Abstract
Background:
Ankle fractures are among the most common injuries treated by orthopaedic surgeons, yet little guidance exists in postoperative protocols for ankle fractures concerning time of immobilization. Here, we aim to investigate the association between early mobilization and patient-reported outcomes. Our null hypothesis was that no difference in Patient-Reported Outcomes Measurement Information System (PROMIS) scores would be identified in patients when comparing the effect of time of immobilization.
Methods:
A retrospective review identified ankle fractures that underwent surgical fixation between 2015 and 2020 at a level 1 trauma center and its associated facilities. One hundred nineteen patients from 9 providers met inclusion criteria for our final analysis. Forty-seven patients were immobilized for <6 weeks (early) and 68 patients were immobilized for ≥6 weeks (late). Our primary outcome measures included the PROMIS questionnaire, time of immobilization, and time to full weightbearing. Our secondary outcome measures included time to return to work, wound complications (infection, delayed healing), and complications associated with fracture fixation (loss of reduction, delayed union, reoperation, hardware failure). Repeated measures analysis of variance as well as linear mixed outcome regression were used to predict each of the PROMIS outcomes of anxiety, depression, physical function, and pain interference. Each model included the predictors of age, sex, race, body mass index (BMI), diabetes, rheumatoid arthritis, smoking status, payor, provider, time to radiographic union, time to return to work, time to full weightbearing, and early vs late immobilized groups.
Results:
We found no differences in PROMIS scores between mobilization groups even when controlling for possible confounders such as age, BMI, rheumatoid arthritis, smoking status, and diabetes mellitus (P > .05). Furthermore, we found no differences in complications associated with fracture fixation (P > .05). Across our cohort, lower physical function scores were associated with higher BMI, increasing age, and longer time to return to work/play (P < .05). Our analysis further showed that depression, anxiety, pain interference, and physical function levels improve as a function of time (P < .05). Higher BMI was also noted to have a significant impact on PROMIS depression and anxiety when controlling for other variables. African Americans had greater pain interference scores (P < .05).
Conclusion:
Our study suggests that early mobilization in a walker boot after operative treatment of ankle fractures is a safe alternative to casting in non-neuropathic patients. When considering operative treatment of ankle fractures, factors such as increasing age and BMI are likely to negatively affect postoperative anxiety, physical function, and depression PROMIS scores regardless of immobilization time.
Level of Evidence:
Level III, retrospective cohort study.
Keywords: early mobilization, ankle fracture, PROMIS
Introduction
Ankle fractures are one of the most common fractures treated by orthopaedic surgeons, accounting for 2.1 million (13%) of all fractures per year.3 Unstable ankle fractures are usually addressed via open reduction with internal fixation whereas stable injury patterns are best treated nonoperatively.4,13,16,25 Although the indications for and management of unstable ankle fractures are generally agreed upon, the postoperative rehabilitation protocols with respect to time to initiation of ankle range of motion and allowing full weightbearing continues to remain a subject of debate. Traditional postoperative fracture care has been nonweightbearing with cast immobilization for 6 weeks; however, recent studies have advocated for earlier mobilization in a walker boot for bimalleolar, trimalleolar, or unstable supination-external rotation fractures without syndesmotic injury.23 Proponents of earlier mobilization claim that this postoperative course results in decreased time to return to function and decreased incidence of muscle atrophy, pressure wounds, and joint stiffness that can be seen with casting.1,7,10,19,20 On the contrary, proponents of cast immobilization suggest that a period of ankle immobilization results in decreased surgical wound complications, decreased incidence of fracture displacement, and decreased pain during the initial phase of healing.15
Comparative studies investigating early mobilization to longer cast immobilization have yielded contradictory results.7,15 The aim of this study was to assess whether there is a difference in Patient-Reported Outcomes Measurement Information System (PROMIS) scores in patients that were removed from a cast or splint and allowed to mobilize the ankle at <6 weeks (early) compared to patients immobilized in a cast or splint ≥6 weeks (late). PROMIS has been validated as an outcome metric that allows patients to record a variety of symptoms.17 PROMIS has been widely used in prior studies and has compared favorably to or outperformed other outcome measures when it comes to capturing patient experience after orthopaedic procedures.11,14
Our null hypothesis was that no difference in PROMIS scores, complications, or radiographic union would be identified in patients when comparing the effect of time of immobilization.
