Abstract
Background:
Despite the importance of return-to-play (RTP) rates, second anterior cruciate ligament (ACL) injury rates, and patient-reported outcomes of athletes returning to sports after ACL reconstruction (ACLR), these outcomes have not been evaluated together across a single cohort nor the pre- and intraoperative factors influencing outcomes explored.
Purpose:
To prospectively report outcomes after ACLR relating to RTP, second ACL injury, and International Knee Document Committee (IKDC) scores in a large cohort of athletes at a single center to examine the influence of pre- and intraoperative variables on these outcomes.
Design:
Cohort study; Level of evidence, 3.
Methods:
A consecutive cohort of 1432 athletes undergoing primary ACLR by 2 orthopaedic surgeons was followed up prospectively more than 2 years after surgery. Pre- and intraoperative findings were reported with outcomes at follow-up relating to RTP, second ACL injury, and IKDC. Between-group differences for each outcome were reported and the predictive ability of pre- and intraoperative variables relating to each outcome assessed with logistic regression.
Results:
There was >95% follow-up 2 years after surgery. The RTP rate was 81%, and of those who returned, 1.3% of those with patellar tendon grafts and 8.3% of those with hamstring grafts experienced ipsilateral rerupture (hazard ratio, 0.17). The contralateral ACL injury rate was 6.6%, and the IKDC score at follow-up was 86.8, with a greater proportion of patients with patellar tendon grafts scoring <80 on the IKDC (odds ratio, 1.56; 95% CI, 1.15–3.12). There was no relationship between time to RTP and second ACL injury, and there was a moderate correlation between ACL–Return to Sport After Injury score and RTP at follow-up (P < .001, rho = 0.46). There were a number of differences in pre- and intraoperative variables between groups for each outcome, but they demonstrated a poor ability to predict outcomes in level 1 athletes at 2-year follow-up.
Conclusion:
Findings demonstrated high overall RTP rates, lower reinjury rates with patellar tendon graft after 2-year follow-up in level 1 athletes, and no influence of time to RTP on second ACL injury. Despite differences between groups, there was poor predictive ability of pre- and intraoperative variables. Results suggest pre- and intraoperative variables for consideration to optimize outcomes in level 1 athletes after ACLR, but future research exploring other factors, such as physical and psychological recovery, may be needed to improve outcome prediction after ACLR.
Keywords: anterior cruciate ligament reconstruction, return to play, reinjury, athletes
Anterior cruciate ligament (ACL) rupture is a common knee injury in sports involving landing, pivoting, and change of direction. ACL reconstruction (ACLR) is the primary means of restoring structural stability to the knee to facilitate return to high-demand activities and sports.12 There are a number of outcomes used to assess the success of ACLR, including rate of return to play (RTP), secondary ACL injury incidence (to either the ipsilateral ACLR limb or the contralateral/non-ACLR limb), and patient-reported outcomes such as the International Knee Documentation Committee (IKDC) questionnaire.22 Despite the value of these outcomes, they have not been reported together on a single cohort of athletes after ACLR. Without reporting these outcomes concurrently, it is difficult to interpret the results of previous research—for example, a low reinjury rate may be a result of a low RTP rate, or a high RTP rate but low IKDC score might suggest that athletes are returning to play despite ongoing symptoms in the knee. Therefore, reporting all 3 main outcomes gives a more comprehensive overview of how the athlete fared after surgery and how the outcomes are interlinked. Differences in pre- and intraoperative variables relating to better and worse outcomes (ie, reinjury/no reinjury) have been investigated to explore factors that influence outcome. However, the ability of pre- and intraoperative data to predict these outcomes and thus inform surgeons’ clinical decision making and prognosis setting before surgery has not been investigated.
A resumption of preinjury sporting participation (ie, RTP), especially in high-demand level 1 sports (as defined by sports involving landing, pivoting, and hard cutting),15 is one of the primary indications for surgical reconstruction and patient goals thereafter.12,27 However, RTP rates are not as high as one might expect, with 55% of ACLR athletes reported to return to competitive sports.5 When athletes do RTP after ACLR, it is often despite ongoing knee symptoms and low levels of patient-reported knee function. The IKDC questionnaire is a commonly used measure of patient-perceived knee function and has been validated for use after ACLR.3,16 Lower IKDC scores have been reported in older populations, females, those with lower quadriceps strength, and individuals after ACLR as compared with previously uninjured athletes.4,33,35 Whether pre- and intraoperative data can predict future low RTP rates and scores relating to IKDC at follow-up has not been investigated.
Resumption of high-intensity level 1 sport confers an increased risk of second ACL injury. There is a higher risk of subsequent ACL injury after ACLR than in healthy populations,25 seen not only in the ipsilateral ACLR-limb but also in the previously uninjured contralateral/non-ACLR limb. A number of pre- and intraoperative variables have been suggested to be associated with second ACL injury risk, including age, sex, graft selection, and level of sport played.37–39 The predictive value of these measures in isolation or combination to identify those susceptible to second ACL injury is unknown.
Recovery of physical measures such as strength, power, and movement during testing after ACLR has been suggested to influence outcomes, especially relating to IKDC and subsequent injury to both the ACLR and non-ACLR knee.15,19,30,33,35 To accurately assess the influence of pre- and intraoperative variables on outcomes after ACLR and to minimize heterogeneity in physical recovery after surgery, postoperative pathways that include assessment of physical function and give feedback on progress and remaining physical deficits may hold relevance. The consistency of these pathways may ensure that those returning to high-demand level 1 sports are more physically prepared to do so. They may also allow for more accurate analysis of the role of pre- and intraoperative variables than previous studies involving large registries with multiple surgeons, orthopaedic centers, and potentially different rehabilitation and physical review pathways.
The aim of this study was to report a prospective in-depth follow-up (RTP, second ACL injury, and IKDC) on a consecutive cohort of athletes who underwent primary ACLR, followed by a physical review pathway. A secondary aim was to identify the association of pre- and intraoperative variables with each of the 3 outcomes and to assess the ability of these variables to predict each outcome after 2 years after surgery.
METHODS
Participants were prospectively recruited at a single institution between January 1, 2014, and September 31, 2016, from the caseload of 2 orthopaedic surgeons specializing in knee surgery and were consecutively recruited once diagnosis had been confirmed with MRI and orthopaedic review and a surgery date had been set. All those between the ages of 13 and 45 years who were undergoing primary ACLR, including those with previous contralateral injury, were included regardless of level or sports participation. Those with revision ACLR, those undergoing concurrent repair/reconstruction of other knee ligaments, and those outside the age range were excluded. The study was registered at ClinicalTrials.gov (NCT02771548), and all participants provided informed consent before the collection of study data. Ethical approval for the study was received from the hospital ethics committee.
The study protocol was explained to participants, and after consent they completed a preoperative questionnaire that captured data relating to age, sex, sporting participation, intention to RTP after ACLR, primary mechanism of injury, and Marx Activity Score at the time of injury. Surgery was carried out at the clinic by the 2 referring surgeons using equivalent arthroscopic and surgical techniques: bone–patellar tendon–bone (BPTB) or hamstring tendon (HT) autografts, with graft and tunnel placement within anatomic footprints and with graft selection guided by case history and surgeon preference. No allograft-based surgical reconstructions were included in the current analysis. BPTB grafts were secured with metal interference screws (Softsilk; Smith & Nephew). HT grafts were fixed with an EndoButton CL Ultra (Smith & Nephew) for femoral fixation and a soft tissue screw (Biosure PK; Smith & Nephew) for tibial fixation. Routine arthroscopy was performed to address coexisting intra-articular pathology and treated accordingly. Extra-articular lateral tenodesis was carried out at the surgeon’s discretion on a small cohort.26 Initial analysis revealed no difference in outcomes relating to this procedure, and these patients were included in the overall analysis. All intraoperative data were recorded at the time of surgery in the ACL registry that was set up for this study. Participants were instructed to undergo weightbearing as tolerated using 2 elbow crutches for approximately 2 weeks after surgery and were reviewed by their surgeon at 2 weeks, 3 months, and 6 to 9 months after surgery. Given the geographical spread of participants, the majority underwent rehabilitation by clinicians/therapists local to their place of residence. As part of their review process, they underwent a battery of physical tests to chart the progress of their rehabilitation. All participants were advised by their orthopaedic surgeon to achieve restoration of strength and power (>90% limb symmetry index) and not to RTP (defined as unrestricted resumption of their preinjury sport) before at least the 6-month mark after surgery. Participants were then followed up 2 years after surgery via email and telephone by the ACL registry coordinator who was responsible for scheduling of review assessments and completion of 2-year follow-up. At follow-up, participants completed the IKDC, ACL–Return to Sport After Injury (ACL-RSI), and Marx Activity Scale questionnaires and a RTP questionnaire that recorded information regarding the ability and timing of return to sports and level of participation as well as any subsequent injury to the ACLR knee or non-ACLR knee. Participants who experienced a second ACL injury to either knee were identified at follow-up or if they returned to the clinic for management before that time point with a diagnosis of ipsilateral or contralateral ACL injury confirmed with MRI.
