Abstract
Background:
Surgical techniques and associated outcomes in treating acute and chronic extra-articular ligament knee injuries are in evolution, and there is question as to whether repair or reconstruction is optimal.
Purpose/Hypothesis:
The purpose of this study was to compare the subsequent surgery rate between surgical repair versus reconstruction for all extra-articular ligament injuries of the knee utilizing a large database. Our hypothesis was that overall surgical repair of both lateral and medial extra-articular knee injuries would have a higher revision rate than those treated by reconstruction.
Study Design:
Cohort study; Level of evidence, 3.
Methods:
The PearlDiver Mariner data set (2010-2019), with 122 million patients, was utilized to generate 2 patient cohorts: those who underwent surgical repair and those who underwent surgical reconstruction of a knee extra-articular ligament injury. All patients had a minimum of 2 years follow-up. Rates of concomitant or subsequent cruciate ligament reconstruction and rates of secondary procedures were assessed and compared between the 2 cohorts.
Results:
In total, 3563 patients were identified: extra-articular ligament reconstruction was performed for 2405 (67.5%), and repair was performed for 1158 (32.5%). Cruciate ligament reconstruction was performed for 986 (27.7%), of which 888 of 986 (90.1%) were performed on the same day as their extra-articular ligament procedure. At 2-year follow-up, the reconstruction cohort had higher rates of revision surgery compared with the repair cohort (8.2% vs 2.5%; P < .001).
Conclusion:
Using a large national database, knee extra-articular ligamentous reconstructions (those on both the lateral and the medial side) had a 3.3 times higher rate of revision surgery compared with repair at 2-year follow-up. Further study is needed to investigate the causes leading to revision surgery and to determine the optimal surgical treatment for both medial and lateral extra-articular knee ligament injuries.
Keywords: extra-articular ligament, knee, ligament reconstruction, ligament repair
The ligaments of the knee joint can be classified as either intra-articular or extra-articular. The intra-articular ligaments in the knee are located centrally and include the anterior cruciate ligament (ACL) and the posterior cruciate ligament (PCL). 5 The extra-articular ligaments are located on the periphery of the knee joint, both medially and laterally, and include ligaments such as the lateral collateral ligament (LCL), medial collateral ligament (MCL), and medial patellofemoral ligament (MPFL). 5,18 Indications of operative intervention for acute isolated injuries of the extra-articular ligaments are very focused and uncommonly needed. 18 Treatment of chronic, isolated injuries of the extra-articular ligaments are less common and usually occur in a combined ligament injury pattern, for example PCL–posterolateral corner (PLC). 26 The 2 main methods for surgical treatment of extra-articular ligamentous injuries are either repair or reconstruction. 26 However, the optimal surgical treatment is not well-defined.
The treatment for MCL injuries can vary from nonoperative modalities to various surgical interventions. However, the majority of isolated medial collateral ligament injuries are first- or second-degree injuries (partial tears) and heal with nonoperative management and restrictive motion bracing. 9,14,16,27 Surgical indications of medial collateral ligament injuries are typically reserved for failed nonoperative treatment of third-degree lesions (3° = complete tears) often in conjunction with a cruciate injury, displaced femoral or tibial-sided avulsions or combined injury, which include the posterior oblique ligament–posteromedial complex. 15,26,33 When surgical treatment is indicated, there are reports of excellent outcomes with either MCL repair with graft augmentation or MCL reconstruction. 7,8 However, there is a paucity of literature comparing the outcomes of MCL reconstructions and repairs.
Isolated lateral ligamentous knee injuries are rare 4 and usually occur with concomitant injuries to the PLC, PCL, ACL, or lateral meniscus. 20 Due to potential severe and long-term morbidity associated with lateral-sided ligament and PLC injuries, surgical intervention is more common. 13,17,22,28 While McCarthy et al 25 found no statistical difference between failure rates of the repair versus reconstruction groups, other studies in the literature have reported statistically significant higher failure rates with LCL repair when compared with reconstruction. 21,30 Part of the discrepancy arises from underpowered studies due to an injury with a low incidence, making it difficult to conduct large, prospective studies. 1
The major extra-articular ligaments in the knee include the LCL, MCL, and MPFL. 5 Surgical indications and techniques for extra-articular ligament knee injuries are not well-defined in the literature but are evolving. 7,8,10,11 For extra-articular ligamentous injuries that are addressed surgically, there is debate over which method, repair or reconstruction, optimizes functional outcomes. In terms of the LCL, several recent studies with cohorts of 30 to 60 patients have reported higher failure rates of LCL repair when compared with reconstruction. 21,30 Furthermore, studies have shown promising outcomes for both repair and reconstruction of surgically treated 3° MCL injuries; however, it is still unknown which technique provides better outcomes, as no study has been able to compare the 2 techniques directly.
The purpose of the current study was to use a large national patient database to compare the subsequent revision surgery rates between surgical repairs and reconstructions of all extra-articular ligamentous knee injuries to help determine the optimal surgical strategy. The literature has suggested that repair for both lateral and medial extra-articular ligaments may confer a higher failure rate than those treated through reconstructive efforts. Therefore, we hypothesized that the revision rate of extra-articular knee injuries treated with surgical reconstruction would be lower than those treated with surgical repair for both lateral and medial extra-articular knee injuries.
