Abstract
Background
Hypertension is a serious threat to public health globally owing to its high prevalence and related complications. It is the main risk factor for cardiovascular disease, kidney disease, eye problems, and death. Self-care practices have been emphasized as a major element in reducing and preventing complications from hypertension. Thus, this study aimed to assess hypertension self-care practices and associated factors in Bale Zone, Southeast Ethiopia.
Methods
A health facility-based cross-sectional study was conducted at three public hospitals from April 1 to May 31, 2021. Data were entered into Epi-Data version 4.6 and exported to Statistical Package for the Social Sciences (SPSS) version 25.0 for analysis. The study participants were characterized using descriptive statistics. The associations between self-care practice and independent variables were modeled using binary logistic regression analysis. Adjusted odds ratios with a 95% confidence interval were used to estimate the association between self-care practice and independent variables. The statistical significance of the association was declared at p < 0.05.
Results
This study involved 405 hypertensive patients, with a response rate of 96.7%. The overall level of good self-care practice was 33.1% (95% CI: 28.6, 37.5). The multivariable logistic regression model showed that age under 65 years (AOR = 3.77, 95% CI: 1.60–8.89), good knowledge of hypertension self-care practice (AOR = 6.36, 95% CI: 2.07–19.56), absence of a depression (AOR = 6.08, 95% CI: 1.24–29.73) and good self-efficacy (AOR = 3.33, 95% CI: 1.12–9.87) were independent predictors of good self-care practice.
Conclusion
The level of good hypertension self-care practice in the study area was low. Hence, it is crucial to expand non-communicable disease control programs and implement public health interventions on self-care for hypertension. Moreover, to enhance hypertension self-care practices, patient-centered interventions are essential.
Keywords: Self-care, Hypertension, Blood pressure control, Bale Zone
Introduction
Hypertension is a significant public health challenge in both developed and developing countries because of its high prevalence and associated complications [1–3]. Systolic blood pressure exceeding 140 mmHg or diastolic blood pressure higher than 90 mmHg as determined by at least two distinct readings taken at different times, or 130/85 mmHg at home, is considered to be hypertension [4]. Nearly a billion people worldwide suffer from hypertension, with two-thirds of those individuals residing in low-income countries [5]. It is also the primary global preventable cause of premature death and disability [3, 6].
One-third of adults worldwide have hypertension, and by 2025, that number is estimated to rise to 1.56 billion adults worldwide, with more than 125 million of those individuals living in sub-Saharan Africa [7–9]. A systematic review and meta-analysis conducted in 2020 estimated that the prevalence of hypertension in Ethiopia is predicted to reach 21.81 percent [10].
Hypertension is the main risk factor for cardiovascular disease, kidney disease, eye problems, and death [5, 11, 12]. Uncontrolled hypertension can result in heart attack, heart failure, and stroke, as well as renal failure, blindness, blood vessel rupture, and cognitive impairment [13]. It contributes to 10.4 million deaths worldwide each year [14]. About 45% of deaths from heart disease and 51% of deaths from stroke are attributable to hypertension [15]. The World Health Organization (WHO) estimates that hypertension complications account for 9.4 million annual deaths, accounting for 17% of all cardiovascular disease-related deaths worldwide[6].
The actual cause of hypertension is uncertain, but research shows that risk can be increased by modifying factors like heavy alcohol use, lack of physical activity, high salt intake, smoking, and a higher body mass index, and avoiding these factors is an essential aspect of self-care practice [6, 9, 16]. Self-care practices are an important and cost-effective non-pharmacologic tool for regulating blood pressure, preventing and minimizing complications, and reducing the ensuing morbidity, disability, and death [17–19]. Taking drugs as prescribed, following a low-salt diet, limiting alcohol use, exercising regularly, managing a healthy weight, avoiding smoking, monitoring blood pressure, lowering stress, and having routine health checkups are all part of self-care practices [4, 20].
Patients must follow self-management protocols for hypertension to meet treatment objectives by raising the quality of life, preventing complications, and spending less on medical care [21–23]. Patients need to start self-care practices before commencing their prescribed medications, as well as continue doing so afterward. Yet, self-care practices are still low in developing countries like Ethiopia [2, 17].
According to previous studies various factors, including sex, age, educational status, place of residence, occupational status, socioeconomic status, time since diagnosis, comorbidity, source of information about self-care and knowledge of disease and treatment, self-efficacy, social support are all associated with components of hypertension self-care practice [24–29].
Although there are few studies on self-care practices among hypertensive patients in Ethiopia, there is no evidence regarding hypertension self-care practices and associated in the study area. Due to this, it was determined that assessing self-care practices and associated factors might help in designing programs and developing strategies for efficient health education and patient empowerment as well as helping close knowledge gaps. Therefore, this study aimed to assess the level of self-care practices and associated factors among hypertensive patients in Bale Zone, Southeastern Ethiopia.
Specific objectives
To determine the level of hypertension self-care practices among adult hypertensive patients in public hospitals of Bale zone in 2021.
To identify factors associated with hypertension self-care practices.
Methods and materials
Study design, setting, and period
An institutional-based cross-sectional study was conducted in the Bale Zone, Southeastern Ethiopia from April 1 to May 31, 2021. The Bale Zone is the second largest of the 20 zones in the Oromia Regional State, located 430 km from Addis Ababa, the capital city of Ethiopia. According to the Central Statistical Agency's 2007 population census, the zone's total population is estimated to be 1,402,492, with 688,975 females. The zone has five hospitals, 82 health centers, and 381 health posts. The current study was conducted in three public hospitals, namely Madda Walabu University Goba Referral Hospital (MWU GRH), Bale Robe General Hospital (BRGH), and Dello Menna General Hospital (DMGH).