Statistical Analysis
The demographic, intraoperative, and 2-year follow-up data for the cohort were reported with descriptive statistics. Differences in survival (up to 36 months after surgery) between ipsilateral and contralateral injury; BPTB and HT grafts; and early (6 to <9 months after surgery), middle (9–12 months), and late (13–16 months) RTP times were explored with a Kaplan-Meier survival analysis. Additionally, a Cox proportional hazard regression was calculated for graft type and RTP class during the analysis. To test for differences in the resulting Kaplan-Meier estimate, a log-rank test (>2 classes) or a multivariate log-rank test was performed. If a significant difference was observed, the log-rank test was performed for different ranges of the data (up to 1 month, up to 2 months, continuing up to 36 months) to determine the month of onset of the differences. The relationship between the 3 main outcome measures—RTP, IKDC, and second ACL injury (ipsilateral and contralateral separately)—and pre-, intra-, and follow-up data was explored. Given the potential influence of preoperative intent to RTP and participation in level 1 sports on outcomes, only those who intended to RTP before surgery and were involved in level 1 sports were included in the analysis relating to RTP and ipsilateral and contralateral injury (Figure 1). For the IKDC analysis, those who achieved a normal IKDC score (ie, >90) and those who had a poor IKDC score (<80) were selected for analysis. The standard error of measure for IKDC is between 3.2 and 5.6 points, so a minimum 10-point gap between groups was selected to offer clear differentiation between better and poorer scores.10,14 To examine relationships between measures, a point biserial correlation coefficient was used (as the measures were binary). To examine differences between groups for each variable (ie, RTP vs no RTP; ipsilateral ACL injury vs no ipsilateral ACL injury; contralateral ACL injury vs no contralateral ACL injury; IKDC <80 vs IKDC >90), a χ2 contingency table for nominal-type features was used. Where significant results were observed within the χ2 analysis, odds ratios (ORs) were computed. Last, a logistic regression was fitted to a selection of preoperative variables (sex, mechanism of injury, age, sport) and intraoperative variables (graft type, meniscal/chondral injury, extra-articular tenodesis; stepwise forward selection: P = .01 in, P = .05 out) to predict each outcome. The Marx Activity Scale was the only preoperative data point not included in the regression analysis owing to incomplete follow-up. The regression generation and testing methodology is explained in detail in the Appendix (available in the online version of this article).
Figure 1.
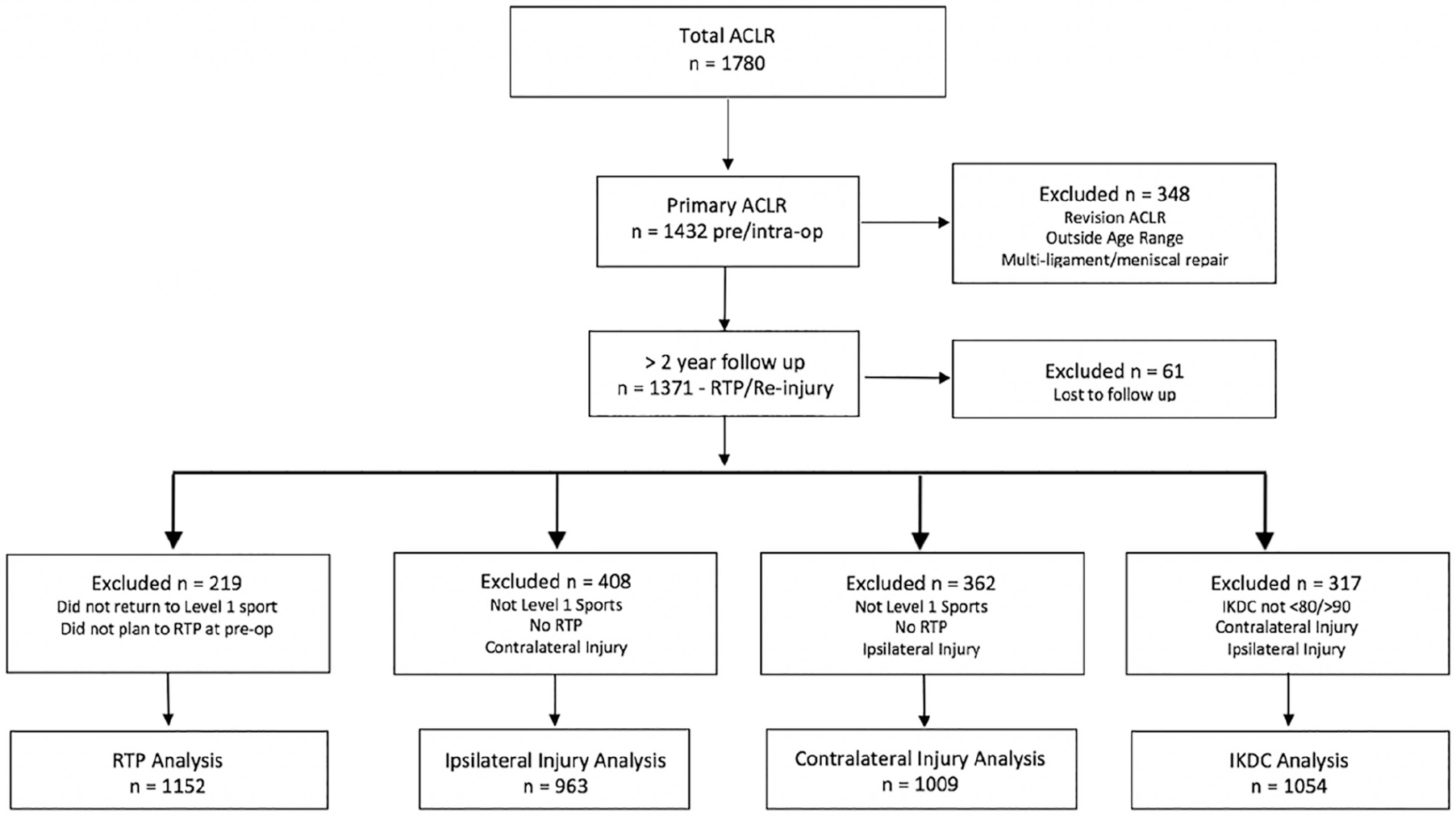
Flowchart of participant inclusion in analysis. ACLR, anterior cruciate ligament reconstruction; IKDC, International Knee Documentation Committee; RTP, return to play.
RESULTS
Preoperative Data
There were 1780 consecutive ACLRs carried out by the 2 surgeons between January 2014 and September 2016, with 1432 of these primary ACLRs and the majority of participants male (75%) (Table 1). Field sports were the most common activity at the time of primary injury; 90% of those undergoing surgery participated in level 1 sports (involving landing and sidestepping). Most athletes (95%) planned resumption of a similar or higher level of sport after surgery. Pivoting and sidestepping was the most common mechanism of primary injury (47%), and the mean time from initial injury to surgery was 4.5 months.
TABLE 1.
Patient Demographic and Preoperative Dataa
| n | % | |
|---|---|---|
|
| ||
| Total ACLR surgical procedures | 1780 | |
| Primary ACLRs between 13 and 45 y | 1432 | 80 |
| Sex | ||
| Male | 1068 | 75 |
| Female | 364 | 25 |
| Age, y | 24.3 ± 7.3b | |
| Sports played at time of injury | ||
| Gaelic football | 569 | 40 |
| Football (soccer) | 266 | 19 |
| Hurling | 209 | 15 |
| Rugby | 158 | 11 |
| Snow sports | 74 | 5 |
| Basketball | 29 | 2 |
| Racket sports | 6 | <1 |
| Athletics | 6 | <1 |
| Other | 115 | 8 |
| Preoperative expected level of sport return | ||
| Higher level | 329 | 23 |
| Same level | 1062 | 74 |
| Lower level | 15 | 1 |
| Other sport | 20 | 1 |
| No return | 5 | <1 |
| Mechanism of primary injury | ||
| Direct contact | 284 | 20 |
| Indirect contact | 219 | 15 |
| Noncontact | 929 | 65 |
| Pivoting/sidestepping | 670 | 47 |
| Jumping/landing | 293 | 20 |
| Being tackled | 252 | 18 |
| Tackling | 105 | 7 |
| Other | 116 | 8 |
| Preoperative Marx Activity Scale score (74% patients)b | 10.9 ± 5.1 | |
| Time from injury to surgery, mob | 4.56 ± 10.7 | (1–147) |
ACLR, anterior cruciate ligament reconstruction.