Methods
Inclusion criteria for the study were patients with isolated unstable ankle fractures requiring open reduction and internal fixation, available medical records and imaging, and minimum 4 months’ follow-up. Patients with the following characteristics were excluded: open fractures, pilon fractures, revision cases, HbA1c > 8, peripheral neuropathy, neurologic injury, uncontrolled seizure disorder, less than 4 months’ follow-up, polytrauma, preexisting impaired mobility, initial use of ex-fix, and pregnancy (Table 1). After obtaining institutional review board’s approval, our billing database was surveyed for patients with the following combination of Current Procedural Terminology codes (27769, 27784, 27792, 27814, 27822, 27829) to identify patients with isolated unstable ankle fractures requiring open reduction and internal fixation from January 2015 to January 2020 (Figure 1). Eligible patients were then placed into their appropriate study group based on their duration of immobilization (early vs late) (Figure 1). Ankle fractures included were lateral malleolar fractures with ligamentous injury (bimalleolar-equivalent fractures), bimalleolar fractures, and trimalleolar or equivalent fractures. All surgeries were performed either by 4 fellowship-trained foot and ankle orthopaedic surgeons or 5 fellowship-trained trauma orthopaedic surgeons. We tabulated demographic data including age, gender, diabetes, rheumatoid arthritis, smoking status, ethnicity, and fracture type (Table 2). Records of identified patients were then reviewed to obtain our primary outcome measure, the prospectively collected PROMIS scores for physical function (PROMIS v2.0), pain interference (PROMIS v1.1), and depression (PROMIS v1.0). Scores were obtained in clinic prospectively during every postoperative visit via entry into a tablet given to each patient on arrival, at each postoperative visit. For purposes of this study, time of completion of the survey was approximated to 1, 3, 6, and 12 months postoperation. Survey responses closest to these time points were used for each patient. Secondary outcome measures included time to return to work, wound complications (infection, delayed healing, dehiscence), and complications associated with fracture fixation (loss of reduction of >2 mm change in position, time to union, reoperation, hardware failure) and was assessed by the treating surgeons during follow-up and recorded in the patient chart.
Table 1.
Inclusion and Exclusion Criteria for Enrollment of Patients Into the Study.
| Inclusion Criteria | Exclusion Criteria |
|---|---|
| Isolated and unstable malleolus fractures (ie, lateral or medial malleolar fractures) | Open fractures |
| Pilon fractures | |
| Revision cases | |
| Bimalleolar/trimalleolar fractures | HbA1c > 8 mg/dL |
| <4 mo of follow-up | |
| Maisonneuve fractures | Polytrauma |
| Uncontrolled seizure disorder | |
| Available records/imaging | Peripheral neuropathy |
| Neurologic injury | |
| Minimum 4 mo of follow-up | Pregnancy |
| Initial use of external fixation |
Figure 1.

Flow diagram demonstrating study design.
Table 2.
Baseline Characteristics of Study Population.a
| Characteristics | Overall | Early | Late | P Value |
|---|---|---|---|---|
| Time of immobilization, mean ± SE | 4.87 ± 0.1 | 3 ± 0.11 | 6.16 ± 0.06 | <.001 |
| Age, mean ± SD | 66 ± 16.66 | 40.77 ± 13.75 | 52.69 ± 16.84 | <.001 |
| BMI, mean ± SD | 31.6 ± 7.52 | 31.27 ± 7.52 | 31.75 ± 7.59 | .79 |
| Gender | ||||
| M | 40 (35) | 22 (47) | 18 (26) | .02 |
| F | 75 (65) | 25 (53) | 50 (74) | |
| Race | ||||
| Black | 13 (11) | 7 (15) | 6 (9) | .36 |
| White | 95 (83) | 36 (77) | 59 (87) | |
| Asian/Hispanic/other | 7 (6) | 4 (8) | 3 (4) | |
| Diabetes | ||||
| Yes | 7 (6) | 4 (9) | 3 (4) | .37 |
| No | 108 (94) | 43 (91) | 65 (96) | |
| Rheumatoid arthritis | ||||
| Yes | 2 (2) | 1 (2) | 1 (1) | .79 |
| No | 113 (98) | 46 (98) | 67 (99) | |
| Smoker | ||||
| Yes | 11 (10) | 7 (15) | 4 (6) | .11 |
| No | 104 (90) | 40 (85) | 64 (94) | |
| Fracture | ||||
| Uni- or bimalleolar equivalent | 48 (42) | 22 (47) | 26 (38) | .16 |
| Bimalleolar | 46 (40) | 14 (30) | 32 (47) | |
| Trimalleolar | 21 (18) | 11 (23) | 10 (15) | |
Abbreviation: BMI, body mass index.