Methods
Patient Cohorts
The PearlDiver Mariner database (2010-2019), which is based on insurance claims and has data available on approximately 122 million patients, was utilized to generate 2 cohorts: patients who underwent repair of an extra-articular knee ligament, and patients who underwent reconstruction of an extra-articular knee ligament. All patients with <2 years of active follow-up were excluded. An exemption from our institutional review board was obtained, as the database contains only deidentified data.
The repair cohort consisted of all patients who underwent primary surgical repair of a knee extra-articular ligament injury (identified by Current Procedural Terminology [CPT] codes 27405, 27409, or 27557), either in isolation or in combination with cruciate ligament repair or reconstruction (Table 1). The reconstruction cohort consisted of all patients who underwent surgical reconstruction of a knee extra-articular ligament injury (identified by CPT codes 27427, 27429, or 27558), also either in isolation, or in combination with cruciate ligament repair/reconstruction (Table 1). Patients who underwent both extra-articular knee ligament repair and reconstruction on the same day were assigned to the reconstruction cohort.
Table 1.
Current Procedural Terminology (CPT) Codes Used for Extra-articular Repair, Reconstruction, and Secondary Surgery
| Code | Description |
|---|---|
| Extra-articular Ligamentous Repair Procedure Codes | |
| CPT-27405 | Repair primary torn ligament and/or capsule knee; collateral |
| CPT-27409 | Repair primary torn ligament and/or capsule knee; collateral and cruciate ligaments |
| CPT-27557 | Open treatment of knee dislocation with or without internal or external fixation; with primary ligamentous repair |
| Extra-articular Ligamentous Reconstruction Procedure Codes | |
| CPT-27427 | Ligamentous reconstruction (augmentation) knee; extra-articular |
| CPT-27429 | Ligamentous reconstruction (augmentation) knee; intra-articular (open) and extra-articular |
| CPT-27558 | Open treatment of knee dislocation with or without internal or external fixation; with primary ligamentous repair with augmentation/reconstruction |
| Description of Secondary Surgery Procedure Codes Queried | |
| CPT-27418 | Anterior tibial tubercleplasty |
| CPT-27427 | Extra-articular knee ligamentous reconstruction |
| CPT-27429 | Open intra-articular and extra-articular knee ligamentous reconstruction |
| CPT-27440 | Arthroplasty knee tibial plateau |
| CPT-27441 | Arthroplasty knee tibial plateau; with debridement and partial synovectomy |
| CPT-27442 | Knee arthroplasty: femoral condyles or tibial plateau(s) |
| CPT-27443 | Knee arthroplasty: femoral condyles or tibial plateau(s); with debridement and partial synovectomy |
| CPT-27445 | Knee arthroplasty: hinge prosthesis |
| CPT-27446 | Knee arthroplasty: condyle and plateau; medial OR lateral compartment |
| CPT-27447 | Knee arthroplasty: condyle and plateau; medial AND lateral compartments with or without patella resurfacing |
| CPT-27450 | Femur shaft or supracondylar osteotomy with fixation |
| CPT-27457 | Proximal tibia osteotomy including fibular excision or osteotomy after epiphyseal closure |
| CPT-27557 | Open treatment of knee dislocation with or without internal or external fixation; with primary ligamentous repair |
| CPT-27558 | Open treatment of knee dislocation with or without internal or external fixation; with primary ligamentous reconstruction |
Next, the extra-articular ligament repair and reconstruction cohorts were queried for secondary surgical procedures of the knee within 2 years after primary surgery. Rates of secondary procedures after their index procedure were assessed, including any extra-articular ligament reconstruction, knee arthroplasty, tibial or femoral osteotomy, and/or anterior tibial tubercleplasty and this was compared between the repair and reconstruction cohorts. Secondary nonligamentous procedures, or revision secondary surgeries, were included as these procedures could be indicated secondarily if residual subjective ligamentous instability was still present or if mechanical alignment or unloading procedures were indicated. Of the original patient population, a secondary analysis was conducted comparing secondary surgery among extra-articular repair and reconstruction patients who were matched for age, sex, and Elixhauser Comorbidity Index (ECI). Rates of concomitant or subsequent cruciate ligament reconstruction were also compared between the repair and reconstruction cohorts. For the purposes of this study, “failure” was defined as a secondary procedure.
Data Analysis
Frequency, age distribution, rates of secondary surgery, and type of secondary procedures were compared using Fisher exact tests for categorical data and a t test for continuous data. Finally, a Kaplan-Meier survival curve was created to evaluate survival of the index procedures. Comparison of the 2 groups was performed with log-rank (Mantel-Cox) test. Stata Version 14 (Stata) was used for analysis. Significance was defined with a 2-sided alpha level of ≤.05.