Mean ± SD (range).
Intraoperative Data
The BPTB graft was the most commonly used graft (80%) for primary ACLRs (Table 2). Medial meniscal injury was reported in 24% of surgical procedures and lateral meniscal injury in 38%. Injury to the medial and lateral femoral condylar surfaces was reported in 17% and 15% of cases, respectively, with a low incidence of injury to tibial and patellofemoral surfaces reported (<1%).
TABLE 2.
Intraoperative Findings
| n | % | |
|---|---|---|
|
| ||
| Graft type | ||
| Patellar | 1142 | 80 |
| Hamstring | 290 | 20 |
| Extra-articular tenodesis | 32 | 2.2 |
| Medial meniscal injury | ||
| Nil | 1093 | 76 |
| Left in situ | 159 | 11 |
| Meniscectomy | 109 | 8 |
| Repair | 71 | 5 |
| Lateral meniscal injury | ||
| Nil | 888 | 62 |
| Left in situ | 233 | 16 |
| Meniscectomy | 270 | 19 |
| Repair | 41 | 3 |
| Medial femoral condyle | ||
| Nil | 1194 | 83 |
| Grade 1–2 | 171 | 12 |
| Grade 3–4 | 67 | 5 |
| Lateral femoral condyle | ||
| Nil | 1215 | 85 |
| Grade 1–2 | 196 | 14 |
| Grade 3–4 | 21 | 1 |
| Medial tibial condyle | ||
| Nil | 1420 | 99 |
| Grade 1–2 | 8 | <1 |
| Grade 3–4 | 4 | <1 |
| Lateral tibial condyle | ||
| Nil | 1421 | 99 |
| Grade 1–2 | 9 | <1 |
| Grade 3–4 | 2 | <1 |
| Patella | ||
| Nil | 1399 | 98 |
| Grade 1–2 | 28 | 1 |
| Grade 3–4 | 5 | <1 |
| Trochlea | ||
| Nil | 1417 | 99 |
| Grade 1–2 | 9 | <1 |
| Grade 3–4 | 6 | <1 |
Two-Year Follow-up
There was 95.7% follow-up >2 years after surgery (mean, 28.4 months; range, 24–55 months) on RTP and second ACL injury outcomes (Table 3). Return to sport was achieved by 81% of athletes across sports at 11.1 ± 5.1 months (mean ± SD) after surgery, with 82% of those participating in level 1 sports returning to participation. The reinjury rate to the ACLR knee was 2.7% for all ACLRs, with 1.3% of BPTB and 8.3% of HT grafts experiencing reinjury. The mean time from surgery to ipsilateral injury was 21.4 ± 10.4 months and from RTP to reinjury, 12.5 ± 9.6 months. The incidence of injury to the contralateral (non-ACLR) limb was 6.6% at 24.6 ± 10.2 months after surgery and 15.2 ± 10.1 months after RTP. The mean IKDC score at follow-up for noninjured participants (no second ACL injury) was 86.8 ± 10.1; Marx Activity Scale score, 9.9 ± 5.2; and ACL-RSI score, 74.8 ± 22.6.
TABLE 3.
Two-Year Follow-up Outcomesa
| n or Mean 6 SD | % or Range | |
|---|---|---|
|
| ||
| Follow-up (primary ACLRs, n = 1432) | 1371 | 95.7 |
| Time to follow-up, mo | 28.4 ± 7.9 | 24–55 |
| RTP (all sports) | ||
| Yes | 1152 | 81 |
| No | 219 | 15 |
| Unknown | 61 | 4 |
| Time to RTP, mo | 11.1 ± 5.1 | 3–32 |
| RTP level 1 sports (n = 1237) | 1012 | 82 |
| Second ACL injury | ||
| Ipsilateral total | 39 | 2.7 |
| Ipsilateral BPTB graft | 15 | 1.3 |
| Ipsilateral HT graft | 24 | 8.3 |
| Contralateral | 94 | 6.6 |
| Time to second ACL injury, mo | ||
| Ipsilateral surgery to injury | 21.4 ± 10.4 | 7–50 |
| Hamstring surgery to injury | 19.8 ± 9.9 | 4–40 |
| Patellar surgery to injury | 23.9 ± 11.2 | 8–50 |
| Ipsilateral RTP to injury | 12.5 ± 9.6 | 1–42 |
| Contralateral surgery to injury | 24.6 ± 10.2 | 8–50 |
| Contralateral RTP to injury | 15.2 ± 10.1 | 1–45 |
| IKDC score (83% patients) | 86.8 ± 10.1 | |
| >90 | 848 | 60 |
| <80 | 206 | 14 |
| Marx Activity Scale score (72% patients) | 9.9 ± 5.2 | |
| ACL-RSI score (48% patients) | 74.8 ± 22.6 | |
ACL, anterior cruciate ligament; ACLR, anterior cruciate ligament reconstruction; ACL-RSI, ACL-Return to Sport After Injury; BPTB, bone–patellar tendon–bone; HT, hamstring tendon; IKDC, International Knee Documentation Committee; RTP, return to play.
The Kaplan-Meier survival analysis reported a lower survival rate of the contralateral limb as compared with the ipsilateral limb over time (P < .001) (Figure 2) with differences in survival commencing from month 20 after surgery. There was a superior survival rate of the BPTB graft relative to the HT graft over time from month 11 after surgery (P < .001) (Figure 3). The BPTB graft had an 83% lower reinjury rate each month (hazard ratio, 0.17; 95% CI, 0.08–0.34). There was no difference in survival distribution among those who made an early (6 to <9 months), middle (9–12 months), or late (13–16 months) return to sports after surgery when ACL injury to either knee (P = .234) or the ACLR (ipsilateral) knee on its own (P = .434) was assessed.
Figure 2.
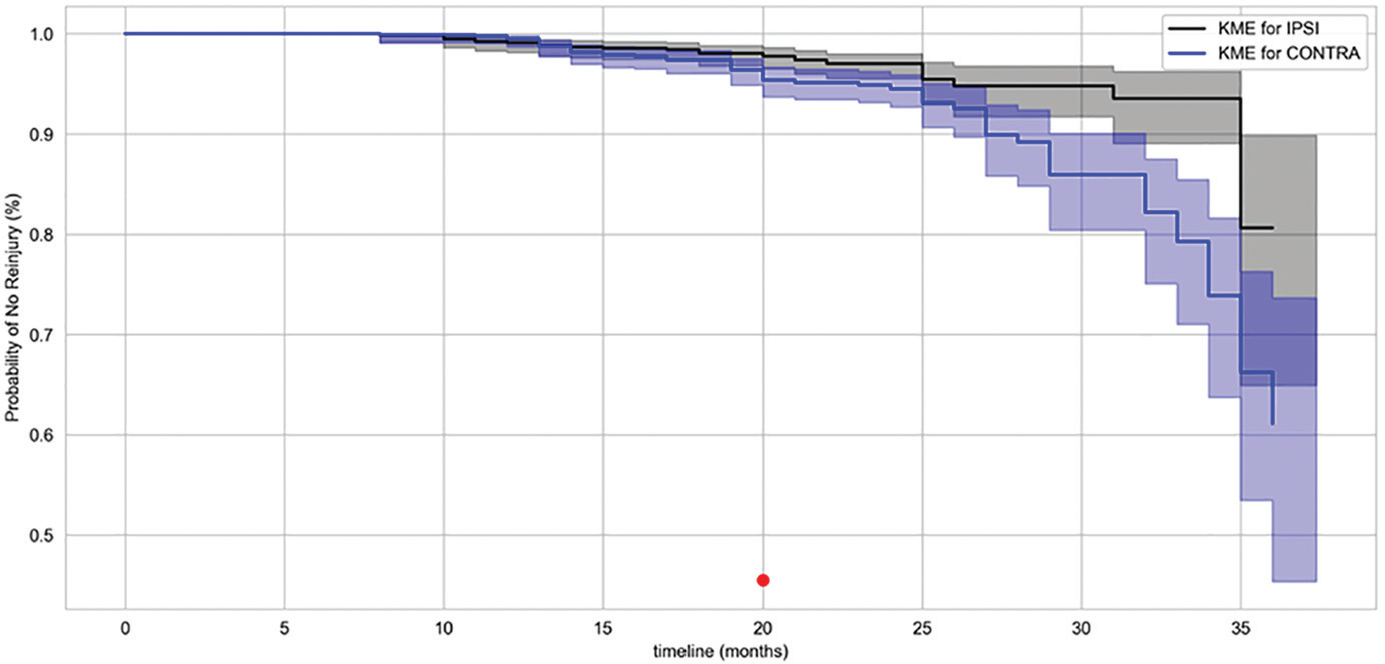
Kaplan-Meier survival analysis for ipsilateral vs contralateral anterior cruciate ligament (ACL). The dot indicates the first month that a difference in survival was detected between groups. CONTRA, contralateral ACL injury; IPSI, ipsilateral ACL injury; KME, Kaplan-Meier estimate.