Unless otherwise noted, values are n (%). P values in bold indicate statistical significance (P < .05).
Postoperative Course
All patients at the time of surgery were placed in a well-padded short leg splint postoperatively. They were kept nonweightbearing to allow the incisions to heal. Suture removal was performed at least 2 weeks postoperatively when deemed to be healing appropriately. After the first postoperative visit, the patients were either placed back in a short leg fiberglass cast until at least the 6-week mark (late mobilization group) or in a walker boot (early mobilization group). The decision to use either protocol was dependent on surgeon preference and/or expert opinion.
Patients in the late mobilization group were placed in a short leg fiberglass cast at their first postoperative visit and were instructed to remain nonweightbearing until the next follow-up (at least 6 weeks of total immobilization). Typically, at the 6-week postoperative visit, their cast was removed, and patients were placed in a walker boot. They were instructed to remove the boot and perform ankle range of motion exercises and begin full weightbearing in the boot. These patients were prescribed physical therapy for ROM and strengthening. They were also instructed to wean the boot over the next 2-4 weeks as tolerated, at which time they were allowed to transition into a regular shoe.
Patients in the early mobilization group were placed in a walker boot at their first postoperative visit and were instructed to remain nonweightbearing. They were instructed at their first postoperative visit to remove the boot and perform ankle range of motion exercises as well and prescribed physical therapy. Full weightbearing in the boot was allowed between 4 and 6 weeks postoperatively based on surgeon discretion.
A variety of fixation constructs were used consisting of lag screws and neutralization or bridge plates. Surgical constructs were determined by the treating surgeon preference and fracture pattern. The first postoperative visit was typically scheduled for 2 or 3 weeks after surgery and subsequent appointments were scheduled as close as possible to the 6-week, 3-month, 6-month, and 12-month mark. Follow-up periods were at the discretion of the treating surgeons.
Radiographic Review
Postoperative ankle radiographs were reviewed in this study by 4 fellowship-trained orthopaedic foot and ankle surgeons. Weightbearing postoperative radiographs closest to 3 months and 6 months were evaluated for complications associated with fracture fixation (loss of reduction, presence of union at 3 or 6 months, hardware failure). If radiographs demonstrated union and intact hardware at 3 months, then the 6-month radiographs (or last available radiograph if <6 months) were not evaluated. If, however, union was not achieved by 3 months, then additional radiographs closest to the 6-month mark were evaluated to determine union or other complications associated with fracture fixation.
Statistical Analysis
The data were analyzed using R, version 4.1 (R Foundation for Statistical Computing, Vienna, Austria). An unequal variance t test was used to identify differences between 2 means. A chi-squared test was used for categorical values such as fracture union. A one-way analysis of variance was used to identify differences between more than 2 means. Repeated measures analysis of variance with post hoc paired t tests were used to determine a difference over time between the same variable. An analysis using PROMIS score variables adjusting for age, BMI, smoking status, diabetes status, and rheumatoid arthritis was performed using a linear mixed effects regression model, and post hoc power analyses were obtained. All graphs generated have 95% CI ranges represented graphically. A P value of <.05 was used for significance level for all tests. Missing PROMIS data were dropped from the analysis.
Two post hoc power analyses were performed, the first analysis demonstrated that sufficient pairs (n = 115) were available to detect an effect size as small as 0.23 in a study with power of 0.8. The second analysis performed found that there were enough observations to detect an effect as small as 0.43 for independent comparisons with study power of 0.8. These effect sizes range from small (0.2) to medium (0.5).
