Abstract
Background:
Osteochondral autograft transfer (OAT) is a useful technique for full-thickness cartilage lesions of the distal femur. Various techniques recommend harvesting a plug 2 mm longer than the recipient hole to allow for graft impaction. Grafts with limited compressibility may not sit flush when impacted.
Purpose:
To compare the compressibility/shortening of OAT donor plug regions from the distal femur of human cadaveric knees after impaction.
Study Design:
Controlled laboratory study.
Methods:
A total of 20 cadaveric knees (mean age, 70.3 ± 8.4 years) were divided into 4 donor regions: medial intercondylar (IC) notch, lateral IC notch, medial trochlea, and lateral trochlea. Each region was subdivided into 4 zones: far superior (FSZ), middle superior (MSZ), middle inferior (MIZ), and far inferior (FIZ). A total of 320 grafts (6-mm diameter, 15-mm depth) were extracted, and a custom-built machine was used to strike the graft 5 times using a predetermined energy of 0.11 J. The graft length was measured initially and after each impact. Statistical analysis of the compressibility for each of the 4 regions and all 16 zones was performed utilizing analysis of variance, with post hoc testing using the Fisher’s least significant difference.
Results:
Compression in the lateral IC notch, medial IC notch, medial trochlea, and lateral trochlea was 2.4 ± 1.5, 2.1 ± 0.7, 3.1 ± 2.2, and 2.1 ± 0.6 mm, respectively, with significant differences between the 4 regions (P < .01) and the most compression in the medial trochlea (P < .01). Subgroup analysis showed that the lateral trochlea had higher compressibility for FIZ versus MIZ (P = .02) and the lateral IC notch had higher compressibility for FSZ versus FIZ and MIZ (P < .05 for both).
Conclusion:
Compressibility varied between OAT donor sites in the distal femur. OAT donor grafts showed the highest compressibility in the medial trochlea (3.1 mm) and lateral IC notch FSZ (3.0 mm).
Clinical Relevance:
The lateral trochlea, medial IC notch, and the lower zones of the lateral IC notch grafts should not be oversized more than 2 mm in length, as these grafts may not compress adequately.
Keywords: articular cartilage, biomechanics articular cartilage, compressibility, knee, osteochondral autograft transplant (OAT)
Cartilage defects in the knee can lead to significant patient morbidity. Patients with focal cartilage defects have pain and functional limitations that affect their quality of life similarly to patients with severe osteoarthritis, which can make treatment challenging as these patients are often younger and more active. 12,26 Various surgical options exist for treating cartilage lesions, with osteochondral autograft transfer (OAT) representing an option that replaces both bone and cartilage. 35 Single-plug OAT and mosaicplasty have shown successful outcomes at long-term follow-up with better clinical outcomes and higher level of athletic activity when compared with microfracture. 7,18,24,31
OAT is used for full-thickness cartilage lesions of the distal femur between 1 and 2 cm in diameter. 1,5,30 Nonweightbearing or minimal weightbearing areas of the knee are an ideal area for graft harvest in an attempt to minimize donor site morbidity. 5,7,35 The medial trochlea is considered a preferred donor site due to low contact pressures and convex surface that mimics the weightbearing region of the condyles. 26 While uncommon, donor site morbidity does still occur where harvest sites have overgrown or underfilled with fibrocartilage that replaces the hyaline cartilage and subchondral bone that was harvested. 19 Ideally, an OAT graft would sit flush in the recipient site with respect to cartilage contour and thickness. 21 Various techniques recommend harvesting a plug 1 to 2 mm longer than the recipient hole to allow for graft impaction. 4,10,29 A clinical dilemma exists with regard to leaving an osteochondral plug slightly proud versus subjecting the graft to additional force to seat the graft flush with the surrounding articular cartilage. Thus, a further understanding of the compressibility of the different regions of the distal femur would be advantageous for a surgeon to understand when considering harvest sites for OAT procedures.
The primary objective of this study was to compare the compressibility/shortening of OAT donor plug regions from the distal femur of human cadaver knees after impaction. We hypothesized there would be a difference in compression of grafts from different areas of the knee which leads to our secondary objective, to determine which donor sites are more suitable in terms of providing the most compressibility.
