31 studies are described in Table 1, Table 2, Table 3, and Table 4. Of the 31 papers included in the final review, 12 were from the United States, 5 from Australia, and the remaining countries of origin varied with representation from Finland, France, Sweden, Switzerland, Singapore, Germany, Spain, China, and Saudi Arabia. The sample size ranged from 40 participants54 to 8,001 participants.33 Additionally, JBI (Joanna Briggs Institute) checklists for analytical cross-sectional and cohort studies were used to further evaluate the studies.8 All studies met the components of checklists, except for 1 study in which the authors did not control the analysis for the confounders.46
Table 1.
Studies assessing autonomic/hemodynamic metrics.
| Study | Study Size/Type | Type of PSG (Level 1 or 2) | Sex (% male) | Mean BMI (kg/m2) | Mean AHI (/h) | Mean Age (years) | % OSA Participants | Metric | Outcome | Results |
|---|---|---|---|---|---|---|---|---|---|---|
| Thomas (2009)28 USA | 5247/Retro of Pros | 1 | 51.6 | 28.7 | 9.1 | 62.2 | 47.6 | CPC (e-LFCNB) | CV outcomes | Elevated LFCNB, was associated with greater severity of sleep apnea and fragmented sleep. After adjustment for potential confounders, an independent association with prevalent hypertension and stroke was found. |
| Magnusdottir (2020)29 USA | 241/Retro of Pros | 2 | 73 | 34 | 25.5 | 63 | 100 | CPC | Nocturnal blood pressure response to CPAP | CPC-derived sleep quality impacted 24-h MAP and MDP, as well as BP during wake |
| Blanchard (2021)20 France | 7205/Retro of Pros | 2 | 62.3 | 29 | 22 | 60 | 86.7 | PRV | AF | PRV indices were independent predictors of AF incidence. |
| Azarbarzin (2021)9 USA | 5970/Retro of pros | 1 | MESA: 47.5 SHHS: 47.7 | MESA: 28.8 SHHS: 28.3 | MESA: 19.3 SHHS: 14.1 | MESA: 68.5 SHHS: 64.2 | MESA: 3.9 SHHS: 29 | ΔHR | CV disease and all-cause mortality | In MESA, HR was associated with NT-proBNP, coronary calcium, and Framingham risk, and in SHHS, individuals with a high ΔHR were at increased risk of nonfatal/fatal CVD and all-cause mortality |
| Kwon (2021)15 USA | 1407/Retro of Pros | 2 | 47.5 | 28.8 | 19.5 | 68.4 | Not referenced | PAT response | CV outcomes | Increase in average PAT response was associated with LV mass, CPB score, CAC prevalence and 18% higher risk of incident CVD |
| Alomri (2022)45 Saudi Arabia | 75/Retro | 1 | 70 | 33.2 | Not referenced | 41.1 | 84 | SBP derived from PAT | Cognitive dysfunction (Austin Maze test) | Nocturnal peaks in SBP and difference between resting and nocturnal peaks of SBP in OSA were associated with visuospatial dysfunction, even after controlling for age, smoking status, depressive symptoms, hypoxia, and sleep fragmentation |
| Trzepizur (2022)22 France | 5358/Retro of Pros | 2 | 63.66 | 30 | 27 | 60 | 100 | PRV | MACEs | PRV was not associated with MACEs. |
| Blanchard (2021)21 France | 3597/Retro of Pros | 2 | 63 | 28 | 20 | 58 | 85 | PRV | Risk of stroke incidence | Nighttime sympathetic/parasympathetic tone (PRV) was associated with stroke risk. |
| Hirotsu (2020)16 Switzerland | 2162/Cross-sectional | 2 | 49 | 26.2 | Not referenced | 57 | Not referenced | PWA | Hypertension, diabetes, and CV event | Independent association of PWA-drop features (lower frequency, longer duration, and greater area under the curve) with hypertension, diabetes, and CV events |
| Strassberger (2021)17 Sweden | 358/Retro | 1 | 64 | 30 | 13 | 55 | 100 | CRI | CV risk | Pulse wave analysis during sleep provides a powerful approach for cardiovascular risk assessment in addition to conventional sleep study parameters |
| Berger (2022)23 Switzerland | 1784/Retro of Pros | 1 | 48.2 | 26 | Not referenced | 58 | Not referenced | HRV | CVD | In a fully adjusted model, AC, DC, and HRF were the only HRV metrics significantly associated with incident CVD events |
AC = acceleration capacity, AF = atrial fibrillation, AHI = apnea-hypopnea index, BMI = body mass index, BP = blood pressure, CPB = carotid plaque burden, CPAP = continuous positive airway pressure, CPC = cardiopulmonary coupling, CRI = Cardiac Risk Index, CV = cardiovascular, CVD = cardiovascular disease, DC = deceleration capacity, e-LFCNB = narrow-band elevated low frequency coupling, HR = heart rate, HRV = heart rate variability, LV = Left Ventricular, MACE = major adverse cardiovascular event, MDP = mean diastolic blood pressure, MESA = Multi-Ethnic Study of Atherosclerosis, M/F = male/female, NT-proBNP = N-terminal prohormone BNP, ODI = oxygen desaturation index, OSA = obstructive sleep apnea, PAT = pulse arrival time, Pros = prospective, PRV = pulse rate variability, PSG = polysomnography, PWA = pulse wave amplitude, Retro = retrospective, Retro of Pros = retrospective analysis of prospective study, SBP = systolic blood pressure, SHHS = Sleep Heart Health Study.
Table 2.
Studies assessing EEG metrics.
| Study | Study Size/Type | Type of PSG (Level 1 or 2) | Sex (% male) | Mean BMI (kg/m2) | Mean AHI (/h) | Mean Age (years) | % OSA Participants | Metric | Outcome | Results |
|---|---|---|---|---|---|---|---|---|---|---|
| Schwartz (2006)50 Germany | 100/Cross-sectional | 1 | Not referenced | Not referenced | Not referenced | Not referenced | Not referenced | Arousal duration | ESS | Longer arousals correlated more strongly with ESS than the frequency or time attributable to the more numerous brief arousals. |
| Vakulin (2016)49 Australia | 76/Cross-sectional | 1 | 81 | 32.2 | 29.8 | 42.8 | 100 | EEG power Spectrum analysis | Driving simulator performance | Among clinical and quantitative EEG variables, significant predictors of worse steering deviation were total EEG power during NREM and REM sleep, beta EEG power in NREM and delta EEG power in REM and sleep onset latency. |
| Azarbarzin (2020)46 USA | 1378/Retro of Pros | 1 | 67.6 | 30 | 22 | 65 | 100 | LR-ORP | Risk of car crash | Compared to the lowest quartile of sleep depth coherence, individuals in the highest quartile had a 62% lower risk of accident. |
| Kim (2021)31 USA | 2055/Cross-sectional | 1 | 46 | 14.8 | 28.7 | 68.4 | Not referenced | ORP | Hypertension | ORP was not associated with blood pressure changes |
| Lechat (2021)32 Australia | 5084/Retro of Pros | 1 | 47.3 | 28.1 | 9.9 | 63 | Not referenced | Delta EEG power | All-cause mortality | Disrupted delta EEG power during sleep was associated with a 32% increased risk of all-cause mortality compared with no fragmentation. |
| Djonlagic (2021)47 USA | 3819/Retro of Pros | 2 | MESA:48 MrOS: 100 | Not referenced | Not referenced | Not referenced | Not referenced | EEG Metrics | Cognitive performance MESA: DSCT, CASI, DSF, DSB MrOS: Trails B, 3MS, DVT | Cognitive performance was related to sleep across macro architecture and multiple spectral, spindle, SO and spindle–SO coupling domains. Associated metrics fell across at least three broad classes. |
| Shahrbabaki (2021)33 Australia | 8001/Retro of Pros | SHHS:1 MrOS:2 SOF:2 | 62.5 | MrOS:27.2 SHHS:28.3 SOF:27.7 | MrOS:20.1 SHHS:9.5 SOF:27.6 | MrOS:76.6 SHHS: 64 SOF:82.9 | Not referenced | AB | Mortality: all cause and CV | In women, AB was associated with all-cause mortality and CV mortality. In men, it was not clear (results were reverse in SHHS and MrOS) |
| McCloy (2021)48 Australia | 190/Retro | 1 | 61 | 36.5 | 28.5 | 56 | 100 | SBI | Vigilance | SBI used to model sleep spindle characteristics to PVT indices and the proposed model were able to detect patients with vigilance marker |
| Duce (2021)51 Australia | 65/Retro | 1 | 55 | 31.7 | 26.1 | 53 | 100 | Arousal duration | Cognitive outcomes | PVT impaired group had more EEG arousals greater than 5 s, 7 s, and 15 s in duration. |
AB = arousal burden, AHI = apnea-hypopnea index, BMI = body mass index, CASI = Cognitive Abilities Screening Instrument, DSB = Digit Span Test (backward), DSCT = Digit Symbol Coding Test, DSF = Digit Span Test (forward), DVT = Digit Vigilance Test, EEG = electroencephalography, ESS = Epworth Sleepiness Scale, MESA = Multi-Ethnic Study of Atherosclerosis, MrOS = Osteoporotic Fractures in Men Study, NREM = non–rapid eye movement, ODI = oxygen desaturation index, ORP = odds ratio product, OSA = obstructive sleep apnea, Pros = prospective, PSG = polysomnography, PVT = Psychomotor Vigilance Test, RDI = respiratory disturbance index, REM = rapid eye movement, Retro = retrospective, Retro of Pros = retrospective analysis of prospective study, SBI = spindle burst characteristics, SD = standard deviation, SHHS = Sleep Heart Health Study, SO = slow oscillation, SOF = Study of Osteoporotic Fractures, SWA = slow-wave activity, 3MS = Mini-Mental State Examination.