Results
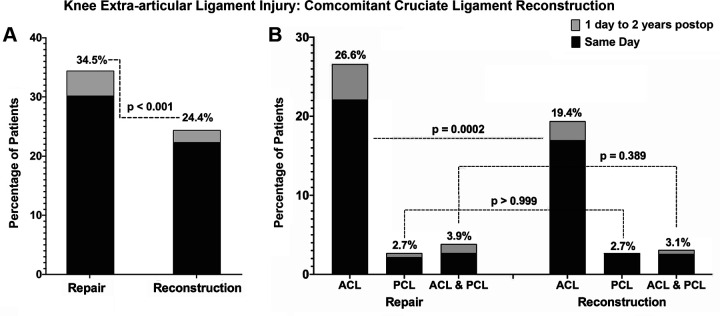
A total of 3563 patients with surgically treated extra-articular ligament injuries were identified who met inclusion criteria. Of those, 2405 (67.5%) were treated with reconstruction and 1158 (32.5%) were treated with repair (Figure 1). Cruciate ligament reconstruction was performed for 986 (27.7%), of which 888 of 986 (90.1%) were performed on the same day as their extra-articular ligament procedure. Overall, at 2-year follow-up, the reconstruction cohort had higher rates of revision surgery compared with the repair cohort (8.2% vs 2.5%; P < .001). The mean (±SD) age of the reconstruction cohort was 29.3 ± 13.2 years, with 61.6% being female. The mean (±SD) age of the repair cohort was 36.6 ± 15.2 years, with 41.3% being female.
Figure 1.
Study population: patients undergoing reconstruction versus repair for extra-articular ligamentous knee injuries.
In the population matched for age, sex, and ECI, there were a total of 1958 patients. Of those, 1000 (51.1%) were treated with reconstruction and 958 (48.9%) were treated with repair. The mean (±SD ) age of the reconstruction cohort was 34.0 ± 14.3 years, 46.6% female. The mean (±SD) age of the repair cohort was 34.0 ± 14.5 years, 46.1% female.
Among the matched reconstruction cohort, there were 93 patients who also underwent open extra-articular knee ligament repair (CPT-27405) on the same day as their extra-articular knee ligament reconstruction, and 10 or fewer patients who underwent open extra-articular and intra-articular knee ligament repair (CPT-27409) on the same day as their extra-articular knee ligament reconstruction. To protect patient privacy in the PearlDiver Mariner data set, exact patient numbers cannot be provided for groups of 10 or fewer patients.
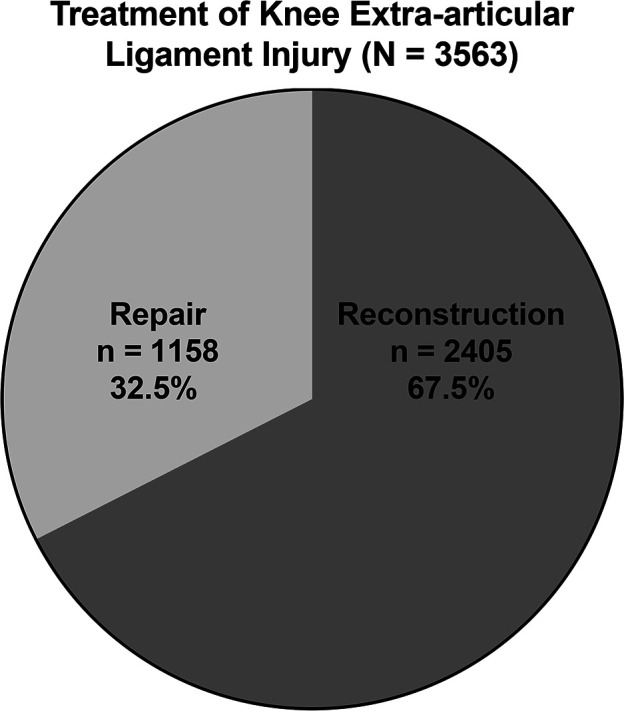
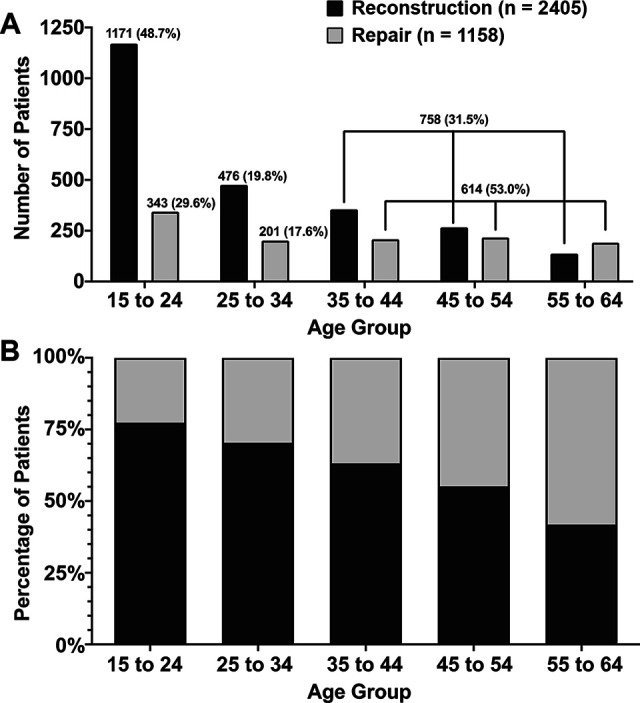
The percentage of patients undergoing extra-articular knee ligament reconstruction or repair was examined by age group. Patients aged 15 to 24 years comprised a significantly higher percentage of the extra-articular knee ligament reconstruction cohort when compared with the percent of the repair cohort aged 15 to 24 years (48.7% vs 29.6%; P < .001). Conversely, patients aged 35 to 64 years accounted for a significantly higher percentage of the repair cohort when compared with the percentage of the reconstruction cohort aged 35 to 64 years (53.0% vs 31.5%, P < .001; Figure 2). Patients who underwent extra-articular repair had a higher frequency of concomitant or subsequent cruciate ligament reconstruction between the 2 cohorts, with 34.5% of patients in the repair cohort undergoing cruciate ligament reconstruction, compared with 24.4% in the reconstruction cohort (P < .001) (Table 2 and Figure 3A). There was a statistically higher rate of arthroscopic ACL reconstruction among the extra-articular ligament repair cohort when compared with the reconstruction cohort (28.2% vs 18.1%, P < .001; Table 2) within the subsequent 2 years. There were no differences in the rates of arthroscopic PCL reconstruction between the 2 groups (6.2% vs 4.9%, P = .111), or open intra-articular ligament reconstruction (5.8% vs 5.6%, P = .817) (Table 2).