Study population and eligibility criteria
The study population consisted of all adult hypertensive patients on follow-up care at the selected public hospitals during the study period and those who met the inclusion criteria. The study included hypertensive patients aged 18 and older who had been on follow-up care for at least 6 months, based on diagnosis codes in the patient hospital records. Patients with cognitive impairment and those who were critically ill during the data collection period were excluded from the study.
Sample size determination and sampling procedure
The sample size was calculated using a single population proportion formula assuming: Zα/2 = 1.96, 95% confidence level, a margin of error (d = 0.045), and a proportion of good self-care practice (p = 0.299) from a previous study conducted in Harar [30]. By considering a 5% nonresponse rate, the final total sample size becomes 419.
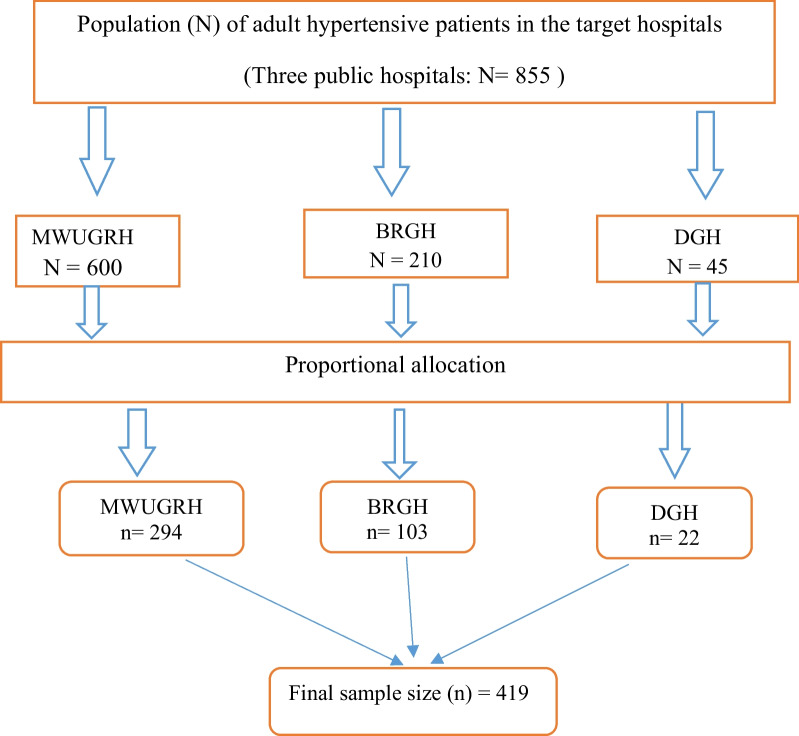
The calculated sample size was proportionally allotted to the selected hospitals based on their preceding 3 months’ average client flow for hypertension follow-up during the study period. Accordingly, there were expected to be 855 hypertensive patients across the three hospitals during the study period (i.e., 600 in MWU GRH, 210 in BRGH, and 45 in DMGH) and the calculated sample size was distributed in accordance with this (Fig. 1). To determine the required number of participants from each hospital, we calculated the k-value by dividing the total number of hypertensive patients in the three hospitals by the calculated sample size. Thus, the calculated k-value becomes two. The index participant was then chosen at random from 1 to 2 in each hospital. Accordingly, every second participant was chosen using a systematic random sampling technique until the required sample size was reached.
Fig. 1 .
Schematic presentation of sampling technique used to select the study subjects from public hospitals in Bale Zone, Southeast Ethiopia, 2021
Data collection tools and procedures
For data collection, an interviewer-administered structured questionnaire that had been pretested and verified was used. The questionnaires were adapted from validated scales, and published articles [26, 28, 30–37], and were amended for the context of the study. The questionnaire contains socio-demographic characteristics, clinical profiles of the patients, knowledge about hypertension and self-care practice, and psychosocial related factors (depression, self-efficacy, and social support). Six trained nurses, who are Bachelor of Science degree holders, supervised by three Masters of Science degree holder nurses collected the data.
Study variables
Dependent variable
Good self-care practices
Independent variables
Socio-demographic variables: age, sex, marital status, occupation, place of residence, educational level, and monthly income. Clinical factors: duration of the disease, comorbidity, family history of hypertension, follow-up miss, and body mass index (BMI). Knowledge of hypertension and self-care. Psychosocial factors: social support, depression, and self-efficacy.
Study measurements
Self-care practice
Self-care practice was measured using the hypertensive self-care activity level effect (H-SCALE) [32]. The scale is divided into six domains (medication adherence, weight management, physical activity, smoking, low-salt diet, and alcohol consumption). When patients scored average or higher on the H-SCALE questions, they were regarded as having good self-care practices.
Medication adherence:
Three items containing the number of days in the last 7 days assessed medication adherence. The responses were summed (range: 0–21), and the participants who reported that they had followed these three recommendations on all weekdays were considered adherents (score = 21)[32, 38].
Weight management
Weight management was assessed using 10 items based on a 5-point Likert scale ranging from 1 (strongly disagree) to 5(strongly agree) with a sum ranging from 10 to 50. Patients who received 40 out of 50 total points were considered to be good weight management practice adherents [32].
Physical activity
Two items were used to assess physical activity. The responses were then added up (range: 0–14). Participants were deemed physically active if they had a score of eight or higher [32].
