Abstract
Background:
Recently there has been an increase in minimally invasive surgery (MIS) for the correction of hallux valgus deformity. This systematic review aims to evaluate and present the current literature on MIS hallux valgus correction in studies reporting the use of the Shannon burr with distal metatarsal osteotomies to help establish evidence-based guidelines for surgeons using this technique.
Methods:
Two independent authors performed a systematic literature search using the following databases: PubMed, Embase, and the Cochrane library. The Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) protocol and the Cochrane Handbook guidelines were followed. All studies included were published from 2008 to 2022 and included the use of the Shannon burr during distal metatarsal osteotomies MIS for hallux valgus and at least 12-month follow-up. The MINORS score criteria was used to evaluate the strength and quality of 17 studies by 3 authors. Statistical analysis and meta-analysis were not performed because of the heterogeneity of the included studies and the data being descriptive.
Results:
A total of 17 studies were reviewed. A total of 911 subjects were included, and 1088 MIS procedures were performed. The average follow-up was 23.8 (12-59.1) months. American Orthopaedic Foot & Ankle Society scale and visual analog scale scores improved from 52.1 (41-62.5) to 90.3 (83.3-97.1) and 4.9 (3-8.2) to 0.8 (0-1.9). Satisfaction rates were very high among the studies that reported it. The hallux valgus angle, intermetatarsal angle, and distal metatarsal articular angle improved from 31.4 (23.5-44.1) to 11.1 (7-17.2), 13.4 (8.1-18.6) to 7.3 (4.2-10.3), and 12.3 (9-16.3) to 4.1 (1-6.7), respectively. The complication rate was 16.6%, and recurrence was 2.2%. Nonunion comprised 0.4%, infections 1.1%, nerve injury 2.2%, avascular necrosis 0%, hallux varus 0.09%, transfer metatarsalgia 0.1%, and hardware removal 6.2%.
Conclusion:
MIS for the treatment of hallux valgus using the Shannon burr appears to be a safe and effective therapy, with appropriate correction of the hallux valgus deformity, improvement in functional outcomes, high patient satisfaction, low recurrence, and acceptable complication rates.
Level of Evidence:
Level II, systematic review.
Keywords: hallux valgus, MIS, bunions, distal osteotomy, outcomes, systematic review, Shannon burr
Introduction
Hallux valgus is one of the most common deformities treated by orthopaedic foot and ankle surgeons.28,31 There are many treatment options, which range from nonsurgical modalities to more than 100 surgical techniques.33,39
The recent literature highlights an increasing interest and potential benefit in minimally invasive (MIS) hallux valgus surgical correction. A recent meta-analysis by Ji et al15 comparing MIS hallux valgus surgery vs open surgical treatment suggested improved clinical and radiologic outcomes with MIS compared with open treatment. In another meta-analysis comparing MIS vs open surgery, no inferiority was reported on radiographic outcomes for MIS.33 Additionally, a review by Trnka et al37 reported no inferiority in radiographic or clinical outcomes for MIS vs open cohorts. The meta-analysis by Lu et al22 showed no inferiority for MIS vs open treatment in patient satisfaction and an increase in excellent-good radiographic outcomes.
The Shannon burr is often used to help perform the osteotomies for several MIS hallux valgus surgical techniques. The utilization of the Shannon burr allows the surgeon to perform a less invasive approach for hallux valgus correction with very small incisions. The Shannon burr is also used in other procedures such as percutaneous bunionette correction, percutaneous calcaneal osteotomy, and lesser toe procedures.11,18,19,25,26
Considering the recent influx of research on the topic of MIS hallux valgus correction, prior systematic reviews still include many procedures that did not use a Shannon burr but traditional saws. Additionally, many of these studies looked at proximal and distal osteotomies and first- and second-generation MIS instrumentation and osteotomies that may or may not have had fixations. Currently newer-designed third- and fourth-generation MIS surgical techniques and instruments have evolved and the most commonly done MIS osteotomy are distal metatarsal osteotomies including chevron Akin (MICA) and transverse osteotomies and Akin (PETA) with beveled screw fixation.15,22,33,37 Therefore, the goal of this systematic review was to analyze and present the currently available literature on MIS surgery for hallux valgus correction specifically using the Shannon burr in distal metatarsal osteotomies. To our knowledge, this will be the first systematic review focusing on the use of the Shannon burr for MIS hallux valgus correction with distal metatarsal osteotomies. The aim of this review is to help provide surgeons with evidence-based guidelines and set patient expectations when considering using MIS hallux valgus correction with a Shannon burr for distal metatarsal osteotomies.
Methods and Search Strategy
The systematic literature review included all studies that were published from 2008 to 2022. The databases used were PubMed, Embase, and the Cochrane library. The following items were included: (minimally invasive surgery hallux valgus) OR (percutaneous bunion surgery) OR (percutaneous hallux valgus surgery) OR (minimally invasive bunion surgery) OR (hallux valgus minimally invasive), without a language filter. Initial screening of titles, abstracts, and full-text studies was performed. The Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) protocol and the Cochrane Handbook guidelines were followed.13,30 The MINORS Score criteria were used to evaluate the strength and quality of the studies.34
Inclusion and Exclusion Criteria
Inclusion criteria were any studies published from 2008 to 2022 that included the use of the Shannon burr during distal metatarsal osteotomies MIS for hallux valgus. Excluded studies were not in English, included children, did not specify the use of the Shannon burr, did not use screws for fixation, or did not have a 12-month follow-up.
Data Collection and Abstraction
Three investigators independently evaluated titles, abstracts, and full text from the studies found in the search. The following data were extracted: authors, the title of studies, journal of publication, year of publication, country, level of evidence, number of subjects, use of Shannon burr, type of osteotomy performed, type of fixation performed, number of procedures performed, mean age, sex, American Orthopaedic Foot & Ankle Society (AOFAS) score, hallux valgus angle (HVA), intermetatarsal angle (IMA), visual analog scale (VAS) score, patient satisfaction, final follow-up time, control group, surgical procedures, severity of hallux valgus, and complications.