Figure 2.
Comparison by age group of patients undergoing reconstruction versus repair of extra-articular ligamentous knee injury: (A) number of patients and (B) percentage of patients.
Table 2.
Comparison of Extra-Articular Repair vs. Reconstruction Stratified by Cruciate Reconstruction a
| Description | Repair (n = 1158) |
Reconstruction (n = 2405) |
P |
|---|---|---|---|
| Cruciate ligament reconstruction | 399 (34.5) | 587 (24.4) | <.001 |
| Arthroscopic ACL reconstruction (CPT-29888) | 327 (28.2) | 436 (18.1) | <.001 |
| Arthroscopic PCL reconstruction (CPT-29889) | 72 (6.2) | 118 (4.9) | .111 |
| Open intra-articular ligament reconstruction (CPT-27428) | 67 (5.8) | 135 (5.6) | .817 |
a Data are reported as No. of patients (%). Boldface P values indicate statistically significant difference between groups (P < .05). ACL, anterior cruciate ligament; CPT, Current Procedural Terminology; PCL, posterior cruciate ligament.
Figure 3.
(A) Comparison of concomitant cruciate ligament reconstruction in patients who underwent repair or reconstruction for extra-articular knee ligament injury. There was a statistically higher rate of concomitant cruciate ligament reconstruction in the extra-articular knee ligament repair cohort, driven by a higher rate of arthroscopic ACL reconstruction in the repair cohort. (B) Comparison of concomitant cruciate ligament reconstruction among a matched population of patients who underwent repair or reconstruction of a knee extra-articular ligament injury. There was a statistically higher rate of concomitant ACL reconstruction in the extra-articular knee ligament repair cohort (P = .0002). ACL, anterior cruciate ligament; PCL, posterior cruciate ligament; Postop, postoperative.
Among the matched population, there was also a statistically higher rate of arthroscopic ACL reconstruction among the extra-articular ligament repair cohort when compared with the reconstruction cohort (26.6% vs 19.4%; P = .0002) (Figure 3B). There were no differences in the rates of arthroscopic PCL reconstruction between the 2 groups (2.7% vs 2.7%; P > .999) ( Figure 3B), or combined arthroscopic ACL and PCL reconstruction (3.9% vs 3.1%; P = .389) (Figure 3B). There was also no statistical difference in open intra-articular ligament reconstruction (6.0% vs 7.0%; P = .356).
Rates of revision secondary surgeries were stratified by index reconstruction or repair and are depicted in Figure 4. In the reconstruction cohort, 196 (8.2%) of 2405 patients underwent a revision secondary surgical procedure within 2 years of their index procedure. In the repair cohort, 29 (2.5%) of 1158 patients underwent a revision secondary surgical procedure within 2 years of their index procedure (P < .001).
Figure 4.
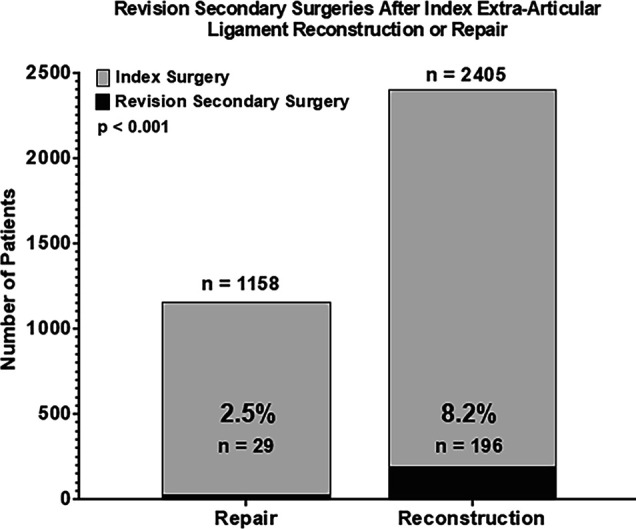
Revision secondary surgery rates at 2 years, reconstruction versus repair of extra-articular knee ligament injury. Secondary surgeries include revision reconstruction, total knee arthroplasty, anterior tibial tubercleplasty, distal femoral osteotomy, or high tibial osteotomy. The repair cohort had a lower rate of secondary surgery compared with the reconstruction cohort (P < .001).