Smoking
Smoking was assessed by one item whether the patients smoked or even a puff in the last 7 days. Patients were classified as nonsmokers if they had not smoked or had not taken even one puff in the last 7 days [32].
Low-salt diet
Twelve items were used to measure the low-salt diet. After the mean was calculated, a patient is considered adherent to the low-salt diet if they scored ≥ 6(indicating the participant followed low-salt diet practice on 6 out of 7 days) [32].
Alcohol consumption
Three items were used to assess alcohol intake. When patients did not drink alcohol at all, they were regarded as abstainers [32, 39].
Knowledge
The Hypertension Evaluation of Lifestyle and Management (HELM) scale was used to assess knowledge of hypertension. Patients were deemed to have adequate or good knowledge if their scores were at or above the mean [34].
Self-efficacy
Self-efficacy was assessed using the Self-Efficacy to Manage Chronic Disease Scale (SEMCD). The SEMCD is a set of six measures ranging from 1 (not at all confident) to 10 (totally confident). If the patient responds to self-efficacy questions above the mean of six items, he/she was regarded as having good self-efficacy [36].
Depression
Depression was screened using the patient health questionnaire-9 (PHQ-9). The PHQ-9 scale goes from 0 (not at all) to 3 (nearly every day) The total number of points ranges from 0 to 27 and if the participant scores ≥ 10, he/she were considered to have depression [37].
Social support
Social support was measured by the Oslo Social Support Scale (OSSS-3) containing three items: A four-point Likert scale with a range of 1 to 4 is used to rate the first item. Ratings for the second and third items are given on a five-point Likert scale with a range of 1 to 5. The total range of scores is between 3 and 14. Poor support was defined as 3 to 8, moderate support as 9 to 11, and strong support as 12 or higher [35].
Data quality management
To assure the quality of the data, data collectors and supervisors were trained for 2 days on research ethics, data collection tools, and procedures. The questionnaire was first prepared in English and then translated into Afan Oromo and back to English to ensure consistency. We pretested the questionnaire on 5% of the total sample (21 hypertensive patients on follow-up) in Ginner Hospital to check for its validity likewise, we adjusted and rearranged some of the questions to ensure clarity, ease of understanding, and cohesion. Investigators and supervisors strictly supervised the data collection process.
Data processing and analysis
The collected data were coded, cleaned, and reviewed for completeness to reduce data entry errors. The data were then entered into Epi-Data version 4.6 before being exported to the Statistical Package for the Social Sciences (SPSS) version 25.0 for analysis. The normality assumptions were checked to assess the distribution of continuous variables and choose the ideal summary measure. Descriptive statistics were done using frequency, percentage, mean, and standard deviation. Before regression analysis was conducted data were checked for multi-collinearity, normality, linearity, independence of residuals, and outliers, and no significant violations of the regression analysis's assumptions were identified. A bi-variable logistic regression model was used to identify those variables having a p-value of < 0.25 to be considered as potential candidate variables for multivariable logistic regression to control confounders. Hosmer and Lemeshow’s goodness-of-fit test was used to check the model adequacy, considering good fit at a p-value ≥ 0.05. Afterward, a multivariable logistic regression analysis was performed to identify factors associated with good self-care practices. Adjusted odds ratios (AOR) with a 95% confidence interval were used to report the results. Statistical significance was deemed at a p-value of < 0.05.
Result
Socio-demographic characteristics of participants
A total of 405 hypertensive patients participated in the study, with a response rate of 96.7%. Of the total participants, 237(51.9%) were males and 212 (52.3%) reside in an urban area. The mean age of the participants was 53 (SD: ± 4.31) years. About 309(76.3%) of them were married, and 141 (34.8%) attended college and above (Table 1).
Table 1.
Socio-demographic characteristics of hypertensive patients in public hospitals of Bale Zone, Southeast Ethiopia, 2021 (n = 405)
| Variables | Category | Frequency | Percentage |
|---|---|---|---|
| Sex | Male | 237 | 58.5 |
| Female | 168 | 41.5 | |
| Age (years) | < 65 | 243 | 60.0 |
| ≥ 65 | 162 | 40.0 | |
| Residence area | Urban | 193 | 47.7 |
| Rural | 212 | 52.3 | |
| Marital status | Single | 66 | 16.3 |
| Married | 288 | 71.1 | |
| Divorced | 28 | 6.9 | |
| Widowed | 23 | 5.7 | |
| Occupational status | Student | 51 | 12.6 |
| Self-employed | 148 | 36.5 | |
| Employed | 136 | 33.6 | |
| Unemployed | 24 | 5.9 | |
| Housewife | 46 | 11.4 | |
| Educational status | Unable to read and write | 92 | 22.7 |
| Able to read and write | 81 | 20.0 | |
| Primary school | 53 | 13.1 | |
| Secondary school | 38 | 9.4 | |
| College and above | 141 | 34.8 | |
| Monthly income | < 2500 ETB | 64 | 15.8 |
| 2500–3500 ETB | 70 | 17.3 | |
| > 3500 ETB | 271 | 66.9 |
ETB Ethiopian Birr
Clinical, therapeutic life change, and self-care practice-related characteristics of participants
In this study, 93 (23%) of the participants had medically confirmed other comorbid diseases, 92 (22.7%) had a family history of hypertension, and 193(47.7%) had a normal body mass index. In terms of the duration of hypertension diagnosis, 239 (59%) of participants were diagnosed less than 5 years ago and 209(51.6%) had a history of missed follow-up. About 254 (62.7%) of the participants had good knowledge about self-care practices for hypertension and 202(49.9%) of them got information about self-care practice from a healthcare professional. Among the participants, 168 (41.5%) had good self-efficacy, 102 (25.2%) had depression, and 148 (36.5%) had strong social support (Table2).