Statistical Analysis and Assessment for Risk of Bias
The MINORS score was used to evaluate the quality and bias of the 17 nonrandomized controlled trials (Table 1).12,34 The average score among all studies was 16.5, with a range of 13 to 24. These scores represent high-quality studies. Meta-analysis of the collective data was not performed because of the heterogeneity of the included studies.
Table 1.
MINORS Score.a
| Study | Aim | Inclusion | Prospective | Endpoints | Unbiased | Follow-up | Loss | Calculation | CG | G | Baseline | SA | Total Scoreb |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Burg et al3 | 2 | 2 | 0 | 2 | 0 | 2 | 2 | 2 | 0 | 0 | 0 | 2 | 14 |
| Holme et al14 | 2 | 2 | 2 | 2 | 0 | 2 | 2 | 2 | 0 | 0 | 0 | 2 | 16 |
| Chan et al4 | 2 | 2 | 2 | 2 | 0 | 2 | 1 | 2 | 0 | 0 | 0 | 2 | 15 |
| Liszka and Gądek21 | 2 | 2 | 0 | 2 | 0 | 2 | 2 | 2 | 0 | 0 | 0 | 2 | 14 |
| de Carvalho et al5 | 2 | 2 | 2 | 2 | 0 | 2 | 2 | 2 | 0 | 0 | 0 | 2 | 16 |
| Díaz Fernández6 | 2 | 2 | 0 | 2 | 0 | 2 | 2 | 2 | 0 | 0 | 0 | 2 | 14 |
| Tay et al35 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 24 |
| Brogan et al2 | 2 | 2 | 2 | 2 | 0 | 2 | 1 | 2 | 2 | 2 | 2 | 2 | 21 |
| Jowett and Bedi16 | 2 | 2 | 2 | 2 | 0 | 2 | 1 | 2 | 0 | 0 | 0 | 2 | 15 |
| Mikhail et al27 | 2 | 2 | 0 | 2 | 0 | 2 | 2 | 2 | 0 | 0 | 0 | 2 | 14 |
| Lai et al20 | 2 | 2 | 2 | 2 | 2 | 2 | 1 | 2 | 2 | 2 | 2 | 2 | 23 |
| Frigg et al9 | 2 | 2 | 0 | 2 | 0 | 2 | 2 | 2 | 0 | 0 | 0 | 2 | 14 |
| Nunes et al29 | 2 | 2 | 2 | 2 | 0 | 2 | 2 | 2 | 0 | 0 | 0 | 2 | 16 |
| Ghioldi et al10 | 2 | 2 | 0 | 2 | 0 | 2 | 1 | 2 | 0 | 0 | 0 | 2 | 13 |
| Kurashige17 | 2 | 2 | 2 | 2 | 0 | 2 | 0 | 2 | 0 | 0 | 0 | 2 | 14 |
| Marijuschkin et al24 | 2 | 2 | 2 | 2 | 0 | 2 | 2 | 2 | 0 | 0 | 0 | 2 | 16 |
Aim: a clearly stated aim. Inclusion: inclusion of consecutive patients. Prospective: prospective collection of data. Endpoint: endpoints appropriate to the aim of the study. Unbiased: unbiased assessment of the study endpoint. Follow-up: follow-up period appropriate to the aim of the study. Loss: loss to follow-up <5%. Calculation: prospective calculation of the study size. CG: an adequate control group. G: contemporary group. Baseline: baseline equivalence of groups. SA: adequate statistical analyses.
Scores: 0 = not reported; 1 = reported by study but inadequate; 2 = reported and adequate.
Results
Characteristics of the Systematic Review Search and Study Demographics
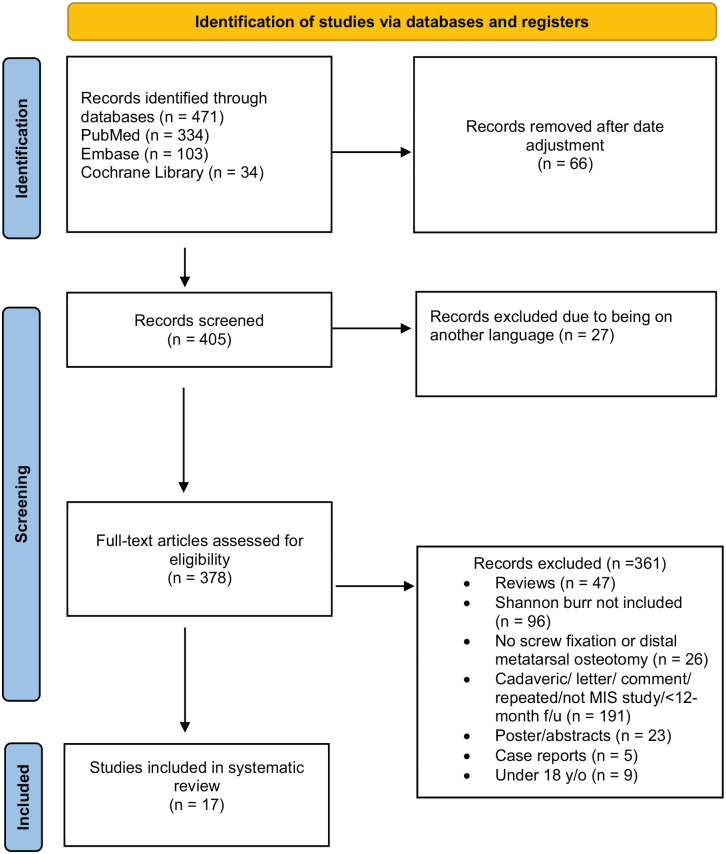
A total of 471 results were found after the primary database search (Figure 1). After adjusting for the date criteria, 405 studies were analyzed. A total of 17 studies were included in the systematic review after passing screening criteria. A total of 1081 subjects and 1284 procedures were found in the studies. There were 1088 MIS procedures including the Shannon burr. The average age for patients was 54.4 years. Follow-up times among studies had an average of 23.8 months (range 12-59.1). Among the studies, the level of evidence ranged from II to IV. There are 8 level III, 8 level IV, and 1 level II studies. Four studies had control groups. Characteristics and demographics of the studies are listed in Table 2.