Table 3.
Studies assessing oximetric metrics.
| Study | Study Size/Type | Type of PSG (Level 1 or 2) | Sex (% male) | Mean BMI (kg/m2) | Mean AHI (/h) | Mean Age (years) | % OSA Participants | Metric | Outcome | Results |
|---|---|---|---|---|---|---|---|---|---|---|
| Azarbarzin (2019)36 USA | 7854/Retro of Pros | MrOS: 2 SHHS: 1 | MrOS: 100 SHHS: 45.3 | MrOS: 27.2 SHHS: 28.3 | MrOS: 15.7 SHHS: 17.1 | MrOS: 74.3 SHHS: 61.0 | MrOS: 39.8 SHHS: 26 | HB | CVD mortality and all-cause mortality | Individuals in the MrOS study with hypoxic burden in the highest 2 quintiles had hazard ratios of 1.81 and 2.73, respectively, compared with the first quintile for CV-related mortality. The group in the SHHS with HB in the highest quintile had a hazard ratio of 1.96 for CV-related mortality. |
| Azarbarzin (2020)37 USA | 7534/Retro of Pros | MrOS: 2 SHHS: 1 | MrOS: 100 SHHS: 45.3 | MrOS: 27.1 SHHS:28.3 | MrOS: 11.4 SHHS: 8.6 | MrOS: 76.2 SHHS: 63.6 | Not referenced | HB | HF | The sleep HB was associated with incident HF in men in 2 independent cohorts. Moreover, HB predicted incident HF in groups with both high and low AHI levels. |
| Azarbarzin (2021)9 USA | 5970/Retro of Pros | 1 | MESA: 47.5 SHHS: 47.7 | MESA: 28.8 SHHS: 28.3 | MESA: 19.3 SHHS: 14.1 | MESA: 68.5 SHHS: 64.2 | MESA: 3.9 SHHS: 28 | HB | CVD and all-cause mortality | Relationship between delta HR and fatal CVD or all-cause mortality was strengthened in patients with a high HB. They also noted no association between a high delta HR and fatal CVD or all-cause mortality in those with a low HB. |
| Jackson (2021)38 USA | 1895/Retro of Pros | 2 | 46.3 | 28.8 | Not referenced | 68.2 | Not referenced | HB | Chronic kidney disease | ASHB was associated with moderate-to-severe CKD. Black women in highest vs lowest quantile of ASHB also had a higher CKD prevalence. |
| Kim (2021)31 USA | 2055/Cross-sectional | 1 | 46/54 | 28.7 | 14.8 | 68.4 | Not referenced | HB | Hypertension | Higher burden was associated with higher BP. |
| Trzepizur (2022)22 France | 5358/Retro of Pros | 2 | 63.66/36.34 | 30 | 27 | 60 | 200 | HB | MACE | HB was an independent predictor of incident CV events and death. |
| Blanchard (2021)21 France | 3597/Retro of Pros | 2 | 63 | 28 | 20 | 58 | 85 | HB | Risk of stroke incidence | HB was associated with stroke risk in OSA patients. |
| de Chazal (2021)39 Australia | 4686/Retro of Pros | 2 | 48/52 | Not referenced | Not referenced | >40 | Not referenced | REDTA | CVD mortality | Hazard ratios in adjusted Cox analysis for predicting cardiovascular death using REDTA are up to 1.90 in the third quantile. |
| Wang (2020)41 China | 102/Cross-sectional | 1 | 67/33 | 29.5 | 63 | 100 | 50.3 | ODR | Hypertension | ODR was more strongly associated with elevation of BP and BPV in patients with severe OSA |
| Kwon (2021)42 USA | 2631/Retro of Pros | 2 | 100/0 | 27.2 | 18 | 76.4 | Not referenced | LFCt | CVD and all-cause mortality | LFCt was independently associated with both CV and all-cause mortality in older men with SDB, independent of both baseline CV burden and conventional SDB metrics. |
| Kainulainen (2020)52 Finland | 743/Retro | 1 | 58.7 | 35.1 | 23.7 | 56.8 | 100 | Desaturation severity, obstruction severity, respiratory event duration | PVT reaction time and the number of lapses | Desaturation severity is significantly associated with increased risk of impaired PVT performance. |
| Muraja-Murro (2013)43 Finland | 226/Retro | 1 | Not referenced | 29.3 | 19.5 | 54.6 | 38.8 | Desaturation severity, obstruction severity, respiratory event duration | Mortality | Obstruction severity was the only parameter which was related statistically significantly to mortality in the severe OSA category |
AHI = apnea-hypopnea index, BMI = body mass index, BP = blood pressure, BPV = blood pressure variability, CKD = chronic kidney disease, CV = cardiovascular, CVD = cardiovascular disease, HB = hypoxic burden, HF = heart failure, HR = heart rate, LFCt = lung to finger circulation time, MACE = major adverse cardiovascular event, MESA = Multi-Ethnic Study of Atherosclerosis, MrOS = Osteoporotic Fractures in Men Study, ODI = oxygen desaturation index, ODR = oxygen desaturation rate, OSA = obstructive sleep apnea, Pros = prospective, PSG = polysomnography, PVT = Psychomotor Vigilance Test, REDTA = Respiratory Event Desaturation Transient Area, Retro = retrospective, Retro of Pros = retrospective analysis of prospective study, SD = standard deviation, SDB = sleep-disordered breathing, SHHS = Sleep Heart Health Study.
Table 4.
Studies assessing respiratory event–related metrics.
| Study | Study Size/Type | Type of PSG (Level 1 or 2) | Sex (% male) | Mean BMI (kg/m2) | Mean AHI (/h) | Mean Age (years) | % OSA Participants | Metric | Outcome | Results |
|---|---|---|---|---|---|---|---|---|---|---|
| Goh (2018)53 Singapore | 821/Retro | 1 | 67 | 28 | 28 | 48 | 100 | Apneic and Hypopneic load | ESS | Linear regression analysis found age (P < .001), apnea load (P = .005), REM (P = .021) and stage 1 sleep duration (P = .042) were independent factors correlated to ESS. |
| Butler (2019)44 USA | 5712/Retro of Pros | 1 | 48 | 28.1 | 13.8 | 63.3 | 67 | Respiratory event duration | All-cause mortality | Individuals with the shortest-duration events had a significantly increased hazard ratio for all-cause mortality |
| Kim (2021)31 USA | 2055/Cross-sectional | 1 | 46 | 28.7 | 14.8 | 68.4 | Not referenced | Duty cycle and IFL | Hypertension | Higher duty cycle and IFL were associated with lower BP |
| Mediano (2007)54 Spain | 40/Retro | 1 | 100 | 32 | 61 | 50 | 100 | Apnea duration | EDS | Longer apnea duration can be a determinant of excessive daytime sleepiness in OSA patients |
AHI = apnea hypopnea index, BMI = body mass index, BP = blood pressure, EDS = excessive daytime sleepiness, ESS = Epworth Sleepiness Scale, IFL = inspiratory flow limitation, ODI = oxygen desaturation index, OSA = obstructive sleep apnea, Pros = prospective, PSG = polysomnography, RDI = respiratory disturbance index, REM = rapid eye movement, Retro = Retrospective, Retro of Pros = retrospective analysis of prospective study, SD = standard deviation.