Table 2.
Clinical, therapeutic life change and self-care practice-related characteristics of participants in public hospitals of Bale Zone, Southeast Ethiopia, 2021 (n = 405)
| Variables | Category | Frequency | Percentage |
|---|---|---|---|
| Comorbidity | Yes | 93 | 23.0 |
| No | 312 | 77.0 | |
| Family history of hypertension | Yes | 92 | 22.7 |
| No | 313 | 77.3 | |
| Body mass index (k/m2) | Underweight (< 18.5) | 49 | 12.1 |
| Normal (18.5–24.9) | 193 | 47.7 | |
| Overweight (25–29.9) | 101 | 24.9 | |
| Obese (≥ 30) | 62 | 15.3 | |
| Duration of hypertension diagnosis (years) | < 5 | 239 | 59.0 |
| ≥ 5 | 166 | 41.0 | |
| Follow-up miss | Yes | 209 | 51.6 |
| No | 196 | 48.4 | |
| Hypertension self-care knowledge and practice | Poor | 254 | 62.7 |
| Good | 151 | 37.3 | |
| Source of information about self-care practice | Family Members | 163 | 40.2 |
| Health professionals | 202 | 49.9 | |
| Mass Media | 40 | 9.9 | |
| Level of social support | Strong | 148 | 36.5 |
| Moderate | 25 | 6.2 | |
| Low | 232 | 57.3 | |
| Level of self-efficacy | Good | 168 | 41.5 |
| Poor | 237 | 58.5 | |
| Depression | Yes | 102 | 25.2 |
| No | 330 | 74.8 |
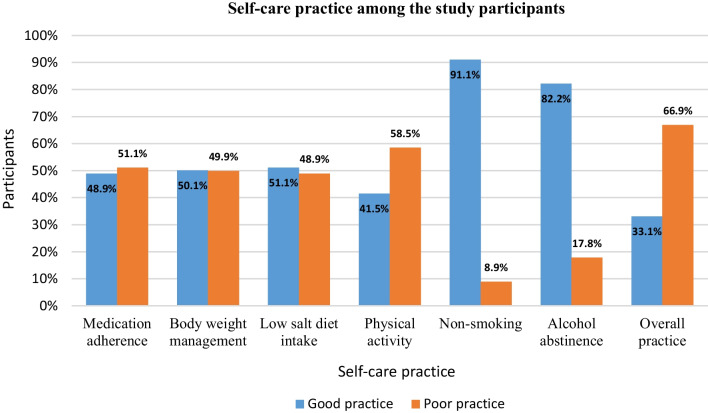
Hypertension self-care practices
The overall level of good self-care practice was 33.1% (95% CI: 28.6, 37.5), determined from the six domains of self-care practice. About 198 (48.9%) of patients had good antihypertensive medication adherence; 203 (50.1%) were good weight management practitioners; 207 (51.1%) practiced a low-salt diet intake, 168 (41.5%) were good practitioners of the recommended level of physical activity; and 369 (91.1%) and 333 (82.2%) were nonsmokers and alcohol abstainers, respectively (Fig. 2).
Fig. 2.
Hypertension self-care practices of the participants in public hospitals of Bale Zone, South East Ethiopia, 2021 (n = 405)
Factors associated with hypertension self-care practice
Both bivariate and multivariate analyses were performed to examine the association between independent variables and good self-care practice. Those variables in the bivariate analysis that showed an association with the outcome variable were chosen as candidate variables for multivariable logistic regression analysis at a p-value < 0.25.
As a result, in the bivariate analysis, sex, age, place of residence, duration of hypertension diagnosis, knowledge of hypertension self-care practice, depression, self-efficacy, and level of social support were significantly associated with good self-care practice. After adjusting for potential confounding variables using multivariable binary logistic regression analysis, age, knowledge of hypertension self-care practice, depression, and self-efficacy were independent predictors of good self-care practice at a p-value < 0.05.
In this study, the odds of having good self-care practice were 3.77 times higher among patients aged younger than 65 years compared with patients who were 65 and olde r(AOR = 3.77, 95% CI: 1.60–8.89). Hypertensive patients with good self-efficacy had 3.33 times greater odds of practicing good self-care practice than those who had poor self-efficacy (AOR = 3.33, 95% CI: 1.12–9.87). The odds of having good self-care among patients with good knowledge of hypertension self-care practice were 6.36 times higher than those with poor knowledge of hypertension self-care practice (AOR = 6.36, 95% CI: 2.07–19.56). Moreover, patients without depression had 6.08 greater odds of having good hypertension self-care practices than patients with depression (AOR = 6.08, 95% CI: 1.24–29.73) (Table 3).
Table 3.