Results
Demographics
A total of 115 patients were included in the study. The early immobilization group was immobilized for 3 ± 0.11 (SE) weeks and the late group immobilized for 6.16 ± 0.06 (SE) weeks, which was a statistically significant difference (P < .001). Forty patients were male, and 75 patients were female. A statistically significant difference was noted in gender between the 2 groups (P < .01; Table 2). The average age in the early and late groups were 40.8 and 52.7 years, respectively, which represented a statistically significant difference (P < .01) (Table 2). Body mass index (BMI) was calculated for both groups, early (30.52) and late (31.75) (P = .57), with a range of 20.66-55.79 (Table 2). Ninety-five patients were Caucasian (36 early, 59 late), 13 were Black (7 early, 6 late), 7 Asian/Hispanic/Other (4 early, 3 late), with no significant difference in early vs late treatment between the groups (P = .36; Table 2). There were 11 smokers included in the study, 7 in the early group and 4 in the late group (P = .11; Table 2). There were 7 diabetes patients in the study, 4 in the early group and 3 in the late group, which was not significantly different between groups (P = .37; Table 2). Ankle fractures included in the study were lateral malleolar fractures with ligamentous injury (bimalleolar-equivalent fractures), bimalleolar fractures, and trimalleolar or equivalent fractures. No significant difference in fracture types were identified between treatment groups (P = .11; Table 2). Two patients in the study had rheumatoid arthritis, 1 in either group (Table 2).
Return to Work and Sport
For the early mobilization group, return to work/play was 4.81 weeks as opposed to 5.61 weeks for the late mobilization groups(P < .01). The range was between 2 and 7.5 weeks in the early mobilization group and 2.5 and 13 weeks for the late mobilization group.
PROMIS Outcomes Between Mobilization Groups
After the 3-month postoperative visit, 9 patients in the early group and 8 patients in the late group did not have PROMIS scores available for the 6-month visit. Eight of these patients did have 1-year PROMIS scores available, leaving only 9 patients who had not completed at least 3 postoperative PROMIS questionnaires in the study. Between mobilization groups, no significant difference in mean pain interference, physical function, anxiety, or depression measures were identified at any time point (P > .05; Figure 2).
Figure 2.
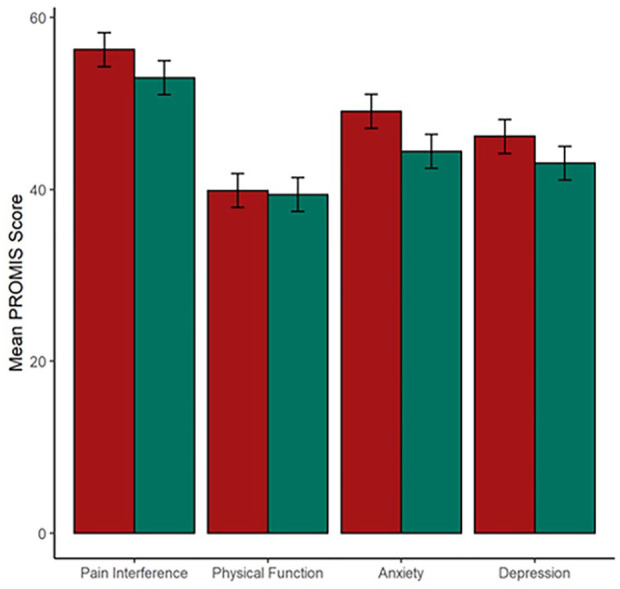
PROMIS outcomes between immobilization groups. Red: early immobilization (<6 weeks); green: late immobilization (>6 weeks). Ranges represent 95% CI. PROMIS, Patient-Reported Outcomes Measurement Information System.
Our data showed that at final follow up, higher BMI, increasing age, and longer time to return to work/sport were associated with lower physical function scores (P < .05). When both groups were pooled together, depression, anxiety, and pain interference levels improved over time among all study participants (P < .05) (Figures 3-5); however, these effects were not seen when a multivariate analysis was performed. Higher pain interference scores were noted for African Americans compared with other groups of patients (F = 5.02, P = .010; 95% CI 0.03, 0.31). There was no difference in union rates between the early and late mobilization groups.