Identification of alternative metrics
Of the 31 studies included in the extraction, we categorized the outcomes into 2 main subgroups (ie, 1) CV/metabolic outcomes and mortality, 2) cognitive function– and vigilance-related outcomes). Metrics were also grouped into 4 categories based on the signals used from PSG (autonomic/hemodynamic metrics, EEG-related metrics, oximetry metrics, and respiratory event-related metrics: see Table 1, Table 2, Table 3, and Table 4). In each group of outcomes, we described each metric based on its category.
Cardiovascular/metabolic outcomes and mortality
Twenty-six studies reported CV/metabolic outcomes and mortality in patients with OSA. From these studies, 11 investigated autonomic/hemodynamic metrics, 11 studies investigated oximetric metrics, and 5 studies reported EEG metrics and respiratory-related metrics.
Autonomic/hemodynamic metrics: 11 studies
These metrics were derived from pulse oximetry (photoplethysmography [PPG]) for estimating blood pressure (BP) changes and heart rate variability (HRV) or derived from ECG signals combined with respiratory data. Five unique CV-related metrics were described (see Table 1).
Heart rate response to respiratory events
Elevated heart rate response to respiratory events (“ΔHR”) was recently introduced by Azarbarzin and colleagues.9 This metric was shown to be associated with deleterious CV outcomes in patients with OSA.9 The risk was exclusively observed in individuals with no excessive daytime sleepiness. Activation of sympathetic activity is associated with an increase in the heart rate, the magnitude of which may also be affected by the severity of respiratory events,10 the intensity of cortical arousal,11 and the responsiveness of the autonomic nervous system.12 Therefore, it is plausible that the OSA-specific heart rate response may reflect important aspects of the autonomic response to respiratory events, useful to predict CV and metabolic outcomes. The ΔHR was defined as the difference between a maximum pulse rate (derived from the oximetry signal) during a subject-specific search window and the minimum pulse rate during apneas and hypopneas. Individuals with OSA who demonstrated an elevated ΔHR were at increased risk of nonfatal and fatal CVD and all-cause mortality (hazard ratio [95% confidence interval] = 1.60 [1.28–2.00], 1.68 [1.22–2.30], and 1.29 [1.07–1.55], respectively) in the Sleep Heart Health Study (SHHS). Of note, this cohort predominantly included middle-aged or older individuals (mean age = 64.2 ± 11 years). Further studies are needed to prospectively replicate these findings in younger individuals.
Pulse arrival time
Another alternative metric extracted from PPG, pulse arrival time (PAT), has been a widely used surrogate of pulse transit time, and has been used to estimate BP.13 Arterial stiffening from increased BP leads to a rise in pulse wave velocity and a fall in PAT.13 Since nocturnal sleep BP is an important prognostic marker of CV health, PAT assessment during sleep may provide useful information related to CV health in patients with OSA. PAT is calculated from the time interval between ECG R-waves and the pulse wave detected by pulse oximetry. An increase in PAT is indicative of an increase in BP.14 Kwon and colleagues15 calculated the PAT response to respiratory events using the area under the PAT waveform (first derivate of PAT) following respiratory events. Cross-sectional analyses revealed that higher PAT response was associated with higher left ventricular mass (5.7 g/m2 higher in the fourth compared with the first quartile, P < .007) and a higher carotid plaque burden score (0.37 higher in the fourth compared with the first quartile, P = .02). A nonsignificant association with greater odds of coronary artery calcification was also observed (P = .06). Finally, they showed that a 1-standard-deviation increase in average PAT response was associated with 18% higher risk of incident CVD. While these findings may help better identify high-risk individuals with OSA, further studies are needed to prospectively confirm them in younger individuals. Furthermore, the calculation of PAT requires more sophisticated signal processing techniques that may hinder its utility in routine clinical care.
Pulse wave characteristics
In a study in 2020, Hirotsu and colleagues16 examined the clinical significance of pulse wave amplitude (PWA) drops, extracted from PPG signal during sleep, as a biomarker for cardiometabolic disorders. The amplitude of the PPG signal was considered as a surrogate of the PWA. PWA variations seem to be proportional to the sympathetic outflow directed to the vessels, reflecting sympathovagal balance. Thus, they hypothesized that PWA-drop features during sleep would be independently associated with hypertension, diabetes, and previous CV events as these conditions are associated with impairments in the autonomic nervous system and vascular function. After preprocessing of PPG signal and derivation of peaks and nadirs, time course and first derivate of PWA-variation were extracted. PWA-drops with an amplitude > 30% and a duration > 4 heart beats, their frequency, duration, and area under the curve (AUC) were calculated. They showed that lower PWA-drop index, longer duration, and greater AUC were associated with increased risk of hypertension, diabetes, or CV events. Participants in the lowest quartile compared with those in the highest quartile of mean duration-normalized PWA-drop index had a significantly higher odds ratio (OR) of hypertension (OR = 1.60 [1.19–2.16]), CV event (OR = 3.26 [1.33–8.03]), and diabetes (OR = 1.71 [1.06–2.76]). Similar results were reported for mean duration- and mean AUC-normalized PWA-drop indexes. In another study by Strassberger and colleagues,17 a novel cardiac risk index (CRI) was computed based on pulse wave signals derived from pulse oximetry, reflecting vascular stiffness, cardiac variability, vascular autonomic tone, and nocturnal hypoxia. CRI calculated using an algorithm that computed 9 parameters (pulse index, oxygen saturation [SpO2] index, PWA index, respiratory-related pulse oscillations, pulse propagation time, periodic and symmetric desaturations, time under 90% SpO2, difference between pulse and SpO2 index, and arrhythmia) from PPG signal.18 They showed that CRI but not AHI or ODI significantly increased the area under the receiver operating characteristic curve (AUC) after controlling for confounders. Moreover, comparison of the ODI and CRI indicated only the novel risk index had an independent influence on CV risk prediction.
Both studies revealed the benefits of PPG-derived metrics to predict cardiometabolic outcomes. However, the mean age of participants in both studies was younger in comparison to most of the studies, and investigation of these metrics on prospective cohorts with different characteristics would be essential.
Pulse rate variability/HRV
HRV is a noninvasive tool for the assessment of autonomic nervous activity. Pulse rate variability (PRV) derived from nocturnal pulse oximetry can provide a measurement of HRV during sleep.19 This specific metric was studied by Blanchard and colleagues20 to assess the association between PRV and the onset of atrial fibrillation (AF) in patients with suspected OSA. After artifact removal, pulse-to-pulse intervals were calculated by identifying local peaks (R-waves). Normal-to-normal (NN) beat intervals (intervals between normal R-peaks), the standard deviation (SD) of NN intervals (SDNN), and the root mean square of the successive NN differences (RMSSD) were calculated. Higher PRV, as assessed by SDNN and RMSSD, and a lower ratio of low-frequency and high-frequency PRV (a measure of sympathetic to parasympathetic autonomic balance) were associated with a higher risk of AF. The association remained highly significant after adjusting for confounders. Finally, they showed that patients with the highest quartile of T90 (the percentage of recording time with oxygen saturation < 90%) and RMSSD had a lower AF survival than those with only 1 or neither of these conditions. Blanchard and colleagues21 in another large multicenter, clinic-based cohort investigated if these PSG-derived indices of HRV could predict stroke incidence. They showed that patients with lower ratio of low-frequency and high-frequency PRV were at higher risk of stroke after adjusting for confounding risk factors and positive airway pressure adherence. A 1-unit increase in log-transformed low frequency (LF):high frequency (HF) ratio was associated with a 44% decrease in stroke risk. The association was stronger in patients aged more than 60 years. However, stroke incidence was more strongly associated with HF PRV among nonobese individuals compared with those with obesity. Recently, Trzepizur and colleagues22 tested PRV on a cohort from France to examine its association with major adverse CV events (MACEs). Log-transformed PRV indices (ln SDNN, ln LF, ln HF, and ln LF-to-HF ratio) were found to be associated with incident MACEs in unadjusted models, but the association weakened and became nonsignificant after adjusting for confounders. Finally, Berger and his colleagues23 assessed the association between nocturnal HRV and CVD incidence over 4 years in a population-based sample. Polysomnography-based ECGs were exported to analyze time- and frequency-domain HRV, Poincaré plots indices, detrended fluctuation analysis, acceleration capacity (AC) and deceleration capacity (DC), entropy, heart rate fragmentation, and heart rate turbulence.