Rates of secondary surgeries stratified by index reconstruction or repair and matched by age, gender, and ECI are depicted in Figure 5. In the matched reconstruction cohort of 1000 patients (age [mean ± SD], 34.0 ± 14.3 years; 46.6% female), 78 (7.8%) underwent a revision secondary surgical procedure within 2 years of their index procedure. This rate is significantly higher than the matched repair cohort of 958 patients (age [mean ± SD], 34.0 ± 14.5 years; 46.1% female), where 24 (2.5%) underwent a revision surgical procedure within 2 years of their index procedure (P < .001).
Figure 5.
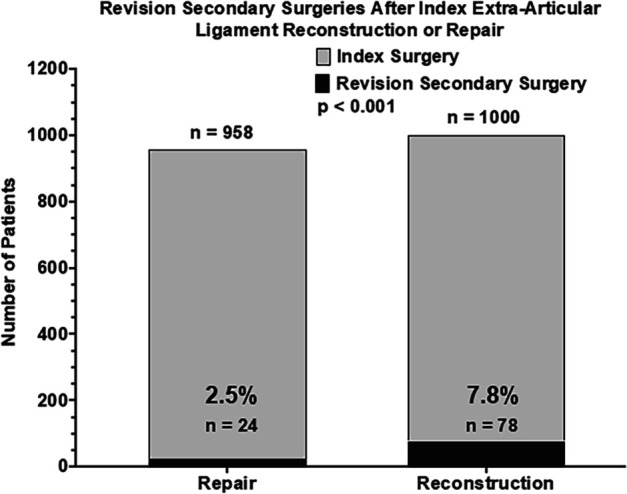
Revision secondary surgery rates at 2 years, reconstruction versus repair of extra-articular knee ligament injury, after patient populations have been matched by age, sex, and ECI. Secondary surgery is defined as revision extra-articular ligament reconstruction, total knee arthroplasty, anterior tibial tubercleplasty, distal femoral osteotomy, or high tibial osteotomy. When matched by age, sex, and ECI, the repair cohort had a lower rate of secondary surgery compared with the reconstruction cohort (P < .001). ECI, Elixhauser Comorbidity Index.
In addition, the incidence of manipulation of knee joint under general anesthesia (CPT-27570) and arthroscopic lysis of adhesions (CPT-29884) was evaluated for the 2 years after index surgery in the matched reconstruction and repair cohorts. Patients who underwent extra-articular knee ligament repair had higher odds of undergoing manipulation of the knee joint under general anesthesia (5.2% vs 2.4%; odds ratio, 2.2; P = .001) when compared with the reconstruction cohort. There was no statistical difference in the incidence of arthroscopic lysis of adhesions between the repair and reconstruction cohort (2.5% vs 2.1%; P = .651).
The matched population was also analyzed with respect to sex, as stated in the PearlDiver Mariner data set. When stratifying by gender, the secondary surgery rate was significantly higher in the reconstruction cohort than the repair cohort for both male (6.4% vs 2.3%; P = .0014) and female (9.4% vs 2.7%; P < .0001) patients. When comparing the secondary surgery rates of male versus female patients, there was no difference among either the reconstruction cohort (6.4% vs 9.4%; P = .077) or the repair cohort (2.3% vs 2.7%; P = .836)
Survivorship curves after index extra-articular ligament procedure are shown in Figure 6. At 2 years after the index procedure, the repair cohort had a higher survivorship compared with the reconstruction cohort (97.5% vs 91.9%; P < .001). Survivorship of extra-articular ligament repair was also statistically higher when calculated in a population matched by age, sex, and ECI (97.5% vs 92.2%; P < .001) (Figure 7).
Figure 6.
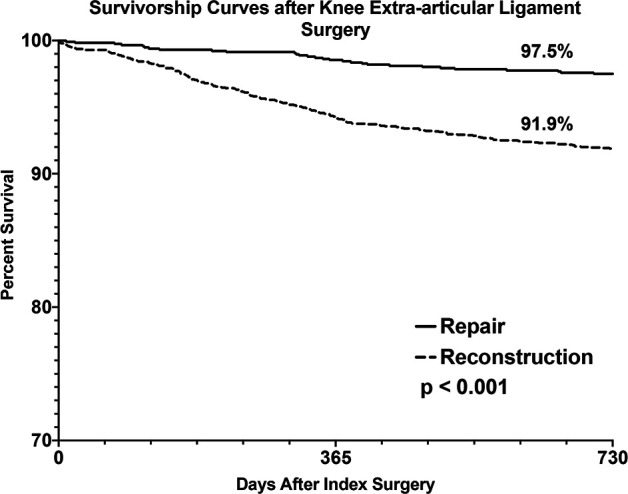
Kaplan-Meier survival curve of secondary surgery in the 2 years after extra-articular knee ligament reconstruction versus repair. Secondary surgery is defined as revision extra-articular ligament reconstruction, total knee arthroplasty, anterior tibial tubercleplasty, distal femoral osteotomy, or high tibial osteotomy. The repair cohort had a higher survivorship compared with the reconstruction cohort (97.5% vs 91.9%; P < .001).
Figure 7.