Figure 3.

PROMIS anxiety as a function of time. Ranges represent 95% CI. ns, not significant; PROMIS, Patient-Reported Outcomes Measurement Information System. *P < .05. **P < .01. ****P < .0001.
Figure 4.

PROMIS pain interference as a function of time. Ranges represent 95% CI. ns, not significant; PROMIS, Patient-Reported Outcomes Measurement Information System. *P < .05. **P < .01. ****P < .0001.
Figure 5.

PROMIS depression as a function of time. Ranges represent 95% CI. ns, not significant; PROMIS, Patient-Reported Outcomes Measurement Information System. ****P < .0001.
Multivariate analyses were performed using a linear regression model for both study groups to look at the effect of BMI and diabetes on PROMIS scores (Figures 6-9). For the PROMIS measure of anxiety, lower anxiety scores were noted from the 1-month to the 3-month postoperative visit (P = .004, 95% CI −8.59 to −1.68, β −5.14) and a reduction from the 1-month to the 6-month postoperative visit (P = .01, 95% CI −8.99 to −1.25, β −5.12), respectively.
Figure 6.

Adjusted anxiety PROMIS scores between mobilization groups at varying time points. Red: early immobilization(<6 weeks); green: late immobilization (>6 weeks). Ranges represent 95% CI. PROMIS, Patient-Reported Outcomes Measurement Information System. **P < .01. ***P < .001.
Figure 7.

Adjusted PROMIS depression scores between mobilization groups at varying time points. Red: early immobilization (<6 weeks); green: late immobilization (>6 weeks). Ranges represent 95% CI. PROMIS, Patient-Reported Outcomes Measurement Information System. ***P < .001.
Figure 8.

Adjusted PROMIS physical function scores between mobilization groups at varying time points. Red: early immobilization (<6 weeks); green: late immobilization (>6 weeks). Ranges represent 95% CI. PROMIS, Patient-Reported Outcomes Measurement Information System. ***P < .001.
Figure 9.

Adjusted PROMIS pain interference scores between mobilization groups at varying time points. Red: early immobilization (<6 weeks); green: late immobilization (>6 weeks). Ranges represent 95% CI. PROMIS, Patient-Reported Outcomes Measurement Information System. *P < .05.
Age and BMI were found to independently impact physical function scores when other variables were controlled (P = .002, 95% CI −0.25 to −0.06, β −0.15, and P = .002, 95% CI −0.48 to −0.1, β −0.29, respectively). Multivariate analysis of pain interference demonstrated improvement with pain over time but no clinically relevant difference between mobilization groups by the end of the follow-up period (Figure 9). However, for the early group, there was a significant reduction in pain interference from the 1-month postoperative visit to the 3-month (P = .019, 95% CI −7.8 to −0.72, β −4.27) and 6-month (P = .001, 95% CI −10.98 to −3.06, β −7.02) postoperative visits.
Complications
All patients in the study maintained radiographic alignment. At 3 months there was no statistical difference in union rate, with 76.6% and 81% in the early and late mobilization groups, respectively (P = .45, χ2 0.56). All patients had evidence of radiographic healing by 6 months after surgery. Hardware failure was a rare occurrence in the study and was present in 2 patients in the early group vs 4 in the late mobilization group, which did not reach significance (P = .63, χ2 0.22). There was a statistically significant difference in the number of wound complications among groups (P = .03, χ2 4.54), with no wound complications in the early mobilization group and 6 in the late mobilization group, none of which required repeat surgery for irrigation and debridement. One patient required removal of their syndesmotic screw because of ankle stiffness. There were no differences in complications associated with fracture fixation noted between mobilization groups (P > .05).