To distinguish between vagal and sympathetic factors that affect HRV, they used a signal processing algorithm to separately characterize deceleration and acceleration of heart rate. Heartbeat intervals longer than the preceding interval are identified as DC and, for computation of AC, heartbeat intervals shorter than the preceding interval are identified as AC.24 They showed that nocturnal novel HRV parameters (eg, AC, DC, and heart rate fragmentation) were better predictors of CVD events than traditional HRV parameters (eg, SDNN, RMSSD, HF). In a fully adjusted model, AC (hazard ratio per 1-SD increase [95% confidence interval] = 1.59 [1.17–2.16]; P = .004), DC (0.63 [0.47–0.84], P = .002), and heart rate fragmentation (1.41 [1.11–1.78], P = 0.005) were the only features significantly associated with incidence of CVD events.
Considering the results of these 4 studies that investigated HRV-related indices to predict CV/metabolic outcomes and mortality, it seems that the metrics (eg, HF, LF, RMSSD) that were associated with outcomes in 1 study did not persist in other studies. Therefore, more investigations on HRV-related metrics need to be done to derive a reliable metric associated with this group of metrics. The other reported issues with HRV in sleep-related studies are the assumption of stationarity of this signal, which is not true in sleep apnea, and the complexity of HRV calculation.25,26
Cardiopulmonary coupling
Cardiopulmonary coupling (CPC) is an ECG-based metric designed to combine information from HRV and ECG-derived respiration.27 Briefly, this method proposed to characterize sleep stability using a continuous single-channel ECG, by mathematically combining QRS wave amplitude fluctuations that are related to the mechanical effects of respiration with HRV changes that are associated with neuro-autonomic tone modulation. Thomas and colleagues,28 using the data from the SHHS cohort, found that an ECG-derived spectrographic marker related to LF CPC (narrow-band elevated LF) was associated with greater sleep apnea severity. This narrow-band elevated LF coupling was also associated with prevalent hypertension and stroke (OR [95% confidence interval] = 1.02 [1.01–1.04], P = .001, and 1.65 [1.19–2.29], P = .003, respectively), after adjustment for potential confounders. In 2020, Magnusdottir and colleagues29 examined if changes in objective sleep quality index assessed through cardiopulmonary-coupling analysis impacted BP in patients with OSA at high-CV risk. The sleep quality index metric consists of a measure of sleep stability as stable sleep (HF coupling), unstable sleep (LF coupling), sleep fragmentation (elevated LF coupling broad-band), and a marker of periodic breathing (periodicity, elevated LF coupling narrow-band). The sleep quality index was presented on a scale of 0 to 100 in which a higher number represented a better quality of sleep. They found that CPAP therapy significantly improved BP, with improvement in mean arterial BP during sleep (MAP Sleep) when compared with nocturnal supplemental oxygen therapy or healthy lifestyle and sleep education therapy. They also showed that sleep quality impacted 24-hour mean arterial pressure, mean diastolic BP, and BP during wakefulness. Elevated LF coupling derived from CPC analysis was investigated in 2 cohorts with different characteristics (eg, mean age, sex, PSG type). The results showed this metric could be useful to predict cardiometabolic outcomes in patients with OSA.
EEG metrics; 3 studies
More in-depth analysis of EEG may provide new insights into how OSA is associated with health outcomes. These studies used metrics derived from EEG spectral analyses, spindle morphology, and arousal duration. Out of 9 studies that reported EEG metrics, 3 of them investigated the association between EEG metrics and CV/metabolic outcomes and mortality and the rest reported cognitive function– and vigilance-related outcomes (see Table 2).
Odds ratio product
OSA reduces overall sleep depth because of frequent respiratory events and arousals. Poor quality sleep and excessive wake time have been independently associated with hypertension.31 Odds ratio product (ORP) is a proprietary metric that quantifies sleep depth based on quantitative analysis of the EEG power spectra. ORP ranges from 0 to 2.5, with lower values indicative of deeper sleep.30 Kim and colleagues31 examined the association of ORP with BP in the Multi-Ethnic Study of Atherosclerosis (MESA) cohort; they showed that higher ORP was not significantly associated with BP in unadjusted or adjusted models.
EEG power
Delta wave activity is a key feature of deep sleep. Therefore, overnight power spectral analysis of delta activity might be a useful measure of sleep disturbance. Disrupted sleep could, in turn, affect cardiometabolic activity. Lechat and colleagues32 investigated whether power spectral measures and spectral entropy-based markers of delta wave activity (0.5 to 4.5 Hz) during sleep predicted mortality stronger than conventional sleep quality and disturbance metrics, including wake after sleep onset, arousal index, and average power across EEG frequency bands. The degree of uniformity of the delta wave density function was quantified using spectral entropy. The spectral entropy was computed by calculating the Shannon entropy of the power spectrum of the delta wave density function. A higher spectral entropy (higher frequency fluctuations in delta power) and a lower spectral entropy (short or absent delta power activity fluctuations) of EEG delta power (ie, the upper and lower tertiles of entropy distribution function) during sleep were associated with a 32% increased risk of all-cause mortality compared with the mid-tertile of the entropy distribution function, after adjusting for total sleep time and other clinical-related covariates including sleep apnea. This association was of a similar magnitude to a reduction in total sleep time from 6.5 hours to 4.25 hours. In addition to replication of these findings across different age- and sex-specific groups, future studies are needed to determine the associations of delta wave entropy with subjective and objective measures of daytime sleepiness and symptoms.
Arousal burden
Arousals impact heart rate, BP, and cardiac hemodynamics may also disrupt the circadian rhythm of the CV system, which is associated with unfavorable metabolic outcomes, such as higher BP. Shahrbabaki and colleagues33 studied arousal burden (AB; total duration of arousals normalized by total sleep time) to predict the risk of cardiac events and all-cause mortality. For women from the SHHS, and the Study of Osteoporotic Fractures (SOF) there was a correlation between AB and CV-related and all-cause mortality. For men, the link between AB and mortality was not clear. The association for men could not be reproduced in both cohorts. For example, in the SHHS, AB was only associated with all-cause mortality; however, in the Osteoporotic Fractures in Men Study (MrOS), AB was associated with CV mortality but not all-cause mortality (all-cause mortality—MrOS: HR = 1.11, P = .261; SHHS-men: HR=1.31, P = .011; CV mortality—MrOS: HR=1.35, P = .034; SHHS-men: HR=1.24, P = .271). Considering the reported results from all investigated cohorts, this metric does not appear to predict CV-related outcomes and mortality across sex-specific subgroups. Another issue with AB is that, compared with respiratory events/desaturations, arousal scoring is highly variable in the clinical and research settings and therefore it may be challenging to get an accurate measure of arousal duration.34,35 Furthermore, developing algorithms for arousal scoring appears to be challenging.
Oximetric metrics: 11 studies
Novel metrics related to continuous oxygen saturation from overnight PSG data have been well documented. Eleven studies examined the association between oxygen saturation metrics and CV/metabolic outcomes and mortality while 7 studies considered “hypoxic burden” as a metric for their research (Table 3).