Methods
Before testing, a systematic approach was devised for naming the areas of the knee being tested. Each knee was divided into 4 regions (medial intercondylar [IC] notch, lateral IC notch, medial trochlea, lateral trochlea). These 4 donor regions were chosen due to their location as they involve minimal or no weightbearing and are therefore deemed to be adequate sites to use in the OAT procedure. Each region was subdivided into 4 zones: far superior (FSZ), middle superior (MSZ), middle inferior (MIZ), and far inferior (FIZ) to yield a total of 16 donor grafts per knee (Figure 1).
Figure 1.
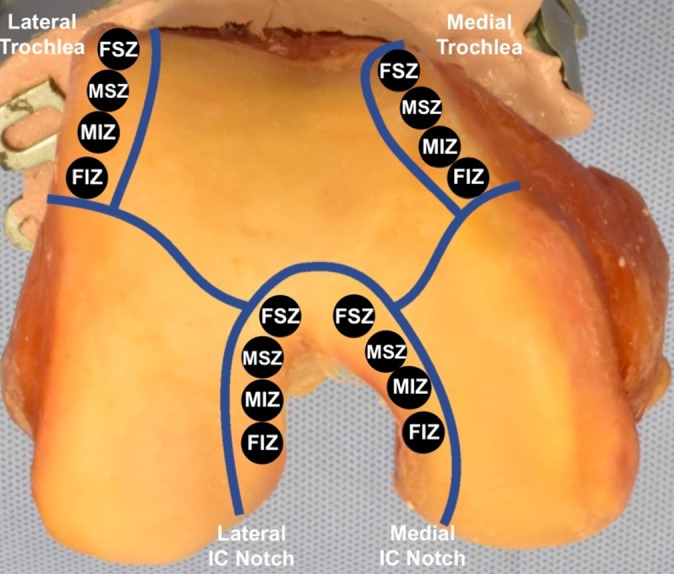
Distal view of a cadaveric right femur showing the naming conventions and locations of the graft harvest sites. Each region was subdivided into 4 zones. FIZ, far inferior zone; FSZ, far superior zone; IC, intercondylar; MIZ, middle inferior zone; MSZ, middle superior zone.
To test the compressibility of the grafts, 20 cadaver knees were used (13 right knees and 7 left knees). A total of 14 cadaver knees were male, and 6 were female. The mean age of the cadaver knees was 70.3 years ± 8.4 (range, 55-89 years). A total of 320 grafts were extracted using an OATS Kit (Arthrex) at 6 mm diameter and 15 mm depth in accordance with manufacturer recommendations. Older cadavers were not excluded due to previous evidence that showed no correlation between age and biomechanical properties (crush strength and trabecular bone stiffness) in the femur condyles. 6,28
Once extracted, the donor grafts were labeled according to their zone, number, and the cadaveric knee from which they were harvested. Careful labeling was done to ensure that the donor graft being tested was the same one extracted. A custom-made apparatus was assembled to perform the compressibility testing of the grafts with a 6.5 mm–diameter cylinder socket (Figure 2). The 6 mm–diameter instrumented cylinder mallet, with a mass of 11 oz (312 g), was dropped from a height of 37.4 mm, which resulted in an energy of 0.11. The height and weight of the custom apparatus were chosen carefully after ample testing to donor grafts. The height and weight provided optimum results for this experiment, while also limiting the amount of grafts that would crack from the force. This predetermined force was taken from a calibration of an orthopaedic surgeon performing the same operation to simulate the compression when placing a donor graft into a recipient site. Each graft was struck 5 times. At the end of each hit, the reduction in height of the graft was measured through the position of the mallet recorded in real time through a laser-distance sensor micrometer (LMI Technologies). The cartilage plugs were also inspected for cracks after each hit. The number of strikes delivered to the graft was selected based on trials conducted before the experiment using a force that was acquired by an orthopaedic surgeon doing this procedure. Five hits allowed maximum compression of the grafts without developing cracks. The experiment was limited to only 5 hits because more hits would have increased the likelihood of developing cracks in the grafts, greatly limiting our data. The graft lengths were then compiled and analyzed using WinDaq acquisition software (DATAQ Instruments), from which the average final length, average total compression, and average compression percentage along with their respective standard deviations were determined for each of the 16 zones.