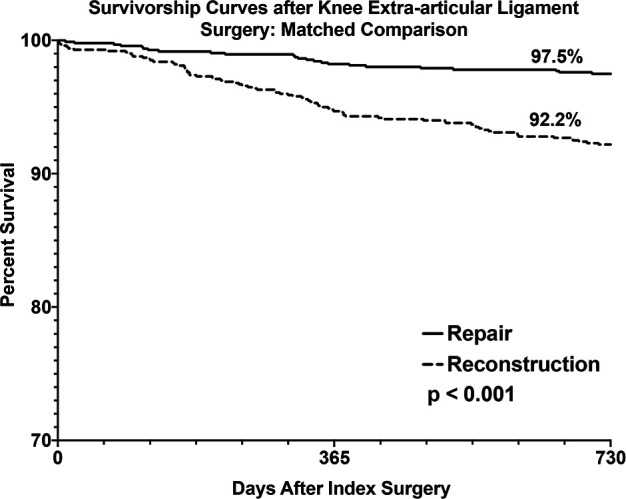
Kaplan-Meier survival curve of secondary surgery in the 2 years after extra-articular knee ligament reconstruction versus repair, among patients matched by age, sex, and Elixhauser Comorbidity Index. Secondary surgery is defined as revision extra-articular ligament reconstruction, total knee arthroplasty, anterior tibial tubercleplasty, distal femoral osteotomy, or high tibial osteotomy. The repair cohort had a higher survivorship compared with the reconstruction cohort (97.5% vs 92.2%; P < .001).
Discussion
In the current study, we assessed the rate of secondary surgery after both knee extra-articular ligamentous reconstruction and knee extra-articular ligamentous repair. Using a 122 million patient database, 3563 patients were identified for analysis, which showed that reconstruction of extra-articular ligament knee injuries was more commonly performed than repair. Our initial hypothesis was rejected given that the rate of revision surgery for knee extra-articular ligamentous reconstruction was 3.3 times higher than the rate of revision surgery after primary ligamentous repair within 2 years after index procedure. These findings have important implications for future studies as well as for treatment of extra-articular ligamentous injuries around the knee.
The MCL is the primary stabilizer of the medial aspect of the knee and works to resist valgus loads. 19 Studies across the literature have shown excellent outcomes with both repair and reconstructive treatment of isolated MCL injuries as well as those that occur concomitantly with ACL tears. However, given that isolated injuries that receive surgical treatment are rare, no study has compared outcomes with respect to repair or reconstruction of the ligament. While this study includes all of the extra-articular ligaments in the knee, our findings support and emphasize the need for future studies to examine the differences in repair versus reconstruction surgical treatment of the MCL, as there may be a difference in the revision rate.
While surgical intervention for acute extra-articular lateral-sided injuries of the knee has been shown to have better outcomes than nonoperative treatment, 12,13,17,22 –24,28,32 controversy still exists as to whether reconstruction or repair should be performed. 21 –23,30,31 While isolated LCL injuries that require surgery are rare, the majority of operative LCL cases are seen in combined injury patterns that involve the PLC. 29 Nevertheless, early reports of acute repair of the PLC demonstrate good-to-fair results in 88% to 100% of patients. 2,3,6 However, it is important to note the heterogeneity of multiligamentous knee injuries in comparing the literature. Limitations of multiligamentous knee injury studies arise from the various combinations of extra- and intra-articular ligaments involved, the mechanism of injury (high or low velocity), and acuity/chronicity (ie, recurrent patellar dislocation vs acute trauma). These multiligamentous injuries may include various combinations of ACL and/or PCL injuries in addition to the numerous permutations of extra-articular ligament injuries that are often difficult to categorize in research studies, with most past studies utilizing an aggregated category to encapsulate these various combinations. Further, existing databases, including the one used in the present study, are limited in the granularity of how the injury occurred and other relevant clinical factors such as chronic pathologies of surrounding structures such as the extensor mechanism. Thus, in evaluating the present study, it is important to keep in mind the generalizations that were necessary to assess such a large cohort.
Recent studies have compared outcomes of PLC repair and reconstruction and reported failure rates as high as 40% for primary repairs of the PLC. 21,23,30 In a 2005 study of 64 patients (39 repairs, 25 reconstructions), higher rates of failure after primary repair of the PLC were seen. 30 However, patients were not randomized, allowing for the introduction of selection bias. Specifically, there was variability between the 2 cohorts of patients who sustained PLC injuries. 30 In 2010, Levy et al 21 examined 28 patients who underwent surgical intervention for a PLC injury and found higher failure rates in the repair cohort (4 failures in 10 total repairs) when compared with their reconstruction cohort (1 failure in 18 total reconstructions). Both studies commented that, in those patients where repairs failed, the revision second surgery was equivalent to a successful first-time repair in their cohorts.
The current study compares the repair and reconstruction of all extra-articular knee ligament injuries in the largest cohort to date. At 2-year follow-up, the reconstruction cohort had an 8.2% rate of revision surgery, compared with 2.5% in the repair cohort. When the cohorts were matched by age, sex, and ECI, the difference between the reconstruction and repair cohorts was even more pronounced. These findings are different from those of previous studies that demonstrated superior results with extra-articular reconstructions, such as those studies comparing PLC reconstruction and repair. 21,23,30
Limitations
The limitations of this study are inherent to a database study. The database relies on the accuracy of reimbursement claims data. In addition, patients that changed insurance to a provider outside of the Mariner data set may be lost within the 2-year follow-up time period of this study. Furthermore, the inclusion of patients in this study was reliant on the accuracy of CPT coding. However, this study is unable to specify what extra-articular ligament was repaired or reconstructed, reason for patient selection, severity of the ligamentous injury, or the type of graft used in the case of reconstruction, as they are indistinguishable based on CPT codes. While heterogeneity in complexity and techniques exists even within the procedures performed on these ligaments, the large sample size allows for analysis of extra-articular ligamentous injuries that have not been reported previously.