Hypoxic burden
Hypoxic burden (HB) in response to respiratory events (otherwise, known as sleep apnea–specific hypoxic burden) is defined as the total area under the desaturation curve from a pre–respiratory event baseline and calculated as the sum of individual burdens divided by total sleep time. Azarbarzin and colleagues36 showed that HB strongly predicted CVD mortality (MrOS and SHHS cohorts) and all-cause mortality (only in MrOS). Patients in MrOS and SHHS cohorts with HB in the highest quintile had a hazard ratio of 2.73 (P < .001) and 1.96 (P < .05) for CV-related mortality, respectively, whereas the AHI was an unreliable predictor. In 2021, Azarbarzin’s group used HB in conjunction with ΔHR changes (see autonomic/hemodynamic metrics section above) and found that the relationship between ΔHR and fatal CVD or all-cause mortality was stronger in patients with a high HB.9 No association between a high ΔHR and fatal CVD or all-cause mortality was observed in those with a low HB. In a recent large multicenter clinical cohort of patients with OSA, Blanchard and colleagues21 showed that patients with higher HB were at higher risk of stroke after adjusting for confounding risk factors (adjusted hazard ratio = 1.30; 95% confidence interval: 1.05–1.61; P = .02). However, the association was nonsignificant after exclusion of 29 patients with transient ischemic attack. Recently, Trzepizur and colleagues22 demonstrated that HB was associated with an increased risk of MACEs or all-cause mortality. Interestingly, a stronger association between HB and MACEs was observed in women and younger patients. In another study, Azarbarzin and colleagues37 examined the association between HB and incident heart failure in 2 independent cohorts (SHHS and MrOS). HB was associated with an increased risk for incident heart failure in men after considering demographic factors and comorbidities. Every 1-SD increase in HB was associated with an 18% and 22% increased risk of incident heart failure in SHHS and MrOS, respectively. Importantly, HB was found to predict incident heart failure in individuals with both a high and a low AHI. In addition to these longitudinal associations, HB was also shown to be associated with increased BP and chronic kidney disease (CKD) in cross-sectional analyses. In 2021, Kim and colleagues31 assessed the associations between BP and OSA-specific HB in participants from the MESA cohort. They found that a higher HB was linked to higher blood pressure, such that for every 1-SD increase in HB there was an associated 1.1% increase in systolic and 1.9% increase in diastolic BP among those not taking hypertension medications. Finally, in the same cohort (MESA), Jackson and colleagues38 showed a significant association between HB and CKD. Participants in the highest HB quintile (in comparison to the lowest) were at greater risk of CKD (36% significantly higher moderate-to-severe CKD prevalence ratio = 1.36 [1.00–1.86]). The prevalence of CKD was also higher in Black women in the highest vs lowest quantile of HB.
HB as a metric for evaluation of oxygen desaturation in response to respiratory events has been evaluated in different studies and cohorts. HB can be measured from home sleep tests, which is increasingly becoming popular. However, future studies are needed to demonstrate the utility of this metric in a younger population with sleep apnea and to determine its utility to predict CPAP benefit. Finally, an automated and standardized method is needed to calculate this metric from in-home and in-laboratory studies.
Respiratory event desaturation transient area
Philip de Chazal and colleagues39 sought to develop a metric that could be used to measure hypoxemia based on the area under the oxygen saturation (SpO2) signal without requiring estimation of pre-event baseline saturation, thereby simplifying calculation compared with HB. For each respiratory event, they calculated the area between 100% and the SpO2 curve from midway through the event and extending for 2.5 event lengths. The respiratory event desaturation transient area (REDTA) value was then calculated by summing the areas for events and dividing by 3,600. Using the SHHS cohort, the hazard ratio in adjusted analysis for predicting CVD using REDTA was 1.71 (1.09–2.69) in the last quintile compared with the first quintile, which was similar to Azarbarzin’s metric (HB).36 In contrast to HB, a dose–response relationship between CVD mortality and REDTA was not observed as the hazard ratio in the adjusted analysis. It was highest in the third quintile and decreased for the fourth and fifth quintiles.
Oxygen desaturation rate
The oxygen saturation variations in OSA disease are cyclic drops in saturation rather than a sustained drop in oxygen saturation during sleep. HF intermittent hypoxemia characterized by cycles of hypoxemia with reoxygenation differs from sustained LF hypoxemia, which might lead to endothelial dysfunction that can further contribute to hypertension development.40 Wang and colleagues41 investigated the association between oxygen desaturation rate and BP in patients with OSA. The decrease in SpO2 during apnea from the start of the desaturation to the nadir of desaturation divided by the duration of desaturation was used to calculate oxygen desaturation rate (ODR). Comparisons between the 2 groups of greater ODR vs lesser ODR showed significantly higher systolic BP values in the high-ODR group as well as short-term BP variability (event-related BP elevation) and the prevalence of hypertension. Investigating this metric on different cohorts with greater size, considering patients with mild and severe OSA, and evaluating this metric on longitudinal studies need to be done in future studies.
Lung to finger circulation time
Sleep study–derived circulation time (Ct) reflects oxygen transport time from the lung to the periphery. Long Ct is a sign of circulation delay in patients with heart failure. Therefore, prolonged Ct derived from PSG could indicate subclinical heart failure.42 Kwon and colleagues42 quantified lung to finger Ct (LFCt), the average time between the end of respiratory events and nadir oxygen desaturations associated with those events. LFCt was significantly associated with an increased risk for CVD and all-cause mortality; the hazard ratios for the last quartile were 1.36 (1.02–1.81), P = .04, and 1.35 (1.14–1.60), P < .001, respectively, compared with the first quartile. Even though their proposed metric was able to predict CVD and mortality in patients with OSA, evaluation of LFCt on cohorts with a lower mean age and in both men and women needs to be done. Furthermore, we do not know the extent to which this metric is related to OSA. This metric may be a marker of subclinical heart failure and, therefore, future CPAP-related studies are needed to better understand this metric.
Desaturation severity and obstructive severity
Muraja-Murro and colleagues43 investigated the association between duration or depth of obstruction (length of apneas or hypopneas), severity of desaturation events (area of desaturation events), obstruction severity, and mortality rate. The “obstruction severity” parameter was the sum of the products of apnea and hypopnea duration and related desaturation areas normalized with the total analyzed time. They showed that the obstruction severity parameter was higher in deceased patients than in alive patients with severe OSA. In addition, the “obstruction severity” was the only parameter related to mortality in the severe OSA category based on a multivariable logistic regression analysis. Future studies are needed to prospectively validate this metric in larger, more diverse studies with longer follow-up durations.
Respiratory event–related metrics: 2 studies
Three novel respiratory event–related metrics derived from airflow/nasal pressure signals from overnight PSG data linked to CV/metabolic outcomes and mortality have been reported (Table 4).
Event duration
In a study by Butler and colleagues,44 short event duration, a potential marker of reduced arousal threshold, was shown to predict all-cause mortality in the SHHS cohort. Individuals with the shortest duration of respiratory events experienced a 20% increased mortality rate compared with those with the longest events. This relationship was observed in both men and women and was strongest in those with moderate sleep apnea. Although the reported metric was able to predict mortality in SHHS patients, the physiological interpretation of how a shorter event might lead to a higher rate mortality needs further investigation. Similar to other studies, future work is needed to replicate these findings in other cohorts, including in younger individuals.
Duty cycle and inspiratory flow limitation
Kim and colleagues31 examined the association of airflow limitation with increased BP. Airflow limitation was assessed using duty cycle (inspiratory time/total respiratory cycle time) and percentage of breaths with flow limitation from the nasal pressure signal. Flow limitation is present when peak flow occurs very early or very late in inspiration. Inspiratory flow limitations (IFLs) are usually terminated by arousals, which may contribute to acute elevations in BP through sympathetic activation.31 They showed that a higher NREM IFL was associated with a lower diastolic BP after adjusting for baseline covariates, hypoxia, and sleep depth. REM IFL was not associated with systolic and diastolic BP after covariate adjustment. A higher NREM duty cycle was associated with a lower systolic BP after adjusting for baseline covariates; this association was significant after adjusting for HB and sleep depth. They also reported a higher REM duty cycle was associated with lower systolic BP. There were no significant associations of NREM or REM duty cycle with diastolic BP. In this study, they hypothesized that metrics of increased inspiratory resistance (IFL, duty cycle) would be associated with higher BP; however, they found the opposite. Investigating these metrics on cohorts with different characteristics (eg, age, BMI) might reveal more information about this metric.
Cognitive function– and vigilance-related outcomes
Of 10 studies that investigated cognitive function– and vigilance-related outcomes, the majority of studies reported EEG-related metrics associated with this group of outcomes.
Autonomic/hemodynamic metrics: 1 study
Finding the association between this group of metrics and cognitive outcomes reported in just one recent study.
Pulse arrival time (PAT)
PAT was introduced previously (see above). Since acute hypertension is known to be linked to an increased risk of cerebral microbleeds, Alomri and colleagues45 investigated whether nocturnal elevations in BP derived from PAT were associated with cognitive dysfunction in patients with OSA. The maximum value of nocturnal systolic BP and the difference between resting and nocturnal systolic BP peaks were independently associated with poor performance on the Austin Maze test (a test of visuospatial dysfunction) after controlling for several confounders including age, smoking status, depressive symptoms, hypoxia, and sleep fragmentation. No association was observed with sustained attention, reaction time, or memory. Using PAT as a surrogate of BP might be able to predict cognitive dysfunction in patients with OSA; however, evaluation of this metric on different metrics with greater size is undeniable.