Figure 1.
Prisma flow diagram for search strategy and selection criteria.
Table 2.
Demographics and Characteristic of the Studies.
| Author | Country | Level of Evidence | Participants, n | Mean Age, y | Feet, n | Women, n | Follow-up, mo | Control Group | Osteotomy |
|---|---|---|---|---|---|---|---|---|---|
| Burg et al3 | Israel | III | 20 | 66 | 21 | 17 | 12 | No | Chevron-Akin |
| Holme et al14 | England | IV | 40 | 51 | 40 | 38 | 12 | No | Chevron-Akin |
| Chan et al4 | Singapore | IV | 8 | 50.7 | 13 | 5 | 35 | No | Chevron-Akin |
| Liszka and Gądek21 | Poland | III | 54 | 54.5 | 103 | 97 | 12 | No | Chevron-Akin |
| de Carvalho et al5 | USA | IV | 47 | 55.9 | 70 | 39 | 31.6 | No | Chevron-Akin |
| Díaz Fernández6 | Spain | IV | 24 | 59 | 24 | 24 | 24 | No | RI, DMMO’s, Akin |
| Tay et al35 | Singapore | III | 60 (30 MIS) | 51.7 (MIS) | 60 (30 MIS) | 47 (21 MIS) | 24 | Yes | Chevron-Akin |
| Brogan et al2 | England | III | 81 (49 MIS) | 53 (MIS) | 81 (49 MIS) | 78 (46 MIS) | 24 | Yes | Chevron-Akin |
| Jowett and Bedi16 | Australia | IV | 78 | 55 | 106 | 76 | 25 | No | Chevron-Akin |
| Mikhail et al27 | USA | III | 248 | 55.1 | 274 | 218 | 12.9 | No | Chevron-Akin |
| Lai et al20 | Singapore | III | 87 (29 MIS) | 54.3 (MIS) | 87 (29 MIS) | 77 (25 MIS) | 24 | Yes | Chevron-Akin |
| Frigg et al9 | Switzerland | II | 98 (48 MIS) | 48 (MIS) | 98 (48 MIS) | 85 (41 MIS) | 24 | Yes | Chevron-Akin |
| Nunes et al29 | Brazil | IV | 40 | 50.4 | 50 | 37 | 16.1 | No | Chevron-Akin |
| Ghioldi et al10 | Argentina | III | 46 | 53.9 | 60 | 41 | 33.5 | No | Bösch |
| Kurashige17 | Japan | IV | 40 | 59.9 | 40 | 34 | 18.6 | No | Chevron-Akin |
| Marijuschkin et al24 | Brazil | IV | 72 | 58.8 | 112 (86 MIS) | 64 | 17.2 | No | Akin, chevron, RI |
| Lucas y Hernandez et al23 | France | III | 38 | 48 | 45 | 35 | 59.1 | No | R-L-chevron |
Abbreviations: DMMOs, distal metatarsal minimally invasive osteotomies; MIS, minimally invasive surgery; RI, Reverdin-Isham; R-L-chevron, reverse-L-chevron.
Clinical Outcomes: AOFAS Score, VAS Score, and Satisfaction Rate
Preoperative and last follow-up AOFAS scores were reported in 13 studies. The average score improved from 52.1 (range 41-62.5) to 90.3 (range 83.3-97.1). Statistically significant improvement was reported in 10 studies. Three studies reported significant improvements in the Foot Function Index, Japanese Society for Surgery of the Foot Scale, and Manchester-Oxford Foot Questionnaire scores, which are comparable to the AOFAS score.2,17,27 One study did not report AOFAS or any comparable score.29 Preoperative and last follow-up visual analog scale (VAS) score was reported in 7 studies, and in 5 it was reported as statistically significant. The average score improved from 4.9 (range 3-8.2) to 0.8 (range 0-1.9). A total of 6 studies reported satisfaction rates. In 2 studies, a 100% satisfaction rate was reported.3,14 A satisfaction rate higher than 90% was reported in 2 studies.23,27 In addition, the satisfaction rate was higher than 80% in 3 studies, and in 2 studies the satisfaction rate was higher in the MIS group vs open surgery (Table 3).16,20,35 Cosmesis was shown to be better in the MIS group compared to the open group.9
Table 3.
AOFAS, VAS Scores, and Satisfaction Rate at Last Follow-up.