Figure 2.
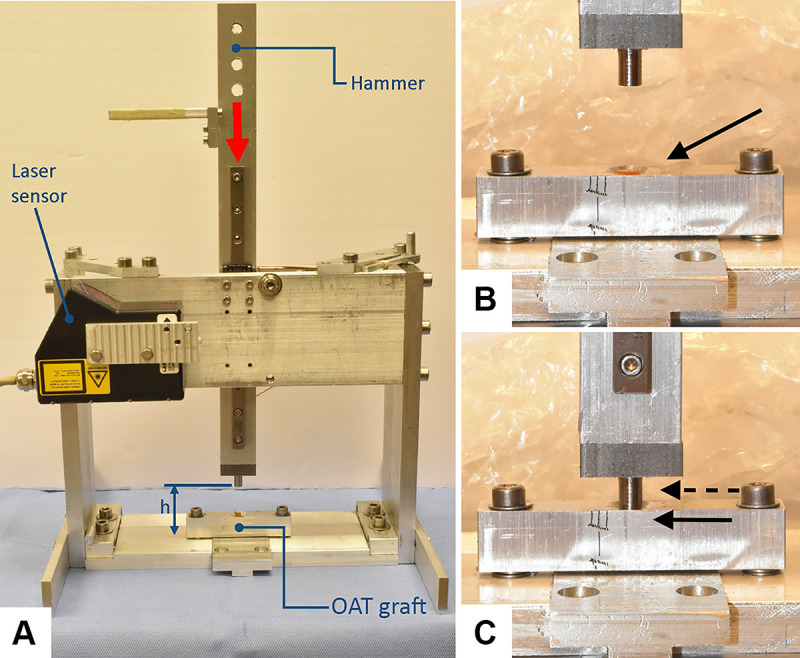
(A) Custom apparatus designed to deliver a predetermined force to determine compressibility of OAT grafts. The red arrow demonstrates the vector of the force of the hammer, and h represents the distance from the mallet to the rigid base supporting the graft. (B) Well containing at OAT plug (black arrow) before being struck by predetermined force. (C) Well (black arrow) containing an OAT plug after being struck by a predetermined force and solid cylinder (dashed arrow). OAT, osteochondral autograft transfer.
Statistical Analysis
Numerical data among the 4 different regions and 16 different zones were compared using analysis of variance (ANOVA). Post hoc analysis between regions was performed with the Fisher’s least significant difference test.
Results
The compression values for the medial IC notch, lateral IC notch, medial trochlea, and lateral trochlea are shown in Table 1. There was a significant difference in the amount of compression between all 4 regions (P < .01), and the medial trochlea had significantly more compression than each of the 3 other regions (P < .01 for all) (Table 1).
Table 1.
Compression Values of the 4 Donor Regions a
| Region | Compression, mm |
|---|---|
| Medial IC notch | 2.11 ± 0.84 |
| Lateral IC notch | 2.41 ± 1.22 |
| Medial trochlea | 3.11 ± 1.5* |
| Lateral trochlea | 2.06 ± 0.78 |
a Data are reported as mean ± SD. IC, intercondylar.
* Significant difference compared with each of the other regions (P < .01 for all).
A subgroup analysis was performed in the zones of each region. There was no significant difference in compressibility across the 4 zones of the medial trochlea (P = .37) and medial IC notch (P = .69). The lateral trochlea showed higher compressibility only for the FIZ versus MIZ (P = .02). The lateral IC notch showed higher compressibility for the FSZ versus the FIZ and MIZ (P < .05) (Table 2 and Figure 3).
Table 2.