Figure 3.
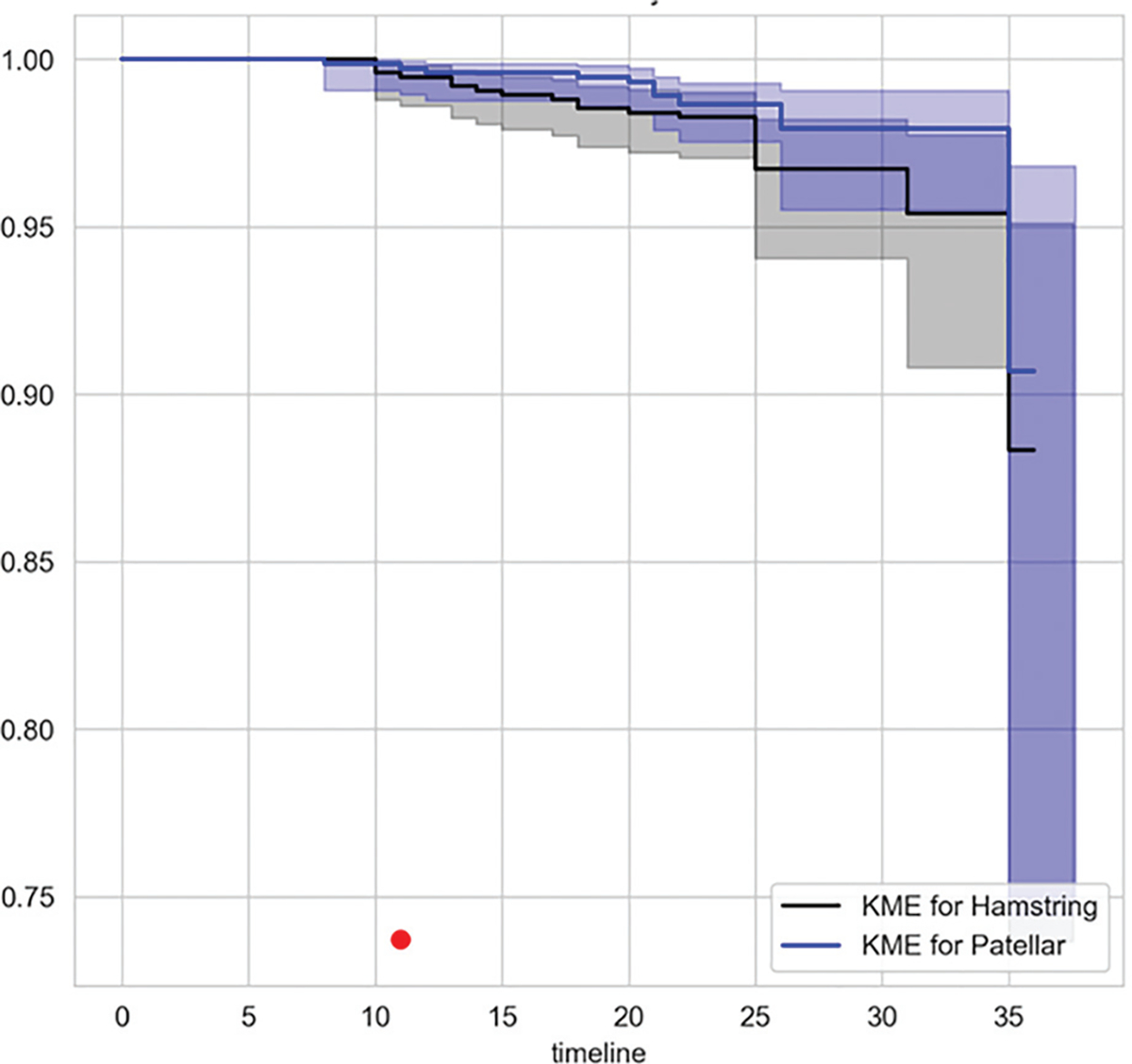
Kaplan-Meier survival analysis for bone–patellar tendon–bone vs hamstring tendon graft. The dot indicates the first month that a difference in survival was detected between groups. KME, Kaplan-Meier estimate.
Differences in RTP vs No RTP
The differences between athletes who achieved RTP and those who did not after 2-year follow-up are reported in Table 4. Those athletes who preoperatively determined that they did not plan to return to the same level of activity (n = 28) and those who did not play level 1 sports (n = 182) were removed from the analysis. There was a weak correlation between age (negative correlation) and RTP and preoperative Marx Activity Scale score and RTP, with younger athletes and those with higher preoperative Marx scores returning to sports (P < .001; rho = −0.18 and 0.17, respectively). There was a moderate correlation between ACL-RSI score at follow-up and RTP (P < .001, rho = 0.56) and a weak correlation between IKDC at follow-up and RTP (P < .001, rho = 0.29). There was a significant difference in RTP between groups depending on the presence of injury to the medial (P = .008) or lateral (P = .041) meniscus, with higher rates of return in those with no medial meniscal tear or when left in situ and those with no lateral meniscal tear or meniscectomy. Similarly, there was a difference in RTP depending on the presence of medial femoral condyle injury (P = .002), with those with a grade 3–4 injury having a lower rate of return (OR, 3.03; 95% CI, 1.58–5.55). When pre- and intraoperative variables were fit to RTP with a stepwise forward logistic regression, only age met the inclusion criterion (older athletes were less likely to RTP), and the generated logistic regression achieved an accuracy of 64% (baseline, 87%) with an AUC of 0.66 (sensitivity, 0.66; specificity, 0.65), indicating poor ability of pre- and intraoperative data to predict RTP after 2-year follow-up.
TABLE 4.
Differences Between RTP and No RTP at Follow-upa
| RTP, n (%) or Mean ± SD |
|||||
|---|---|---|---|---|---|
| Yes | No | P Value | Statistic | OR: No RTP (95% CI) | |
|
| |||||
| Sex | |||||
| Male | 794 (86) | 124 (14) | .813 | 0.06b | |
| Female | 201 (86) | 33 (14) | |||
| Age, y | 22.7 ± 6.2 | 26.1 ± 6.7 | <.001c | −0.18d | |
| Preoperative Marx score | 11.8 ± 4.8 | 9.2 ± 5.3 | <.001c | 0.17d | |
| Injury mechanism | |||||
| Jumping/landing | 200 (89) | 24 (11) | .07 | 8.67b | |
| Sidestep/pivot | 467 (86) | 79 (14) | |||
| Tackling | 78 (79) | 20 (21) | |||
| Being tackled | 205 (89) | 24 (11) | |||
| Other | 45 (81) | 10 (19) | |||
| Injury contact | |||||
| Direct | 207 (88) | 29 (12) | .473 | 1.5b | |
| Indirect | 160 (84) | 31 (16) | |||
| Noncontact | 628 (86) | 97 (14) | |||
| Graft type | |||||
| BPTB | 795 (86) | 129 (14) | .739 | 0.6b | |
| HT | 200 (88) | 28 (12) | |||
| Extra-articular tenodesis | |||||
| Yes | 972 (87) | 150 (13) | .166 | 2.46b | |
| No | 23 (77) | 7 (23) | |||
| Medial meniscus treatment | |||||
| Nil | 778 (88) | 111 (12) | .008c | 11.91b | |
| Left in situ | 123 (87) | 17 (13) | 0.97 (0.56–1.66) | ||
| Meniscectomy | 52 (76) | 16 (24) | 2.17 (1.19–3.84) | ||
| Repair | 41 (74) | 13 (26) | 2.22 (1.14–4.34) | ||
| Lateral meniscus treatment | |||||
| Nil | 599 (87) | 87 (13) | .041c | 9.96b | |
| Left in situ | 155 (79) | 39 (21) | 1.72 (1.13–2.63) | ||
| Meniscectomy | 212 (84) | 39 (16) | 0.81 (0.51–1.29) | ||
| Repair | 28 (82) | 6 (18) | 1.47 (0.59–3.70) | ||
| Chondral pathology: MFC | |||||
| Nil | 858 (87) | 126 (13) | .002c | 12.58b | |
| Grade 1–2 | 103 (87) | 16 (13) | 1.05 (0.60–1.85) | ||
| Grade 3–4 | 34 (69) | 15 (31) | 3.03 (1.58–5.55) | ||
| Chondral pathology: LFC | |||||
| Nil | 851 (87) | 124 (13) | .107 | 4.47b | |
| Grade 1–2 | 131 (81) | 30 (19) | |||
| Grade 3–4 | 13 (81) | 3 (19) | |||
| ACL-RSI score | 79.4 ± 19.5 | 41.3 ± 24.1 | <.001c | 0.56d | |
| IKDC score | 88.5 ± 8.8 | 81.2 ± 10.5 | <.001c | 0.29d | |
ACL-RSI, ACL-Return to Sport After Injury; BPTB, bone–patellar tendon–bone; HT, hamstring tendon; IKDC, International Knee Documentation Committee; LFC, lateral femoral condyle; MFC, medial femoral condyle; OR, odds ratio; RTP, return to play.