| AOFAS Score | VAS Score | Satisfaction Rate, % | |||||
|---|---|---|---|---|---|---|---|
| Author | Pre | Post | P Value | Pre | Post | P Value | |
| Burg et al3 | 41.6 | 86.1 | <.01 | NR | NR | 100 | |
| Holme et al14 | 48.2 | 93.4 | <.01 | NR | NR | 100 | |
| Chan et al4 | 59 | 93.7 | .001 | 5.1 | 0 | .001 | NR |
| Liszka and Gądek21 | 41 | 89.5 | NR | NR | NR | NR | |
| de Carvalho et al5 | 43.9 | 92.6 | <.01 | 8.24 | 1.19 | .01 | NR |
| Díaz Fernández6 | 45.8 | 91.2 | <.0001 | NR | NR | NR | |
| Tay et al35 | 54.3 | 83.3 | <.001 | 5.5 | 1.1 | <.001 | 86 MIS vs 73 open |
| Brogan et al2 | NR (MOXFQ 46.6) | NR (MOXFQ 13) | <.001 | NR | NR | NR | |
| Jowett and Bedi16 | 56 | 87 | <.001 | NR | NR | 87 | |
| Mikhail et al27 | NR (FFI 48 and 44) | NR (FFI 18 and 25) | <.001 | NR | NR | 91.60 | |
| Lai et al20 | 58.6 | 87.4 | <.05 | 4 | 0.7 | <.05 | 82.8 MIS vs 81 open |
| Frigg et al9 | 52 | 95 | NR | 3 | 0 | NR | NR |
| Nunes et al29 | NR | NR | NR | NR | NR | NR | |
| Ghioldi et al10 | 65.3 | 89.9 | NR | 5.2 | 1.1 | NR | NR |
| Kurashige17 | NR (JSSF 65.3) | NR (JSSF 97.9) | <.0001 | 3.9 | 1.1 | <.0001 | NR |
| Marijuschkin et al24 | 49.2 | 88.6 | <.05 | NR | NR | NR | NR |
| Lucas y Hernandez et al23 | 62.5 | 97.1 | 1.32 × 10−27 | NR | NR | NR | 97 |
Abbreviations: AOFAS, American Orthopaedic Foot & Ankle Society; FFI, Foot Function Index; JSSF, Japanese Society for Surgery of the Foot Scale; MIS, minimally invasive surgery; MOXFQ, Manchester-Oxford Foot Questionnaire; NR, not reported; Post, postintervention; Pre, preintervention; VAS, visual analog scale.
Radiographic Outcomes: Hallux Valgus, Intermetatarsal, and Distal Metatarsal Articular Angle Results
The average follow-up was 23.8 (12-59.1) months. Preoperative and follow-up HVA was reported in all studies. The was an average improvement from 31.4 (range 23.5-44.1) to 11.1 (range 7-17.2). Only 2 studies did not report if the improvement was statistically significant.9,10 Preoperative and follow-up IMA was reported in all studies. There was an average improvement from 13.4 (range 8.1-18.6) to 7.3 (range 4.2-10.3). Only 2 studies did not report if the improvement was statistically significant.9,10 Preoperative and follow-up distal metatarsal articular angle (DMAA) was reported in 4 studies. There was an average improvement from 12.3 (range 9-16.3) to 4.1 (range 1-6.7). Two studies reported statistically significant improvement, and the other 2 studies did not report if significance was found (Table 4).
Table 4.
HVA, IMA, and DMAA Results.
| HVA | IMA | DMAA | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Study | Pre | Post | P Value | Pre | Post | P Value | Pre | Post | P Value |
| Burg et al3 | 44.1 | 12.5 | <.01 | 8.1 | 4.3 | <.01 | NR | NR | NR |
| Holme et al14 | 31.7 | 12.1 | <.01 | 13.2 | 6.7 | <.01 | NR | NR | NR |
| Chan et al4 | 30.4 | 10.9 | <.001 | 13.9 | 10.2 | .001 | NR | NR | NR |
| Liszka and Gądek21 | 33.8 | 13.5 | <.05 | 14.9 | 7.7 | <.05 | NR | NR | NR |
| de Carvalho et al5 | 30.3 | 11.3 | <.01 | 14.8 | 7.5 | <.01 | 16.3 | 6.7 | <.01 |
| Díaz Fernández6 | 36.5 | 12.2 | <.0001 | 13.8 | 7 | <.0001 | 13.9 | 6 | <.0001 |
| Tay et al35 | 23.5 | 7.7 | <.002 | 13.5 | 7.5 | <.001 | NR | NR | NR |
| Brogan et al2 | 26.6 | 10.4 | <.001 | 11.7 | 6.8 | <.001 | 9 | 1 | NR |
| Jowett and Bedi16 | 29.7 | 10.3 | <.001 | 14 | 7.6 | <.001 | NR | NR | N |
| Mikhail et al27 | 29.1 | 8.9 | <.001 | 13.4 | 4.9 | <.001 | NR | NR | NR |
| Lai et al20 | 29.9 | 8.8 | <.05 | 14.6 | 10.3 | <.05 | NR | NR | NR |
| Frigg et al9 | 25 | 7 | NR | 13 | 6 | NR | 10 | 3 | NR |
| Nunes et al29 | 32.5 | 7.3 | <.001 | 14.2 | 4.2 | <.001 | NR | NR | NR |
| Ghioldi et al10 | 31 | 17.7 | NR | 12 | 8.7 | NR | NR | NR | NR |
| Kurashige17 | 39.3 | 12.8 | <.0001 | 18.6 | 8.4 | <.0001 | NR | NR | NR |
| Marijuschkin et al24 | 35.1 | 17.2 | <.05 | 13.7 | 9.3 | <.05 | NR | NR | NR |
| Lucas y Hernandez et al23 | 26.2 | 9.6 | <.05 | 11.8 | 7.9 | <.05 | NR | NR | NR |
Abbreviations: DMAA, distal metatarsal articular angle; HVA, hallux valgus angle; IMA, intermetatarsal angle; NR, not reported; Post, postprocedural; Pre, preprocedural.
Complications
The rate of complications was reported by all studies. The total number of complications among all studies was 181 of 1088 (16.6%). The total number of recurrences was 24 of 1088 (2.2%). There were reported 7 of 1088 (0.6%) revision surgeries for recurrence. There was a total of 13 of 1088 (1.1%) infections reported including 4 deep tissue infections and 7 superficial infections. The other 2 infections were not specified if they were superficial or deep. There was a total of 25 of 1088 (2.2%) nerve injuries, including a similar range for numbness, paresthesia, and chronic regional pain syndrome. The total number of nonunions was 5 (0.4%), avascular necrosis 0, burns 0, transfer metatarsalgia 1 (0.09%), hallux varus 1 (0.09%), and hardware removal 68 (6.2%). Table 5 has the total number of complications and in detail the number of recurrence or revisions, nonunion, avascular necrosis, burns, transfer metatarsalgia, hallux varus, type of infections, nerve injuries, and screw/hardware removal per study.