Compression Values Among the 16 Donor Locations for Osteochondral Autograft Plugs a
| Zone | Medial IC Notch | Lateral IC Notch | Medial Trochlea b | Lateral Trochlea |
|---|---|---|---|---|
| FSZ | 1.95 ± 0.90 | 2.98 ± 1.43 c | 3.43 ± 1.36 | 2.22 ± 0.79 |
| MSZ | 2.03 ± 0.89 | 2.43 ± 1.41 | 2.63 ± 1.25 | 1.89 ± 0.51 |
| MIZ | 2.24 ± 0.80 | 2.18 ± 0.95 | 3.07 ± 1.56 | 1.78 ± 0.77 |
| FIZ | 2.19 ± 0.79 | 2.09 ± 0.93 | 3.29 ± 1.75 | 2.33 ± 0.90 |
a Data are reported as mean ± SD. FIZ, far inferior zone; FSZ, far superior zone; IC, intercondylar; MIZ, middle inferior zone; MSZ, middle superior zone.
b The medial trochlea had significantly more compression than the other regions (P < .01).
c The lateral IC notch showed significantly higher compressibility in the FSZ versus the far FIZ and MIZ (P < .05 for both).
Figure 3.
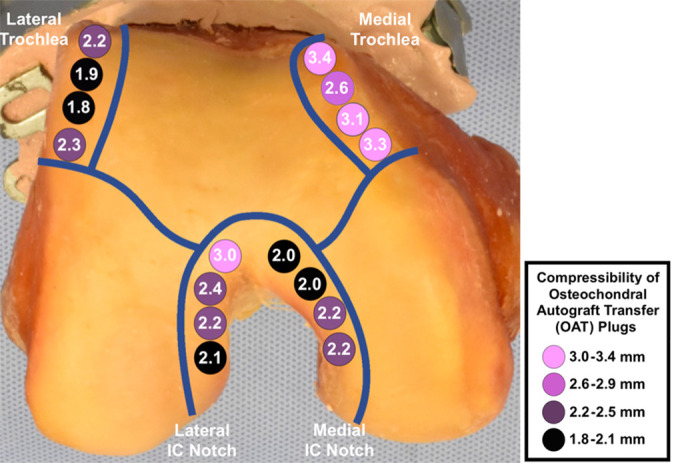
Distal view of a cadaveric right femur showing mean compressibility values of the 16 donor zones of the knee. Lighter purple shading indicates higher compressibility, and darker purple shading indicates less compressibility. The medial trochlea and the far superior zone of the lateral IC notch had the highest amounts of compressibility. IC, intercondylar; OAT, osteochondral autograft transfer
When comparing the compressibility of zones for each region, only the FSZ of the lateral IC notch was not significantly different than the medial trochlea (P = .66). There was a weak correlation between graft compression and age (r = .166, P = .003). Also, there were 5 plugs with cracks after 320 trials. The specific zones with cracks were 1 MSZ medial trochlea, 1 FSZ medial IC notch, 1 MIZ lateral IC notch, and 2 FSZ lateral IC notch. There was no difference in the distribution of cracks among the 16 zones (P =. 28).
Discussion
OAT is a useful technique for treating full-thickness cartilage lesions of the distal femur. 30 Various techniques recommend harvesting a plug 2 mm longer than the recipient hole to allow for graft impaction. 30 As the graft is seated, the compaction of cancellous bone for a graft of matching or slightly longer length helps hold the graft in place via a press-fit mechanism, improving biomechanical stability. 5,25,26 It has also been shown that different regions of bone can have different densitomes, or different bone density leading to differing amount of structural integrity. 20 Ideally, all grafts will sit flush with the surrounding articular surface; however, a delicate balance exists between proud grafts, flush grafts that are difficult to seat, and oversunk grafts. Our study shows that OAT donor grafts show the highest compressibility in the medial trochlea and lateral IC notch. While these donor regions can compress 3 mm, other regions compressed ≤2 mm.
Osteochondral plugs that sit proud have been found to increase contact pressures in the joint and cause damage to the articular surface of the plug. 11,9,17 In addition, osteochondral plugs sunk beneath the articular surface also increase contact pressure, though not to the extent of elevated plugs. 8,17 Studies even show that angled plugs can have increased peak contact pressure that returns to normal when impacted to flush with surrounding cartilage. 16,34 Plugs that are sunk too deep may fill with fibrocartilage, while plugs that are too proud may result in shearing off of the protruding cartilage. 13,23,27,32 Kock et al 15 showed that, whereas a cartilage defect almost doubled the surrounding contact pressure, a flush 3-plug mosaicplasty in human cadaver knees reduced border contact pressure by 30%. Careful impaction should be done and may avoid a recessed graft during the time of surgery.