Database studies also do not have specific types of information, such as time to surgery, and so the decision to perform, and perhaps the success of a repair, may be influenced by injury chronicity. This can be particularly pertinent, as advocates of repair typically recommend a repair procedure be performed in the acute (<6 weeks) time frame and that all midsubstance tears of the posterolateral corner be reconstructed. 10,11 Finally, we defined success as lack of subsequent surgery, but another way of measuring or defining success is through examination of the surgically treated ligament, either clinically or with stress radiographs, which is not possible here. Similarly, other outcomes, such as patient-reported outcomes, return to sports/activity/work, and functional outcomes were not available in the database and would be better evaluated in prospective studies. However, despite these limitations, we still believe that these findings are notable, given that the results are contrary to the majority of previous studies that have demonstrated that reconstruction has better outcomes, regardless of the ligament involved.
Conclusion
Previous comparison studies of knee extra-articular ligament repairs and reconstructions favor reconstructions, but are based on patient data collected >15 years ago with small sample sizes. With substantially more power than previous studies, the current study found that the revision rate of extra-articular ligamentous reconstruction around the knee was 3.3 times higher than the failure rate of primary ligamentous repair within the first 2 years of follow-up after the index procedure. Further study is needed to evaluate the differences in need for revision surgery and to determine the optimal surgical treatment for extra-articular knee ligament injury.
Footnotes
Final revision submitted September 3, 2022; accepted September 13, 2022.
One or more of the authors has declared the following potential conflict of interest or source of funding: research reported in this publication was supported by the National Institute of Diabetes and Digestive and Kidney Diseases of the National Institutes of Health (award No. T35DK104689). D.L.R. has received education payments from Gemini Mountain Medical and hospitality payments from Desert Mountain Medical. D.W. has received education payments from Arthrex and hospitality payments from Desert Mountain Medical and is a paid associate editor for The Orthopaedic Journal of Sports Medicine. G.P.T. has received education payments from Gemini Mountain Medical and hospitality payments from Desert Mountain Medical. R.C.S. has received grant support from DJO, education payments from Arthrex, and hospitality payments from Desert Mountain Medical and Smith & Nephew. M.J.M. has received consulting fees and speaking fees from Smith & Nephew. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval was not sought for the present study.
References
- 1. Arom GA, Yeranosian MG, Petrigliano FA, Terrell RD, McAllister DR. The changing demographics of knee dislocation: a retrospective database review. Clin Orthop Relat Res. 2014;472(9):2609–2614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Baker CL, Jr, Norwood LA, Hughston JC. Acute combined posterior cruciate and posterolateral instability of the knee. Am J Sports Med. 1984;12(3):204–208. [DOI] [PubMed] [Google Scholar]
- 3. Baker CL, Jr, Norwood LA, Hughston JC. Acute posterolateral rotatory instability of the knee. J Bone Joint Surg Am. 1983;65(5):614–618. [PubMed] [Google Scholar]
- 4. Bushnell BD, Bitting SS, Crain JM, Boublik M, Schlegel TF. Treatment of magnetic resonance imaging-documented isolated grade III lateral collateral ligament injuries in National Football League athletes. Am J Sports Med. 2010;38(1):86–91. [DOI] [PubMed] [Google Scholar]
- 5. Cheng X, Liu F, Zhou D, Paulus AC. Surgical intra- and extra-articular anterior cruciate ligament reconstruction: a meta-analysis. BMC Musculoskelet Disord. 2020;21(1):414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. DeLee JC, Riley MB, Rockwood CA, Jr. Acute posterolateral rotatory instability of the knee. Am J Sports Med. 1983;11(4):199–207. [DOI] [PubMed] [Google Scholar]
- 7. DeLong JM, Waterman BR. Surgical repair of medial collateral ligament and posteromedial corner injuries of the knee: a systematic review. Arthroscopy. 2015;31(11):2249–2255.e2245. [DOI] [PubMed] [Google Scholar]
- 8. DeLong JM, Waterman BR. Surgical techniques for the reconstruction of medial collateral ligament and posteromedial corner injuries of the knee: a systematic review. Arthroscopy. 2015;31(11):2258–2272.e2251. [DOI] [PubMed] [Google Scholar]
- 9. Fetto JF, Marshall JL. Medial collateral ligament injuries of the knee: a rationale for treatment. Clin Orthop Relat Res. 1978;132:206–218. [PubMed] [Google Scholar]