EEG metrics: 6 studies
Six out of 9 studies reported associations between EEG-related metrics and cognitive function and vigilance outcomes (Table 2).
ORP
Azarbarzin and colleagues46 studied the relationship between interhemispheric ORP coherence (LR-OPR, correlation between ORP from left and right hemispheres) and the risk of car crashes. Patients in the highest quartile of LR-OPR had a 62% lower risk of crash compared with the lowest quartile. Although the methods for derivation of this metric are easy to understand, the mean age of participants in this study was high. Moreover, the lack of control for confounders limits the impact of this study.
EEG metrics
Djonlagic and colleagues47 studied which aspect of sleep EEG was most strongly associated with cognitive performance and processing speed in adult patients from the MrOS and MESA cohorts. Using EEG spectrum analysis from over 150 objective sleep metrics, they found 23 metrics associated with cognitive performance. Promising metrics fell across 3 broad classes: (class 1) sleep duration and continuity (eg, REM duration [min], sleep efficiency); (class 2) spindle activity and spindle–slow oscillation coupling (eg, fast spindle count [N2], slow spindles–slow oscillation coupling, fast spindles–slow oscillation coupling; fast spindles center frequency = 15 Hz and slow spindles center frequency = 11 Hz); and (class 3) slow-wave sleep (eg, slow/delta [N3], slow/delta [N2 + N3], slow oscillations wavelength [N3]). As results, in terms of class 1 metrics, increased REM duration, sleep efficiency, and sleep maintenance efficiency were associated with better cognitive performance. In terms of class 2, higher count and integrated spindle activity were associated with better cognitive performance for both fast and slow N2 spindles, as well as higher fast spindle integrated spindle activity per minute. For class 3, higher relative slow power (during both N2 and N3) but lower relative delta power (N3) were associated with worse cognitive performance.
Spindle Burst Index
A novel metric based on bursts of spindles (Spindle Burst Index [SBI]) was reported by McCloy and colleagues.48 They examined links between SBI and objective vigilance as assessed by the Psychomotor Vigilance Test (PVT) indices (number of lapses and reaction time) using data acquired from diagnostic PSGs. The SBI was defined as the percentage of burst spindles in a sleep block (eg, stage 2 sleep). They classified sleep spindles as bursts if they occurred within a maximum inter-spindle interval of 20 seconds (ie, spindles occurred in proximity to each other). Spindle characteristics were used to model standardized (z score) lapse and median reaction time (MdRT) scores, and to groups based on zLapse and zMdRT scores. Their proposed model using spindle characteristics mapped to MdRT with an accuracy of 91.9% (sensitivity and specificity of the model were 88.9%, and 89.1%, respectively, for detecting patients with the lowest median reaction times as a vigilance marker). More research on this model needs to be done to validate their proposed model.
EEG power
Vakulin et al49 used EEG power spectral analysis (absolute EEG spectral power across all frequencies [0.5–32 Hz]) to identify predictors of driving simulator performance. Significant predictors of worse steering deviation were greater total EEG power during NREM and REM sleep, greater beta (15–32 Hz) EEG power in NREM, and greater delta (0.5–4.5 Hz) EEG power in REM as well as sleep-onset latency.
Arousal duration
Schwartz and Moxley50 examined longer EEG arousal duration as a novel arousal definition and showed that longer durations (15–60 seconds) were better associated with self-reported sleepiness in patients with OSA than standard arousal durations (3–10 seconds). A study by Duce and colleagues51 examined the extent to which changing the minimum cortical arousal duration improved the link between sleep fragmentation and neurocognitive outcomes. They showed that there was no difference between the impaired and unimpaired groups in the PVT test (The PVT outcomes were calculated: mean 1/reaction time [RT], median RT, slowest 10% 1/RT, and the number of lapses) with respect to the standard, 3-second minimum EEG arousal duration (P = .220). However, the impaired group showed significantly increased EEG arousal indices that required a minimum duration of 5 seconds (P = .034), 7 seconds (P = .041), and 15 seconds (P = .036). Moreover, comparisons of receiver-operator characteristic (ROC) curves of minimum EEG arousal duration thresholds for the identification of patients with OSA with impaired PVT performance indicated the AUC, the specificity, and the positive likelihood ratio increased as the threshold for the duration of EEG arousals increased.
Oximetric metrics: 1 study
Desaturation severity and obstructive severity
Kainulainen and colleagues52 examined how metrics derived from oximetry signal (desaturation duration, desaturation severity, and obstruction severity [explained in the previous section]) were associated with impaired vigilance (PVT reaction time and number of lapses). They showed that the duration of apneas and hypopneas, duration of desaturations, and obstruction severity do not seem to affect PVT performance as much as the severity of desaturations.
Respiratory event–related metrics: 2 studies
Apnea or hypopnea load
Goh and colleagues53 sought to investigate if apnea or hypopnea load, which considers event duration and not just the presence or absence of respiratory events, had a better correlation with the Epworth Sleepiness Scale score than the AHI. Using linear regression analysis, apnea load (P = .005) was independently associated with Epworth Sleepiness Scale score. Moreover, in 2007, Mediano and colleagues54 investigated the association between apnea duration and excessive daytime sleepiness in patients with OSA. They showed that apnea duration in the group with excessive daytime sleepiness was higher than in the non–excessive daytime sleepiness group (ie, 29 ± 8 and 22 ± 7, respectively; P = .008). Both of this metrics have been examined in the association of apnea and hypopnea load in 2 different cohorts. Their results showed that apnea load could be beneficial for predicting cognitive dysfunction– and vigilance-related outcomes.
DISCUSSION
In this comprehensive systematic review, we identified 31 studies that identified promising alternative PSG metrics that have the potential to better predict OSA-related complications than standard metrics. These alternative metrics can leverage the richness of the raw PSG data into generating a more nuanced description of the disease. Broadly speaking, we found 4 general categories of alternative metrics pertaining to hemodynamic-related, EEG-related, desaturation indices, and respiratory event data. These metrics were used to predict a broad range of OSA-associated outcomes, including CVD, cognitive dysfunction, hypertension, CKD, car crash risk, and all-cause mortality. Identifying biometric profiles based on PSG may help stratify patients more at risk of the effects of OSA and could significantly affect patient management. For example, if a patient was identified as having a high risk of CVD, one would be more aggressive in terms of OSA management and management of other CV risk factors (eg, hypertension, hyperlipidemia, inactivity). In addition, these profiles may help identify potential pharmacologic targets for therapy; for example, if a patient with high sympathetic activity was identified based on PSG metrics, they might be more likely to benefit from a beta-blocker to improve CV risk.55
We also identified several limitations in the studies published to date. Many of the studies included were retrospective analyses of prospective outcomes and used established cohorts. Most were community-based cohorts and their generalizability to patients seen in sleep clinics could be questioned. In addition, for SHHS and MrOS specifically, the mean age was high (ie, 76.6 and 64 years for MrOS and SHHS, respectively33) and MrOS specifically only studied men, which might again limit generalizability. However, some of these metrics (eg, hypoxic burden36) have been validated in both clinical and community-based cohorts. In order to bring these and other metrics to clinical use, future work should focus not only on identifying more novel metrics but also to validate previously identified metrics across other populations. There is also an urgent need to apply them to the prospective studies, with prespecified analyses and outcomes. In addition, we would envision that these features might be used to select patients for inclusion in randomized controlled trials of OSA therapy. For example, if features indicative of patients at high risk of incident CV risk could be identified, they may be targeted for clinical trials examining impacts of therapy on CV risk reduction. Furthermore, we would envision that eventually these metrics could be incorporated into machine-learning models that could help find the best metrics or combination of metrics associated with specific outcome or refine prediction models for OSA-related complications. However, we feel that different metrics would likely be more useful for particular outcomes; for example, metrics predictive of CV risk might not be that helpful in predicting the risk of dementia.
The PSG provides a wealth of physiologic information that goes beyond the AHI and other standard PSG metrics that might help risk-stratify patients with adverse health outcomes. OSA is being increasingly considered a heterogeneous disease both from the perspective of underlying mechanisms as well as in terms of clinical manifestations. A long-term OSA management outlook where clinicians and patients are provided a more nuanced representation of their disease, especially with regard to the risk of future adverse OSA-related outcomes, is an exciting prospect for the field of sleep medicine.