Factors associated with self-care practices of hypertensive patients in public hospitals of Bale Zone Public hospitals, Southeast Ethiopia, 2021 (n = 405)
| List of variables | Self-care practice | COR (95% CI) | AOR (95% CI) | |
|---|---|---|---|---|
| Good (%) | Poor (%) | |||
| Sex | ||||
| Male | 95 (40.1) | 142 (59.9) | 1.00 | |
| Female | 39 (23.2) | 129 (76.8) | 2.21 (1.42–3.44)* | |
| Age (years) | ||||
| < 65 | 105 (78.4) | 138 (50.9) | 3.49 (2.17–5.61)* | 3.77(1.60–8.89)** |
| ≥ 65 | 29 (21.6) | 133 (49.1) | 1.00 | 1.00 |
| Residence area | ||||
| Urban | 91 (67.9) | 102 (37.6) | 3.50 (2.26–5.43)* | |
| Rural | 43 (32.1) | 169 (62.4) | 1.00 | |
| Duration of HTN diagnosis (years) | ||||
| < 5 | 96 (71.6) | 143 (52.8) | 2.26 (1.44–3.52)* | |
| ≥5 | 38 (28.4) | 128 (47.2) | 1.00 | |
| Knowledge of HTN Self-care practice | ||||
| Good | 100 (74.6) | 51 (18.8) | 12.68 (7.74–20.79)* | 6.36(2.07–19.56)** |
| Poor | 34 (25.4) | 220 (81.2) | 1.00 | 1.00 |
| Depression | ||||
| No | 113 (84.3) | 190 (70.1) | 2.29 (1.34–3.94)* | 6.08(1.24–29.73)** |
| Yes | 21 (15.7) | 81 (29.9) | 1.00 | 1.00 |
| Self-efficacy | ||||
| Good | 105 (78.4) | 63 (23.2) | 11.95 (7.26–19.67)* | 3.33(1.12–9.87)** |
| Poor | 29 (21.6) | 208 (76.8) | 1.00 | 1.00 |
| Level of social support | ||||
| Low | 35 (26.1) | 197 (72.7) | 1.00 | |
| Moderate | 15 (11.2) | 10 (3.7) | 2.69 (2.12–3.42)* | |
| Strong | 84 (62.7) | 64 (23.6) | 1.13 (1.48–2.71)* | |
COR crude odds ratio, CI confidence interval, AOR adjusted odds ratio, HTN hypertension. *Significant at p-value < 0.25 in unadjusted logistic regression analysis, **Significant at p < 0.05 in adjusted logistic regression analysis, 1.00 = Reference
Discussion
Self-care is an important non-pharmacological technique that helps to control blood pressure and is beneficial for the treatment and prevention of hypertension. This study assessed self-care practices and associated factors among hypertensive patients in public hospitals in southeastern Ethiopia.
The findings of this study showed that 33.1% (95% CI: 28.6, 37.5) of patients practiced good self-care. Based on the findings of this study around one in three hypertensive patients practiced good self-care practice as advised by the hypertension management protocol. This finding is in line with studies conducted in Harar (29.9%) [30], and West Bengal (37.1%) [40]. This finding was higher than that of studies done in Mekele (20.3%) [41], South Ethiopia (24%) [22], and Debre Berhan (24%) [42]. On the contrary, this finding was lower than studies conducted in Nekemte (68.92%), Gondar (59.4%), Debre Tabor (54.1%) [25], Harar (62.1%) [43] Addis Ababa (51%) [44], Dessie (49%) [26], Saudi Arabia (74.4%) [24] and South India (60.6%) [45]. This inconsistency could be explained by variations in sample size, socioeconomic and cultural differences, levels of understanding of hypertension and its management, differences in the methods and tools used to gather the data, and the methodological disparities between studies. For instance, the WHO STEPwise approach risk factor for non-communicable disease surveillance (STEPS) was used in a Harar study. The Dessie study made use of a tool for practicing hypertension self-care that had 20 items and rated out of four points on a Likert-type scale for each. Moreover, the South Ethiopia study investigated self-care practices using just lifestyle-related characteristics, disregarding medication adherence.
This study showed that the odds of having good self-care practice were 3.77 times higher among younger adults (i.e., patients aged less than 65 years) compared with older adults (i.e., patients who were 65 years and above). This result is supported by studies conducted in India [46], Mekelle [41], Jimma [47], DebreTabor[25], and South, Ethiopia [22]. The possible reason could be the younger the patient, the more likely they are to be educated and driven to exercise good self-care practices and this might also be due to older people's diminishing cognitive function, increased comorbid conditions, and other factors that may make it challenging for them to maintain their lives. This finding, however, contradicts the findings of a study done in Israel [48], Harar [30], Dessie [26], and Addis Ababa [31], which revealed that younger patients were less likely to practice good self-care. This might be due to sample size and participant age categorization variations between the studies.
This study indicated that the odds of practicing good self-care were 3.33 times greater than those with good self-efficacy compared with those who had poor self-efficacy. This result is similar to the findings of a systematic review that reported higher self-efficacy being associated with engagement in self-care behaviors [49]. Studies conducted at the University of North Carolina [33] and Saudi Arabia [50] also showed that Self-efficacy is a strong predictor of good self-care practices. This might be the reason that patients with self-efficacy are aware that their condition is manageable and are confident in dealing with their illness, which enables them to engage in effective self-care practices.
Depression was another significant factor associated with good self-care practices. In this study, patients without depression had sixfold greater odds of having good hypertension self-care practices than patients with depression. This finding is consistent with a study conducted in Deagu, Korea [51]. This might be due to the reason that cognitive side effect of depression that impedes the ability to concentrate and retain appropriate self-care practices.
This study ascertained that patients with good knowledge of hypertension self-care practice were 6.36 times more likely to practice good self-care than those with poor knowledge. This finding is in agreement with studies done in Saudi Arabia [24], Iran [52] Addis Ababa [31], Mekele [41], Debre Tabor [25], and Harar [30]. A study conducted in Debre Brehan also revealed that patients with poor knowledge of hypertension self-care practices were 2.6 times more likely to have poor self-care practices [42]. The justification could be that well-informed patients are aware of their condition, its management, potential complications, and control methods. Patients who are aware of hypertension and its treatment also give self-care practices more heed.