Table 5.
Complications per Study.
| Author | Hallux Varus | Nerve Injury | Infection | Recurrence | Nonunion | Avascular Necrosis | Burns | Transfer Metatarsalgia | Removal of Hardware and Screws |
|---|---|---|---|---|---|---|---|---|---|
| Burg et al3 | 0 | 0 | 0 | 0 | 1a | 0 | 0 | 0 | 2 |
| Holme et al14 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 4 |
| Chan et al4 | 0 | 0 | 1 (superficial) | 0 | 0 | 0 | 0 | 0 | 0 |
| Liszka and Gądek21 | 0 | 2 (transient numbness) | 0 | 0 | 0 | 0 | 0 | 0 | 4 |
| de Carvalho et al5 | 0 | 2 (unspecified) | 0 | 3 (2)a | 0 | 0 | 0 | 0 | 10 |
| Díaz Fernández6 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 3 |
| Tay et al35 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Brogran et al2 | 0 | 4 (paresthesia) | 0 | 1b | 0 | 0 | 0 | 0 | 4 |
| Jowett and Bedi16 | 0 | 0 | 2 (deep) | 12b | 0 | 0 | 0 | 0 | 16 |
| Mikhail et al27 | 1b | 5 (CRPS) | 6 (1 deep, 5 superficial) | 4 (3a) | 2 (2a) | 0 | 0 | 0 | 0 |
| Lai et al20 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Frigg et al9 | 0 | 9 (5 CRPS, 4 numbness) | 2 (unspecified) | 3 (2a) | 0 | 0 | 0 | 0 | 12 |
| Nunes et al29 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Ghioldi et al10 | 0 | 0 | 2 (1 deep, 1 superficial) | 0 | 0 | 0 | 0 | 0 | 4 |
| Kurashige17 | 0 | 2 (transient numbness) | 0 | 0 | 0 | 0 | 0 | 0 | 2 |
| Marijuschkin et al24 | 0 | 1 (neuropathy) | 0 | 1b | 2b | 0 | 0 | 2 | 6 |
| Lucas y Hernandez et al23 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 |
Abbreviation: CRPS, complex regional pain syndrome.
Number of patients who underwent revision surgery.
Patient did not undergo revision surgery.
Discussion
This review is the first and largest to our knowledge to specifically examine the usage of the Shannon burr when performing MIS distal metatarsal osteotomies in hallux valgus surgery. The results of this study demonstrate that MIS hallux valgus surgery using a Shannon burr appears to be safe and effective at correction of the hallux valgus deformity with improvement in patient functional outcomes, high patient satisfaction, low recurrence rates, and acceptable complication rates.
This review showed significant improvement in patient functional outcomes after MIS hallux valgus correction. MIS hallux valgus correction when compared to open procedures were found to have no differences in clinical outcome when comparing VAS and AOFAS scores.2,9,20,35 Ji et al’s15 meta-analysis reported no difference between the MIS and the open surgery cohort; however, when only comparing their 8 randomized controlled trials, they found a higher AOFAS score in the MIS group. This review found an average increase of 38 points, with an average AOFAS score of 90.3 at the last follow-up. No study showed a decrease in functional outcome scores after MIS hallux valgus surgery.
When deciding between various surgical procedures for hallux valgus correction, the degree of deformity often dictates which surgical procedure should be done. Traditionally, smaller HVAs often require a distal osteotomy whereas larger deformities tend to require more proximal osteotomies or fusions.8 This review found that patients with mild to moderate HVA and IMA could benefit from MIS hallux valgus surgery with improved correction of their IMA and HVA.4,14,35
Often, moderate hallux valgus with IMA greater than 13 degrees traditionally requires a more proximal metatarsal osteotomy; however, with the ability to translate the metatarsal head almost 100% when using MIS techniques, more moderate bunions may be corrected with distal osteotomies.8 Our review found that MIS hallux valgus correction with a Shannon burr allows for appropriate correction and significant reduction of HVA, IMA, and DMAA in mild to moderate bunion deformities.2,9 When comparing MIS hallux valgus to open procedures, on average there was no difference reported in HVA, IMA, and DMAA.2,35 However individual studies did have varying results, with Lai et al20 reporting statistically significant improvement in HVA results for the MIS group when compared to open surgery. The study by Frigg et al9 reported statistically significant improvement in the IMA for the open surgery group when compared with the MIS group; however, the study also reported DMAA was statistically significantly better for the MIS group when compared to the open surgery group. This review found that the average HVA decreased from 31.4 (range 23.5-44.1) to 11.1 (range 7-17.2). The average IMA decreased from 13.4 (range 8.1-18.6) to 7.3 (range 4.2-10.3), and the average DMAA decreased from 12.3 (range 9-16.3) to 4.1 (range 1-6.7) degrees.
This review found that satisfaction was very high on average for patient undergoing MIS hallux valgus correction, with 2 studies showing a higher satisfaction rate among the MIS group compared with the open group.20,35 However, some individual studies had varying results, and the meta-analysis by Sing et al33 reported no difference among MIS vs open groups. A total of 7 studies included a satisfaction rate in their data, and all of them reported a >80% rate of satisfaction among their patients.3,14,16,20,23,27,35 There were 3 studies that reported a satisfaction rate of >95% among their patients.3,14,23
Recurrence is a common complication after hallux valgus, with a recent meta-analysis by Ezzatvar et al7 finding a recurrence rate of 24.9% for open hallux valgus correction. Our review found a very low recurrence rate after MIS hallux valgus correction of 2.2% at an average follow-up of 23.8 months (range 12-59.1). The number of recurrences that had to be revised was 0.6% (7/1088). There was only 1 case of hallux varus after surgery that was painless, and the patient did not want to proceed with revision surgery.27
Some literature reports a higher complication rate with MIS hallux valgus correction, specially citing concern for nerve injury, recurrence, and nonunion due to use of the Shannon burr, percutaneous technique, and large metatarsal head shift.36 This review found a 16.6% complication rate with MIS hallux valgus correction, which is higher than that reported in the literature for open procedures of 7% to 8%.36 However, excluding hardware irritation and removal the overall rate of complication was 10.3%. The rate of recurrence of 2.2%, nerve damage of 2.4%, and nonunion rate of 0.4% found in this review was similar to that reported in Barg et al’s1 systematic review of open hallux valgus surgical correction, where the recurrence rate was 4.9%, nerve injury 3%, and nonunion rate 0.04%. In their analysis, they showed that specifically for distal metatarsal osteotomies, the recurrence rate was 4.1%, nerve injury 3.3%, and nonunion rate 0.01%, similar to the results of this study.