While every attempt should be made to prevent excessively proud grafts, grafts that are difficult to seat may potentially cause problems. Patil et al 25 showed that in human cadaver knees, an osteochondral graft longer than the recipient hole requires a high force to seat the plug flush with the articular surface and the highest force to recess the graft 2 mm below the surrounding surface. Increased insertion forces reduce chondrocyte viability, which impacts graft survival and healing. 2,25 Reduction in viable chondrocytes was directly related to the mean force of the impact suggesting multiple lower force impacts rather than a few powerful blows. 14,36 If the graft becomes damaged during insertion, the graft may fracture and sink further into the recipient site, effectively rendering an osteochondral defect. 26 Fortunately, typical insertion forces do not significantly reduce chondrocyte viability. 25
It is advantageous for the surgeon to understand the compressibility of OAT plugs from different regions of the knee and to understand how the grafts will sit within the defect once they have been impacted. Whereas there is a paucity of studies evaluating the compressibility of different OAT donor regions, some studies have analyzed the biomechanical properties of different distal femur regions. Burgers et al 3 showed that the ultimate strain and yield were different between superior and inferior regions of the femur condyle. Another study by Nakabayashi et al 22 determined there were differences in the strength of bone in the condyles based on depth and region.
Although we did not determine the specific biomechanical properties of each region in this study, we focused more on the clinical application of how much compression occurs from each donor site. We found that OAT donor grafts showed the highest compressibility from the medial trochlea (3.1 mm) and lateral IC notch FSZ (3.0 mm). Thus, lateral trochlea, medial IC notch, and lateral IC notch MIZ/FIZ grafts should not be oversized more than 2 mm, as these grafts may not compress adequately. It should also be noted that, within each region, there was a large amount of variability in the amount of compression. This is likely a result of the large changes of compression within each specific zone of each region. For example, the FSZ of the lateral IC notch compressed 3.0 mm, while the FIZ in the same region compressed only 2.1 mm.
We also found a weak correlation between age and OAT compressibility. While other regions of bone have significant biomechanical relationships with age, some studies show that this relationship is weak in the femur condyles and trochlea. 6,28 Similar to previous studies, our results show that there is a weak correlation between age and compression in the trochlea and femur condyles.
Limitations
There are several limitations to our study. First, our study looked solely at the compressibility of 6 mm–diameter OAT plugs. While the diameter of the plug is chosen based on the size of the lesion, a 6 mm–diameter plug is on the smaller end of autograft plugs, which could affect overall compressibility when looking at larger size lesions requiring OAT plugs or mosaicplasty. This size was chosen because it is a common size utilized arthroscopically and this size allowed for testing of 4 zones within each region. Also, the graft compression was performed in a confined cylindrical rigid volume that kept the graft in coaxial position with the instrumented mallet. While this choice allowed repeatability of the experimental conditions, it must be noted that the rigidity of this construct does not represent the boundary conditions experienced by the graft in a real knee, in which surrounding trabecular bone exercises friction on the wall of the graft. The measured compression values may not replicate the compressions in real implantation but, given uniformity in testing conditions, we expect that the comparison between regions is not affected.
Second, the average age of the cadaver knees was 70.25 years, with the youngest cadaver knee at 55 years of age. This is significantly older than a typical surgical candidate would be for an OAT procedure. 5,30 While the cadavers used were older than typical OAT patients, there is evidence that the biomechanical properties of the femur condyle are not correlated with age. A previous study of cadavers age 31 to 88 years showed that the modulus of elasticity of trabecular bone from the femur condyle was not correlated with age or osteoarthritis. 28 The authors showed that subchondral bone modulus of elasticity had a moderate correlation with age and a strong correlation with osteoarthritis. 28 Another study showed that the femur condyles have poor correlation between crush strength and age. 6 Similarly, our study showed a weak correlation between age and graft compression.