Limitations of the study
Since the study participants' self-care practices have relied on self-reports, there may be a recall and social desirability bias.
Conclusion
The study found that the level of good hypertension self-care practice in the study area was low. Age under 65 years, good knowledge of hypertension self-care practice, absence of depression, and good self-efficacy were independent predictors of good self-care practice. Continuous monitoring and follow-up of patient's adherence to the self-management protocol are required, with a greater focus on identifying factors that may hamper patients' adherence to the hypertension self-care protocols. To accomplish this, policymakers should consider these aspects when developing public health initiatives on hypertension self-care and when bolstering ongoing non-communicable disease reduction programs. Moreover, public health facilities should increase their efforts to give patients and families specialized instruction on all components of self-care practice.
Acknowledgements
The authors would like to express their gratitude to data collectors, supervisors, and all the study participants for their cooperation
Abbreviations
- AOR
Adjusted odds ratio
- BRGH
Bale Robe General Hospital
- COR
Crude odds ratio
- CI
Confidence interval
- DMGH
Dello Menna General Hospital
- ETB
Ethiopian Birr
- HTN
Hypertension
- HELM
Hypertension Evaluation of Lifestyle and Management
- H-SCALE
Hypertension-related Self-Care Activity Level
- MSPSS
Multidimensional Perceived Social Support Scale
- MWU GRH
Madda Walabu University Goba Referral Hospital
- SPSS
Statistical Package for Social Science
Author contributions
DAT, TAT, and AMG worked on the conception and design of the study, training and supervising the data collectors, data analysis, and interpretation of the data. YMN redid the statistical analysis and drafted the manuscript. YMN, MSG, and AMG critically reviewed the draft manuscript and wrote the final version. All authors read and approved the final manuscript.
Funding
This study received no specific grant from any funding agency.
Availability of data and materials
All data and materials are available from the corresponding author without undue reservation.
Declarations
Ethics approval and consent to participate
Ethical clearance was obtained from the Institutional Review Board (IRB) of Madda Walabu University College of Medical and Health Sciences. Then, an official permission letter and support were provided to the respective hospitals before data collection. The objective and benefits of the study were described to the participants during the data collection period and informed written consent was obtained to assure their choice of participation or refusal. Anonymity and privacy safeguards were used throughout the research process to protect respondents' rights and maintain confidentiality. The study's procedures were all conducted in line with the principles of the Helsinki Declaration [53].
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Saha A, Alleyne G. Recognizing noncommunicable diseases as a global health security threat. Bull World Health Organ. 2018;96(11):792–793. doi: 10.2471/BLT.17.205732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mills KT, Bundy JD, Kelly TN, Reed JE, Kearney PM, Reynolds K, et al. Global disparities of hypertension prevalence and control: a systematic analysis of population-based studies from 90 countries. Circulation. 2016;134(6):441–450. doi: 10.1161/CIRCULATIONAHA.115.018912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2224–2260. doi: 10.1016/S0140-6736(12)61766-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Unger T, Borghi C, Charchar F, Khan NA, Poulter NR, Prabhakaran D, et al. 2020 international society of hypertension global hypertension practice guidelines. Hypertension. 2020;75(6):1334–1357. doi: 10.1161/HYPERTENSIONAHA.120.15026. [DOI] [PubMed] [Google Scholar]
- 5.Kaptoge S, Pennells L, De Bacquer D, Cooney MT, Kavousi M, Stevens G, et al. World Health Organization cardiovascular disease risk charts: revised models to estimate risk in 21 global regions. Lancet Glob Health. 2019;7(10):e1332–e1345. doi: 10.1016/S2214-109X(19)30318-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.World Health Organization . A global brief on hypertension: silent killer, global public health crisis: World Health Day 2013. Geneva: World Health Organization; 2013. [Google Scholar]
- 7.Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J. Global burden of hypertension: analysis of worldwide data. Lancet. 2005;365(9455):217–223. doi: 10.1016/S0140-6736(05)17741-1. [DOI] [PubMed] [Google Scholar]
- 8.Guwatudde D, Nankya-Mutyoba J, Kalyesubula R, Laurence C, Adebamowo C, Ajayi I, et al. The burden of hypertension in sub-Saharan Africa: a four-country cross-sectional study. BMC Public Health. 2015;15(1):1211. doi: 10.1186/s12889-015-2546-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ogah OS, Rayner BL. Recent advances in hypertension in sub-Saharan Africa. Heart. 2013;99(19):1390–1397. doi: 10.1136/heartjnl-2012-303227. [DOI] [PubMed] [Google Scholar]
- 10.Tiruneh SA, Bukayaw YA, Yigizaw ST, Angaw DA. Prevalence of hypertension and its determinants in Ethiopia:a systematic review and meta-analysis. Widmer RJ, editor. PLoS ONE. 2020;15(12):e0244642. doi: 10.1371/journal.pone.0244642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fraser-Bell S, Symes R, Vaze A. Hypertensive eye disease: a review: hypertensive eye disease: review. Clin Experiment Ophthalmol. 2017;45(1):45–53. doi: 10.1111/ceo.12905. [DOI] [PubMed] [Google Scholar]