Chi-square analysis.
P < .05.
Point biserial correlation.
Differences in Ipsilateral Reinjury and No Ipsilateral Reinjury
The differences between athletes who had an ipsilateral ACL injury and those who did not at follow-up are reported in Table 5. For the comparisons of ipsilateral reinjury rates, there were 222 athletes who did not return to play, 90 who had a contralateral ACL injury, and 156 who did not play level 1 sports or had a combination thereof and were excluded from the analysis. There was a significant difference in ipsilateral injury depending of graft choice, with 11.9% of HT grafts experiencing an ipsilateral injury as compared with 1.9% of BPTB grafts (P < .001, chi = 40.39; OR, 6.80). There was a weak correlation between age and ipsilateral injury (P < .003, coefficient = 0.10), with those with an ipsilateral injury younger than those without. The logistic regression model with pre- and intraoperative data to predict ipsilateral ACL injury selected HT graft, male sex, age, and sidestep primary injury mechanism to be included in the model. The logistic regression reported an accuracy of 76% (baseline, 96%) with a receiver operating characteristic (ROC) area under the curve (AUC) of 0.73 (sensitivity, 0.76; specificity, 0.69), indicating that pre- and intraoperative data had only fair accuracy in predicting ipsilateral ACL injury and that the accuracy is well below the baseline.
Table 5.
Differences Between in Ipsilateral Anterior Cruciate Ligament Injury and No Ipsilateral Injurya
| Ipsilateral Injury, n (%) or Mean ± SD |
|||||
|---|---|---|---|---|---|
| Yes | No | P Value | Statistic | OR: Ipsilateral Injury (95% CI) | |
|
| |||||
| Sex | |||||
| Male | 32 (4) | 736 (96) | .485 | 0.49b | |
| Female | 6 (3) | 189 (97) | |||
| Age, y | 20.3 ± 5.1 | 24.2 ± 7.2 | .003c | 0.10d | |
| Preoperative Marx score | 11.4 (4.9) | 11.7 (5.1) | .803 | 0.01d | |
| Injury mechanism | |||||
| Jumping/landing | 7 (3) | 189 (97) | .992 | 0.27b | |
| Sidestep/pivot | 19 (4) | 432 (96) | |||
| Tackling | 3 (4) | 73 (96) | |||
| Being tackled | 7 (3) | 189 (97) | |||
| Other | 2 (5) | 42 (95) | |||
| Injury contact | |||||
| Direct | 8 (4) | 199 (96) | .885 | 0.25b | |
| Indirect | 7 (4) | 143 (96) | |||
| Noncontact | 23 (4) | 583 (96) | |||
| Graft type | |||||
| BPTB | 15 (1.9) | 755 (98.1) | <.001c | 40.39b | 6.80 (3.48–13.31) |
| HT | 23 (11.9) | 170 (89.1) | |||
| Extra-articular tenodesis | |||||
| Yes | 0 (0) | 24 (100) | .337 | 0.92b | |
| No | 38 (4) | 901 (96) | |||
| Medial meniscus treatment | |||||
| Nil | 31 (4) | 721 (96) | .779 | 1.09b | |
| Left in situ | 3 (2) | 112 (98) | |||
| Meniscectomy | 3 (5) | 53 (95) | |||
| Repair | 1 (2) | 38 (98) | |||
| Lateral meniscus treatment | |||||
| Nil | 25 (4) | 559 (96) | .504 | 3.33b | |
| Left in situ | 8 (5) | 140 (95) | |||
| Meniscectomy | 5 (2) | 198 (98) | |||
| Repair | 0 (0) | 28 (100) | |||
| Chondral pathology: MFC | |||||
| Nil | 34 (4) | 797 (96) | .427 | 1.7b | |
| Grade 1–2 | 4 (4) | 95 (96) | |||
| Grade 3–4 | 0 (0) | 33 (100) | |||
| Chondral pathology: LFC | |||||
| Nil | 31 (3) | 790 (97) | .786 | 0.48b | |
| Grade 1–2 | 6 (5) | 123 (95) | |||
| Grade 3–4 | 1 (7) | 12 (93) | |||
BPTB, bone–patellar tendon–bone; HT, hamstring tendon; LFC, lateral femoral condyle; MFC, medial femoral condyle; OR, odds ratio.
Chi-square analysis.
P < .05.
Point biserial correlation.
Differences in Contralateral Injury and No Contralateral Injury
The differences between athletes who had a contralateral ACL injury and those did not at follow-up are reported in Table 6. Those athletes who had not returned to play (n = 222), those who had an ipsilateral ACL injury (n = 39), and those who did not play level 1 sports (n = 159) or had a combination thereof were removed from the analysis. Of the variables examined, only age had a significant but weak relationship with contralateral ACL injury (P < .001, rho = −0.16), with those with a contralateral injury younger than those without. The logistic regression based on pre- and intraoperative data to predict contralateral ACL injury selected age, male sex, and noncontact injury mechanism to be included in the model. The logistic regression achieved an accuracy of 63% (baseline, 96%) with an AUC of 0.71 (sensitivity, 0.63; specificity, 0.64), indicating that pre- and intraoperative data have only fair accuracy in predicting contralateral ACL injury and that the accuracy is well below the baseline.
Table 6.
Differences Between in Contralateral Anterior Cruciate Ligament Injury and No Contralateral Injurya
| Contralateral Injury, n (%) or Mean ± SD |
||||
|---|---|---|---|---|
| Yes | No | P Value | Statistic | |
|
| ||||
| Sex | ||||
| Male | 66 (8) | 736 (92) | .829 | 0.05a |
| Female | 18 (8) | 189 (92) | ||
| Age, y | 19.7 ± 4.2 | 24.2 ± 7.2 | <.001c | −0.16d |
| Preoperative Marx score | 12.4 ± 4.3 | 11.4 ± 5.0 | .303 | 0.04d |
| Injury mechanism | ||||
| Jumping/landing | 17 (8) | 189 (92) | .671 | 2.36b |
| Sidestep/pivot | 40 (8) | 432 (92) | ||
| Tackling | 3 (4) | 73 (96) | ||
| Being tackled | 20 (9) | 189 (91) | ||
| Other | 4 (9) | 42 (91) | ||
| Injury contact | ||||
| Direct | 15 (7) | 199 (93) | .73 | 0.63b |
| Indirect | 14 (9) | 143 (91) | ||
| Noncontact | 55 (9) | 583 (91) | ||
| Graft type | ||||
| BPTB | 66 (8) | 755 (92) | .495 | 0.47b |
| HT | 18 (9) | 170 (91) | ||
| Extra-articular tenodesis | ||||
| Yes | 0 (0) | 24 (100) | .135 | 2.23b |
| No | 84 (9) | 901 (91) | ||
| Medial meniscus treatment | ||||
| Nil | 67 (9) | 721 (91) | .975 | 0.22b |
| Left in situ | 10 (8) | 112 (92) | ||
| Meniscectomy | 4 (7) | 53 (3) | ||
| Repair | 3 (7) | 38 (93) | ||
| Lateral meniscus treatment | ||||
| Nil | 48 (8) | 559 (92) | .477 | 3.50b |
| Left in situ | 19 (12) | 140 (88) | ||
| Meniscectomy | 15 (7) | 198 (93) | ||
| Repair | 2 (7) | 27 (93) | ||
| Chondral pathology: MFC | ||||
| Nil | 68 (8) | 797 (92) | .105 | 2.63b |
| Grade 1–2 | 14 (13) | 95 (87) | ||
| Grade 3–4 | 2 (6) | 33 (94) | ||
| Chondral pathology: LFC | ||||
| Nil | 74 (9) | 790 (91) | .711 | 0.14b |
| Grade 1–2 | 10 (7) | 123 (93) | ||
| Grade 3–4 | 0 (0) | 12 (100) | ||
BPTB, bone–patellar tendon–bone; HT, hamstring tendon; LFC, lateral femoral condyle; MFC, medial femoral condyle.