Finally, we did not measure the cartilage thickness in the plugs, but there could be a possible relationship between the thickness of the cartilage and the compressibility of the donor plug. Multiple studies have cited that the donor osteochondral plugs which come from low load-bearing areas are thinner compared with the surrounding cartilage in the load-bearing recipient sites. 33
Conclusion
Compressibility varies between OAT donor sites in the distal femur. OAT donor grafts show the highest compressibility in the medial trochlea (3.1 mm) and lateral IC notch FSZ (3.0 mm). Lateral trochlea, medial IC notch, and the lower zones of the lateral IC notch grafts should not be oversized more than 2 mm in length, as these grafts may not compress adequately.
Acknowledgment
The authors acknowledge Baraa Shihadeh for preparation of the manuscript.
Footnotes
Final revision submitted September 21, 2022; accepted October 11, 2022.
One or more of the authors has declared the following potential conflict of interest or source of funding: P.A.M. has received education payments from Midsouth Orthopedics and honoraria from Vericel. C.M. has received education payments from Arthrex and hospitality payments from Smith & Nephew and Stryker. R.S.B. has received education payments from Midsouth Orthopedics, consulting fees from Zimmer Biomet, and hospitality payments from Arthrex and Stryker. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from the Louisiana State University Health Sciences Center-Shreveport (ref No. STUDY00001241).
References
- 1. Biant LC, McNicholas MJ, Sprowson AP, Spalding T. The surgical management of symptomatic articular cartilage defects of the knee: consensus statements from United Kingdom knee surgeons. Knee. 2015;22(5):446–449. doi:10.1016/j.knee.2015.06.001 [DOI] [PubMed] [Google Scholar]
- 2. Borazjani BH, Chen AC, Bae WC, Sah RL, Firestein GS, Bugbee WD. Effect of impact on chondrocyte viability during insertion of human osteochondral grafts. J Bone Joint Surg Am. 2006;88(9):1934–1943. [DOI] [PubMed] [Google Scholar]
- 3. Burgers TA, Mason J, Niebur G, Ploeg HL. Compressive properties of trabecular bone in the distal femur. J Biomech. 2008;41(5):1077–1085. doi:10.1016/J.JBIOMECH.2007.11.018 [DOI] [PubMed] [Google Scholar]
- 4. Cole BJ, Pascual-Garrido C, Grumet RC. Surgical management of articular cartilage defects in the knee. J Bone Joint Surg Am. 2009;91(7):1778–1790. [PubMed] [Google Scholar]
- 5. Coons DA, Barber FA. Arthroscopic osteochondral autografting. Orthop Clin North Am. 2005;36(4):447–458. doi:10.1016/j.ocl.2005.05.007 [DOI] [PubMed] [Google Scholar]
- 6. Crookshank M, Coquim J, Olsen M, Schemitsch EH, Bougherara H, Zdero R. Biomechanical measurements of axial crush injury to the distal condyles of human and synthetic femurs. Proc Inst Mech Eng H. 2012;226(4):320–329. doi:10.1177/0954411912438038 [DOI] [PubMed] [Google Scholar]
- 7. DiBartola AC, Everhart JS, Magnussen RA, et al. Correlation between histological outcome and surgical cartilage repair technique in the knee: a meta-analysis. Knee. 2016;23(3):344–349. doi:10.1016/j.knee.2016.01.017 [DOI] [PubMed] [Google Scholar]
- 8. D’Lima DD, Chen PCY, Colwell CW, Jr. Osteochondral grafting: effect of graft alignment, material properties, and articular geometry. Open Orthop J. 2009;3(1):61–68. doi:10.2174/1874325000903010061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Du PZ, Markolf KL, Boguszewski DV, et al. Effects of proud large osteochondral plugs on contact forces and knee kinematics: a robotic study. Am J Sports Med. 2018;46(9):2122–2127. doi:10.1177/0363546518770415 [DOI] [PubMed] [Google Scholar]