Many reasons for this increase in complication rate with MIS hallux valgus surgery can be considered. The hardware removal rate accounted for almost 40% of all complications as is likely due to screw prominence after swelling resolves given the entry point on the medial border of the first ray. Newer-generation implants are designed to minimize this problem, and future studies will need to see if this rate of hardware irritation decreases. However, given these findings, we recommend that surgeons be meticulous about their hardware placement and make sure prominence is minimized before leaving the operating room.
The Shannon burr, a high-torque, low-speed burr, is designed to limit soft tissue injury, including nerve damage. Nerve injuries are a common concern for surgeons considering MIS hallux valgus procedures. In our review, it was found that 2.4% of patient had some form of nerve-related injury. In the systematic review by Barg et al,1 they found an overall rate of 3% nerve injury in open hallux valgus procedure, and for distal metatarsal osteotomy it was 3.3%. which is similar to the findings from our review.
Some literature suggests that MIS hallux valgus surgery has a higher risk of nonunion and avascular necrosis compared to open procedures.38 This review found 5 cases (0.4%) of nonunion among all studies, and 2 cases were revised. There were no cases of avascular necrosis reported. This rate of nonunion is higher than that reported in the systematic review by Barg et al1 of 0.01% for distal metatarsal osteotomies. We believe this may be due to multiple factors. Use of the burr does result in heat generation, and a recent study by Reddy et al32 showed that cool water irrigation may play a role in minimizing heat generation. If the burr does generate too much heat, this could cause thermal necrosis of bone and may be a factor that could contribute to nonunions. Malreduction with large metatarsal head shifts can occur as there is a learning curve associated with MIS hallux valgus correction. Because these distal osteotomies are both transverse and chevron along with a potential for 100% shift, these must be fixed adequately to provide stability of the osteotomy. If this shift has inadequate fixation, it could lead to mechanical instability and contribute to nonunions. Additionally, there is a learning curve associated with MIS hallux valgus surgery that has been shown to be between 60 and 70 cases, with improved results after this, which could affect outcomes of MIS hallux valgus correction.4,5,9,16 We believe the result of nonunion in MIS hallux valgus correction may be multifactorial and include various levels of skill, surgical technique used, and fixation techniques. However, it is beyond the scope of this review to identify the causality of the nonunions and determine if these factors played a role. More prospective studies must be done to assess if they contribute to nonunions in MIS hallux valgus correction. Surgeons should be aware of this risk and counsel patients appropriately.
Some literature suggests several benefits of MIS hallux valgus surgery over open procedures, including lower pain, less stiffness, and better cosmesis secondary to less soft tissue stripping.9,36 This review found that less pain and improved cosmesis were shown in several studies comparing MIS to open procedures for treatment of hallux valgus.9,36 The study by Torrent et al36 reported that compared with open procedures, pain was statistically significant less in MIS hallux valgus procedures based on VAS scores. In this review, cosmesis was shown to be better in the MIS group compared with the open group as well.9
Limitations
The limitations of this systematic review include that there were no randomized controlled trials that met our inclusion criteria. Additionally, different techniques including MIS techniques for correction of hallux valgus were done in various studies, not standardizing the surgical technique; however, they all did use the Shannon burr, performed distal metatarsal osteotomies, and had to have screw fixation. Controlling for the tool to do the osteotomy, location of the osteotomy, fixation techniques, and follow-up length improved the homogeneity of our data. We are unable to make a comparison between open vs MIS based on this study alone. It is possible that MIS cases were less severe and prone to selection bias; however, most studies reported comparable results between open and minimally invasive surgery when the criteria for procedure were the same. Heterogeneity among studies is another limitation of this review. Another limitation of this review is that some of the studies included only reported evidence on samples smaller than 50 patients. In addition, the AOFAS forefoot score is not validated; however, it is commonly used and helpful in most studies.
Conclusion
MIS for the treatment of hallux valgus using the Shannon burr appears to be a safe and effective therapy for hallux valgus correction. The outcomes of this technique show appropriate correction of the hallux valgus deformity, improvement in functional outcomes, high patient satisfaction, low recurrence rates, and acceptable complication rates. When patients fail nonsurgical therapy for hallux valgus, MIS may be an alternative to open surgical techniques. However, the higher complication rate should be taken into consideration when choosing an MIS approach compared to an open approach for hallux valgus correction. We hope this systematic review helps surgeons provide evidence-based guidelines and set expectations for their patients when considering using MIS hallux valgus correction with a Shannon burr.
Footnotes
Ethical Approval: Ethical approval was not sought for the present study because it is a systematic review.