ABBREVIATIONS
- AB
arousal burden
- AC
acceleration capacity
- AHI
apnea-hypopnea index
- BP
blood pressure
- CKD
chronic kidney disease
- CPAP
continues positive airway pressure
- CPC
cardiopulmonary coupling
- Ct
circulation time
- CV
cardiovascular
- CVD
cardiovascular disease
- DC
deceleration capacity
- ECG
electrocardiogram
- EEG
electroencephalography
- EMG
electromyography
- HB
hypoxic burden
- HF
high frequency
- HRV
heart rate variability
- IFL
inspiratory flow limitation
- LF
low frequency
- LFCt
lung to finger circulation time
- MASE
major adverse cardiovascular event
- MESA
Multi-Ethnic Study of Atherosclerosis
- MrOS
Osteoporotic Fractures in Men Study
- NREM
non–rapid eye movement
- ODI
oxygen desaturation index
- ODR
oxygen desaturation rate
- ORP
odds ratio product
- OSA
obstructive sleep apnea
- PAT
pulse arrival time
- PPG
photoplethysmography
- PRV
pulse rate variability
- PSG
polysomnography
- PVT
Psychomotor Vigilance Test
- REDTA
respiratory event desaturation transient area
- REM
rapid eye movement
- SBI
Spindle Burst Index
- SD
standard deviation
- SHHS
Sleep Heart Health Study
- SOF
Study of Osteoporotic Fractures
- SpO2
oxygen saturation
DISCLOSURE STATEMENT
All authors have seen and approved the manuscript. Work for this study was performed at the University of British Columbia (UBC). Dr. Najib Ayas’s funding: Vancouver Coastal Health Research Institute Innovation funding, BC Lung Association Operating Grant, Canadian institutes of health research Operating Grant. Dr. Rachel Jen: VCHRI Investigator Grant. Dr. Azarbarzin reports grant funding from National Institute of Health, American Heart Association, American Academy of Sleep Medicine Foundation, and Somnifix. There are no other funding sources from other authors. A.A. serves as a consultant for Apnimed, Somnifix, Inspire, and Respicardia, outside the submitted work. A.A. is an author in some of the studies reported in this review. The other authors report no conflicts of interest.
REFERENCES
- 1. Benjafield AV , Ayas NT , Eastwood PR , et al . Estimation of the global prevalence and burden of obstructive sleep apnoea: a literature-based analysis . Lancet Respir Med. 2019. ; 7 ( 8 ): 687 – 698 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Chen W , Li Y , Guo L , Zhang C , Tang S . An umbrella review of systematic reviews and meta-analyses of observational investigations of obstructive sleep apnea and health outcomes . Sleep Breath. 2022. ; 26 ( 1 ): 167 – 188 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Pevernagie DA , Gnidovec-Strazisar B , Grote L , et al . On the rise and fall of the apnea-hypopnea index: a historical review and critical appraisal . J Sleep Res. 2020. ; 29 ( 4 ): e13066 . [DOI] [PubMed] [Google Scholar]
- 4. Malhotra A , Ayappa I , Ayas N , et al . Metrics of sleep apnea severity: beyond the apnea-hypopnea index . Sleep. 2021. ; 44 ( 7 ): zsab030 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Moher D , Liberati A , Tetzlaff J , Altman DG ; PRISMA Group . Preferred Reporting Items for Systematic Reviews and Meta-Analyses: the PRISMA statement . PLoS Med. 2009. ; 6 ( 7 ): e1000097 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Sands SA , Terrill PI , Edwards BA , et al . Quantifying the arousal threshold using polysomnography in obstructive sleep apnea . Sleep. 2018. ; 41 ( 1 ): zsx183 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Stanchina M , Robinson K , Corrao W , Donat W , Sands S , Malhotra A . Clinical use of loop gain measures to determine continuous positive airway pressure efficacy in patients with complex sleep apnea. A pilot study . Ann Am Thorac Soc. 2015. ; 12 ( 9 ): 1351 – 1357 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Moola S , Munn Z , Tufanaru C , et al . Systematic Reviews of Etiology and Risk . In: Aromataris E , Munn Z , eds. JBI Manual for Evidence Synthesis. JBI; ; 2020. [Google Scholar]
- 9. Azarbarzin A , Sands SA , Younes M , et al . The sleep apnea-specific pulse-rate response predicts cardiovascular morbidity and mortality . Am J Respir Crit Care Med. 2021. ; 203 ( 12 ): 1546 – 1555 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Azarbarzin A , Ostrowski M , Moussavi Z , Hanly P , Younes M . Contribution of arousal from sleep to postevent tachycardia in patients with obstructive sleep apnea . Sleep. 2013. ; 36 ( 6 ): 881 – 889 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Azarbarzin A , Ostrowski M , Hanly P , Younes M . Relationship between arousal intensity and heart rate response to arousal . Sleep. 2014. ; 37 ( 4 ): 645 – 653 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Caples SM , Gami AS , Somers VK . Obstructive sleep apnea . Ann Intern Med. 2005. ; 142 ( 3 ): 187 – 197 . [DOI] [PubMed] [Google Scholar]
- 13. Finnegan E , Davidson S , Harford M , et al . Pulse arrival time as a surrogate of blood pressure . Sci Rep. 2021. ; 11 ( 1 ): 22767 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Mukkamala R , Hahn JO , Inan OT , et al . Toward ubiquitous blood pressure monitoring via pulse transit time: theory and practice . IEEE Trans Biomed Eng. 2015. ; 62 ( 8 ): 1879 – 1901 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Kwon Y , Wiles C , Parker BE , et al . Pulse arrival time, a novel sleep cardiovascular marker: the multi-ethnic study of atherosclerosis . Thorax. 2021. ; 76 ( 11 ): 1124 – 1130 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Hirotsu C , Betta M , Bernardi G , et al . Pulse wave amplitude drops during sleep: clinical significance and characteristics in a general population sample . Sleep. 2020. ; 43 ( 7 ): zsz322 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Strassberger C , Zou D , Penzel T , et al . Beyond the AHI-pulse wave analysis during sleep for recognition of cardiovascular risk in sleep apnea patients . J Sleep Res. 2021. ; 30 ( 6 ): e13364 . [DOI] [PubMed] [Google Scholar]
- 18. Sommermeyer D , Zou D , Ficker JH , et al . Detection of cardiovascular risk from a photoplethysmographic signal using a matching pursuit algorithm . Med Biol Eng Comput. 2016. ; 54 ( 7 ): 1111 – 1121 . [DOI] [PubMed] [Google Scholar]
- 19. Qin H , Keenan BT , Mazzotti DR , et al . Heart rate variability during wakefulness as a marker of obstructive sleep apnea severity . Sleep. 2021. ; 44 ( 5 ): zsab018 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Blanchard M , Gervès-Pinquié C , Feuilloy M , et al . Association of nocturnal hypoxemia and pulse rate variability with incident atrial fibrillation in patients investigated for obstructive sleep apnea . Ann Am Thorac Soc. 2021. ; 18 ( 6 ): 1043 – 1051 . [DOI] [PubMed] [Google Scholar]
- 21. Blanchard M , Gervès-Pinquié C , Feuilloy M , et al . Hypoxic burden and heart rate variability predict stroke incidence in sleep apnoea . Eur Respir J. 2021. ; 57 ( 3 ): 2004022 . [DOI] [PubMed] [Google Scholar]
- 22. Trzepizur W , Blanchard M , Ganem T , et al . Sleep apnea-specific hypoxic burden, symptom subtypes, and risk of cardiovascular events and all-cause mortality . Am J Respir Crit Care Med. 2022. ; 205 ( 1 ): 108 – 117 . [DOI] [PubMed] [Google Scholar]
- 23. Berger M , Pichot V , Solelhac G , et al . Association between nocturnal heart rate variability and incident cardiovascular disease events: the HypnoLaus population-based study . Heart Rhythm. 2022. ; 19 ( 4 ): 632 – 639 . [DOI] [PubMed] [Google Scholar]
- 24. Bauer A , Kantelhardt JW , Barthel P , et al . Deceleration capacity of heart rate as a predictor of mortality after myocardial infarction: cohort study . Lancet. 2006. ; 367 ( 9523 ): 1674 – 1681 . [DOI] [PubMed] [Google Scholar]