- 10. Guzman AJ, Dela Rueda T, Rayos Del Sol SM, et al. Arthroscopic osteochondral autograft transfer system procedure of the lateral femoral condyle with donor-site backfill using osteochondral allograft plug. Arthrosc Tech. 2021;10(12):e2683–e2689. doi:10.1016/j.eats.2021.08.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Harris JD, Solak KK, Siston RA, Litsky A, Richards J, Flanigan DC. Contact pressure comparison of proud osteochondral autograft plugs versus proud synthetic plugs. Orthopedics. 2011;34(2):97. doi:10.3928/01477447-20101221-06 [DOI] [PubMed] [Google Scholar]
- 12. Heir S, Nerhus TK, Røtterud JH, et al. Focal cartilage defects in the knee impair quality of life as much as severe osteoarthritis: a comparison of knee injury and osteoarthritis outcome score in 4 patient categories scheduled for knee surgery. Am J Sports Med. 2010;38(2):231–237. doi:10.1177/0363546509352157 [DOI] [PubMed] [Google Scholar]
- 13. Huang FS, Simonian PT, Norman AG, Clark JM. Effects of small incongruities in a sheep model of osteochondral autografting. Am J Sports Med. 2004;32(8):1842–1848. doi:10.1177/0363546504264895 [DOI] [PubMed] [Google Scholar]
- 14. Kang RW, Friel NA, Williams JM, Cole BJ, Wimmer MA. Effect of impaction sequence on osteochondral graft damage: the role of repeated and varying loads. Am J Sports Med. 2010;38(1):105–113. doi:10.1177/0363546509349038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Kock NB, Smolders JMH, Van Susante JLC, Buma P, Van Kampen A, Verdonschot N. A cadaveric analysis of contact stress restoration after osteochondral transplantation of a cylindrical cartilage defect. Knee Surg Sports Traumatol Arthrosc. 2008;16(5):461–468. doi:10.1007/s00167-008-0494-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Koh JL, Kowalski A, Lautenschlager E. The effect of angled osteochondral grafting on contact pressure a biomechanical study. Am J Sports Med. 2006;34(1):116–119. doi:10.1177/0363546505281236 [DOI] [PubMed] [Google Scholar]
- 17. Koh JL, Wirsing K, Lautenschlager E, Zhang LO. The effect of graft height mismatch on contact pressure following osteochondral grafting: a biomechanical study. Am J Sports Med. 2004;32(2):317–320. doi:10.1177/0363546503261730 [DOI] [PubMed] [Google Scholar]
- 18. Krych AJ, Harnly HW, Rodeo SA, Williams RJ. Activity levels are higher after osteochondral autograft transfer mosaicplasty than after microfracture for articular cartilage defects of the knee: a retrospective comparative study. J Bone Joint Surg Am. 2012;94(11):971–978. doi:10.2106/JBJS.K.00815 [DOI] [PubMed] [Google Scholar]
- 19. LaPrade RF, Botker JC. Donor-site morbidity after osteochondral autograft transfer procedures. Arthroscopy. 2004;20(7):e69–e73. doi:10.1016/j.arthro.2004.06.022 [DOI] [PubMed] [Google Scholar]
- 20. Massey PA, Caldwell C, Vauclin CP, et al. The ideal cortical button location on the lateral femur for anterior cruciate ligament suspensory fixation is 30 mm proximal to the lateral epicondyle. Arthrosc Sports Med Rehabil. 2021;3(5):e1255–e1262. doi:10.1016/j.asmr.2021.03.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Massey PA, Lowery MT, Houk G, McClary KN, Barton RS, Solitro GF. Ideal donor site for osteochondral autografting of the distal femur using radius of curvature: a 3-dimensional high-resolution scanner comparison. Cartilage. 2021;13(1_suppl):928S–936 S. doi:10.1177/19476035211007914 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Nakabayashi Y, Wevers HW, Cooke TDV, Griffin M. Bone strength and histomorphometry of the distal femur. J Arthroplasty. 1994;9(3):307–315. doi:10.1016/0883-5403(94)90086-8 [DOI] [PubMed] [Google Scholar]