The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Tyler Gonzalez, MD, MBA, reports consulting fees from Stryker, DJO, and Novastep. ICMJE forms for all authors are available online.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Tyler Gonzalez, MD, MBA,  https://orcid.org/0000-0002-3210-8097
https://orcid.org/0000-0002-3210-8097
Rodrigo Encinas, BS,  https://orcid.org/0000-0002-4033-9012
https://orcid.org/0000-0002-4033-9012
J. Benjamin Jackson III, MD, MBA,  https://orcid.org/0000-0002-9444-087X
https://orcid.org/0000-0002-9444-087X
References
- 1. Barg A, Harmer JR, Presson AP, Zhang C, Lackey M, Saltzman CL. Unfavorable outcomes following surgical treatment of hallux valgus deformity: a systematic literature review. J Bone Joint Surg Am. 2018;100(18):1563-1573. doi: 10.2106/JBJS.17.00975 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Brogan K, Lindisfarne E, Akehurst H, Farook U, Shrier W, Palmer S. Minimally invasive and open distal chevron osteotomy for mild to moderate hallux valgus. Foot Ankle Int. 2016;37(11):1197-1204. doi: 10.1177/1071100716656440 [DOI] [PubMed] [Google Scholar]
- 3. Burg A, Tal Frenkel R, Nyska M, Ohana N, Segal D, Palmanovich E. Treating hallux valgus associated metatarsus adductus by minimally invasive surgery: a simple solution for a difficult problem. J Foot Ankle Surg. 2022;61(5):1091-1097. doi: 10.1053/j.jfas.2022.01.027 [DOI] [PubMed] [Google Scholar]
- 4. Chan CX, Gan JZ, Chong HC, Rikhraj Singh I, Ng SYC, Koo K. Two year outcomes of minimally invasive hallux valgus surgery. Foot Ankle Surg. 2019;25(2):119-126. doi: 10.1016/j.fas.2017.09.007 [DOI] [PubMed] [Google Scholar]
- 5. de Carvalho KAM, Baptista AD, de Cesar Netto C, Johnson AH, Dalmau-Pastor M. Minimally invasive chevron-Akin for correction of moderate and severe hallux valgus deformities: clinical and radiologic outcomes with a minimum 2-year follow-up. Foot Ankle Int. 2022;43(10):1317-1330. doi: 10.1177/10711007221114123 [DOI] [PubMed] [Google Scholar]
- 6. Díaz Fernández R. Use of a percutaneous osteotomy with plate fixation in hallux valgus correction. Foot Ankle Surg. 2019;25(2):106-112. doi: 10.1016/j.fas.2017.09.002 [DOI] [PubMed] [Google Scholar]
- 7. Ezzatvar Y, López-Bueno L, Fuentes-Aparicio L, Dueñas L. Prevalence and predisposing factors for recurrence after hallux valgus surgery: a systematic review and meta-analysis. J Clin Med. 2021;10(24):5753. doi: 10.3390/jcm10245753 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Fraissler L, Konrads C, Hoberg M, Rudert M, Walcher M. Treatment of hallux valgus deformity. EFORT Open Rev. 2016;1(8):295-302. doi: 10.1302/2058-5241.1.000005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Frigg A, Zaugg S, Maquieira G, Pellegrino A. Stiffness and range of motion after minimally invasive chevron-Akin and open scarf-Akin procedures. Foot Ankle Int. 2019;40(5):515-525. doi: 10.1177/1071100718818577 [DOI] [PubMed] [Google Scholar]
- 10. Ghioldi ME, Chemes LN, Dealbera ED, De Prado M, Del Vecchio JJ. Modified Bösch osteotomy combined with a percutaneous adductor tendon release for the treatment of hallux valgus deformity: learning curve. Foot Ankle Spec. Published online March 3, 2022. doi: 10.1177/19386400221079198 [DOI] [PubMed] [Google Scholar]
- 11. Gutteck N, Haase K, Kielstein H, Delank KS, Arnold C. Biomechanical results of percutaneous calcaneal osteotomy using two different osteotomy designs. Foot Ankle Surg. 2020;26(5):551-555. doi: 10.1016/j.fas.2019.07.004 [DOI] [PubMed] [Google Scholar]
- 12. Higgins JP, Altman DG, Gøtzsche PC, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. doi: 10.1136/bmj.d5928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Higgins JPT, Thomas J, Chandler J, et al. , eds. Cochrane Handbook for Systematic Reviews of Interventions. 2nd ed. John Wiley & Sons; 2019. [Google Scholar]
- 14. Holme TJ, Sivaloganathan SS, Patel B, Kunasingam K. Third-generation minimally invasive chevron Akin osteotomy for hallux valgus. Foot Ankle Int. 2020;41(1):50-56. doi: 10.1177/1071100719874360 [DOI] [PubMed] [Google Scholar]
- 15. Ji L, Wang K, Ding S, Sun C, Sun S, Zhang M. Minimally invasive vs. open surgery for hallux valgus: a meta-analysis. Front Surg. 2022;9:843410. doi: 10.3389/fsurg.2022.843410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Jowett CRJ, Bedi HS. Preliminary results and learning curve of the minimally invasive chevron Akin operation for hallux valgus. J Foot Ankle Surg. 2017;56(3):445-452. doi: 10.1053/j.jfas.2017.01.002 [DOI] [PubMed] [Google Scholar]
- 17. Kurashige T. Radiographic and clinical results of minimally invasive chevron Akin osteotomy for moderate to severe hallux valgus deformities. Foot Ankle Spec. Published online October 6, 2021. doi: 10.1177/19386400211045911 [DOI] [PubMed] [Google Scholar]
- 18. Laffenêtre O, Millet-Barbé B, Darcel V, Lucas y, Hernandez J, Chauveaux D. Percutaneous bunionette correction: results of a 49-case retrospective study at a mean 34 months’ follow-up. Orthop Traumatol Surg Res. 2015;101(2):179-184. doi: 10.1016/j.otsr.2014.11.017 [DOI] [PubMed] [Google Scholar]
- 19. Laffenêtre O, Perera A. Distal minimally invasive metatarsal osteotomy (“DMMO” procedure). Foot Ankle Clin. 2019;24(4):615-625. doi: 10.1016/j.fcl.2019.08.011 [DOI] [PubMed] [Google Scholar]