- 25. Penzel T . Is heart rate variability the simple solution to diagnose sleep apnoea? Eur Respir J. 2003. ; 22 ( 6 ): 870 – 891 . [DOI] [PubMed] [Google Scholar]
- 26. Wu HT , Soliman EZ . A new approach for analysis of heart rate variability and QT variability in long-term ECG recording . Biomed Eng Online. 2018. ; 17 ( 1 ): 54 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Keim-Malpass J , Clark MT , Lake DE , Moorman JR . Towards development of alert thresholds for clinical deterioration using continuous predictive analytics monitoring . J Clin Monit Comput. 2020. ; 34 ( 4 ): 797 – 804 . [DOI] [PubMed] [Google Scholar]
- 28. Thomas RJ , Weiss MD , Mietus JE , Peng CK , Goldberger AL , Gottlieb DJ . Prevalent hypertension and stroke in the Sleep Heart Health Study: association with an ECG-derived spectrographic marker of cardiopulmonary coupling . Sleep. 2009. ; 32 ( 7 ): 897 – 904 . [PMC free article] [PubMed] [Google Scholar]
- 29. Magnusdottir S , Hilmisson H , Thomas RJ . Cardiopulmonary coupling-derived sleep quality is associated with improvements in blood pressure in patients with obstructive sleep apnea at high-cardiovascular risk . J Hypertens. 2020. ; 38 ( 11 ): 2287 – 2294 . [DOI] [PubMed] [Google Scholar]
- 30. Younes M , Ostrowski M , Soiferman M , et al . Odds ratio product of sleep EEG as a continuous measure of sleep state . Sleep. 2015. ; 38 ( 4 ): 641 – 654 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Kim JS , Azarbarzin A , Wang R , et al . Association of novel measures of sleep disturbances with blood pressure: the Multi-Ethnic Study of Atherosclerosis . Thorax. 2020. ; 75 ( 1 ): 57 – 63 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Lechat B , Hansen KL , Melaku YA , et al . A novel electroencephalogram-derived measure of disrupted delta wave activity during sleep predicts all-cause mortality risk . Ann Am Thorac Soc. 2022. ; 19 ( 4 ): 649 – 658 . [DOI] [PubMed] [Google Scholar]
- 33. Shahrbabaki SS , Linz D , Hartmann S , Redline S , Baumert M . Sleep arousal burden is associated with long-term all-cause and cardiovascular mortality in 8001 community-dwelling older men and women . Eur Heart J. 2021. ; 42 ( 21 ): 2088 – 2099 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Bonnet MH , Doghramji K , Roehrs T , et al . The scoring of arousal in sleep: reliability, validity, and alternatives . J Clin Sleep Med. 2007. ; 3 ( 2 ): 133 – 145 . [PubMed] [Google Scholar]
- 35. Redline S , Budhiraja R , Kapur V , et al . The scoring of respiratory events in sleep: reliability and validity . J Clin Sleep Med. 2007. ; 3 ( 2 ): 169 – 200 . [PubMed] [Google Scholar]
- 36. Azarbarzin A , Sands SA , Stone KL , et al . The hypoxic burden of sleep apnoea predicts cardiovascular disease-related mortality: the Osteoporotic Fractures in Men Study and the Sleep Heart Health Study . [published correction appears in Eur Heart J. 2019 Apr 7;40(14):1157] Eur Heart J. 2019. ; 40 ( 14 ): 1149 – 1157 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Azarbarzin A , Sands SA , Taranto-Montemurro L , et al . The sleep apnea-specific hypoxic burden predicts incident heart failure . Chest. 2020. ; 158 ( 2 ): 739 – 750 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Jackson CL , Umesi C , Gaston SA , et al . Multiple, objectively measured sleep dimensions including hypoxic burden and chronic kidney disease: findings from the Multi-Ethnic Study of Atherosclerosis . Thorax. 2021. ; 76 ( 7 ): 704 – 713 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. de Chazal P , Sadr N , Dissanayake H , et al . Predicting cardiovascular outcomes using the Respiratory Event Desaturation Transient Area derived from overnight sleep studies . Annu Int Conf IEEE Eng Med Biol Soc. 2021. ; 2021 : 5496 – 5499 . [DOI] [PubMed] [Google Scholar]
- 40. Foster GE , Poulin MJ , Hanly PJ . Intermittent hypoxia and vascular function: implications for obstructive sleep apnoea . Exp Physiol. 2007. ; 92 ( 1 ): 51 – 65 . [DOI] [PubMed] [Google Scholar]
- 41. Wang N , Meng Z , Ding N , et al . Oxygen desaturation rate as a novel intermittent hypoxemia parameter in severe obstructive sleep apnea is strongly associated with hypertension . J Clin Sleep Med. 2020. ; 16 ( 7 ): 1055 – 1062 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Kwon Y , Sands SA , Stone KL , et al . Prolonged circulation time is associated with mortality among older men with sleep-disordered breathing . Chest. 2021. ; 159 ( 4 ): 1610 – 1620 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Muraja-Murro A , Kulkas A , Hiltunen M , et al . The severity of individual obstruction events is related to increased mortality rate in severe obstructive sleep apnea . J Sleep Res. 2013. ; 22 ( 6 ): 663 – 669 . [DOI] [PubMed] [Google Scholar]
- 44. Butler MP , Emch JT , Rueschman M , et al . Apnea-hypopnea event duration predicts mortality in men and women in the Sleep Heart Health Study . Am J Respir Crit Care Med. 2019. ; 199 ( 7 ): 903 – 912 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Alomri RMA , Kennedy GA , Wali S , Alhejaili F , Zelko M , Robinson SR . Association between cognitive dysfunction and nocturnal peaks of blood pressure estimated from pulse transit time in obstructive sleep apnoea . Sleep Med. 2022. ; 90 : 185 – 191 . [DOI] [PubMed] [Google Scholar]
- 46. Azarbarzin A , Younes M , Sands SA , et al . Interhemispheric sleep depth coherence predicts driving safety in sleep apnea . J Sleep Res. 2021. ; 30 : e13092 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Djonlagic I , Mariani S , Fitzpatrick AL , et al . Macro and micro sleep architecture and cognitive performance in older adults . [published correction appears in Nat Hum Behav. 2020 Dec 16;] Nat Hum Behav. 2021. ; 5 ( 1 ): 123 – 145 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. McCloy K , Duce B , Hukins C , Abeyratne U . Mapping sleep spindle characteristics to vigilance outcomes in patients with obstructive sleep apnea . Annu Int Conf IEEE Eng Med Biol Soc. 2021. ; 2021 : 704 – 707 . [DOI] [PubMed] [Google Scholar]
- 49. Vakulin A , D’Rozario A , Kim JW , et al . Quantitative sleep EEG and polysomnographic predictors of driving simulator performance in obstructive sleep apnea . Clin Neurophysiol. 2016. ; 127 ( 2 ): 1428 – 1435 . [DOI] [PubMed] [Google Scholar]
- 50. Schwartz DJ , Moxley P . On the potential clinical relevance of the length of arousals from sleep in patients with obstructive sleep apnea . J Clin Sleep Med. 2006. ; 2 ( 2 ): 175 – 180 . [PubMed] [Google Scholar]
- 51. Duce B , Kulkas A , Töyräs J , Terrill P , Hukins C . Longer duration electroencephalogram arousals have a better relationship with impaired vigilance and health status in obstructive sleep apnoea . Sleep Breath. 2021. ; 25 ( 1 ): 263 – 270 . [DOI] [PubMed] [Google Scholar]
- 52. Kainulainen S , Duce B , Korkalainen H , et al . Severe desaturations increase psychomotor vigilance task-based median reaction time and number of lapses in obstructive sleep apnoea patients . Eur Respir J. 2020. ; 55 ( 4 ): 1901849 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Goh JC , Tang J , Cao JX , Hao Y , Toh ST . Apnoeic and hypopnoeic load in obstructive sleep apnoea: correlation with Epworth Sleepiness Scale . Ann Acad Med Singap. 2018. ; 47 ( 6 ): 216 – 222 . [PubMed] [Google Scholar]
- 54. Mediano O , Barceló A , de la Peña M , Gozal D , Agusti A , Barbé F . Daytime sleepiness and polysomnographic variables in sleep apnoea patients . Rev Port Pneumol. 2007. ; 13 ( 6 ): 896 – 898 . [DOI] [PubMed] [Google Scholar]
- 55. Peres BU , Allen AJH , Shah A , et al . Obstructive sleep apnea and circulating biomarkers of oxidative stress: a cross-sectional study . Antioxidants. 2020. ; 9 ( 6 ): 476 . [DOI] [PMC free article] [PubMed] [Google Scholar]