- 23. Nakagawa Y, Suzuki T, Kuroki H, Kobayashi M, Okamoto Y, Nakamura T. The effect of surface incongruity of grafted plugs in osteochondral grafting: a report of five cases. Knee Surg Sport Traumatol Arthrosc. 2007;15(5):591–596. doi:10.1007/s00167-006-0253-0 [DOI] [PubMed] [Google Scholar]
- 24. Pareek A, Reardon PJ, Maak TG, Levy BA, Stuart MJ, Krych AJ. Long-term outcomes after osteochondral autograft transfer: a systematic review at mean follow-up of 10.2 years. Arthroscopy. 2016;32(6):1174–1184. doi:10.1016/j.arthro.2015.11.037 [DOI] [PubMed] [Google Scholar]
- 25. Patil S, Butcher W, D’Lima DD, Steklov N, Bugbee WD, Hoenecke HR. Effect of osteochondral graft insertion forces on chondrocyte viability. Am J Sports Med. 2008;36(9):1726–1732. doi:10.1177/0363546508316765 [DOI] [PubMed] [Google Scholar]
- 26. Patil S, Tapasvi SR. Osteochondral autografts. Curr Rev Musculoskelet Med. 2015;8(4):423–428. doi:10.1007/s12178-015-9299-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Pearce SG, Hurtig MB, Clarnette R, Kalra M, Cowan B, Miniaci A. An investigation of 2 techniques for optimizing joint surface congruency using multiple cylindrical osteochondral autografts. Arthroscopy. 2001;17(1):50–55. doi:10.1053/jars.2001.19966 [DOI] [PubMed] [Google Scholar]
- 28. Peters AE, Akhtar R, Comerford EJ, Bates KT. The effect of ageing and osteoarthritis on the mechanical properties of cartilage and bone in the human knee joint. Sci Reports 2018;8(1):5931. doi:10.1038/s41598-018-24258-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Rowland R, Colello M, Wyland DJ. Osteochondral autograft transfer procedure: arthroscopic technique and technical pearls. Arthrosc Tech. 2019;8(7):e713–e719. doi:10.1016/j.eats.2019.03.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Sherman SL, Thyssen E, Nuelle CW. Osteochondral autologous transplantation. Clin Sports Med. 2017;36(3):489–500. doi:10.1016/j.csm.2017.02.006 [DOI] [PubMed] [Google Scholar]
- 31. Solheim E, Hegna J, Strand T, Harlem T, Inderhaug E. Randomized study of long-term (15-17 years) outcome after microfracture versus mosaicplasty in knee articular cartilage defects. Am J Sports Med. 2018;46(4):826–831. doi:10.1177/0363546517745281 [DOI] [PubMed] [Google Scholar]
- 32. Sun J, Hou XK, Yong K, Shi M. Incongruity affecting osteochondral repair by mosaicplasty technique in an animal model. Arch Orthop Trauma Surg. 2013;133(6):781–788. doi:10.1007/s00402-013-1711-z [DOI] [PubMed] [Google Scholar]
- 33. Thaunat M, Couchon S, Lunn J, Charrois O, Fallet L, Beaufils P. Cartilage thickness matching of selected donor and recipient sites for osteochondral autografting of the medial femoral condyle. Knee Surg Sport Traumatol Arthrosc. 2007;15(4):381–386. doi:10.1007/s00167-006-0222-7 [DOI] [PubMed] [Google Scholar]
- 34. Walter C, Trappe D, Beck A, Jacob C, Hofmann UK. Effect of graft positioning on dissipated energy in knee osteochondral autologous transplantation - a biomechanical study. J Orthop Res. 2020;38(8):1727–1734. doi:10.1002/jor.24612 [DOI] [PubMed] [Google Scholar]
- 35. Welton KL, Logterman S, Bartley JH, Vidal AF, McCarty EC. Knee cartilage repair and restoration: common problems and solutions. Clin Sports Med. 2018;37(2):307–330. doi:10.1016/j.csm.2017.12.008 [DOI] [PubMed] [Google Scholar]
- 36. Whiteside RA, Jakob RP, Wyss UP, Mainil-Varlet P. Impact loading of articular cartilage during transplantation of osteochondral autograft. J Bone Joint Surg Br. 2005;87(9):1285–1291. doi:10.1302/0301-620X.87B9.15710 [DOI] [PubMed] [Google Scholar]