Chi-square analysis.
P < .05.
Point biserial correlation.
Differences in IKDC Score <80 and >90
The differences between those with an IKDC score <80 and >90 at follow-up are reported in Table 7. A sex disparity was seen, with a greater proportion of males achieving IKDC >90 (P < .001). There was a weak correlation between age and IKDC score, with those with >90 younger than those with <80 (P < .001, coefficient = −0.18). In addition, there were differences between groups in relation to level of sport, with those participating in level 2 sports having a higher proportion of athletes with IKDC <80 (P < .001; OR = 2.26). There were differences in the intraoperative data: those with a BPTB graft were more likely to have IKDC <80 (OR, 1.56). In addition, differences were present in relation to medial meniscal injury (P < .001), with higher proportions of those with IKDC <80 having undergone meniscectomy (OR, 2.62) or meniscal repair (OR, 2.15). Similarly, injury to the medial femoral condyle was detrimental, with athletes with IKDC <80 having a higher proportion of grade 3–4 chondral injuries (P < .001; OR, 3.6). The logistic regression predicting IKDC >90 used age, sex, and sidestepping injury mechanism for inclusion in the regression and achieved an accuracy of 59% in the testing data (baseline, 80%) with an AUC of 0.63 (sensitivity, 0.71; specificity, 0.57), suggesting a poor ability of pre- and intraoperative data to predict who will achieve IKDC >90 at follow-up.
TABLE 7.
Differences Between IKDC Score <80 and .90a
| IKDC, n (%) or Mean ± SD |
|||||
|---|---|---|---|---|---|
| <80 | >90 | P Value | Statistic | OR: <80 (95% CI) | |
|
| |||||
| Sex | |||||
| Male | 138 (17) | 664 (83) | .002b | 9.91c | |
| Female | 68 (27) | 184 (73) | 1.72 (1.23–2.43) | ||
| Age, y | 26.8 ± 7.5 | 23.6 ± 6.7 | <.001b | −0.18d | |
| Sports played when injured | |||||
| Level 1 | 163 (18) | 756 (82) | <.001b | 15.48c | |
| Level 2 | 43 (32) | 92 (68) | 2.26 (1.65–3.45) | ||
| Marx score | 10.2 ± 5.4 | 11.7 ± 4.8 | .086 | 0.07d | |
| Injury mechanism | |||||
| Jumping/landing | 42 (19) | 185 (81) | .098 | 7.82c | |
| Sidestep/pivot | 99 (20) | 401 (80) | |||
| Tackling | 20 (26) | 56 (74) | |||
| Being tackled | 26 (15) | 150 (85) | |||
| Other | 19 (26) | 56 (74) | |||
| Injury contact | |||||
| Direct | 39 (19) | 167 (81) | .821 | 0.39c | |
| Indirect | 32 (21) | 123 (79) | |||
| Noncontact | 135 (20) | 557 (80) | |||
| Graft type | |||||
| BPTB | 176 (21) | 658 (79) | .039b | 4.27c | 1.56 (1.15–3.12) |
| HT | 30 (14) | 190 (86) | |||
| Extra-articular tenodesis | |||||
| Yes | 5 (22) | 18 (78) | .773 | 0.08c | |
| No | 201 (19) | 830 (81) | |||
| Medial meniscus treatment | |||||
| Nil | 141 (17) | 680 (83) | <.001b | 17.03c | |
| Left in situ | 24 (21) | 88 (79) | 1.24 (0.75–2.06) | ||
| Meniscectomy | 27 (35) | 51 (65) | 2.62 (1.54–4.45) | ||
| Repair | 14 (33) | 29 (67) | 2.15 (1.09–4.25) | ||
| Lateral meniscus treatment | |||||
| Nil | 118 (18) | 527 (82) | .104 | 6.17c | |
| Left in situ | 38 (23) | 128 (77) | |||
| Meniscectomy | 38 (28) | 170 (82) | |||
| Repair | 12 (34) | 23 (66) | |||
| Chondral pathology: MFC | |||||
| Nil | 161 (18) | 723 (82) | .001b | 17.97c | |
| Grade 1–2 | 25 (22) | 93 (78) | 1.15 (0.70–1.89) | ||
| Grade 3–4 | 20 (38) | 32 (62) | 3.60 (1.92–6.73) | ||
| Chondral pathology: LFC | |||||
| Nil | 168 (19) | 728 (81) | .192 | 3.3c | |
| Grade 1–2 | 36 (25) | 110 (75) | |||
| Grade 3–4 | 2 (17) | 10 (83) | |||
BPTB, bone–patellar tendon–bone; HT, hamstring tendon; IKDC, International Knee Documentation Committee; LFC, lateral femoral condyle; MFC, medial femoral condyle; OR, odds ratio.
P < .05.
Chi-square analysis.
Point biserial correlation.
DISCUSSION
This prospective longitudinal study reports outcomes at a minimum of 2 years after surgery from a large cohort of athletes, 90% of whom were playing high-demand level 1 sports, who underwent ACLR with a postoperative physical review pathway at a single center. The cohort was comprehensively characterized and followed up (95%), with reports across a range of domains, including RTP, IKDC, and second ACL injury. The results demonstrated a lower reinjury rate for BPTB graft and a high level of RTP for those returning to level 1 sports at follow-up, with a higher percentage of those returning to level 1 sports achieving IKDC >90. In addition, RTP 6 months after surgery did not influence a second ACL injury. The study identified differences in pre- and intraoperative data between those who had better and worse outcomes. However, the results highlighted the difficulty in using these data points to predict outcomes over 2 years after surgery. The study demonstrates the success of this management pathway in athletes returning to high-demand level 1 sports and suggests other factors (eg, physical and psychological recovery after surgery) that may need to be explored in conjunction with pre- and intraoperative data to better predict positive outcomes after ACLR.
Return to Play
The 82% RTP rate reported in this study for the entire cohort was comparable to previous reviews in the literature,5,21 and the 81% rate for those involved in level 1 sports was much higher than the 65% returning to preinjury sport and 55% returning to competitive sports.5 Differences between those who had and had not returned to level 1 sports at follow-up included age (greater RTP rate with weak correlation to younger age, rho = −0.18), in keeping with the previous literature.5,7 In addition, there were lower RTP rates in those with medial or lateral meniscal injury or grade 3–4 medial femoral chondral injuries present at the time of surgery. The influence of meniscal and chondral injury on RTP rates after primary ACLR has not been reported in the literature and may warrant further exploration. Its effect on RTP after revision ACLR has been investigated, with no influence of meniscal injury but with a negative effect of chondral injury on RTP rates.1 The main reasons cited in the literature for non-RTP after ACLR are fear of reinjury, ongoing knee symptoms, and social factors.6,11 This is supported in this study, with lower IKDC scores (patient-reported outcome relating to knee function) and ACL-RSI scores (patient-reported readiness to RTP) in those who had not returned to play. Given the main factors for non-RTP outlined here, it was intuitive that there would be an inability to predict RTP based on pre- and intraoperative data, with results reporting a poor prediction accuracy of 64% and an AUC of 0.66. However, the follow-up time for this study is relatively short, and it is unknown if these factors, especially those relating to meniscal and chondral injury, had an effect on the ability to continue sporting participation with longer follow-up.
Second ACL Injury
This study reported an overall reinjury rate of 2.7%, with a rate of 1.3% for BPTB and 8.3% for HT. When only those who returned to level 1 sports were examined, the reinjury rate was 1.9% for BPTB and 11.9% for HT. The overall reinjury rate is favorable compared with other large cohorts with 2-year follow-up at 4.4%13,18 and Swedish registries that reported a revision rate of only 1.8% (as opposed to all reinjuries).2 There was a clear difference in rerupture rate between HT and BPTB grafts, with a significant difference in graft survival (P < .001). BPTB had an 84% lower risk of injury every month (HR, 0.17) and was almost 7 times less likely to rerupture at >2-year follow-up. There is differing evidence on the influence of graft selection in reinjury in the literature. In a meta-analysis by Freedman et al,13 as well as in a systematic review of Scandinavian registries,37 lower rerupture rates for BPTB grafts were reported. However, other systematic reviews reported no difference in rerupture rates in graft selection, albeit at longer follow-up.23,36 Additional differences between those who had an ipsilateral injury and those who did not in this study related to age, with younger athletes having higher ipsilateral injury rates, although the correlation was weak (rho = 0.11, P < .001). Younger athletes have been widely reported to be at higher risk of reinjury in the previous literature,38,40 principally through higher levels of RTP in high-risk sports, as seen in our data relating to RTP in level 1 sports. The predictive ability of pre- and intraoperative data to identify ipsilateral ACL injury was fair (76% accuracy; ROC, 0.73), with hamstring graft selection the dominant factor. The accuracy was not superior to suggesting by default that no athlete would experience reinjury; however, the low numbers relating to reinjury make more accurate prediction difficult. The influence of graft type may be a point for consideration during the clinical decision making of those treating level 1 athletes who want to RTP.