- 10. Geeslin AG, LaPrade RF. Outcomes of treatment of acute grade-III isolated and combined posterolateral knee injuries: a prospective case series and surgical technique. J Bone Joint Surg Am. 2011;93(18):1672–1683. [DOI] [PubMed] [Google Scholar]
- 11. Geeslin AG, Moulton SG, LaPrade RF. A systematic review of the outcomes of posterolateral corner knee injuries, part 1: surgical treatment of acute injuries. Am J Sports Med. 2016;44(5):1336–1342. [DOI] [PubMed] [Google Scholar]
- 12. Harner CD, Waltrip RL, Bennett CH, et al. Surgical management of knee dislocations. J Bone Joint Surg Am. 2004;86(2):262–273. [DOI] [PubMed] [Google Scholar]
- 13. Hoover NW. Injuries of the popliteal artery associated with fractures and dislocations. Surg Clin North Am. 1961;41:1099–1112. [DOI] [PubMed] [Google Scholar]
- 14. Indelicato PA. Non-operative treatment of complete tears of the medial collateral ligament of the knee. J Bone Joint Surg Am. 1983;65(3):323–329. [PubMed] [Google Scholar]
- 15. Jacobson KE, Chi FS. Evaluation and treatment of medial collateral ligament and medial-sided injuries of the knee. Sports Med Arthrosc Rev. 2006;14(2):58–66. [DOI] [PubMed] [Google Scholar]
- 16. Kannus P. Long-term results of conservatively treated medial collateral ligament injuries of the knee joint. Clin Orthop Relat Res. 1988;226:103–112. [PubMed] [Google Scholar]
- 17. Kennedy JC. Complete dislocation of the knee joint. J Bone Joint Surg Am. 1963;45:889–904. [PubMed] [Google Scholar]
- 18. Kharaz YA, Canty-Laird EG, Tew SR, Comerford EJ. Variations in internal structure, composition and protein distribution between intra- and extra-articular knee ligaments and tendons. J Anat. 2018;232(6):943–955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Kovachevich R, Shah JP, Arens AM, et al. Operative management of the medial collateral ligament in the multi-ligament injured knee: an evidence-based systematic review. Knee Surg Sports Traumatol Arthrosc. 2009;17(7):823–829. [DOI] [PubMed] [Google Scholar]
- 20. Krukhaug Y, Molster A, Rodt A, Strand T. Lateral ligament injuries of the knee. Knee Surg Sports Traumatol Arthrosc. 1998;6(1):21–25. [DOI] [PubMed] [Google Scholar]
- 21. Levy BA, Dajani KA, Morgan JA, et al. Repair versus reconstruction of the fibular collateral ligament and posterolateral corner in the multiligament-injured knee. Am J Sports Med. 2010;38(4):804–809. [DOI] [PubMed] [Google Scholar]
- 22. Levy BA, Dajani KA, Whelan DB, et al. Decision making in the multiligament-injured knee: an evidence-based systematic review. Arthroscopy. 2009;25(4):430–438. [DOI] [PubMed] [Google Scholar]
- 23. Levy BA, Fanelli GC, Whelan DB, et al. Controversies in the treatment of knee dislocations and multiligament reconstruction. J Am Acad Orthop Surg. 2009;17(4):197–206. [DOI] [PubMed] [Google Scholar]
- 24. Liow RY, McNicholas MJ, Keating JF, Nutton RW. Ligament repair and reconstruction in traumatic dislocation of the knee. J Bone Joint Surg Br. 2003;85(6):845–851. [PubMed] [Google Scholar]
- 25. McCarthy M, Ridley TJ, Bollier M, et al. Posterolateral knee reconstruction versus repair. Iowa Orthop J. 2015;35:20–25. [PMC free article] [PubMed] [Google Scholar]
- 26. Miyamoto RG, Bosco JA, Sherman OH. Treatment of medial collateral ligament injuries. J Am Acad Orthop Surg. 2009;17(3):152–161. [DOI] [PubMed] [Google Scholar]
- 27. O’Connor GA. Symposium: functional rehabilitation of isolated medial collateral ligament sprains. Collateral ligament injuries of the joint. Am J Sports Med. 1979;7(3):209–210. [DOI] [PubMed] [Google Scholar]
- 28. Rihn JA, Groff YJ, Harner CD, Cha PS. The acutely dislocated knee: evaluation and management. J Am Acad Orthop Surg. 2004;12(5):334–346. [DOI] [PubMed] [Google Scholar]
- 29. Shon OJ, Park JW, Kim BJ. Current concepts of posterolateral corner injuries of the knee. Knee Surg Relat Res. 2017;29(4):256–268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Stannard JP, Brown SL, Farris RC, McGwin G, Jr, Volgas DA. The posterolateral corner of the knee: repair versus reconstruction. Am J Sports Med. 2005;33(6):881–888. [DOI] [PubMed] [Google Scholar]
- 31. Stannard JP, Stannard JT, Cook JL. Repair or reconstruction in acute posterolateral instability of the knee: decision making and surgical technique introduction. J Knee Surg. 2015;28(6):450–454. [DOI] [PubMed] [Google Scholar]
- 32. Tzurbakis M, Diamantopoulos A, Xenakis T, Georgoulis A. Surgical treatment of multiple knee ligament injuries in 44 patients: 2-8 years follow-up results. Knee Surg Sports Traumatol Arthrosc. 2006;14(8):739–749. [DOI] [PubMed] [Google Scholar]
- 33. Wilson TC, Satterfield WH, Johnson DL. Medial collateral ligament “tibial” injuries: indication for acute repair. Orthopedics. 2004;27(4):389–393. [DOI] [PubMed] [Google Scholar]