- 12.Chia YC, Ching SM. Prevalence and predictors of resistant hypertension in a primary care setting: a cross-sectional study. BMC Fam Pract. 2014;15(1):131. doi: 10.1186/1471-2296-15-131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dorans KS, Mills KT, Liu Y, He J. Trends in prevalence and control of hypertension according to the 2017 American College of Cardiology/American Heart Association (ACC/AHA) Guideline. J Am Heart Assoc. 2018;7(11):e008888. doi: 10.1161/JAHA.118.008888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Stanaway JD, Afshin A, Gakidou E, Lim SS, Abate D, Abate KH, et al. Global, regional, and national comparative risk assessment of 84 behavioral, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. The Lancet. 2018;392(10159):1923–1994. doi: 10.1016/S0140-6736(18)32225-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Arguedas JA, Perez MI, Wright JM. Treatment blood pressure targets for hypertension. Cochrane Database Syst Rev. 2009 doi: 10.1002/14651858.CD004349.pub2. [DOI] [PubMed] [Google Scholar]
- 16.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, et al. The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: the JNC 7 report. JAMA. 2003;289(19):2560–2572. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 17.Amsterdam EA, Venugopal S, Bui J, Thevakumar B, Thinda A, Virk S, et al. Management of Hypertension: JNC 8 and Beyond. Cardiovasc Innov App. 2016;1(4):409–416. [Google Scholar]
- 18.Williams B, Mancia G, Spiering W, AgabitiRosei E, Azizi M, Burnier M, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur Heart J. 2018;39(33):3021–3104. doi: 10.1093/eurheartj/ehy339. [DOI] [PubMed] [Google Scholar]
- 19.Weber MA, Schiffrin EL, White WB, Mann S, Lindholm LH, Kenerson JG, et al. Clinical practice guidelines for the management of hypertension in the community: a statement by the American Society of Hypertension and the International Society of Hypertension. J Clin Hypertens (Greenwich) 2014;16(1):14–26. doi: 10.1111/jch.12237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ike SO, Aniebue PN, Aniebue UU. Knowledge, perceptions, and practices of lifestyle-modification measures among adult hypertensives in Nigeria. Trans R Soc Trop Med Hyg. 2010;104(1):55–60. doi: 10.1016/j.trstmh.2009.07.029. [DOI] [PubMed] [Google Scholar]
- 21.Akhter N. Self-management among patients with hypertension in Bangladesh. Thailand: Prince of Songkla University; 2010. [Google Scholar]
- 22.Buda ES, Hanfore LK, Fite RO, Buda AS. Lifestyle modification practice and associated factors among diagnosed hypertensive patients in selected hospitals, South Ethiopia. Clin Hypertens. 2017;23:26. doi: 10.1186/s40885-017-0081-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bodenheimer T, Lorig K, Holman H, Grumbach K. Patient self-management of chronic disease in primary care. JAMA. 2002;288(19):2469–2475. doi: 10.1001/jama.288.19.2469. [DOI] [PubMed] [Google Scholar]
- 24.Bakhsh LA, Adas AA, Murad MA, Nourah RM, Hanbazazah SA, Aljahdali AA, et al. Awareness and Knowledge on Hypertension and its Self- Care Practices Among Hypertensive Patients in Saudi Arabia. AIMDR [Internet]. 2017. http://www.aimdrjournal.com/pdf/vol3Issue5/ME13_OA_V3N5.pdf. Accessed 5 Oct 2022.
- 25.Gelaw S, Yenit MK, Nigatu SG. Self-care practice and associated factors among hypertensive patients in debre tabor referral Hospital, Northwest Ethiopia, 2020. Moreira TMM, editor. Int J Hypertens. 2021;11(2021):1–9. doi: 10.1155/2021/3570050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ademe S, Aga F, Gela D. Hypertension self-care practice and associated factors among patients in public health facilities of Dessie town, Ethiopia. BMC Health Serv Res. 2019;19(1):51. doi: 10.1186/s12913-019-3880-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hu H, Li G, Arao T. Prevalence rates of self-care behaviors and related factors in a rural hypertension population: a questionnaire survey. Int J Hypertens. 2013;2013:526949. doi: 10.1155/2013/526949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Labata BG, Ahmed MB, Mekonen GF, Daba FB. Prevalence and predictors of self-care practices among hypertensive patients at Jimma University Specialized Hospital, Southwest Ethiopia: a cross-sectional study. BMC Res Notes. 2019;12(1):86. doi: 10.1186/s13104-019-4125-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.ZinatMotlagh SF, Chaman R, Sadeghi E, Eslami AA. Self-Care Behaviors and Related Factors in Hypertensive Patients. Iran Red Crescent Med J. 2016;18(6):e35805. doi: 10.5812/ircmj.35805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hussen FM, Adem HA, Roba HS, Mengistie B, Assefa N. Self-care practice and associated factors among hypertensive patients in public health facilities in Harar Town, Eastern Ethiopia: a cross-sectional study. SAGE Open Med. 2020;8:2050312120974145. doi: 10.1177/2050312120974145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tibebu A, Bekele DM, Negesa L. Adherence to recommended lifestyle modifications and factors associated with hypertensive patients attending chronic follow-up units of selected public hospitals in Addis Ababa. Ethiopia PPA. 2017;11:323–330. doi: 10.2147/PPA.S126382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Warren-Findlow J, Basalik DW, Dulin M, Tapp H, Kuhn L. Preliminary validation of the Hypertension Self-Care Activity Level Effects (H-SCALE) and clinical blood pressure among patients with hypertension. J Clin Hypertens (Greenwich) 2013;15(9):637–643. doi: 10.1111/jch.12157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Warren-Findlow J, Seymour RB, Brunner Huber LR. The association between self-efficacy and hypertension self-care activities among African American adults. J Community Health. 