- 20. Lai MC, Rikhraj IS, Woo YL, Yeo W, Ng YCS, Koo K. Clinical and radiological outcomes comparing percutaneous chevron-Akin osteotomies vs open scarf-Akin osteotomies for hallux valgus. Foot Ankle Int. 2018;39(3):311-317. doi: 10.1177/1071100717745282 [DOI] [PubMed] [Google Scholar]
- 21. Liszka H, Gądek A. Percutaneous transosseous suture fixation of the Akin osteotomy and minimally invasive chevron for correction of hallux valgus. Foot Ankle Int. 2020;41(9):1079-1091. doi: 10.1177/1071100720935036 [DOI] [PubMed] [Google Scholar]
- 22. Lu J, Zhao H, Liang X, Ma Q. Comparison of minimally invasive and traditionally open surgeries in correction of hallux valgus: a meta-analysis. J Foot Ankle Surg. 2020;59(4):801-806. doi: 10.1053/j.jfas.2019.03.021 [DOI] [PubMed] [Google Scholar]
- 23. Lucas y, Hernandez J, Golanó P, Roshan-Zamir S, Darcel V, Chauveaux D, Laffenêtre O. Treatment of moderate hallux valgus by percutaneous, extra-articular reverse-L Chevron (PERC) osteotomy. Bone Joint J. 2016;98-B(3):365-373. doi: 10.1302/0301-620X.98B3.35666 [DOI] [PubMed] [Google Scholar]
- 24. Marijuschkin I, Souza ML, Diaz JLG, Carvalho P. Percutaneous hallux valgus: an algorithm for the surgical treatment. Rev Bras Ortop (Sao Paulo). 2021;56(4):504-512. doi: 10.1055/s-0040-1721367 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Michels F, Demeulenaere B, Cordier G. Consensus in percutaneous bunionette correction. Orthop Traumatol Surg Res. 2021;107(6):102642. doi: 10.1016/j.otsr.2020.03.029 [DOI] [PubMed] [Google Scholar]
- 26. Mifsut-Miedes D, Rodríguez-Collell JR, Valverde-Navarro A, González-Soler EM. Percutaneous trapeziometacarpal arthrodesis in thumb carpometacarpal joint arthritis: a new surgical approach. Case Rep Orthop. 2021;2021:6881168. doi: 10.1155/2021/6881168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Mikhail CM, Markowitz J, Di Lenarda L, Guzman J, Vulcano E. Clinical and radiographic outcomes of percutaneous chevron-Akin osteotomies for the correction of hallux valgus deformity. Foot Ankle Int. 2022;43(1):32-41. doi: 10.1177/10711007211031218 [DOI] [PubMed] [Google Scholar]
- 28. Nix S, Smith M, Vicenzino B. Prevalence of hallux valgus in the general population: a systematic review and meta-analysis. J Foot Ankle Res. 2010;3:21. doi: 10.1186/1757-1146-3-21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Nunes GA, Ferreira GF, Baumfeld T, Filho MVP, Baumfeld D, Lam P. Minimally invasive chevron Akin: locking the metatarsal-cuneiform joint. Foot Ankle Spec. Published online February 22, 2022. doi: 10.1177/19386400221079155 [DOI] [PubMed] [Google Scholar]
- 30. Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi: 10.1136/bmj.n71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Perez Boal E, Becerro de Bengoa Vallejo R, Fuentes Rodriguez M, Lopez Lopez D, Losa Iglesias ME. Geometry of the proximal phalanx of hallux and first metatarsal bone to predict hallux abducto valgus: a radiological study. PLoS One. 2016;11(11):e0166197. doi: 10.1371/journal.pone.0166197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Reddy SC, Schipper ON, Li J. The effect of chilled vs room-temperature irrigation on thermal energy dissipation during minimally invasive calcaneal osteotomy of cadaver specimens. Foot Ankle Orthop. 2022;7(4):24730114221136548. doi: 10.1177/24730114221136548 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Singh MS, Khurana A, Kapoor D, Katekar S, Kumar A, Vishwakarma G. Minimally invasive vs open distal metatarsal osteotomy for hallux valgus - a systematic review and meta-analysis. J Clin Orthop Trauma. 2020;11(3):348-356. doi: 10.1016/j.jcot.2020.04.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological Index for Non-Randomized Studies (minors): development and validation of a new instrument. ANZ J Surg. 2003;73(9):712-716. doi: 10.1046/j.1445-2197.2003.02748.x [DOI] [PubMed] [Google Scholar]
- 35. Tay AYW, Goh GS, Koo K, Yeo NEM. Third-generation minimally invasive chevron-Akin osteotomy for hallux valgus produces similar clinical and radiological outcomes as scarf-Akin osteotomy at 2 years: a matched cohort study. Foot Ankle Int. 2022;43(3):321-330. doi: 10.1177/10711007211049193 [DOI] [PubMed] [Google Scholar]
- 36. Torrent J, Baduell A, Vega J, Malagelada F, Luna R, Rabat E. Open vs minimally invasive scarf osteotomy for hallux valgus correction: a randomized controlled trial. Foot Ankle Int. 2021;42(8):982-993. doi: 10.1177/10711007211003565 [DOI] [PubMed] [Google Scholar]
- 37. Trnka HJ. Percutaneous, MIS and open hallux valgus surgery. EFORT Open Rev. 2021;6(6):432-438. doi: 10.1302/2058-5241.6.210029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Trnka HJ, Krenn S, Schuh R. Minimally invasive hallux valgus surgery: a critical review of the evidence. Int Orthop. 2013;37(9):1731-1735. doi: 10.1007/s00264-013-2077-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Ying J, Xu Y, István B, Ren F. Adjusted indirect and mixed comparisons of conservative treatments for hallux valgus: a systematic review and network meta-analysis. Int J Environ Res Public Health. 2021;18(7):3841. doi: 10.3390/ijerph18073841 [DOI] [PMC free article] [PubMed] [Google Scholar]