Discussion
This study demonstrates that there were no differences in PROMIS scores between early and delayed mobilization following ankle fracture surgery. However, it must be noted that the study population varied in age and gender with a significantly younger patient population in the early mobilization group and significantly more women in the late group than the early group. Given this disparity regarding age between the study groups, a regression analysis was performed controlling for age. The findings indicated that age does affect PROMIS measures of anxiety, physical function, and depression in the overall group but did not result in a difference in PROMIS scores between the 2 groups. In addition, patients in the early mobilization group were not at an increased risk for hardware failure. These findings are consistent with prior reports that also demonstrated no difference in functional outcomes between early vs delayed mobilization.2,6,8,9
Historically, postoperative rehabilitation following ankle fracture surgery includes delayed mobilization. Recently, however, the temporal relationship of mobilization following surgery has been challenged with many in favor of early mobilization.7,9,20,24 Dehghan et al7 demonstrated in their study that there was no difference in range of motion, return to work, and hardware failures between early vs late weightbearing groups for unstable ankle fractures. Other studies have demonstrated that early mobilization and early weightbearing theoretically allows young active patients to return to work earlier, minimizes disability, and may even have superior patient satisfaction scores.5,7 Lehtonen et al15 demonstrated a significant difference in postoperative complications in favor of cast immobilization, with an overall complication rate of 66% in the early mobilization group compared with 16% in the delayed mobilization group. Most of these complications were wound complications such as superficial infection, deep wound infection, and wound dehiscence. It should be noted that patients in the early mobilization group of this study were placed into a functional Air-Stirrup ankle brace (Aircast) immediately following the procedure. This contrasts with our study, where every patient was immobilized in a splint at least until the first postoperative visit and placed in a controlled ankle motion boot following this. Several other previous studies have demonstrated early postoperative adverse events favoring cast immobilization, with many adverse events being issues with surgical wound healing.12,15 Although we did not observe improved PROMIS scores in the early mobilization group, we did observe a significant difference in wound complications, with the early mobilization group reporting no wound complications as opposed to 6 observed in the late mobilization group. It should be noted that our late mobilization group was significantly older, which can be considered a predisposing factor to wound complications. It must also be stated that we excluded patients with uncontrolled diabetes and open ankle fractures, as such, our findings cannot be extrapolated to these patient populations with potential for increased risk of wound complication. In a meta-analysis by Sernandez et al,18 there were differences in outcomes and no differences related to wound complications once stable fixation was achieved.
Regarding time to fracture union and hardware failure, our study demonstrated no difference in time to fracture union between the mobilization groups. Dehghan et al7 in a randomized controlled trial corroborated these findings, reporting no cases of loss of reduction or hardware failure in either group. In another study by Simanski et al,20 it was shown that an early weightbearing group demonstrated equivalent rates of healing compared to a later weightbearing group, with only one pseudarthrosis developing in a patient in the late mobilization group.
Physical function scores though not significantly different between mobilization groups were worse in patients with higher BMI, increasing age, and increased time to return to work. This was further supported by our study’s multivariate analysis, which showed that when other variables were controlled for, age and BMI independently affected physical function. These findings are corroborated by Stavem et al22 and Simske et al21 showing a relationship between higher BMI and age to lower functional outcomes and increased complication rates. It may be hypothesized that these factors may lead to lower functional results and should be routinely discussed while counseling patients preoperatively.
Our study illustrates that levels of depression, anxiety, and physical function improve over time (P < .05). Our multivariate analysis showed that BMI is an independent predictor of higher PROMIS anxiety and depression. This association has not been well studied in orthopaedic literature.
Although data were collected in a prospective nature at each postoperative visit, the study design and analysis were retrospective in nature. This did not allow for randomization or anonymizing to occur. Groups were mostly based on already established postoperative protocols. PROMIS data, as the name suggests, comes directly from patients and requires some interpretation and introspection into the appropriate responses. Randomized trials would be required to address these limitations. Our groups were found to be demographically different, with the late mobilization group having a significantly higher proportion of women and were found to be significantly older (52.7 years) compared with the early group (40.8 years), which may have an impact on our results. Another limitation of our study is an inconsistent period of immobilization among patients in each group. Immobilization only differed by an average of 3 weeks between the groups (3 ± 0.11 [SE] weeks for the early group and 6.16 ± 0.06 [SE] weeks for the late group). This may not be sufficient time to demonstrate a clear clinical difference in any of the primary and secondary outcomes studied. Additional prospective and randomized trial would be beneficial in clearly identifying any PROMIS score differences between these postoperative protocols. Additionally, based on the injury pattern and baseline level of function, the treating surgeons likely adapted their postoperative protocol to account for these factors, thereby biasing the results.