2012;37(1):15–24. doi: 10.1007/s10900-011-9410-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Schapira MM, Fletcher KE, Hayes A, Eastwood D, Patterson L, Ertl K, et al. The development and validation of the hypertension evaluation of lifestyle and management knowledge scale. J Clin Hypertens (Greenwich) 2012;14(7):461–466. doi: 10.1111/j.1751-7176.2012.00619.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kocalevent RD, Berg L, Beutel ME, Hinz A, Zenger M, Härter M, et al. Social support in the general population: standardization of the Oslo social support scale (OSSS-3) BMC Psychol. 2018;6(1):31. doi: 10.1186/s40359-018-0249-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ritter PL, Lorig K. The English and Spanish self-efficacy to manage chronic disease scale measures were validated using multiple studies. J Clin Epidemiol. 2014;67(11):1265–1273. doi: 10.1016/j.jclinepi.2014.06.009. [DOI] [PubMed] [Google Scholar]
- 37.Kroenke K, Spitzer RL. The PHQ-9: a new depression diagnostic and severity measure. Psychiatr Ann. 2002;32(9):509–515. [Google Scholar]
- 38.Lavsa SM, Holzworth A, Ansani NT. Selection of a validated scale for measuring medication adherence. J Am Pharm Assoc. 2011;51(1):90–94. doi: 10.1331/JAPhA.2011.09154. [DOI] [PubMed] [Google Scholar]
- 39.Khavari KA, Farber PD, Douglass FM. A scale for the indirect assessment of alcohol intake. The alcohol use predictor scale. J Stud Alcohol. 1979;40(7):683–692. doi: 10.15288/jsa.1979.40.683. [DOI] [PubMed] [Google Scholar]
- 40.Dasgupta A, Sembiah S, Paul B, Ghosh A, Biswas B, Mallick N. Assessment of self-care practices among hypertensive patients: a clinic-based study in a rural area of Singur, West Bengal. Int J Community Med Public Health. 2017;5(1):262. [Google Scholar]
- 41.Gebremichael GB, Berhe KK, Beyene BG, Gebrekidan KB. Self-care practices and associated factors among adult hypertensive patients in Ayder Comprehensive Specialized Hospital, Tigray, Ethiopia, 2018. BMC Res Notes. 2019;12(1):489. doi: 10.1186/s13104-019-4502-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Getnet M. Magnitude and determinants of poor self-care practices and associated factors among hypertensive patients attending at Debre Berhan Referral Hospital, Amhara Regional State, Ethiopia. 2021. 10.21203/rs.3.rs-664091/v1.
- 43.Nadewu AN, Geda B. Adherence to Healthy Lifestyle among Hypertensive Patients in Harar Region, Eastern Ethiopia. Prim Health Care [Internet]. 2018. https://www.omicsonline.org/open-access/adherence-to-healthy-lifestyle-among-hypertensive-patients-in-harar-region-eastern-ethiopia-2167-1079-1000308-106554.html. Accessed 6 Oct 2022.
- 44.Mahmud Ahmed S, Belaye TM. Assessment of knowledge, self-care practice, and associated factors among hypertensive patients the public hospital of Addis Ababa Ethiopia 2016 G.C. IJCTS. 2020;6(2):28. [Google Scholar]
- 45.Joseph N, Chiranjeevi M, Sen S, Singh P, Saini M, Beg S. Awareness on hypertension and its self-management practices among hypertensive patients attending outreach clinics of a medical college in South India. Kathmandu Univ Med J (KUMJ) 2016;14(55):202–209. [PubMed] [Google Scholar]
- 46.Bilal M, Haseeb A, Lashkerwala SS, Zahid I, Siddiq K, Saad M, et al. Knowledge, awareness and self-care practices of hypertension among cardiac hypertensive patients. Global J Health Sci. 2016;8(2):9. doi: 10.5539/gjhs.v8n2p9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Abdulwahed A, Seid A. Level of self-care practice and associated factors among hypertensive patients in Jimma University Specialized Hospital, South West Ethiopia. RS. 2020;5(2):12. [Google Scholar]
- 48.Heymann AD, Gross R, Tabenkin H, Porter B, Porath A. Factors associated with hypertensive patients’ compliance with recommended lifestyle behaviors. Sat. 2011;20:21. [PubMed] [Google Scholar]
- 49.Tan FCJH, Oka P, Dambha-Miller H, Tan NC. The association between self-efficacy and self-care in essential hypertension: a systematic review. BMC Fam Pract. 2021;22(1):44. doi: 10.1186/s12875-021-01391-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Bahari G, Scafide K, Krall J, Mallinson RK, Weinstein AA. Mediating role of self-efficacy in the relationship between family social support and hypertension self-care behaviors: a cross-sectional study of Saudi men with hypertension. Int J Nurs Pract. 2019;25(6):e12785. doi: 10.1111/ijn.12785. [DOI] [PubMed] [Google Scholar]
- 51.Sung KW, Kim MH. Self-care behaviors and depressive symptoms of low-income elderly women with hypertension. J Korean Acad Nurs. 2008;38(4):593. doi: 10.4040/jkan.2008.38.4.593. [DOI] [PubMed] [Google Scholar]
- 52.Larki A, Tahmasebi R, Reisi M. Factors predicting self-care behaviors among low health literacy hypertensive patients based on health belief model in Bushehr District, South of Iran. Int J Hypertens. 2018;2018:1–7. doi: 10.1155/2018/9752736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.World Medical Association World Medical Association Declaration of Helsinki. Ethical principles for medical research involving human subjects. Bull World Health Organ. 2001;79(4):373. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data and materials are available from the corresponding author without undue reservation.