The study also reported a higher overall contralateral injury rate than ipsilateral injury rate (6.6% vs 2.7% overall) and significant differences in survival (P < .001). The contralateral ACL injury rate in those returning to level 1 sports was 9%, with the only difference between those who went on to contralateral injury and those who did not relating to age (weak correlation [rho = −0.16, P < .001] with higher injury rate in younger athletes), which is in agreement with the previous literature.29,38,41 As there were few differences in pre- and intraoperative data, there was a low ability to predict who would experience a contralateral injury, with a lower-than-baseline accuracy (63% vs 96%) and AUC of 0.71. Given the higher incidence of contralateral ACL injury, future work needs to prospectively identify those at higher risk so that those factors can be addressed before RTP.
Of particular interest in this study was the absence of relationship between time to RTP and either contralateral or ipsilateral injury. Early return had been suggested to be a risk factor for rerupture to the operated graft19 and other injury to the operated knee,15 with the risk of rerupture highest in the first year after return and with some recommending that return to sports be delayed until 2 years after surgery.28 This relationship with time from surgery has been suggested to be due to the time required for graft ligamentization8,17,31 and redevelopment of movement and physical qualities after surgery.15,19 However, our study reported a mean time to injury after surgery of 21.4 months for ipsilateral injury and 24.6 months for contralateral injury. The time from RTP to injury was 12.5 months for ipsilateral injury and 15.2 months for contralateral injury. In addition, there was no difference in survival of contralateral or ipsilateral knee among those who returned from 6 to <9 months, from 9 to 12 months, and from 12 to 16 months. Our results do not therefore support a timeline-based restriction on RTP relating to second ACL injury after 6 months after surgery.
International Knee Documentation Committee
This study reported outcomes relating to IKDC scores after 2 years with results comparable to normative data of those with a history of knee injury and to other ACLR studies.3,20 To identify the relationship between pre- and intraoperative findings and IKDC scores, the cohort was split into those who had poorer outcome (IKDC <80) and those who had a better outcome or return to normative levels (IKDC >90). A number of factors were identified as being different between groups, with a higher percentage of younger athletes, males, those playing level 1 sports, and those with higher preoperative Marx activity score having IKDC >90, which is in agreement with previous literature.3 There was a difference between groups relating to graft type, with those having an HT more likely to have IKDC >90. Graft site morbidity and additional quadriceps weakness after BPTB have been suggested to be a source of increased knee symptoms after ACLR as compared with HT, and this may be a contributor to the difference in scores.4,32 This is an often-cited reason for selection of HT graft over BPTB for ACLR. However, given that the primary indication for ACLR is to provide structural stability to the knee to participate in high-demand activities and based on the higher reinjury rate in HT reported in this study, pre- and postoperative targeting of quadriceps strength and lower limb function after BPTB graft selection to offset the reported difference IKDC may be more appropriate than a change in graft selection. Those achieving IKDC >90 were younger than those <80. Higher self-reported knee function in younger athletes may contribute to the higher RTP rate and therefore the higher second ACL injury rate seen in younger athletes in the aforementioned outcomes. Injury to the medial compartment to either the meniscus or the medial femoral condyle was also different between groups, with those with medial meniscectomy or medial meniscal repair as well as those with grade 3–4 changes in medial femoral condyle more likely to have IKDC <80. This is in keeping with previous results where medial meniscal but not lateral meniscal tears at the time of surgery had a greater influence on IKDC score as well as grade 3–4 chondral changes.9 It may also reflect that ACL injury is often a precursor to the early-onset knee osteoarthritis.24 The prediction model selected age, sex, and sidestep injury mechanism as the key variables to predict IKDC >90, but the model demonstrated poor accuracy (59%; ROC, 0.63). Given the short-term follow-up, the influence of the intraoperative findings—particularly to the meniscus and chondral surfaces—may have a more pronounced influence on IKDC at later follow-up.
Limitations
There are a number of limitations to this study. First, only 2 surgeons who specialize in knee surgery carried out the large number of reconstructions, and this may reduce the generalizability of the results and the comparison with registries with larger numbers of contributing surgeons. There was a very high follow-up rate (95%) after 2 years, but there was a large spread in time to follow-up (24–55 months). This may have influenced the results, with potentially lower rates of both second ACL injury and RTP, less recall bias, and fewer differences in IKDC scores if follow-up had been completed over a shorter period around the 2-year mark. There was a larger number (80%) of BPTB grafts than HT grafts (20%), creating the potential for performance bias in favor of the more commonly used graft. However, the 2 surgeons carried out 290 HT grafts reconstructions over the 20-month period between them, which would be more than what most single-graft surgeons would complete in the same period and well in excess of the recommended 35 per year required to minimize the risk of future surgery on the same knee.34 A forward stepwise logistic regression model was used to assess the ability of pre- and intraoperative data on outcomes after 2 years. The use of nonlinear models may have enhanced the ability of those variables to predict outcomes, but given the low accuracy and AUC in the ROC for all outcomes, it is unlikely that there would be a major change in the interpretation of the results. Given the challenges in predicting outcome using pre- and intraoperative data alone, future research should examine the influence of other postoperative variables, such as biomechanical measures during RTP testing, as well as psychological and social factors, and should combine pre- and intraoperative data with biomechanical measures to improve predictive accuracy across outcomes.
CONCLUSION
This study prospectively reports across a range of outcomes, including RTP, second ACL injury, and IKDC, in a large cohort of athletes with 95% follow-up over 2 years after surgery. There were high levels of RTP to level 1 sports (81%) with low rerupture rates in those athletes with BPTB graft (1.9%), who had a lower reinjury risk every month than those who underwent HT ACLR. There were a number of differences in pre- and intraoperative data relating to each outcome, but these variables had poor ability to predict outcome after 2 years, suggesting that additional factors may influence these outcome.
Supplementary Material
Footnotes
Registration: NCT02771548 (ClinicalTrials.gov identifier).
The authors declared that they have no conflicts of interest in the authorship and publication of this contribution. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
For reprints and permission queries, please visit SAGE’s Web site at http://www.sagepub.com/journalsPermissions.nav.