Prior to PROMIS, the visual analog scale was one tool used to quantify pain at different time periods of recovery. With PROMIS, pain interference is felt to be a more useful tool to quantify how much pain prevents patients from carrying out daily activities and it correlates closely with legacy measures such as visual analog scale.
It is unclear why African Americans in our study had significantly higher pain interference than other patients. No studies currently exist studying pain interference in African Americans or other racial minority groups. This finding remains an area for future investigation into contributing factors such as microaggressions, access to physical therapy or differences in perioperative expectations such as pain level, and time of recovery. It is clear, however, that proper preoperative counseling is important not only in this group but across all patients to ensure that expectations are appropriately set.
Conclusion
The current study demonstrated that after controlling for multiple confounding factors, there was no significant difference regarding pain interference, physical function, anxiety, or depression between patients who were immobilized in a cast for ≥6 weeks than those immobilized in a boot for <6 weeks following ankle fracture surgery. Regarding wound complications and complications associated with fracture fixation, there also was no significant difference between the 2 groups. This is true when controlling for factors such as age, BMI, smoking status, diabetes mellitus, and rheumatoid arthritis. Our study does suggest that early mobilization in a walker boot after operative treatment of ankle fractures is a safe alternative to casting in nonneuropathic patients.
Footnotes
Ethical Approval: Ethical approval for this study was obtained from IRB#202002028.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. ICMJE forms for all authors are available online.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Dwayne D. Carney, MD, MPH,  https://orcid.org/0000-0002-0646-6966
https://orcid.org/0000-0002-0646-6966
Jeffrey E. Johnson, MD,  https://orcid.org/0000-0003-2055-9998
https://orcid.org/0000-0003-2055-9998
Sandra E. Klein, MD,  https://orcid.org/0000-0003-2416-1186
https://orcid.org/0000-0003-2416-1186
Jonathon D. Backus, MD,  https://orcid.org/0000-0003-2426-170X
https://orcid.org/0000-0003-2426-170X
References
- 1. Ağır İ, Tunçer N, Küçükdurmaz F, Gümüstaş S, Akgül ED, Akpinar F. Functional comparison of immediate and late weight bearing after ankle bimalleolar fracture surgery. Open Orthop J. 2015;9:188-190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Ahl T, Dalén N, Lundberg A, Bylund C. Early mobilization of operated on ankle fractures. Prospective, controlled study of 40 bimalleolar cases. Acta Orthop Scand. 1993;64(1):95-99. [DOI] [PubMed] [Google Scholar]
- 3. American Academy of Orthopaedic Surgeons. The Burden of Musculoskeletal Diseases in the United States. American Academy of Orthopaedic Surgeons; 2008. [Google Scholar]
- 4. Bauer M, Jonsson K, Nilsson B. Thirty-year follow-up of ankle fractures. Acta Orthop Scand. 1985;56:103-106. [DOI] [PubMed] [Google Scholar]
- 5. Black JD, Bhavikatti M, Al-Hadithy N, Hakmi A, Kitson J. Early weight-bearing in operatively fixed ankle fractures: a systematic review. Foot (Edinb). 2013;23(2-3):78-85. doi: 10.1016/j.foot.2013.05.002 [DOI] [PubMed] [Google Scholar]
- 6. Cimino W, Ichtertz D, Slabaugh P. Early mobilization of ankle fractures after open reduction and internal fixation. Clin Orthop Relat Res. 1991;267:152-156. [PubMed] [Google Scholar]
- 7. Dehghan N, McKee MD, Jenkinson RJ, et al. Early weightbearing and range of motion versus non-weightbearing and immobilization after open reduction and internal fixation of unstable ankle fractures: a randomized controlled trial. J Orthop Trauma. 2016;30(7):345-352. [DOI] [PubMed] [Google Scholar]
- 8. DiStasio AJ, Jaggears FR, DePasquale LV, Frassica FJ, Turen CH. Protected early motion versus cast immobilization in postoperative management of ankle fractures. Contemp Orthop. 1994;29(4):273-277. [PubMed] [Google Scholar]
- 9. Dogra AS, Rangan A. Early mobilisation versus immobilisation of surgically treated ankle fractures. Prospective randomised control trial. Injury. 1999;30(6):417-419. [DOI] [PubMed] [Google Scholar]
- 10. Firoozabadi R, Harnden E, Krieg JC. Immediate weightbearing after ankle fracture fixation. Adv Orthop. 2015;2015:491976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Gausden EB, Levack A, Nwachukwu BU, Sin D, Wellman DS, Lorich DG. Computerized adaptive testing for patient reported outcomes in ankle fracture surgery. Foot Ankle Int. 2018;39(10):1192-1198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Hedström M, Ahl T, Dalén N. Early postoperative ankle exercise. A study of postoperative lateral malleolar fractures. Clin Orthop Relat Res. 1994;300:193-196. [PubMed] [Google Scholar]
- 13. Kristensen KD, Hansen T. Closed treatment of ankle fractures. Stage II supination-eversion fractures followed for 20 years. Acta Orthop Scand. 1985;56:107-109. [DOI] [PubMed] [Google Scholar]
- 14. Lash N, Horne G, Fielden J, Devane P. Ankle fractures: functional and lifestyle outcomes at 2 years. ANZ J Surg. 2002;72(10):724-730. [DOI] [PubMed] [Google Scholar]
- 15. Lehtonen H, Jarvinen TL, Honkonen S, Nyman M, Vihtonen K, Järvinen M. Use of a cast compared with a functional ankle brace after operative treatment of an ankle fracture. A prospective, randomized study. J Bone Joint Surg Am. 2003;85(2):205-211. [DOI] [PubMed] [Google Scholar]
- 16. Michelson JD. Ankle fractures resulting from rotational injuries. J Am Acad Orthop Surg. 2003;11(6):403-412. [DOI] [PubMed] [Google Scholar]
- 17. Segal G, Elbaz A, Parsi A, et al. Clinical outcomes following ankle fracture: a cross-sectional observational study. J Foot Ankle Res. 2014;7(1):50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Sernandez H, Riehl J, Fogel J. Do early weight-bearing and range of motion affect outcomes in operatively treated ankle fractures: a systematic review and meta-analysis. J Orthop Trauma. 2021;35(8):408-413. doi: 10.1097/BOT.0000000000002046 [DOI] [PubMed] [Google Scholar]
- 19. Shaffer MA, Okereke E, Esterhai JL, et al. Effects of immobilization on plantar-flexion torque, fatigue resistance, and functional ability following an ankle fracture. Phys Ther. 2000;80(8):769-780. [PubMed] [Google Scholar]
- 20. Simanski CJ, Maegele M, Lefering R, et al. Functional treatment and early after an ankle fracture: a prospective study. J Orthop Trauma. 2006;20(2):108-114. [DOI] [PubMed] [Google Scholar]
- 21. Simske NM, Benedick A, Audet MA, Vallier HA. Ankle fractures in patients over age 55 years: predictors of functional outcome. OTA Int. 2020;3(3):e080. doi: 10.1097/OI9.0000000000000080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Stavem K, Naumann MG, Sigurdsen U, Utvåg SE. The association of body mass index with complications and functional outcomes after surgery for closed ankle fractures [published correction appears in Bone Joint J. 2017 Dec;99-B(12 ):1696]. Bone Joint J. 2017;99-B(10):1389-1398. doi: 10.1302/0301-620X.99B10.BJJ-2016-1038.R1 [DOI] [PubMed] [Google Scholar]
- 23. Swart E, Bezhani H, Greisberg J, Vosseller JT. How long should patients be kept non-weight bearing after ankle fracture fixation? a survey of OTA and AOFAS members. Injury. 2015;46(6):1127-1130. [DOI] [PubMed] [Google Scholar]
- 24. Thomas G, Whalley H, Modi C. Early mobilization of operatively fixed ankle fractures: a systematic review. Foot Ankle Int. 2009;30(7):666-674. doi: 10.3113/FAI.2009.0666 [DOI] [PubMed] [Google Scholar]
- 25. Yde J, Kristensen KD. Ankle fractures: supination-eversion fractures of stage IV. Primary and late results of operative and non-operative treatment. Acta Orthop Scand. 1980;51:981-990. [DOI] [PubMed] [Google Scholar]