REFERENCES
- 1.Anand BS, Feller JA, Richmond AK, Webster KE. Return-to-sport outcomes after revision anterior cruciate ligament reconstruction surgery. Am J Sports Med. 2016;44(3):580–584. [DOI] [PubMed] [Google Scholar]
- 2.Andernord D, Desai N, Bjornsson H, Ylander M, Karlsson J, Samuelsson K. Patient predictors of early revision surgery after anterior cruciate ligament reconstruction: a cohort study of 16,930 patients with 2-year follow-up. Am J Sports Med. 2015;43(1):121–127. [DOI] [PubMed] [Google Scholar]
- 3.Anderson AF, Irrgang JJ, Kocher MS, Mann BJ, Harrast JJ. The International Knee Documentation Committee Subjective Knee Evaluation Form: normative data. Am J Sports Med. 2006;34(1):128–135. [DOI] [PubMed] [Google Scholar]
- 4.Anderson MJ, Browning WM 3rd, Urband CE, Kluczynski MA, Bisson LJ. A systematic summary of systematic reviews on the topic of the anterior cruciate ligament. Orthop J Sports Med. 2016;4(3):2325967116634074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ardern CL, Taylor NF, Feller JA, Webster KE. Fifty-five per cent return to competitive sport following anterior cruciate ligament reconstruction surgery: an updated systematic review and meta-analysis including aspects of physical functioning and contextual factors. Br J Sports Med. 2014;48(21):1543–1552. [DOI] [PubMed] [Google Scholar]
- 6.Ardern CL, Webster KE, Taylor NF, Feller JA. Return to the preinjury level of competitive sport after anterior cruciate ligament reconstruction surgery: two-thirds of patients have not returned by 12 months after surgery. Am J Sports Med. 2011;39(3):538–543. [DOI] [PubMed] [Google Scholar]
- 7.Brophy RH, Schmitz L, Wright RW, et al. Return to play and future ACL injury risk after ACL reconstruction in soccer athletes from the Multicenter Orthopaedic Outcomes Network (MOON) group. Am J Sports Med. 2012;40(11):2517–2522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Claes S, Verdonk P, Forsyth R, Bellemans J. The “ligamentization” process in anterior cruciate ligament reconstruction: what happens to the human graft? A systematic review of the literature. Am J Sports Med. 2011;39(11):2476–2483. [DOI] [PubMed] [Google Scholar]
- 9.Cox CL, Huston LJ, Dunn WR, et al. Are articular cartilage lesions and meniscus tears predictive of IKDC, KOOS, and Marx activity level outcomes after anterior cruciate ligament reconstruction? A 6-year multicenter cohort study. Am J Sports Med. 2014;42(5):1058–1067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Crawford K, Briggs KK, Rodkey WG, Steadman JR. Reliability, validity, and responsiveness of the IKDC score for meniscus injuries of the knee. Arthroscopy. 2007;23(8):839–844. [DOI] [PubMed] [Google Scholar]
- 11.Czuppon S, Racette BA, Klein SE, Harris-Hayes M. Variables associated with return to sport following anterior cruciate ligament reconstruction: a systematic review. Br J Sports Med. 2014;48(5):356–364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dingenen B, Gokeler A. Optimization of the return-to-sport paradigm after anterior cruciate ligament reconstruction: a critical step back to move forward. Sports Med. 2017;47(8):1487–1500. [DOI] [PubMed] [Google Scholar]
- 13.Freedman KB, D’Amato MJ, Nedeff DD, Kaz A, Bach BR Jr. Arthroscopic anterior cruciate ligament reconstruction: a metaanalysis comparing patellar tendon and hamstring tendon autografts. Am J Sports Med. 2003;31(1):2–11. [DOI] [PubMed] [Google Scholar]
- 14.Greco NJ, Anderson AF, Mann BJ, et al. Responsiveness of the International Knee Documentation Committee Subjective Knee Form in comparison to the Western Ontario and McMaster Universities Osteoarthritis Index, modified Cincinnati Knee Rating System, and Short Form 36 in patients with focal articular cartilage defects. Am J Sports Med. 2010;38(5):891–902. [DOI] [PubMed] [Google Scholar]
- 15.Grindem H, Snyder-Mackler L, Moksnes H, Engebretsen L, Risberg MA. Simple decision rules can reduce reinjury risk by 84% after ACL reconstruction: the Delaware-Oslo ACL cohort study. Br J Sports Med. 2016;50(13):804–808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Irrgang JJ, Anderson AF, Boland AL, et al. Development and validation of the International Knee Documentation Committee Subjective Knee Form. Am J Sports Med. 2001;29(5):600–613. [DOI] [PubMed] [Google Scholar]
- 17.Janssen RP, Scheffler SU. Intra-articular remodelling of hamstring tendon grafts after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2014;22(9):2102–2108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kaeding CC, Pedroza AD, Reinke EK, Huston LJ, Spindler KP. Risk factors and predictors of subsequent ACL injury in either knee after ACL reconstruction: prospective analysis of 2488 primary ACL reconstructions from the MOON Cohort. Am J Sports Med. 2015;43(7):1583–1590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kyritsis P, Bahr R, Landreau P, Miladi R, Witvrouw E. Likelihood of ACL graft rupture: not meeting six clinical discharge criteria before return to sport is associated with a four times greater risk of rupture. Br J Sports Med. 2016;50(15):946–951. [DOI] [PubMed] [Google Scholar]
- 20.Lee DY, Karim SA, Chang HC. Return to sports after anterior cruciate ligament reconstruction—a review of patients with minimum 5-year follow-up. Ann Acad Med Singapore. 2008;37(4):273–278. [PubMed] [Google Scholar]
- 21.Lefevre N, Klouche S, Mirouse G, Herman S, Gerometta A, Bohu Y. Return to sport after primary and revision anterior cruciate ligament reconstruction: a prospective comparative study of 552 patients from the FAST Cohort. Am J Sports Med. 2017;45(1):34–41. [DOI] [PubMed] [Google Scholar]
- 22.Lynch AD, Logerstedt DS, Grindem H, et al. Consensus criteria for defining “successful outcome” after ACL injury and reconstruction: a Delaware-Oslo ACL cohort investigation. Br J Sports Med. 2015;49(5):335–342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Magnussen RA, Carey JL, Spindler KP. Does autograft choice determine intermediate-term outcome of ACL reconstruction? Knee Surg Sports Traumatol Arthrosc. 2011;19(3):462–472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Magnussen RA, Spindler KP. The effect of patient and injury factors on long-term outcome after anterior cruciate ligament reconstruction. Curr Orthop Pract. 2011;22(1):90–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Montalvo AM, Schneider DK, Yut L, et al. “What’s my risk of sustaining an ACL injury while playing sports?” A systematic review with meta-analysis. Br J Sports Med. 2019;53(16):1003–1012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Moran CJ, Verdonk PC, Lagae K, DeClercq G. Anterior Cruciate Ligament Reconstruction. Berlin, Heidelberg: Springer; 2014. [Google Scholar]
- 27.Myklebust G, Bahr R. Return to play guidelines after anterior cruciate ligament surgery. Br J Sports Med. 2005;39(3):127–131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nagelli CV, Hewett TE. Should return to sport be delayed until 2 years after anterior cruciate ligament reconstruction? Biological and functional considerations. Sports Med. 2017;47(2):221–232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Paterno MV, Huang B, Thomas S, Hewett TE, Schmitt LC. Clinical factors that predict a second ACL injury after ACL reconstruction and return to sport: preliminary development of a clinical decision algorithm. Orthop J Sports Med. 2017;5(12):2325967117745279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Paterno MV, Schmitt LC, Ford KR, et al. Biomechanical measures during landing and postural stability predict second anterior cruciate ligament injury after anterior cruciate ligament reconstruction and return to sport. Am J Sports Med. 2010;38(10):1968–1978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pauzenberger L, Syre S, Schurz M. “Ligamentization” in hamstring tendon grafts after anterior cruciate ligament reconstruction: a systematic review of the literature and a glimpse into the future. Arthroscopy. 2013;29(10):1712–1721. [DOI] [PubMed] [Google Scholar]
- 32.Petersen W, Taheri P, Forkel P, Zantop T. Return to play following ACL reconstruction: a systematic review about strength deficits. Arch Orthop Trauma Surg. 2014;134(10):1417–1428. [DOI] [PubMed] [Google Scholar]
- 33.Pietrosimone B, Lepley AS, Harkey MS, et al. Quadriceps strength predicts self-reported function post-ACL reconstruction. Med Sci Sports Exerc. 2016;48(9):1671–1677. [DOI] [PubMed] [Google Scholar]
- 34.Schairer WW, Marx RG, Dempsey B, Ge Y, Lyman S. The relation between volume of ACL reconstruction and future knee surgery. Orthop J Sports Med. 2017;5(7)(suppl 6):2325967117S2325900298. [Google Scholar]
- 35.Schmitt LC, Paterno MV, Hewett TE. The impact of quadriceps femoris strength asymmetry on functional performance at return to sport following anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 2012;42(9):750–759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Spindler KP, Kuhn JE, Freedman KB, Matthews CE, Dittus RS, Harrell FE Jr. Anterior cruciate ligament reconstruction autograft choice: bone-tendon-bone versus hamstring: does it really matter? A systematic review. Am J Sports Med. 2004;32(8):1986–1995. [DOI] [PubMed] [Google Scholar]
- 37.Svantesson E, Hamrin Senorski E, Baldari A, et al. Factors associated with additional anterior cruciate ligament reconstruction and register comparison: a systematic review on the Scandinavian knee ligament registers. Br J Sports Med. 2019;53(7):418–442. [DOI] [PubMed] [Google Scholar]
- 38.Sward P, Kostogiannis I, Roos H. Risk factors for a contralateral anterior cruciate ligament injury. Knee Surg Sports Traumatol Arthrosc. 2010;18(3):277–291. [DOI] [PubMed] [Google Scholar]
- 39.Webster KE, Feller JA. Exploring the high reinjury rate in younger patients undergoing anterior cruciate ligament reconstruction. Am J Sports Med. 2016;44(11):2827–2832. [DOI] [PubMed] [Google Scholar]
- 40.Wiggins AJ, Grandhi RK, Schneider DK, Stanfield D, Webster KE, Myer GD. Risk of secondary injury in younger athletes after anterior cruciate ligament reconstruction: a systematic review and meta-analysis. Am J Sports Med. 2016;44(7):1861–1876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wright RW, Magnussen RA, Dunn WR, Spindler KP. Ipsilateral graft and contralateral ACL rupture at five years or more following ACL reconstruction: a systematic review. J Bone Joint Surg Am. 2011;93(12):1159–1165. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


